Abstract
Global recognition that the complex and multicausal problems of malnutrition require all players to collaborate and to invest towards the same objective has led to increased private sector engagement as exemplified through the Scaling Up Nutrition Business Network and mechanisms for blended financing and matched funding, such as the Global Nutrition for Growth Compact. The careful steps made over the past 5 to 10 years have however not taken away or reduced the hesitation and scepticism of the public sector actors towards commercial or even social businesses. Evidence of impact or even a positive contribution of a private sector approach to intermediate nutrition outcomes is still lacking. This commentary aims to discuss the multiple ways in which private sector can leverage its expertise to improve nutrition in general, and complementary feeding in particular. It draws on specific lessons learned in Bangladesh, Côte d'Ivoire, India, Indonesia, and Madagascar on how private sector expertise has contributed, within the boundaries of a regulatory framework, to improve availability, accessibility, affordability, and adequate use of nutritious foods. It concludes that a solid evidence base regarding the contribution of private sector to complementary feeding is still lacking and that the development of a systematic learning agenda is essential to make progress in the area of private sector engagement in nutrition.
Keywords: case studies, complementary feeding, evidence, infant nutrition, private sector, regulatory framework
1. INTRODUCTION
Over 3 m annual child deaths are due to malnutrition (45% of all deaths in children), with poor complementary feeding being one of the significant drivers of infant and child malnutrition and mortality globally (Black et al., 2013). Using locally available and culturally acceptable foods lies at the basis of the complementary diet for older infants and young children. Evidence suggests, however, that substantial constraints exist to ensuring a nutrient adequate diet because of ingredient availability, time, and cost constraints. Even where economic barriers can be overcome, the adequacy of some nutrients may be difficult to achieve using only local ingredients (Osendarp et al., 2016).
The Pan American Health Organization and the World Health Organization (WHO), in their guiding principles for complementary feeding of the breastfed child (PAHO and WHO, 2003, World Health Organization 2003), have recognized that alternative ways to fill nutrient gaps in local complementary foods are needed, and could be provided through fortified complementary foods (FCF) or home fortification of locally made complementary foods with multiple nutrient powders (MNPs). Four years later, in 2008, a WHO‐UNICEF consultation concluded inter alia, “Where locally available foods alone will not satisfy nutritional requirements, various types of products offer promise. They may include centrally produced fortified foods, micronutrient powders, and lipid‐based nutrient supplements. Further research and carefully monitored applications at scale are needed to generate more evidence on which product is best for which circumstance, how best to promote their correct utilization, and their contribution to improving nutritional, developmental and health status in different circumstances” (World Health Organization and United Nations Children's Fund, 2008).
It is the private sector, be it small farmers or large food processors, which produces the locally available foods and the centrally produced fortified foods. Yet, the Global Nutrition Report (International Food Policy Research Institute, 2015) indicates that there is very limited, independently generated, evidence of impact of public–private partnerships on reducing child malnutrition. This is no surprise as public–private sector collaboration to improve infant and young child feeding of low‐income populations is relatively recent, with few examples for impact. In addition, the involvement of private sector in infant feeding is extremely sensitive due to inappropriate marketing and noncompliance of companies with the International Code of Marketing of Breast Milk Substitutes (World Health Organisation, 1981).
So, what has been done to fill the gap in availability and affordability of nutritious complementary foods and supplements (CFS) for low‐income consumers? Over the past 10 years, a number of commercial and partly subsidized solutions have been developed (Afsana, Haque, Sobhan, & Shahin, 2014; Bruyeron, Denizeau, Berger, & Trèche, 2010; Global Alliance for Improved Nutrition, 2015a; Global Alliance for Improved Nutrition, 2015b; Kayser, Klarsfeld, & Brossard, 2014; Nguyen et al., 2016; Reerink, 2014). Little is known however about the successes and failures of these experiences or their impact on nutrition indicators. This commentary is a first attempt to review some lessons learned on private sector engagement in child nutrition, on the basis of a number of case studies.
2. METHODS
Private sector expertise and capacity is mainly leveraged for production, distribution, and demand creation (ensuring improved availability, quality, accessibility, delivery, uptake, and affordability) of nutritious CFS (Figure 1). But it is the mandate of public sector to set the boundaries and create an enabling environment that protects the consumer (i.e., the child) and guides private sector to comply with policies, nutrition standards, and appropriate marketing guidelines. Only if the interplay between these two sectors is in balance, will there be a potential impact of private sector engagement on adequate use of the nutritious food or supplement and ultimately on nutritional status.
