Abstract
Around 200 million people were affected by conflict and natural disasters in 2015. Whereas those populations are at a particular high risk of death, optimal breastfeeding and complementary feeding practices could prevent almost 20% of deaths amongst children less than 5 years old. Yet, coverage of interventions for improving infant and young child feeding (IYCF) practices in emergencies is low, partly due to lack of evidence. Considering the paucity of data generated in emergencies to inform programming, we conducted an evidence map from reviews that included low‐ and middle‐income countries and looked at several interventions: (a) social and behavioural change interpersonal and mass communication for promoting breastfeeding and adequate complementary feeding; (b) provision of donated complementary food; (c) home‐based fortification with multiple micronutrient powder; (d) capacity building; (e) cash transfers; (f) agricultural or fresh food supply interventions; and (g) psychological support to caretakers. We looked for availability of evidence of these interventions to improve IYCF practices and nutritional status of infants and young children. We identified 1,376 records and included 28 reviews meeting the inclusion criteria. The highest number of reviews identified was for behavioural change interpersonal communication for promoting breastfeeding, whereas no review was identified for psychological support to caretakers. We conclude that any further research should focus on the mechanisms and delivery models through which effectiveness of interventions can be achieved and on the influence of contextual factors. Efforts should be renewed to generate evidence of effectiveness of IYCF interventions during humanitarian emergencies despite the challenges.
Keywords: breastfeeding, cash transfers, complementary feeding, feeding practices, infant, young child
1. BACKGROUND
Humanitarian emergencies affect millions of people each year with around 59.5 million forcibly displaced by violence and conflict and 141 million affected by natural disasters in 2015 (OCHA, 2015). Those populations, and especially young children, are at a particular high risk of death (Reed, Keely, & Waldman, 2001).
Furthermore, 13% of all deaths amongst children less than 5 years old could be averted if breastfeeding was practiced optimally, whereas good complementary feeding could prevent another 6% of deaths (Jones et al., 2003). Globally, the deaths of 823,000 children aged 5 and under could be prevented yearly if breastfeeding practices were scaled up to near universal level (Victora et al., 2016). International recommendations include starting breastfeeding within an hour of birth; exclusive breastfeeding for the first 6 months of life; continued breastfeeding for at least 2 years; and complementary feeding with nutritionally adequate, appropriately prepared, and safe foods, in addition to breast milk (WHO, 2015). In addition, optimal foetal and child nutrition and development are dependent on optimal care and low disease burden (Black et al., 2013).
Poor infant and young child feeding (IYCF) practices are common in non‐emergency circumstances (Requejo, Victora, & Bryce, 2015). This is compounded by further challenges during emergencies, including misconceptions about breastfeeding, inappropriate feeding prior to and during disasters, food insecurity hampering the procurement of nutritious food, competing household needs, and stress and psychological trauma that affect childcare practices (Save the Children, 2012). Moreover, donations of breast milk substitutes (BMS) and nontargeted distributions of BMS might also interfere with and undermine breastfeeding. Studies that investigated the consequences of poor IYCF practices and inappropriate BMS distributions in emergencies showed adverse effect on morbidity and mortality (Arvelo et al., 2010; Hipgrave, Assefa, Winoto, & Sukotjo, 2012; Jakobsen et al., 2003).
Despite these facts, programmes addressing IYCF practices are far less commonly implemented than programmes treating malnourished children, such as community‐based management of acute malnutrition. This might be because treatment models usually get more attention than prevention models; urgent needs to address suboptimal IYCF may not be fully recognised by global public health leaders, and there is limited guidance on how to put a practical set of steps in place to support infant and young child feeding in emergencies (IYCF‐E). A review investigating the reasons for the poor uptake of IYCF‐E programmes highlighted the following practical actions at global level that would most help practitioners to continue or strengthen IYCF‐E programming: (a) development of practical step‐by‐step guidance on how to do IYCF‐E in different contexts; (b) development of evaluation tools to measure outcome and impact; (c) creation of an evidence base; (d) delivery of training; (e) advocacy for funding; and (f) experience‐sharing and development of multisectoral links (Save the Children, 2012). The lack of evidence on the effectiveness of IYCF‐E programmes has also been highlighted by several papers reviewing evidence‐based nutrition interventions in emergencies (Blanchet, Sistenich, & Ramesh, 2015; Webb et al., 2014).
Considering the paucity of data generated in emergency contexts, one can draw on evidence from non‐emergency settings to inform programming in emergencies (Allen, 2014), and especially from low‐ and middle‐income countries (LMIC), where most of the emergencies occur. However, guidelines on child health care in emergency settings seldom draw on available evidence (Turner, Barnes, Reid, & Garrubba, 2010).
To better inform IYCF‐E programming, we mapped evidence from reviews that included LMIC and looked at interventions that are commonly implemented in emergencies. We looked at the breadth, quality, and depth of the available evidence as well as the main gaps in evidence.
Key messages.
More reviews should focus on the mechanisms and delivery models through which effectiveness of interventions can be achieved.
The main weaknesses in quality of reviews were insufficiency in assessment of quality of primary studies and the lack of a comprehensive search strategy.
The overlapping of primary studies in several reviews of the same intervention might increase the influence of these studies on the overall findings.
Efforts should be renewed to generate evidence of effectiveness of IYCF interventions during humanitarian emergencies despite the challenges.
2. METHODOLOGY
We conducted an evidence gap map analysis (Snilstveit, Vojtkova, Bhavsar, & Gaarder, 2013) mapping out literature reviews and presenting a visual overview of existing evidence and gaps using a framework representing the universe of relevant interventions and outcomes for IYCF‐E.
2.1. Scope
The study framework included nutrition specific and nutrition sensitive interventions aimed at sustaining or improving IYCF practices and/or nutritional status that are commonly implemented in emergencies (Global Nutrition Cluster, 2011; The Sphere Project, 2011): (a) social and behavioural change interpersonal communication for promoting breastfeeding (SBC‐IPC‐BF); (b) social and behavioural change interpersonal communication for promoting adequate complementary feeding (SBC‐IPC‐CF); (c) social and behaviour change mass communication (SBC‐MC) for promoting breastfeeding and adequate complementary feeding; (d) provision of donated complementary food; (e) home‐based fortification with multiple micronutrient powder (MNP); (f) capacity building; (g) cash transfers (CT), microcredit, or vouchers; (h) agricultural or fresh food supply interventions for diet diversification; and (i) psychological support to caretakers.
The outcomes considered encompassed (a) IYCF awareness and knowledge; (b) IYCF attitudes and beliefs; (c) IYCF practices, including (1) early initiation of breastfeeding, (2) exclusive breastfeeding amongst infants 0–6 months, (3) breastfeeding rate, (4) duration of breastfeeding, (5) meal frequency, (6) diet diversity, and (7) micronutrient intake; and (d) nutritional status, including (1) ponderal growth, (2) linear growth, and (3) micronutrient status. Ponderal growth comprised weight gain, change in weight‐for‐height/length, and wasting whereas linear growth included height/length gain, change in height/length‐for‐age, and stunting.
2.2. Search strategy
We conducted a systematic review of published reviews on Campbell Library for systematic reviews databases, the Cochrane Database of Systematic Reviews, the Database of Abstracts of Reviews of Effects, Health Systems Evidence, Health Evidence, and the 3ie Database of systematic reviews. Snowballing, that is, tracking back and pursuing references of relevant papers, was also used. Inclusion was limited to peer‐reviewed reviews published between January 2000 and April 2016 in English or French. Reviews limited to studies conducted in only high‐income countries were discarded. When reviews where periodically revised, we only included the latest update. We used specific key words for each intervention (Appendix S1).
2.3. Critical appraisal
Due to resource constraints, we were not able to appraise the quality of the reviews, but we reported available data on quality of primary studies, quality of evidence generated, and quality of review methodology.
2.3.1. Quality of primary studies
When reported in the reviews, we mentioned criteria for assessing primary studies and results of appraisal of their quality.
2.3.2. Quality of evidence
When reported in the reviews, we described criteria and judgement about the quality of the evidence. Criteria for rating the quality of the evidence differed across study but were generally based on the extent and design quality of the primary studies included in the reviews and on the strength of the overall association calculated in the meta‐analyses. The quality of evidence was generally classified by the reviews as low, medium, or high quality of evidence.
