This randomized noninferiority trial compares the effect of virtual reality vs face-to-face cardiopulmonary resuscitation (CPR) training on CPR quality measured by chest compression depth and rate on CPR manikins.
Key Points
Question
Does virtual reality (VR) cardiopulmonary resuscitation (CPR) training result in CPR quality and performance comparable with face-to-face training?
Findings
In this randomized noninferiority trial of 381 individuals, VR training resulted in noninferior chest compression rate but inferior compression depth; proportions of participants fulfilling guideline-endorsed compression depth or rate recommendations were lower in VR training, although overall these criteria were met in more than 50%. Cardiopulmonary resuscitation scenario performance and chest compression fraction were worse, but leaning was less common than in face-to-face training.
Meaning
Although VR training may lead to chest compression rates similar to face-to-face training, it needs further development to achieve comparable compression depth and overall CPR performance.
Abstract
Importance
Bystander cardiopulmonary resuscitation (CPR) is crucial for survival after cardiac arrest but not performed in most cases. New, low-cost, and easily accessible training methods, such as virtual reality (VR), may reach broader target populations, but data on achieved CPR skills are lacking.
Objective
To compare CPR quality between VR and face-to-face CPR training.
Design, Setting, and Participants
Randomized noninferiority trial with a prospective randomized open blinded end point design. Participants were adult attendees from the science section of the Lowlands Music Festival (August 16 to 18, 2019) in the Netherlands. Analysis began September 2019.
Interventions
Two standardized 20-minute protocols on CPR and automated external defibrillator use: instructor-led face-to-face training or VR training using a smartphone app endorsed by the Resuscitation Council (United Kingdom).
Main Outcomes and Measures
During a standardized CPR scenario following the training, we assessed the primary outcome CPR quality, measured as chest compression depth and rate using CPR manikins. Overall CPR performance was assessed by examiners, blinded for study groups, using a European Resuscitation Council–endorsed checklist (maximum score, 13). Additional secondary outcomes were chest compression fraction, proportions of participants with mean depth (50 mm-60 mm) or rate (100 min−1-120 min−1) within guideline ranges, and proportions compressions with full release.
Results
A total of 381 participants were randomized: 216 women (57%); median (interquartile range [IQR]) age, 26 (22-31) years. The VR app (n = 190 [49.9%]) was inferior to face-to-face training (n = 191 [50.1%]) for chest compression depth (mean [SD], VR: 49 [10] mm vs face to face: 57 [5] mm; mean [95% CI] difference, −8 [−9 to −6] mm), and noninferior for chest compression rate (mean [SD]: VR: 114 [12] min−1 vs face to face: 109 [12] min−1; mean [95% CI] difference, 6 [3 to 8] min−1). The VR group had lower overall CPR performance scores (median [IQR], 10 [8-12] vs 12 [12-13]; P < .001). Chest compression fraction (median [IQR], 61% [52%-66%] vs 67% [62%-71%]; P < .001) and proportions of participants fulfilling depth (51% [n = 89] vs 75% [n = 133], P < .001) and rate (50% [n = 87] vs 63% [n = 111], P = .01) requirements were also lower in the VR group. The proportion of compressions with full release was higher in the VR group (median [IQR], 98% [59%-100%] vs 88% [55%-99%]; P = .002).
Conclusions and Relevance
In this randomized noninferiority trial, VR training resulted in comparable chest compression rate but inferior compression depth compared with face-to-face training. Given the potential of VR training to reach a larger target population, further development is needed to achieve the compression depth and overall CPR skills acquired by face-to-face training.
Trial Registration
ClinicalTrials.gov identifier: NCT04013633
Introduction
Cardiac arrest constitutes a major health care problem, with more than 300 000 deaths annually in the United States alone.1 Early automated external defibrillator (AED) use and high-quality cardiopulmonary resuscitation (CPR) are important determinants of survival.2,3,4,5,6 However, most individuals with cardiac arrest do not receive any form of bystander CPR, which may be because most civilians are not currently trained in CPR.2,3,7,8,9,10 Therefore, increasing awareness, willingness, and capability to perform CPR is promoted as a key issue in international practice guidelines and by leading health care authorities.11,12,13,14,15,16,17
Face-to-face training has long been the standard, but new, low-cost, and fast training methods have recently emerged that may hold the potential to reach a much larger target population. Lifesaver VR (http://lifesavervr.org.uk/) is an innovative, immersive, and interactive educational smartphone app that virtually teaches CPR to app users; the app was developed and endorsed by the Resuscitation Council (United Kingdom) and is specifically mentioned in current CPR guidelines.14,18 It has recently been updated to incorporate a virtual reality (VR) enhancement, allowing users to learn CPR in a realistic, interactive VR setting. Experts in the field consider VR as one of the most promising tools in medical training in general and CPR training in particular.19,20 Virtual reality training through the app can be performed at home at a low cost at any moment and takes approximately 20 minutes to complete. Virtual reality training may therefore overcome important barriers for layperson CPR training.14,21 However, data on the achieved CPR quality are lacking.
To address this gap in knowledge, we performed the Lowlands Saves Lives trial, a randomized clinical trial comparing CPR quality between face-to-face and VR training using the smartphone app. This study was conducted during Lowlands Science, a section of the 3-day Lowlands Music Festival that is specifically dedicated to conducting scientific research.
Methods
Aim and Hypothesis
The methodology of the present study was previously published.22 The primary aim of this study was to compare CPR quality between face-to-face CPR training and training using the VR app. Our hypothesis was that training with the VR app would result in CPR quality that is noninferior to CPR quality achieved by face-to-face training.
Overview of the Study Design and Oversight
The Lowlands Saves Lives trial was a parallel, 1:1 randomized clinical trial with a prospective randomized open blinded end point (PROBE) design.23,24 The Consolidated Standards of Reporting Trials (CONSORT) reporting guideline was also followed.
