Abstract
Background
Peripheral facial nerve palsy is the most common functional disturbance of a cranial nerve. 60–75% of cases are idiopathic.
Methods
This review is based on a selective literature search proceeding from the current, updated German-language guideline on the diagnosis and treatment of idiopathic facial nerve palsy.
Results
The recommended drug treatment consists of prednisolone 25 mg bid for 10 days, or 60 mg qd for 5 days followed by a taper to off in decrements of 10 mg per day. This promotes full recovery (number needed to treat [NNT] = 10; 95% confidence interval [6; 20]) and lessens the risk of late sequelae such as synkinesia, autonomic disturbances, and contractures. Virostatic drugs are optional in severe cases (intense pain or suspicion of herpes zoster sine herpete) and mandatory in cases of varicella-zoster virus (VZV) infection. Corneal protection with dexpanthenol ophthalmic ointment, artificial tears, and a nocturnal moisture-retaining eye shield has been found useful in practice. In cases of incomplete recovery with residual facial weakness, both static and microsurgical dynamic methods can be used to restore facial nerve function.
Conclusion
Because 25–40% of cases of facial nerve palsy are not idiopathic, differential diagnosis is very important; key diagnostic methods include a clinical neurological examination, otoscopy, and a lumbar puncture for cerebrospinal fluid examination. High-level evidence supports corticosteroid treatment for the idiopathic form of the disorder.
Facial nerve palsy is the most common cranial nerve disease. Its idiopathic form (Bell’s palsy) accounts for 60–75% of cases. 7–40 cases arise per 100 000 persons per year; the incidence is similar in men and women (1– 3). The incidence may be higher in pregnant women and lower in children (e1– e3). Early diagnosis and the immediate initiation of treatment once a diagnosis has been made can improve the outcome (4). Nonetheless, treatment in routine clinical practice is highly variable at present and has been criticized as inadequate and in need of improvement (3, 5, 6).
Learning objectives
This article is intended to enable the reader to:
determine and assess the clinical manifestations of the disorder
know the main differential diagnoses
know the principles of pharmacological and non-pharmacological treatment
gain an overview of the optimal treatment for residual disturbances of facial nerve function.
Method
This review is based on publications retrieved by a selective search in the PubMed and Cochrane Library databases and on the updated German-language guideline on the diagnosis and treatment of idiopathic facial nerve palsy (2017) (7). The search was for meta-analyses and randomized clincal trials from the years 2013–2017 containing the key words “facial palsy,” “Bell’s palsy,” “facial paralysis,” or “facial paresis.”
History and physical examination
Incidence.
Facial nerve palsy is the most common cranial nerve disease. Its idiopathic form (Bell’s palsy) accounts for 60–75% of cases. 7–40 cases arise per 100 000 persons per year; the incidence is similar in men and women.
Idiopathic facial nerve palsy usually manifests itself as sudden weakness of the muscles of facial expression on one side of the face. It is often first noticed by the patient upon looking in a mirror, or by members of the patient’s family. Drooling from the corner of the mouth can also be the initial symptom. Simultaneously with the onset of weakness, patients often report pain behind the ear and paresthesia on the ipsilateral cheek. An abnormality of taste and, more rarely, hyperacusis can also be present as accompaniments to the main symptom (paresis) (1).
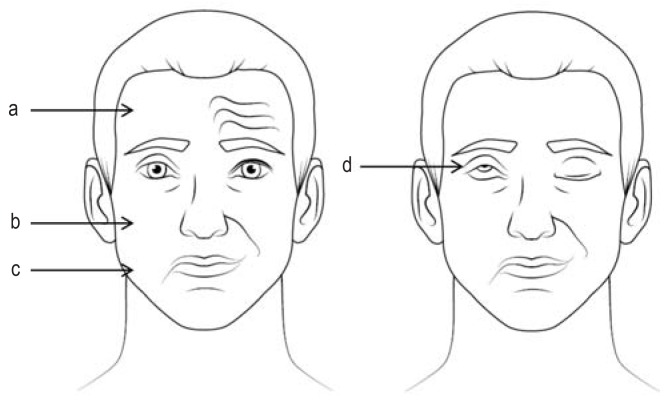
Peripheral facial nerve palsy can be distinguished clinically from central facial palsy (e.g., due to stroke) by its involvement of the muscles of the forehead as well (figure 1) (e4, e5). If the frontalis muscle functions normally, but the middle and lower portions of the face are affected, the lesion is probably central (supranuclear), because the portion of the facial nerve nucleus subserving the frontalis muscle receives afferent input from both cerebral hemispheres and therefore keeps functioning normally in the presence of a unilateral central lesion (e4). The typical features of peripheral facial nerve palsy are a lack of wrinkling of the forehead, low eyebrow position (eyebrow ptosis), incomplete lid closure, hanging corner of the mouth, and a flattened nasolabial fold (figure 1). An incomplete, mainly perioral peripheral facial nerve palsy may be difficult to distinguish from a central facial palsy.
Figure 1.
Clinical features of right-sided peripheral facial nerve palsy: a) lessened innervation of the forehead; b) flattened nasolabial fold; c) drooping corner of mouth; d) impaired lid closure with Bell phenomenon when the patient is asked to close the eyes.
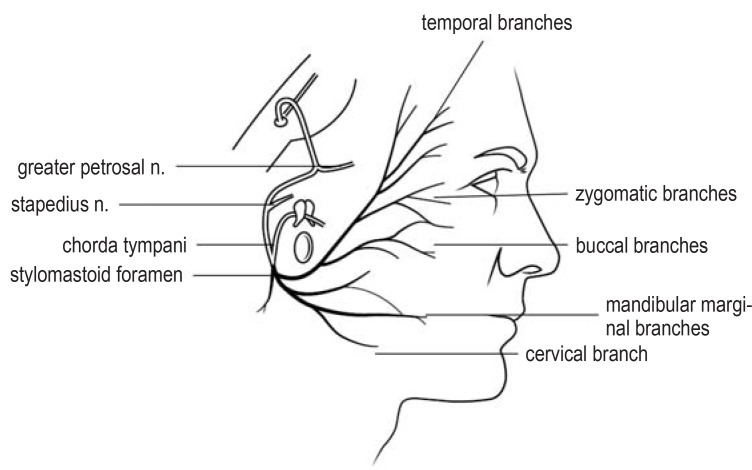
Because of the complex anatomy of the seventh cranial nerve (figure 2) (e6), the manifestations of a partial or total loss of facial nerve function can be highly variable. Important criteria for facial nerve function include lid closure, hearing, the secretion of tears and saliva, and taste. Incomplete lid closure and a pathologically altered tear film—especially when accompanied by corneal hypesthesia, as in 10% of cases—are associated with a risk of corneal ulceration (1). Dysfunction of the stapedius muscle, which is innervated by a branch of the facial nerve, causes hypersensitivity to low-frequency sounds (hyperacusis); patients often also describe a disturbance of taste on one side, manifesting itself as an unpleasant, abnormal sensation while eating (8). It is important to determine by physical examination whether any additional neurological deficits are present that are not due to facial nerve dysfunction.
Figure 2.
Course and branches of the facial nerve. The intracranial course is shown as transparent (modified from [e6]; with the kind permission of Thieme).
Initial manifestations.