2.3.3. Methodological quality of reviews
We used the rating performed by http://www.healthevidence.org using criteria similar, but not identical, to AMSTAR (HealthEvidence, n.d.). The scoring system included appraisal of the following 10 criteria: (a) focused research question that includes the description of population, intervention, comparison, and outcome; (b) explicit selection criteria of studies, including decisions related to the target population, intervention, outcome(s), and the research design (e.g., Randomised Control Trial (RCT), cohort, and participatory); (c) comprehensive search strategy, including multiple database searches and a variety of other search strategies; (d) search strategy covering a sufficient time period (usually a minimum of 10 years); (e) level of evidence of included studies depending on research design; (f) methodological quality assessment of included studies using a standardised assessment tool/scale and including specific criteria related to research design, study sample, participation rate, sources of bias, data collection, attrition rate, and data analysis; (g) quality assessment of studies conducted by two authors; (h) assessment of appropriateness of combining study results (e.g., test of homogeneity); (i) determination of an overall measure of effect by assigning the studies of highest methodological quality greater weigh; and (j) author's interpretation of results of included studies supported by the data.
Reviews were rated strong if total score was 8–10; moderate if total score 5–7; and weak if total score 4 or less.
2.4. Overlapping of primary studies
We listed primary studies included in each review, compared them, and reported the number of overlapping studies.
3. RESULTS
We identified 1,376 records (Figure 1). After exclusion of duplicated records, title and abstract reading of all papers, and a full text reading of selected papers, we included 28 reviews that met the inclusion criteria (Bassani et al., 2013; Berti, Krasevec, & FitzGerald, 2004; Bhutta et al., 2008; Chapman, Morel, Anderson, Damio, & Pérez‐Escamilla, 2010; De‐Regil, Suchdev, Vist, Wallester, & Peña‐Rosas, 2011; Dewey & Adu‐afarwuah, 2008; Gibson & Anderson, 2009; Gilmore & McAuliffe, 2013; Giugliani, Horta, Loret de Mola, Lisboa, & Victora, 2015; Hall, 2011; Haroon, Das, Salam, Imdad, & Bhutta, 2013; Howe‐Heyman & Lutenbacher, 2016; Imdad, Yakoob, & Bhutta, 2011; Jolly et al., 2012; Kristjansson et al., 2015; Lagarde, Haines, & Palmer, 2007; Lagarde, Haines, & Palmer, 2009; Lassi, Das, Zahid, Imdad, & Bhutta, 2013; Leroy, Ruel, & Verhofstadt, 2009; Lewin et al., 2010; Masset, Haddad, Cornelius, & Isaza‐Castro, 2012; De Oliveira, Camacho, & Tedstone, 2001; Pega, Sy, Walter, & Lhachimi, 2015; Renfrew, McCormick, Wade, Quinn, & Dowswell, 2012; Salam, MacPhail, Das, & Bhutta, 2013; Sguassero, de Onis, Bonotti, & Carroli, 2012; Sinha et al., 2015; Sudfeld, Fawzi, & Lahariya, 2012; Sunguya et al., 2013). For reviews used as a basis for Lancet series, we included the most detailed versions published in other journals rather than the Lancet reference: Giugliani et al. (2015) and Sinha et al. (2015) were used to develop the first and second paper of the Lancet Series on breastfeeding published early 2016 (Rollins et al., 2016; Victora et al., 2016;) whereas Bhutta et al. (2013) based their paper of the Lancet Series on Maternal and Child Nutrition on the reviews by Bassani et al., 2013; Haroon et al., 2013; Lassi et al., 2013; and Salam et al., 2013.
Figure 1.
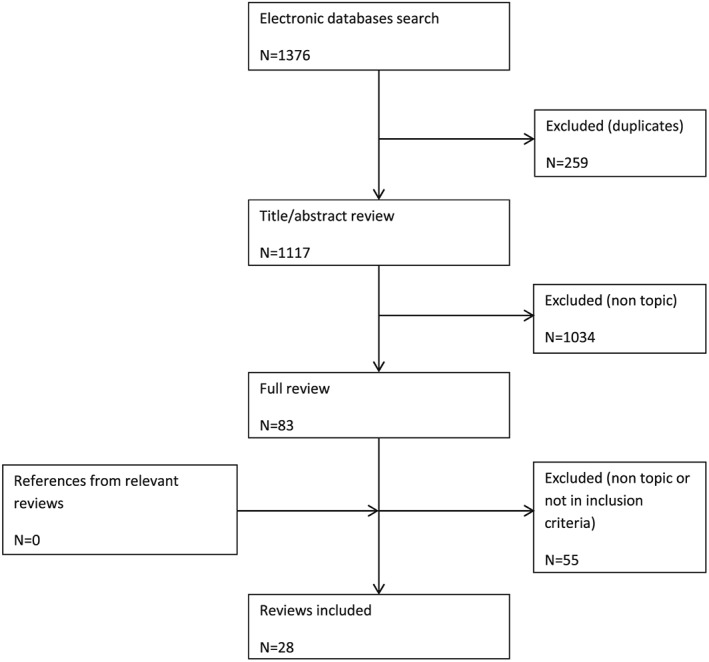
Flow diagram of reviews
Most reviews examined several outcomes, and some also examined several interventions. Overall, the most investigated outcomes were linear growth, ponderal growth, exclusive breastfeeding rate amongst 0‐ to 6‐month olds, and micronutrient status whereas few reviews investigated complementary feeding practices, and no review investigated IYCF awareness and knowledge (Table 1).
Table 1.
Number of reviews examining the effect of IYCF interventions on caretaker's IYCF awareness, knowledge and practices, and child's nutritional status
| IYCF awareness and knowledge | IYCF practices | Nutritional status | Total number of systematic reviews per interventionc | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Early initiation of breast‐ feeding |
Exclusive breast‐feeding 0–6 month olds |
Breast‐feeding rate | Breast‐feeding duration | Re‐lactation | Breast milk substitute consumption | Feeding frequency and diet diversity | Micronutrient intakes | Ponderal growtha | Linear growthb | Micronutrient status | ||
| Social and behaviour change interpersonal communication for promoting breastfeeding | ||||||||||||
| 0 | 1 | 10 | 8 | 3 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 13 |
| Social and behaviour change interpersonal communication for promoting adequate complementary feeding | ||||||||||||
| 0 | NA | NA | NA | NA | NA | NA | 1 | 1 | 3 | 4 | 1 | 4 |
| Social and behaviour change mass communication for promoting adequate breastfeeding and complementary feeding | ||||||||||||
| 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Provision of donated complementary food | ||||||||||||
| NA | NA | NA | NA | NA | NA | NA | 0 | 0 | 5 | 6 | 2 | 6 |
| Home fortification with multiple micronutrient supplementation | ||||||||||||
| NA | NA | NA | NA | NA | NA | NA | NA | 0 | 2 | 2 | 3 | 3 |
| Capacity building | ||||||||||||
| 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Psychological support to mothers | ||||||||||||
| 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cash transfer and microcredit | ||||||||||||
| 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 2 | 4 | 2 | 5 |
| Agricultural or fresh food supply interventions for diet diversification | ||||||||||||
| NA | NA | NA | NA | NA | NA | NA | 3 | 0 | 4 | 4 | 2 | 4 |
| Total number of systematic reviews per outcome | ||||||||||||
| 0 | 2 | 11 | 9 | 3 | 0 | 0 | 5 | 1 | 17 | 21 | 10 | ‐a |
Note. IYCF = infant and young child feeding.
Includes weight gain, change in weight‐for‐height/length, and wasting defined as weight‐for‐height/length < −2 Z‐scores.
Includes height/length gain, change in height/length‐for‐age, and stunting defined as height/length‐for‐age < −2 Z‐scores.
Total number of systematic reviews for an intervention can be less than the total of the columns because most reviews looked at several outcomes.
Nineteen reviews described quality of primary studies and 14 reviews reported quality of evidence. We extracted appraisal of methodological quality of reviews from health evidence for 19 of the 28 reviews.
3.1. Social and behaviour change interpersonal communication for promoting breastfeeding
The effectiveness of SBC‐IPC‐BF was examined by the highest number of reviews (Table 1). They especially focused on exclusive breastfeeding amongst 0‐ to 6‐month olds and on breastfeeding rate whereas only the most recent review examined early initiation of breastfeeding. One review looked at anthropometric nutritional status. Three reviews focused specifically on LMIC or developing countries (Bhutta et al., 2008; Gilmore & McAuliffe, 2013; Hall, 2011; Appendix S2). Ten of the 13 reviews included meta‐analyses.
The reviews focused on effectiveness of different modalities of interventions, such as settings, for example, community, households, and health system (Giugliani et al., 2015; Hall, 2011; Haroon et al., 2013; Sinha et al., 2015); delivery models, for example, group versus individual counselling (Bhutta et al., 2008; De Oliveira et al., 2001; Haroon et al., 2013) or face to face versus telephone (Renfrew et al., 2012); type of counsellor, for example, lay health workers, professional health workers, and peer support (Chapman et al., 2010; Gilmore & McAuliffe, 2013; Jolly et al., 2012; Lewin et al., 2010; Renfrew et al., 2012; Sudfeld et al., 2012); timing of counselling: antenatal and postnatal care (Chapman et al., 2010; De Oliveira et al., 2001; Jolly et al., 2012; Renfrew et al., 2012); and intensity of counselling (Chapman et al., 2010; De Oliveira et al., 2001; Gilmore & McAuliffe, 2013; Jolly et al., 2012; Appendix S2). Some reviews also studied the effect of interventions according to the background rate of breastfeeding (Renfrew et al., 2012) or formula feeding (Sudfeld et al., 2012), rural versus urban areas (Sinha et al., 2015), and income level of countries (Giugliani et al., 2015; Jolly et al., 2012; Sinha et al., 2015).
Overall, the majority of reviews for which methodological quality was available (10 out of 13) showed moderate quality (6 out of 10), whereas 3 showed high quality (Table 2). The main quality problem (for 7 out of 10) was the inadequacy of criteria for assessment of quality of primary studies, and the absence of assessment by two independent reviewers (Table 3).
Table 2.
Gap map analysis of availability, methodological qualitya and quality of evidenceb of reviews examining the effect of Infant and Young Child Feeding (IYCF) interventions on caretaker's IYCF awareness, knowledge and practices, and child's nutritional status
| IYCF practices | Nutritional status | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Early initiation of breast feeding | Exclusive breast feeding 0‐6 month olds | Breast feeding rate | Breast feeding duration | Re‐lactation | BMS consumption | Feeding frequency and diet diversity | Micro‐nutrient intakes | Ponderal growth | Linear growth | Micro‐nutrient status | |
| Social and behaviour change interpersonal communication for promoting breastfeeding | |||||||||||
| High quality of evidence |