The study complied with the principles of the Declaration of Helsinki.25 The protocol, available in Supplement 1, was approved by the research ethics committee of the Radboud University Medical Center (Radboudumc, Nijmegen, the Netherlands). An independent clinical research organization (Diagram BV) was responsible for monitoring participant data. Participants were randomized to either face-to-face CPR training or CPR training using the VR app (eFigure 1 in Supplement 2). All participants provided written informed consent.
Setting
This study was conducted from August 16 to 18, 2019, at Lowlands Science, a section of the 3-day Lowlands Music Festival (Biddinghuizen, the Netherlands; 55 000 attendees) dedicated exclusively to scientific research.26 Lowlands Science was located at an area separated from the rest of the festival, providing a closed section with an optimal infrastructure for conducting scientific research (eFigure 2 in Supplement 2).
Population
Eligible for inclusion were adult (≥18 years) attendees of Lowlands Science. Participants who were deemed not capable of performing either the training or the posttraining CPR test (eg, physical or cognitive impairment) were excluded by the physicians dedicated to this task. Second, participants with elevated alcohol levels (≥0.5‰, the Dutch legal driving limit) who failed a tandem gait test were also excluded. For this purpose, we performed a law enforcement–grade alcohol breathalyzer test in all participants (AlcoTrue P; Bluepoint Medical). As such, participants with an alcohol level of 0.5‰ or higher who passed a tandem gait test were included.
Randomization and Blinding
Randomization was performed online using Castor Electronic Data Capture. We used a random block randomization algorithm and stratified randomization according to alcohol level, using a binary cutoff value of less than 0.5‰ vs 0.5‰ or higher. The rationale was that in music festivals, alcohol consumption is allowed and common, and alcohol intake may affect CPR skills. Randomization was performed on site in real time. Owing to the nature of the intervention, participants were not blinded, but the outcome assessors were.
Interventions
A standardized 20-minute CPR training was provided by an independent, experienced instructor certified by the Dutch Resuscitation Council, who was not part of the study team and not an employee of the Radboudumc. The training protocol was designed under supervision of our national Basic Life Support course director and based on CPR guidelines and previous brief training protocols.14,27 The ratio of instructors to participants was 1:5. Chest compressions and ventilations were taught using certified CPR manikins (Little Anne; Laerdal Medical). Automated external defibrillator use was practiced using training AEDs (Zoll AED Trainer 3; Zoll Medical).
During VR training, individuals participated in a filmed CPR scenario while wearing VR goggles and headphones, which took approximately 20 minutes. Users became actively involved with the resuscitation of an individual experiencing cardiac arrest and simulated chest compressions by performing compressions on a pillow. The app provided feedback on compression speed and instructions on compression depth. It also taught skills needed for adequate AED use. As equipment, we used smartphones (Samsung S7), headphones, and VR goggles (Zeiss VR One Plus; Carl Zeiss). Both training protocols, a graphical impression of the training areas and in-game footage from the VR app, can be found in eAppendix 1 in Supplement 2.
Outcomes
After the training, CPR quality and overall CPR performance were assessed during a standardized CPR scenario.28 Cardiopulmonary resuscitation tests were performed in closed examination rooms by assessors blinded for study group. The protocol can be found in eAppendix 2 in Supplement 2. Outcome measures were based on current CPR guidelines and on a consensus document describing the preferred outcomes for reporting on CPR quality.16,17,29
The primary outcome measure was CPR quality, expressed as depth (millimeters) and rate (minute−1) of chest compressions. A 2019 review on CPR education confirmed that compression rate and depth are the most widely studied CPR-quality parameters, with strong associations with patient outcome.30 These were measured objectively using certified CPR manikins (Resusci Anne QCPR; Laerdal Medical). The manikins recorded CPR quality parameters, which were stored on an operating device (SimPad; Laerdal Medical) and downloaded for offline analysis.
The key secondary outcome measure was the overall CPR performance expressed as a real-time appointed score by assessors blinded for study group, using the European Resuscitation Council endorsed CPR checklist (eAppendix 2 in Supplement 2). Video recordings of CPR skill tests were made of a subset of participants who provided consent for this additional study feature. A random sample of 20% of all video recordings was reviewed by an external event committee, blinded for study group.
In addition, we gathered data on a series of additional secondary outcome measures. For the present analysis, we report on flow fraction (percentage of time where compressions are given, ie, chest compression fraction) and proportion of compressions with full release (as a measure for leaning). Finally, we calculated proportions of participants meeting guideline CPR quality criteria (ie, the proportion of participants with an average chest compression rate of 100 min−1 to 120 min−1 and the proportion with a mean chest compression depth of 50 mm to 60 mm).16,17
Statistical Analysis
In this noninferiority trial, the null hypothesis was that the VR training app is inferior to face-to-face training. To ensure adequate sample size for both quality parameters, we defined our noninferiority margins based on previous work.27,28,31,32 Appreciating that the increase in compression depth for instructor-led training is 5 mm when compared with pretraining, and that a decrease of 5 mm has been associated with lower survival changes after cardiac arrest, the noninferiority margin was 5 mm.31,32 With an expected standard deviation of 10 mm,27,28,31 an α of 5%, and a power of 90%, we calculated 69 participants per group.
A priori, we determined that our study should be adequately powered in the sample of participants without recent CPR training (within 2 years)31,33 and that we also wanted to explore results in those with training. We anticipated a maximum of 20% of participants with previous training.33 Thus, 80% or more was anticipated not to have had previous training. To achieve adequate power in the sample without training, required groups size was increased with 25%.
Finally, sample size was further increased to account for a 10% dropout rate. Hence, the desired sample size was 1.25 × 1.10 × 69 = 95 participants per group. This also provides adequate power to test noninferiority for chest compression rate, with a noninferiority margin of 17 min−1 and standard deviation of 20 min−1, based on the same studies as for depth.27,28,31
Study parameters were assessed for normal distribution and accordingly reported as means (SDs) or medians (interquartile ranges [IQR]). Primary outcomes were tested for noninferiority using 1-sided 2-sample t tests. Continuous data were compared using t tests or Mann-Whitney U tests and categorical variables reported as numbers (%) and compared using χ2 or Fisher exact tests, whichever appropriate. Prespecified subgroup analyses were performed. A P value of less than .05 was considered statistically significant. Analyses were performed using Stata version 15.1 (StataCorp). Analysis began in September 2019.
Results
Participant Flow and Recruitment
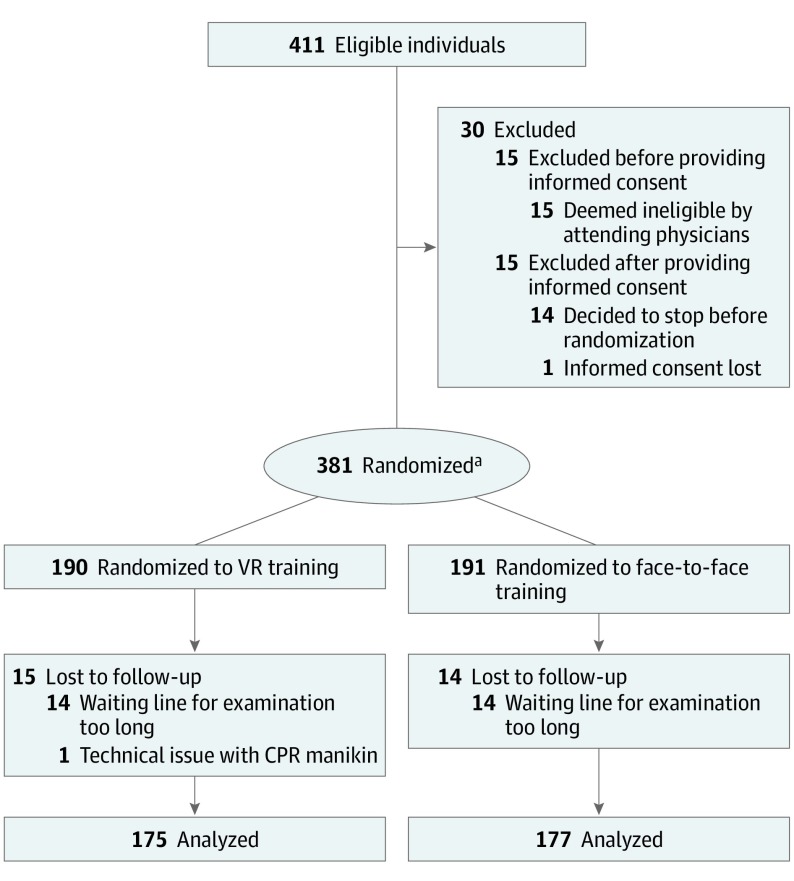
Overall, 396 participants provided informed consent (Figure 1). Of these, 15 (4%) were excluded before randomization; participant withdrawal was mainly related to long waiting lines. As such, 381 participants were randomized: 190 (49.9%) to the VR training app group and 191 (50.1%) to the face-to-face training group. Of all randomized participants, 29 (8%) (15 in the VR and 14 in the face-to-face group, P = .84) decided not to participate in the posttraining CPR test, mainly owing to long waiting lines. Thus, outcome assessment was performed in 352 (92%) of all randomized participants.
Figure 1. CONSORT Flow Diagram.
CPR indicates cardiopulmonary resuscitation; VR, virtual reality.
aAll included participants were able to pass the tandem gait test, if applicable.
Baseline Data
Of 381 individuals, 216 (57%) were women. The median (IQR) age was 26 (22-31) years, and the median (IQR) weight was 70 (63-79) kg (Table). The predominant education level was university education (171 of 381 [45%]). Of all participants, 62 of 381 (16%) had an alcohol level of 0.5% or higher. A total of 58 of 358 participants (16%) had recent CPR training. Baseline characteristics did not differ between both study groups, with the exception of the proportion of health care professionals, which was 16% (n = 31) in the VR training group and 25% (n = 48) in the face-to-face training group (P = .03).
Table. Baseline Characteristics of the Study Populationa.
| Characteristic | Total No. | No. (%) | P Value | ||
|---|---|---|---|---|---|
| Overall (N = 381) | VR (n = 190) | Face to Face (n = 191) | |||
| Women | 379 | 216 (57) | 109 (57) | 107 (57) | .88 |
| Age, median (IQR), y | 381 | 26 (22-31) | 26 (23-31) | 26 (22-31) | .69 |
| Weight, median (IQR), kg | 378 | 70 (63-79) | 70 (64-78) | 71 (62-80) | .86 |
| University education | 381 | 171 (45) | 86 (45) | 85 (45) | .88 |
| Health care professional | 380 | 79 (21) | 31 (16) | 48 (25) | .03 |
| Alcohol level, median (IQR), ‰ | 381 | 0 (0-0.34) | 0 (0-0.36) | 0 (0-0.31) | .64 |
| Alcohol level ≥0.5‰ | 381 | 62 (16) | 35 (18) | 27 (14) | .26 |
| Drugs or narcotics ≤24 h | 369 | 93 (25) | 42 (23) | 51 (28) | .27 |
| Previous CPR course ≤2 y | 358 | 58 (16) | 28 (16) | 30 (17) | .77 |
| BLS course | NA | 49 (84) | 24 (86) | 25 (83) | >.99 |
| ALS course | NA | 9 (16) | 4 (14) | 5 (17) | |
| Witnessed a cardiac arrest | 381 | 57 (15) | 30 (16) | 27 (14) | .65 |
Abbreviations: ALS, advanced life support; BLS, basic life support; CPR, cardiopulmonary resuscitation; IQR, interquartile range; NA, not applicable; VR, virtual reality.
Missing data can be either missing or reported as “Do not wish to disclose” by the participants.
Primary Outcomes
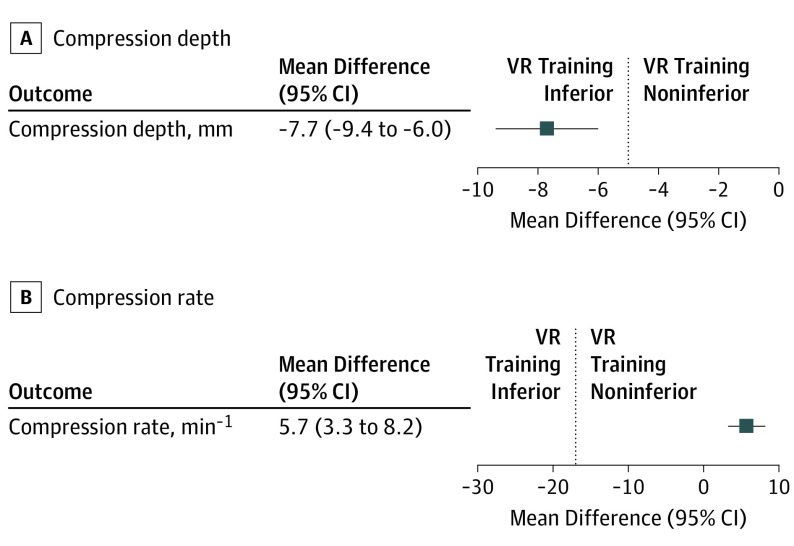
The mean (SD) chest compression depth was 49.1 (10.0) mm in the VR group compared with 56.8 (5.4) mm in the face-to-face group. The mean difference between VR and face-to-face training was −7.7 (95% CI, −9.4 to −6.0) mm. Given the predefined noninferiority margin of −5 mm, VR training was inferior to face-to-face training for chest compression depth, with a P value for inferiority of .99.
The mean (SD) chest compression rate was 114.3 (11.8) min−1 in the VR group, compared with 108.6 (11.6) min−1 in the face-to-face group. The mean (95% CI) difference between VR and face-to-face was 5.7 (3.3-8.2) min−1. Given the predefined noninferiority margin of −17 min−1, VR training was noninferior to face-to-face training for chest compression rate, with a P value for noninferiority of <.001 (Figure 2).
Figure 2. Forest Plots of the Mean Difference in Chest Compression Depth and Rate Between Virtual Reality (VR) and Face-to-Face Training.
Forest plots for the mean difference (95% CI) in chest compression depth and rate between virtual reality (VR) and face-to-face training. The prespecified noninferiority margins were −5 mm for depth and −17 min−1 for rate. For depth, the P value for noninferiority was .99. For rate, the P value for noninferiority was <.001. Dashed line indicates noninferioirity margin.
Secondary Outcomes
Median (IQR) CPR performance score (maximum score, 13) was 10 (8-12) in the VR group compared with 12 (12-13) in the face-to-face training group (P < .001). Individual items of the checklist are reported in the Table in Supplement 2. The intraclass correlation coefficient for assessment by the on-site examiners and the event committee was 0.81. Given this high level of agreement, the reported CPR scores are those of the on-site assessors.
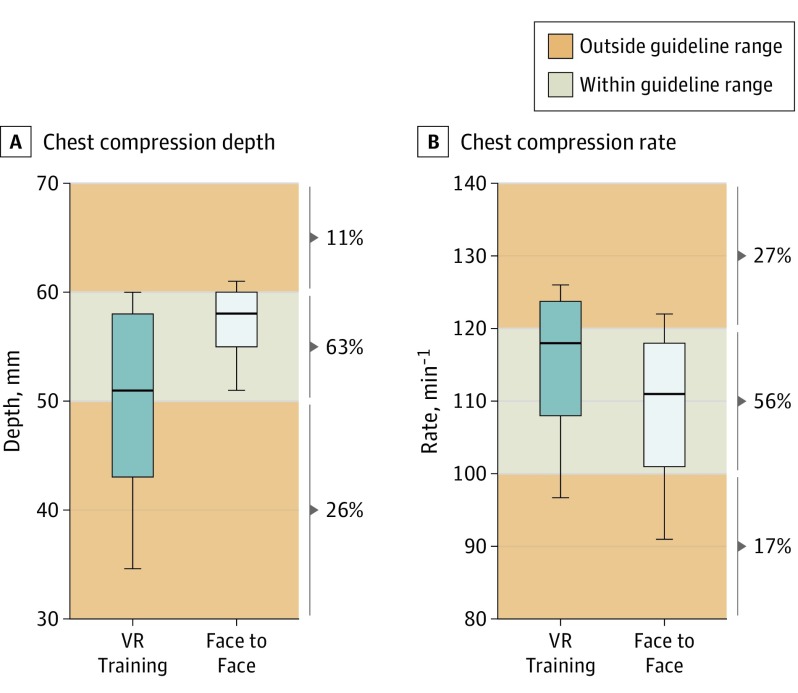
Average chest compression depth within the guideline endorsed range of 50 mm to 60 mm was seen in 51% (n = 89) of VR group, compared with 75% (n = 133) in the face-to-face training group (χ2 = 22.28; P < .001). For the guideline-endorsed chest compression rate of 100 min−1 to 120 min−1, these proportions were 50% (n = 87) in the VR group and 63% (n = 111) in the face-to-face training group (χ2 = 6.04; P = .01). Compression depth and rate in relation to guideline ranges can be found in Figure 3.
Figure 3. Boxplots of Chest Compression Depth and Rate in Relation to Guideline Recommendations.
Boxplots of chest compression rate and depth. Whiskers are 10th and 90th percentiles. Percentages at the side of each graph indicate the proportion of participants with compression depth or rate that is below, within, or above guideline-endorsed ranges respectively. VR indicates virtual reality.
Median flow fraction (ie, chest compression fraction) was 61% (IQR, 52%-66%) in the VR group compared with 67% (IQR, 62%-71%) in the face-to-face training group (P < .001). The proportion of compressions with full release was higher in the former than in the latter (98% [IQR, 59%-100%] vs 88% [IQR, 55%-99%]; P = .002).
Ancillary Analyses
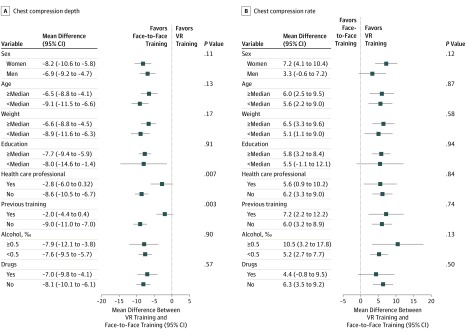
Prespecified subgroup analyses are shown in Figure 4. Heterogeneity of the effect of VR training on chest compression depth was suggested in subgroup analyses according to being a health care professional (P = .007 for interaction) and previous CPR training (P = .003 for interaction). Differences between VR and face-to-face training were significantly smaller in the subgroups with previous training and the subgroup of health care professionals. No other intervention-by-subgroup interactions were identified, neither for compression depth nor for rate.
Figure 4. Subgroup Analyses for Chest Compression Depth and Rate.
Forest plot on prespecified subgroup analyses based on sex, age, weight, education, health care professional, previous cardiopulmonary resuscitation (CPR) training (within 2 years), alcohol level, and drug/substance use. Mean differences in compression depth (A) (millimeters) and compression rate (B) (compressions minute−1) between virtual reality (VR) and face-to-face training, with 95% confidence intervals. The P value for interaction is for testing whether the effect of the intervention on compression depth and rate differs between the subgroups.
Discussion
In this randomized trial including 381 participants recruited on the science section of a music festival, VR compared with face-to-face CPR-training resulted in noninferior chest compression rate but inferior chest compression depth. Overall CPR performance, proportions of participants with average compression depth or rate within guideline ranges, and chest compression fraction were lower in the VR group. Contrastingly, the proportion of compressions with full release was higher. This study confirms the potential of brief face-to-face training to achieve adequate CPR skills27 and provides valuable input for further development of VR training. Although VR may lead to more widely disseminated CPR training, this study suggests that it should be developed further to achieve CPR skills comparable with those acquired by face-to-face training, particularly in terms of compression depth.
Previous Studies and Current Methodology
In follow-up of previous studies on professional pre- and in-hospital treatment strategies, we now performed this study on layperson cardiac arrest care.34,35 Given the prognostic effect of bystander CPR, several health care authorities call for studies on innovative CPR training methods to further disseminate CPR skills among civilians.11,14,15,36,37 Of these innovations, VR is considered one of the most promising, as demonstrated by feasibility studies and reports on questionnaires conducted among CPR professionals.19,20,38,39,40,41 To our knowledge, this is the first study to evaluate the effect of Lifesaver VR training on CPR quality. Whereas previous studies compared VR with other (mobile) apps or compared face-to-face training with apps or games without VR, we now compared VR training directly with face-to-face CPR training.18,33,42
Notably, evaluation of lay education in resuscitation strategies is still a relatively new field of research, with limited high-quality data, and studies are heterogenous in design and prone to bias.14,43 We aimed to address these issues by using a PROBE design and standardized CPR skill assessment, with independent data monitoring.
CPR Quality and Performance Metrics
Our results show that VR training results in noninferior chest compression rate but inferior compression depth. This indicates that VR seems less suitable than face-to-face training to provide adequate bystander CPR. However, even in the VR group, at least half of the participants met the guideline-endorsed depth or rate requirements. Moreover, previous studies showed decreased survival in case of compression depth less than 38 mm, which we found in only 14% of participants in the VR group and 2% in the face-to-face group.32,44 This confirms the potential to acquire life-saving CPR skills in brief CPR training sessions.27 Notably, CPR performance metrics in our study were comparable with previous studies on brief and multihour training.27,28,31
In a previous study evaluating brief VR CPR training in which compressions were not practiced on a pillow but by pressing a button, average compression depth was 38 mm, compared with 49 mm in the present VR and 57 mm in our face-to-face group.33 In a 2019 large study on multihour training,28 the proportion of participants with an average compression rate between 100 min−1 to 120 min−1 in their instructor-led group was 41%, compared with 50% in the present VR and 63% in the face-to-face groups. For the required average depth of 50 mm to 60 mm, this proportion was 57% in the previous study, compared with 51% in the present VR and 75% in the face-to-face groups.28 Notably, the results from our face-to-face group are in line with a previous study on brief instructor-led training, in which the brief training resulted in similar CPR quality as multihour training.27 To further improve comparisons between education strategies, a 2019 review31 underscored the need for uniform reporting of outcome measures.
The CPR performance score was lower in the VR group, indicating that VR might be less suitable than face-to-face training for acquiring knowledge on the entire CPR algorithm. As can be seen in the eTable in Supplement 2, the difference in CPR performance score between both groups was mainly driven by lower proportions in the subcategory CPR, whereas the AED items were more evenly distributed. With regard to this score, it should be noted that although it is the official CPR performance checklist of the European Resuscitation Council, we are unaware of studies that evaluated its external validity.
We found a median chest compression fraction of more than 60% in both groups, which is in line with guideline recommendations.16,17 Data on the relationship between leaning and survival are scarce, but guidelines recommend minimization of leaning based on pathophysiological insights from mechanistic studies.16,17 Proportions of compressions with full release were high in both groups and highest in the VR group, indicating that this skill can be taught during brief CPR training.