Idiopathic facial nerve palsy usually manifests itself as sudden weakness of the muscles of facial expression on one side of the face. It is often first noticed by the patient upon looking in a mirror, or by members of the patient’s family.
The severity of facial nerve palsy is usually rated on the six-point House and Brackmann scale, with grade I corresponding to normal facial nerve function and grade VI corresponding to complete paralysis (table 1) (9). Further rating scales (the Stennert index, the Sunnybrook scale) and standardized photographic and video documentation are used mainly for follow-up of residual weakness and after facial nerve reanimation surgery (10, e7).
Table 1. The House and Brackmann scale for the severity of peripheral facial nerve palsy.
| Grade | Description | Finding at rest | Forehead innervation | Lid closure | Mouth innervation |
| I | normal | normal | normal | normal | normal |
| II | mild dysfunction | normal | reduced | nearly normal | nearly normal |
| III | moderate dysfunction | normal | still barely possible | still barely possible | reduced |
| IV | moderately severe dysfunction | normal | none | incomplete | asymmetrical |
| V | severe dysfunction | asymmetrical | none | incomplete | asymmetrical |
| VI | total paralysis | complete loss of tone | none | none | none |
Pathophysiology
Pathophysiology.
The main current hypotheses of the pathophysiology of facial nerve palsy involve the reactivation of herpes simplex virus infection (HSV type 1) or else a cell-mediated autoimmune inflammatory response.
The main current hypotheses of the pathophysiology of facial nerve palsy involve the reactivation of herpes simplex virus infection (HSV type 1) or else a cell-mediated autoimmune inflammatory response (11, 12). The viral hypothesis is supported by the demonstration of herpes simplex virus DNA in the geniculate ganglion and endoneural fluid obtained at decompressive surgery and in the saliva of affected patients. It is presumed that episodes can be provoked by stress or by an infection of another type, in analogy to herpes labialis. Less consistent with the viral hypothesis are the absence of mucocutaneous changes and the low frequency of recurrence compared to herpes labialis (11).
In the autoimmune hypothesis, idiopathic facial nerve palsy is considered a mononeuritic variant of Guillain-Barré syndrome (GBS). Supportive findings include a diminution of T suppressor cells and an increase of B lymphocytes in the affected patients, along with elevated serum concentrations of interleukin-1, interleukin-6, and tumor necrosis factor alpha (11). There is also the interesting epidemiological observation of a significant rise in the incidence of peripheral facial nerve palsy in Switzerland after the introduction of intranasal influenza vaccination (13). It is presumed that an infection (or vaccination, as in Switzerland) can induce a mononeuritic immune response directed against myelin antigens in a peripheral nerve, in this case the facial nerve.
Autoimmune hypothesis.
In the autoimmune hypothesis, idiopathic facial nerve palsy is considered a mononeuritic variant of Guillain-Barré syndrome supported by a diminution of T suppressor cells, an increase of B lymphocytes, and elevated serum chemokines.
Palsy may develop in a multistep process beginning with inflammation leading to edema and swelling. This, in turn, can lead to compression of the nerve in the fallopian canal, where the normal nerve passes through its narrowest bony enclosure (the nerve occupies 99% of the cross-section of the canal in adults, but only 80% in children); hypoperfusion (strangulation) of the nerve ensues, leading to damage of axons and myelin sheaths and to nerve dysfunction (e8, e9). The possible role of further factors (the weather, exposure to cold or to a draft) has not been conclusively determined; there is weak evidence for a link with rapid changes of atmospheric temperature and pressure (rises by more than 6 hPa) (e10).
Differential diagnostic considerations
The idiopathic form of peripheral facial nerve palsy accounts for 60–75% of cases. An etiology can be identified in the remaining 25–40% (Table 2), most commonly neuroborreliosis and herpes zoster oticus (Ramsay Hunt syndrome) (1, 10, 14, e11). Herpes zoster should be considered as a possible cause in all cases, particularly if the patient has severe pain and even if no herpetic blisters are present (herpes zoster sine herpete). The diagnostic evaluation for potential causes of peripheral facial nerve palsy thus includes the history (tick bite, erythema migrans, pain), clinical neurological examination, and inspection of the ear, including otoscopy. Less commonly, peripheral facial nerve palsy can be due to infection with rickettsia, HIV, human herpesvirus 6, mumps virus, cytomegalovirus, and rubella virus (10, 12), or to sarcoidosis (Heerfordt syndrome), Sjögren syndrome, and carcinomatous meningitis. In Melkersson-Rosenthal syndrome, facial palsy recurs multiple times on the same side or on alternating sides, accompanied by lip and tongue swelling and by lingua plicata. Facial nerve palsy as a component of GBS can be recognized by the additional motor deficits that arise at about the same time, and by its bilaterality. Cerebrospinal fluid examination plays an important role in the differentiation of these potential etiologies. Masses in the cerebellopontine angle, Miller Fisher syndrome (a GBS variant with marked oculomotor dysfunction and ataxia), petrous bone fractures, parotid tumors, and otogenic processes should be identifiable on the basis of the history and suitable ancillary studies (10, 15).
Table 2. The differential diagnosis of peripheral facial nerve palsy (modified from [10, 15, 23]).
| Cause | Remarks |
| idiopathic | |
| idiopathic facial nerve palsy (Bell’s palsy) | common |
| traumatic | |
| petrous bone fracture | surgery may be indicated |
| infectious | |
| borreliosis | lumbar puncture; antibiotic treatment tailored to the stage and extent of the ‧infection |
| HIV | in the seroconversion phase with lymphocytic pleocytosis, also in the late phase with meningeal lymphomatosis |
| herpes zoster oticus | lumbar puncture; virostatic agents |
| other viral pathogens: cytomegalovirus, rubella virus, mumps virus, influenza B virus, Coxsackie virus; pathogens of other types: rickettsia, ehrlichiosis | rare |
| Guillain-Barré syndrome | lumbar puncture, with determination of ganglioside autoantibodies when indicated; treatment: intravenous immunoglobulin (IVIG), possibly plasmapheresis |
| acute and chronic otitis media | otological consultation |
| neoplastic | |
| schwannoma | facial n. (rare), vestibular n. |
| meningioma, glomus tumor | originating in the cerebellopontine angle, often with further cranial nerve deficits |
| malignant tumors | skull base tumors, parotid carcinoma |
| cholesteatoma | slow onset, gradual worsening |
| metabolic | |
| diabetes mellitus | mainly in association with arterial hypertension |
| pregnancy | increased risk mainly in the last trimester |
| rare sporadic cases | sarcoidosis, Wegener disease, Sjögren syndrome, Melkersson-Rosenthal ‧syndrome, acute lymphatic leukemia, carotid artery dissection in the neck |
Important diagnostic steps.
The diagnostic evaluation for potential causes of peripheral facial nerve palsy includes the history (tick bite, erythema migrans, pain), clinical neurological examination, and inspection of the ear, including otoscopy.