|

|
|||||||||
| Moderate quality of evidence |

|

|
|||||||||
| Low quality of evidence |
|

|
|||||||||
| Unknown quality of evidence |

|

|

|

|

|

|
|||||
| Social and behaviour change interpersonal communication for promoting adequate complementary feeding | |||||||||||
| High quality of evidence | NA | NA | NA | NA | NA | NA |

|
||||
| Moderate quality of evidence | NA | NA | NA | NA | NA | NA |

|

|
|||
| Low quality of evidence | NA | NA | NA | NA | NA | NA | |||||
| Unknown quality of evidence | NA | NA | NA | NA | NA | NA |

|

|

|

|

|
| Social and behaviour change mass communication for promoting breastfeeding and adequate complementary feeding | |||||||||||
| High quality of evidence | |||||||||||
| Moderate quality of evidence | |||||||||||
| Low quality of evidence | |||||||||||
| Unknown quality of evidence |

|
||||||||||
| Provision of donated complementary food | |||||||||||
| High quality of evidence |

|
||||||||||
| Moderate quality of evidence |

|

|
|||||||||
| Low quality of evidence |

|

|
|||||||||
| Unknown quality of evidence |

|

|

|
||||||||
| Home fortification with multiple micronutrient supplementation | |||||||||||
| High quality of evidence | NA | NA | NA | NA | NA | NA | NA |
 c
c
|
|||
| Moderate quality of evidence | NA | NA | NA | NA | NA | NA | NA |

|

|
 c
c
|
|
| Low quality of evidence | NA | NA | NA | NA | NA | NA | NA | ||||
| Unknown quality of evidence | NA | NA | NA | NA | NA | NA | NA |

|
 c
c
|
||
| Capacity building | |||||||||||
| High quality of evidence |

|
||||||||||
| Moderate quality of evidence | |||||||||||
| Low quality of evidence | |||||||||||
| Unknown quality of evidence | |||||||||||
| Cash transfer, micro‐credit and vouchers | |||||||||||
| High quality of evidence | |||||||||||
| Moderate quality of evidence |

|

|

|
||||||||
| Low quality of evidence |

|

|

|

|
|||||||
| Unknown quality of evidence |

|

|
|||||||||
| Agricultural or fresh food supply interventions for diet diversification | |||||||||||
| High quality of evidence | NA | NA | NA | NA | NA | NA | |||||
| Moderate quality of evidence | NA | NA | NA | NA | NA | NA | |||||
| Low quality of evidence | NA | NA | NA | NA | NA | NA |

