Abstract
The objectives of this study were to estimate the age of complementary feeding introduction (CFI) and investigate the related health, demographic, and socio‐economic factors.
Analyses were based on 10,931 infants from the French national birth cohort ELFE, born in 2011. Health, demographic, and socio‐economic data concerning infants and parents were collected at birth (face‐to‐face interviews and medical records) and 2 months (telephone interviews). Data on milk feeding and CFI practices were collected at birth and 2 months then monthly from 3 to 10 months using online or paper questionnaires. The associations between both health and social factors and CFI age were tested by multivariable multinomial logistic regressions. The mean CFI age was 5.2 ± 1.2 months; 26% of the infants started complementary feeding before 4 months of age (CF < 4 months), 62% between 4 and 6 months of age, and 12% after 6 months of age (CF > 6 months). CF < 4 months was more likely when mothers smoked, were overweight/obese, younger (<29 years), and used their personal experience as an information source in child caregiving and when both parents were not born in France. CF < 4 months was less likely when the infant was a girl, second‐born, when the mother breastfed longer, and had attended at least one birth preparation class. Mothers of second‐born infants and who breastfed their child longer were more likely to introduce CF > 6 months. Couples in which fathers were born in France and mothers were not born in France were less likely to introduce CF > 6 months. CF < 4 months occurred in more than 25% of the cases. It is important to continue promoting clear CFI recommendations, especially in smoking, overweight, young, not born in France, and nonbreastfeeding mothers.
Keywords: birth cohort, caregiving, complementary feeding, food frequency questionnaire, infant feeding, socio‐economic factors
Abbreviations
- BMI:
Body mass index
- CF < 4 months:
Introduction to complementary foods before 4 months of age
- CF > 6 months:
Introduction to complementary foods after 6 months of age
- CF:
Complementary foods
- CFg:
Complementary feeding
- CFI:
Complementary feeding introduction
- ELFE:
Etude longitudinale française depuis l'enfance
- ESPGHAN:
European Society for Paediatric Gastroenterology, Hepatology and Nutrition
- PCU:
Per consumption unit
- PNNS:
French National Program for Nutrition and Health
- WA:
Weeks of amenorrhoea
- WHO:
World Health Organization
1. INTRODUCTION
Exclusive breastfeeding is recommended until 6 months of age by the World Health Organization (WHO, 2003). Then, the introduction of complementary foods (CF) to infants' diet at 6 months of age is recommended to meet their growing nutritional needs, with continued breastfeeding up to 2 years of age. For healthy term‐born infants living in Europe, the European Society for Paediatric Gastroenterology Hepatology and Nutrition recommends that CF be introduced after 17 weeks and no later than 26 weeks while the infant is still breastfeeding (Agostoni et al., 2008; M. Fewtrell et al., 2017). The 2005 French National Program for Nutrition and Health (PNNS) recommendations state that complementary feeding (CFg) should ideally be introduced at 6 months but should not start before 4 months (Nutrition group guides of the PNNS, 2005; Health comes with eating, 2005).
CFg introduction (CFI) may influence infants' nutritional status and has short‐ and long‐term effects on health, especially regarding growth, obesity, and allergies (M. Fewtrell et al., 2017; A. D. Jones et al., 2014; Michaelsen, Larnkjaer, Lauritzen, & Molgaard, 2010; Michaelsen, Larnkjaer, & Molgaard, 2013; Moss & Yeaton, 2014; Onyango, Borghi, de Onis, Casanovas, & Garza, 2014; Pearce & Langley‐Evans, 2013), although the association between the timing of CFg and childhood obesity remains controversial (Burdette, Whitaker, Hall, & Daniels, 2006; Moorcroft, Marshall, & McCormick, 2011). CFg practices are also likely to influence later eating behaviour (L. Jones et al., 2015; Nicklaus, 2016; Schwartz, Scholtens, Lalanne, Weenen, & Nicklaus, 2011). CFI and its associated factors have been little studied in France to date (Betoko et al., 2013; Boudet‐Berquier, Salanave, de Launay, & Castetbon, 2016).
In other developed countries, CFg has been shown to be initiated later (i.e., after the fifth month of life) when mothers breastfed their infant, were older, did not smoke, had a normal body weight, and had attained a higher education level or higher socio‐economic status (Kronborg, Foverskov, & Vaeth, 2014; Rebhan, Kohlhuber, Schwegler, Koletzko, & Fromme, 2009; Schiess et al., 2010; Scott, Binns, Graham, & Oddy, 2009; Wen, Kong, Eiden, Sharma, & Xie, 2014; Wijndaele, Lakshman, Landsbaugh, Ong, & Ogilvie, 2009). However, there has been little research on the associations of paternal characteristics with the timing of CFI (Betoko et al., 2013; Camara et al., 2015; Gross et al., 2010).
The present study aims to first describe the age at CFI in a French birth cohort and then assess the factors associated with infant age at CFI, including health, demographic, and socio‐economic factors in addition to caregiving practices.
Key messages.
Most of the infants (62%) received their first CF between 4 and 6 months of age, 26% received CF<4 months, and 12% beyond 6 months.
Mothers who smoked during pregnancy were overweight/obese, were younger, were born outside France, and were more likely to introduce CF<4 months.
Mothers of girl, those of a second‐born infant, who attended at least one birth preparation class and breastfed longer, were less likely to introduce CF<4 months; breastfeeding duration was positively related to CFI>6 months.
It is important to continue promoting clear CF recommendations, especially to families more likely to introduce CF<4 months.
2. MATERIAL AND METHODS
2.1. Study population
The present analysis was based on data from the Etude longitudinale française depuis l'enfance (ELFE) study, a nationally representative birth cohort study that included 18,258 children born in a random sample of 349 maternity units in France in 2011 (Vandentorren et al., 2009). All infants who were born in the 320 maternity units that agreed to participate, on the 25 selected recruitment days over the four seasons, and met the inclusion criteria, were included. The inclusion criteria were as follows: children born after 33 weeks of amenorrhoea; mothers aged ≥18 years who were not planning to move outside Metropolitan France in the next 3 years; and mothers able to read French, Arabic, Turkish, or English, the most common languages spoken by women giving birth in France.
The ELFE study received approval from the Consultative Committee for the Treatment of Information for Health Research (Comité Consultatif sur le Traitement des Informations pour la Recherche en Santé), the national data protection authority (Commission Nationale Informatique et Libertés), and the National Statistics Council.
Each mother had to sign consent for herself and her child. If fathers were present on the inclusion days, they also provided consent; if not, they were informed about the right to oppose their child's participation. Fifty‐one percent of the contacted parents agreed to their child's participation. Data were collected in standardized interviews conducted by trained interviewers and by self‐completed questionnaires, previously tested in a pilot study (Vandentorren et al., 2009).
Each mother was interviewed face‐to‐face at the maternity ward for medical information regarding her pregnancy, her newborn, and her general characteristics. Additional information was provided by medical records from the obstetric and paediatric files. Two months post‐partum, telephone interviews were conducted with mothers and fathers to assess the following: demographic and socio‐economic variables (country of birth, number of family members, educational level, employment, and monthly income); health variables of both infants and parents; and milk feeding practices during the first 2 months.
2.2. Milk and CFg information collection
Information regarding milk feeding practices was collected prospectively as described elsewhere (Wagner et al., 2015). The infant's age at breastfeeding cessation was collected during the 1‐year follow‐up. Breastfeeding duration up to 12 months was considered, as a continuous variable, expressed in months. Therefore, when the term “breastfed longer” is used here, it refers to a characteristic positively associated with breastfeeding duration. Infants' CF consumption was collected monthly from 3 to 10 months post‐partum, using an online or paper self‐reported questionnaire. This questionnaire consisted of 26 food items (fruit juices, other sweetened beverages, regular cow's milk, semi‐skimmed or skimmed cow milk, infant cereals, potatoes, green beans, carrots, peas, artichokes, other vegetables, pasta/rice, bread, meat, fish, egg yolks, egg whites, cheese, yogurt, apples, bananas, strawberries, peaches, other fruits, biscuits, and other desserts). The frequency of their consumption during the last month was recorded on a 5‐point scale: not yet introduced (0), introduced once (1), several times (2), often (3), and every day or almost every day (4). The food items were chosen to reflect the variety of the infant diet during CFg, especially fruits and vegetables, which are traditionally the first food groups provided to infants in France at CFI (Betoko et al., 2013; Lange et al., 2013), and to focus on nutritional recommendations. An imputation method for missing data was applied, as described in Data S1.
2.3. Definition of age at CFg initiation
Based on the above questionnaire, age at CFI was defined as the age at the month of the first introduction of any food other than water, breast milk, or baby formula that occurred more than once (i.e., Levels 2, 3, or 4 of the consumption frequency scale). This definition prevented us from considering the occasional consumption of a given food (Boudet‐Berquier et al., 2016; Lange et al., 2013; Salanave, deLaunay, Boudet‐Berquier, Guerrisi, & Castetbon, 2016) as CFI. The age at CFI was categorized as follows: during the third and fourth months of life (CF < 4 months); between 4 and 6 months of age, that is, during the fifth month and the sixth month of life; and strictly after 6 months of age (CF > 6 months), that is, from the first day of the seventh month onwards.
2.4. Infant and parental characteristics
All variables and their modalities are briefly described in Table 1 and further detailed in Data S2 .
Table 1.
