Key Points
Question
Is there a difference in maternal blood loss with delayed (60 seconds after birth) vs immediate umbilical cord clamping in term cesarean delivery?
Findings
In this randomized clinical trial that included 113 women undergoing scheduled cesarean delivery at term, there was no significant difference in the change in maternal hemoglobin at postoperative day 1 with delayed, compared with immediate, umbilical cord clamping (−1.90 g/dL vs −1.78 g/dL).
Meaning
In scheduled term cesarean deliveries, there was no significant difference in the change in maternal hemoglobin level at postoperative day 1 with delayed, compared with immediate, umbilical cord clamping.
Abstract
Importance
The American College of Obstetricians and Gynecologists recommends a delay in umbilical cord clamping in term neonates for at least 30 to 60 seconds after birth. Most literature supporting this practice is from low-risk vaginal deliveries. There are no published data specific to cesarean delivery.
Objective
To compare maternal blood loss with immediate cord clamping vs delayed cord clamping in scheduled cesarean deliveries at term (≥37 weeks).
Design, Setting, and Participants
Randomized clinical trial performed at 2 hospitals within a tertiary academic medical center in New York City from October 2017 to February 2018 (follow-up completed March 15, 2018). A total of 113 women undergoing scheduled cesarean delivery of term singleton gestations were included.
Interventions
In the immediate cord clamping group (n = 56), cord clamping was within 15 seconds after birth. In the delayed cord clamping group (n = 57), cord clamping was at 60 seconds after birth.
Main Outcomes and Measures
The primary outcome was change in maternal hemoglobin level from preoperative to postoperative day 1, which was used as a proxy for maternal blood loss. Secondary outcomes included neonatal hemoglobin level at 24 to 72 hours of life.
Results
All of the 113 women who were randomized (mean [SD] age, 32.6 [5.2] years) completed the trial. The mean preoperative hemoglobin level was 12.0 g/dL in the delayed and 11.6 g/dL in the immediate cord clamping group. The mean postoperative day 1 hemoglobin level was 10.1 g/dL in the delayed group and 9.8 g/dL in the immediate group. There was no significant difference in the primary outcome, with a mean hemoglobin change of −1.90 g/dL (95% CI, −2.14 to −1.66) and −1.78 g/dL (95% CI, −2.03 to −1.54) in the delayed and immediate cord clamping groups, respectively (mean difference, 0.12 g/dL [95% CI, −0.22 to 0.46]; P = .49). Of 19 prespecified secondary outcomes analyzed, 15 showed no significant difference. The mean neonatal hemoglobin level, available for 90 neonates (79.6%), was significantly higher with delayed (18.1 g/dL [95% CI, 17.4 to 18.8]) compared with immediate (16.4 g/dL [95% CI, 15.9 to 17.0]) cord clamping (mean difference, 1.67 g/dL [95% CI, 0.75 to 2.59]; P < .001). There was 1 unplanned hysterectomy in each group.
Conclusions and Relevance
Among women undergoing scheduled cesarean delivery of term singleton pregnancies, delayed umbilical cord clamping, compared with immediate cord clamping, resulted in no significant difference in the change in maternal hemoglobin level at postoperative day 1.
Trial Registration
ClinicalTrials.gov Identifier: NCT03150641
This randomized clinical trial compares the effect of immediate vs delayed cord clamping on change in maternal hemoglobin in scheduled cesarean deliveries (c-sections) at term (≥37 weeks).
Introduction
Delayed umbilical cord clamping in term neonates has been shown to result in improved neonatal hemoglobin levels at 24 to 48 hours of life, improved iron stores at 3 to 6 months of age, and improved neurodevelopmental indices through 4 years of age.1,2,3,4 Given these benefits, the American College of Obstetricians and Gynecologists in January 2017 expanded the recommendation for delayed umbilical cord clamping for at least 30 to 60 seconds after birth from only preterm to both preterm and term neonates, irrespective of mode of delivery.5
While the evidence for neonatal benefit with delayed cord clamping at term is strong, data related to maternal outcomes, particularly after cesarean delivery, are largely lacking. Women delivering by cesarean, in which the mean blood loss is at least twice that of a vaginal delivery with the potential for increased bleeding from delayed hysterotomy closure,6,7 are underrepresented in the literature. A systematic review on delayed cord clamping at term showed no differences in any measures of maternal blood loss, but the included studies generally focused on low-risk women expected to deliver vaginally.1 Of 15 randomized trials of delayed cord clamping at term, involving nearly 4000 women and neonate pairs, only 3 trials included women who delivered by cesarean, with a combined total of 87 cesarean deliveries, accounting for only 2.2% of the population on which the American College of Obstetricians and Gynecologists recommendations are based.4,8,9,10
Ultimately, there are no published prospective data specific to women undergoing cesarean delivery, with maternal and neonatal outcomes lacking. This randomized trial was conducted to compare maternal blood loss with immediate cord clamping vs delayed cord clamping in cesarean delivery at term. The study hypothesis was that delayed cord clamping would be associated with increased maternal blood loss, as proxied by the postoperative change in maternal hemoglobin.