Neurophysiological ancillary diagnostic studies
If the clinical examination has been properly conducted and documented and the etiology has been reliably determined, with clear regression of the findings under appropriate treatment over the short term, no further neurophysiological testing is necessary. There are, however, rare cases in which the palsy cannot be dependably classified as peripheral or central on clinical grounds alone (e.g., if there has been prior damage to the facial nerve, if the present lesion is incomplete, or if the patient cannot fully cooperate with the examination). In such cases, transcranial canalicular magnetic stimulation is a useful ancillary neurophysiological study. The demonstration of canalicular hypoexcitability—a finding that is present in idiopathic facial nerve palsy from the first day onward—strongly supports peripheral extracerebral origin in all but a few cases (GBS, borreliosis). A blink reflex study (stimulation of the supraorbital branch, recording of the summed potential of the orbicularis oculi muscle) contributes to the topographical localization of the lesion. Pathological reflex responses on the paretic side indicate that the lesion can only lie in the facial nerve nucleus, the pontine fibers of the nerve, or its extrapontine course (e12).
Electroneurography (ENG) and electromyography (EMG) can both be used for prognostication (e13, e14). ENG with recording of the muscle summed action potential (MSAP) after transcutaneous supramaximal electrical stimulation of the facial nerve near the parotid gland reveals the extent of axonal injury as early as 10–14 after the onset of symptoms. A reduction of amplitude by less than 90% compared to the normal side is associated with a favorable prognosis (e12).
If the facial nerve palsy appears to be complete on clinical examination but the EMG reveals that potentials are generated when the patient attempts voluntary contraction of the muscles, it can be concluded that the nerve remains in continuity at least in part, and recovery is more likely. A finding of re-innervation potentials over the later course of the condition likewise indicates a favorable prognosis. On the other hand, pathological spontaneous activity on an EMG 10–14 days after symptom onset indicates axonal damage and thus an unfavorable prognosis.
Imaging studies
Positive signals.
If the facial nerve palsy appears to be complete on clinical examination but the EMG reveals that potentials are generated when the patient attempts voluntary contraction of the muscles, it can be concluded that the nerve remains in continuity at least in part, and recovery is more likely.
In patients with typical clinical manifestations, imaging studies can, in principle, be dispensed with (16). On the other hand, if there are any atypical features (slowly worsening paresis, accessory symptoms such as nystagmus, hypacusis, tinnitus, sensory deficits, diplopia, further cranial nerve disorders), tomographic imaging (preferably magnetic resonance imaging [MRI] without and with contrast medium) is urgently indicated, with a focus on potential lesions of the cerebellopontine angle, petrous bone, parotid gland, or brainstem (16– 18). Computed tomography is often performed in hospitalized patients before lumbar puncture in order to detect CSF circulation disorders and thereby avert the danger of herniation due to CSF removal. This measure is thought to improve patient safety, but the need for it has not been documented in clinical trials (e15).
Laboratory tests
A complete blood count and measurement of inflammatory parameters (serum C-reactive protein concentration, erythrocyte sedimentation rate) on the initial presentation of the patient are of little use in differential diagnosis, but borrelia serology is recommended, especially when borreliosis is strongly suspected on the basis of the history and physical examination, as well as in children, because the percentage of cases of borreliosis presenting with an isolated facial nerve palsy is particularly high in children (34% to 56%, including varicella-zoster virus [VZV] infections) (e16, e17). If there is clinical suspicion of herpes zoster oticus, VZV serology can be performed; this technique, however, is unsuitable for early diagnosis and should be repeated in 7–10 days in order to detect a rise in anti-VZV immunoglobulin G (IgG) and the presence of VZV-immunoglobulin M (IgM). If a viral origin is suspected, the recommended technique for detecting the causative virus is the polymerase chain reaction (PCR), e.g., from a CSF sample (e18). In clinically atypical cases of facial nerve palsy, or when other cranial nerves are affected as well, the measurement of antiganglioside autoantibodies may yield evidence of immunopathic cranial nerve damage (19).
Cerebrospinal fluid examination
CSF examination.
Lumbar puncture markedly increases the reliability of the diagnostic work-up and is recommended by neurologists as a standard part of it. In 10–40% of cases initially diagnosed clinically as idiopathic peripheral facial nerve palsy, an abnormal CSF finding is made with specific implications for treatment.
Lumbar puncture markedly increases the reliability of the diagnostic work-up and is recommended by neurologists as a standard part of it. In 10–40% of cases initially diagnosed clinically as idiopathic peripheral facial nerve palsy, an abnormal CSF finding is made with specific implications for treatment (20– 24). The main CSF laboratory parameters to be tested are cell count, protein, cytology, lactate, borrelia antibody specificity index (ASI), VZV (PCR), and CXCL13. CSF investigation enables the detection of herpes zoster oticus with 85% sensitivity and of borreliosis and other infections with 100% sensitivity (25). This is a particularly important matter in the tick season (April to October); specific treatment can be initiated as soon as the CSF findings are received from the laboratory. The risks and complications of lumbar puncture should always be borne in mind, however, and less invasive methods of pathogen detection should be considered as alternatives (26).
Specialized consultations.
Any abnormality of the ear, parotid gland, mastoid process, or tympanic membrane and/or any disturbance of hearing is an indication for examination by an otorhinolaryngologist. Potential corneal involvement calls for ophthalmological consultation.
Specialized consultations
Any abnormality of the ear, parotid gland, mastoid process, or tympanic membrane and/or any disturbance of hearing is an indication for examination by an otorhinolaryngologist. Potential corneal involvement calls for ophthalmological consultation. Pregnant and postpartum women with peripheral facial palsy should be seen by an obstetrician as well (7, 27).
Glucocorticoids.
Oral glucocorticoid treatment is supported by high-quality evidence from meta-analyses of randomized clinical trials.
Pharmacotherapy
Glucocorticoids
Adverse side effects.
The side effect profile of short-term glucocorticoid treatment for idiopathic facial nerve palsy is no worse than control.
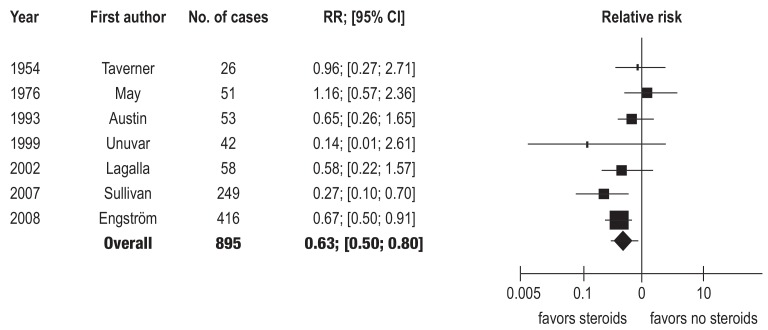
Oral glucocorticoid treatment is supported by high-quality evidence from meta-analyses of randomized clinical trials (7, 28). Treatment should be initiated as soon as possible after the onset of symptoms (<72 hours) in either of the two schemata from the most recent randomized trials, i.e., either prednisolone 25 mg bid for 10 days (4), or, alternatively, prednisolone 60 mg qd for 5 days, followed by a taper to off with a reduction of the dose by 10 mg each day from day 6 onward (22). From an endocrinological viewpoint, the single daily dose of glucocorticoid is best taken in the morning, as this suppresses the adrenal axis to a lesser extent (29). In meta-analyses of randomized, clinical trials, most recently by Madhok et al. (2016), glucocorticoid treatment was found to bring about a significantly better and more rapid recovery of facial nerve function (RR 0.63; 95% confidence interval (CI) [0.50; 0.80], n = 895; 7 trials), with a number needed to treat (NNT) of 10; [6; 20] (figure 1) (30). Glucocorticoid treatment has been found to be beneficial with respect to secondary endpoints as well—in particular, motor synkinesia and autonomic dysfunction, (RR 0.64; [0.45; 0.91]; n = 485, 3 trials; NNT = 11; [6; 49]). The side effect profile of short-term glucocorticoid treatment for this indication is no worse than control (30).