Studied characteristics and their modalities
| Characteristics | Modalities |
|---|---|
| Infant's characteristics | |
| Sex | Boy; girl |
| Birth rank | First‐born; second‐born; third‐born; or more‐born |
| Twin birth | Yes; no |
| Gestational age, weeks of amenorrhea (WA) | 33–37; 37–39; ≥40 |
| Birthweight (grams) | <2,500; 2,500–3,999; ≥4,000 |
| Milk protein allergy | Yes; no |
| Self‐reported family history of allergy | Yes; no |
| Maternal health characteristics | |
| Mode of delivery | Vaginal; caesarean |
| Post‐partum smoking | Yes; no |
| Self‐reported prepregnancy BMI | <18.5: lean; 18.5–24.9: normal; 25–29.9: overweight; ≥30: obese |
| Number of birth preparation classes attended for this pregnancy | 0; 1–5; ≥6 |
| Edinburgh postnatal depression scale score | Continuous variable from 0 to 30. The higher the score, the higher the probability of post‐partum depressiona |
| Maternal demographic and socio‐economic characteristics | |
| Maternal age at delivery (years) | <25; 25–29; 30–34; ≥35 |
| Maternal education level (years) | ≤9; 10–12; >12 |
| Maternal occupation type | None or student; farmer or craftswoman; executive; intermediate worker; manual worker; office employee |
| Maternal employment status when the infant was 2 months old | Employed; independent; unemployed |
| Paternal demographic and socio‐economic characteristics | |
| Paternal age (years) | <27; 27–31; 32–36; ≥37 |
| Paternal occupation type | None or student; farmer or craftsman; executive; intermediate worker; manual worker; office employee |
| Household characteristics | |
| Marital status | Single mother; married or civil union; or living together |
| Monthly family income per consumption unit (PCU; euros) | <600; 600–1,099; 1,100–1,799; 1,800–2,999; ≥3,000 |
| Parental country of birth | Both born in France; mother not born in France and father born in France; mother born in France and father not born in France; both not born in France |
| Familial feeding habits | |
| Duration of any breastfeeding Continuous variable expressed in months | Included exclusive (no food given other than breast milk and rehydration solutions); predominant (no milk other than breast milk, but water and baby teas were allowed); or partial (infant formula given in addition to breast milk) |
| Reasons for feeding choice at birth | Health or welfare of the child; convenience; relationship with the child; medical advice or contraindication; usual choice of relatives |
| Maternal concerns about child's health | No concerns; feeding issues; other issues |
| Maternal reaction when the child did not eat much at 2 months of life | “Did not insist”; “insisted or tried later”; “never happened” |
| Familial caregiving practices | |
| Father's presence at delivery | Yes; no |
| Mother's use of personal experience in child caregiving as care information sourceb | Yes; no |
| Anticipated infant care arrangements for when the mother returned to work | Mother only; family only (father or someone else); home nurse mainly; nursery only; nanny only; others only; at least two caregivers other than the mother and home nurse |
| Distribution of home duties between parents | Equal; unequal, more on the mother; unequal, more on the father |
| Distribution of care duties between parents | Quite equal; unequal, more on the mother; equal or a greater participation of the father |
| Variables of adjustment | |
| Season of inclusion | 25 recruiting days were selected to represent each season: from April 1 to April 4; from June 27 to July 4; from September 27 to October 4; from November 28 to December 5 |
| Maternity unit size | Number of birth each year: 145–699; 700–1,009; 1,010–1,418; 1,422–2,187; 2,197–5,215 |
| Residential region | East‐Parisian Basin; west‐Parisian Basin; Parisian region; east; Mediterranean region; north; west; south‐east; south‐west |
Note. BMI = body mass index.
Murray L, Carothers AD. The validation of the Edinburgh Post‐natal Depression Scale on a community sample. British Journal of Psychiatry. 1990;157(2):288–290.doi:http://dx.doi.org/10.1192/bjp.157.2.288.
Different sources of information were also explored, only this variable was used in this study (see Data S2 ).
2.5. Sample selection
Of the 18,258 initially included infants, 17,579 were eligible (Figure 1). We then excluded infants with very little or no information (n = 5,654) regarding CFg, leading to a sample of 11,925 infants. The age of CFI could be calculated for 9,427 of them without imputation; the imputation process led to a final sample of 10,931 infants.
Figure 1.
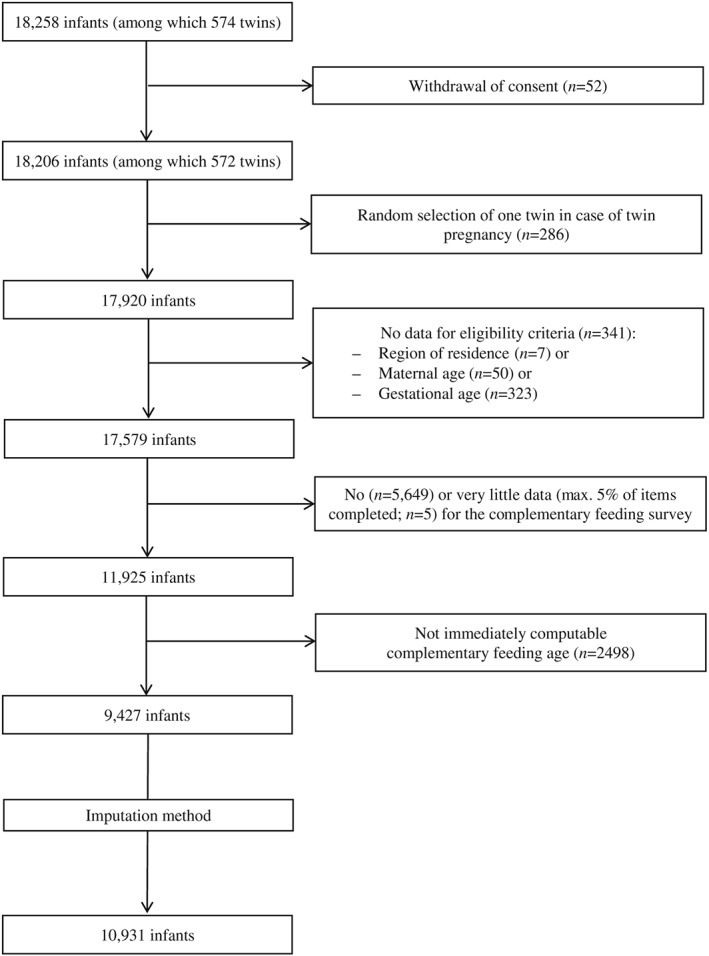
Flow chart of selection of analysis population (complementary feeding age)
2.6. Statistical analyses
To provide statistics representative of all French infants born in 2011, we weighted data related to age at CFI to account for the sample design, nonparticipation at inclusion, and specific nonresponse to the infant feeding questionnaire. The weighting also included calibration on margins from the state register's statistical data and the 2010 French National Perinatal study (Blondel, Lelong, Kermarrec, Goffinet, & National Coordination Group of the National Perinatal, 2012) for the following variables: age, region, marital status, migration status, level of education, and parity. The weighting method was used according to procedures recommended by the French National Institute of Statistics and Economic Studies (INSEE; Caron, 2005; Sautory, 1991). Further information on both the survey carried out at the maternity ward and the CFg data can be found online (in French) on the ELFE data access platform (https://pandora.vjf.inserm.fr/doc/ELFE_NoteDet0.pdf and https://pandora.vjf.inserm.fr/doc/PonderationSicomiam.pdf, respectively). Details on the weighting methods for the infant feeding questionnaire have been translated into English and can be provided on request.
The associations between age at CFI and the potential factors listed in Table 1 were assessed by multinomial logistic regressions on unweighted variables. The association of each variable with age at CFI was first tested in bivariate models; then, factors with a significance level of p < .01 (to account for population size) were included in the multivariable model that adjusted for maternity unit size, season of inclusion, and region of residence. In the multivariable model, the significance level was set at p < .01. All analyses were performed using SAS 9.3 (SAS, Cary, NC). Multicollinearity was assessed by checking that the variance inflation factor was below 5 (Allison, 1999).
3. RESULTS
3.1. Characteristics of the study population
The characteristics of the study population, as well as those of the participants who did not report any information about CFg, are described in Table 2 . Mothers of included participants were older, more educated, more likely to hold an intermediate or executive occupation, to have been born in France, and to have a normal body mass index (BMI) and less likely to be single mothers and to smoke after birth than those excluded from the analysis. Included mothers breastfed for a longer duration than nonincluded ones, that is, 3.5 months on average for any breastfeeding.
Table 2.
Characteristics of the study population (with and without data on complementary feeding introduction age)
| N (%) | ||||
|---|---|---|---|---|
| Characteristics | All | Infants with CFI age: included participants | Infants without CFI age: excluded from the analysis | p valuea |
| All | 17,579 | 10,931 | 6,648 | |
| Child characteristics | ||||
| Sex | .37 | |||
| Girl | 8,540 (48.58) | 5,340 (48.85) | 3,200 (48.15) | |
| Boy | 9,037 (51.41) | 5,591 (51.15) | 3,446 (51.85) | |
| Birth rank | <.0001 | |||
| 1st | 7,800 (44.37) | 5,033 (46.04) | 2,767 (41.68) | |
| 2nd | 6,278 (35.71) | 4,052 (37.07) | 2,226 (33.53) | |
| ≥3 | 3,492 (19.86) | 1,846 (16.89) | 1,646 (24.79) | |
| Twin birth | <.0001 | |||
| No | 17,302 (98.42) | 10,795 (98.76) | 6.507 (97.88) | |
| Yes | 277 (1.58) | 136 (1.24) | 141 (2.12) | |
| Gestational age (weeks of amenorrhea) | <.0001 | |||
| 33–37 | 872 (4.96) | 468 (4.28) | 404 (6.08) | |
| 37–39 | 8,544 (48.60) | 5,153 (47.14) | 3,391 (51.01) | |
| ≥40 | 8,163 (46.44) | 5,310 (48.58) | 2,853 (42.92) | |
| Birth weight (grams) | <.0001 | |||
| <2,500 | 789 (4.49) | 407 (3.77) | 382 (5.82) | |
| 2,500–3,999 | 15,260 (86.81) | 9,534 (88.27) | 5,726 (87.21) | |
| ≥4,000 | 1,318 (7.50) | 860 (7.96) | 458 (6.98) | |
| Cow's milk protein allergy | ||||
| Yes | 217 (1.40) | 141 (1.32) | 76 (1.60) | .18 |
| No | 15,257 (98.60) | 10,570 (98.68) | 4,687 (98.40) | |
| Maternal characteristics | ||||
| Mode of delivery | .0109 | |||
| Vaginal | 14,154 (80.52) | 8,860 (82.44) | 5,294 (80.90) | |
| Caesarean | 3,137 (17.85) | 1,887 (17.56) | 1,250 (19.10) | |
| Postnatal smoking | <.0001 | |||
| Yes | 3,129 (17.80) | 1,769 (16.59) | 1,360 (29.53) | |
| No | 12,139 (69.05) | 8,893 (83.41) | 3,246 (70.47) | |
| Prepregnancy BMI (kg/m2) | <.0001 | |||
| <18.5 | 1,359 (7.73) | 769 (7.11) | 590 (9.08) | |
| 18.5–24.9 | 11,191 (63.66) | 7,271 (67.18) | 3,920 (60.34) | |
| 25–29.9 | 3,039 (17.29) | 1,802 (16.65) | 1,237 (19.04) | |
| ≥30 | 1,730 (9.84) | 981 (9.06) | 749 (11.53) | |
| Age (years) | <.0001 | |||
| <25 | 2,141 (12.18) | 843 (7.71) | 1,298 (19.52) | |
| 25–29 | 5,479 (31.17) | 3,382 (30.94) | 2,097 (31.54) | |
| 30–34 | 6,190 (35.21) | 4,301 (39.35) | 1,889 (28.41) | |
| ≥35 | 3,769 (21.44) | 2,405 (22) | 1,364 (20.52) | |
| Education level (years) | <.0001 | |||
| ≤9 | 3,325 (18.91) | 1,195 (10.96) | 2,130 (32.16) | |
| 10–12 | 3,672 (20.89) | 1,876 (17.21) | 1,796 (27.11) | |
| ≥12 | 10,530 (59.90) | 7,832 (71.83) | 2,698 (40.73) | |
| Occupation type | <.0001 | |||
| No occupation/student | 499 (2.84) | 157 (1.44) | 342 (5.72) | |
| Farmer/craftswoman | 653 (3.71) | 394 (3.62) | 259 (4.33) | |
| Executive | 2,941 (16.73) | 2,308 (21.22) | 633 (10.59) | |
| Intermediate | 3,876 (22.05) | 2,882 (26.49) | 994 (16.62) | |
| Manual worker | 608 (3.46) | 271 (2.49) | 337 (5.64) | |
| Office employee | 8,282 (47.11) | 4,867 (44.74) | 3,415 (57.11) | |
| Employement status | ||||
| Employed | 10,894 (67.08) | 8,059 (74.74) | 2,835 (50.70) | <.0001 |
| Unemployed | 4,790 (29.2) | 2,219 (20.58) | 2,571 (45.98) | |
| Independent | 690 (4.21) | 504 (4.67) | 186 (3.33) | |
| Paternal characteristics | ||||
| Age (years) | <.0001 | |||
| <27 | 2,141 (12.18) | 1,012 (9.36) | 1,129 (17.88) | |
| 27–31 | 5,257 (29.91) | 3,393 (31.37) | 1,864 (29.52) | |
| 32–36 | 5,191 (29.53) | 3,596 (33.24) | 1,595 (25.26) | |
| ≥37 | 4,542 (25.84) | 2,816 (26.03) | 1,726 (27.34) | |
| Occupation type | <.0001 | |||
| No occupation/student | 156 (0.93) | 64 (0.60) | 92 (1.53) | |
| Farmer/craftswoman | 1,837 (10.95) | 1,120 (10.42) | 717 (11.92) | |
| Executive | 3,693 (22.02) | 2,866 (26.66) | 827 (13.74) | |
| Intermediate | 2,222 (13.25) | 1,647 (15.32) | 575 (9.56) | |
| Manual worker | 2,457 (14.65) | 1,226 (11.40) | 1,231 (20.46) | |
| Office employee | 6,404 (38.19) | 3,829 (35.61) | 2,575 (42.80) | |
| Household characteristics | ||||
| Marital status when the child is 2months | <.0001 | |||
| Single mother | 735 (4.18) | 244 (2.27) | 491 (9.57) | |
| Married/civil union/living together | 15,124 (86.03) | 10,487 (97.73) | 4,637 (90.43) | |
| Monthly income per consumption unit (euros) | <.0001 | |||
| <600 | 776 (4.41) | 265 (2.54) | 511 (11.23) | |
| 600–1,099 | 2,713 (15.43) | 1,409 (13.50) | 1,304 (28.65) | |
| 1,100–1,799 | 6,840 (38.91) | 4,949 (47.40) | 1,891 (41.54) | |
| 1,800–2999 | 3,890 (22.13) | 3,196 (30.61) | 694 (15.25) | |
| ≥3,000 | 773 (4.40) | 621 (5.95) | 152 (3.34) | |
| Parental country of birth | <.0001 | |||
| Mother and father France | 13,776 (78.37) | 9,410 (86.85) | 4,366 (68.11) | |
| Mother abroad and father France | 983 (5.59) | 504 (4.65) | 479 (7.47) | |
| Mother France and father abroad | 1,219 (6.93) | 591 (5.45) | 628 (9.80) | |
| Mother and father abroad | 1,267 (7.21) | 330 (3.05) | 937 (14.62) | |
| Familial caregiving characteristics | ||||
| Father's presence at delivery | <.0001 | |||
| Yes | 14,228 (80.94) | 9,320 (86.35) | 4,908 (75.14) | |
| No | 3,097 (17.62) | 1,473 (13.65) | 1,624 (24.86) | |
| Maternal feeding practices | ||||
| Breastfeeding duration (exclusive or not, months) | ||||
| N | 17,569 | 10,931 | 6,638 | <.0001 b |
| mean ± SD | 3.15 ± 3.83 | 3.53 ± 4.07 | 2.52 ± 3.29 | |
Note. CFI = complementary feeding introduction; BMI = body mass index. In bold: significant modality (p < .01).
Based on Χ2 test, comparing infants with CFI age and without CFI age.
Based on t test, comparing infants with CFI age and without CFI age.
In bold: significant modality (p < .01).
3.2. Age at CFI
All but three infants had received CF at 10 months of age, the end of the follow‐up period. The mean age at CFI was 5.2 ± 1.2 months (median, 5 months; interquartile range 1–3, 4–6 months), and 26% of the children were introduced to CF before 4 months of age, 62% between 4 and 6 months of age, and 12% to after 6 months. Eleven percent were introduced to CF at 6 months of age.
3.2.1. Factors associated with CF introduction
Some factors were not significant in the bivariate analyses and are not reported further: twin birth, gestational age, birthweight, milk protein allergy, Edinburgh Postnatal Depression Scale, and distribution of care duties between parents. The results of the bivariate analyses for the significant variables are presented in Table S1 and described in Data S3 .
3.2.2. Multivariable analysis
Some factors were not significant in the multivariable analyses: mode of delivery, family history of allergy, maternal employment status and occupation type, paternal age and occupation type, marital status, father's presence at delivery, distribution of home duties between parents, infant care arrangements, reasons for feeding choice at birth, and maternal concerns about the child's health (Table 2). The R 2 of the multinomial multivariable model was 0.1477. This model was significantly different from the empty model.
3.2.3. Factors associated with CFI before 4 months of age
After adjustment for all of the factors listed in Table 3, smoking mothers after birth were more likely to introduce CF before 4 months than those who did not smoke. Self‐reported overweight or obese mothers (before pregnancy) were more likely to introduce CF before 4 months than those with a normal BMI. No association was found between a prepregnancy maternal BMI under 18.5 kg/m2 and CF < 4 months. The youngest mothers, under 29 years old, were more likely to introduce CF before 4 months than mothers aged 30–34 years. Mothers who reported using their personal experience as an information source in child caregiving were more likely to introduce CF before 4 months than mothers who did not use this information source. Furthermore, couples in which neither parent was born in France were more likely to introduce CF before 4 months compared to couples in which both parents were born in France. Maternal education level was significantly associated with age at CFI, with a large effect in bivariate analysis but a less marked effect in multivariate analysis, related to a marginally significant modality: Mothers who attended less than 9 years of school tended to be more likely to introduce CF before 4 months.
Table 3.