Methods
Study Oversight
This randomized clinical trial was conducted at 2 hospitals—1 academic hospital and 1 community hospital—within a single university-based medical center in New York City. The study protocol, available in the Supplement, was approved by the institutional review board at Columbia University Irving Medical Center, New York, New York (Protocol No. AAAR2937). Written informed consent was obtained from all participants before randomization.
Screening and Recruitment
Women scheduled for cesarean delivery at the participating hospitals were screened for eligibility on a daily basis. Women with singleton gestations undergoing scheduled cesarean delivery at term (at or beyond 37 weeks 0 days) were eligible for study enrollment. Women for whom a delay in umbilical cord clamping might adversely affect maternal or neonatal outcomes were excluded. Specifically, those with placenta previa or placenta abruption, prenatally diagnosed fetal anomalies, known fetal anemia, or fetal growth restriction with abnormal Dopplers were excluded. Women with preeclampsia, significant maternal anemia (preoperative hemoglobin level ≤7 g/dL), bleeding disorders, planned cord blood banking, or refusal of blood products were also excluded. Additionally, owing to research staff availability, women with cesarean deliveries scheduled on weekends or postponed to evening hours were deemed ineligible for participation. Gestational age was assigned by best obstetric estimate using a standard method based on last menstrual period and ultrasound.
Randomization and Treatment
Eligible women were approached by obstetric clinicians (ie, the covering attending, fellow, resident, or physician assistant) and consented by research staff on the day of scheduled cesarean delivery. Once in the operating room, consenting women were randomly assigned in a 1:1 ratio to either immediate cord clamping or delayed cord clamping. The randomization sequence was generated by the study biostatistician (C.V.A.) based on the random number sequence generator function in SAS version 9.4 (SAS Institute), with stratification by hospital site, and performed electronically using the Research Electronic Data Capture (REDCap) platform.11 Given the nature of the interventions, blinding of obstetricians, intraoperative research staff, and patients was infeasible.
Procedures
Immediate cord clamping was defined as clamping within 15 seconds of birth and delayed cord clamping as clamping at 60 seconds after birth (in accordance with the 2017 American College of Obstetricians and Gynecologists recommendations).5 As is standard practice for all scheduled cesarean deliveries at the participating hospitals, preoperative hemoglobin level was assessed on a complete blood count obtained within 72 hours prior to delivery. Cesarean deliveries were performed by residents, fellows, and attending physicians, with appropriate supervision. A research staff member was present in the operating room for all deliveries and recorded intraoperative data, including the time from delivery to cord clamping. For the group undergoing delayed cord clamping, the research staff member announced to the obstetric surgical team when 60 seconds had passed. In the interval from delivery to delayed cord clamping, the neonate was placed on the mother’s legs at the level of the placenta. The obstetric team dried and stimulated the neonate on the sterile field. There was immediate and ongoing visual assessment by the pediatric team, who are present for all cesarean deliveries at the participating hospitals, with cord clamping performed prior to 60 seconds if clinically indicated to facilitate neonatal resuscitation. Earlier cord clamping could also be performed at the discretion of the obstetric team if there was any concern for maternal hemodynamic instability. Umbilical cord milking was not performed. As standard protocol, routine postpartum oxytocin was administered in all cases on delivery of the neonate, regardless of timing of cord clamping.
After delivery of the placenta, an umbilical cord segment was obtained for routine arterial and venous cord blood gas analysis. From this cord segment, an additional venous blood sample was obtained by the research team for point-of-care umbilical cord venous hemoglobin assessment. Placental weight was also measured.
All mothers received routine postoperative and postpartum care. This included administration of intravenous fluids (125 cc/h lactated ringers) until tolerating oral fluids. On postoperative day 1, maternal hemoglobin level was assessed on a complete blood count. Neonates received routine care. At the time of the routine newborn heel stick for New York State Newborn Screening, a sample of blood was obtained for point-of-care testing to assess the neonatal hemoglobin level at 24 to 72 hours of life. If this sample could not be obtained, an additional neonatal heel stick was not performed, and the hemoglobin level was not measured.
Race and ethnicity were self-reported by participants at study enrollment (fixed categories) and were collected to consider the generalizability of the results. The HemoCue Hb 201+ System (HemoCue America) was used for all point-of-care testing. Two authors (L.M. and B.A.) abstracted all demographic, historical, and outcome data from maternal and neonatal medical records. All medical records were reviewed through 30 days after delivery to identify any postpartum or postnatal complications.
Outcomes
The primary outcome was an objective measure of maternal blood loss: the change in maternal hemoglobin level on postoperative day 1 compared with the preoperative hemoglobin level. Secondary maternal outcomes were surgical time, estimated blood loss, postpartum hemorrhage (defined as estimated blood loss >1000 cc), uterotonic administration, and the need for blood transfusion. Although not prespecified, the absolute value of the postoperative day 1 hemoglobin level was also assessed as a secondary maternal outcome. Secondary neonatal outcomes included hemoglobin level at 24 to 72 hours of life, umbilical cord venous hemoglobin, Apgar scores (range, 0-10; 5-minute Apgar score of 0-3 is low, 4-6 is moderately abnormal, and 7-10 is reassuring12), time of first cry, umbilical cord gases, placental weight, birth weight, temperature, need for phototherapy for jaundice, and neonatal intensive care unit (NICU) admission. Data were also collected—but not reported here—regarding neonatal resuscitative interventions, vital signs at NICU admission, and bilirubin levels.