Virostatic agents.
The viral hypothesis (reactivation of HSV type 1) concerning the etiology of idiopathic peripheral facial nerve palsy implies that combined treatment with a glucocorticoid drug and a virostatic drug might be beneficial.
Virostatic agents
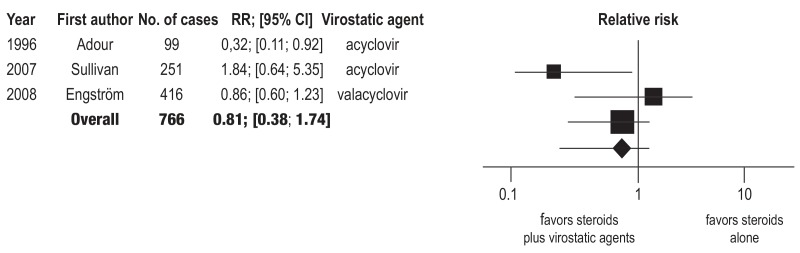
The viral hypothesis (reactivation of HSV type 1) concerning the etiology of idiopathic peripheral facial nerve palsy implies that combined treatment with a glucocorticoid drug and a virostatic drug might be beneficial. The clinical trials that have been performed to date to answer this question are, however, relatively heterogeneous. 10 out of 13 trials had to be excluded from the analysis because of an unknown or high risk of bias affecting the findings. With respect to the primary endpoint (percentage of patients with some degree of residual facial paresis at the end of the study), no significant difference was seen between combined treatment and glucocorticoid monotherapy (RR 0.81; [0.38; 1.74]; 3 trials, n = 766) (figure 3) (31). The reliability of the evidence was assessed as low on the basis of the GRADE criteria (www.gradeworkinggroup.org). A similar finding emerged from the analysis of data from patients with severe facial nerve palsy (House and Brackmann stages V and VI) (RR 0.82; [0.57; 1.17], 2 trials, n = 98) (31). The reliability of the evidence was low here as well. The risk of late sequelae (motor synkinesia and crocodile tears) was significantly lower in the combination therapy group than in the steroid-alone group (RR 0.56; [0.36; 0.87]; n = 469) (31).
Figure 3.
Forest plot of the meta-analysis of randomized and quasi-randomized clinical trials on the question of corticosteroids vs. placebo (modified from [30]; with the kind permission of Wiley). The clinical endpoint is incomplete resolution of weakness 6 months or more after randomization. CI, confidence interval; RR, relative risk; heterogeneity 18%; a fixed-effects model was used in the analysis.
These findings do not permit any general recommendation for antiviral therapy in patients with idiopathic peripheral facial nerve palsy. Combined treatment with a glucocorticoid and a virostatic agent can certainly be considered in individual cases, particularly when the palsy is severe, after discussion of the findings with the patient (32). Virostatic treatment is urgently indicated, however, if the palsy is due to herpes zoster oticus (Ramsay Hunt syndrome). The available drugs are acyclovir (5–10 mg/kg BW IV tid or 800 mg po 5×/d), valacyclovir (1000 mg po tid), brivudine (125 mg po qd), and famcyclovir (250–500 mg po tid) (e19)
Non-pharmacological treatment
Symptomatic treatment
Symptomatic treatment.
If lid closure is incomplete, symptomatic treatment with artificial tears, dexpanthenol ophthalmic ointment, and a nocturnal moisture-retaining eye shield is recommended.
If lid closure is incomplete, symptomatic treatment with artificial tears, dexpanthenol ophthalmic ointment, and a nocturnal moisture-retaining eye shield is recommended. This is often supplemented with exercises, either under the direction of a physiotherapist or with self-observation in a mirror. Nonetheless, a recent meta-analysis on physical therapy (exercise therapy, facial muscle exercises, electrotherapy) revealed neither a significant benefit not a significant harm (e20). Studies on the treatment of facial nerve palsy with acupuncture, a method used in traditional Chinese medicine, do not meet current scientific standards (e21).
Surgery
Surgical decompression is not recommended in the acute phase of the illness, as convincing evidence of benefit is lacking and complications can be severe (e22).
Prognosis and recurrences
The condition has a good prognosis even if untreated. Some 70% of patients recover fully in 6–9 months (33– 35). Patients with less severe palsy (House and Brackmann grade = III) recover better than those with more severe palsy (House and Brackmann grade = IV); elderly patients recover less well than younger ones, and men less well than women (e23). Some 13% of patients go on to have a mild residual paresis (facial asymmetry) that is not distressing (35), while 4% have severe residual paresis and 7% develop pathological accompanying movements (synkinesia) in their further course (e24). Synkinesia and residual autonomic dysfunction (crocodile tears) are thought to reflect an abnormal pattern re-innervation (14, 35). In all cases where there is no recovery at all or a residual paresis nine months after the onset of illness, the diagnosis of Bell’s palsy should be critically reconsidered, and a differential diagnostic re-evaluation should be performed as outlined above (table 2). Facial palsy recurs in ca. 7% of patients; the ipsilateral and contralateral sides are affected with equal frequency (e25).
Challenges in clinical practice
Diabetes mellitus
Diabetes mellitus.
Oral glucocorticoid treatment is recommended, in principle, for diabetic patients as well, although they will need meticulous blood sugar control.
Oral glucocorticoid treatment is recommended, in principle, for diabetic patients as well, although they will need meticulous blood sugar control. Diabetes is a frequent accompanying illness in patients with idiopathic facial nerve palsy (36). It was debated in the older literature whether facial palsy in diabetic patients reflected a diabetic mononeuropathy of microangiopathic origin (e26). With regard to treatment, however, there is only limited available evidence on the treatment of facial palsy in diabetic patients, because such patients were excluded from most of the relevant clinical trials. In one (open) clinical trial, diabetic patients with idiopathic facial nerve palsy had a higher rate of complete recovery of facial weakness if they were treated with glucocorticoids (97% vs. 58%) (e27). In an observational study, diabetic patients were found to have more severe facial weakness at first, but similar outcomes at six months (e28).
Children
Facial nerve palsy is rarer in children and more commonly due to an infection, usually borreliosis (37, e29). There have only been a small number of controlled trials of glucocorticoid therapy in children (e30, e31).
The BellPiC (Bell’s Palsy in Children) trial, now in progress in New Zealand and Australia, is a triple-blinded, randomized superiority trial on the benefit of steroids. Data acquisition is due to be completed in the year 2020 (e32).
Pregnancy
Idiopathic facial palsy may be more common in pregnancy, above all in the last trimester. Putative causes associated with pregnancy include a tendency toward edema and hypercoagulability. Hypertension and pre-eclampsia are risk factors. The prognosis is considered to be somewhat less favorable than in other patients (7). The recommended treatment, as in other adult patients with idiopathic facial nerve palsy, is with glucocorticoids under strict blood sugar control, and should be carried out on an inpatient basis (7, 27). Virostatic agents are generally considered safe for use in pregnancy and should be given if indicated. The treatment must be coordinated with the patient’s obstetrician.