Health, demographic, and socio‐economic characteristics associated with the age of initiation of complementary feeding N = 10,931
| N | Multivariable analysis | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| <4 months | 4–6 months | >6 months | <4 months | >6 months | ||||||
| Total N | 2,336 | 7,117 | 1,478 | p of the variable | p a | OR | 99% CI | p* | OR | 99% CI |
| Health characteristics | ||||||||||
| Infant | ||||||||||
| Sex | <.0001 | |||||||||
| Girl | 1,044 | 3,531 | 765 | <.0001 | 0.78 | 0.69–0.89 | .04 | 1.13 | 0.97–1.32 | |
| Boy | 1,292 | 3,586 | 713 | Reference | Reference | |||||
| Birth rank | <.0001 | |||||||||
| 1st | 1,114 | 3,370 | 549 | Reference | Reference | |||||
| 2nd | 760 | 2,661 | 631 | .006 | 0.78 | 0.65–0.94 | .004 | 1.28 | 1.03–1.59 | |
| ≥3 | 462 | 1,086 | 298 | .45 | 1.08 | 0.84–1.38 | .012 | 1.32 | 0.99–1.76 | |
| Birth | ||||||||||
| Mode of delivery | .77 | |||||||||
| Vaginal | 1,837 | 5,784 | 1,239 | Reference | Reference | |||||
| Caesarean | 463 | 1,213 | 211 | .39 | 1.07 | 0.88–1.30 | .73 | 0.97 | 0.76–1.24 | |
| Maternal | ||||||||||
| Post‐partum smoking | <.0001 | |||||||||
| Yes | 575 | 1,054 | 140 | <.0001 | 1.32 | 1.11–1.56 | .06 | 0.83 | 0.64–1.07 | |
| No | 1,673 | 5,908 | 1,312 | Reference | Reference | |||||
| Prepregnancy BMI (kg/m2) | <.0001 | |||||||||
| <18.5 | 137 | 506 | 126 | .04 | 0.80 | 0.61–1.06 | .04 | 1.26 | 0.95–1.67 | |
| 18.5–24.99 | 1,398 | 4,842 | 1,031 | Reference | Reference | |||||
| 25–29.99 | 476 | 1,112 | 214 | .002 | 1.24 | 1.04–1.47 | .77 | 1.03 | 0.82–1.28 | |
| ≥30 | 307 | 581 | 93 | .005 | 1.27 | 1.02–1.58 | .46 | 0.91 | 0.67–1.25 | |
| Number of birth preparation classes attended | <.0001 | |||||||||
| 0 | 1,067 | 2,205 | 463 | Reference | Reference | |||||
| 1–5 | 455 | 1,556 | 336 | .0008 | 0.78 | 0.64–0.94 | .39 | 0.93 | 0.74–1.16 | |
| ≥6 | 740 | 3,130 | 629 | <.0001 | 0.67 | 0.56–0.81 | .14 | 0.88 | 0.71–1.09 | |
| Familial health characteristics | ||||||||||
| Family history of allergy | .36 | |||||||||
| Yes | 955 | 2,906 | 673 | Reference | Reference | |||||
| No | 1,342 | 4,141 | 793 | .15 | 0.93 | 0.81–1.06 | .12 | 0.91 | 0.78–1.06 | |
| Demographic and socio‐economic characteristics | ||||||||||
| Maternal | ||||||||||
| Age (years) | <.0001 | |||||||||
| <25 | 350 | 444 | 49 | <.0001 | 1.76 | 1.33–2.35 | .11 | 0.74 | 0.45–1.20 | |
| 25–29 | 809 | 2,216 | 357 | .002 | 1.24 | 1.04–1.47 | .04 | 0.84 | 0.68–1.05 | |
| 30–34 | 757 | 2,859 | 686 | Reference | Reference | |||||
| ≥35 | 420 | 1,598 | 387 | .11 | 0.88 | 0.72–1.08 | .58 | 0.96 | 0.77–1.18 | |
| Education level (years) | .002 | |||||||||
| ≤9 | 457 | 659 | 79 | .01 | 1.25 | 1.00–1.56 | .02 | 0.71 | 0.49–1.02 | |
| 10–12 | 549 | 1,150 | 177 | .47 | 1.06 | 0.88–1.27 | .29 | 0.90 | 0.69–1.16 | |
| ≥12 | 1,327 | 5,289 | 1,216 | Reference | ||||||
| Occupation type | .03 | |||||||||
| No occupation/student | 67 | 76 | 14 | .37 | 1.19 | 0.72–1.97 | .27 | 1.42 | 0.62–3.27 | |
| Farmer/craftswoman | 92 | 248 | 54 | .25 | 1.19 | 0.80–1.76 | .20 | 1.27 | 0.78–2.04 | |
| Executive | 305 | 1,593 | 410 | .03 | 0.82 | 0.65–1.04 | .09 | 1.17 | 0.92–1.49 | |
| Intermediate | 469 | 1,946 | 467 | .02 | 0.85 | 0.71–1.02 | .03 | 1.19 | 0.97–1.47 | |
| Manual worker | 96 | 145 | 30 | .94 | 1.01 | 0.69–1.48 | .06 | 1.51 | 0.86–2.66 | |
| Office employee | 1,286 | 3,084 | 497 | Reference | Reference | |||||
| Employment status | .04 | |||||||||
| Employed | 1,521 | 5,390 | 1,148 | Reference | Reference | |||||
| Unemployed | 690 | 1,290 | 239 | .005 | 1.21 | 1.02–1.45 | .44 | 0.93 | 0.74–1.18 | |
| Independent | 78 | 350 | 76 | .21 | 0.83 | 0.56–1.22 | .57 | 0.92 | 0.62–1.36 | |
| Paternal | ||||||||||
| Age (years) | .40 | |||||||||
| <27 | 341 | 586 | 85 | .63 | 1.05 | 0.80–1.38 | .40 | 1.14 | 0.77–1.67 | |
| 27–31 | 756 | 2,258 | 379 | .91 | 1.00 | 0.84–1.21 | .06 | 0.86 | 0.69–1.06 | |
| 32–36 | 645 | 2,374 | 577 | Reference | Reference | |||||
| ≥37 | 550 | 1,840 | 426 | .53 | 1.05 | 0.86–1.27 | .54 | 0.95 | 0.77–1.17 | |
| Occupation type | .05 | |||||||||
| No occupation/student | 12 | 48 | 4 | .005 | 0.36 | 0.14–0.92 | .11 | 0.42 | 0.11–1.68 | |
| Farmer/craftsman | 234 | 742 | 144 | .49 | .94 | 0.74–1.19 | .51 | 0.93 | 0.70–1.24 | |
| Executive | 417 | 1,937 | 512 | .59 | 0.96 | 0.78–1.18 | .51 | 1.06 | 0.85–1.32 | |
| Intermediate | 280 | 1,138 | 229 | .18 | 0.89 | 0.72–1.11 | .25 | 0.90 | 0.70–1.15 | |
| Manual worker | 395 | 712 | 119 | .19 | 1.11 | 0.90–1.40 | .99 | 1.00 | 0.74–1.35 | |
| Office employee | 920 | 2,954 | 455 | Reference | Reference | |||||
| Parental demographic characteristics | ||||||||||
| Marital status when the child was 2 months | .02 | |||||||||
| Single mother | 104 | 128 | 12 | .04 | 1.57 | 0.90–2.77 | .05 | 0.44 | 0.15–1.27 | |
| Married/civil union/living together | 2,169 | 6,871 | 1,447 | Reference | Reference | |||||
| Monthly income per consumption unit (euros) | .012 | |||||||||
| <600 | 118 | 125 | 22 | .001 | 1.64 | 1.10–2.43 | .87 | 1.04 | 0.54–2.02 | |
| 600–1,099 | 435 | 816 | 158 | .39 | 1.07 | 0.87–1.32 | .46 | 1.08 | 0.82–1.44 | |
| 1,100–1,799 | 1,082 | 3,268 | 599 | Reference | Reference | |||||
| 1,800–2,999 | 486 | 2,159 | 551 | .57 | 0.96 | 0.80–1.15 | .01 | 1.23 | 1.01–1.50 | |
| ≥3000 | 78 | 451 | 92 | .12 | 0.79 | 0.54–1.16 | .87 | 0.98 | 0.67–1.42 | |
| Country of birth | .0002 | |||||||||
| Mother and father France | 1,940 | 6,168 | 1,302 | Reference | Reference | |||||
| Mother not‐in‐France and father France | 105 | 338 | 61 | .09 | 1.23 | 0.90–1.70 | .004 | 0.65 | 0.44–0.95 | |
| Mother France and father not‐in‐France | 152 | 369 | 70 | .03 | 1.27 | 0.96–1.69 | .06 | 0.77 | 0.53–1.11 | |
| Mother and father not‐in‐France | 99 | 195 | 36 | .009 | 1.47 | 1.01–2.14 | .06 | 0.69 | 0.41–1.15 | |
| Familial caregiving characteristics | ||||||||||
| Maternal feeding practices | ||||||||||
| Duration of any breastfeeding | 2,336 | 7,117 | 1,478 | <.0001 | <.0001 | 0.92 | 0.90–0.94 | <.0001 | 1.1 | 1.08–1.13 |
| Reasons for feeding choice at birth | .02 | |||||||||
| Health and welfare of the child | 802 | 2,807 | 692 | Reference | ||||||
| Convenience | 349 | 818 | 91 | .90 | 0.99 | 0.80–1.23 | .003 | 0.69 | 0.51–0.96 | |
| Relationship with the child | 159 | 494 | 99 | .18 | 1.15 | 0.88–1.51 | .11 | 0.82 | 0.60–1.13 | |
| Medical advice or contraindication | 348 | 665 | 90 | .04 | 1.19 | 0.95–1.49 | .30 | 0.88 | 0.63–1.21 | |
| Usual choice in relatives | 326 | 1,010 | 247 | .77 | 1.02 | 0.83–1.26 | .58 | 1.05 | 0.84–1.31 | |
| Maternal concerns about child's health | .39 | |||||||||
| No concerns | 1,565 | 5,219 | 1,101 | Reference | Reference | |||||
| Feeding issues | 636 | 1,623 | 317 | .02 | 1.15 | 0.98–1.33 | .67 | 1.03 | 0.86–1.24 | |
| Other issues | 26 | 70 | 18 | .73 | 1.09 | 0.58–2.07 | .77 | 1.08 | 0.53–2.22 | |
| Maternal reaction when her child did not eat much | .004 | |||||||||
| “Did not insist” | 1,040 | 3,328 | 729 | Reference | Reference | |||||
| “Insisted or tried later” | 784 | 2,064 | 350 | .03 | 1.13 | 0.98–1.32 | .01 | 0.83 | 0.69–1.00 | |
| “Never happened” | 423 | 1,563 | 368 | .38 | 0.94 | 0.79–1.13 | .32 | 0.93 | 0.77–1.12 | |
| Parental caregiving characteristics | ||||||||||
| Father's presence at delivery | .06 | |||||||||
| Yes | 1,879 | 6,119 | 1,322 | Reference | Reference | |||||
| No | 422 | 907 | 144 | .63 | 1.04 | 0.84–1.30 | .14 | 0.34 | 0.63–1.13 | |
| Mother using their personal experience in child caregiving as care information source | .006 | |||||||||
| Yes | 1,765 | 5,128 | 1,133 | .0003 | 1.28 | 1.08–1.52 | .98 | 1.00 | 0.81–1.24 | |
| No | 486 | 1,838 | 319 | Reference | Reference | |||||
| Anticipated infant care arrangements for when the mother returned to work | .09 | |||||||||
| Mother only | 670 | 1,675 | 376 | Reference | Reference | |||||
| Family only (father or other member) | 304 | 686 | 114 | .32 | 1.10 | 0.87–1.39 | .76 | 1.04 | 0.75–1.43 | |
| Home nurse mainly | 87 | 289 | 67 | .47 | 1.11 | 0.76–1.62 | .58 | 1.09 | 0.72–1.65 | |
| Nursery only | 153 | 668 | 138 | .01 | 0.76 | 0.57–1.01 | .68 | 1.05 | 0.78–1.42 | |
| Nanny only | 552 | 2,121 | 482 | .34 | 0.93 | 0.76–1.13 | .07 | 1.17 | 0.93–1.47 | |
| At least two caregivers except mother and home nurse | 438 | 1,397 | 252 | .79 | 1.02 | 0.83–1.26 | .77 | 0.97 | 0.75–1.25 | |
| Others only | 33 | 104 | 21 | .98 | 1.01 | 0.57–1.76 | .93 | 1.02 | 0.53–1.97 | |
| Distribution of the home duties between the parents | .49 | |||||||||
| Equal | 1,297 | 4,303 | 955 | Reference | Reference | |||||
| Unequal more on the mother | 733 | 2,093 | 378 | .97 | 1.00 | 0.87–1.16 | .08 | 0.88 | 0.74–1.06 | |
| Unequal more on the father | 41 | 188 | 56 | .84 | 0.96 | 0.60–1.55 | .26 | 1.20 | 0.79–1.83 | |
Note. Multinomial logistic regression. Multivariable model was adjusted on maternity unit size, wave of inclusion, and residential area and included all the significant variables in bivariable analysis. In italics and in bold: significant variable (p < .001); in bold: significant modality (p < .01).
p value of the modality compared to the reference modality.
Conversely, mothers were less likely to introduce CF before 4 months for girls than for boys. Mothers were also less likely to introduce CF before 4 months for a second‐born child than for a first‐born infant. Breastfeeding duration (calculated as a continuous variable until 12 months) was negatively related to CF < 4 months. Mothers who attended at least one birth preparation class, compared with those who did not, were less likely to introduce CF < 4 months.
3.2.4. Factors associated with CFI after 6 months of age
Mothers of second‐born infants were more likely to introduce CF after 6 months than those of first‐born infants. Any breastfeeding duration was positively related to CF > 6 months. If the mother was not born in France and the father was born in France, CF was introduced less often after 6 months, compared with families in which both parents were born in France. The variable “maternal reaction when her infant did not eat much” was related to the age at CFI, as CF > 6 months was marginally less likely when “she insisted or tried later” than when “she did not insist.”
3.2.5. Sensitivity analysis of imputed data
We conducted the same analyses on the sample of 9,427 infants with computable CF age before imputation and found similar results to those obtained with the imputed data (data available on request). Variables that were nonsignificantly related to age at CFI with the nonimputed data were not related to CFI age with the imputed data, whereas variables that were related to the age at CFI with the nonimputed data were also related to CFI age with the imputed data, with comparable significance levels.
4. DISCUSSION
This study provides original insights into CFg practices based on the first representative French birth cohort. Most of the infants (62%) received their first CF between 4 and 6 months of age, 26% received CF before 4 months, 11% began CFg at 6 months as recommended by the WHO, and 12% started later than 6 months. Mothers who smoked after pregnancy, were overweight/obese, were younger, were not born in France, and were less educated were more likely to introduce CF before 4 months. Mothers of girls, of second‐born infants, mothers who attended at least one birth preparation class, and those who breastfed for a longer duration than their counterparts were less likely to introduce CF before 4 months. Breastfeeding duration was positively related to CFI > 6 months.
Three previous studies have described the CFI age in French infants. In 2002, 52% of children were introduced to CF before 4 months in a monocentric study (Bigot‐Chantepie et al., 2005). Among French infants followed in the Etude des Déterminants pré et post natals du développement et de la santé des ENfants (EDEN) cohort, born slightly later (2003–2006) in two university maternity units, 26% were introduced to CF before 4 months (Betoko et al., 2013). These studies were not representative of the French population, and estimated age at CFI was based on the WHO definition, that is, first introduction of any food other than maternal milk regardless of the frequency (WHO, 2007). According to this WHO definition, 33.2% of the children in our study received CF before 4 months. In the 2012 Épidémiologie en France de l'alimentation et de l'état nutritionnel des enfants pendant leur première année de vie (EPIFANE) study (Boudet‐Berquier et al., 2016; Salanave et al., 2016), which was representative of the French population, the median age at CFI (defined as in our study) was 5 months of age, and approximately 13% of the children received CF before 4 months, and 33.2% began CF after 6 months. Beyond methodological differences, the differences in the age at CFI across French studies could reflect improved compliance with recommendations over time. Such an evolution was observed in the United Kingdom: in the Infant Feeding Survey (McAndrew et al., 2012), CF was introduced before 4 months by 85% of mothers in 2000, 54% in 2005, and 30% in 2010. In our study, breastfeeding duration was associated with a later CFI, as widely described in other studies (Fanaro, Borsari, & Vigi, 2007; M. S. Fewtrell, Lucas, & Morgan, 2003; Giovannini et al., 2004; Kronborg et al., 2014; Rebhan et al., 2009; Schiess et al., 2010; Tang, Lee, & Binns, 2015; Tromp et al., 2013; Vingraite, Bartkeviciute, & Michaelsen, 2004; Wasser et al., 2011), including some in France (Boudet‐Berquier et al., 2016; Salanave et al., 2016). Here, the association between breastfeeding duration and CFI was of small amplitude, which could be partially explained by the low rate and short duration of breastfeeding in France compared with other countries (de Lauzon‐Guillain et al., 2013). In the ELFE population, only 28% of the mothers were still breastfeeding at CFI, and only 10% were predominantly breastfeeding after 6 months of age (Wagner et al., 2015), showing a low rate of compliance with WHO breastfeeding recommendations. A short duration of breastfeeding was observed in our study, that is, approximately 3.5 months in the population of those with an available CFI age. Breastfeeding durations longer than 1 year only represented a small part of the study sample. This study confirmed that youngest, overweight/obese, smoking, and less educated mothers were more likely to introduce CF before 4 months, consistent with previous studies (Betoko et al., 2013; Boudet‐Berquier et al., 2016; Kronborg et al., 2014; Rebhan et al., 2009; Salanave et al., 2016; Schack‐Nielsen, Sorensen, Mortensen, & Michaelsen, 2010; Schiess et al., 2010; Wijndaele et al., 2009). Obese mothers may have a less acute perception of the hunger/satiety cues of their children (Gross et al., 2010), which may lead them to introduce CF earlier. Attending at least one birth preparation class was associated with a lower probability of CF < 4 months and a longer breastfeeding duration (Wagner et al., 2015). In the ELFE cohort, women who attended antenatal classes were more compliant with recommendations about their own diet during pregnancy (Kadawathagedara et al., 2014). As no CFg advice is provided in these classes, this finding is likely a marker of a greater interest in health‐related factors such as nutrition among those who chose to attend antenatal classes, leading to better compliance with recommendations.
Being a second‐born child was linked to a decreased probability of CF < 4 months and an increased probability of CF > 6 months. However, mothers who used personal experience to inform their child caregiving began CF < 4 months more often. This suggests that the maternal experience referred to may not involve the mother's own children but may instead pertain to another situation, such as occupational experience or having previously cared for other children. More specifically, the evolution of recommendations could explain the earlier CFI for women who rely on their own experience, because CFI was recommended before 4 months for the previous generation in France (Gojard, 2000). Analysis revealed that in our study, among mothers who reported using their personal experience as information source in child caregiving (“experienced mothers”), 79.7% reported having already taken care of another baby sometimes or often compared with 48.3% of mothers who did not report using their personal experience (“inexperienced mothers”). Interestingly, they especially differed regarding having been a babysitter (48.6% of experienced mothers vs. 34.5% of inexperienced ones) or having taken care of a baby in the course of their occupation (21.2% vs. 7.8%, respectively), but not as much in having taken care of their siblings (29.4% vs. 23%, respectively). Furthermore, it has been suggested in a previous French study that the probability of having cared for younger children prior to motherhood decreased with the level of education (Gojard, 2000). Here, we observed that maternal experience was a significant factor explaining the variability in CFI age, in addition to level of education. Finally, maternal experience could also be related to an intergenerational transmission of infant care and feeding habits, which may differ by social group, as was already observed in France (Gojard, 2000).