Statistical Methods
Based on a prior study of elective cesarean deliveries, a mean (SD) change in hemoglobin level for elective cesarean delivery of −1.37 (0.87) g/dL was estimated.13 Up to 20% crossover rate from the delayed cord clamping group to the immediate cord clamping group was anticipated. Because there is no accepted definition of a minimum clinically important difference in postoperative hemoglobin change, effect size was based on the published SD of the mean.13 Given the burden of maternal morbidity and mortality due to postpartum hemorrhage,14,15 and the paucity of prior data on neonatal benefit of delayed cord clamping in term cesarean delivery, the investigators decided that even a 1-SD greater drop in postoperative maternal hemoglobin level with delayed cord clamping might alter clinical decision-making. Based on these assumptions, setting the power at 90% to detect a 1-SD (0.9 g/dL) difference in the primary outcome between randomization groups, with a 2-tailed type I error rate of α = .05, a sample size of 106 women, or 53 per group, was required.
The data from all participants were analyzed according to the group to which they were randomly assigned, regardless of the actual timing of cord clamping. Primary outcome data were available for all participants. Missing data were otherwise rare (as detailed in the Results section) and data were not imputed. Categorical variables were analyzed using χ2 or Fisher exact test as appropriate. Continuous variables were assessed using either the t test or Wilcoxon rank sum test where appropriate. All hypothesis tests were 2-sided and significance was set at P < .05. An internal data and safety monitor (Quality Assurance Monitor for the Department of Obstetrics and Gynecology) performed monitoring. There were no interim analyses. Because of the potential for type I error due to multiple comparisons, findings for analyses of secondary end points should be interpreted as exploratory. Statistical analyses were performed in SAS version 9.4 (SAS Institute).
Results
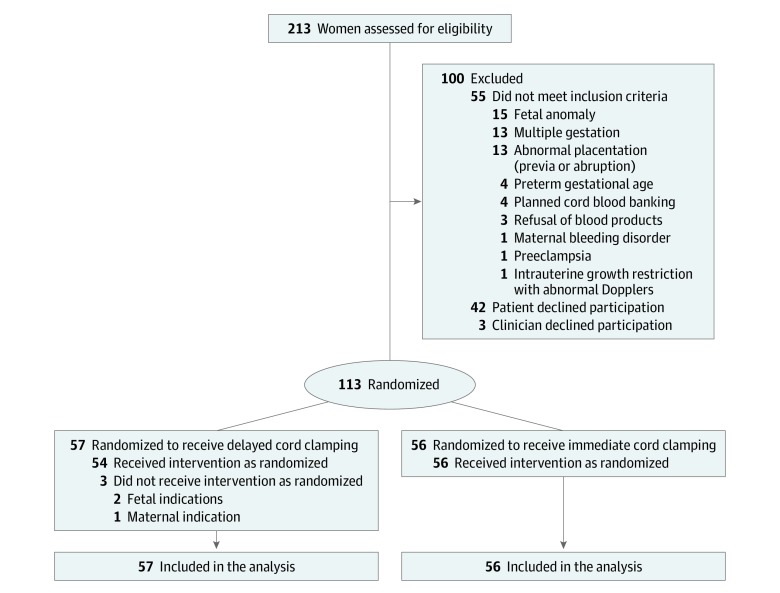
Study recruitment began in October 2017 and was completed in February 2018. A total of 213 women were assessed for eligibility, of which 113 enrolled and underwent randomization (57 to the delayed and 56 to the immediate cord clamping groups; Figure). Follow-up was completed for all participants on March 15, 2018.
Figure. Screening, Enrollment, Randomization, and Follow-up.
Participant Characteristics
Baseline demographic and obstetric characteristics of the study participants are shown in Table 1. Race was reported by 69.9% (79/113) and ethnicity by 98.2% (111/113) of participants. The median gestational age at trial entry, and thus delivery, was 39.1 weeks (interquartile range [IQR], 39.0-39.4) in both groups. The rate of prior postpartum hemorrhage in study participants was low overall (4.4%). The mean (SD) preoperative hemoglobin level was 12.0 (1.2) g/dL in the delayed and 11.6 (1.2) g/dL in the immediate cord clamping group.
Table 1. Baseline Maternal Characteristics.