Prespecified Subgroup Analyses
A prespecified subgroup analysis revealed a significant interaction between previous CPR training and compression depth and between being a health care professional and depth: the difference between study groups was smaller in participants with previous CPR training or participants who were health care professionals. It could be interesting to study VR for retraining of individuals who were initially trained using the standard approach. Retraining is a major topic in current CPR guidelines, and the optimal training method for such trainings is under active investigation.11,14,15,36,37
Owing to our study setting, we studied a sample of young festival attendees. Inherent to this setting, there had been alcohol and drug use among participants. Although the subgroup analyses on these factors should be considered merely hypothesis generating, our findings indicate no significant effect of alcohol or drug use on differences in depth or rate between VR and face-to-face training.
Directions for Further VR App Development
The lower compression depth in the VR group could relate to compressions being practiced on a pillow instead of a manikin, to mimic the situation where the app is used at home. Therefore, no feedback is given on depth, but only on rate. A previous study reported on a VR system with real-time feedback on depth, which may also be beneficial for the present VR app.45 We also found lower scores on the CPR checklist possibly because the steps of the CPR algorithm only appear once in the VR scenario, whereas in face-to-face training these are repeated multiple times. Teaching a complex procedure in small portions prevents cognitive fatigue, therefore providing the CPR algorithm in small steps with repetition in between may be beneficial as well.15,46
Limitations
Although our 20-minute face-to-face training protocol resulted in similar outcomes as a previous brief training protocol in which outcomes and retention were comparable with multihour training, it differs from the standard of current CPR courses.14,47 However, our protocol complies with all guideline requirements on CPR training.14 The study setting resulted in a young, highly educated group of participants. Although this is an important target group for CPR education, it may limit generalizability of our findings to, for example, elderly civilians. Owing to logistical reasons, CPR skills prior to the test were not assessed and no data on retention of CPR skills will be collected. In total, 8% did not perform the examinations because of the sometimes long waiting lines for the 2 examination rooms, which was related to the appointed restriction in square footage for each research group. Furthermore, we unexpectedly found a baseline difference between both groups in the proportion of health care professionals. This was addressed in stratified analyses, which did not alter our conclusions. Lastly, although we found overall acceptable CPR quality in both groups, the actual CPR performance in real life and the corresponding effect on patient outcome are unknown.
Conclusions
In this randomized trial, we found that VR training was noninferior compared with face-to-face training with respect to chest compression rate but inferior with respect to chest compression depth. Although VR training may hold the potential to reach a larger target population, further development is needed to achieve the chest compression depth and overall CPR skills acquired by face-to-face training.
Trial protocol
eFigure 1. Study flowchart
eFigure 2. Graphical impression of the study setting
eTable. Individual components of the CPR-performance checklist
eAppendix 1. Training protocols
eAppendix 2. Post training CPR-test protocol
eReferences
Data sharing statement
References
- 1.Benjamin EJ, Virani SS, Callaway CW, et al. ; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart Disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67-e492. doi: 10.1161/CIR.0000000000000558 [DOI] [PubMed] [Google Scholar]
- 2.Malta Hansen C, Kragholm K, Pearson DA, et al. . Association of bystander and first-responder intervention with survival after out-of-hospital cardiac arrest in North Carolina, 2010-2013. JAMA. 2015;314(3):255-264. doi: 10.1001/jama.2015.7938 [DOI] [PubMed] [Google Scholar]
- 3.Duval S, Pepe PE, Aufderheide TP, et al. . Optimal combination of compression rate and depth during cardiopulmonary resuscitation for functionally favorable survival. JAMA Cardiol. 2019. doi: 10.1001/jamacardio.2019.2717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bobrow BJ, Spaite DW, Vadeboncoeur TF, et al. . Implementation of a regional telephone cardiopulmonary resuscitation program and outcomes after out-of-hospital cardiac arrest. JAMA Cardiol. 2016;1(3):294-302. doi: 10.1001/jamacardio.2016.0251 [DOI] [PubMed] [Google Scholar]
- 5.Fordyce CB, Hansen CM, Kragholm K, et al. . Association of public health initiatives with outcomes for out-of-hospital cardiac arrest at home and in public locations. JAMA Cardiol. 2017;2(11):1226-1235. doi: 10.1001/jamacardio.2017.3471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hansen SM, Hansen CM, Folke F, et al. . Bystander defibrillation for out-of-hospital cardiac arrest in public vs residential locations. JAMA Cardiol. 2017;2(5):507-514. doi: 10.1001/jamacardio.2017.0008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kragholm K, Wissenberg M, Mortensen RN, et al. . Bystander efforts and 1-year outcomes in out-of-hospital cardiac arrest. N Engl J Med. 2017;376(18):1737-1747. doi: 10.1056/NEJMoa1601891 [DOI] [PubMed] [Google Scholar]
- 8.Kitamura T, Kiyohara K, Sakai T, et al. . Public-access defibrillation and out-of-hospital cardiac arrest in Japan. N Engl J Med. 2016;375(17):1649-1659. doi: 10.1056/NEJMsa1600011 [DOI] [PubMed] [Google Scholar]
