Summary
Marfan syndrome is an autosomal dominant connective tissue disorder, predominantly affecting the ocular, skeletal and cardiovascular systems. Here, we present the results of the first genetic testing in 40 Ukrainian Marfan (-like) patients and 10 relatives. We applied a targeted next generation sequencing panel comprising FBN1 and 13 thoracic aortic aneurysm genes. We identified 27 causal mutations in FBN1, obtaining a mutation yield of 67·5%. A significant difference in age at aortic surgery between mutation positive and negative patients was observed. Thus, we conclude that genetic testing is important to identify patients at higher risk for developing life-threatening cardiovascular complications.
1. Introduction
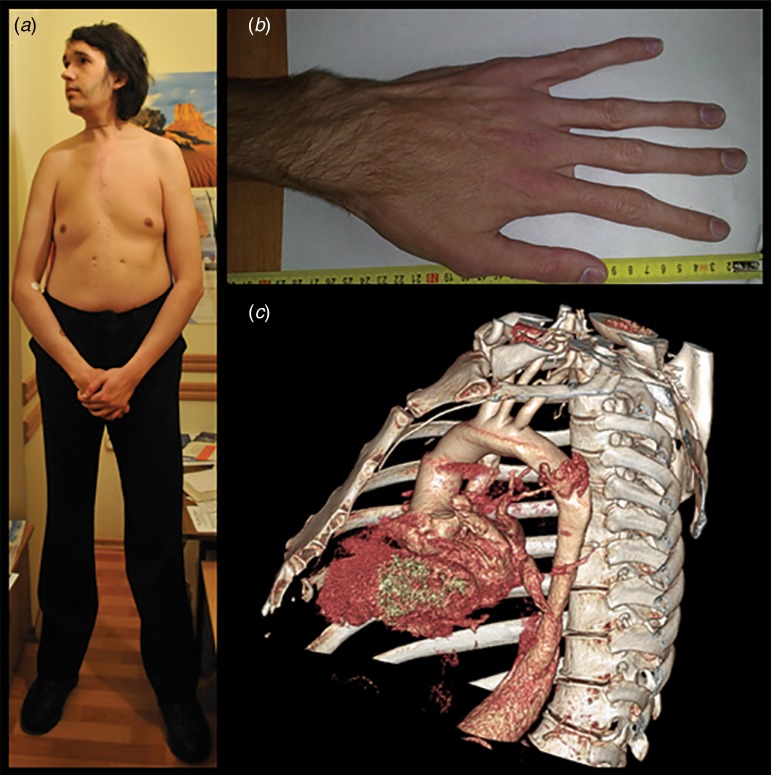
Marfan syndrome (MFS) (OMIM#154700) is an autosomal dominant connective tissue disorder with a prevalence of 0·075 to 0·86 per 5000 individuals (von Kodolitsch et al., 2015). MFS is a multisystemic disorder involving the ocular, skeletal and cardiovascular systems. Myopia and lens dislocation are the most common ocular features, while skeletal involvement is characterized by long bone overgrowth, pectus deformity and arachnodactyly (Fig. 1(a) and (b)). However, the most life-threatening complications in MFS are related to the cardiovascular system (Fig. 1(c)). These include aortic root dilatation primarily at the level of the sinuses of Valsalva, aortic dissection and rupture, mitral valve prolapse, mitral regurgitation and arrhythmias (Van Laer et al., 2013; Cherkas et al., 2016). In 1991, the fibrillin-1 gene (FBN1), which encodes a 350 kDa glycoprotein, was identified as the gene responsible for MFS (Dietz et al., 1991). Fibrillin-1, as a part of the extracellular matrix (ECM), provides elasticity and structural support to tissues and plays an important role in TGF-β signalling. Thus, mutations in FBN1 lead to a loss of ECM integrity and to a dysregulation of the downstream TGF-β signalling pathway (Neptune et al., 2003; Ramachandra et al., 2015).
Fig. 1.
Clinical features of MFS. Typical MFS patients with (a) disproportionate long bone overgrowth, (b) arachnodactyly and (c) thoracic aortic aneurysm.