| Characteristic | No. (%) | |
|---|---|---|
| Delayed Cord Clamping Group (n = 57) | Immediate Cord Clamping Group (n = 56) | |
| Hospital site | ||
| Academic | 25 (43.9) | 31 (55.4) |
| Community | 32 (56.1) | 25 (44.6) |
| Demographic | ||
| Maternal age, mean (SD), y | 31.6 (5.5) | 33.5 (4.9) |
| Prepregnancy body mass index, median (IQR)a | 27.9 (23.9-31.2) | 26.6 (23.8-30.4) |
| Race | n = 38 | n = 41 |
| White | 24 (63.2) | 23 (56.1) |
| Black | 13 (34.2) | 16 (39.0) |
| Asian | 1 (2.6) | 2 (4.9) |
| Hispanic ethnicity, No./total No. (%) | 42/57 (73.7) | 40/54 (74.1) |
| Prenatal care provider | ||
| Private | 10 (17.5) | 21 (38.2) |
| Clinic | 44 (77.2) | 34 (61.8) |
| No prenatal care | 3 (5.3) | 0 |
| Use during pregnancy | ||
| Tobacco | 2 (3.5) | 0 |
| Alcohol | 1 (1.8) | 1 (1.8) |
| Drug | 1 (1.8) | 1 (1.8) |
| Gestational diabetes | 5 (8.8) | 1 (1.8) |
| Hypertension | ||
| Chronic | 0 | 2 (3.6) |
| Gestational | 0 | 1 (1.8) |
| Obstetric | ||
| Gestational age at enrollment/delivery, median (IQR), wk | 39.1 (39.0-39.4) | 39.1 (39.0-39.4) |
| Nulliparous | 4 (7.0) | 5 (8.9) |
| No. of prior cesarean deliveries | ||
| None | 8 (14.0) | 7 (12.5) |
| 1 | 34 (59.7) | 36 (64.3) |
| ≥2 | 15 (26.3) | 13 (23.2) |
| No. of prior vaginal deliveries | ||
| None | 46 (80.7) | 48 (85.7) |
| 1 | 6 (10.5) | 7 (12.5) |
| ≥2 | 5 (8.8) | 1 (1.8) |
| Prior | ||
| Myomectomy | 4 (7.0) | 3 (5.4) |
| Postpartum hemorrhage | 2 (3.6) | 3 (5.4) |
| Preoperative maternal hemoglobin level, mean (SD), g/dL | 12.0 (1.2) | 11.6 (1.2) |
Abbreviation: IQR, interquartile range.
Calculated as weight in kilograms divided by height in meters squared.
Surgical characteristics for each group are shown in Table 2. All cases were performed under neuraxial anesthesia. Delivery was via a low transverse hysterotomy in all but 1 case in the immediate cord clamping group where a J incision was required.
Table 2. Surgical Characteristics.
| Characteristic | No. (%) | |
|---|---|---|
| Delayed Cord Clamping Group (n = 57) | Immediate Cord Clamping Group (n = 56) | |
| Primary indication for cesarean delivery | ||
| Elective repeat | 41 (71.9) | 42 (75.0) |
| Malpresentation | 3 (5.3) | 8 (14.3) |
| Prior myomectomy | 5 (8.8) | 3 (5.4) |
| Macrosomia | 2 (3.5) | 1 (1.8) |
| Prior vertical/unknown scar | 2 (3.5) | 1 (1.8) |
| Other | 2 (3.5) | 1 (1.8) |
| Primary maternal request | 1 (1.8) | 0 |
| Prior shoulder dystocia or third-/fourth-degree laceration | 1 (1.8) | 0 |
| Anesthesia type | ||
| Spinal | 46 (80.7) | 49 (87.5) |
| Combined spinal-epidural | 9 (15.8) | 6 (10.7) |
| Epidural | 2 (3.5) | 1 (1.8) |
| Skin incision | ||
| Pfannenstiel | 56 (98.2) | 55 (98.2) |
| Vertical | 1 (1.8) | 1 (1.8) |
| Hysterotomy type | ||
| Low transverse | 57 (100) | 55 (98.2) |
| Classical | 0 | 0 |
| T or J incision | 0 | 1 (1.8) |
| Anterior placenta | 23 (40.4) | 32 (57.1) |
| Tubal ligation performed | 17 (29.8) | 11 (19.6) |
| Intraoperative intravenous fluid volume, mean (SD), cc | 1913 (576) | 1930 (489) |
Intervention
The median time to cord clamping was 63 seconds (IQR, 61-65) in the delayed cord clamping group and 6 seconds (IQR, 5-8) in the immediate cord clamping group. Of the 113 included women-neonate pairs, 110 (97.3%) underwent cord clamping at the assigned time interval. Three of 57 women (5.3%) in the delayed cord clamping group had cord clamping performed prior to 60 seconds. In 2 of those cases, the cord was clamped early to facilitate neonatal resuscitation after difficult deliveries. In 1 case, the cord was clamped early for maternal indication, specifically for concern for maternal bleeding in a quaternary cesarean with delivery through an anterior placenta.
Primary Outcome
Primary outcome data were available for all participants. The hemoglobin level at postoperative day 1 was assessed at a median of 18.9 hours (IQR, 16.4-21.2) and 19.4 hours (IQR, 17.3-21.3) after delivery in the delayed and immediate groups, respectively (P = .24). There was no significant difference in maternal blood loss as assessed by the change in maternal hemoglobin level (Table 3). The mean hemoglobin level at postoperative day 1 was 10.1 g/dL (95% CI, 9.8-10.4) in the delayed group and 9.8 g/dL (95% CI, 9.5-10.2) in the immediate group (mean difference, 0.27 g/dL [95% CI, −0.21 to 0.74]; P = .26). Compared with the preoperative hemoglobin level, the hemoglobin level at postoperative day 1 demonstrated a mean decrease of −1.90 g/dL (95% CI, −2.14 to −1.66) in the delayed cord clamping group and −1.78 g/dL (95% CI, −2.03 to −1.54) in the immediate cord clamping group (mean difference, 0.12 g/dL [95% CI, −0.22 to 0.46]; P = .49).