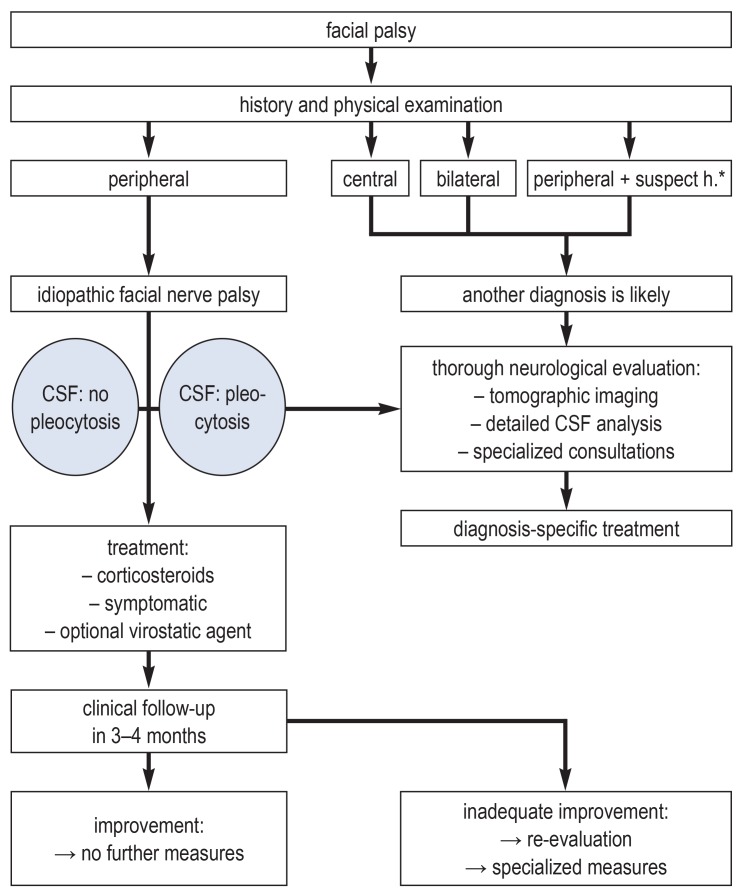
Inpatient or outpatient treatment
Idiopathic facial nerve palsy can generally be treated on an outpatient basis. The typical general practitioner may see only one case every two years, but reliable clinical diagnosis and early treatment are very important (5, 38). Hospitalization may be needed to ensure an appropriately broad, rapid, and accurate differential diagnostic work-up (table 2) and the initiation of treatment without delay. Other factors such as cerebrospinal fluid analysis, care at night and on weekends, and individual characteristics of the patient (atypical symptoms, severity of weakness, comorbidities) must be considered as well. A care algorithm is given in Figure 5
Figure 5.
Decision tree for acute facial nerve palsy depending on the clinical presentation. *suspect history (pain, gradual development, additional symptoms)
Management of residual weakness
Measures for the eye
Children.
Facial nerve palsy is rarer in children and more commonly due to an infection, usually borreliosis. There have only been a small number of controlled trials of glucocorticoid therapy in children.
Pregnant women.
The recommended treatment, as in other adult patients with idiopathic facial nerve palsy, is with glucocorticoids under strict blood sugar control, and should be carried out on an inpatient basis. The treatment must be coordinated with the patient’s obstetrician.
In case of residual facial weakness with incomplete lid closure, lid-loading measures can be used. External metal plates attached to the stretched upper eyelid, without touching the lashes, can be used temporarily; later, custom-prepared platinum weights can be implanted under the orbicularis oculi muscle under local anesthesia (internal lid-loading) (e33, e34). Denervation sometimes leads to ectropion of the lower lid, usually on the nasal side, which can be treated surgically by horizontal tightening (lateral tarsal strip, tarsorrhaphy, etc.) (e35). Eyelid surgery can almost always be carried out under local anesthesia and leads to good functional closure for the protection of the eye (39). Incomplete resolution of facial nerve palsy can also result in residual weakness, contractures, autonomic disturbances (crocodile tears), or synkinesia; such problems can be treated with special exercise programs and with botulinum toxin injections for chemodenervation. Botulinum toxin injections are effective for crocodile tears as well.
Surgical restoration of facial nerve function
Facial nerve reanimation.
Microsurgical dynamic facial nerve reanimation is performed to restore the innervation of the facial muscles and enable the recovery of active facial expression. These procedures are intended for patients with inadequate nerve regeneration or severe residual weakness.
Microsurgical dynamic facial nerve reanimation is performed to restore the innervation of the facial muscles and enable the recovery of active facial expression. These procedures are intended for patients with inadequate nerve regeneration or severe residual weakness. Surgery must be timed before muscle atrophy becomes too severe, thus usually 6–15 months after the onset of weakness. The main surgical methods are primary nerve suture and bridging the nerve with an autologous nerve graft from the greater auricular or sural nerve (39). If the proximal portion of the nerve is unavailable, nerve anastomoses can be performed, e.g., with portions of the ipsilateral hypoglossal, accessory, or masseteric nerve; this type of treatment, however, generally leads to dysfunction of the donor nerves and does not restore emotional control of facial expression (39, 40). Spontaneous, emotionally responsive facial expression is more likely to be restored by cross-facial-nerve grafting, in which selected muscles of facial expression are connected to the intact contralateral facial nerve with a nerve graft from, e.g., the sural nerve (39). In case of irreversible muscle atrophy, muscle transfer can be performed (donor muscle, gracilis m.; donor nerve, hypoglossal n., contralateral facial n., and others). Static surgical procedures (tightening, suturing) can be used to restore the corner of mouth to a neutral position (39). These procedures generally have success rates of more than 80–90%, but they should only be performed in centers with adequate experience (e36).
Figure 4.
Forest plot of the meta-analysis of randomized and quasi-randomized clinical trials on the question of corticosteroids plus virostatic agent vs. corticosteroids alone (modified from [31]; with the kind permission of Wiley).
CI, confidence interval; RR, relative risk; a random-effects model was used in the analysis.
Further information on CME.
Participation in the CME certification program is possible only over the Internet: cme.aerzteblatt.de. This unit can be accessed until 5 January 2020. Submissions by letter, e-mail or fax cannot be considered.
-
the following CME units can still be accessed for credit:
“Actinic Keratosis and Cutaneous Squamous Cell Carcinoma” (issue 37/2019) until 6 December 2019
“Benign Breast Disease in Women” (issue 33–34/2019) until 10 November 2019
“Psychopharmacological Treatment in Older People” (issue 29–30/2019) until 1 October 2019
This article has been certified by the North Rhine Academy for Continuing Medical Education. Participants in the CME program can manage their CME points with their 15-digit “uniform CME number” (einheitliche Fortbildungsnummer, EFN), which is found on the CME card (8027XXXXXXXXXXX). The EFN must be stated during registration on www.aerzteblatt.de (“Mein DÄ”) or else entered in “Meine Daten,” and the participant must agree to communication of the results.
CME credit for this unit can be obtained via cme.aerzteblatt.de until 5 January 2020. Only one answer is possible per question. Please select the answer that is most appropriate.