In 80 to 100% of MFS patients, a FBN1 mutation can be identified (Loeys et al., 2004; Faivre et al., 2011; Radonic et al., 2011; Sheikhzadeh et al., 2011; Aalberts et al., 2012; Yang et al., 2012; Proost et al., 2015; von Kodolitsch et al., 2015). Despite the presence of identical mutations, a large inter- and intra-familial phenotypic variability is observed, suggesting that modifiers may be involved (Van Laer et al., 2013). Genetic testing is important, as on the one hand, the identification of a pathogenic FBN1 mutation can be very helpful to establish an adequate treatment and management scheme for the proband and affected family members. On the other hand, unaffected family members can be reassured and be released from further clinical follow-up. Here, we present the first genetic testing in a Ukrainian cohort of 40 MFS probands and 10 family members.
2. Materials and methods
Probands in this study were consecutive patients derived from the two largest cardiovascular centres of Ukraine, accessible to all Ukranians. The probands were referred for evaluation of aortic root aneurysm or aortic root surgery. As such, this group is most probably biased towards more extreme cardiovascular phenotypes, but can be considered as representative for the Ukranian population (Zhuraev et al., 2014). All probands and their family members underwent a thorough clinical examination, including a slitlamp exam and physical exam. Based on the clinical findings, the systemic score was calculated according to www.marfan.org/dx/score. Twenty-eight patients met the diagnostic criteria for MFS, based on the original and revised Ghent nosology (www.marfan.org/dx/rules) (De Paepe et al., 1996; Loeys et al., 2010), while 12 were suspected of a MFS-related syndrome. None of the individuals refused inclusion in the study, but three probands were excluded because their DNA was of insufficient quality. The local ethical committee approved the clinical and genetic program for MFS.
Probands were screened with a next generation sequencing (NGS) panel, comprising 14 genes involved in thoracic aortic aneurysms (TAA) (Proost et al., 2015). Enrichment of the regions of interest was performed with a custom Haloplex target enrichment kit according to the supplier's protocol (Agilent Technologies, Santa Clara, CA), followed by NGS on MiSeq (Illumina, San Diego, CA) using 150 bp paired-end sequencing reads. Next, data analysis was performed with a tailored pipeline and our in-house developed VariantDB was used to annotate and interpret the variants (Vandeweyer et al., 2014; Proost et al., 2015). Decisions on the pathogenicity of variants were based on their presence in specific mutation databases, including Human Gene Mutation Database (HGMD) (www.hgmd.cf.ac.uk) and Universal Mutation Database (UMD) FBN1 (www.umd.be/FBN1/), which also contain the relevant links to the literature and/or on the functional importance of specific residues and their conservation across the TGF-β binding (TB) and the (calcium-binding) epidermal growth factor (EGF)-like domains as demonstrated in Supplementary Tables S1(a)–(c) (e.g., the conserved cysteine residues in EGF-like domains and the first four amino acids of the EGF-like domain, the so-called DIDE motif).
The variants found with NGS were confirmed by Sanger sequencing using the BigDye® Terminator Cycle Sequencing kit (Applied Biosystems, Life Technologies, Carlsbad, CA), followed by capillary electrophoresis on an ABI3130XL (Applied Biosystems). Multiplex ligation-dependent probe amplification (MLPA) was performed on samples that remained negative after TAA NGS panel testing.
We performed statistical analysis for possible genotype/phenotype correlations in the FBN1 mutation positive and mutation negative groups using the Mann–Whitney U-test for continuous variables and the Fisher's exact test for categorical variables. The patients carrying a variant of unknown significance (VUS) in TGFBR1 and FLNA (patient 1 and 22, respectively) were excluded from this analysis. The patients carrying both a FBN1 mutation and one or more VUS were placed in the mutation positive group.
3. Results and discussion
Of the 40 probands, 27 had causal mutations in FBN1, one patient had a VUS in TGFBR1, and one patient had a VUS in FLNA. In addition to the FBN1 mutation, four patients had additional variants in either FBN1, SMAD3, FLNA or NOTCH1 (Table 1). At this moment, we cannot exclude that these VUS may modify the phenotype caused by the FBN1 mutation. Of the 27 mutations in FBN1, 12 were missense, 11 predicted a premature termination codon (nine nonsense and two frameshifts) and four affected splice sites. Ten of these FBN1 variants were novel. Except one (c.3845A > G; p.Asn1282Ser in patient 17), the FBN1 mutations were not present in the ExAC database (Table 1). No large deletions/duplications could be detected by MLPA.
Table 1.
Mutation or VUS positive probands.
| # | Exon | Gene | cDNA base change | Predicted amino acid change | Type of mutation; domaina | Predictionb MutationTaster, PolyPhen-2 and Sift | Previously describedc | ExAC Frequency |
|---|---|---|---|---|---|---|---|---|
| MFS patients | ||||||||
| 2 | 14 | FBN1 | c.1709G > A | p.Cys570Tyr | Missense mutation; conserved cys in calcium-binding EGF-like#8 | P (0·999), P (0·997), P (0·002) | CM013918; UMD | / |
| 3 | 44 | FBN1 | c.5368C > T | p.Arg1790* | Nonsense mutation | P (1·000), NA, NA | CM054694; UMD | / |
| 25 | FBN1 | c.2956G > A | p.Ala986Thr | VUS | P (0·999), P (0·458), B (0·100) | UMD | 0·001508 | |
| 4 | Intron 51 | FBN1 | c.6313 + 3insT | / | Splice site mutation | NA | CS022105 | / |
| 5 | Intron 37 | FBN1 | c.4582 + 1G > T | / | Splice site mutation | NA | Novel | / |
| 6 | 64 | FBN1 | c.7828G > A | p.Glu2610Lys | Missense mutation, DIDE consensus sequenced | P (0·999), P (0·999), P (0·003) | CM972822; UMD | / |
| 7 | Intron 13 | FBN1 | c.1589–1G > A | / | Splice site mutation | NA | Novel | / |
| 8 | 10 | FBN1 | c.1090C > T | p.Arg364* | Nonsense mutation | P (1·000), NA, NA | CM032224; UMD | / |
| 9 | 55 | FBN1 | c.6629G > A | p.Cys2210Tyr | Missense mutation; conserved cys in calcium-binding EGF-like#38 | P (0·999), P (0·997), P (0·000) | Novel | / |
| 10 | 34 | FBN1 | c.4096G > A | p.Glu1366Lys | Missense mutation, DIDE consensus sequenced | P (0·999), P (0·995), P (0·980) | CM040037; UMD | / |
| 25 | FBN1 | c.2956G > A | p.Ala986Thr | VUS | P (0·999), P (0·458), B (0·100) | UMD | 0·001508 | |
| 12 | 49 | FBN1 | c.5947A > T | p.Lys1983* | Nonsense mutation | P (1·000), NA, NA | Novel | / |
| 13 | 38 | FBN1 | c.4621C > T | p.Arg1541* | Nonsense mutation | P (1·000), NA, NA | CM993159; UMD | / |
| 14 | 4 | FBN1 | c.254G > T | p.Cys85Phe | Missense mutation; conserved cys in EGF-like#1 | P (1·000), P (0·999), P (1·000) | Novel | / |
| 16 | 25 | FBN1 | c.2963G > A | p.Trp988* | Nonsense mutation | P (1·000), NA, NA | UMD | / |
| 17 | 32 | FBN1 | c.3845A > G | p.Asn1282Ser | Missense mutation, DIDE consensus sequenced | P (0·757), P (0·803), P (0·970) | CM972807; UMD | 0·0000742 |
| 9 | SMAD3 | c.1269T > G | p.Ser423Arg | VUS | P (0·999), P (0·980), P (0·002) | Novel | / | |
| 19 | 32 | FBN1 | c.3960T > A | p.Cys1320* | Nonsense mutation | P (1·000), NA, NA | CM054723; UMD | / |
| 20 | 63 | FBN1 | c.7712G > A | p.Cys2571Tyr | Missense mutation; conserved cys in calcium-binding EGF-like#45 | P (1·000), P (0·999), P (1·000) | Novel | / |
| 23 | 58 | FBN1 | c.7180C > T | p.Arg2394* | Nonsense mutation | P (1·000), NA, NA | CM993162; UMD | / |
| 24 | 22 | FBN1 | c.2639G > A | p.Gly880Asp | Missense mutation | P (1·000, P (1·000), P (1·000) | UMD | / |
| 25 | 35 | FBN1 | c.4222T > C | p.Cys1408Arg | Missense mutation; conserved cys in calcium-binding EGF-like#24 | P (1·000), P (0·999), P (1·000) | CM098517; UMD | / |
| 26 | 66 | FBN1 | c.8352_8353insT | p.Thr2785Tyrfs*16 | Frameshift mutation | NA | Novel | / |
| 27 | Intron 16 | FBN1 | c.1960 + 1G > A | / | Splice site mutation | NA | UMD | / |
| 34 | NOTCH1 | c.6413C > T | p.Pro2138Leu | VUS | P (0·999), P (0·494), B (0·599) | Novel | 0·000008763 | |
| 2 | FLNA | c.182G > A (A/–) | p.Ser61Asn | VUS | P (0·824), B (0·000), B (1·000) | Novel | / | |
| 28 | 64 | FBN1 | c.7831T > C | p.Cys2611Arg | Missense mutation; conserved cys in calcium-binding EGF-like#45 | P (1·000), P (0·998), P (1·000) | Novel | / |
| 29 | 4 | FBN1 | c.254G > A | p.Cys85Tyr | Missense mutation; conserved cys in EGF-like#1 | P (1·000), P (0·999), P (1·000) | Novel | / |
| MFS-like patients | ||||||||
| 1 | 4 | TGFBR1 | c.709A > G | p.Arg237Gly | VUS | P (0·999); P (0·997); P (0·002) | Novel | / |
| 11 | 63 | FBN1 | c.7754T > C | p.Ile2585Thr | Missense mutation | P (0·999), P (0·642), B (0·543) | CM972820; UMD | / |
| 15 | 61 | FBN1 | c.7549C > T | p.Gln2517* | Nonsense mutation | P (1·000), NA, NA | Novel | / |
| 18 | 58 | FBN1 | c.7039_7040delAT | p.Met2347 fs*19 | Frameshift mutation | NA | CD020234; UMD | / |
| 21 | 14 | FBN1 | c.1693C > T | p.Arg565* | Nonsense mutation | P (1·000), NA, NA | CM950438; UMD | / |
| 22 | 22 | FLNA | c.3421G > A (A/−) | p.Ala1141Thr | VUS | P (0·999), P (0·939), B (0·051) | Novel | 0·0003147 |
Nucleotide numbering uses +1 as the A of the ATG translation initiation codon in the reference sequence, with the initiation codon as codon 1. Patient numbers are in accordance with the patient numbers in Table 2.
: not present in ExAC B: benign; NA: not available; P: pathogenic.
Numbering of domains is based on Uniprot entry: P35555 (see Supplementary Table S1(a)–(c) for the relevant alignments).
dbSNFP, integrated into the VariantDB annotation tool (Vandeweyer et al., 2014), was used to automatically generate the prediction scores of MutationTaster, Polyphen-2 and SIFT respectively, as described by Liu et al., 2011.
In the UMD FBN1 (www.umd.be/FBN1/) or in the HGMD (public part: www.hgmd.cf.ac.uk/ac).
DIDE consensus sequence: Asp–Ile–Asp–Glu (see Supplementary Table S1(a)).