Table 3. Primary and Secondary Maternal Outcomes.
| Outcome | Delayed Cord Clamping Group (n = 57) | Immediate Cord Clamping Group (n = 56) | Difference (95% CI)a |
P Valueb |
|---|---|---|---|---|
| Primary Maternal Outcome | ||||
| Change in maternal hemoglobin from preoperative to postoperative day 1, mean (95% CI), g/dL | −1.90 (−2.14 to −1.66) | −1.78 (−2.03 to −1.54) | 0.12 (−0.22 to 0.46)c | .49 |
| Secondary Maternal Outcomes | ||||
| Total surgical time, median (IQR), min | 58.0 (51.0 to 71.0) | 54.0 (46.0 to 69.5) | 3.0 (−6.0 to 12.0)d | .18 |
| Estimated blood loss, median (IQR), cc | 800 (800 to 1000) | 800 (800 to 800) | 0 (0 to 0)d | .13 |
| Postpartum hemorrhage (estimated blood loss >1000 cc), No. (%) | 5 (8.8) | 4 (7.1) | 1.7 (−9.5 to 12.9)e | >.99 |
| Uterotonic administration, No. (%) | 4 (7.0) | 4 (7.1) | −0.13 (−9.33 to 9.56)e | >.99 |
| Hysterectomy, No. (%)f | 1 (1.8) | 1 (1.8) | 0.1 (−4.8 to 4.9)e | >.99 |
| Blood transfusion, No. (%) | 0 | 2 (3.6) | −3.6 (−8.4 to 1.3)e | .24 |
| Postoperative day 1 hemoglobin level, mean (95% CI), g/dLf | 10.1 (9.8 to 10.4) | 9.8 (9.5 to 10.2) | 0.27 (−0.21 to 0.74)c | .26 |
Abbreviation: IQR, interquartile range.
The mean differences were calculated using the 2-sample t test difference of means. The median differences were calculated using quantile regression.
P values were unadjusted and 2-sided.
Mean difference.
Median difference.
Risk difference.
Outcome not prespecified in protocol.
Secondary Maternal Outcomes
The median surgical time was 58.0 minutes (IQR, 51.0-71.0) in the delayed group and 54.0 minutes (IQR, 46.0-69.5) in the immediate group. There were no statistically significant differences seen in any secondary measures of maternal blood loss (Table 3). Only 2 patients required blood transfusion; both women were in the immediate cord clamping group and each received 2 units of packed red blood cells for symptomatic anemia on postoperative day 1.
Secondary Neonatal Outcomes
Secondary neonatal outcomes are displayed in Table 4. Neonatal hemoglobin data were available for 90 of the 113 delivered neonates (79.6%). At 24 to 72 hours of life, there was a 1.7-g/dL higher neonatal hemoglobin level with delayed, compared with immediate, cord clamping (mean, 18.1 g/dL [95% CI, 17.4-18.8] vs 16.4 g/dL [95% CI, 15.9-17.0]; mean difference, 1.67 g/dL [95% CI, 0.75-2.59]; P < .001). Results for umbilical cord arterial blood gas were available in 87.7% of cases (50/57) in the delayed cord clamping group and 98.2% of cases (55/56) in the immediate cord clamping group (P = .06). The umbilical cord arterial pH was statistically significantly lower in the delayed cord clamping group compared with the immediate cord clamping group (median, 7.26 [IQR, 7.21-7.29] vs 7.28 [IQR, 7.23-7.31]; P = .03). This was associated with a statistically significantly greater arterial base excess in the delayed cord clamping group (median, −1.5 [IQR, −3.4 to 0.0] vs −0.1 [−1.7 to 0.8]; P = .004). Results for umbilical cord venous blood gas were available in 94.7% of cases (54/57) in the delayed cord clamping group and 98.2% of cases (55/56) in the immediate cord clamping group (P = .62). Results from venous cord gas studies were not significantly different between groups. There were no other significant differences in neonatal outcomes, including need for phototherapy for jaundice, which was only required in 1 case in the immediate cord clamping group. There were no neonatal blood transfusions.
Table 4. Secondary Neonatal Outcomes.