|

|

|

|
|
| Unknown quality of evidence | NA | NA | NA | NA | NA | NA |

|

|

|

|
|
 Weak quality review,
Weak quality review,  Moderate quality review,
Moderate quality review,  Strong quality review,
Strong quality review,  Unknown quality review,
Unknown quality review,  Size indicating 1 review,
Size indicating 1 review,  Size indicating 2 reviews,
Size indicating 2 reviews,  Size indicating 3 reviews
Size indicating 3 reviews
Methodological quality of review is reported as rated by health evidence (HealthEvidence, n.d.);
Quality of evidence is reported from the review, if available.
One review reported moderate, high and low quality of evidence for anaemia and haemoglobin status, iron deficiency, and iron status, respectively.
Table 3.
Number of reviews according to criteria of methodological quality
| Clearly focused PICO | Appropriate inclusion criteria of primary study | Comprehensive search strategy | Adequate duration of search strategy | Level of evidence of included studies clearly illustrated | Adequate quality assessment of included studies conducted | Quality assessment of included studies transparent | Appropriate combining of results across studies | Appropriate weighting of results across studies |
Author interpretation of results supported by data |
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ya | Nb | Uc | Y | N | U | Y | N | U | Y | N | U | Y | N | U | Y | N | U | Y | N | U | Y | N | U | Y | N | U | Y | N | U |
| Social and behaviour change interpersonal communication for promoting breastfeeding | |||||||||||||||||||||||||||||
| 10 | 0 | 3 | 9 | 1 | 3 | 4 | 6 | 3 | 10 | 0 | 3 | 10 | 0 | 3 | 3 | 7 | 3 | 2 | 8 | 3 | 10 | 0 | 3 | 7 | 3 | 3 | 7 | 3 | 3 |
| Social and behaviour change interpersonal communication for promoting adequate complementary feeding | |||||||||||||||||||||||||||||
| 2 | 0 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 2 | 1 | 1 | 2 | 0 | 2 | 2 | 1 | 1 | 2 | 2 | 0 | 2 | 0 | 0 | 2 | 2 | 0 | 2 |
| Social and behaviour change mass communication for promoting adequate breastfeeding and complementary feeding | |||||||||||||||||||||||||||||
| 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 |
| Provision of complementary food | |||||||||||||||||||||||||||||
| 4 | 0 | 2 | 4 | 0 | 2 | 2 | 2 | 2 | 4 | 0 | 2 | 3 | 1 | 2 | 2 | 2 | 3 | 1 | 3 | 2 | 4 | 0 | 2 | 1 | 0 | 2 | 4 | 0 | 2 |
| Home fortification with multiple micronutrient supplementation | |||||||||||||||||||||||||||||
| 1 | 0 | 2 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 0 | 2 |
| Capacity building | |||||||||||||||||||||||||||||
| 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
| Cash transfer and microcredit | |||||||||||||||||||||||||||||
| 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 |
| Agricultural or fresh food supply interventions for diet diversification | |||||||||||||||||||||||||||||
| 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 | 0 | 0 | 5 |
Note. PICO = population, intervention, comparison, and outcome.
Yes, criteria is present.
No, criteria is not present.
Unknown: Data not available.
For exclusive breastfeeding, 40% (4 out of 10) of the reviews was of moderate methodological quality, 30% (3 out of 10) was of high quality and quality was not reported for 30% (3 out of 10) of the reviews, whereas quality of evidence was not appraised for 60% (6 out of 10) of the reviews, was high for 20% (2 out of 10), and medium and low for 10% (1 of 10) of the reviews, respectively (Table 2).
For breastfeeding rate, 37% of the reviews (3 out of 8) was of medium methodological quality, 12% (1 of 8) was of weak and strong quality, respectively, and a quarter (2 out of 8) was of unknown quality. The majority of the reviews did not report on quality of evidence, although amongst the three with data available, one each reported high, medium, and low quality of evidence. The review looking at anthropometric nutritional status was of medium methodological quality and did not report on the quality of evidence. Ten of the 13 reviews included meta‐analyses.
Sixty‐one percent of the reviews had less than 25% of studies in common whereas 9% had more than 75% of studies in common (Table 4 and Appendix S2).
Table 4.
Proportion of reviews with overlapping primary studies
| < 25% of overlapping primary studies | 26–50% of overlapping primary studies | 51–75% of overlapping primary studies | >75% of overlapping primary studies | |
|---|---|---|---|---|
| Social and behaviour change interpersonal communication for promoting breastfeeding | 61% | 18% | 12% | 9% |
| Social and behaviour change interpersonal communication for promoting adequate complementary feeding | 8% | 34% | 50% | 8% |
| Provision of donated complementary food | 40% | 20% | 23% | 17% |
| Home fortification with multiple micronutrient supplementation | 33% | 50% | 17% | 0% |
| Cash transfer and microcredit | 70% | 5% | 15% | 10% |
| Agricultural or fresh food supply interventions for diet diversification | 17% | 66% | 17% | 0% |
3.2. Social and behaviour change interpersonal communication for promoting adequate complementary feeding
Four reviews looked at the effectiveness of SBC‐IPC‐CF (Table 1). They mainly explored the effect on nutritional status and all conducted meta‐analyses. Three of the four reviews targeted developing countries (Appendix S3). The reviews generally did not investigate the specificities of SBC‐IPC‐CF intervention delivery, but some reviews looked at the effectiveness of interventions according to food security contexts (Bhutta et al., 2008; Lassi et al., 2013).
Half of the reviews (2 out of 4) exploring effect of SBC‐IPC‐CF on nutritional status were of medium methodological quality, and the other half was of unknown quality (Table 2). The major quality problems were the lack of a comprehensive search strategy (2 out of 2) and of quality assessment of included studies (2 out of 2; Table 3 and Appendix S3). Half and a quarter of the reviews reported moderate and high quality of evidence, respectively, and the other quarter did not report on quality of evidence (Table 2). The majority of the reviews (58%) included in the SBC‐IPC‐CF analysis contained more than 50% of overlapping primary studies (Table 4 and Appendix S3).
3.3. Social and behaviour change mass communication for improving breastfeeding and adequate complementary feeding
Only one review of unknown methodological quality and quality of evidence studied the effectiveness of SBC‐MC on exclusive breastfeeding rate amongst 0‐ to 6‐month olds (Tables 1 and 2 and Appendix S4). Moreover, the evidence was extremely limited, with the review only identifying one single primary study (Bhutta et al., 2008).
3.4. Provision of donated complementary food
Six reviews looked at the effectiveness of provision of complementary foods (Table 1). They only explored the effect on nutritional status and all conducted meta‐analyses. All the reviews but one focused on developing countries or LMIC (Appendix S5). One review looked at the effect of the number of Kcalories provided, the location of feeding (day care, preschool, or feeding centre vs. home), and the level of supervision (Kristjanson et al., 2015). The other reviews did not look specifically at the effect of food distribution implementation factors nor at the type of food distributed, but all highlighted the heterogeneity of these parameters across studies. Moreover, most studies included in the reviews also involved a nutrition education component; therefore, the effect observed could not be only attributed to the provision of a food supplement.
A third of the reviews (2 of 6 reviews) were of medium, strong, and unknown methodological quality, respectively (Table 2). Inadequate (2 out of 4 reviews) and non‐transparent review (3 out of 4) of primary studies as well as absence of comprehensive search strategy (2 out of 4) was the major shortfalls for the reviews assessed (Table 3 and Appendix S5).
Two reviews reported medium quality of evidence whereas one review reported low and one reported high quality of evidence, and two further reviews did not report on this parameter at all (Table 2). The majority of the reviews (60%) looking at the provision of complementary food contained less than 50% of overlapping studies (Table 4).
3.5. Home fortification with multiple micronutrients powders
Three reviews of high (33%) and unknown (67%) methodological quality examined the effect of MNP on nutritional status (Tables 1 and 2). Two reviews did not report on quality of evidence whereas one reported moderate quality of evidence for anaemia and haemoglobin status, high quality of evidence for iron deficiency, and low quality of evidence for iron status. All conducted meta‐analyses. One review examined the effectiveness of MNP depending on settings with different prevalences of anaemia and malaria endemicity, length of intervention, and sex (De‐Regil et al., 2011; Appendix S6).
Most of them (83%) had less than 50% of primary studies in common (Table 4 and Appendix S6).
3.6. Capacity building
The only existing review studied the effect of health worker training on caretaker's feeding practices (Sunguya et al., 2013; Appendix S7). The methodological quality of the review was strong, and the review showed high quality of evidence (Table 2).
3.7. Cash transfers, microcredit, and vouchers
Five reviews investigated the effect of CT on different outcomes, mostly related to nutritional status, with only one examining effect on IYCF practices (Table 1). Three included meta‐analyses. Two reviews focused on LMIC (Bhutta et al., 2008; Lagarde et al., 2007), and one focused on humanitarian disasters (Pega et al., 2015; Appendix S8). One review investigated the effect of the amount of cash (Leroy et al., 2009), and two reviews investigated difference in effect on different age groups (Lagarde et al., 2007; Leroy et al., 2009).
Methodological quality of reviews was not available whereas quality of evidence was low and medium for two reviews each and not reported in one review (Table 2). Seventy percent of the reviews included less than 25% of common primary studies (Table 4 and Appendix S8).
3.8. Agricultural or fresh food supply interventions for increasing diet diversity
The four reviews examining agricultural programmes and fresh food distribution for diet diversification mainly investigated the effectiveness on nutritional status (Table 1). None of them included meta‐analyses.
The only review appraising quality of evidence reported low quality (Table 2). Appraisal of methodological quality was unavailable for all reviews. Only 17% of the reviews included more than 50% of common primary studies (Table 4 and Appendix S9).
3.9. Psychological support to caregivers
No study reviewed the effectiveness of psychological support to caregivers (Table 1).
4. DISCUSSION
4.1. Gaps in evidence
A number of reviews need to be conducted due to current lack of evidence. A review on the effectiveness of psychological support to mothers on IYCF practices and children's nutritional status is urgently needed and would be especially relevant for emergencies, where stress and trauma are widespread. Because staff capacity is generally low in these settings, looking at interventions dispensed by low‐skilled staff would be specifically relevant. Very little evidence also exists on the impact of SBC‐MC and of health staff capacity building. The lack of attention to these interventions might be because they are often embedded in larger IYCF interventions and might be difficult to investigate in isolation.
Except for SBC‐IPC‐BF, most of the reviews did not examine effects on IYCF practices. This is unfortunate because investigation of these intermediate outcomes between interventions and nutritional status would be fundamental to understand the mechanisms through which effectiveness can be achieved. New initiatives, such as Research on Food Assistance for Nutritional Impact (REFANI), have been recently set‐up in this direction to understand the pathway of action of provision of complementary food and of CT on nutritional status (Action against Hunger, n.d.).
Generally, few reviews examined the effect of intervention delivery models, patient characteristics, and contexts, with the exception of SBC‐IPC‐BF.
4.2. Major quality weaknesses
The majority of the reviews across all interventions did not report on the quality of evidence generated, which limited their utility for use by practitioners because the level of confidence in the results is not known.
Appraisal of methodological quality was available from HealthEvidence for around two‐third of the reviews. Knowing about quality of reviews is crucial for practitioners to judge reliability of results and therefore their potential use for improving interventions. Unfortunately, quality appraisal was not available from HealthEvidence for CT and agricultural or fresh food supply interventions. This might be because these are not health interventions, although they examined effectiveness on health and nutrition outcomes. It would be useful that the same mechanism as evaluation of reviews of health interventions be put in place for reviews of nonhealth interventions.
Amongst the reviews that were appraised for quality across all interventions, most were of moderate quality, showing that improvement in review methodology is needed. The major quality drawbacks were insufficiency in criteria set for assessment of quality of primary studies; assessment of primary studies conducted by one person, instead of two persons confronting their views; and lack of comprehensive search strategy. Those factors are fundamental for setting the basis of quality of reviews. Ensuring that all available studies are included in the review will ensure representativeness and inclusiveness, whereas quality of primary studies will greatly influence the quality of the overall evidence generated.
4.3. Overlapping studies
The same primary studies were included in several reviews. The more often a primary study was included in the reviews, the stronger its influence on the evidence generated by the whole reviews was. Moreover, studies with positive results have a greater tendency to be published than studies with neutral results, which might overestimate effectiveness of interventions (Easterbrook, Berlin, Gopalan, & Matthews, 1991). When examining the breadth of evidence from reviews about effectiveness of a specific intervention, overlap of primary studies should be taken into account. This would be especially crucial for the reviews with a substantial overlap of primary studies, such as SB‐IPC‐CF and provision of complementary food. Ideally, a review of reviews could be undertaken that would include all studies from previous reviews, relevant to the specific criteria of the review of reviews. This would allow avoiding over‐representation of some studies on the evidence.
4.4. Implications for policy and programming
A wealth of evidence from LMIC was identified for several interventions currently implemented in humanitarian emergencies. However, the implementation of these programmes might face additional difficulties in some emergency settings. For example, the barriers to breastfeeding that mothers often report, such as lack of proper food and stress (Save the Children, 2013), should be addressed by providing specific support. Moreover, implementing quality SBC‐IPC might be challenging due to impeded access, lack of skilled staff, and difficulties in carrying out training but could be overcome by developing innovative implementation models. In situations of food insecurity, which characterise a large proportion of humanitarian emergencies, a significant part of the population might not be able to afford nutrient‐dense food in sufficient quantity (Chastre & Lejeune, 2009), limiting the usefulness of SBC‐IPC‐CF. Specific delivery models of interventions that have not been investigated by the reviews included in this study, such as links with community‐based management of acute malnutrition (Norton et al., 2009), might also be especially relevant in emergencies.
4.5. Implications for monitoring of interventions
Huge gaps in monitoring and evaluation of IYCF programmes in emergencies hamper appropriate reporting and appraisal of programmes efficacy. Although standard indicators have been defined (WHO, 2010) their practical use in monitoring and evaluation has not been delineated. To our knowledge, there is no comprehensive guidance on monitoring and impact evaluation of IYCF‐E programmes and no set benchmark to estimate programme efficacy. Results of reviews and especially magnitude of potential impact generated by meta‐analyses should be more widely used to help determinate meaningful indicators and benchmarks to assess efficacy and impact of IYCF‐E programmes, taking into account factors that might play a role on effectiveness, such as children's age range, baseline level of breastfeeding initiation and BMS consumption, and urban versus rural settings.
4.6. Implication for research
Although reviews of existing evidence of effectiveness of IYCF interventions in LMIC can provide valuable guidance for designing programmes in emergencies, as described above, specific circumstances linked to emergencies might influence delivery models and their effectiveness. Moreover, IYCF‐E interventions are generally set in conjunction with interventions from different sectors, such as health, water, sanitation and hygiene, or food security. Implementation of concurrent interventions can be expected to reinforce the effectiveness of IYCF‐E interventions, but these interactions have seldom been studied. Research aimed at examining the pathways of actions of the interventions, the influence of contextual factors, and delivery models on the outcomes would be especially relevant. In addition, social forces and cultural and market factors also influence breastfeeding practices and the broader enabling environment needs to be considered (Glass & McAtee, 2006; Rollins et al., 2016). Exploring areas of legislation, policy, financing, and enforcement, would be essential to further understand factors of success. Despite the difficulties in conducting research in emergencies (Ager et al., 2014), generation of evidence in these specific contexts is crucial. Funding initiatives targeted at humanitarian emergencies, such as the Humanitarian Innovation Fund and the Research for Health in Humanitarian Crises, have been recently created (ELRHA, n.d.). However, no IYCF‐E research project has received funding yet, possibly due to absence of project submission, insufficient quality of projects submitted, or IYCF‐E not being seen as a priority area.
4.7. Limitations
First, although great efforts were made to construct the search terms to be inclusive of all possible definitions and vocabulary, bias may have been introduced in the search terminology used.
Second, only one person was able to assess the reviews for eligibility and extract the data, because of resource constraints. We were also not able to appraise the quality of the reviews included in this study, but we reported available quality rating from HealthEvidence. Quality rating was also available from Health Systems Evidence (Shea et al., 2007) using a score somewhat different from the score used by HealthEvidence. However, we choose to only use the rating by HealthEvidence for better comparison across reviews. Moreover, results of assessment of each criterion were available from HealthEvidence, which made possible the analysis of major quality drawbacks.
5. CONCLUSION
Some evidence has been found to exist about effectiveness of IYCF interventions in LMIC that can inform intervention programming and monitoring in emergencies amid the little evidence generated so far in these contexts. More studies should focus on the mechanisms and delivery models through which effectiveness of interventions can be achieved. This would enable to adjust programming according to contexts and maximise effectiveness. In addition, efforts should be renewed to generate evidence of effectiveness of IYCF interventions during humanitarian emergencies despite the challenges, in view of their potential to decrease morbidity and mortality.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
CP, PB, PH, AM, and JF conceived the study and wrote the protocol. CP conducted the literature searches and abstracted the data. CP analysed the data and wrote the first draft of the manuscript; all authors revised the draft and approved the final manuscript.
Supporting information
Data S1. Supplementary Appendix 1‐ Key words
Data S2. Supplementary Appendix 2: Evidence of effectiveness of social and behaviour change interventions for promoting breasfeeding on caretaker's Infant and Young Child Feeding awareness, knowledge and practices and on child's nutritional status
Data S3. Supplementary Appendix 3: Evidence of effectiveness of social and behaviour change interventions for promoting adequate complementary feeding on caretaker's infant and young child feeding awareness, knowledge and practices and on child's nutritional status
Data S4. Supplementary Appendix 4: Evidence of effectiveness of social and behaviour change mass communication on caretaker's infant and young child feeding awareness, knowledge and practices and on child's nutritional status
Data S5. Supplementary Appendix 5: Evidence of effectiveness of provision of donated complementary food on caretaker's infants and young child feeding awareness, knowledge and practices and on child's nutritional status
Data S6. Supplementary Appendix 6: Evidence of effectiveness of home‐fortification with micro‐nutrient powders on caretaker's infant and young child feeding awareness, knowledge and practices and on child's nutritional status
Data S7. Supplementary Appendix 7: Evidence of effectiveness of capacity building on caretaker's infant and young child feeding awareness, knowledge and practices and on child's nutritional status
Data S8. Supplementary Appendix 8: Evidence of effectiveness of cash transfer and micro‐credit interventions for increasing diet diversity on caretaker's infant and young child feeding awareness, knowledge and practices and on child's nutritional status
Data S9. Supplementary Appendix 9: Evidence of effectiveness of agricultural or fresh food supply interventions for increasing diet diversity on caretaker's infant and young children awareness, knowledge and practices and on child's nutritional status
ACKNOWLEDGMENT
We are very grateful to Andrew Hall for his comments on the study.
Prudhon C, Benelli P, Maclaine A, Harrigan P, Frize J. Informing infant and young child feeding programming in humanitarian emergencies: An evidence map of reviews including low and middle income countries. Matern Child Nutr. 2018;14:e12457 10.1111/mcn.12457
REFERENCES
- Action against Hunger (n.d.) REFANI‐research on food assistance for nutritional impact. Availabe at: http://www.actionagainsthunger.org/refani (Accessed 10 June 2016).
- Ager, A. , Burnham, G. , Checchi, F. , Gayer, M. , Grais, R. F. , Henkens, M. , … Spiegel, P. (2014). Strengthening the evidence base for health programming in humanitarian crises. Science, 345, 1290–1292. [DOI] [PubMed] [Google Scholar]
- Allen, C. (2014). A resource for those preparing for and responding to natural disasters, humanitarian crises, and major healthcare emergencies. Journal of Evidence‐Based Medicine, 7(4), 234–237. [DOI] [PubMed] [Google Scholar]
- Arvelo, W. , Kim, A. , Creek, T. , Legwaila, K. , Puhr, N. , Johnston, S. , … Bowen, A. (2010). Case‐control study to determine risk factors for diarrhea among children during a large outbreak in a country with a high prevalence of HIV infection. International Journal of Infectious Diseases, 14(11), e1002–e1007. [DOI] [PubMed] [Google Scholar]