As our TAA NGS assay has a validated high sensitivity, and as MLPA excluded the presence of large deletions/insertions, we can largely rule out the possibility of false negatives in the coding regions. Only deep intronic mutations and mutations in the 5´- and 3´-untranslated regions will remain undetected with the applied methodology, but we expect that these account for only a minor fraction of all MFS patients. Thus, a possible explanation for the relatively low yield may be the fact that several mutation negative probands did not fulfill the diagnostic criteria for MFS. Indeed, of the 27 FBN1-positive probands, only 15% (four out of 27) had a systemic score below seven, while this was 67% (six out of nine) for the nine FBN1-negative probands. Furthermore, only one of the 15 FBN1 negative patients did present ectopia lentis. As such, more Marfan-like than true Marfan (fulfilling clinical diagnostic criteria) presentations were present in the FBN1-negative group. Moreover, Marfan-like patients that remained negative with the gene panel, may carry mutations in more recently identified TAA genes or yet to be identified TAA genes.
For six of the probands, DNA of family members was available and segregation analysis was performed. The p.Cys570Tyr mutation (patient 2) was found in three additional affected family members (Table 2). Although all family members presented with ectopia lentis, only two have undergone aortic surgery (ages 20 years and 33 years). Also the p.Ile2585Thr (patient 11), the p.Arg2394* (patient 23) and the p.Cys85Tyr (patient 29) mutations segregated with the MFS phenotype in four additional family members. The truncating mutation (p.Lys1983*) identified in patient 12 was also found in his mother. She had no aortic root dilatation, but presented with mitral valve prolapse and skeletal features including wrist sign, pectus carinatum and tall stature. As a direct result of our genetic testing, she is now in regular cardiovascular follow-up and has been started on losartan in order to delay future aortic surgery.
Table 2.
Clinical data of 40 MFS probands and their family members.
| Patient | Gender | Diagnosis | Mutation | Systemic score | Surgery | Surgery aortic root (mm) | Age at surgery | Ectopia lentis |
|---|---|---|---|---|---|---|---|---|
| MFS patients and their relatives | ||||||||
| 2·1 | F | MFS | FBN1: p.Cys570Tyr | 10 | Yes | 63 | 20 | Yes |
| 2·2 | M | MFS | FBN1: p.Cys570Tyr | 11 | Yes | 73 | 33 | Yes |
| 2·3 | M | MFS | FBN1: p.Cys570Tyr | 8 | No | / | / | Yes |
| 2·4 | F | MFS | FBN1: p.Cys570Tyr | 7 | No | / | / | Yes |
| 3 | F | MFS | FBN1: p.Arg1790*, | 8 | Yes | 53 | 41 | No |
| FBN1: p.Ala986Thr | ||||||||
| 4 | M | MFS | FBN1: c.6313 + 3insT | 11 | Yes | 79 | 28 | No |
| 5 | M | MFS | FBN1: c.4582 + 1G > T | 11 | Yes | 59 | 32 | Yes |
| 6 | F | MFS | FBN1: p.Glu2610Lys | 7 | Yes | 67 | 25 | No |
| 7 | M | MFS | FBN1: c.1589–1G > A | 13 | Yes | 64 | 33 | No |
| 8 | F | MFS | FBN1: p.Arg364* | 8 | Yes | 66 | 31 | No |
| 9 | F | MFS | FBN1: p.Cys2210Tyr | 9 | Yes | 62 | 42 | No |
| 10 | M | MFS | FBN1: p.Glu1366Lys, | 12 | Yes | 72 | 40 | No |
| FBN1: p.Ala986Thr | ||||||||
| 12·1 | M | MFS | FBN1: p.Lys1983* | 11 | Yes | 57 | 22 | No |
| 12·2 | F | MFS | FBN1: p.Lys1983* | 6 | No | / | / | No |
| 13 | M | MFS | FBN1: p.Arg1541* | 9 | Yes | 70 | 52 | No |