| Outcome | Delayed Cord Clamping Group (n = 57) | Immediate Cord Clamping Group (n = 56) | Difference (95% CI)a | P Valueb |
|---|---|---|---|---|
| Neonatal hemoglobin level at 24-72 h of life, mean (95% CI), g/dL | 18.1 (17.4 to 18.8) | 16.4 (15.9 to 17.0) | 1.67 (0.75 to 2.59)c | <.001 |
| No. | 46 | 44 | ||
| Umbilical cord venous hemoglobin, mean (95% CI), g/dL | 14.0 (13.6 to 14.4) | 13.9 (13.6 to 14.3) | 0.07 (−0.42 to 0.56)c | .78 |
| Neonatal crying/breathing established before cord clamping, No. (%) | 52 (92.9) | 26 (46.4) | 46.4 (31.7 to 61.1)d | <.001 |
| Apgar scores, median (IQR), mine | ||||
| 1 | 9 (8 to 9) | 9 (9 to 9) | 0 (0 to 0)f | .39 |
| 5 | 9 (9 to 9) | 9 (9 to 9) | 0 (0 to 0)f | .26 |
| Infant birth weight, mean (95% CI), g | 3405 (3286 to 3523) | 3448 (3350 to 3546) | −43 (−195 to 109)c | .57 |
| Placental weight, mean (95% CI), g | 599 (567 to 630) | 636 (606 to 667) | −38 (−81 to 6)c | .09 |
| Neonatal temperature, median (IQR), °C | 36.8 (36.7 to 37.0) | 36.8 (36.6 to 36.9) | 0 (−0.1 to 0.1)f | .33 |
| Phototherapy for jaundice, No. (%) | 0 | 1 (1.8) | −1.8 (−5.3 to 1.7)d | .50 |
| NICU admission, No. (%) | 4 (7.0) | 1 (1.8) | 5.2 (−2.2 to 12.7)d | .36 |
| Umbilical cord measures, median (IQR) | ||||
| Arterial pH | 7.26 (7.21 to 7.29) | 7.28 (7.23 to 7.31) | −0.02 (−0.04 to 0.003)f | .03 |
| No. | 50 | 55 | ||
| Arterial base excess | −1.5 (−3.4 to 0.0) | −0.1 (−1.7 to 0.8) | −1.1 (−2.3 to 0.1)f | .004 |
| No. | 50 | 55 | ||
| Cord venous pH | 7.32 (7.29 to 7.35) | 7.34 (7.30 to 7.36) | −0.02 (−0.04 to 0.002)f | .19 |
| No. | 54 | 55 | ||
| Cord venous base excess | −1.3 (−2.7 to −0.1) | −1.3 (−2.6 to −0.4) | 0 (−0.9 to 0.9)f | .79 |
| No. | 54 | 55 |
Abbreviations: IQR, interquartile range; NICU, neonatal intensive care unit.
The mean differences were calculated using the 2-sample t test difference of means. The median differences were calculated using quantile regression.
P values were unadjusted and 2-sided.
Mean difference.
Risk difference.
The Apgar score is the sum of 5 elements each scored 0, 1, or 2 (best): Appearance, Pulse, Grimace, Activity, and Respiration; range, 0-10 (5-minute Apgar score of 0-3 is low, 4-6 is moderately abnormal, and 7-10 is reassuring12).
Median difference.
Five neonates were admitted to the NICU. In the delayed cord clamping group, there were 4 NICU admissions: 1 for transient tachypnea of the newborn, 2 for respiratory distress syndrome, and 1 for monitoring for neonatal hemolytic anemia in the setting of anti-Kell alloimmunization as well as a postnatal diagnosis of a cleft palate. In the immediate cord clamping group, 1 neonate was admitted to the NICU for a postnatal diagnosis of a coarctation of the aorta. The rate of NICU admission was not significantly different between groups (7.0% vs 1.8%, P = .36; Table 4).
Adverse Maternal and Neonatal Events
Two women underwent unplanned hysterectomy. The first case was a woman in the delayed cord clamping group with an unanticipated placenta accreta; delayed cord clamping was performed as planned prior to identification of the abnormal placentation. The second case was a woman in the immediate cord clamping group who had a uterine window that could not be reapproximated adequately, necessitating hysterectomy. There were no cases of clinical coagulopathy and no surgical injuries occurred (ie, cystotomy, ureteral injury, bowel injury). There were no maternal ICU admissions. At 30 days postpartum, additional complications were rare. In the delayed cord clamping group, there was 1 case of wound cellulitis and 1 wound seroma. In the immediate cord clamping group, there was 1 wound seroma and 1 maternal readmission for postpartum preeclampsia with severe features.
Discussion
In this randomized clinical trial, delayed cord clamping for 60 seconds during scheduled term cesarean delivery did not result in increased maternal blood loss compared with immediate cord clamping, as proxied by the postoperative change in maternal hemoglobin level. The mean difference in the primary outcome (change in maternal hemoglobin at postoperative day 1) between the delayed and immediate cord clamping groups was 0.12 g/dL, with a narrow confidence interval that did not include any clinically important differences in maternal hemoglobin level.
Delayed cord clamping during scheduled cesarean delivery was also not significantly associated with any other measures of increased maternal blood loss. This is consistent with the data from women delivering primarily vaginally in prior randomized trials of delayed cord clamping at term1 and fills a gap in the literature related to outcomes after scheduled cesarean delivery at term.
Concern from obstetricians about the unknown effect of delayed cord clamping during cesarean delivery has been identified as a barrier to implementation of delayed cord clamping.16 To our knowledge, this is the first randomized trial evaluating maternal outcomes with delayed cord clamping specifically in scheduled cesarean delivery at term. A particular strength of this study is the use of maternal hemoglobin change—an objective measure of blood loss—as the primary outcome measure. There was a low rate of cord clamping prior to 60 seconds within the delayed cord clamping group, speaking to the feasibility of delayed cord clamping in cesarean deliveries.