- Bassani, D. G. , Arora, P. , Wazny, K. , Gaffey, M. F. , Lenters, L. , & Bhutta, Z. A. (2013). Financial incentives and coverage of child health interventions: A systematic review and meta‐analysis. BMC Public Health, 13(Suppl 3), S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berti, P. R. , Krasevec, J. , & FitzGerald, S. (2004). A review of the effectiveness of agriculture interventions in improving nutrition outcomes. Public Health Nutrition, 7(5), 599–609. [DOI] [PubMed] [Google Scholar]
- Bhutta, Z. A. , Ahmed, T. , Black, R. E. , Cousens, S. , Dewey, K. , Giugliani, E. , … Maternal and Child Undernutrition Study Group . (2008). What works? Interventions for maternal and child undernutrition and survival. Lancet, 371, 417–440. [DOI] [PubMed] [Google Scholar]
- Bhutta, Z. A. , Das, J. K. , Rizvi, A. , Gaffey, M. F. , Walker, N. , Horton, S. , … Black, R. E. (2013). Evidence‐based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet, 382, 452–477. [DOI] [PubMed] [Google Scholar]
- Black, R. E. , Victora, C. G. , Walker, S. P. , Bhutta, Z. A. , Christian, P. , de Onis, M. , … Maternal and Child Nutrition Study Group . (2013). Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet, 382, 427–451. [DOI] [PubMed] [Google Scholar]
- Blanchet, K. , Sistenich, V. , & Ramesh, A. (2015). An evidence review of research on health interventions in humanitarian crises. Available at: http://www.elrha.org/wp-content/uploads/2015/01/Evidence-Review-22.10.15.pdf (Accessed 9 June 2016).
- Chapman, D. J. , Morel, K. , Anderson, A. K. , Damio, G. , & Pérez‐Escamilla, R. (2010). Breastfeeding peer counseling: From efficacy through scale‐up. Journal of Human Lactation, 26(3), 314–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chastre, C. , & Lejeune, S. , (2009). The Minimum Cost of a Healthy Diet Findings from piloting a new methodology in four study locations. Available at: http://www.savethechildren.org.uk/resources/online-library/the-minimum-cost-of-a-healthy-diet (Accessed 10 June 2016).
- De Oliveira, M. I. , Camacho, L. A. , & Tedstone, A. E. (2001). Extending breastfeeding duration through primary care: A systematic review of prenatal and postnatal interventions. Journal of Human Lactation, 17(4), 326–343. [DOI] [PubMed] [Google Scholar]
- De‐Regil, L. , Suchdev, P. , Vist, G. , Wallester, S. , & Peña‐Rosas, J. P. (2011). Home fortification of foods with multiple micronutrient powders for health and nutrition in children under two years of age (Review). Cochrane Database of Systematic Reviews, 7(9), CD008959. [DOI] [PubMed] [Google Scholar]
- Dewey, K. G. , & Adu‐afarwuah, S. (2008). Review Article Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Maternal & Child Nutrition, 4, 24–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easterbrook, P. J. , Berlin, J. A. , Gopalan, R. , & Matthews, D. R. (1991). Publication bias in clinical research. Lancet, 337, 867–872. [DOI] [PubMed] [Google Scholar]
- ELRHA (n.d.) Humanitarian Innovation Fund. Available at http://www.elrha.org/ (Accessed 10 June 2016).
- Gibson, R. S. , & Anderson, V. P. (2009). A review of interventions based on dietary diversifica‐ tion or modification strategies with the potential to enhance intakes of total and absorbable zinc. Food and Nutrition Bulletin, 30(Suppl 1), S108–S143. [DOI] [PubMed] [Google Scholar]
- Gilmore, B. , & McAuliffe, E. (2013). Effectiveness of community health workers delivering preventive interventions for maternal and child health in low‐ and middle‐income countries: A systematic review. BMC Public Health, 13, 847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giugliani, E. R. J. , Horta, B. L. , Loret de Mola, C. , Lisboa, B. O. , & Victora, C. G. (2015). Effect of breastfeeding promotion interventions on child growth: a systematic review and meta‐analysis. Acta Paediatrica, 104(467), 20–29. [DOI] [PubMed] [Google Scholar]
- Glass, T. , & McAtee, M. (2006). Behavioral Science at the crossroads in public health: Extending the horizons, envirioning the future. Social Science and Medicine, 62, 1650–1671. [DOI] [PubMed] [Google Scholar]
- Global Nutrition Cluster . (2011). Harmonised Training Package. Available at http://nutritioncluster.net/trainings/. (Accessed 9 June 2016).
- Hall, J. (2011). Effective community‐based interventions to improve exclusive breast feeding at four to six months in low‐ and low‐middle‐income countries: A systematic review of randomised controlled trials. Midwifery, 27(4), 497–502. [DOI] [PubMed] [Google Scholar]
- Haroon, S. , Das, J. K. , Salam, R. A. , Imdad, A. , & Bhutta, Z. A. (2013). Breastfeeding promotion interventions and breastfeeding practices: A systematic review. BMC Public Health, 13(Suppl 3), S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HealthEvidence (n.d.) Quality assessment tool Available from: http://www.healthevidence.org/documents/our-appraisal tools/QATool&Dictionary_01Jun16.pdf. (Accessed 9 June 2016).
- Hipgrave, D. B. , Assefa, F. , Winoto, A. , & Sukotjo, S. (2012). Donated breast milk substitutes and incidence of diarrhoea among infants and young children after the May 2006 earthquake in Yogyakarta and Central Java. Public Health Nutrition, 15(2), 307–315. [DOI] [PubMed] [Google Scholar]
- Howe‐Heyman, A. , & Lutenbacher, M. (2016). The baby‐friendly hospital initiative as an intervention to improve breastfeeding rates: A review of the literature. Journal of Midwifery and Women's Health, 61(1), 77–102. [DOI] [PubMed] [Google Scholar]
- Imdad, A. , Yakoob, M. Y. , & Bhutta, Z. A. (2011). Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health, 11(Suppl 3), S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakobsen, M. , Sodemann, M. , Nylén, G. , Balé, C. , Nielsen, J. , Lisse, I. , & Aaby, P. (2003). Breastfeeding status as a predictor of mortality among refugee children in an emergency situation in Guinea‐Bissau. Journal of tropical medicine & international health, 8(11), 992–996. [DOI] [PubMed] [Google Scholar]
- Jolly, K. , Ingram, L. , Khan, K. S. , Deeks, J. J. , Freemantle, N. , & MacArthur, C. (2012). Systematic review of peer support for breastfeeding continuation: Metaregression analysis of the effect of setting, intensity, and timing. Bristich Medical Journal, 344, d8287. [DOI] [PubMed] [Google Scholar]
- Jones, G. , Steketee, R. W. , Black, R. E. , Bhutta, Z. A. , Morris, S. S. , & the Bellagio Child Survival Study Group . (2003). Child survival II How many child deaths can we prevent this year? Lancet, 362, 65–71. [DOI] [PubMed] [Google Scholar]
- Kristjansson, E. , Francis, D. , Benkhalti, J. M. , Welch, V. , Batal, M. , Greenhalgh, T. , … Petticrew, M. (2015). Food supplementation for improving the physical and psychosocial health of socio‐economically disadvantaged children aged three months to five years. Campbell Systematic Reviews, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagarde, M. , Haines, A. , & Palmer, N. (2007). Conditional cash transfers for improving uptake of health interventions. Journal of the American Medical Association, 298(16), 1900–1910. [DOI] [PubMed] [Google Scholar]
- Lagarde, M. , Haines, A. , & Palmer, N. (2009). The impact of conditional cash transfers on health outcomes and use of health services in low and middle income countries. Cochrane Database of Systematic Reviews, (Issue), 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassi, Z. S. , Das, J. K. , Zahid, G. , Imdad, A. , & Bhutta, Z. A. (2013). Impact of education and provision of complementary feeding on growth and morbidity in children less than 2 years of age in developing countries: A systematic review. BMC Public Health, 13(Suppl 3), S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leroy, J. L. , Ruel, M. , & Verhofstadt, E. (2009). The impact of conditional cash transfer programmes on child nutrition: A review of evidence using a programme theory framework. Journal of Development Effectiveness, 1(2), 103–129. [Google Scholar]