| 14 | M | MFS | FBN1: p.Cys85Phe | 12 | Yes | 73 | 22 | Yes |
| 16 | F | MFS | FBN1: p.Trp988* | 9 | Yes | 72 | 25 | No |
| 17 | M | MFS | FBN1: p.Asn1282Ser, | 9 | Yes | 78 | 29 | No |
| SMAD3: p.Ser423Arg | ||||||||
| 19 | M | MFS | FBN1: p.Cys1320* | 11 | Yes | 65 | 32 | No |
| 20 | M | MFS | FBN1: p.Cys2571Tyr | 9 | Yes | 71 | 19 | Yes |
| 23·1 | F | MFS | FBN1: p.Arg2394* | 8 | Yes | 60 | 32 | Yes |
| 23·2 | F | MFS | FBN1: p.Arg2394* | 7 | No | / | / | Yes |
| 24 | M | MFS | FBN1: p.Gly880Asp | 9 | No | / | / | Yes |
| 25 | M | MFS | FBN1: p.Cys1408Arg | 7 | Yes | 110 | 24 | Yes |
| 26·1 | F | MFS | FBN1: p.Thr2785Tyr fs*16 | 14 | Yes | 79 | 24 | No |
| 26·2 | F | Unaffected | No | 3 | No | / | / | No |
| 26·3 | M | Unaffected | No | 2 | No | / | / | No |
| 27 | M | MFS | FBN1: c.1960 + 1G > A, | 13 | Yes | 64 | 35 | Yes |
| NOTCH1: p.Pro2138Leu, | ||||||||
| FLNA: p.Ser61Asn | ||||||||
| 28 | M | MFS | FBN1: p.Cys2611Arg | 9 | Yes | 90 | 23 | No |
| 29·1 | F | MFS | FBN1: p.Cys85Tyr | 6 | Yes | 61 | 39 | Yes |
| 29·2 | F | MFS | FBN1: p.Cys85Tyr | 11 | No | / | / | Yes |
| 29·3 | M | MFS | FBN1: p.Cys85Tyr | 5 | No | / | / | Yes |
| 31 | M | MFS | No | 10 | Yes | 65 | 49 | No |
| 32 | M | MFS | No | 11 | Yes | 78 | 31 | No |
| 33 | M | MFS | No | 11 | Yes | 68 | 37 | No |
| 34 | M | MFS | No | 10 | No | / | / | No |
| 40 | M | MFS | No | 11 | Yes | 120 | 31 | Yes |
| MFS-like and their relatives | ||||||||
| 1 | M | MFS-like | TGFBR1: p.Arg237Gly | 6 | Yes | 67 | 42 | No |
| 11·1 | F | MFS-like | FBN1: p.Ile2585Thr | 3 | Yes | 70 | 49 | No |
| 11·2 | M | MFS-like | FBN1: p.Ile2585Thr | 5 | No | / | / | No |
| 15 | M | MFS-like | FBN1: p.Gln2517* | 5 | Yes | 57 | 43 | No |
| 18 | F | MFS-like | FBN1: p.Met2347 fs*19 | 5 | Yes | 64 | 48 | No |
| 21 | M | MFS-like | FBN1: p.Arg565* | 6 | Yes | 74 | 30 | No |
| 22 | M | MFS-like | FLNA: p.Ala1141Thr | 3 | Yes | 70 | 57 | No |
| 30 | F | MFS-like | No | 2 | Yes | 78 | 43 | No |
| 35 | M | MFS-like | No | 2 | Yes | 73 | 45 | No |
| 36 | M | MFS-like | No | 4 | Yes | 50 | 46 | No |
| 37 | M | MFS-like | No | 6 | No | / | / | No |
| 38 | M | MFS-like | No | 4 | Yes | 57 | 64 | No |
| 39 | M | MFS-like | No | 4 | Yes | 67 | 64 | No |
Patient numbers are in accordance with the patient numbers in Table 1 and suffixes indicate family members.
: no surgery.
Next, statistical analysis for possible genotype/phenotype correlations was performed (Table 3). We found a significant difference between the FBN1 mutation positive and mutation negative patients for the age at surgery (Mann–Whitney U, p = 0·006) and the presence of ectopia lentis (Fisher's exact test, p = 0·036). Patients with a mutation in FBN1 had aortic surgery at an earlier age (32 years on average) than mutation negative patients (46 years on average). This emphasizes the importance of genetic screening for the identification of patients that are at higher risk for developing aortic aneurysms and dissection. According to the literature, a higher frequency of truncating and splicing variants in FBN1 can be observed in patients with an aortic event (Baudhuin et al., 2015). In our cohort, no significant difference could be observed between truncating or splice variants and missense variants in patients with an aortic event (Fisher's exact test, p = 0·282). Of course, our study was not sufficiently powered to detect such differences.