Specific to cesarean delivery, a recently published pilot study examined the safety of delayed cord clamping for 90 to 120 seconds in a convenience sample of 39 women undergoing elective cesarean delivery at term compared with 112 historical controls undergoing immediate cord clamping at cesarean delivery.17 Similar to this study, the authors found no difference in maternal hemoglobin levels. However, the pilot study paradoxically found a lower estimated blood loss and maternal transfusion rate with delayed cord clamping, but results may be confounded by the subjective nature of estimated blood loss assessment and temporal changes in practice with the use of historical controls. A retrospective study by Rhoades and colleagues18 comparing outcomes before and after institution of a universal delayed cord clamping protocol at term included a subgroup analysis of 196 women who underwent cesarean delivery. The primary outcome, postpartum hemorrhage of 1000 cc or greater, was increased postprotocol in cesarean deliveries. However, postpartum hemorrhage was assessed by a subjective measure of blood loss, and, as in this study, there was no significant difference in objective measures of maternal blood loss including postoperative hemoglobin levels, uterotonic therapy, or blood transfusion with cesarean delivery.
This trial additionally found that delayed cord clamping in scheduled cesarean delivery at term achieved significantly higher neonatal hemoglobin levels at 24 to 72 hours of life. The observed increase in neonatal hemoglobin level after delayed cord clamping in this randomized clinical trial was similar to that found in prior studies of delayed cord clamping in primarily vaginal deliveries (mean difference, 1.5 g/dL [95% CI, 1.21-1.78]).1 Similar magnitude increases in neonatal hemoglobin levels in prior studies have been associated with decreased iron deficiency at 3 to 6 months and improved neurodevelopmental outcomes through 4 years of age.1,2,3,4 Although prior studies have shown an increase in neonatal jaundice requiring phototherapy with delayed cord clamping at term, this study did not find a significant association.1
Prior data are mixed on the effect of delayed cord clamping on cord arterial pH, with 2 studies showing a small but statistically significant decrease in pH19,20 and 4 studies showing no difference.10,18,21,22 Delayed cord clamping was, in this study, associated with a statistically lower umbilical cord arterial pH and base excess compared with immediate cord clamping. However, the absolute difference between groups was small (0.02 for pH and −1.4 for base excess) and the median pH and base excess were still in the normal range for both groups. With a cord pH above 7.20, the odds of neonatal morbidity and mortality are low.23 Thus, the observed differences in this study are unlikely to be of clinical significance in a vigorous term infant, but further studies are needed to understand the physiology and potential risks for nonvigorous neonates.
Limitations
This study has several limitations. First, the study included only scheduled term cesarean deliveries of singleton gestations. As such, these results may not be generalizable to intrapartum, emergency, twin (or higher-order multiple gestation), or preterm cesarean deliveries. Further studies are warranted to assess the effect of delayed cord clamping in such cases. Second, because there is no accepted definition of a clinically important postoperative hemoglobin change, the chosen effect size for the primary outcome was based on a single study of elective cesarean deliveries and author opinion. Therefore, in clinical practice, the implications of the primary study results should be considered on an individual patient basis. Third, the trial was not powered to assess clinically important, but infrequent, secondary outcomes (ie, maternal blood transfusion), and few of these outcomes were reported. Fourth, the trial did not assess longer durations of delayed cord clamping, which have been recommended by some professional societies.24,25 Nevertheless, the study results demonstrate a neonatal benefit after just 60 seconds. Fifth, because 30-day outcomes were ascertained by medical record review, postpartum and/or postnatal complications that were managed outside the participating medical center could not be identified. Sixth, examining long-term neonatal outcomes, such as iron stores and child neurodevelopment, was beyond the scope of this trial.
Conclusions
Among women undergoing scheduled cesarean delivery of term singleton pregnancies, delayed umbilical cord clamping, compared with immediate cord clamping, resulted in no significant difference in the change in maternal hemoglobin level at postoperative day 1.
Trial Protocol
References
- 1.McDonald SJ, Middleton P, Dowswell T, Morris PS. Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes. Cochrane Database Syst Rev. 2013;(7):CD004074. doi: 10.1002/14651858.CD004074.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andersson O, Lindquist B, Lindgren M, Stjernqvist K, Domellöf M, Hellström-Westas L. Effect of delayed cord clamping on neurodevelopment at 4 years of age: a randomized clinical trial. JAMA Pediatr. 2015;169(7):631-638. doi: 10.1001/jamapediatrics.2015.0358 [DOI] [PubMed] [Google Scholar]