- Lewin, S. , Munabi‐Babigumira, S. , Glenton, C. , Daniels, K. , Bosch‐Capblanch, X. , van Wyk, B. E. , … Scheel, I. B. (2010). Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. The Cochrane Database of Systematic Reviews, 3, CD004015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masset, E. , Haddad, L. , Cornelius, A. , & Isaza‐Castro, J. (2012). Effectiveness of agricultural interventions that aim to improve nutritional status of children: Systematic review. British Medical Journal, 344, d8222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton R., Lhotska L, Wilkinson C., Deconinck H., Morrison P., Gribble K., et al. (2009). Integration of IYCF support into CMAM facilitator's guide Available at: http://www.ennonline.net/integrationiycfintocmam (Accessed 10 June 2016).
- OCHA . (2015). World humanitarian data and trends. Available at: http://www.unocha.org/data-and-trends-2015/. (Accessed 9 June 2016).
- Pega, F. , Sy, L. , Walter, S. , & Lhachimi, S. K. (2015). Unconditional cash transfers for assistance in humanitarian disasters: Effect on use of health services and health outcomes in low‐ and middle‐income countries (Review). Cochrane Database of Systematic Reviews, 9, CD011247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed, H. E. , Keely, C. B. , & Waldman, R. (2001). Understanding Mortality Patterns in Complex Humanitarian Emergencies In Reed H., & Keely C. (Eds.), Forced migration and mortality. Roundtable on the demography of forced migration, committee on population, commission on behavioral social sciences and education (pp. 1–37). . Wahington (DC): National Academies Press (US). [Google Scholar]
- Renfrew, M. J. , McCormick, F. M. , Wade, A. , Quinn, B. , & Dowswell, T. (2012). Support for healthy breastfeeding mothers with healthy term babies. The Cochrane Database of Systematic Reviews, 5, CD001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Requejo, J. , Victora, C. , & Bryce, J. (2015). A Decade of Tracking Progress for Maternal, Newborn and Child Survival. The 2015 Report. Available at: http://countdown2015mnch.org/documents/2015Report/CDReport_2015_ex-profiles_final.pdf (Accessed 9 June 2016). [DOI] [PMC free article] [PubMed]
- Rollins, N. C. , Bhandari, N. , Hajeebhoy, N. , Horton, S. , Lutter, C. K. , Martines, J. C. , … on behalf of The Lancet Breastfeeding Series Group . (2016). Why invest, and what it will take to improve breastfeeding practices? Lancet, 387, 491–504. [DOI] [PubMed] [Google Scholar]
- Salam, R. A. , MacPhail, C. , Das, J. K. , & Bhutta, Z. A. (2013). Effectiveness of micronutrient powders (MNP) in women and children. BMC Public Health, 13(Suppl 3), S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Save the Children . (2012). Infant and Young Child Feeding in Emergencies : why are we not delivering at scale ? A review of global gaps, challenges and ways forward. Available at: http://www.savethechildren.org.uk/resources/online-library/infant-and-young-child-feeding-emergencies-why-are-we-not-delivering-scale (Accessed 9 June 2016).
- Save the Children . (2013). Superfood for babies‐How overcoming barriers to breastfeeding will save children's lives. Available at: http://www.savethechildren.org/atf/cf/%7B9def2ebe-10ae-432c-9bd0-df91d2eba74a%7D/SUPERFOOD%20FOR%20BABIES%20ASIA%20LOW%20RES%282%29.PDF (Accessed 10 June 2016).
- Sguassero, Y. , de Onis, M. , Bonotti, A. M. , & Carroli, G. (2012). Community‐based supplementary feeding for promoting the growth of children under five years of age in low and middle income countries. Cochrane Database of Systematic Reviews, 6, CD005039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea, B. J. , Grimshaw, J. M. , Wells, G. A. , Boers, M. , Andersson, N. , Hamel, C. , … Bouter, L. M. (2007). Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology, 7, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha, B. , Chowdhury, R. , Sankar, M. J. , Martines, J. , Taneja, S. , Mazumder, S. , … Bhandari, N. (2015). Interventions to improve breastfeeding outcomes: A systematic review and meta‐analysis. Acta Paediatrica, 104(467), 114–134. [DOI] [PubMed] [Google Scholar]
- Snilstveit, B. , Vojtkova, M. , Bhavsar, A. , & Gaarder, M. (2013). Evidence Gap Maps: A Tool for Promoting Evidence‐Informed Policy and Prioritizing Future Research. Policy Research Working Paper 6725. Available at: https://openknowledge.worldbank.org/bitstream/handle/10986/16941/WPS6725.pdf (Accessed: 9 June 2016). [DOI] [PubMed]
- Sudfeld, C. R. , Fawzi, W. W. , & Lahariya, C. (2012). Peer support and exclusive breastfeeding duration in low and middle‐income countries: A systematic review and meta‐analysis. PloS One, 7(9), e45143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunguya, B. F. , Poudel, K. C. , Mlunde, L. B. , Shakya, P. , Urassa, D. P. , Jimba, M. , & Yasouka, J. (2013). Effectiveness of nutrition training of health workers toward improving caregivers' feeding practices for children aged six months to two years: A systematic review. Nutrition Journal, 12, 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Sphere Project . (2011). Humanitarian charter and minimum standards in humanitarian response. Available at: http://www.sphereproject.org/handbook/ (Accessed 9 June 2016).
- Turner, T. J. , Barnes, H. , Reid, J. , & Garrubba, M. (2010). Evidence for perinatal and child health care guidelines in crisis settings: Can Cochrane help? BMC Public Health, 10.1186/1471-2458-10-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora, C. G. , Bahl, R. , Barros, A. J. D. , França, G. V. , Horton, S. , Krasevec, J. , … for The Lancet Breastfeeding Series Group . (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet, 387, 475–490. [DOI] [PubMed] [Google Scholar]
- Webb, P. , Boyd, E. , Pee, S. , De Lenters, L. , Bloem, M. , & Schultink, W. (2014). Nutrition in emergencies: Do we know what works? Food Policy, 49, 33–40. [Google Scholar]
- WHO . (2010). Indicators for assessing infant and young child feeding practices. Part 1: Definitions . WHO: Geneva: Available at: http://www.who.int/maternal_child_adolescent/documents/9789241596664/en (Accessed 6 June 2016). [Google Scholar]
- WHO . (2015). Infant and young child feeding‐fact sheet No 342 Available at: http://who.int/mediacentre/factsheets/fs342/en/ (Accessed 9 June 2016).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supplementary Appendix 1‐ Key words
Data S2. Supplementary Appendix 2: Evidence of effectiveness of social and behaviour change interventions for promoting breasfeeding on caretaker's Infant and Young Child Feeding awareness, knowledge and practices and on child's nutritional status
Data S3. Supplementary Appendix 3: Evidence of effectiveness of social and behaviour change interventions for promoting adequate complementary feeding on caretaker's infant and young child feeding awareness, knowledge and practices and on child's nutritional status
Data S4. Supplementary Appendix 4: Evidence of effectiveness of social and behaviour change mass communication on caretaker's infant and young child feeding awareness, knowledge and practices and on child's nutritional status
Data S5. Supplementary Appendix 5: Evidence of effectiveness of provision of donated complementary food on caretaker's infants and young child feeding awareness, knowledge and practices and on child's nutritional status
Data S6. Supplementary Appendix 6: Evidence of effectiveness of home‐fortification with micro‐nutrient powders on caretaker's infant and young child feeding awareness, knowledge and practices and on child's nutritional status
Data S7. Supplementary Appendix 7: Evidence of effectiveness of capacity building on caretaker's infant and young child feeding awareness, knowledge and practices and on child's nutritional status
Data S8. Supplementary Appendix 8: Evidence of effectiveness of cash transfer and micro‐credit interventions for increasing diet diversity on caretaker's infant and young child feeding awareness, knowledge and practices and on child's nutritional status
Data S9. Supplementary Appendix 9: Evidence of effectiveness of agricultural or fresh food supply interventions for increasing diet diversity on caretaker's infant and young children awareness, knowledge and practices and on child's nutritional status