Table 3.
Clinical data of 38 MFS probands and their family members.
| Mutation | |||
|---|---|---|---|
| Negative | Positive | p-value | |
| Male | 11 | 20 | 0·099 |
| Female | 2 | 15 | 0·099 |
| Surgery | 9 | 27 | 0·710 |
| Aortic diameter at surgery (mm) | 73 | 69 | 0·693 |
| Age at surgery | 46 | 32 | 0·006 |
| Ectopia lentis | 1 | 15 | 0·036 |
4. Conclusion
In conclusion, we identified FBN1 gene mutations in Ukrainian MFS patients for the first time. Since the clinical picture of these patients is not always clear, genetic screening can help to establish a diagnosis and to identify patients at high risk for developing life-threatening complications such as aortic aneurysm and dissection.
Acknowledgments
We are grateful to all patients who participated in this study. B. L. Loeys is senior clinical investigator and J. A. N. Meester is a predoctoral researcher of the Fund for Scientific Research, Flanders (FWO, Belgium). This research was supported by funding from the University of Antwerp (Lanceringsproject), the Fund for Scientific Research, Flanders (FWO, Belgium) (G.0221·12), an ERC starting grant to B. L. Loeys and the Hercules Foundation.
Declaration of interest
None.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0016672316000112.
click here to view supplementary material
References
- Aalberts J. J., Thio C. H., Schuurman A. G., van Langen I. M., van der Pol B. A., van Tintelen J. P. & van den Berg M. P. (2012). Diagnostic yield in adults screened at the Marfan outpatient clinic using the 1996 and 2010 Ghent nosologies. American Journal of Medical Genetics. Part A 158A, 982–988. [DOI] [PubMed] [Google Scholar]
- Baudhuin L. M., Kotzer K. E. & Lagerstedt S. A. (2015). Increased frequency of FBN1 truncating and splicing variants in Marfan syndrome patients with aortic events. Genetics in Medicine 17, 177–187. [DOI] [PubMed] [Google Scholar]
- Cherkas A. & Zhuraev R. (2016). A marked decrease in heart rate variability in Marfan syndrome patients with confirmed FBN1 mutations. Cardiology Journal 23, 23–33. [DOI] [PubMed] [Google Scholar]
- De Paepe A., Devereux R. B., Dietz H. C., Hennekam R. C. & Pyeritz R. E. (1996). Revised diagnostic criteria for the Marfan syndrome. American Journal of Medical Genetics 62, 417–426. [DOI] [PubMed] [Google Scholar]
- Dietz H. C., Cutting G. R., Pyeritz R. E., Maslen C. L., Sakai L. Y., Corson G. M., Puffenberger E. G., Hamosh A., Nanthakumar E. J. & Curristin S. M. (1991). Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature 352, 337–339. [DOI] [PubMed] [Google Scholar]
- Faivre L., Collod-Beroud G., Ades L., Arbustini E., Child A., Callewaert B., Loeys B., Binquet C., Gautier E., Mayer K., Arslan-Kirchner M., Grasso M., Beroud C., Hamroun D., Bonithon-Kopp C., Plauchu H., Robinson P. N., De Backer J., Coucke P., Francke U., Bouchot O., Wolf J. E., Stheneur C., Hanna N., Detaint D., De Paepe A., Boileau C. & Jondeau G. (2011). The new Ghent criteria for Marfan syndrome: what do they change? Clinical Genetics 81, 433–442. [DOI] [PubMed] [Google Scholar]
- Liu X., Jian X. & Boerwinkle E. (2011). dbNSFP: a lightweight database of human nonsynonymous SNPs and their functional predictions. Human Mutation 32, 894–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeys B. L., Dietz H. C., Braverman A. C., Callewaert B. L., De Backer J., Devereux R. B., Hilhorst-Hofstee Y., Jondeau G., Faivre L., Milewicz D. M., Pyeritz R. E., Sponseller P. D., Wordsworth P. & De Paepe A. M. (2010). The revised Ghent nosology for the Marfan syndrome. Journal of Medical Genetics 47, 476–485. [DOI] [PubMed] [Google Scholar]
- Loeys B., De Backer J., Van Acker P., Wettinck K., Pals G., Nuytinck L., Coucke P. & De Paepe A. (2004). Comprehensive molecular screening of the FBN1 gene favors locus homogeneity of classical Marfan syndrome. Human Mutation 24, 140–146. [DOI] [PubMed] [Google Scholar]
- Neptune E. R., Frischmeyer P. A., Arking D. E., Myers L., Bunton T. E., Gayraud B., Ramirez F., Sakai L. Y. & Dietz H. C. (2003). Dysregulation of TGF-beta activation contributes to pathogenesis in Marfan syndrome. Nature Genetics 33, 407–411. [DOI] [PubMed] [Google Scholar]
- Proost D., Vandeweyer G., Meester J. A., Salemink S., Kempers M., Ingram C., Peeters N., Saenen J., Vrints C., Lacro R. V., Roden D., Wuyts W., Dietz H. C., Mortier G., Loeys B. L. & Van Laer L. (2015). Performant mutation identification using targeted next generation sequencing of 14 thoracic aortic aneurysm genes. Human Mutation 36, 808–814. [DOI] [PubMed] [Google Scholar]
- Radonic T., de Witte P., Groenink M., de Bruin-Bon R., Timmermans J., Scholte A., van den Berg M., Baars M., van Tintelen J., Kempers M., Zwinderman A. & Mulder B. (2011). Critical appraisal of the revised Ghent criteria for diagnosis of Marfan syndrome. Clinical Genetics 80, 346–353. [DOI] [PubMed] [Google Scholar]
- Ramachandra C. J., Mehta A., Guo K. W., Wong P., Tan J. L. & Shim W. (2015). Molecular pathogenesis of Marfan syndrome. International Journal of Cardiology 187, 585–591. [DOI] [PubMed] [Google Scholar]
- Sheikhzadeh S., Kade C., Keyser B., Stuhrmann M., Arslan-Kirchner M., Rybczynski M., Bernhardt A. M., Habermann C. R., Hillebrand M., Mir T., Robinson P. N., Berger J., Detter C., Blankenberg S., Schmidtke J. & von Kodolitsch Y. (2011). Analysis of phenotype and genotype information for the diagnosis of Marfan syndrome. Clinical Genetics 82, 240–247. [DOI] [PubMed] [Google Scholar]
- Van Laer L., Proost D. & Loeys B. L. (2013). Educational paper. Connective tissue disorders with vascular involvement: from gene to therapy. European Journal of Pediatrics 172, 997–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandeweyer G., Van Laer L., Loeys B., Van den Bulcke T. & Kooy R. F. (2014). VariantDB: a flexible annotation and filtering portal for next generation sequencing data. Genome Medicine 6, 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Kodolitsch Y., De Backer J., Schuler H., Bannas P., Behzadi C., Bernhardt A. M., Hillebrand M., Fuisting B., Sheikhzadeh S., Rybczynski M., Kölbel T., Püschel K., Blankenberg S. & Robinson P. N. (2015). Perspectives on the revised Ghent criteria for the diagnosis of Marfan syndrome. The Application of Clinical Genetics 8, 137–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J. H., Han H., Jang S. Y., Moon J. R., Sung K., Chung T. Y., Lee H. J., Ki C. S. & Kim D. K. (2012). A comparison of the Ghent and revised Ghent nosologies for the diagnosis of Marfan syndrome in an adult Korean population. American Journal of Medical Genetics. Part A 158A, 989–995. [DOI] [PubMed] [Google Scholar]
- Zhuraev R. K. & Zerbino D. D. (2014). Marfan syndrome: clinical and pathomorphological restructurings after surgical treatment of aortic aneurysm. Angiologii͡a i Sosudistai͡a Khirurgii͡a 20, 14–20. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0016672316000112.
click here to view supplementary material