- 9.Hasselqvist-Ax I, Riva G, Herlitz J, et al. . Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372(24):2307-2315. doi: 10.1056/NEJMoa1405796 [DOI] [PubMed] [Google Scholar]
- 10.Blewer AL, Ibrahim SA, Leary M, et al. . Cardiopulmonary resuscitation training disparities in the United States. J Am Heart Assoc. 2017;6(5):6. doi: 10.1161/JAHA.117.006124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Panchal AR, Cash RE, Crowe RP, et al. . Delphi analysis of science gaps in the 2015 American Heart Association cardiac arrest guidelines. J Am Heart Assoc. 2018;7(13):7. doi: 10.1161/JAHA.118.008571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malta Hansen C, Rosenkranz SM, Folke F, et al. . Lay bystanders’ perspectives on what facilitates cardiopulmonary resuscitation and use of automated external defibrillators in real cardiac arrests. J Am Heart Assoc. 2017;6(3):6. doi: 10.1161/JAHA.116.004572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Søreide E, Morrison L, Hillman K, et al. ; Utstein Formula for Survival Collaborators . The formula for survival in resuscitation. Resuscitation. 2013;84(11):1487-1493. doi: 10.1016/j.resuscitation.2013.07.020 [DOI] [PubMed] [Google Scholar]
- 14.Greif R, Lockey AS, Conaghan P, Lippert A, De Vries W, Monsieurs KG; Education and implementation of resuscitation section Collaborators; Collaborators . European Resuscitation Council guidelines for resuscitation 2015: section 10: education and implementation of resuscitation. Resuscitation. 2015;95:288-301. doi: 10.1016/j.resuscitation.2015.07.032 [DOI] [PubMed] [Google Scholar]
- 15.Cheng A, Nadkarni VM, Mancini MB, et al. ; American Heart Association Education Science Investigators; and on behalf of the American Heart Association Education Science and Programs Committee, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Council on Cardiovascular and Stroke Nursing; and Council on Quality of Care and Outcomes Research . Resuscitation education science: educational strategies to improve outcomes from cardiac arrest: a scientific statement from the American Heart Association. Circulation. 2018;138(6):e82-e122. doi: 10.1161/CIR.0000000000000583 [DOI] [PubMed] [Google Scholar]
- 16.Kleinman ME, Brennan EE, Goldberger ZD, et al. . Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18)(suppl 2):S414-S435. doi: 10.1161/CIR.0000000000000259 [DOI] [PubMed] [Google Scholar]
- 17.Perkins GD, Handley AJ, Koster RW, et al. ; Adult basic life support and automated external defibrillation section Collaborators . European resuscitation council guidelines for resuscitation 2015: section 2: adult basic life support and automated external defibrillation. Resuscitation. 2015;95:81-99. doi: 10.1016/j.resuscitation.2015.07.015 [DOI] [PubMed] [Google Scholar]
- 18.Yeung J, Kovic I, Vidacic M, et al. . The school Lifesavers study-A randomised controlled trial comparing the impact of Lifesaver only, face-to-face training only, and Lifesaver with face-to-face training on CPR knowledge, skills and attitudes in UK school children. Resuscitation. 2017;120:138-145. doi: 10.1016/j.resuscitation.2017.08.010 [DOI] [PubMed] [Google Scholar]
- 19.Wong MAME, Chue S, Jong M, Benny HWK, Zary N. Clinical instructors’ perceptions of virtual reality in health professionals’ cardiopulmonary resuscitation education. SAGE Open Med. 2018;6:2050312118799602. doi: 10.1177/2050312118799602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Semeraro F, Scapigliati A, Ristagno G, et al. . Virtual reality for CPR training: how cool is that? dedicated to the “next generation”. Resuscitation. 2017;121:e1-e2. doi: 10.1016/j.resuscitation.2017.09.024 [DOI] [PubMed] [Google Scholar]
- 21.Sasson C, Haukoos JS, Bond C, et al. . Barriers and facilitators to learning and performing cardiopulmonary resuscitation in neighborhoods with low bystander cardiopulmonary resuscitation prevalence and high rates of cardiac arrest in Columbus, OH. Circ Cardiovasc Qual Outcomes. 2013;6(5):550-558. doi: 10.1161/CIRCOUTCOMES.111.000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nas J, Thannhauser J, Vart P, et al. . Rationale and design of the Lowlands Saves Lives trial: a randomised trial to compare CPR quality and long-term attitude towards CPR performance between face-to-face and virtual reality training with the Lifesaver VR app. BMJ Open. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hansson L, Hedner T, Dahlöf B. Prospective randomized open blinded end-point (PROBE) study: a novel design for intervention trials.:Prospective Randomized Open Blinded End-Point. Blood Press. 1992;1(2):113-119. doi: 10.3109/08037059209077502 [DOI] [PubMed] [Google Scholar]
- 24.Ford I, Norrie J. Pragmatic trials. N Engl J Med. 2016;375(5):454-463. doi: 10.1056/NEJMra1510059 [DOI] [PubMed] [Google Scholar]
- 25.World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 26.de Ronde A, van Aken M, de Puit M, de Poot C. A study into fingermarks at activity level on pillowcases. Forensic Sci Int. 2019;295:113-120. doi: 10.1016/j.forsciint.2018.11.027 [DOI] [PubMed] [Google Scholar]
- 27.Roppolo LP, Pepe PE, Campbell L, et al. . Prospective, randomized trial of the effectiveness and retention of 30-min layperson training for cardiopulmonary resuscitation and automated external defibrillators: the American Airlines Study. Resuscitation. 2007;74(2):276-285. doi: 10.1016/j.resuscitation.2006.12.017 [DOI] [PubMed] [Google Scholar]
- 28.Bylow H, Karlsson T, Claesson A, Lepp M, Lindqvist J, Herlitz J. Self-learning training versus instructor-led training for basic life support: a cluster randomised trial. Resuscitation. 2019;139:122-132. doi: 10.1016/j.resuscitation.2019.03.026 [DOI] [PubMed] [Google Scholar]