Boys were more likely than girls to be introduced to CF before 4 months. This has already been described (Kronborg et al., 2014; Wright, Parkinson, & Drewett, 2004), although not systematically (Betoko et al., 2013; Hendricks, Briefel, Novak, & Ziegler, 2006; Scott et al., 2009; Wijndaele et al., 2009). Mothers may have found that boys “needed more” or “were hungry,” as suggested by a prospective population‐based cohort study conducted in the United Kingdom in 2004 (Wright et al., 2004). In this study, male babies were introduced to CF before 3 months more frequently than girls, and this was partly related to their larger size and therefore higher energy requirements. The maternal perception of the infant's hunger cues could also have been different between boys and girls: Mothers who introduced CFg earlier recognized that the perceived needs of their baby (“seemed hungry” and “it was the right time”) were of greater influence than external advice from health professionals or written materials (Wright et al., 2004).
This study provides original insights into paternal factors, of which some, such as country of birth, remain significant in the multivariate analyses. Few studies describe paternal influences on young children's feeding behaviour (Betoko et al., 2013; Camara et al., 2015; Chary, Messmer, & Rohloff, 2011; Walsh, Cameron, Crawford, Hesketh, & Campbell, 2016; Walsh, Cameron, Hesketh, Crawford, & Campbell, 2015), but there is growing evidence that paternal factors, such as education or BMI, may affect the child's growth (Parikka et al., 2015). Although infant feeding practices may mainly depend on the mother, it may also be influenced by the father who may have different dietary habits (Bertin et al., 2016; Si Hassen et al., 2016). Moreover, their dietary habits may be differently stratified according to income, occupation, and education level than those of mothers (Lioret et al., 2012; Northstone, 2012). Thus, it was important to study whether these paternal characteristics, as well as those linked to breastfeeding practices in this cohort, were linked to CFg practices. Here, some factors were significant in the bivariate analysis (marital status, father's age, occupation type, monthly income, and parental country of birth); however, only parental country of birth remained significant after adjustments were made for other factors, confirming that maternal factors are more strongly associated with CFI age than paternal factors.
The factors associated with earlier CFI were consistent with those linked to a lower breastfeeding initiation rate and shorter duration, except for the infant's sex, which was not linked with breastfeeding initiation or duration in the ELFE cohort (Kersuzan et al., 2014; Wagner et al., 2015), and parental country of birth. Mothers who were not born in France were more likely to breastfeed and for a longer duration (Kersuzan et al., 2014; Wagner et al., 2015), although they were more likely to initiate CF < 4 months and less likely to initiate CF > 6 months than those born in France. Thus, cultural factors are important to consider when providing CFg advice.
In the EPIFANE study, a score for compliance with national nutritional recommendations was constructed to account for the conduct of CFg (Boudet‐Berquier et al., 2016). This score was higher in the mothers born outside France than mothers born in France, and we found that mothers born outside France were more likely to introduce CF before 4 months, which is not recommended in France. The higher compliance score in mothers born outside France in the EPIFANE study may be driven by other practices than timing of CFg, such as offering added fats or eggs before 12 months. Alternatively, this different observation may be related to the different prevalence of mothers born outside France in the two studies: 18% in the EPIFANE study versus 13% in the ELFE study.
Some demographic and socio‐economic maternal characteristics that are independently associated with CFI age may also be associated with each other (being young, obese, a smoker, less educated, and born outside France), indicating a “disadvantaged mother” profile. These mothers may be less likely to adhere to CFI recommendations as a result of several barriers: caregiving habits determined by different social norms, financial difficulties, and different perceptions of physiological cues of hunger and satiation. Such “disadvantaged profiles” may determine health inequalities. Traditional means of information or health promotion, such as nutritional health campaigns (for example, in the PNNS), allow increasing global knowledge about “healthy habits” in the general population (Estaquio et al., 2009). However, they do not necessarily lead to modifications towards healthier habits in the same way between different social groups and thus may fail to reduce health inequalities (Escalon, Beck, & Bossard, 2013). Our data emphasize the need to further support individual‐focused initiatives with health‐enhancing environmental strategies and innovative methods. Such a programme, Text4baby, was developed in the United States, aiming to provide adequate health advice to pregnant mothers and mothers of infants under 1 year old; its results included, for example, some improvement in attitudes against maternal alcohol consumption (Evans, Wallace, & Snider, 2012). Repeated information may be needed, starting before birth during birth preparation classes and across the first year by trained midwives, paediatricians, or general practitioners serving families. The results based on the ELFE cohort may help to identify the target population that may need messages promoting good nutrition.
This study must be viewed in light of its strengths and limitations. For the first time, this study reports data on CF practices from a nationally representative French sample, with prospective monthly collection of CFg practices. We were able to address a large number of factors simultaneously to reflect the multidimensionality of factors associated with feeding practices. It can be noted that the age at CFI was calculated with a precision of 1 month.
Some limitations are to be taken into account to generalize these results. The food frequency feeding questionnaire was self‐administered; it may, therefore, be prone to a social desirability bias, although no judgmental evaluation was returned to the parents. Neither numbered monthly frequencies nor portion sizes were collected, because a pilot study (unpublished data) showed that it was challenging to collect this type of information in this cohort. Because many variables were collected apart from nutrition, the questionnaire had to be easy to fill out.
A significant refusal rate was observed at the inclusion period, because almost 51% of the parents did not consent to participate. This is a common limitation to all longitudinal cohort studies. The parents of included children engaged themselves and their children for a planned follow‐up of 20 years. Such commitment could have hindered their participation, especially because the consent was asked in the 2 to 3 days after birth in the maternity unit.
To address the potential impact of missing data on the age at CFI, an imputation method was applied, which can lead to some biases. However, the imputation method was defined to be as conservative as possible, taking into account the longitudinal profile of CFI of the respondents. We indeed observed that the results of the analyses conducted on our nonimputed data led to conclusions consistent with those drawn from the imputed data set (full results available on request).
Nevertheless, the participants who answered the CFg questionnaire presented selection bias compared with the whole ELFE population. Nonrespondent mothers were younger, less educated, more likely to be born outside France, and more likely to smoke, and they had a higher BMI; that is, they were more likely to represent disadvantaged families, which may lead to underestimations of significance and/or effect sizes. However, to obtain nationally representative from this specific questionnaire on CFg practices, we weighted the data to take into account the inclusion procedure and biases related to nonconsent and nonresponse. This weighting was applied to calculate population estimates of age at CFI but was not used for the multivariable analyses, in order to avoid too many assumptions regarding nonrespondents' feeding practices. Multivariable analyses were only adjusted for variables that were discriminant between consent and nonconsent samples at inclusion and those that were related to sampling design (maternity unit size, parental region of residence, and recruitment wave). With a sample of almost 11,000 children, the categories depicting the disadvantaged families were still large enough to calculate significant estimations of their relationship with the age at CFI. Therefore, our study is powerful enough to draw some reliable conclusions about those categories and the feeding practices of parents therein.
In other respects, we focused all our multivariate analyses on testing the main effects of the possible determinants of CFI age. Considering the numerous factors included in the analysis, the interactions were not tested in these models, but they could be further studied.
The relationship between health status and CFI age was not evaluated. Parents of most children with severe congenital medical conditions may have refrained from participating, either at inclusion or at CFI age. Very few children (<1%) were declared “in bad health” at 2 months, and no link between transferring to a Neonatal Intensive Care Unit and CFI age was found in this study. Moderate preterm birth (33–37 weeks of amenorrhoea) was not associated with a later CFI age, as already described (Fanaro et al., 2007), and could be explained by the lack of clear CFI recommendations in France for preterm children.
Finally, the relationship between anthropometric measurements and CF practices was not evaluated in this study (A. D. Jones et al., 2014), because these data were not yet available except for birth weight. However, this relationship will be assessed specifically in future studies.
In conclusion, as in other developed countries, the introduction of CF in this French sample mostly began after 4 months of age, but few of the mothers followed the WHO recommendation to introduce CF at 6 months of age. It is important to continue promoting clear messages regarding CF recommendations, especially in families more likely to introduce CF before 4 months, namely, families with young mothers who were not born in France, smoke, are overweight, or do not breastfeed. Our results underscore the need to develop innovative public health actions towards the groups that are less receptive to nutritional messages, such as parents born outside the country, informed by qualitative research on how these groups perceive infant feeding.
Future studies within this cohort will examine the relationship between the timing and progress of milk and CFg practices and children's early and later growth, obesity, and allergy risk.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
SG, CT, MAC, BLG, and SN designed the data collection, which was supervised and coordinated by MAC. XT designed the sampling procedure. MB, CT, SG, SN, and MAC conceptualized and/or designed research. EK, MB, and SN designed the analyses, which were performed by EK and SN. SW contributed to the statistical analyses. MB, EK, and SN analysed and interpreted the results. EK, SW, CK, CT, SG, XT, MAC, BLG, and SL contributed to the interpretation of the results. MB and EK wrote the initial paper, which was then reviewed and revised by SW, CK, CT, SG, XT, and MAC. BLG, SL, and SN critically reviewed the manuscript. MB, BLG, and SN had primary responsibility for final content.
Supporting information
Data S1. Imputation method
Data S2. Description of the studied variables.
Data S3. Results of the bivariate analyses.
Table S1. Results of the bivariate analyses of the characteristics associated with the age of introduction of complementary feeding.
ACKNOWLEDGMENTS
The authors acknowledge people who collected the data, and the families of the children followed up in the ELFE study.