Figure 1.
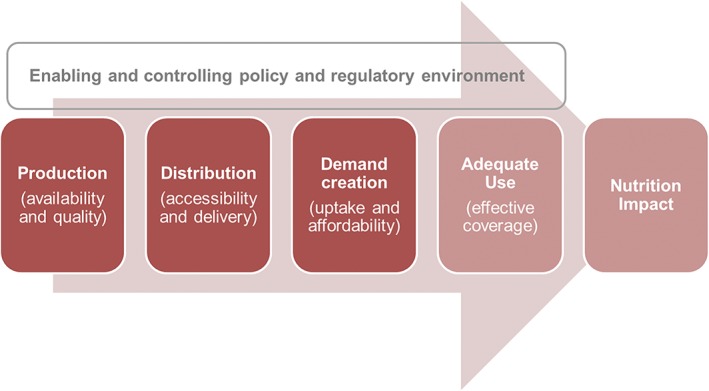
Conceptual framework for private sector engagement in infant and young child nutrition
The conceptual framework in Figure 1 has been used to review a number of case studies, mainly published in grey literature.
The Global Business School Network carried out an external review of five GAIN case studies, predominantly demonstrating contributions to availability and quality of CFS, accessibility and delivery, affordability, but less so on uptake of products by the target groups or appropriate use (Global Alliance for Improved Nutrition, 2014a; Global Alliance for Improved Nutrition, 2014b; Global Alliance for Improved Nutrition, 2014c, Global Alliance for Improved Nutrition, 2014d; Global Alliance for Improved Nutrition, 2014e). These five case studies were incorporated in the documentation of lessons learned, across 17 countries between 2008 and 2014 (Global Alliance for Improved Nutrition, 2015a; Global Alliance for Improved Nutrition, 2015b). Coverage and consumption of FCF was estimated in two of these projects (Leyvraz, Wirth, et al, 2016; Leyvraz, Rohner, et al., 2016).
Kayser et al. (2014) reviewed the business models of seven projects, of which six aimed to increase accessibility through commercial sales of nutritious CFS for 6–24 month old infants to low‐income families in developing countries. Lessons were drawn regarding the importance of value proposition, promotion and compliance strategies, effectiveness and efficiency of distribution strategies, and the sustainability of these various models. For each case study, information is included with regard to sales or coverage, price, but very limited information was provided with regard to effective use of the products or nutrition impact.
The experience of GRET, a French NGO and its Nutridev initiative in Burkina Faso, Madagascar and Vietnam, was reviewed with regard to the feasibility of local production, marketing, and distribution of FCF to increase usage of high‐quality foods among children of low‐income families in a self‐sustaining manner (Bruyeron et al., 2010). Production and sales are reported, but no data were available with regard to coverage and consumption of the products.
A few examples of social marketing or micro franchise approaches to deliver home fortification with MNPs have been reviewed, including Bangladesh, Madagascar, and Vietnam (Afsana et al., 2014; Nguyen et al., 2016; Reerink, 2014). Sales data and any coverage are available, but information on effective use of MNPs is not available for Madagascar or Vietnam. Contact coverage and effective coverage (respectively, any use and use of 60 MNP sachets in 6 months) are being monitored closely in Bangladesh but not yet published (Khondker, 2016).
Lessons from these case studies have been categorised according to the elements of the conceptual framework and are summarised below (Figure 1).
3. PRODUCTION: AVAILABILITY AND QUALITY
The case studies show that it is feasible to produce high‐quality and acceptable CFS for the target population, children 6–23 months (Bruyeron et al., 2010; Global Alliance for Improved Nutrition, 2015a; Kayser et al., 2014). Nevertheless, small and medium size local companies in low‐income countries are facing considerable barriers to produce high‐quality nutritious food products because their capabilities in sourcing of raw materials, defining product composition, manufacturing, quality assurance, and control are limited. Moreover, their ability to comply with mandatory regulations and product standards is often nonexistent. This is further complicated by the fact that global guidance (Codex Alimentarius, 1991; World Health Organization, 2011) and national product standards are not always aligned. In all case studies reviewed, this barrier was easily overcome by providing technical assistance to the local companies, which helped to improve nutritional quality of the product and apply appropriate food safety measures, as illustrated in the India case study (Box 1).
Box 1 India case study: government‐owned industry produces for Integrated Child Development Services (ICDS).
Andrah Pradesh Foods is a government‐owned company, based in Hyderabad, which produces amongst others fortified supplementary food called Bal Amrutham distributed for free to children 6–36 months and pregnant and lactating women in the ICDS. Between 2010 and 2014, AP Foods worked together with GAIN to improve the nutritional quality of the product (e.g., taking out vanaspati, thus eliminating trans fats, and fortification with micronutrients), packaging improvements leading to increased shelf life and a more attractive product. The partnership acted as a catalyst for a substantial financial investment by the state government in a new production facility, enabling AP Foods to increase reach from 60% to 100% of the community centres, reaching 3 million people with nutritious food take‐home rations. Though government‐owned, the business‐centred approach of AP foods has led to improved quality of product and packaging, increased efficiencies, and increased reach.
(Global Alliance for Improved Nutrition, 2014a).
Whether the available CFS will reach the intended target groups, at scale, and in a sustainable manner, really depends on the viability of the business case. Review of the various business models (Kayser et al., 2014) disclosed that bringing nutritious CFS for low‐income consumers to the market is not necessarily a profit‐making activity. Ingredients and packaging of high quality come at a cost, whereas the price per unit needs to remain affordable for those populations most in need. Sustainability of a nutritious foods business can only be achieved when reaching scale of production and sales. This is extremely challenging with sales through retail or microfranchise channels, without access to the institutional market, as demonstrated in the Côte d'Ivoire case study below (Box 2). A viable business case, based on a market and competitor analysis, requires a minimum level of demand.
Box 2 Côte d'Ivoire case study: Nutritional quality and food safety come at a cost.
Protein Kissée‐La (PKL), a local Ivorian company, is an established player in the market of baby porridges and is not a formula producer. Its Farinor brand has enjoyed strong brand equity for the past 20 years. PKL wished to improve the nutritional quality of the product, aligned with the revised Codex Alimentarius standards (Codex Alimentarius, 1991) while at the same time redesigning a higher quality packaging to improve overall shelf‐life, food safety, and quality. Affordability to rural and lower income consumers was also a key priority, with the original 50 g sachet price set at $0.25 per two serving pack, filling a niche in the market.
However, capital expenditures including import, equipment, electricity, and construction costs came at a higher than expected cost in post‐civil war Côte d'Ivoire. The prioritisation of quality, which called for higher priced inputs, resulted in a negative profit margin. In order to be able to keep the product in the market and to ensure sustainability, PKL had to (a) increase the price of the product while still remaining the cheapest fortified product on the market; (b) accept a later break‐even point (about 6 years in the future), that is, the moment when investments are being recovered and real profit starts being made; and (c) to cross subsidise the production of the product with its other profit‐making business category, thereby increasing the risk for the entire company. Because of the low profit margin, cash flow was limited resulting in limited investments in demand creation, which in its turn, inhibited uptake by retailers and limits market growth. For small local businesses such as PKL, it is challenging to bring a high‐quality product to the market that is affordable to the neediest of consumers, without access to a mass market (e.g, institutional demand) to reach market sustainability.
(Global Alliance for Improved Nutrition, 2014b; Kayser et al., 2014)
4. DISTRIBUTION: ACCESSIBILITY AND DELIVERY
Reaching the targeted low‐income populations is an equal challenge for public sector and private sector, as the reviewed case studies confirmed. Free delivery through public health systems (see India ICDS case study) offers equitable access, but these systems often experience challenges in capacity, capability, supply, and monitoring systems. In many developing countries, commercial retail markets are immature and sometimes even nonexistent, especially in rural areas. Moreover, commercial distributors and retailers take a profit margin on the final product price, which is about 10% for large established players and up to 40–50% for small players (personal communication). This difference can be explained by the business risk of less known products not selling fast and taking up shelf space, whereas well‐known brands have larger sales volumes thanks to more intense marketing efforts.
To reach the intended target groups with nutritious CFS therefore requires innovation and exploration of multiple and new delivery channels, which are not purely commercial but rather based on social marketing or microfranchising models. Kayser et al. (2014) concluded that in rural and more mature markets, traditional retail would be the most cost‐effective delivery channel for nutritious products; where as in densely populated urban areas, a door‐to‐door sales force could also create demand and build client loyalty. The case studies on MNP delivery against payment in Madagascar, Vietnam, and Bangladesh (Afsana et al., 2014; Nguyen et al., 2016; Reerink, 2014) provide additional lessons. In Vietnam, the National Institute of Nutrition pioneered the distribution of MNPs provided for sale through the public health system. The pilot showed that the sale of MNPs and the provision of infant and young child‐feeding counselling are effective for groups accessing the health system. Following the success of the pilot, the government of Vietnam has now included the scale up of MNPs in their National Nutrition Strategy (Nguyen et al., 2016). The Bangladesh case study in Box 3 shows the success of building on an existent large distribution network that covers hard‐to‐reach rural populations in achieving sales as well as effective use at scale.
Box 3 Bangladesh case study: selling MNP's by 49,000 BRAC community workers.
In Bangladesh, BRAC, the largest NGO in the world, distributes and sells “Pusthikona”: a locally produced MNP, through its large network of frontline community workers (Shastya Shebikas). These local BRAC agents are often viewed as the most trusted reference point in their village. In addition to promoting and selling a basket of health care products, they provide free services to the other community members, including promotion of hygiene and nutrition practices. The Shastya Shebikas play a critical role in promoting optimal complementary feeding practices for children 6 to 24 months of age; for which, MNPs can be one of the options. When the pilot project showed disappointing results of uptake and effective use of MNP's, a monthly monitoring tool was developed to allow rapid data analysis and course correction. Stock and supply mechanisms have been strengthened to avoid stock out. Counselling skills and sales techniques of the frontline workers have been improved through monthly refresher training, and an incentive system has been implemented to encourage repeat sales of MNP's and adequate use of MNPs by target children in the households. Monthly sales have increased ninefold between 2014 and 2016. The uptake through the traditional network of doctors and pharmacists of the MNP producer, Renata Pharmaceuticals, has proven less effective than the microfranchised approach of BRAC.
5. UPTAKE AND AFFORDABILITY
With high‐quality nutritious CFS available, the target consumer will still need to be motivated and able to try and use them. Behavior change communication or demand creation activities are driving this (or in private sector terms: marketing and promotion). Awareness raising alone is not sufficient however, if the price is too high or if the consumer is not motivated.
Low‐income consumers are cash constrained and have low purchasing power, thus the absolute price of a product is important. Results for Development Institute (2013) estimated that 0.03 USD for one MNP sachet seems affordable across most countries. Most of the MNP case studies cited have executed willingness‐to‐pay studies with consumers in order to identify the optimal price point that supports a viable business case and is affordable for low‐income households.
Kayser et al. (2014) state that price is not the only driver of demand and that low‐income consumers are not just looking for cheap products, but are ready to pay for CFS that offer them a relevant benefit in terms of value‐for‐money. The benefits or value proposition for consumers in terms of product, packaging, brand, and price are important demand factors that trigger the first trial of a product. Sometimes, these are more important demand drivers than the longer term health benefits. Caregivers are looking for short‐term rewards and reasons to procure and use specialized products. A good example of this is the Nutrizaza project in Madagascar that tapped into the convenience factor by offering ready‐to‐eat fortified porridges to mothers in the urban slums of Antananarivo, delivered at home or at a baby restaurant (Bruyeron et al., 2010; Kayser et al., 2014).
Although insights into the motivations of consumers can be used successfully to drive demand for a product, any statement or claim made to persuade the consumer needs to be truthful. Claims concerning health benefits or nutrient content need to be able to withstand scientific scrutiny (see below in enabling and controlling policy and regulatory environment).
5.1. Adequate use and effective coverage
Little information is available in the case studies on appropriate use and effective coverage.
Two consumption surveys have been published that determine the coverage of fortified supplementary foods, linked to the India and the Côte d'Ivoire case studies (Boxes 1 and 2). Awareness and any consumption of the fortified take‐home rations were very high (94% and 87%, respectively) in the India study, whereas 57% of the target children consumed the food every day (Leyvraz, Wirth, et al., 2016). This is tenfold higher than the national average of target children consuming the take‐home ration, which was estimated at 5.6% (International Institute for Population Sciences, IIPS and Macro International, 2007).
In the Côte d'Ivoire study, a high percentage of caregivers (85%) had heard of the PKL‐branded products, and a high proportion of the children 6–23 months (70%) had been given any fortified complementary food of which more than 50% was the PKL product. Regular utilisation of the PKL products (i.e., at least once per week), however, was low (5%). There was no difference in regular utilisation between poor and nonpoor (Leyvraz, Rohner, et al., 2016).
These two examples demonstrate that awareness and any coverage are insufficient indicators if one wishes to establish nutrition impact. Even when sales of nutritious CFS are high, impact on nutritional status of the target population will depend on the quantity and frequency that a target individual will consume. The same is true for public sector interventions, where often reach is reported but information on who was reached and how much was consumed is not being collected.
Getting the consumers to use a product as per recommendation requires specific attention and targeted interventions. In the Bangladesh case study (Box 3), a steady and considerable increase in sales of MNPs has taken place over the past 2 years. By August 2016, sales have reached 3.9 million sachets per month (from 420,000 in August 2014), with total contact coverage of 1,272,656 children. It is estimated that 258,045 children have consumed the effective course of 60 sachets over 6 months since September 2014. To increase effective use, we find that the community workers are receiving a financial incentive for every child that has consumed 60 MNP sachets over the course of 6 months. Behavior change tools have also been developed such as a calendar and stickers, which remind the mother of giving the child one MNP sachet every 2nd day (Khondker, 2016).
5.2. Enabling and controlling policy and regulatory environment
Whereas, the case studies reviewed in this commentary demonstrate that subsidised or hybrid market‐based approaches can help to increase access to nutritious CFS, there is at the same time a critical need to set the boundaries in which they can operate. This includes amongst others normative guidance on product composition, product claims, and on marketing and promotion of nutritious food products and supplements.
Although every country has its own set of national food and nutrition labeling regulations, at international level, it is the Codex Alimentarius that provides guidance to governments on food product standards, nutrition labeling, claims, and use of health and nutrition claims. The revision of the Codex guidelines on formulated complementary foods for older infants and young children was published after a five‐year‐long process involving many technical experts to incorporate scientific evidence that emerged over the past 20 years (Codex Alimentarius, 1991, Global Alliance for Improved Nutrition 2016). Following this revision, there is a need to translate the guidance to the country context, as the example of Indonesia points out (Box 4).
The need for regulation and enforcement of regulation is painfully evident from the fact that infant formula producers continue to violate the International Code on Marketing of Breast Milk Substitutes (World Health Organisation, 1981). In the absence of guidance on marketing of complementary foods, this malpractice has influenced the debates on promotion of complementary foods, leading in some countries to a grey area on what was allowed and in others to prohibition of any marketing of any food for children under 2 years. This situation has considerably improved with the adoption by the World Health Assembly of a resolution to provide guidance on ending the inappropriate promotion of foods for infants and young children (World Health Organization, 2016). A scientific and regulatory advisory group had worked 4 years to compile evidence, which informed the guidance note.
The government's role in creating a regulatory environment is vital in defining product standards, ensuring appropriate promotion of CFS and ending inappropriate promotion, thereby ensuring a level‐playing field for the private sector. In the same way as governments sometimes require technical support to translate international guidelines to the national context, do small and medium sized enterprises need help to understand how to comply with national regulations and standards.
Box 4 Indonesia case study: role of government in setting boundaries for private sector.
Whereas, the global Codex Alimentarius standards for formulated complementary foods have been revised in 2013, based on a thorough review of scientific evidence, product standards in many countries still need to be updated. In Indonesia, the authorities accept that commercial complementary foods are available in the market and are being used by mothers but that a strong regulatory framework is required to ensure that breastfeeding is protected and that these products are adequately formulated. Discrepancies between the revised Codex Alimentarius and Indonesia guidance included fortification levels of some micronutrients, and the portion size, which under the Indonesia standard, was so large that it could lead to displacing breastfeeding. Cognisant of these issues, the Directorate of Nutrition under the Ministry of Health (Kemenkes), convened a meeting in October 2015, bringing together the Indonesian Food and Drugs Monitoring, academic experts, nutrition partners, and representatives of food companies, to agree on a process to review the Indonesia standard in the context of the Codex Alimentarius revisions, 2013. As a result of that meeting, Kemenkes plans to issue new national guidelines in 2017 on both the composition and portion sizes of fortified complementary food in order to align with WHO and Codex Alimentarius guidelines.
(Personal communication R. Menon, Country Director GAIN Indonesia)
6. DISCUSSION
There is an increasing set of experiences on private sector approaches, as this paper demonstrates, but progress on making quality CFS available and affordable is slow. Why is progress in this area stuck?
There are very few publications, peer‐reviewed or in grey literature, or well‐designed studies that provide rigorous evidence regarding the contribution of private sector to nutrition, and most specifically regarding the uptake and use of these products. Many questions remain unanswered: Are these products reaching the intended target groups, the most vulnerable, and are they being consumed, in sufficient quantity and frequency to potentially have a nutrition impact? Are commercial CFS having a negative impact on breastfeeding? Are CFS needed to complement the consumption of locally grown foods or will they replace them in the long run? Will the profit motive of business not surpass the social or nutrition objective? To answer these questions, a structured learning agenda needs to be developed. The indicators and research methods to measure market‐based access to CFS and impact on feeding practices and nutritional status need to be defined. However, market penetration and regular consumption of products take years to achieve, which makes it challenging to measure nutrition outcomes and impact, especially linear growth, in a market‐based setting where most variables cannot be controlled.
Without evidence, it is challenging to overcome the lack of trust between the two sectors. Principles of engagement for public–private or multi‐stakeholder partnerships that can help to create trust have been defined by many such as the Engagement Principles of the Scaling Up Nutrition Movement (Scaling Up Nutrition Movement, 2016) or principles for public–private partnerships in food and nutrition research (Alexander et al., 2015). Important similarities are found across these sets of principles with regard to being transparent on intent and impact, transparent in communication, defining common public (health) objectives, being rights based and inclusive, and avoiding or managing conflicts of interest. Transparent communication around the intent and impact of private sector engagement in the production and distribution of CFS will be fundamental to build trust for market‐based approaches.
The lack of well‐designed studies and hard evidence was an important limiting factor for this paper. Nonetheless, on the basis of the reviewed case studies, a number of critical determinants of success were identified for market‐based approaches to increase access to CFS for infants and young children.
Local small‐ and medium‐sized food companies require technical assistance from a credible technical agency to de‐risk their investments in producing and marketing CFS.
A viable business model for CFS requires access to institutional markets to complement the initial low demand through retail or sales force channels
CFS must be delivered through channels, which are close to the target population and make it easy to procure them.
Relevant consumer benefits, including those that are not nutrition or health related, can be used as aspirational drivers to create demand.
Effective use or coverage of CFS needs to be monitored regularly as overall reach or sales does not give any indication about potential nutrition impact.
Special interventions are needed to go beyond awareness raising and encouraging any use, towards inciting effective (regular) use of CFS.
Technical expertise can help to provide clarity to private sector and governments around international and national normative guidance on food standards and promotion of CFS, thus creating a level‐playing field for private sector.
In conclusion, although private sector strengths to innovate, drive efficiency and scale, hold promise to contribute to improved availability, accessibility, and affordability of nutritious CFS for vulnerable groups, there is insufficient solid evidence to support this. To move this area forward, we find that it is crucial to develop a structured learning agenda, with agreed indicators for success, and overcome the barriers of doing research in an uncontrolled market setting.
Technical backbone organisations can play a fundamental role and bring the various private and public sector players together around one common goal, while creating transparency around the noncommon goals. With their understanding of the political, scientific, and nutrition programmatic environment, such organisations can help business to design an effective approach, support governments in establishing an enabling regulatory environment, and work with the research community to ensure the implementation of a rigorous learning agenda.
SOURCE OF FUNDING
GAIN received funding from the Bill & Melinda Gates Foundation, the Children's Investment Fund Foundation, and the Government of the Netherlands for its Infant and Young Child Nutrition Global Program, including the referenced projects in Bangladesh, Cote d'Ivoire, India, and Indonesia.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest. AP Foods is a government‐owned company without shareholders.
CONTRIBUTIONS
ML wrote the manuscript; RM, MY, and IR presented their case studies at the First Foods meeting and provided the case study input for this paper; and DT contributed to writing and reviewing the entire manuscript and provided the references.
ACKNOWLEDGEMENT
We would like to thank UNICEF for the organisation of First Foods, a global meeting to accelerate progress on complementary feeding in young children, in Mumbai, November 2015, which allowed the authors to present their case studies and prepare this paper.
van Liere M J, Tarlton D, Menon R, Yellamanda M, Reerink I. Harnessing private sector expertise to improve complementary feeding within a regulatory framework: Where is the evidence? Matern Child Nutr. 2017;13(S2):e12429 10.1111/mcn.12429
Footnotes
For the sake of this simplified conceptual framework, sourcing of raw ingredients is not included.
Appropriate use is the use of the food product as recommended. Effective coverage refers to the number of percentage of the population group having consumed the product as per recommendations for nutrition impact.
Contact coverage is defined as those children having used MNPs at least once.
REFERENCES
- Afsana, K. , Haque, M. R. , Sobhan, S. , & Shahin, S. A. (2014). BRAC's experience in scaling‐up MNP in Bangladesh. Asia Pacific Journal of Clinical Nutrition, 23(3), 377–383. [DOI] [PubMed] [Google Scholar]
- Alexander, N. , Rowe, S. , Brackett, R. E. , Burton‐Freeman, B. , Hentges, E. J. , Kretser, A. , … Ohlhorst, S. (2015). Achieving a transparent, actionable framework for public‐private partnerships for food and nutrition research. American Journal of Clinical Nutrition, 101(6), 1359–1363. [DOI] [PubMed] [Google Scholar]
- Black R.E., Victora C.G., Walker S.P., Bhutta Z.A., Christian P., de Onis M.., … The Maternal and Child Nutrition Study Group (2013). Maternal and child undernutrition and overweight in low‐income and middle‐income countries, Lancet 380: 427–451. [DOI] [PubMed] [Google Scholar]
- Bruyeron, O. , Denizeau, M. , Berger, J. , & Trèche, S. (2010). Marketing complementary foods and supplements in Burkina Faso, Madagascar and Vietnam: lessons learnt from the Nutridev program. Food and Nutrition Bulletin, 31(2), S154–S167. [DOI] [PubMed] [Google Scholar]
- Codex Alimentarius (1991). Guidelines on formulated complementary foods for older infants and young children. CAC/GL 08‐1991 Adopted in 1991; Revised in 2013. Available at http://www.fao.org/fao-who-codexalimentarius/standards/list-of-standards/en/ (Accessed 15th May 2016).
- Global Alliance for Improved Nutrition (2014a). Case study: Better business practices boost Indian government efforts to provide nutritious food to young families . Geneva. http://www.gainhealth.org/wp-content/uploads/2015/02/Andhra-Pradesh-Case-Study-Better-Business-Practices-Boost-Indian-Government-Efforts-to-Provide-Nutritious-Food-to-Young-Families.pdf (Accessed 30th October 2016).
- Global Alliance for Improved Nutrition (2014b). Case study: Investing in a Côte d'Ivoire entrepreneur to ensure children's first foods are fortified, Geneva. http://www.gainhealth.org/wp-content/uploads/2015/02/Entrepreneur-to-Ensure-Childrens-First-Foods-are-Fortified.pdf (Accessed 30th October 2016).
- Global Alliance for Improved Nutrition (2014c). Case study: Empowering women entrepreneurs to produce fortified food for mothers and children in Rajasthan . Geneva.http://www.gainhealth.org/wp-content/uploads/2015/02/Empowering-Women-Entrepreneurs-to-Produce-Fortified-Food-for-Mothers-and-Children-Rajasthan.pdf. (Accessed 30th October 2016).
- Global Alliance for Improved Nutrition (2014d). Home fortification in Kenya: Lessons from implementation at the county level . Geneva. http://www.gainhealth.org/wp-content/uploads/2014/07/Home-fortification-in-Kenya-lessons-from-implementation-at-the-county-level.pdf (Accessed 30th October 2016).
- Global Alliance for Improved Nutrition (2014e). A complex puzzle: Generic behavior change and home fortification to improve nutrition in South Africa. Geneva. http://www.gainhealth.org/wp-content/uploads/2014/07/South-Africa-Nutrimark-GBSN-Case-Study1.pdf (Accessed 30th October 2016).
- Global Alliance for Improved Nutrition (2015a).Improving complementary feeding: Assessing public and private sector business models . Paper 1, GAIN IYCN Working Paper Series, Geneva. Available at http://www.gainhealth.org/wp-content/uploads/2015/04/WhitePaper1_final.pdf (Accessed 15th May 2016).
- Global Alliance for Improved Nutrition (2015b). Promoting optimal infant feeding practices and effective use of complementary foods for infants: Delivery lessons. Paper 2, GAIN IYCN Working Paper Series, Geneva. Available at http://www.gainhealth.org/wp-content/uploads/2015/04/WhitePaper2_final.pdf (Accessed 15th May 2016).
- Global Alliance for Improved Nutrition (2016). Strengthening the enabling environment for scaling up access to good quality complementary foods. Paper 3, GAIN IYCN Working Paper Series, Geneva. Available at http://www.gainhealth.org/wp-content/uploads/2016/03/WhitePaper3_final_low_res.pdf (Accessed on 15th May 2016).
- International Food Policy Research Institute (2015). Global nutrition report 2015: actions and accountability to advance nutrition and sustainable development. DC: Washington. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Institute for Population Sciences (IIPS) and Macro International (2007). National Family Health Survey (NFHS‐3), 2005–06: India: Volume I. Mumbai: IIPS. [Google Scholar]
- Kayser O., Klarsfeld L. and Brossard S. (2014). Marketing nutrition for the base of the pyramid. Introducing successful practices for improved access to nutritious complementary foods: Key lessons from case studies. Hystra Hybrid Strategy Consulting: Paris, 2014 Available at http://www.gainhealth.org/knowledge-centre/marketing-nutrition-base-pyramid-3/ (Accessed on 15th May 2016). [Google Scholar]
- Khondker R. (2016). How to combine the 4 P's in a programmatic approach: Driving demand of multiple micronutrient powders as part of optimal IYCN in Bangladesh. Paper presented at Micronutrient Forum, Cancun, Mexico.
- Leyvraz, M. , Wirth, J. P. , Woodruff, B. A. , Sankar, R. , Sodani, P. R. , Sharma, N. D. , & Aaron, G. J. (2016). High coverage and utilization of fortified take‐home rations among children 6–35 months of age provided through the integrated child development services program: Findings from a cross‐sectional survey in telangana, india. PloS One, 11(10), e0160814. doi: 10.1371/journal.pone.0160814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyvraz M., Rohner F., Konan A.G., Essp L.J., Woodruff B.A., Norte A., Bonfoh B., Aaron G.J. (2016) High awareness but low coverage of a locally fortified complementary food in Abidjan, Cote d'Ivoire: Findings from a cross‐sectional survey. PloS One, 2016. Manuscript accepted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen, M. , Poonawala, A. , Leyvraz, M. , Berger, J. , Schofield, D. , Tran, Thuy N. , Tran, Khan V. , Do Thi Bao, H. , Wieringa, F.T. (2016). A delivery model for home fortification of complementary foods with micronutrient powders: Innovation in the context of vietnamese health systems strengthening. Nutrients , 8, 5, 259; available from http://www.mdpi.com/2072-6643/8/5/259, (Accessed on 30th October 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osendarp, S. , Broersen, B. , Van Liere, M. J. , De‐Regil, L. , Bahirathan, L. , Klassen, E. , et al. (2016). Complementary feeding diets made of local foods can be optimized, but additional interventions will be needed to meet iron and zinc requirements in 6‐23 month old children in low and middle income countries. Food and Nutrition Bulletin. 0379572116655239. doi: 10.1177/0379572116655239 [DOI] [PubMed] [Google Scholar]
- PAHO & WHO (2003). Guiding principles for complementary feeding of the breastfed child , Washington DC. Available at http://www.who.int/nutrition/publications/guiding_principles_compfeeding_breastfed.pdf (Accessed on 15th May 2016).
- Reerink, I. (2014). Lessons learned from market based approaches to mnp distribution and promotion, October 19, 2014, included in SPRING. 2015. Micronutrient Powders Consultation: Lessons Learned for Operational Guidance—Meeting Report. Arlington, VA: Strengthening Partnerships, Results, and Innovations in Nutrition Globally (SPRING) project.
- Results for Development Institute (2013). Nutrition for a better tomorrow: Scaling up delivery of micronutrient powders for infants and young children , available at http://www.r4d.org/nutrition-for-a-better-tomorrow. (Accessed on 30 Oct 2016).
- Scaling Up Nutrition Movement . SUN movement principles of engagement. Available at http://scalingupnutrition.org/about-sun/the-vision-and-principles-of-sun/ (Accessed on 30 Oct 2016).
- World Health Organisation (1981). International code for marketing of breast milk substitutes. Geneva: WHO, 1981. Available at http://www.who.int/nutrition/publications/code_english.pdf (Accessed on 15th May 2016). [Google Scholar]
- World Health Organization (2003) Global strategy for infant and young child feeding . Geneva: WHO; Available at http://apps.who.int/iris/bitstream/10665/42590/1/9241562218.pdf?ua=1&ua=1 (Accessed on 15th May 2016). [Google Scholar]
- World Health Organization (2011). Guideline: Use of multiple micronutrient powders for home fortification of foods consumed by infants and children 6–23 months of age . Geneva, World Health Organization, available at http://www.who.int/nutrition/publications/micronutrients/guidelines/guideline_mnp_infants_children/en/ (Accessed on 31st October 2016).
- World Health Organization (2016). Guidance on ending the inappropriate promotion of foods for infants and young children. Provisional agenda item 12.1. available at http://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_7Add1-en.pdf (Accessed on 31st October 2016).
- World Health Organization and United Nations Children's Fund (2008). Strengthening action to improve feeding of infants and young children 6‐23 months of age in nutrition and child health programmes: Report of proceedings . Geneva, 6–9 October 2008. Available at http://apps.who.int/iris/bitstream/10665/44034/1/9789241597890_eng.pdf (Accessed on 15th May 2016).