Question 1
What are the usual initial symptoms of idiopathic facial nerve palsy of sudden onset?
rotatory vertigo
weakness of the muscles of facial expression on one side of the face
limited range of motion of the cervical spine
pain in a circumscribed area of the temples bilaterally
sensorineural hearing loss
Question 2
What finding distinguishes peripheral from central facial palsy?
exacerbated cluster headache
diminished sensation
drooping corner of the mouth
loss of function of forehead muscles
hearing loss
Question 3
When is magnetic resonance imaging indicated as part of the diagnostic work-up?
if there is an abnormality of taste
if the patient drools from the corner of the mouth while drinking
if there are paresthesiae on the affected cheek
if there are any accessory symptoms
if there is retroauricular pain
Question 4
What is the incidence of idiopathic facial nerve palsy?
1–10 per 100 000 people per year
3–20 per 50 000 people per year
7–40 per 100 000 people per year
8–60 per 100 000 people per year
9–80 per 100 000 people per year
Question 5
Which of the following is now considered a possible causative factor for facial nerve palsy?
inadequate vaccination against paramyxoviruses
reactivation of a herpes simplex virus type 1 infection
maternal togavirus infection in the first trimester
chronic hepatitis E infection
recurrent infections due to influenza viruses
Question 6
What treatment regimen is recommended for the oral administration of glucocorticoids?
25 mg bid for 10 days
20 mg bid for 8 days
15 mg bid for 6 days
10 mg bid for 4 days
5 mg bid for 2 days
Question 7
What is a potentially beneficial treatment of a persistent lid-closure deficit?
lid loading
lid lifting
specific patient exercises
traditional Chinese medicine
optic nerve decompression
Question 8
What is the most common cause of symptomatic (i.e., secondary) peripheral facial nerve palsy?
borreliosis
sarcoidosis
HIV infection
Guillain-Barré syndrome
parotid tumor
Question 9
What cerebrospinal fluid parameter increases the reliability of diagnosis of facial palsy associated with herpes zoster oticus?
hyperphosphorylated tau protein
varicella-zoster viral DNA
beta-amyloid
erythrophages
albumin quotient
Question 10
When are virostatic drugs indicated?
when a herpetic rash is present in the ear canal
in patients who also have diabetes mellitus
if corneal involvement is suspected
in patients over age 70
in children
►Participation only via Internet: cme.aerzteblatt.de
Acknowledgments
Translated from the original German by Ethan Taub,M.D.
Footnotes
Conflict of interest statement
The authors state that they have no conflict of interest.
References
- 1.Gilden DH. Bell’s palsy. N Engl J Med. 2004;351:1323–1331. doi: 10.1056/NEJMcp041120. [DOI] [PubMed] [Google Scholar]
- 2.Rowlands S, Hooper R, Hughes R, Burney P. The epidemiology and treatment of Bell‘s palsy in the UK. Eur J Neurol. 2002;9:63–67. doi: 10.1046/j.1468-1331.2002.00343.x. [DOI] [PubMed] [Google Scholar]
- 3.Morales DR, Donnan P, Daly F, van Sta T, Sullivan FM. Impact of clinical trial findings on Bell’s palsy management in general practice in the UK 2001-2012: interrupted time series regression analysis. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-003121. e003121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sullivan FM, Swan IR, Donnan PT, et al. Early treatment with prednisolone or acyclovir in Bell‘s palsy. N Engl J Med. 2007;357:1598–1607. doi: 10.1056/NEJMoa072006. [DOI] [PubMed] [Google Scholar]
- 5.Glass GE, Tzafetta K. Optimising treatment of Bell’s palsy. Br J Gen Pract. 2014 e:807–809. doi: 10.3399/bjgp14X683041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Plumbaum K, Volk GF, Boeger D, et al. Inpatient treatment of patients with acute idiopathic peripheral facial palsy: a population-based health care research study. Clin Otolaryngol. 2017;42:1267–1274. doi: 10.1111/coa.12862. [DOI] [PubMed] [Google Scholar]
- 7.Heckmann JG, Lang C, Urban P, et al. Therapie der idiopathischen Fazialisparese (Bell’s palsy) Akt Neurol. 2017;44:712–727. [Google Scholar]
- 8.Heckmann JG, Heckmann SM, Lang CJ, Hummel T. Neurological aspects of taste disorders. Arch Neurol. 2003;60:667–671. doi: 10.1001/archneur.60.5.667. [DOI] [PubMed] [Google Scholar]
- 9.House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93:146–147. doi: 10.1177/019459988509300202. [DOI] [PubMed] [Google Scholar]
- 10.Finkensieper M, Volk GF, Guntinas-Lichius O. Erkrankungen des Nervus facialis. Laryngo-Rhino-Otologie. 2012;91:121–142. doi: 10.1055/s-0031-1300965. [DOI] [PubMed] [Google Scholar]
- 11.Zhang W, Xu L, Luo T, Wu F, Zhao B, Li X. The etiology of Bell’s palsy: a review. J Neurol. 2019 doi: 10.1007/s00415-019-09282-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ronthal M. Bell’s palsy: pathogenesis, clinical features, and diagnosis in adults. www.uptodate.com/contents/bells-palsy-pathogenesis-clinical-features-and-diagnosis-in-adults? (last accessed on 22 March 2019) [Google Scholar]
- 13.Mutsch M, Zhou W, Rhodes P, et al. Use of the inactivated intranasal influenza vaccine and the risk of Bell’s palsy in Switzerland. N Engl J Med. 2004;350:896–903. doi: 10.1056/NEJMoa030595. [DOI] [PubMed] [Google Scholar]
- 14.Peitersen E. Bell‘s palsy: the spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta Otolaryngol Suppl. 2002;549:4–30. [PubMed] [Google Scholar]
- 15.Finsterer J. Mangement of peripheral facial nerve palsy. Eur Arch Otorhinolaryngol. 2008;265:743–752. doi: 10.1007/s00405-008-0646-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dammann F, Grees H, Kösling S, Kress B, Lell M. Radiologische Diagnostik im Kopf-Hals-Bereich Leitlinie der Deutschen Röntgengesellschaft (DRG). Registernummer 039-093. www.awmf.org/leitlinien/detail/ll/039-093.html (last accessed on 13 September 2019) [Google Scholar]
- 17.Burmeister HP, Baltzer PA, Klingner CM, Pantel M, Kaiser WA. Computer- und Magnetresonanztomographie des N. facialis. HNO. 2010;58:433–442. doi: 10.1007/s00106-010-2101-2. [DOI] [PubMed] [Google Scholar]
- 18.Su BM, Kuan EC, St John MA. What is the role of imaging in the evaluation of the patient presenting with unilateral facial paralysis? Laryngoscope. 2018;128:297–298. doi: 10.1002/lary.26825. [DOI] [PubMed] [Google Scholar]
- 19.Banati M, Vachalova I, Vynogradova I, Heckmann JG. Isolierte Hirnnerven-Läsionen: Gangliosid-Autoantikörper als Hinweis auf Immunneuropathie. Dtsch Med Wochenschr. 2015;140:1154–1157. doi: 10.1055/s-0041-103406. [DOI] [PubMed] [Google Scholar]
- 20.Kohler A, Chofflon M, Sztajzel R, Magistris MR. Cerebrospinal fluid in acute peripheral facial palsy. J Neurol. 1999;246:165–169. doi: 10.1007/s004150050328. [DOI] [PubMed] [Google Scholar]
- 21.Hato N, Yamada H, Kohno H, et al. Valaciclovir and prednisolone treatment for Bell‘s palsy: a multicenter, randomized, placebo-controlled study. Otol Neurotol. 2007;28:408–413. doi: 10.1097/01.mao.0000265190.29969.12. [DOI] [PubMed] [Google Scholar]
- 22.Engström M, Berg T, Stjernquist-Desatnik A, et al. Prednisolone and valaciclovir in Bell‘s palsy: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet Neurol. 2008;7:993–1000. doi: 10.1016/S1474-4422(08)70221-7. [DOI] [PubMed] [Google Scholar]
- 23.Fuller G, Morgan C. Bell’s palsy syndrome: mimics and chameleons. Pract Neurol. 2016;16:439–444. doi: 10.1136/practneurol-2016-001383. [DOI] [PubMed] [Google Scholar]
- 24.Henkel K, Lange P, Eiffert H, Nau R, Spreer A. Infections in the differential diagnosis of Bell’s palsy: a plea for performing CSF analysis. Infection. 2017;45:147–155. doi: 10.1007/s15010-016-0933-8. [DOI] [PubMed] [Google Scholar]
- 25.Zimmermann J, Jesse S, Kassubek J, Pinkhardt E, Ludolph AC. Differential diagnosis and peripheral facial nerve palsy—a retrospective clinical, MRI- and CSF-based study. J Neurol. 2019 doi: 10.1007/s00415-019-09387-w. [DOI] [PubMed] [Google Scholar]
- 26.Gröschel K, Gröschel S. Diagnostische Lumbalpunktion. Dtsch Med Wochenschr. 2015;140:738–740. doi: 10.1055/s-0041-102251. [DOI] [PubMed] [Google Scholar]
- 27.Hussain A, Nduka C, Moth P, Malhotra R. Bell’s facial nerve palsy in pregnancy: a clinical review. J Obstet Gynaecol. 2017;37:409–415. doi: 10.1080/01443615.2016.1256973. [DOI] [PubMed] [Google Scholar]
- 28.Gronseth GS, Paduga R. Evidence-based guidelines update: steroids and antivirals for Bell palsy Report of the guideline development subcommittee of the American Academy of Neurology. Neurology. 2012;79:2209–2213. doi: 10.1212/WNL.0b013e318275978c. [DOI] [PubMed] [Google Scholar]
- 29.Ehrchen J. Prinzipien der Steroidtherapie. Hautarzt. 2012;63:973–984. doi: 10.1007/s00105-012-2471-3. [DOI] [PubMed] [Google Scholar]
- 30.Madhok VB, Gagyor I, Somasundara D, Sullivan M, Gammie F, Sullivan F. Corticosteroids for Bell’s palsy (idiopathic facial paralysis) Cochrane Database Syst Rev. 2016;5 doi: 10.1002/14651858.CD001942.pub5. CD001942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gagyor I, Madhok VB, Daly F, Sullivan F. Antiviral treatment for Bell‘s palsy (idiopathic facial paralysis) Cochrane Database of Sys Rev. 2019;8 doi: 10.1002/14651858.CD001869.pub9. CD001869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sullivan F, Daly F, Gagyor I. Antiviral agents added to corticosteroids for early treatment of adults with acute idiopathic facial nerve paralysis (Bell palsy) JAMA. 2016;316:874–875. doi: 10.1001/jama.2016.10160. [DOI] [PubMed] [Google Scholar]
- 33.Ronthal M. Bell’s palsy: treatment and prognosis in adults. www.uptodate.com/contents/bells-palsy-treatment-and-prognosis-in-adults (last accessed on 22 March 2019) [Google Scholar]
- 34.Volk GF, Klingner C, Finkensieper M, Witte OW, Guntinas-Lichius O. Prognostication of recovery time after acute peripheral facial palsy: a prospective cohort study. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-003007. pii: e003007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peitersen E. The natural history of Bell‘s palsy. Am J Otol. 1982;4:107–111. [PubMed] [Google Scholar]
- 36.Zhao H, Zhang X, Tang YD, Zhu J, Wang XH, Li ST. Bell’s palsy: clinical analysis of 372 cases and review of related literature. Eur Neurol. 2017;77:168–172. doi: 10.1159/000455073. [DOI] [PubMed] [Google Scholar]
- 37.Nau R, Christen HJ, Eiffert H. Lyme disease—current state of knowledge. Dtsch Arztebl Int. 2009;106:72–81. doi: 10.3238/arztebl.2009.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Holland J. Bell’s palsy. BMJ Clin Evid. 2011 pii: 1204. [PMC free article] [PubMed] [Google Scholar]
- 39.Berghaus A, San Nicolo M. Fazialisparese - wenn die Mimik erlischt. MMW Fortschr Med. 2015;157:42–45. doi: 10.1007/s15006-015-3538-8. [DOI] [PubMed] [Google Scholar]
- 40.Volk GF, Pantel M, Guntinas-Lichius O. Modern concepts in facial nerve reconstruction. Head Face Med. 2010;6 doi: 10.1186/1746-160X-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E1.Hilsinger RL Jr, Adour KK, Doty HE. Idiopathic facial paralysis, pregnancy, and the menstrual cycle. Ann Otol Rhinol Laryngol. 1975;84:433–442. doi: 10.1177/000348947508400402. [DOI] [PubMed] [Google Scholar]
- E2.Hellebrand MC, Friebe-Hoffmann , Bender HG, Kojda G, Hoffmann TK. Das Mona-Lisa-Syndrom - die periphere Fazialisparese in der Schwangerschaft. Z Geburtsh Neonatol. 2006;210:126–134. doi: 10.1055/s-2006-947216. [DOI] [PubMed] [Google Scholar]
- E3.Guntinas-Lichius O. Ist die Fazialisparese in der Schwangerschaft ein eigenes Krankheitsbild? HNO. 2012;60:96–97. doi: 10.1007/s00106-011-2449-y. [DOI] [PubMed] [Google Scholar]
- E4.Mumenthaler M. Neurologischer Untersuchungskurs, Teil II. Dtsch Arztebl. 1974:3463–3476. [Google Scholar]
- E5.Urban P. Idiopathische Hirnnervenausfälle. Nervenarzt. 2017;88:1439–1459. doi: 10.1007/s00115-017-0396-x. [DOI] [PubMed] [Google Scholar]
- E6.Rohen J. Topographische Anatomie. Stuttgart: Schattauer-Verlag. (10) 2017 [Google Scholar]
- E7.Volk GF, Schaede RA, Thielker J, et al. Reliability of grading of facial palsy using a video tutorial with synchronous video recording. Laryngoscope. 2019 doi: 10.1002/lary.27739. [DOI] [PubMed] [Google Scholar]
