Abstract
Some 37% (~64 million) South Asian children under 5 years are stunted. Most stunting occurs during the complementary feeding period (6–23 months). Our objective was to (a) characterize complementary feeding practices in South Asia and (b) review the effectiveness of information, education, and counselling (IEC) interventions aiming to improve complementary feeding in South Asia. We conducted a comprehensive review of (a) the latest nationally representative survey data and (b) peer‐reviewed interventions (January 1990 to December 2015) that used IEC as the main strategy to improve complementary feeding. The analytical sample included 30,966 children aged 6–23 months. Foods made from grains are the main complementary food (76.8% of children). Only 33.2% of children are fed fruits and vegetables rich in vitamin A and a mere 17.1% are fed complementary foods containing meat, fish, poultry and/or eggs. Timely introduction, minimum meal frequency, minimum dietary diversity, and minimum acceptable diet were estimated at 57.4%, 47.7%, 33.0%, and 20.5%, respectively. The evidence on the effectiveness of IEC interventions is limited in quantity, quality, and scale. The 12 intervention studies that met the inclusion criteria indicate that IEC interventions delivered by many types of primary care workers/community resource persons using multiple contact opportunities improved the timeliness, frequency, diversity, and/or adequacy of complementary feeding. However, acceptability, availability, and affordability seem to constrain improvements in diet diversity, particularly foods of animal origin. The small size of most intervention studies and the training and/or supervision intensity of counsellors raise concerns about the potential for scale and/or sustainability of some of the interventions reviewed.
Keywords: complementary feeding, infants and young children, South Asia
1. BACKGROUND
The linear growth of healthy children from birth to 5 years of age is remarkably similar the world over (Multi Centre Growth Reference Study Group, 2006). Yet, recent global estimates indicate that 23% of children aged 0–59 months (i.e., 155 million) have stunted growth due to chronic nutrition deprivation (UNICEF, WHO, WBG, 2017). It is estimated that stunting—a height‐for‐age z‐score below −2 of the median in the World Health Organization Child Growth Standards—is the cause of about 1 million child deaths annually (Black et al., 2013). For the children who survive, stunting causes lasting damage, including poor cognition and educational performance in childhood; reduced productivity and earnings in adulthood; and, if accompanied by excessive weight gain in later childhood, increased risk of chronic diseases (Black et al., 2013; de Onis & Branca, 2016; Dewey & Begum, 2011; Victora et al., 2008).
Globally, it is acknowledged that most stunting in low‐ and middle‐income countries happens during the 1000 day period that encompasses pregnancy and the child's first 2 years after birth (Dewey & Vitta, 2013). Considerable growth faltering occurs during the prenatal period and the first 6 months of life and additional linear growth faltering still happens after the first 2 years of life (Leroy, Ruel, Habicht, & Frongillo, 2014). However, evidence shows that the largest proportion of stunting in low‐ and middle‐income countries occurs during the complementary feeding period (6–23 months), the ~500 day transition time from exclusive breastfeeding to consuming a wide range of family foods while breastfeeding continues (WHO, 1998).
During the complementary feeding period, children consume small amounts of foods, given their small gastric capacity. Consequently, complementary foods need to have high nutrient density (i.e., the amount of each nutrient per 100 kcal of food) and be fed frequently to support optimal physical growth and brain development. Meeting the nutritional needs of children 6–23 months old can be challenging, particularly, but not exclusively, in resource poor settings and can lead to stunted growth and development in infancy and early childhood (Dewey, 2016). Therefore, ensuring adequate complementary foods and feeding for children 6–23 months old is critical to achieve the global target of reducing by 40% the number of stunted under five year olds—from about 171 million in 2010 to about 100 million—by 2025 (WHO, 2012).
South Asia is at the epicentre of the global child‐stunting crisis. The latest available data indicate that 37% (~64 million) of South Asia's children aged 0–59 months are stunted. Levels of child stunting in South Asia are comparable to those in sub‐Saharan Africa (36%), twice higher than those in the Middle‐East and Northern‐Africa (18%), and 3 times higher than those in East Asia and the Pacific (12%) or Latin America (10%; UNICEF, 2015). The high prevalence of stunting and the region's large child population (~26% of the world's children under 5 years) means that South Asia bears ~40% of the global burden of child stunting (UNICEF South Asia, 2015). Recent analyses indicate that children's poor diets in the first years of life are a main driver of child stunting in South Asia (Corsi, Mejía‐Guevara, & Subramanian, 2015; Smith & Haddad, 2014; Aguayo & Menon, 2016; Aguayo, Nair, Badgaiyan, & Krishna, 2016). Thus, researchers and practitioners have not hesitated to refer to the situation of complementary feeding in South Asia as a crisis (Menon, 2012).
The availability of recent survey and research data documenting complementary feeding practices in infants and young children aged 0–23 months, the availability of internationally‐agreed upon indicators to assess the adequacy of complementary feeding practices for children 6–23 months old (WHO 2008a; WHO 2008b; Daelmans, Dewey, & Arimond, 2009), and the global drive to reduce child stunting as part of the post‐2015 global development agenda (WHO, 2015) make it possible and necessary to take stoke of complementary feeding practices in South Asia.
The objective of this paper is twofold: (a) to characterize current complementary feeding practices for infants and young children 6–23 months old in South Asia and (b) to review the evidence base on the effectiveness of information, education, and counselling (IEC) interventions aiming to improve complementary feeding practices in children 6–23 months old in South Asia. Using the results from these two objectives, we then identify advocacy, policy, programme, and research priorities to protect, promote, and support optimal complementary feeding in South Asia post‐2015.
Key messages.
South Asia is at the epicentre of the global child stunting crisis. Some 37% (~64 million) of South Asia's children aged 0–59 months have stunted growth. Most stunting occurs during the complementary feeding period (6–23 months).
Foods made from grains are the main complementary food (76.8% of children 6–23 months); whereas, only 33.2% is fed fruits and vegetables rich in vitamin A, and a mere 14% is fed complementary foods containing meat, fish, poultry, and/or eggs.
Timely introduction of complementary foods, minimum meal frequency, minimum dietary diversity, and minimum acceptable diet in children aged 6–23 months was estimated at 57.4%, 47.7%, 33.0%, and 20.5%, respectively.
IEC interventions delivered by primary care workers/community resource persons using multiple contacts/opportunities improved timeliness, frequency, diversity, and/or adequacy of complementary feeding. However, acceptability, availability, and affordability seem to constrain improvements in diet diversity, particularly foods of animal origin.
The small size of most intervention studies and the training and/or supervision intensity of counsellors raise concerns about the potential for scale and/or sustainability of some of the interventions reviewed.
2. METHODS
For the purpose of this analysis, South Asia includes the eight countries under the umbrella of the South Asia Association for Regional Cooperation: Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, and Sri Lanka. To meet the objectives of the analysis, we conducted a comprehensive review of two sources of data and information:
The latest nationally representative nutrition survey in Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, and Sri Lanka: For each country, we included in the analysis the latest nutrition survey published before December 31, 2015, that met the following criteria: (a) a well‐defined population‐based sampling frame; (b) a probabilistic sampling procedure; (c) a national‐level representative sample; and (d) use of internationally agreed upon measurements and indicators to assess feeding practices in children aged 6–23 months. The surveys included in the review are Afghanistan, National Nutrition Survey 2013; Bangladesh, Demographic and Health Survey (DHS) 2011; Bhutan, National Nutrition Survey 2015; India, National Family and Health Survey 2006; Maldives, DHS 2009; Nepal, DHS 2011; Pakistan, DHS 2013; and Sri Lanka, DHS 2007.
All peer‐reviewed IEC intervention studies on complementary feeding for infants and young children published between January 1990 and December 2015 for the eight South Asian countries included in our review: Research articles were identified through online search using PubMed (National Academy of Medicine and National Institutes of Health). We used as search term <complementary feeding> combined with <Afghanistan>, <Bangladesh>, <Bhutan>, <India>, <Maldives>, <Nepal>, <Pakistan>, <Sri Lanka>, and <Asia> and we applied the following search filters: language <English>; text availability <abstract>; species <human>; age range: <0–23 months>; and search fields: <title/abstract>. We only included IEC intervention studies that reported changes in complementary feeding practices as an outcome. We did not include IEC intervention studies on complementary feeding that focused on other outcomes (anthropometry, morbidity, or early childhood development for example) but did not report changes in complementary feeding practices. Similarly, we did not include studies that focused on the provision of single/multiple micro/macro nutrient supplementation with or without IEC.
3. FINDINGS
This section is organized as follows. First, we review the most recent national household surveys in South Asian countries to characterize current complementary feeding practices for infants and young children aged 6–23 months. Second, we review all relevant IEC intervention studies (1990–2015) to document the effectiveness of IEC interventions aiming to improve complementary feeding practices in children 6–23 months old in South Asia.
3.1. Complementary feeding of infants and young children 6–23 months old in South Asia.
The combined analytical sample included 30,966 children 6–23 months old with data on breastfeeding and complementary feeding practices. Our analysis indicates that most (87.5%) children 6–23 months old are breastfed. Breastfeeding rates in this age group are ≥75% in Bangladesh, India, Maldives, Nepal, Pakistan, and Sri Lanka, and they are ~60% in Afghanistan. Similarly, most children 6–23 months old (85.7%) are fed soft, semisolid, or solid complementary foods. Complementary feeding rates in this age group are ≥85% in all countries (Table 1; Figure 1).
Table 1.
Breastfeeding and complementary feeding in children aged 6–23 months by country in South Asia
| Afghanistan | Bangladesh | India | Maldives | Nepal | Pakistan | Sri Lanka | South Asia | |
|---|---|---|---|---|---|---|---|---|
| NNS 2013 | DHS 2011 | DHS 2006 | DHS 2009 | DHS 2011 | DHS 2012 | DHS 2007 | ||
| Breastmilk | 59.9 | 94.3 | 89.8 | 78.4 | 95.3 | 74.8 | 91.0 | 87.5 |
| Other milk | 24.8 | 48.0 | 67.2 | 43.9 | 49.3 | 50.6 | 46.0 | |
| Any solid or semisolid food | 87.3 | 84.9 | 97.7 | 92.3 | 87.2 | 96.9 | 85.7 | |
| Food made from grains | 76.7 | 75.1 | 77.2 | 96.2 | 88.1 | 72.2 | 95.5 | 76.8 |
| Fruits and vegetables rich in vitamin A | 36.8 | 34.4 | 65.5 | 34.6 | 19.3 | 79.7 | 33.2 | |
| Food made from roots and tubers | 51.0 | 41.1 | 22.6 | 20.2 | 65.0 | 41.5 | 56.4 | 28.6 |
| Other fruits and vegetables | 18.0 | 15.3 | 34.2 | 21.4 | 33.7 | 44.5 | 18.4 | |
| Meat, fish, poultry, eggs | 30.8 | 43.5 | 11.2 | 57.0 | 17.3 | 24.9 | 67.8 | 17.1 |
| Food made from pulses and nuts | 27.1 | 5.9 | 14.4 | 24.0 | 49.1 | 6.0 | 58.3 | 14.0 |
| Cheese, yogurt, other milk products | 6.6 | 11.1 | 41.8 | 9.0 | 13.6 | 27.9 | 11.2 | |
| Fortified baby foods | 5.3 | 15.8 | 51.9 | 7.9 | 15.3 | 34.6 | 14.9 | |
| Infant formula | 6.3 | 10.2 | 47.5 | 2.2 | 5.9 | 53.6 | 9.6 |
Note. NNS = National Nutrition Survey; DHS = Demographic and Health Survey.
Figure 1.
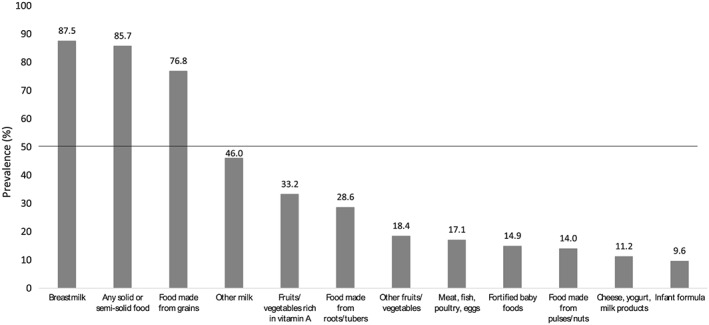
Proportion of South Asian children 6–23 months old who are fed different foods and food groups, 2006–2013
Foods made from grains are the main complementary food as an estimated 76.8% of children aged 6–23 months are fed cereal‐based complementary foods (range from 72.2% in Pakistan to 96.2% in the Maldives). The proportion of children who are fed any of the other food groups is below 50%. Only 1 child in 3 (33.2%) is fed fruits and vegetables rich in vitamin A (range from 19.3% in Pakistan to 79.7% in Sri Lanka), and fewer than 1 child in 5 (17.1%) is fed complementary foods containing meat, fish, poultry, and/or eggs (range 11.2% in India to 67.8% in Sri Lanka). Consumption of complementary foods containing pulses/nuts is a low 14% (range from 6% in Bangladesh and Pakistan to 58.3% in Sri Lanka) and so is the consumption of dairy products (11.2%; range from 6.6% in Bangladesh to 41.8% in the Maldives). An estimated 14.9% of children 6–23 months old is fed fortified complementary foods (range from 5.3% in Bangladesh to 51.9% in the Maldives), and 9.6% is fed infant formula (range from 2.2% in Nepal to 47.5% in the Maldives and 53.6% in Sri Lanka; Table 1; Figure 1).
We assessed complementary feeding practices in children aged 6–23 months using 7 globally accepted indicators for assessing complementary feeding practices (WHO 2008a; WHO 2008b; Table 2; Figures 2, 3).
Table 2.
Indicators of complementary feeding in children aged 6–23 months by country in South Asia
| BF12–15 | BF20–23 | CF6–8 | MMF | MDD | MAD | Fe‐rich | |
|---|---|---|---|---|---|---|---|
| Afghanistan (NNS 2013) | 63.2 | 38.1 | 41.3 | 52.1 | 27.6 | 12.2 | 32.6 |
| Bangladesh (DHS 2011) | 95.0 | 89.6 | 62.6 | 64.5 | 25.2 | 20.9 | 53.6 |
| Bhutan (NNS 2015) | 92.0 | 60.0 | 86.9 | 66.9 | 15.3 | 11.7 | 16.6 |
| India (DHS 2006) | 89.4 | 74.8 | 56.7 | 41.5 | 35.3 | 20.7 | 11.2 |
| Maldives (DHS 2009) | 77.3 | 68.4 | 81.8 | 73.8 | 72.2 | 57.6 | 57.0 |
| Nepal (DHS 2011) | 92.5 | 92.6 | 70.4 | 78.5 | 28.5 | 24.4 | 24.1 |
| Pakistan (DHS 2012) | 80.6 | 56.1 | 56.6 | 62.7 | 22.2 | 14.8 | 34.6 |
| Sri Lanka (DHS 2007) | 92.2 | 83.9 | 86.6 | 86.9 | 88.0 | 80.9 | 67.8 |
| South Asia | 88.1 | 73.1 | 57.4 | 47.7 | 33.0 | 20.5 | 19.4 |
Note. BF12–15 = continued breastfeeding at 1 year; BF20–23 = continued breastfeeding at 2 years; CF6–8 = introduction of solid, semisolid, or soft foods; DHS = Demographic and Health Survey; FE‐rich = consumption of iron rich foods; MAD = minimum acceptable diet; MDD = minimum diet diversity; MMF = minimum meal frequency; NNS = National Nutrition Survey.
Figure 2.
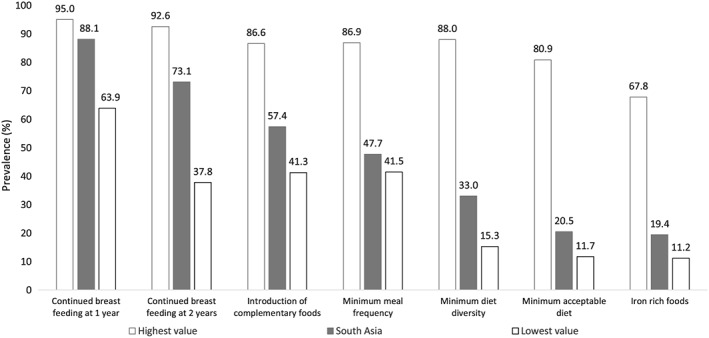
Complementary feeding practices in infants and young children 6–23 months old in South Asia, 2006–2013
Figure 3.
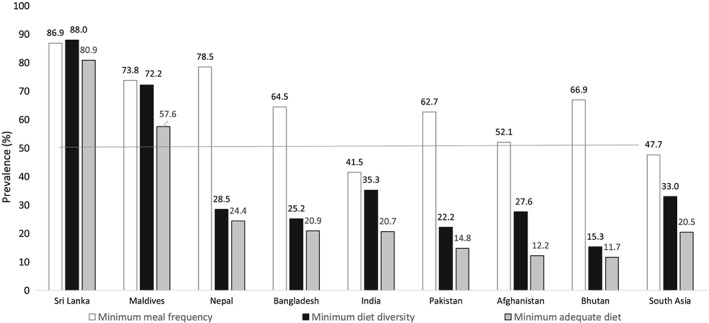
Complementary feeding practices in infants and young children 6–23 months old in South Asian countries, 2006–2013
3.1.1. Continued breastfeeding at 1 year
We estimate that 88.1% of children aged 6–23 months continue to be breastfed at 1 year of age. The proportion of infants aged 12–15 months who were fed breastmilk the day prior to the survey ranges from 63.2% in Afghanistan to 95.0% in Bangladesh. This proportion is ≥3/4 in all countries except Afghanistan.
3.1.2. Continued breastfeeding at 2 years
We estimate that 73.1% of children 6–23 months old continue to breastfeed at 2 years of age. The proportion of infants aged 20–23 months who were fed breastmilk the day prior to the survey ranges from 38.1% in Afghanistan to 92.6% in Nepal. This proportion is ≥2/3 in all countries except Afghanistan, Bhutan, and Pakistan.
3.1.3. Introduction of solid, semi‐solid or soft foods
We estimate that 57.4% of children 6–23 months old are fed soft, semisolid, or solid complementary foods in a timely manner. The proportion of infants 6–8 months who were fed soft, semisolid, or solid foods on the day prior to the survey ranges from 41.3% in Afghanistan to 86.6% in Sri Lanka. This proportion is ≥2/3 only in four countries: Bhutan, Maldives, Nepal, and Sri Lanka.
3.1.4. Minimum meal frequency
We estimate that 47.7% of children 6–23 months old are fed with a minimum frequency. The proportion of children 6–23 months of age who were fed soft, semisolid, or solid foods the minimum number of times or more during the day prior to the survey ranges from 41.5% in India to 86.9% in Sri Lanka. This proportion is ≥2/3 only in four countries: Bhutan, Maldives, Nepal, and Sri Lanka.
3.1.5. Minimum dietary diversity
We estimate that 33.0% of children 6–23 months old are fed diets that meet a minimum diversity. The proportion of children 6–23 months of age who were fed foods from four or more food groups during the day prior to the survey ranges from 15.3% in Bhutan to 88.0% in Sri Lanka. This proportion is ≥50% only in two countries: Maldives and Sri Lanka.
3.1.6. Minimum acceptable diet
We estimate that 20.5% of children 6–23 months old are fed diets that meet a minimum adequacy. The proportion of children 6–23 months of age who were fed a minimum number of times and a minimum number of food groups on the day prior to the survey ranges from 11.7% in Bhutan to 80.9% in Sri Lanka. This proportion is ≥50% only in two countries: Maldives and Sri Lanka.
3.1.7. Consumption of iron rich foods
We estimate that 19.4% of children 6–23 months old are fed iron‐rich foods. The proportion of children 6–23 months of age who were fed iron‐rich foods during the day prior to the survey ranges from 11.2% in India to 67.8% in Sri Lanka. This proportion is ≥50% only in three countries: Bangladesh, Maldives, and Sri Lanka.
3.2. Effectiveness of IEC interventions aiming to improve complementary feeding of children aged 6–23 months in South Asia.
The database search identified 81 publications with one or more of the search terms in the title and/or abstract. Studies were implemented in 6 of the 8 South Asian countries: Afghanistan (1), Bangladesh (21), India (29), Nepal (6), Pakistan (9), and Sri Lanka (3). In‐depth scrutiny of the titles of these 81 publications excluded 25 publications as not relevant to our review, identifying 56 publications as potentially relevant. In‐depth scrutiny of the abstracts of these 56 publications excluded 43 as not relevant to our review and identified 13 as likely relevant to our review. Full text scrutiny of the 13 publications excluded one as not relevant and identified 12 as relevant to our review. Two publications (Bhandari, Mazumder, Bahl, Martines, & Black, 2004; Bhandari, Mazumder, Bahl, Martines, & Black, 2005) referred to the same IEC intervention study, and one publication (Kimmons et al., 2004) reported findings of two IEC interventions. Thus, a total of 12 publications and 12 intervention studies were included in the review (Table 3).
Table 3.
Summary of intervention studies to improve complementary feeding practices through Information, Education, and Counselling
| Study | Country | Setting | Age group | Size | Type | Intervention | Timely introduction | Feeding quantity | Feeding frequency | Diet diversity | Other outcomes |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Aboud et al; 2008Maternal and Child Nutrition, 2008. | Bangladesh | Rural | 12–23 mo | 102 and 100 mother–child pairs in intervention and comparison groups, respectively | Cluster randomized field trial | Counselling on responsive feeding by peereducators. Intervention group 6 weekly sessions on responsive feeding. Control group 6 regular weekly sessions on child nutrition. | ‐ Improved diet diversity (eggs, fruit, vegetables).
‐ Less biscuits–sugar among children in theintervention group . |
‐ Improved mothers' knowledge on responsive feeding: percentage of self‐fed mouthfuls greater in intervention group but no difference in mean number of food mouthfuls per child. | |||
| Collison et al. (2015); Food Nutr Bull, 2015. | India(Bihar) | Rural–urban | 6–23 mo | 30 rural and 30 urban mother–child pairs | User testing: Trial of Improved Practices | 14‐day Trial of Improved Practices trial to test acceptability of low cost and easy to use feeding toolkit (bowl, spoon, and illustrated counselling card. Counselling provided by trained project assistants. | ‐ Improved initiation of complimentary feeding (CF) in infants 6–8 mo. | ‐ Average amount consumed per meal (feeding quantity) increased in all age groups. | ‐ Proportion of children consuming the recommended number of meals per day increased in all age groups. | ‐ Consumption of animal sources of food (meat or eggs) increased among children 6–11 mo. | |
| Kushwaha et al. (2014); PLoS One, 2014. | India (Uttar Pradesh) | Rural | 0–23 mo | 105,000 mother–child pairs | Quasi‐experimental before and after study over 5 years. | Infant and Young Child Feeding (IYCF) counselling to mothers by mother support groups (MSG) through facility‐ and community‐based outreach. Members of the MSG received a token amount of R. 50 per month for their services.
‐ Only 4 IYCF practices. 3 of them related to BF (initiation, exclusive, continued). |
‐ Initiation of CF feeding at T0, T2, and T5 were 54%, 85%, and 96%, respectively. | ||||
| Vazir et al. (2013); Maternal and Child Nutrition, 2013. | India (Andhra Pradesh) | Rural | 0–23 mo | 600 mother–child pairs (200 per comparison group) | Cluster‐randomized trial (12‐mo intervention) | Control group (CG) received routine ICDS services. CF group received ICDS + counselling on WHO recommendations on CF. Responsive CF and play group received same as the CFG + skills for responsive feeding and psychosocial stimulation. Both intervention groups received bi‐weekly visits by trained village women. | ‐ More children in intervention groups were fed liver, poultry, goat meat, egg, spinach, pulses, and added fat (at 9 and 15 mo).
‐ Despite intervention, liver, goat meat, poultry, and greens were fed to <30% of children across groups and eggs and added fat to ~50%. |
||||
| Bhandari et al. 2004; Health Policy and Planning, 2005.
Bhandari et al.; J Nutr, 2004. |
India(Haryana) | Rural | 0–23 mo | 1,025 newborns enrolled: 552 intervention group; 473 control group. | Cluster randomized controlled trial | 4 types of health and nutrition workers (traditional birth attendants, local village‐based workers, auxiliary nurse midwives, and primary care physicians) were trained to counsel mothers at multiple contacts on exclusive BF for the first 6 months and appropriate CF thereafter. The intervention included community and health worker mobilization. | ‐ Meal frequency was higher in the intervention communities at 9 and 18 months of age. | ‐ Significant improvement in consumption of cereal–legume gruels or mixes, milk–cereal gruels or milk–cereal mixes and of undiluted milk at 9 and 18 months in children in the intervention communities.
‐ Low consumption of milk and foods of animal origin. |
|||
| Zaman et al. (2008); J Health Popul Nutr, 2008. | Pakistan, (Lahore) | Urban | 6–23 mo | 375 mother–child pairs (129 pairs intervention and 137 pairs control) | Single‐blind cluster randomized controlled trial | Lady Health Visitors (LHV) were trained in nutrition counselling using IMCI's “Counsel the mother” module. A local adaptation of Pakistan's IMCI “feeding counselling card” was developed in the local language highlighting the recommended foods and frequency of feeding to be discussed with mothers according to the age of the child and to act a s a reminder at home of the recommendations received in the health center. Mother–child pairs were visited at home within 2 weeks, 45 days, and 180 days after recruitment | ‐ Mothers in intervention group were 1.5–3 times more likely to recall correct advice delivered during the consultation.
‐ After 180 days of consultation, the proportion of mothers reporting to offer eggs (47.6% vs 26.7%), chicken/beef/mutton (60.3% vs. 39.7%) or thick kitchuri (65.9% vs. 44.3%) to their children was significantly higher than in the comparison group (p ≤ .05). |
||||
| Brown et al. (1992) Am J Clin Nutr, 1992. | Bangladesh | Rural | 6–12 mo | 62 mother‐breastfed infant pairs in the intervention group and 55 in the comparison group. | Community‐based non‐randomized effectiveness trial. | Village workers hired by BRAC were trained in CF counselling to mothers, including home demonstrations of snack‐type recipes and instruction for enriching meals with energy, protein, and other nutrients. Messages encouraged continued BF in addition to frequent and persistent feeding of new foods, proper food storage, hand washing and washing of utensils before cooking and feeding. | ‐ After intervention, fish/meat consumption in intervention group (66%) was significantly higher than in comparison group (13%). | ||||
| Kilaru et al. (2005); Indian Paediatrics, 2005. | India (Karnataka) | Rural | 5–11 mo | 138 mother‐infant pairs (intervention group n = 69). | Nonrandomized controlled trial (sequential intervention/comparison groups) | Monthly nutrition education delivered by locally trained counsellors (hired by the project) targeted at caregivers of infants aged 5–11 months until 23 months of age. | ‐ Infants in the intervention group were more likely to be fed solids at least four times a day in addition to breastmilk (78% vs. 51%). | ‐ Infants in the intervention group were more likely to be fed a more diverse diet (42% vs. 19%) | ‐ Girls in the intervention group were more likely to report at least 4/6 positive behaviours than girls in the nonintervention group. No significant differences were observed for boys. | ||
| Kimmons et al. (2004); Food Nutr Bull, 2004. | Bangladesh | Rural | 6–12 mo | 30 mother‐infant pairs | Prospective short‐term behavioral change trial | Trial 1 (meal quantity trial): Educational messages to increase the quantity of food offered to and consumed by infants at each meal. Mothers were asked to feed their children more once mothers felt that the feeding session had ended. | ‐ Amounts consumed on days 5 and 7 were significantly greater than the amount consumed on day 1, and the duration of the meals significantly longer on days 4 and 7 vs. day 1.
‐ Mean intake from single meals increased from 40 +/− 23 g on day 1 to 64 +/− 30 g on day 7 (p < .05). ‐ Mothers increased the amount they fed their infants at a meal by 60% and they doubled the amount of time spent feeding at that meal. |
‐ Average meal frequency did not change significantly over the study period. | |||
| Trial 2 (meal frequency trial): Educational message to increase the frequency of complementary food meals. 30 mothers were asked to feed at least three meals per day, and more if possible. A meal was defined as a separate feeding of greater than 10 g. The study lasted for 7 days. No food was provided by the study team. | Meal frequency increased from 2.2 +/− 1.3 on day 1 to 4.1 +/− 1.3 on day 7.
‐ The percentage of mothers who cited time constraints to meal frequency decreased from 47% to 33%, the percentage citing lack of money decreased from 33% to 23%, and the percentage citing lack of food decreased from 13% to 7%. The percentage who responded that the baby did not want to eat more meals than the current level increased from 37% to 47%. |
||||||||||
| Aboud et al. 2009; J Nutr, 2009. | Bangladesh | Rural | 8–20 mo | 108 (intervention group) and 95 (comparison group) mother–child pairs | Cluster‐randomized trial | A 6‐session counselling program that emphasized the practice of responsive feeding to encourage mothers to feed their children in response to children's cues and psychomotor abilities vs. information and counselling delivered by the regular nutrition education programme. | ‐ Percent of self‐fed mouthfuls was 47.8 ± 42.4 in the intervention group compared to 32.2 ± 41.0 in the comparison group (p = .01)
‐ Number of responsive verbalizations was 6.55 ± 5.9 in the intervention mothers and 4.62 ± 4.5 in comparison mothers (p = .01). ‐ Mouthfuls of food eaten by children (self‐fed and mother‐fed) and weight gain were similar in the 2 groups. |
||||
| Roy et al. (2007); Food and Nutrition Bulletin, 2007. | Bangladesh | Rural | 6 to 9 mo | 605 normal and mildly undernourished children | Community‐based, randomized, controlled trial. | Nutrition and stimulation intervention vs. nutrition or stimulation only. Intervention group received weekly nutrition education for 6 mo. The control group received regular BINP services. Emphasis on demonstrations of the preparation of nutrient‐rich local complementary foods, and the prevention, recognition, and treatment of diarrhoea and acute respiratory infections. Community health workers–counsellors delivered the messages to small groups of mothers (6 to 8 mothers in each group). | ‐ Significant increase in the frequency of complementary feeding in the intervention group as compared with the control group (from 30.4% at baseline to 83.8% at end line vs 31% to 19.4% respectively) > The increase was sustained throughout the observation period. |
Six of the 12 intervention studies that met the inclusion criteria of our review were conducted in Bangladesh, five in India, and one in Pakistan. Ten intervention studies were implemented in rural areas, one in an urban setting, and one both in rural and urban areas. All studies included infants and young children 0–23 months old or subsets of this age group. Six studies focused on children in the age group 0–23 months; five studies focused on children aged 6–11 months; and one study focused on children 12–23 months old. The number of mother–child pairs included in the studies ranged from 30 to 1,025 in 11 of the 12 studies. Only one study (Kushwaha et al., 2014) included a larger number of mother–child pairs (n = 105,000). Studies included a variety of designs and methodologies. Six studies included a randomized design either at the individual or cluster levels, two had a nonrandomized design but included a comparison group, and four had a nonrandomized design and did not included a comparison group (i.e., before–after comparison).
IEC services were delivered by different types of providers, including peer educators, mother support groups, trained village women, trained project counsellors, traditional births attendants, village‐based workers, primary care physicians, community health workers, community counsellors, India's Auxiliary Nurse‐Midwives and Anganwadi Workers, and Pakistan's Lady Health Visitors among others.
Only two studies reported the impact of the IEC intervention on the timely introduction of complementary foods. Both intervention studies reported improvements in timely initiation of complementary feeding in infants although none of the intervention studies included a comparison group (Collison et al., 2015; Kushwaha et al., 2014). Similarly, only two studies reported the impact of IEC interventions on feeding quantity, documenting a positive effect of the IEC interventions on the quantity of complementary foods that children were fed per meal: the average amount of complementary food consumed per meal increased in all age groups (Collison et al., 2015), and mothers increased the amount they fed their infants at a meal and the amount of time they spent feeding their children at that meal (Kimmons et al., 2004).
Seven studies reported the impact of the IEC intervention on feeding frequency. Five studies reported that the proportion of children consuming the recommended number of meals per day increased in all age groups (Collison et al., 2015), that meal frequency was higher in the intervention communities at 9 and 18 months (Bhandari et al., 2004), that infants in the intervention group were more likely to be fed solids at least 4 times a day in addition to breastmilk (78% vs. 51%; Kilaru, Griffiths, Ganapathy, & Ghosh, 2005), and that at end line, the frequency of complementary feeding was significantly higher in the intervention group than in the control group (from 30.4% to 83.8% in the intervention group vs. 31% to 19.4% in the control group; Roy et al., 2007). In some instances, increases in feeding frequency were achieved after a short period of intervention. For example, Kimmons and colleagues report that daily meal frequency increased from 2.2 +/− 1.3 on day 1 to 4.1 +/− 1.3 on day 7 (p < 0.05; Kimmons et al., 2004; frequency trial). Only one study reported that the average meal frequency did not change significantly over the study period (Kimmons et al., 2004; quantity trial).
Seven studies reported the impact of the IEC intervention on diet diversity. The seven studies report improvements in children's average diet diversity scores in the intervention groups: children in the intervention groups were more likely to be fed a more diverse diet (42% vs. 19%; Kilaru et al., 2005), and IEC interventions contributed to improve the consumption of fruits and vegetables (Aboud, Moore, & Akhter, 2008) or cereal–legume and milk–cereal gruels or mixes (Bhandari et al., 2004). IEC interventions also contributed to increase the consumption of complementary foods from animal sources (eggs, liver, poultry, meat, and/or fish; Brown et al., 1992; Collison et al., 2015; Vazir et al., 2013). Zaman, Ashraf, and Martines (2008) report that 180 days after the counselling sessions, mothers in the intervention group were more likely than mothers in the comparison group to report to offer eggs (47.6% vs. 26.7%) or chicken, beef, and mutton (60.3% vs. 39.7%) to their children (p ≤ .05). However, despite improvements following the IEC intervention, children's consumption of milk and foods of animal origin was low (Bhandari et al., 2004). Vazir et al. (2013) report that foods of animal origin and/or eggs were fed to less than 30% to 50% of children across groups, respectively. Finally, some studies report that the IEC interventions improved responsive feeding (Aboud et al., 2008; Aboud, Shafique, & Akhter, 2009) and reduced gender differentials in feeding between girls and boys (Kilaru et al., 2005).
4. DISCUSSION
We reviewed the survey and research evidence available to characterize current complementary feeding practices for children 6–23 months old in South Asia and to review the effectiveness of IEC interventions aiming to improve complementary feeding in this age group.
We find that complementary feeding practices in South Asia are far from optimal. Less than 3 in 5 infants (57.4%) aged 6–8 months are fed soft, semisolid, or solid foods, indicating late initiation of complementary feeding for at least 2/5 of children.. Furthermore, less than half of children aged 6–23 months are fed with a minimum frequency per day and only about one‐third are fed diets that meet a minimum diversity. Complementary foods for children aged 6–23 months are primarily cereal‐based diets lacking, for a vast majority of South Asian children, the essential growth‐promoting nutrients provided by fruits and vegetables (only 1 in 3 children 6–23 months old is fed fruits and vegetables) and foods of animal origin (less than 1 in 5 children is fed meat, fish, poultry, and/or eggs).
These regional estimates are driven by the poor indicators of complementary feeding in Afghanistan, Bangladesh, India, Nepal, and Pakistan, the 5 highest population countries in the region, which also happen to be the countries with the largest proportion and number of stunted children in South Asia. Sri Lanka and Maldives stand out as outliers as indicated by children's higher consumption of fruits, vegetables, pulses, dairy, and foods of animal origin. In Sri Lanka, all indicators of complementary feeding—timeliness, minimum frequency, minimum diversity, and minimum adequacy—are above 80%, indicating that South Asian countries can be high performers on complementary feeding.
Our review of the potential effectiveness of IEC interventions to improve complementary feeding practices in South Asia is limited by the low number of intervention studies (n = 12), their emphasis on Bangladesh and India (11 of the 12 studies), their primary focus on rural areas (10 of the 12 studies), and the variety of outcomes that assessed and methodologies used. With these caveats in mind, the intervention studies we reviewed indicate that IEC delivered by peer educators, mothers support groups, trained counsellors, community health workers, primary health care staff, and others were able to improve the timeliness, frequency, diversity, and minimum adequacy of complementary feeding in children.
Authors highlight the importance of good practical skills on counselling and supervision, frequent counselling contacts, incentives for counsellors, and a supportive health system (Kushwaha et al., 2014). Frontline workers trained on counselling skills are more likely to discuss with mothers the foods that are more appropriate for the age of the child and check if the mothers have understood the information provided (Zaman et al., 2008). To achieve high coverage and wide adoption of recommended practices, many types of primary care workers and counselling at multiple opportunities seem essential (Bhandari et al., 2004). There is also evidence that using multiple and existing workers and opportunities for counselling caregivers is feasible, can result in high coverage and impact, and, instead of disrupting ongoing services, can improve them (Bhandari et al., 2005).
Although intervention studies indicate that IEC interventions can improve the consumption of micronutrient rich foods, social norms and time and/or financial resources may constraint the impact of IEC interventions. Mothers and caregivers may find counter to normative infant feeding beliefs that children aged 9 to 11 months need to be fed complementary foods of animal origin (Vazir et al., 2013). In addition, availability and affordability of such foods can also be a constraint to optimal complementary feeding. Mothers may be reluctant to feed young children foods of animal origin because of cost and, may tend to implement the IEC advice–messages that require little time and/or money and avoid to implement those that require more preparation time and/or are more expensive (Brown et al., 1992).
In summary, complementary feeding practices in South Asian children are characterized by late introduction of complementary foods, insufficient feeding frequency, and poor diet diversity. As a result, only 20% of children are fed diets that meet minimum levels of adequacy for appropriate child growth and development. This is of great concern given the high levels of child stunting in South Asia. Recent studies show that better complementary feeding practices predict better linear growth outcomes in South Asian children. In rural Bangladesh, children who were fed a minimum acceptable diet at 9 months had better height‐for‐age outcomes and were less likely to be stunted at age 24 months (Owais et al., 2016). In Nepal, minimum meal frequency and minimum diet diversity were positively associated with height‐for‐age in children 6–23 months. The combination of minimum meal frequency and minimum diet diversity had the greatest effect on indicators of child growth (Crum, Subedi, Mason, Mebrahtu, & Dahal, 2013). In India, poor dietary diversity was an important predictor of stunted growth in children (Corsi et al., 2015). For example, in Maharashtra, children 6–23 months old whose diets did not include eggs had a twofold higher risk of being stunted (Aguayo et al., 2016). In Bhutan, children aged 6–23 months who were not fed complementary foods at 6–8 months had about threefold higher odds of being severely stunted than children who were fed complementary foods (Aguayo, Badgaiyan, & Paintal, 2015).
The evidence on the potential effectiveness of IEC in improving complementary feeding practices in South Asia is limited in quantity, scale, and methodology. The small size of most of the intervention studies and the intensity of the training and supervision of community counsellors and health workers raises concerns with respect to the potential for scale and sustainability of some of these interventions. Recently published findings from a large‐scale intervention program in Bangladesh indicate that the combination of more intensive interpersonal counselling, mass media, and community mobilization (IPC + MM + CM intensive) brought about significantly higher improvements in complementary feeding indicators than a standard nutrition counselling + less intensive MM + CM (nonintensive) intervention. In the intensive group, Complementary Feeding (CF) practices were high: 50.4% for minimum acceptable diet, 63.8% for minimum diet diversity, 75.1% for minimum meal frequency, and 78.5% for consumption of iron‐rich foods. The authors conclude that large‐scale program delivery was feasible and, with the use of multiple platforms, reached 1.7 million households and claim that their study establishes proof of concept for large‐scale behavior change interventions to improve child feeding (Menon et al., 2016).
In conclusion, complementary feeding practices in South Asia are unacceptably poor to ensure that children can grow and develop to their full potential. The improvement of children's diets in the first 2 years of life needs to be an advocacy priority of national and international stakeholders who are concerned by the sustainable development of South Asian nations. Country governments need to ensure that national policies on Food and Nutrition Security and Maternal and Child Nutrition and Health are aligned with internationally agreed‐upon recommendations to protect, promote, and support age‐appropriate complementary foods and feeding practices for infants and young children. National governments and their development partners need to design, implement, and document evidence‐based, large‐scale programs for the promotion and support of improved complementary feeding for children aged 6–23 months. The scarcity of program monitoring and evaluation data in this area is of great concern. Finally, researchers need to be supported to document the main drivers of poor complementary feeding in South Asia and—importantly—the pathways to overcome barriers and constraints to the uptake of recommended complementary feeding practices by caregivers and families.
SOURCE OF FUNDING
United Nations Children's Fund (UNICEF) Regional Office for South Asia (ROSA) for data analysis, interpretation, and manuscript writing.
CONFLICTS OF INTEREST
The author declares that he has no conflict of interest. The opinions expressed on this paper are those of the author and do not necessarily represent an official position by UNICEF.
CONTRIBUTIONS
VMA designed the study and conducted data analysis and manuscript writing.
ACKNOWLEDGEMENT
The author wants to acknowledge the careful insights by the reviewers and the editorial team.
Aguayo VM. Complementary feeding practices for infants and young children in South Asia. A review of evidence for action post‐2015. Matern Child Nutr. 2017;13(S2):e12439 10.1111/mcn.12439
REFERENCES
- Aboud, F. E. , Moore, A. C. , & Akhter, S. (2008). Effectiveness of a community‐based responsive feeding programme in rural Bangladesh. A cluster randomized field trial. Maternal & Child Nutrition, 4(4), 275–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aboud, F. E. , Shafique, S. , & Akhter, S. (2009). A responsive feeding intervention increases children's self‐feeding and maternal responsiveness but not weight gain. Journal of Nutrition, 139(9), 1738–1743. [DOI] [PubMed] [Google Scholar]
- Aguayo, V. M. , & Menon, P. (2016). Stop stunting. Improving child feeding, women's nutrition and household sanitation in South Asia. Maternal & Child Nutrition, 12(1), 3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguayo, V. M. , Badgaiyan, N. , & Paintal, K. (2015). Determinants of child stunting in the Royal Kingdom of Bhutan. An in‐depth analysis of nationally representative data. Maternal & Child Nutrition, 11, 333–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguayo, V. M. , Nair, R. , Badgaiyan, N. , & Krishna, V. (2016). Determinants of stunting and poor linear growth in children under 2 years of age in India. An in‐depth analysis of Maharashtra's comprehensive nutrition survey. Maternal & Child Nutrition, 12(1), 121–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhandari, N. , Mazumder, S. , Bahl, R. , Martines, J. , & Black, R. E. (2004). Bhan MK; Infant Feeding Study Group. An educational intervention to promote appropriate complementary feeding practices and physical growth in infants and young children in rural Haryana, India. Journal of Nutrition, 134(9), 2342–2348. [DOI] [PubMed] [Google Scholar]
- Bhandari, N. , Mazumder, S. , Bahl, R. , Martines, J. , & Black, R. E. (2005). Bhan MK; Infant Feeding Study Group. Use of multiple opportunities for improving feeding practices in under‐twos within child health programmes. Health Policy and Planning, 20(5), 328–336. [DOI] [PubMed] [Google Scholar]
- Black, R. E. , Victora, C. G. , Walker, S. P. , Bhutta, Z. A. , Christian, P. , de Onis, M. , … Uauy, R. Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet, 2013; 382: 427–451. [DOI] [PubMed] [Google Scholar]
- Brown, L. V. , Zeitlin, M. F. , Peterson, K. E. , Chowdhury, A. M. , Rogers, B. L. , Weld, L. H. , & Gershoff, S. N. (1992). Evaluation of the impact of weaning food messages on infant feeding practices and child growth in rural Bangladesh. The American Journal of Clinical Nutrition, 56(6), 994–1003. [DOI] [PubMed] [Google Scholar]
- Collison, D. K. , Kekre, P. , Verma, P. , Melgen, S. , Kram, N. , Colton, J. , … Girard, A. W. (2015). Acceptability and utility of an innovative feeding toolkit to improve maternal and child dietary practices in Bihar. India. Food Nutr Bull, 36(1), 24–32. [DOI] [PubMed] [Google Scholar]
- Corsi, D. J. , Mejía‐Guevara, I. , & Subramanian, S. V. (2015). Risk factors for chronic undernutrition among children in India. Estimating relative importance, population attributable risk and fractions. Social Science and Medicine. 10.1016/j.socscimed.2015.11.014 [DOI] [PubMed] [Google Scholar]
- Crum, J. , Subedi, G. R. , Mason, J. , Mebrahtu, S. , & Dahal, P. (2013). Infant and young child feeding practices are associated with child nutritional status in Nepal. Analysis of the Nepal Demographic Health Survey, 2011 In Ministry of Health and Population and United Nations Children's Fund (UNICEF)). Nepal: Kathmandu. [Google Scholar]
- Daelmans, B. , Dewey, K. , & Arimond, M. (2009). New and updated indicators for assessing infant and young child feeding. Food and Nutrition Bulletin, 30, S256–S262. [DOI] [PubMed] [Google Scholar]
- de Onis, M. , & Branca, F. (2016). Childhood stunting. A global perspective. Maternal & Child Nutrition, 12(1), 12–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewey, K. G. (2016). Reducing stunting by improving maternal, infant and young child nutrition in regions such as South Asia. Evidence, challenges and opportunities. Maternal & Child Nutrition, 12(1), 27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewey, K. G. , & Begum, K. (2011). Long‐term consequences of stunting in early life. Maternal & Child Nutrition, 7, 5–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewey, K. G. , & Vitta, B. S. (2013). Strategies for ensuring adequate nutrient intake for infants and young children during the period of complementary feeding. Washington DC: Alive & Thrive. [Google Scholar]
- Kilaru, A. , Griffiths, P. L. , Ganapathy, S. , & Ghosh, S. (2005). Community‐based nutrition education for improving infant growth in rural Karnataka. Indian Pediatrics, 42(5), 425–432. [PubMed] [Google Scholar]
- Kimmons, J. E. , Dewey, K. G. , Haque, E. , Chakraborty, J. , Osendarp, S. J. , & Brown, K. H. (2004). Behavior‐change trials to assess the feasibility of improving complementary feeding practices and micronutrient intake of infants in rural Bangladesh. Food and Nutrition Bulletin, 25(3), 228–238. [DOI] [PubMed] [Google Scholar]
- Kushwaha, K. P. , Sankar, J. , Sankar, M. J. , Gupta, A. , Dadhich, J. P. , Gupta, Y. P. , … Sharma, B. (2014). Effect of peer counselling by mother support groups on infant and young child feeding practices: The Lalitpur experience. PloS One, 9(11): e109181. 10.1371/journal.pone.0109181 .eCollection 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leroy, J. F. , Ruel, M. , Habicht, J. P. , & Frongillo, E. A. (2014). Linear growth deficit continues to accumulate beyond the first 1,000 days in low‐ and middle‐income countries. Global evidence from 51 national surveys. Journal of Nutrition, 144, 1460–1466. [DOI] [PubMed] [Google Scholar]
- Menon, P. (2012). The crisis of poor complementary feeding in South Asia: Where next? Maternal & Child Nutrition, 8(1), 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon, P. , Nguyen, P. H. , Saha, K. K. , Khaled, A. , Sanghvi, T. , Baker, J. , … Rawat, R. (2016). Combining intensive counselling by frontline workers with a nationwide mass media campaign has large differential impacts on complementary feeding practices but not on child growth. Results of a cluster‐randomized program evaluation in Bangladesh. Journal of Nutrition. 10.3945/jn.116.232314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Multicenter Growth Reference Study Group. World Health Organization (WHO) child growth standards based on length/height, weight and age (2006). Acta Paediatrica, 95(Suppl 450), 76–85. [DOI] [PubMed] [Google Scholar]
- Owais, A. , Schwartz, B. , Kleinbaum, D. G. , Suchdev, P. S. , Faruque, A. S. G. , Das, S. K. , & Stein, A. D. (2016). Minimum acceptable diet at 9 months but not exclusive breastfeeding at 3 months or timely complementary feeding initiation is predictive of infant growth in rural Bangladesh. PloS One, 11(10): e0165128. 10.1371/journal.pone.0165128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy, S. K. , Jolly, S. P. , Shafique, S. , Fuchs, G. J. , Mahmud, Z. , Chakraborty, B. , & Roy, S. (2007). Prevention of malnutrition among young children in rural Bangladesh by a food‐health‐care educational intervention: A randomized, controlled trial. Food and Nutrition Bulletin, 28(4), 375–383. [DOI] [PubMed] [Google Scholar]
- Smith, L. , & Haddad, L. (2014). Reducing child undernutrition. Past drivers and priorities for the post‐MDG era. World Development, 68, 180–204. [Google Scholar]
- United Nations Children's Fund (UNICEF) (2015). The state of the world's children. New York, New York: UNICEF, 2015. [Google Scholar]
- United Nations Children's Fund (UNICEF) South Asia (2015). Stop Stunting in South Asia. A Common Narrative on Maternal and Child Nutrition. UNICEF South Asia, Strategy 2014–2017 In UNICEF Regional Office for South Asia). Nepal: Kathmandu. [Google Scholar]
- United Nations Children's Fund (UNICEF), World Health Organization (WHO), World Bank Group (WBG) (2017). Levels and trends in child malnutrition. Joint child malnutrition estimates In UNICEF, WHO, World Bank Group. New York: Ney York. [Google Scholar]
- Vazir, S. , Engle, P. , Balakrishna, N. , Griffiths, P. L. , Johnson, S. L. , Creed‐Kanashiro, H. , … Bentley, M. E. (2013). Cluster‐randomized trial on complementary and responsive feeding education to caregivers found improved dietary intake, growth and development among rural Indian toddlers. Maternal & Child Nutrition, 9(1), 99–117. 10.1111/j.1740-8709.2012.00413.x. epub 2012 May 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora, C. G. , Adair, L. , Fall, C. , Hallal, P. C. , Martorell, R. , Richter, L. , et al. (2008). Maternal and child undernutrition. Consequences for adult health and human capital. Lancet, 371, 340–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) (1998). Complementary feeding of young children in developing countries. A review of current scientific knowledge. Geneva, Switzerland: WHO. [Google Scholar]
- World Health Organization (WHO) (2008a). Indicators for assessing infant and young child feeding practices. Part I: Definitions Geneva, Switzerland: WHO. [Google Scholar]
- World Health Organization (WHO) (2008b). Indicators for assessing infant and young child feeding practices. Part II: Measurement Geneva, Switzerland: WHO. [Google Scholar]
- World Health Organization (WHO) (2012). Resolution WHA65.6. Maternal, infant and young child nutrition In Sixty‐fifth World Health Assembly, Geneva, 21–26 May. Resolutions and decisions, annexes (WHA65/2012/REC/1)). Geneva. Switzerland: WHO. [Google Scholar]
- World Health Organization (WHO) (2015). Global nutrition targets. Stunting policy brief (WHO/NMH/NHD/14.3). Geneva, Switzerland: WHO. [Google Scholar]
- Zaman, S. , Ashraf, R. N. , & Martines, J. (2008). Training in complementary feeding counselling of healthcare workers and its influence on maternal behaviours and child growth: A cluster‐randomized controlled trial in Lahore, Pakistan. Journal of Health, Population and Nutrition, 26(2), 210–222. [PMC free article] [PubMed] [Google Scholar]