- 29.Kramer-Johansen J, Edelson DP, Losert H, Köhler K, Abella BS. Uniform reporting of measured quality of cardiopulmonary resuscitation (CPR). Resuscitation. 2007;74(3):406-417. doi: 10.1016/j.resuscitation.2007.01.024 [DOI] [PubMed] [Google Scholar]
- 30.Considine J, Gazmuri RJ, Perkins GD, et al. . Chest compression components (rate, depth, chest wall recoil and leaning): a scoping review. Resuscitation. 2019;S0300-9572(19)30608-2. doi: 10.1016/j.resuscitation.2019.08.042 [DOI] [PubMed] [Google Scholar]
- 31.Riggs M, Franklin R, Saylany L. Associations between cardiopulmonary resuscitation (CPR) knowledge, self-efficacy, training history and willingness to perform CPR and CPR psychomotor skills: a systematic review. Resuscitation. 2019;138:259-272. doi: 10.1016/j.resuscitation.2019.03.019 [DOI] [PubMed] [Google Scholar]
- 32.Stiell IG, Brown SP, Nichol G, et al. ; Resuscitation Outcomes Consortium Investigators . What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients? Circulation. 2014;130(22):1962-1970. doi: 10.1161/CIRCULATIONAHA.114.008671 [DOI] [PubMed] [Google Scholar]
- 33.Leary M, McGovern SK, Chaudhary Z, Patel J, Abella BS, Blewer AL. Comparing bystander response to a sudden cardiac arrest using a virtual reality CPR training mobile app versus a standard CPR training mobile app. Resuscitation. 2019;139:167-173. doi: 10.1016/j.resuscitation.2019.04.017 [DOI] [PubMed] [Google Scholar]
- 34.Lemkes JS, Janssens GN, van der Hoeven NW, et al. . Coronary angiography after cardiac arrest without ST-segment elevation. N Engl J Med. 2019;380(15):1397-1407. doi: 10.1056/NEJMoa1816897 [DOI] [PubMed] [Google Scholar]
- 35.Bonnes JL, Brouwer MA, Navarese EP, et al. . Manual cardiopulmonary resuscitation versus CPR including a mechanical chest compression device in out-of-hospital cardiac arrest: a comprehensive meta-analysis from randomized and observational studies. Ann Emerg Med. 2016;67(3):349-360.e3. doi: 10.1016/j.annemergmed.2015.09.023 [DOI] [PubMed] [Google Scholar]
- 36.Bhanji F, Donoghue AJ, Wolff MS, et al. . Part 14: education: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18)(suppl 2):S561-S573. doi: 10.1161/CIR.0000000000000268 [DOI] [PubMed] [Google Scholar]
- 37.Rumsfeld JS, Brooks SC, Aufderheide TP, et al. ; American Heart Association Emergency Cardiovascular Care Committee; Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Council on Quality of Care and Outcomes Research; Council on Cardiovascular and Stroke Nursing; and Council on Epidemiology and Prevention . Use of mobile devices, social media, and crowdsourcing as digital strategies to improve emergency cardiovascular care: a scientific statement from the American Heart Association. Circulation. 2016;134(8):e87-e108. doi: 10.1161/CIR.0000000000000428 [DOI] [PubMed] [Google Scholar]
- 38.Bench S, Winter C, Francis G. Use of a virtual reality device for basic life support training: prototype testing and an exploration of users’ views and experience. Simul Healthc. 2019;14(5):287-292. doi: 10.1097/SIH.0000000000000387 [DOI] [PubMed] [Google Scholar]
- 39.Cerezo Espinosa C, Segura Melgarejo F, Melendreras Ruiz R, et al. . Virtual reality in cardiopulmonary resuscitation training: a randomized trial [in Spanish]. Emergencias. 2019;31(1):43-46. [PubMed] [Google Scholar]
- 40.Khanal P, Vankipuram A, Ashby A, et al. . Collaborative virtual reality based advanced cardiac life support training simulator using virtual reality principles. J Biomed Inform. 2014;51:49-59. doi: 10.1016/j.jbi.2014.04.005 [DOI] [PubMed] [Google Scholar]
- 41.Semeraro F, Frisoli A, Bergamasco M, Cerchiari EL. Virtual reality enhanced mannequin (VREM) that is well received by resuscitation experts. Resuscitation. 2009;80(4):489-492. doi: 10.1016/j.resuscitation.2008.12.016 [DOI] [PubMed] [Google Scholar]
- 42.Drummond D, Delval P, Abdenouri S, et al. . Serious game versus online course for pretraining medical students before a simulation-based mastery learning course on cardiopulmonary resuscitation: a randomised controlled study. Eur J Anaesthesiol. 2017;34(12):836-844. doi: 10.1097/EJA.0000000000000675 [DOI] [PubMed] [Google Scholar]
- 43.Mäkinen M, Niemi-Murola L, Mäkelä M, Castren M. Methods of assessing cardiopulmonary resuscitation skills: a systematic review. Eur J Emerg Med. 2007;14(2):108-114. doi: 10.1097/MEJ.0b013e328013dc02 [DOI] [PubMed] [Google Scholar]
- 44.Stiell IG, Brown SP, Christenson J, et al. ; Resuscitation Outcomes Consortium (ROC) Investigators . What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med. 2012;40(4):1192-1198. doi: 10.1097/CCM.0b013e31823bc8bb [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Semeraro F, Ristagno G, Giulini G, et al. . Virtual reality cardiopulmonary resuscitation (CPR): comparison with a standard CPR training mannequin. Resuscitation. 2019;135:234-235. doi: 10.1016/j.resuscitation.2018.12.016 [DOI] [PubMed] [Google Scholar]
- 46.Young JQ, Van Merrienboer J, Durning S, Ten Cate O. Cognitive Load Theory: implications for medical education: AMEE Guide No. 86. Med Teach. 2014;36(5):371-384. doi: 10.3109/0142159X.2014.889290 [DOI] [PubMed] [Google Scholar]
- 47.Roppolo LP, Heymann R, Pepe P, et al. . A randomized controlled trial comparing traditional training in cardiopulmonary resuscitation (CPR) to self-directed CPR learning in first year medical students: the two-person CPR study. Resuscitation. 2011;82(3):319-325. doi: 10.1016/j.resuscitation.2010.10.025 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial protocol
eFigure 1. Study flowchart
eFigure 2. Graphical impression of the study setting
eTable. Individual components of the CPR-performance checklist
eAppendix 1. Training protocols
eAppendix 2. Post training CPR-test protocol
eReferences
Data sharing statement