- E8.Schliack H. Zur Therapie der idiopathischen Fazialislähmung. Dtsch Arztebl. 1973:562–565. [Google Scholar]
- E9.Wolf SR. Die idiopathische Fazialisparese. HNO. 1998;46:786–798. doi: 10.1007/s001060050314. [DOI] [PubMed] [Google Scholar]
- E10.Franzke P, Bitsch A, Walther M, et al. Weather, weather changes and risk of Bell´s palsy: a multicenter case-crossover study. Neuroepidemiology. 2018;51:207–215. doi: 10.1159/000492671. [DOI] [PubMed] [Google Scholar]
- E11.Evison J, Aebi C, Francioli P, et al. Abklärung und Therapie der Lyme-Borreliose bei Erwachsenen und Kindern. Schweiz Ärztezeitung. 2005;86:2375–2384. [Google Scholar]
- E12.Urban P. Neurophysiologische Diagnostik bei Hirnnervenerkrankungen. J Neurol Neurochir Psychiatr. 2009;10:60–73. [Google Scholar]
- E13.Kim SH, Ryu EW, Yang CW, Yeo SG, Park MS, Byun JY. The prognostic value of electroneurography of Bell´s palsy at the orbicularis oculi versus nasolabial fold. Laryngoscope. 2016;126:1644–1648. doi: 10.1002/lary.25709. [DOI] [PubMed] [Google Scholar]
- E14.Lee DH. Clinical efficacy of electroneurography in acute facial paralysis. J Audiol Otol. 2016;20:8–12. doi: 10.7874/jao.2016.20.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E15.April MD, Long B, Koyfman A. Emergency medicine myths: computed tomography of the head prior to lumbar puncture in adults with suspected bacterial meningitis—due diligence or antiquated practice? J Emerg Med. 2017;53:313–321. doi: 10.1016/j.jemermed.2017.04.032. [DOI] [PubMed] [Google Scholar]
- E16.Jäämaa S, Salonen M, Seppälä I, Piiparinen H, Sarna S, Koskiniemi M. Varicella zoster and borrelia burgdorferi are the main agents associated with facial paresis, especially in children. J Clin Virol. 2003;27:146–151. doi: 10.1016/s1386-6532(02)00169-5. [DOI] [PubMed] [Google Scholar]
- E17.Nigrovic LE, Thompson AD, Fine AM, Kimia A. Clinical predictors of lyme disease among children with a peripheral facial palsy at an emergency department in a lyme disease-endemic area. Pediatrics. 2008;122:e1080–e1085. doi: 10.1542/peds.2008-1273. [DOI] [PubMed] [Google Scholar]
- E18.Sauerbrei A, Eichhorn U, Schacke M, Wutzler P. Laboratory diagnosis of herpes zoster. J Clin Virol. 1999;14:31–36. doi: 10.1016/s1386-6532(99)00042-6. [DOI] [PubMed] [Google Scholar]
- E19.Wutzler P, Gross G, Doerr HW. Antivirale Therapie des Zoster. Dtsch Arztebl. 2003;100:A858–A860. [Google Scholar]
- E20.Teixeira LJ, Valbuza JS, Prado GF. Physical therapy for Bell´s palsy (idiopathic facial paralysis) Cochrane Database Syst Rev. 2011;7 doi: 10.1002/14651858.CD006283.pub3. CD006283. [DOI] [PubMed] [Google Scholar]
- E21.Chen N, Zhou M, He L, Zhou D, Li N. Acupuncture for Bell´s palsy. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD002914.pub5. CD002914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E22.McAllister K, Walker D, Donnan PT, Swan I. Surgical interventions for the early management of Bell´s palsy. Cochrane Database Syst Rev. 2013:;10 doi: 10.1002/14651858.CD007468.pub3. CD007468. [DOI] [PubMed] [Google Scholar]
- E23.Ferreira M, Firmino-Machado J, Marques EA, Santos PC, Simoes AD, Duarte JA. Prognostic factors for recovery in Portugese patients with Bell´s palsy. Neurol Res. 2016;38:851–856. doi: 10.1080/01616412.2016.1209620. [DOI] [PubMed] [Google Scholar]
- E24.Bylund N, Jensson D, Enghag S, et al. Synkinesis in Bell´s palsy in a randomized controlled triel. Clin Otolaryngol. 2017;42:673–680. doi: 10.1111/coa.12799. [DOI] [PubMed] [Google Scholar]
- E25.Dong SH, Jung AR, Jung J, et al. Recurrent Bell´s palsy. Clin Otolaryngol. 2019;44:305–312. doi: 10.1111/coa.13293. [DOI] [PubMed] [Google Scholar]
- E26.Pecket P, Schattner A. Concurrent Bell´s palsy and diabetes mellitus: a diabetic mononeuropathy? J Neurol Neurosurg Psychiatry. 1982;45:652–655. doi: 10.1136/jnnp.45.7.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E27.Saito O, Aoyagi M, Tojima H, Koike Y. Diagnosis and treatment for Bell‘s palsy associated with diabetes mellitus. Acta Otolaryngol Suppl. 1994;511:153–155. doi: 10.3109/00016489409128322. [DOI] [PubMed] [Google Scholar]
- E28.Riga M, Kefalidis G, Danielides V. The role of diabetes mellitus in the clinical presentation and prognosis of Bell palsy. J Am Board Fam Med. 2012;25:819–826. doi: 10.3122/jabfm.2012.06.120084. [DOI] [PubMed] [Google Scholar]
- E29.Drack FD, Weissert M. Outcome of peripheral facial palsy in children—a catamnestic study. Eur J Paediatr Neurol. 2013;17:185–191. doi: 10.1016/j.ejpn.2012.09.003. [DOI] [PubMed] [Google Scholar]
- E30.Khajeh A, Fayyazi A, Soleimani G, Miri-Aliabad G, Shaykh Veisi S, Khajeh B. Comparison of the efficacy of combination therapy of prednisolone—acyclovir with prednisolone alone in Bell‘s palsy. Iran J Child Neurol. 2015;9:17–20. [PMC free article] [PubMed] [Google Scholar]
- E31.Salman MS, MacGregor DL. Should children with Bell‘s palsy be treated with corticosteroids? A systematic review. J Child Neurol. 2001;16:565–568. doi: 10.1177/088307380101600805. [DOI] [PubMed] [Google Scholar]
- E32.Babl FE, Mackay MT, Borland ML, et al. Bell‘s Palsy in Children (BellPIC): protocol for a multicentre, placebo-controlled randomized trial. BMC Pediatrics. 2017;17 doi: 10.1186/s12887-016-0702-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E33.Müller-Jensen K, Jansen M. Behandlung des fehlenden Lidschlusses. Sechs Jahre Erfahrung mit „Lidloading“. Dtsch Arztebl. 1997;94:A747–A750. [Google Scholar]
- E34.Hesse S, Werner C, Melzer I, Bardeleben A. Lidbeschwerung mit einem auf das Oberlid geklebten Bleiplättchen zur vorübergehenden Therapie des Lagophthalmus. Akt Neurol. 2010;37:341–343. [Google Scholar]
- E35.Sommer F. Operative Ektropiumkorrektur. Ophthalmologe. 2010;107:898–904. doi: 10.1007/s00347-009-2124-9. [DOI] [PubMed] [Google Scholar]
- E36.Coyle M, Godden A, Brennan PA, et al. Dynamic reanimation for facial palsy: an overview. Br J Oral Maxillofac Surg. 2013;51:679–683. doi: 10.1016/j.bjoms.2012.12.007. [DOI] [PubMed] [Google Scholar]