Bournez M, Ksiazek E, Wagner S, et al. Factors associated with the introduction of complementary feeding in the French ELFE cohort study. Matern Child Nutr. 2018;14:e12536 10.1111/mcn.12536
REFERENCES
- Agostoni, C. , Decsi, T. , Fewtrell, M. , Goulet, O. , Kolacek, S. , Koletzko, B. , … van Goudoever, J. (2008). Complementary feeding: A commentary by the ESPGHAN Committee on Nutrition. Journal of Pediatric Gastroenterology and Nutrition, 46(1), 99–110. 10.1097/01.mpg.0000304464.60788.bd [DOI] [PubMed] [Google Scholar]
- Allison, P. D. (1999). Multiple regression: A primer (research methods and statistics) (1st ed.). Thousand Oaks: C. P. F. P. Ed. [Google Scholar]
- Bertin, M. , Touvier, M. , Dubuisson, C. , Dufour, A. , Havard, S. , Lafay, L. , … Lioret, S. (2016). Dietary patterns of French adults: Associations with demographic, socio‐economic and behavioural factors. Journal of Human Nutrition and Dietetics, 29(2), 241–254. 10.1111/jhn.12315 [DOI] [PubMed] [Google Scholar]
- Betoko, A. , Charles, M. A. , Hankard, R. , Forhan, A. , Bonet, M. , Saurel‐Cubizolles, M. J. , … de Lauzon‐Guillain, B. (2013). Infant feeding patterns over the first year of life: influence of family characteristics. European Journal of Clinical Nutrition, 67(6), 631–637. 10.1038/ejcn.2012.200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bigot‐Chantepie, S. , Michaud, L. , Devos, P. , Depoortere, M. H. , Dubos, J. P. , Gottrand, F. , & Turck, D. (2005). Feeding practices in infants: A 6‐month prospective cohort study. Archives de Pédiatrie, 12(11), 1570–1576. 10.1016/j.arcped.2005.07.020 [DOI] [PubMed] [Google Scholar]
- Blondel, B. , Lelong, N. , Kermarrec, M. , Goffinet, F. , & National Coordination Group of the National Perinatal, S . (2012). Trends in perinatal health in France from 1995 to 2010. Results from the French National Perinatal Surveys. Journal de Gynécologie, Obstétrique et Biologie de la Reproduction, 41(4), e1–e15. 10.1016/j.jgyn.2012.04.014 [DOI] [PubMed] [Google Scholar]
- Boudet‐Berquier, J. , Salanave, B. , de Launay, C. , & Castetbon, K. (2016). Introduction of complementary foods with respect to French guidelines: Description and associated socio‐economic factors in a nationwide birth cohort (Epifane survey). Maternal & Child Nutrition. 10.1111/mcn.12339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdette, H. L. , Whitaker, R. C. , Hall, W. C. , & Daniels, S. R. (2006). Breastfeeding, introduction of complementary foods, and adiposity at 5 y of age. AJCN, 83(3), 550–558. [DOI] [PubMed] [Google Scholar]
- Camara, S. , de Lauzon‐Guillain, B. , Heude, B. , Charles, M.‐A. , Botton, J. , Plancoulaine, S. , … Lioret, S. (2015). Multidimensionality of the relationship between social status and dietary patterns in early childhood: Longitudinal results from the French EDEN mother‐child cohort. IJBNPA, 12(1), 1–10. 10.1186/s12966-015-0285-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caron, N. (2005). The correction of total nonresponse by reweighting and imputation, INSEE Work Document, M0502.
- Chary, A. N. , Messmer, S. E. , & Rohloff, P. J. (2011). Male influence on infant feeding in rural Guatemala and implications for child nutrition interventions. Breastfeeding Medicine, 6(4), 227–231. 10.1089/bfm.2011.0015 [DOI] [PubMed] [Google Scholar]
- Escalon, H. , Beck, F. , & Bossard, C. (2013). Connection between the knowledge of the recommendations of the National Nutrition and Health Program and patterns of eating behaviour and physical activity. Revue d'Épidémiologie et de Santé Publique, 61(1), 37–47. 10.1016/j.respe.2012.05.007 [DOI] [PubMed] [Google Scholar]
- Estaquio, C. , Kesse‐Guyot, E. , Deschamps, V. , Bertrais, S. , Dauchet, L. , Galan, P. , … Castetbon, K. (2009). Adherence to the French Programme National Nutrition Sante Guideline Score is associated with better nutrient intake and nutritional status. Journal of the American Dietetic Association, 109(6), 1031–1041. 10.1016/j.jada.2009.03.012 [DOI] [PubMed] [Google Scholar]
- Evans, W. D. , Wallace, J. L. , & Snider, J. (2012). Pilot evaluation of the text4baby mobile health program. BMC Public Health, 12, 1031 10.1186/1471-2458-12-1031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fanaro, S. , Borsari, G. , & Vigi, V. (2007). Complementary feeding practices in preterm infants: An observational study in a cohort of Italian infants. Journal of Pediatric Gastroenterology and Nutrition, 45(Suppl 3), S210–S214. 10.1097/01.mpg.0000302974.90867.f1 [DOI] [PubMed] [Google Scholar]
- Fewtrell, M. , Bronsky, J. , Campoy, C. , Domellöf, M. , Embleton, N. , Fidler Mis, N. , … Molgaard, C. (2017). Complementary feeding: A position paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) committee on nutrition. Journal of Pediatric Gastroenterology and Nutrition, 64(1), 119–132. 10.1097/mpg.0000000000001454 [DOI] [PubMed] [Google Scholar]
- Fewtrell, M. S. , Lucas, A. , & Morgan, J. B. (2003). Factors associated with weaning in full term and preterm infants. Archives of disease in childhood Fetal Neonatal Edition, 88(4), F296–F301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giovannini, M. , Riva, E. , Banderali, G. , Scaglioni, S. , Veehof, S. H. , Sala, M. , … Agostoni, C. (2004). Feeding practices of infants through the first year of life in Italy. Acta Paediatrica, 93(4), 492–497. [DOI] [PubMed] [Google Scholar]
- Gojard, S. (2000). L'alimentation dans la prime enfance: Diffusion et réception des normes de puériculture. [Feeding in infancy: Diffusion and reception of the childcare standards]. Revue Française de Sociologie, 41(3), 475–512. 10.2307/3322542 [DOI] [Google Scholar]
- Gross, R. S. , Fierman, A. H. , Mendelsohn, A. L. , Chiasson, M. A. , Rosenberg, T. J. , Scheinmann, R. , & Messito, M. J. (2010). Maternal perceptions of infant hunger, satiety, and pressuring feeding styles in an urban Latina WIC Population. Academic Pediatrics, 10(1), 29–35. 10.1016/j.acap.2009.08.001 [DOI] [PubMed] [Google Scholar]
- Health comes with eating. (2005). Retrieved from http://www.inpes.sante.fr/CFESBases/catalogue/pdf/890.pdf
- Hendricks, K. , Briefel, R. , Novak, T. , & Ziegler, P. (2006). Maternal and child characteristics associated with infant and toddler feeding practices. Journal of the American Dietetic Association, 106(1 Suppl 1), S135–S148. 10.1016/j.jada.2005.09.035 [DOI] [PubMed] [Google Scholar]
- Jones, A. D. , Ickes, S. B. , Smith, L. E. , Mbuya, M. N. , Chasekwa, B. , Heidkamp, R. A. , … Stoltzfus, R. J. (2014). World Health Organization infant and young child feeding indicators and their associations with child anthropometry: A synthesis of recent findings. Maternal & Child Nutrition, 10(1), 1–17. 10.1111/mcn.12070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, L. , Moschonis, G. , Oliveira, A. , de Lauzon‐Guillain, B. , Manios, Y. , Xepapadaki, P. , … Emmett, P. (2015). The influence of early feeding practices on healthy diet variety score among pre‐school children in four European birth cohorts. Public Health Nutrition, 18(10), 1774–1784. 10.1017/S1368980014002390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadawathagedara, M. , Kersuzan, C. , Tichit, C. , Gojard, S. , Charles, M. A. , Lioret, S. , & De Lauzon‐Guillain, B. (2014). Respect des recommandations PNNS chez les femmes enceintes de l'enquête Elfe. Nutrition Clinique et Metabolisme, 28(Suppl 1, Dec 2014), S30–S31. 10.1016/s0985-0562 [DOI] [Google Scholar]
- Kersuzan, C. , Gojard, S. , Tichit, C. , Thierry, X. , Wagner, S. , Nicklaus, S. , … de Lauzon‐Guillain, B. (2014). Breastfeeding prevalence in maternity wards according to parents and delivery characteristics. Results from the ELFE Survey in maternity units, mainland France, 2011. Bulletin Epidémiologique Hebdomadaire (Paris), 27, 440–449. [Google Scholar]
- Kronborg, H. , Foverskov, E. , & Vaeth, M. (2014). Predictors for early introduction of solid food among Danish mothers and infants: An observational study. BMC Pediatrics, 14 10.1186/1471-2431-14-243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange, C. , Visalli, M. , Jacob, S. , Chabanet, C. , Schlich, P. , & Nicklaus, S. (2013). Maternal feeding practices during the first year and their impact on infants' acceptance of complementary food. Food Quality and Preference, 29(2), 89–98. 10.1016/j.foodqual.2013.03.005 [DOI] [Google Scholar]
- de Lauzon‐Guillain, B. , Jones, L. , Oliveira, A. , Moschonis, G. , Betoko, A. , Lopes, C. , … Charles, M. A. (2013). The influence of early feeding practices on fruit and vegetable intake among preschool children in 4 European birth cohorts. IJBNPA, 98(3), 804–812. 10.3945/ajcn.112.057026 [DOI] [PubMed] [Google Scholar]
- Lioret, S. , McNaughton, S. A. , Crawford, D. , Spence, A. C. , Hesketh, K. , & Campbell, K. J. (2012). Parents' dietary patterns are significantly correlated: Findings from the Melbourne Infant Feeding Activity and Nutrition Trial Program. The British Journal of Nutrition, 108(3), 518–526. 10.1017/s0007114511005757 [DOI] [PubMed] [Google Scholar]
- McAndrew, F. , Thompson, J. , Fellows, L. , Large, A. , Speed, M. , & Renfrew, M. J. (2012). Infant feeding survey 2010 consolidated report.
- Michaelsen, K. F. , Larnkjaer, A. , Lauritzen, L. , & Molgaard, C. (2010). Science base of complementary feeding practice in infancy. Current Opinion in Clinical Nutrition and Metabolic Care, 13(3), 277–283. [DOI] [PubMed] [Google Scholar]
- Michaelsen, K. F. , Larnkjaer, A. , & Molgaard, C. (2013). Early diet, insulin‐like growth factor‐1, growth and later obesity. World Review of Nutrition and Dietetics, 106, 113–118. 10.1159/000342555 [DOI] [PubMed] [Google Scholar]
- Moorcroft, K. E. , Marshall, J. L. , & McCormick, F. M. (2011). Association between timing of introducing solid foods and obesity in infancy and childhood: A systematic review. Maternal & Child Nutrition, 7(1), 3–26. 10.1111/j.1740-8709.2010.00284.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss, B. G. , & Yeaton, W. H. (2014). Early childhood healthy and obese weight status: Potentially protective benefits of breastfeeding and delaying solid foods. Maternal and Child Health Journal, 18(5), 1224–1232. 10.1007/s10995-013-1357-z [DOI] [PubMed] [Google Scholar]
- Nicklaus, S. (2016). Complementary feeding strategies to facilitate acceptance of fruits and vegetables: A narrative review of the literature. International Journal of Environmental Research and Public Health, 13(11). 10.3390/ijerph13111160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northstone, K. (2012). Dietary patterns: The importance of sex differences. The British Journal of Nutrition, 108(3), 393–394. 10.1017/s0007114511006337 [DOI] [PubMed] [Google Scholar]
- Onyango, A. W. , Borghi, E. , de Onis, M. , Casanovas, M. D. C. , & Garza, C. (2014). Complementary feeding and attained linear growth among 6–23‐month‐old children. Public Health Nutrition, 17(9), 1975–1983. 10.1017/s1368980013002401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parikka, S. , Mäki, P. , Levälahti, E. , Lehtinen‐Jacks, S. , Martelin, T. , & Laatikainen, T. (2015). Associations between parental BMI, socioeconomic factors, family structure and overweight in Finnish children: A path model approach. BMC Public Health, 15(1), 1–10. 10.1186/s12889-015-1548-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce, J. , & Langley‐Evans, S. C. (2013). The types of food introduced during complementary feeding and risk of childhood obesity: A systematic review. International Journal of Obesity, 37(4), 477–485. 10.1038/ijo.2013.8 [DOI] [PubMed] [Google Scholar]
- Rebhan, B. , Kohlhuber, M. , Schwegler, U. , Koletzko, B. V. , & Fromme, H. (2009). Infant feeding practices and associated factors through the first 9 months of life in Bavaria, Germany. Journal of Pediatric Gastroenterology and Nutrition, 49(4), 467–473. 10.1097/MPG.0b013e31819a4e1a [DOI] [PubMed] [Google Scholar]
- Salanave, B. , deLaunay, C. , Boudet‐Berquier, J. , Guerrisi, C. , & Castetbon, K. (2016). Infant feeding practices during the first year of life. Results from the Epifane study 2012–2013. Saint‐Maurice: Institut de veille sanitaire; Retrieved from http://www.invs.sante.fr [Google Scholar]
- Sautory, O. (1991). Straightening of sampling of household surveys by calibration on margins, INSEE Work document n° F 9103,INSEE.
- Schack‐Nielsen, L. , Sorensen, T. , Mortensen, E. L. , & Michaelsen, K. F. (2010). Late introduction of complementary feeding, rather than duration of breastfeeding, may protect against adult overweight. The American Journal of Clinical Nutrition, 91(3), 619–627. 10.3945/ajcn.2008.27078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiess, S. , Grote, V. , Scaglioni, S. , Luque, V. , Martin, F. , Stolarczyk, A. , … Koletzko, B. (2010). Introduction of complementary feeding in 5 European countries. Journal of Pediatric Gastroenterology and Nutrition, 50(1), 92–98. 10.1097/MPG.0b013e31819f1ddc [DOI] [PubMed] [Google Scholar]
- Schwartz, C. , Scholtens, P. , Lalanne, A. , Weenen, H. , & Nicklaus, S. (2011). Development of healthy eating habits early in life: Review of recent evidence and selected guidelines. Appetite, 57(3), 796–807. [DOI] [PubMed] [Google Scholar]
- Scott, J. A. , Binns, C. W. , Graham, K. I. , & Oddy, W. H. (2009). Predictors of the early introduction of solid foods in infants: Results of a cohort study. BMC Pediatrics, 9(1), 1–9. 10.1186/1471-2431-9-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Si Hassen, W. , Castetbon, K. , Cardon, P. , Enaux, C. , Nicolaou, M. , Lien, N. , … Mejean, C. (2016). Socioeconomic indicators are independently associated with nutrient intake in French adults: A DEDIPAC Study. Nutrients, 8(3), 158 10.3390/nu8030158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang, L. , Lee, A. H. , & Binns, C. W. (2015). Predictors of early introduction of complementary feeding: Longitudinal study. Pediatrics International, 57(1), 126–130. 10.1111/ped.12421 [DOI] [PubMed] [Google Scholar]
- Tromp, I. I. , Briede, S. , Kiefte‐de Jong, J. C. , Renders, C. M. , Jaddoe, V. W. , Franco, O. H. , … Moll, H. A. (2013). Factors associated with the timing of introduction of complementary feeding: The Generation R Study. European Journal of Clinical Nutrition, 67(6), 625–630. 10.1038/ejcn.2013.50 [DOI] [PubMed] [Google Scholar]
- Vandentorren, S. , Bois, C. , Pirus, C. , Sarter, H. , Salines, G. , Leridon, H. , & Elfe, t. (2009). Rationales, design and recruitment for the Elfe longitudinal study. BMC Pediatrics, 9, 58 10.1186/1471-2431-9-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vingraite, J. , Bartkeviciute, R. , & Michaelsen, K. F. (2004). A cohort study of term infants from Vilnius, Lithuania: Feeding patterns. Acta Paediatrica, 93 10.1111/j.1651-2227.2004.tb02936.x [DOI] [PubMed] [Google Scholar]
- Wagner, S. , Kersuzan, C. , Gojard, S. , Tichit, C. , Nicklaus, S. , Geay, B. , … De Lauzon‐Guillain, B. (2015). Breastfeeding duration in France according to parents and birth characteristics. Results from the ELFE longitudinal French study, 2011. Bulletin Epidémiologique Hebdomadaire (Paris), 29, 440–449. [Google Scholar]
- Walsh, A. D. , Cameron, A. J. , Crawford, D. , Hesketh, K. D. , & Campbell, K. J. (2016). Dietary associations of fathers and their children between the ages of 20 months and 5 years. Public Health Nutrition, 19(11), 2033–2039. 10.1017/s136898001600077x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh, A. D. , Cameron, A. J. , Hesketh, K. D. , Crawford, D. , & Campbell, K. J. (2015). Associations between dietary intakes of first‐time fathers and their 20‐month‐old children are moderated by fathers' BMI, education and age. The British Journal of Nutrition, 114(6), 988–994. 10.1017/s0007114515002755 [DOI] [PubMed] [Google Scholar]
- Wasser, H. , Bentley, M. , Borja, J. , Goldman, B. D. , Thompson, A. , Slining, M. , & Adair, L. (2011). Infants perceived as “fussy” are more likely to receive complementary foods before 4 months. Pediatrics, 127(2), 229–237. 10.1542/peds.2010-0166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen, X. , Kong, K. L. , Eiden, R. D. , Sharma, N. N. , & Xie, C. (2014). Sociodemographic differences and infant dietary patterns. Pediatrics. 10.1542/peds.2014-1045 [DOI] [PubMed] [Google Scholar]
- Wijndaele, K. , Lakshman, R. , Landsbaugh, J. R. , Ong, K. K. , & Ogilvie, D. (2009). Determinants of early weaning and use of unmodified cow's milk in infants: A systematic review. Journal of the American Dietetic Association, 109(12), 2017–2028. 10.1016/j.jada.2009.09.003 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2003). Feeding and nutrition of infants and young children In Guidelines for the WHO European region, with emphasis on the former Soviet countries (87). Retrieved from. Geneva: WHO_GuidelinesEuroSoviet. [Google Scholar]
- World Health Organization . (2007). Indicators for assessing infant and young child feeding practices Part 1: Definitions. Retrieved from http://www.who.int/maternal_child_adolescent/documents/9789241596664/en http://apps.who.int/iris/bitstream/10665/43895/1/9789241=596664_eng.pdf
- Wright, C. M. , Parkinson, K. N. , & Drewett, R. F. (2004). Why are babies weaned early? Data from a prospective population based cohort study. Archives of diseases in childhood, 89 10.1136/adc.2003.038448 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Imputation method
Data S2. Description of the studied variables.
Data S3. Results of the bivariate analyses.
Table S1. Results of the bivariate analyses of the characteristics associated with the age of introduction of complementary feeding.