- 3.Rana N, Kc A, Målqvist M, Subedi K, Andersson O. Effect of delayed cord clamping of term babies on neurodevelopment at 12 months: a randomized controlled trial. Neonatology. 2019;115(1):36-42. doi: 10.1159/000491994 [DOI] [PubMed] [Google Scholar]
- 4.Andersson O, Hellström-Westas L, Andersson D, Domellöf M. Effect of delayed versus early umbilical cord clamping on neonatal outcomes and iron status at 4 months: a randomised controlled trial. BMJ. 2011;343:d7157. doi: 10.1136/bmj.d7157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Committee on Obstetric Practice Committee opinion No. 684: delayed umbilical cord clamping after birth. Obstet Gynecol. 2017;129(1):e5-e10. doi: 10.1097/AOG.0000000000001860 [DOI] [PubMed] [Google Scholar]
- 6.Cunningham FG, Leveno KJ, Bloom SL, et al. Cesarean delivery and peripartum hysterectomy In: Williams Obstetrics. 25th ed New York, NY: McGraw-Hill Education; 2018. [Google Scholar]
- 7.Cunningham FG, Leveno KJ, Bloom SL, et al. Obstetrical hemorrhage In: Williams Obstetrics. 25th ed New York, NY: McGraw-Hill Education; 2018. [Google Scholar]
- 8.Ceriani Cernadas JM, Carroli G, Pellegrini L, et al. The effect of timing of cord clamping on neonatal venous hematocrit values and clinical outcome at term: a randomized, controlled trial. Pediatrics. 2006;117(4):e779-e786. doi: 10.1542/peds.2005-1156 [DOI] [PubMed] [Google Scholar]
- 9.Nelson NM, Enkin MW, Saigal S, Bennett KJ, Milner R, Sackett DL. A randomized clinical trial of the Leboyer approach to childbirth. N Engl J Med. 1980;302(12):655-660. doi: 10.1056/NEJM198003203021203 [DOI] [PubMed] [Google Scholar]
- 10.Andersson O, Hellström-Westas L, Andersson D, Clausen J, Domellöf M. Effects of delayed compared with early umbilical cord clamping on maternal postpartum hemorrhage and cord blood gas sampling: a randomized trial. Acta Obstet Gynecol Scand. 2013;92(5):567-574. doi: 10.1111/j.1600-0412.2012.01530.x [DOI] [PubMed] [Google Scholar]
- 11.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Executive summary: neonatal encephalopathy and neurologic outcome, second edition: report of the American College of Obstetricians and Gynecologists’ Task Force on Neonatal Encephalopathy. Obstet Gynecol. 2014;123(4):896-901. doi: 10.1097/01.AOG.0000445580.65983.d2 [DOI] [PubMed] [Google Scholar]
- 13.Horowitz E, Yogev Y, Ben-Haroush A, Rabinerson D, Feldberg D, Kaplan B. Routine hemoglobin testing following an elective cesarean section: is it necessary? J Matern Fetal Neonatal Med. 2003;14(4):223-225. doi: 10.1080/jmf.14.4.223.225 [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention Severe maternal morbidity in the United States. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity.html. Updated November 27, 2017. Accessed September 6, 2019.
- 15.Centers for Disease Control and Prevention Pregnancy Mortality Surveillance . https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-mortality-surveillance-system.htm. Updated June 4, 2019. Accessed September 6, 2019.
- 16.Anton O, Jordan H, Rabe H. Strategies for implementing placental transfusion at birth: a systematic review. Birth. 2019;46(3):411-427. doi: 10.1111/birt.12398 [DOI] [PubMed] [Google Scholar]
- 17.Chantry CJ, Blanton A, Taché V, Finta L, Tancredi D. Delayed cord clamping during elective cesarean deliveries: results of a pilot safety trial. Matern Health Neonatol Perinatol. 2018;4:16. doi: 10.1186/s40748-018-0083-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rhoades JS, Wesevich VG, Tuuli MG, Macones GA, Cahill AG. Implementation and outcomes of universal delayed umbilical cord clamping at term. Am J Perinatol. 2019;36(3):233-242. doi: 10.1055/s-0038-1669908 [DOI] [PubMed] [Google Scholar]
- 19.Wiberg N, Källén K, Olofsson P. Delayed umbilical cord clamping at birth has effects on arterial and venous blood gases and lactate concentrations. BJOG. 2008;115(6):697-703. doi: 10.1111/j.1471-0528.2008.01708.x [DOI] [PubMed] [Google Scholar]
- 20.Valero J, Desantes D, Perales-Puchalt A, Rubio J, Diago Almela VJ, Perales A. Effect of delayed umbilical cord clamping on blood gas analysis. Eur J Obstet Gynecol Reprod Biol. 2012;162(1):21-23. doi: 10.1016/j.ejogrb.2012.01.020 [DOI] [PubMed] [Google Scholar]
- 21.De Paco C, Florido J, Garrido MC, Prados S, Navarrete L. Umbilical cord blood acid-base and gas analysis after early versus delayed cord clamping in neonates at term. Arch Gynecol Obstet. 2011;283(5):1011-1014. doi: 10.1007/s00404-010-1516-z [DOI] [PubMed] [Google Scholar]
- 22.Tang J, Fullarton R, Samson SL, Chen Y. Delayed cord clamping does not affect umbilical cord blood gas analysis. Arch Gynecol Obstet. 2019;299(3):719-724. doi: 10.1007/s00404-019-05048-5 [DOI] [PubMed] [Google Scholar]
- 23.Malin GL, Morris RK, Khan KS. Strength of association between umbilical cord pH and perinatal and long term outcomes: systematic review and meta-analysis. BMJ. 2010;340:c1471. doi: 10.1136/bmj.c1471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization Guideline: Delayed Umbilical Cord Clamping for Improved Maternal and Infant Health and Nutrition Outcomes. Geneva, Switzerland: World Health Organization; 2014. [PubMed] [Google Scholar]
- 25.American College of Nurse-Midwives Position statement: delayed umbilical cord clamping. http://www.midwife.org/ACNM/files/ACNMLibraryData/UPLOADFILENAME/000000000290/Delayed-Umbilical-Cord-Clamping-May-2014.pdf. Accessed December 4, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol