Abstract
The present study addressed the contentious discussions about the benefits and risks of nipple shield use. The objective was to explore self‐reported reasons for using a nipple shield and examine associations pertaining to the mother, the infant and duration of breastfeeding. Data were collected from 4815 Danish mothers (68%) who filled out a self‐administered questionnaire with open and closed question. Data were analyzed by content and statistical descriptive and multivariable analysis. Results showed that 22% of the mothers used nipple shields in the beginning and 7% used it the entire breastfeeding period. Primiparae used nipple shields more often than multiparae, and early breastfeeding problems as well as background factors like lower age, education and higher body mass index were associated with a higher likelihood of using nipple shields. Characteristics of infants associated with introducing nipple shields were lower‐ gestational age and birthweight. The use of nipple shields was furthermore found to be associated with a threefold increased risk of earlier cessation of exclusive breastfeeding: among primiparae odds ratio = 3.80 (confidence interval 2.61–5.53); among multiparae odds ratio = 3.33 (confidence interval 1.88–5.93). Mothers' own descriptions underlined how various early breastfeeding problems led to the use of nipple shields. Some mothers were helped through a difficult period; others described the use creating a kind of dependence. The results highlight how nipple shields may help breastfeeding mothers in the early period but is not necessarily a supportive solution to the inexperienced mother who needs extra support in the early process of learning to breastfeed.
Keywords: breastfeeding, infant, newborn, post‐natal care, sucking behaviour, nipples, protective devices, nipple shield
Introduction
Ability to breastfeed is expected to be a natural process, but in special situations, helping devices may be required. Over the years, the usefulness of nipple shields in relation to breastfeeding has been discussed in the scientific breastfeeding literature. Thirty‐five years ago, a number of negative perspectives on the use of nipple shields were raised (Woolridge et al. 1980), but recent studies have pointed to the benefits (Powers & Tapia 2004; Chertok et al. 2006; Hanna et al. 2013). Meanwhile, nipple shields have changed from thick rubber teats to breast‐shaped shields in ultra‐thin silicone material in different sizes. In Sweden, nipple shields are used by approximately 18% of the new mothers during the first week, 10% at 3 months and 1% at 9 months post‐partum (Ekstrom et al. 2014). The reporting of medium duration of use in the United States varies from 2 weeks (Powers & Tapia 2004) to 6 weeks (Hanna et al. 2013).
Every second, mother experiences difficulties in relation to breastfeeding (Wagner et al. 2013). Early problems have been reported to be significantly associated with ineffective latch, sucking or milk transfer (Kronborg & Vaeth 2009). The need for nipple shields often arises from early latching and sucking problems related to either the mother or the baby. The mother may have flat or inverted nipples (Wilson‐Clay 1996; Powers & Tapia 2004; Chertok 2009), large breasts (Ekstrom et al. 2014), engorgement (Powers & Tapia 2004; Chertok 2009) or pain in connection to sore and damaged nipples (Hanna et al. 2013; Ekstrom et al. 2014). The baby may have difficulties latching onto the breast because of prematurity (Meier et al. 2000), disorganized suck (Powers & Tapia 2004) or poor or weak latch and suck (Powers & Tapia 2004; Chertok 2009; Ekstrom et al. 2014).
Recent clinical studies have shown that the use of nipple shields might help the baby to latch on and thereby avoid early breastfeeding cessation (Hanna et al. 2013). Mothers have mainly reported their experiences of using nipple shields positively and expressed satisfaction in statements such as ‘it made all the difference in the beginning’ (Hanna et al. 2013) and ‘it helped to prevent breastfeeding termination’ (Chertok 2009). Negative experiences have focused on how the use of nipple shields complicated breastfeeding, for example, ‘feedings last longer than without’ (Hanna et al. 2013) and ‘nipple shields caused nipple soreness and inconvenience’ (Chertok 2009).
Earlier physiological studies with a low number of participants have concluded that the use of nipple shields had no impact on hormone release (Amatayakul et al. 1987; Chertok et al. 2006), but there may be a risk that use of nipple shields, measured by breast pumping, reduced milk transfer (Amatayakul et al. 1987) and led to decreased milk production (McClellan et al. 2012). Therefore, pumping was previously recommended to ensure the milk supply in relation to use of nipple shields (Riordan 2005). Recently, it has been pointed out that the consequences of nipple shield use may depend on the guidance given to the mothers (Ekstrom et al. 2014). According to a literature review by McKechnie & Eglash (2010), studies examining consequences of the use of nipple shields generally have considerable limitations and conclude beyond their capability because of small sample sizes and short follow up periods. There is a need to know more about both risks and the benefits of nipple shield use to inform health professionals in practice so they are able to support and guide mothers sufficiently. We collected data from a larger Danish population of breastfeeding mothers and asked both open and closed questions about their use of nipple shields 6 months post‐partum. The aim of the study was first to explore the self‐reported reasons mothers start using a nipple shield, secondly to assess if the use of nipple shields is associated with maternal or infant characteristics or the breastfeeding act and finally to examine associations between the use of nipple shields and duration of exclusive breastfeeding.
Key messages.
The use of nipple shields helped mothers to overcome early breastfeeding problems, but for some mothers, it also influenced the act of breastfeeding in the longer run by developing a dependence.
The use of nipple shields is associated with a shorter breastfeeding period, among primipara independent on the time used and among multipara only for mothers using it during the entire breastfeeding period.
Health professionals should be aware that the use of nipple shields may be an easy but not necessarily supportive solution to the inexperienced mother who needs extra support in the early process of breastfeeding.
Materials and method
Design, setting and participants
In an observational cross‐sectional study design, we collected data from women who had given birth 6 months previously. The study took place in the western part of Denmark including 19 municipalities in both urban and rural areas. Nearly 99% of all deliveries in Denmark take place in hospitals. The seven hospitals participating in this study had adopted the principles of the Baby‐Friendly Hospital initiative, and five had been certified as Baby‐Friendly (WHO 2009). In Denmark, all citizens are assigned a unique civil registration number at birth through the Civil Registration System. This number was used to identify newborns and their mothers. Women who had given birth from 1 April to 30 June and from 1 August to 31 October 2008 were recruited. In the study periods, primiparae usually stayed in the hospital for 4 days, whereas multiparous women without complications returned home within 24 h after the delivery. After discharge from the maternity ward, a health visitor routinely visited the family of the newborn within 10 days following birth. Health visitors in Denmark are registered nurses with 1 year of supplementary training. The home visits are not standardized, but generally health visitors focus on supporting attachment and breastfeeding at their first visit. From 16 April to 14 June 2008, a strike was going on among midwives and health visitors in Denmark; this meant that more primiparae without complications were discharged within 24 h, and more mothers not experiencing early problems received a delayed home visit by the health visitor. The frequency of use of nipple shields did not change during the strike period, and effects of the strike period have been reported elsewhere (Kronborg et al. 2012).
In the study region, the birth rate is approximately 15 000 annual births. All women who lived in the region with a newborn registered on their address in the 5‐month recruitment period were invited to participate in the study. A total of 7113 newborn were included.
Data collection and questionnaire
Data were collected from eligible mothers who received an anonymous, self‐administered questionnaire approximately 6 months after birth with a pre‐paid return envelope for reply. The questionnaire included socio‐demographic questions, maternal questions related to previous breastfeeding experience, early breastfeeding problems, duration of breastfeeding and questions about infant growth and wellbeing.
The questionnaire consisted mainly of questions used in earlier studies (Kronborg et al. 2007) and had in that connection been face and content validated. New questions were developed for this study to collect information on the use of nipple shields and self‐reported breastfeeding duration. The questionnaire was subsequently reviewed by two experts and pilot tested for comprehension and acceptability in two rounds by 12 mothers at different ages and parity, as well as social and ethnic background.
Variables
All measures were collected from the self‐reported questionnaire. The primary study variables included initiation, duration and reasons for use of nipple shields together with initiation and duration of exclusive breastfeeding. Use of nipple shields was measured by asking the mother ‘Did you use a nipple shield when breastfeeding your baby this time?’ (yes all the time, yes in the beginning, no never) and ‘If you used a nipple shield in the beginning, how many days did you use it?’ (number of days). The variables were categorized according to mothers' self‐reported responses defining ‘in the beginning’ as use of nipple shields in a period followed by a breastfeeding period without use of nipple shields, ‘all the time’ as use of nipple shields during the entire breastfeeding period and ‘never’ as not ever having used a nipple shield. The closed questions were followed by the open question ‘Please describe the reason for using the nipple shield, in your own words?’ (text). Duration of exclusive breastfeeding was measured using a slight modification of indicators for assessing breastfeeding practices (WHO 1991) by asking the mother ‘Did you start breastfeeding after giving birth this time?’ (yes or no) and ‘How many months and weeks did your infant receive only your breast milk without any supplement at all?’ Mothers were categorized as exclusively breastfeeding according to the number of weeks where they had given the infant breast milk only and as long as they had no positive registered answers to having started giving the infant anything else than their own breast milk. The outcome factor of breastfeeding duration was cut‐off at 17 weeks in accordance with the Danish recommendations for exclusive breastfeeding for at least 4 months. Additional study variables included variables related to maternal, child and breastfeeding factors. Maternal factors included age (years), body mass index (BMI) (kg/m2), length of education (none, short, medium‐long), smoking (yes, no), self‐reported ethnicity (Danish, other than Danish) parity (primiparous, multiparous) and previous experience with breastfeeding (weeks). Child factors included sex, pacifier used in the first 2 weeks (yes, no), gestational age at birth (weeks) and birthweight (gram). Breastfeeding factors included breastfeeding problems within the first week with respect to pain, latching, damaged nipples, blocked milk ducts, mastitis and worries about having enough milk (all yes, no). The cut‐off at 1 week according to early breastfeeding factors was chosen to catch the early breastfeeding problems and avoid overlap to the breastfeeding duration.
Statistical analysis
Bivariate associations between use of nipple shields, exclusive breastfeeding cessation before week 17 and maternal, infant and early breastfeeding characteristics were first assessed by chi‐squared tests for categorical measures and one‐way analysis of variance for continuous measures. The duration of exclusive breastfeeding according to the use of nipple shields was further examined in survival curves using the Kaplan–Meier method. Duration of exclusive breastfeeding was censored at 17 weeks, and a log‐rank test was used to compare the survival distributions depending on use of nipple shields. Next, multivariable logistic regression analysis was used to evaluate the influence of use of nipple shields on cessation of exclusive breastfeeding before week 17. The analysis was stratified by parity, known from previous research to be influential on the breastfeeding duration (Kronborg & Vaeth 2004; Kronborg & Vaeth 2009) and included infant, maternal and early breastfeeding factors, which have been shown to be important for the use of nipple shield. Covariates included all maternal, infant and early breastfeeding characteristics that were significantly correlated (P < 0.05) with both the use of nipple shields and exclusive breastfeeding duration in the bivariate analysis. Finally, we tested interaction terms to see if the association between use of nipple shields and cessation of exclusive breastfeeding before week 17 was modified by any of the confounding variables. Stata version 12 was used for all statistical analysis (StataCorp 2011, Stata Statistical Software, College Station, Texas).
Content analysis
For the purpose of exploring mothers' descriptions of reasons for using the nipple shield, mothers' answers to the open question were transcribed verbatim and compiled in a 38‐page document of text data. The short descriptions from 807 mothers were analyzed looking for manifest content by using qualitative content analysis. This method is suitable when analyzing texts to distill words into a few content‐related categories and ensuring that words when clustered and categorized share the same meaning (Graneheim & Lundman 2004; Elo & Kyngas 2008). The inductive analysis process included three phases. In the first phase, all the transcribed text was read to achieve a sense of the whole content. In the second phase, the text was reread word by word in order to group the data while going back to the aim of the study. In the third phase, the text was clustered, and meaning units were organized in themes and subthemes with special attention to the patterns and time frame in the data material. Finally, a short description of the substance of each theme was written, and citations from the original text were selected to illustrate the themes. In the content analysis, the focus was on described experiences of the mothers. The descriptions were essential by being experienced by the mothers who answered the open question. Other mothers may have had the same experiences, but they have not been asked. Therefore, the number of mothers describing each experience was not essential.
Ethics
The study was approved by Central Denmark Region Committee on Biomedical and Research Ethics (Jr. nr. 1‐16‐02‐1‐08/068) and the Danish Data Protection Agency (Jr. nr. 2007‐58‐0010). Written information was provided to the women before enrolment.
Results of the statistical analysis
Of the 7113 mother–infant pairs who were registered in the study, 5127 mothers returned the questionnaire resulting in a response rate of 72%. The study population was defined as mothers who started breastfeeding and had complete information on full breastfeeding duration and use of nipple shields. A total of 203 mothers did not start breastfeeding, and information on exclusive breastfeeding duration and use of nipple shields was missing in three and 106 of the mothers, respectively. The study population was hereby reduced to 4815 mother–infant pairs. Fig. 1 shows the selection of the study population. The 109 mothers and infants excluded due to missing data showed no statistically significant difference with respect to mother's age, educational level, gestational age at birth or birthweight when compared with included mothers and infants. No difference in cessation of exclusive breastfeeding before week 17 was found comparing the mothers with information on use of nipple shields with the 106 mothers without.
Figure 1.
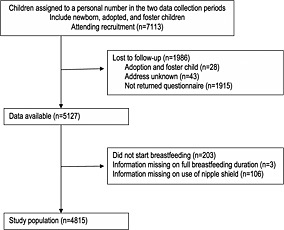
Flow profile and exclusion criteria for selection of study population.
In the study population, 71% (n = 3441) of the mothers had never used a nipple shield, 22% (n = 1037) had used it in the beginning and 7% (n = 340) had used it all the time (Table 1). The mothers who had used the nipple shield all the time were younger, had a higher BMI, lower educational level and were more likely to smoke compared with the mothers who had only used it in the beginning; the mothers who had never used a nipple shield were the least likely to have these characteristics. All associations were statistically significant. Primiparae and multiparae mothers with short previous breastfeeding experience (0–5 weeks) were more likely to have used the nipple shield all the time, whereas the highest proportion of mothers who never used a nipple shield was found among multiparous who had breastfed their last child 17+ weeks. Infant characteristics significantly associated with the use of nipple shield were lower gestational age, lower birthweight and using a pacifier. According to gestational age, 110 of the infants were very/moderate preterm (≤week 33), 263 were late preterm (weeks 34–36) and 4526 were born at term (≥week 37). Among the very/moderate preterm infants, 31.8% were breastfed with a nipple shield in the beginning and 15.3% all the time while this concerned 27.9% and 10.3% among late preterm infants, and 21.2% and 6.8% among term infants, respectively. The proportions of mothers using a nipple shield both in the beginning and all the time were significantly higher among those who had experienced early breastfeeding problems with latching, blocked milk ducts, mastitis or worries about insufficient milk supply. Among mothers who had reported early problems with pain and damaged nipples, a difference was only seen in the proportion of use or no use of the nipple shield in the beginning.
Table 1.
Characteristics of 4815 mother–infant pairs according to use of nipple shields and exclusive breastfeeding duration
| Variable | Values | Use of nipple shields | Duration of exclusive breastfeeding | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All the time | Beginning | Never | P | 0–17 weeks | 17+ weeks | P | |||||||
| N: 340 (%) | N: 1036 (%) | N: 3439 (%) | N: 1774 (%) | N: 3041 (%) | |||||||||
| Maternal factors | |||||||||||||
| Age in years | Mean (SD) | 29.7 | (4.8) | 30.4 | (4.3) | 31.4 | (4.5) | <0.001 | 30.4 | (4.9) | 31.4 | (4.3) | <0.001 |
| Body mass index | Mean (SD) | 25.1 | (5.5) | 24.5 | (5.2) | 24.0 | (4.9) | <0.001 | 24.9 | (5.5) | 23.8 | (4.6) | <0.001 |
| Educational level | None or short | 159 | (7.9) | 436 | (21.6) | 1418 | (70.4) | 0.036 | 930 | (46.2) | 1083 | (53.8) | <0.001 |
| Intermediate | 131 | (6.9) | 433 | (22.7) | 1343 | (70.4) | 616 | (32.3) | 1291 | (67.7) | |||
| Long | 41 | (5.3) | 151 | (19.5) | 583 | (75.2) | 175 | (22.6) | 600 | (77.4) | |||
| Smoking | Yes | 38 | (8.4) | 76 | (16.7) | 340 | (75.0) | 0.021 | 264 | (58.2) | 190 | (41.9) | <0.001 |
| No | 296 | (6.9) | 954 | (22.1) | 3059 | (71.0) | 1489 | (34.6) | 2820 | (65.4) | |||
| Self‐reported ethnicity | Danish | 315 | (7.1) | 976 | (22.0) | 3141 | (70.9) | 0.020 | 1618 | (36.5) | 2814 | (63.5) | 0.104 |
| Other than Danish | 19 | (5.7) | 54 | (16.3) | 259 | (78.0) | 136 | (41.0) | 196 | (59.0) | |||
| Experience in breastfeeding | None, primipara | 237 | (11.5) | 594 | (28.8) | 1233 | (59.7) | <0.001 | 874 | (42.3) | 1190 | (57.7) | <0.001 |
| 0–5 weeks | 37 | (9.1) | 92 | (22.6) | 279 | (68.4) | 291 | (71.3) | 117 | (28.7) | |||
| 6–17 weeks | 32 | (3.7) | 149 | (17.4) | 678 | (78.9) | 376 | (43.8) | 483 | (56.2) | |||
| 17+ weeks | 28 | (2.2) | 167 | (12.9) | 1100 | (84.9) | 181 | (14.0) | 1114 | (86.0) | |||
| Infant factors | |||||||||||||
| Gestational age at birth in weeks | Mean (SD) | 39.1 | (2.5) | 39.2 | (2.3) | 39,5 | (1.9) | <0.001 | 39.2 | (2.2) | 39.5 | (1.9) | <0.001 |
| Birthweight in kilogram | Mean (SD) | 3.4 | (0.7) | 3.5 | (0.6) | 3,6 | (0.6) | <0.001 | 3.5 | (0.6) | 3.6 | (0.6) | <0.001 |
| Sex | Girl | 177 | (7.6) | 498 | (21.3) | 1661 | (71.1) | 0.395 | 842 | (36.0) | 1494 | (64.0) | 0.265 |
| Boy | 163 | (6.6) | 538 | (21.7) | 1778 | (71.7) | 932 | (37.6) | 1547 | (62.4) | |||
| Pacifier used in the first 2 weeks | Yes | 212 | (8.3) | 598 | (23.5) | 1734 | (68.2) | <0.001 | 1125 | (44.2) | 1419 | (55.8) | <0.001 |
| No | 116 | (5.4) | 424 | (19.7) | 1615 | (74.9) | 588 | (27.3) | 1567 | (72.7) | |||
| Early breastfeeding factors | |||||||||||||
| Problems with pain breastfeeding week 1 | No | 179 | (7.5) | 438 | (18.4) | 1770 | (74.2) | <0.001 | 887 | (37.2) | 1500 | (62.8) | 0.298 |
| Yes | 148 | (6.4) | 557 | (24.2) | 1595 | (69.4) | 821 | (35.7) | 1479 | (64.3) | |||
| Problems with latching on week 1 | No | 76 | (2.4) | 424 | (13.5) | 2652 | (84.1) | <0.001 | 999 | (31.7) | 2153 | (68.3) | <0.001 |
| Yes | 246 | (16.4) | 570 | (38.0) | 685 | (45.6) | 686 | (45.7) | 815 | (54.3) | |||
| Problems with damaged nipples week 1 | No | 199 | (6.6) | 547 | (18.1) | 2269 | (75.3) | <0.001 | 1066 | (35.4) | 1949 | (64.6) | 0.087 |
| Yes | 126 | (7.6) | 447 | (27.1) | 1077 | (65.3) | 625 | (37.9) | 1025 | (62.1) | |||
| Problems with plugged milk ducts week 1 | No | 248 | (6.2) | 800 | (20.1) | 2926 | (73.6) | <0.001 | 1429 | (36.0) | 2545 | (64.0) | 0.595 |
| Yes | 74 | (11.6) | 169 | (26.5) | 394 | (61.9) | 236 | (37.1) | 401 | (63.0) | |||
| Problems with mastitis week 1 | No | 300 | (6.7) | 928 | (20.7) | 3247 | (72.6) | <0.001 | 1590 | (35.5) | 2885 | (64.5) | 0.003 |
| Yes | 22 | (13.4) | 53 | (32.3) | 89 | (54.3) | 78 | (47.6) | 86 | (52.4) | |||
| Worries about insufficient milk supply week 1 | No | 218 | (5.8) | 739 | (19.7) | 2791 | (74.5) | <0.001 | 1147 | (30.6) | 2601 | (69.4) | <0.001 |
| Yes | 109 | (11.8) | 249 | (27.0) | 565 | (61.2) | 548 | (59.4) | 375 | (40.6) | |||
| Use of nipple shields | All the time | 234 | (68.8) | 106 | (31.2) | <0.001 | |||||||
| In the beginning | 453 | (43.7) | 583 | (56.3) | |||||||||
| Never | 1087 | (31.6) | 2352 | (68.4) | |||||||||
Missing values excluded; P‐values calculated from chi‐square tests for categorical variables and one‐way analysis of variance for continuous variables.
Exclusive breastfeeding in more than 17 weeks showed significant associations with all maternal and infant factors except mother's self‐reported ethnicity and sex of the infants (Table 1). Experiencing early breastfeeding problems with pain or blocked milk ducts was not significantly associated with exclusive breastfeeding +17 weeks, but the other early breastfeeding factors did show a significant association, although only borderline in relation to problems with damaged nipples. This implies that all study measures except sex of the infant, mother's self‐reported ethnicity and early breastfeeding problems with pain, blocked milk ducts or damaged nipples could confound the association between use of nipple shields and exclusive breastfeeding cessation before week 17.
Kaplan–Meier curves of exclusive breastfeeding duration from weeks 0 to 17 according to use of nipple shields are shown in Fig. 2. The three survival curves were significantly different (log‐rank test: P < 0.001) with the steepest curve for mother–infant pairs who used the nipple shield all the time and the second steepest for the ones who used the nipple shield in the beginning. The proportion of mothers only feeding their child with breast milk at 4 months post‐partum (week 17+) was 31% (n = 340) among the mothers who used nipple shields all the time, 56% (n = 1036) among the mothers who used the nipple shield in the beginning and 68% (n = 3439) among the mothers who never used a nipple shield.
Figure 2.
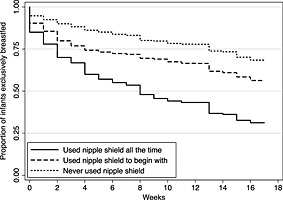
Proportion of infants exclusive breastfed according to mothers' use of nipple shield as a function of the age of the infant (weeks 0–17).
The adjusted logistic regression analysis was based on 3933 mother–infant pairs with information on all confounding variables significantly correlated with both exclusive breastfeeding duration and use of nipple shields (Table 2). Using a nipple shield all the time was associated with more than three times higher odds of cessation of exclusive breastfeeding before week 17 in both primiparae and multiparae mothers when compared with reference groups who never used a nipple shield (primiparae: odds ratio (OR) 3.80, 95% confidence interval (CI) 2.61–5.53; multiparae: (OR 3.33, 95% CI 1.88–5.93). Using a nipple shield in the beginning was associated with 63% higher odds of ending exclusive breastfeeding before week 17 in primiparous mothers (OR 1.63, 95% CI 1.27–2.09), whereas no significant association was seen in multiparous mothers (OR 1.13, 95% CI 0.84–1.52). No moderator effects were found when testing interactions between the confounders and use of nipple shields.
Table 2.
Odds ratios from logistic regression for cessation of exclusive breastfeeding before week 17 and stratified by parity
| Use of nipple shield | Primiparous | Multiparous | All women |
|---|---|---|---|
| N = 1739 | N = 2194 | N = 3933 | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Never | 1 | 1 | 1 |
| All the time | 3.80 (2.61–5.53) | 3.33 (1.88–5.93) | 3.41 (2.51–4.63) |
| In the beginning | 1.63 (1.27–2.09) | 1.13 (0.84–1.52) | 1.40 (1.17–1.69) |
CI, confidence interval; OR, odds ratio.
Use of nipple shields estimates adjusted for the following: maternal factors (age, body mass index, education, smoking and breastfeeding experience), infant factors (gestational age, birthweight and pacifier used in the first 2 weeks) and early breastfeeding factors (problems in week 1 with latching, damaged nipples, mastitis and worries about insufficient milk supply).
Findings in the content analysis
The mothers' descriptions included both the reasons for and their experiences with using the nipple shield. The main reasons for introducing it were painful breastfeeding or problems with latching. The mothers' experiences using the nipple shield differed; some found the nipple shield helpful, others did not. Some struggled subsequently with the dependence the infant had developed using the nipple shield; others had no trouble getting the infant to suck at the breast without the use of nipple shield. Table 3 gives an overview of the themes and subthemes described in the following.
Table 3.
Mothers' descriptions of reasons for and experiences with using a nipple shield (n = 807)
| Themes and subthemes | |
|---|---|
| Painful breastfeeding | |
| Help to relieve painful breastfeeding | |
| Prevent painful breastfeeding | |
| Difficulty latching on | |
| Difficulty related to the mother | |
| Difficulty related to the infant | |
| Nipple shield use helped out or not | |
| Helped over a period | |
| Was not of any help | |
| Made damage | |
| Influence on milk production using nipple shield | |
| Have experienced insufficient milk production | |
| Have experienced sufficient milk production | |
| Dependence on the use of nipple shield | |
| The infant got dependent | |
| Easy to get the infant back on the breast |
Painful breastfeeding
Mothers described how they had sore, injured, blistered or bleeding nipples, or they had infection in the breast that made breastfeeding very painful. One mother described this as ‘the worst pain in my life’. They used the nipple shield to relieve and overcome the pain. Especially multipara with excruciating experiences from their first child used the nipple shield to prevent their nipples from being injured and grow accustomed to breastfeeding: ‘I would avoid the extreme pain this time and used nipple shields to help’.
Difficulty latching on
Descriptions of difficulty latching on were both related to the mother and the infant. Descriptions related to the mothers referred to the breasts such as swollen, engorged or hard and to the nipples such as too little, big, wide, flat, inverted, scarred, soft or not irrigating making it difficult for the infant to latch on. As one mother wrote ‘my breasts were not pointed enough’. Also, too fast or too slow milk flow was mentioned as reasons for using the nipple shield. In other descriptions, the difficulty in latching related to the infant. Some infants had tight frenulum and poor or incorrect sucking technique. Others were very unrestful, eager, impatient, hungry or had an extensive sucking desire: ‘she had no patience and could not get it right’. For infants born prematurely, the nipple shield was used to ease latching on because the infant had no strength, was tired, a little sluggish, lacking sucking reflex or sucking desire.
Helpful or unhelpful
Mothers described how the nipple shield helped them getting started breastfeeding or helped them through a difficult period. The nipple shield was, according to these mothers, crucial for their continuation of breastfeeding: ‘Without nipple shields in the beginning my breastfeeding would never have succeeded’. Other mothers did not find the nipple shield helpful, and some reported that the nipple shield made things worse.
Influence on milk production using nipple shields
Some mothers described they registered no reduction in the milk production or influence on the infant's wellbeing: ‘the nipple shield gave no problems with the amount of milk so I used it all the time’. Other mothers blamed the nipple shield for a reduced milk supply.
Dependence on the use of nipple shields
According to maternal experiences, some infants developed a dependence on the use of the nipple shield. The mothers described it as a bad habit; the infants got frustrated when they were offered the breast without the nipple shield and would not latch on: ‘we tried the nipple shield to get breastfeeding started now he will not let go of it’. Other mothers told it was relatively easy to get the infant back on the breast.
Discussion
The nipple shield was particularly used in the beginning; a minor proportion of mothers used it during the entire breastfeeding period. Primiparae used the nipple shield more often than multiparae, and early breastfeeding problems as well as background factors including younger age, lower education level and higher BMI among mothers and lower gestational age and birthweight among infants were significantly associated with the use of nipple shields both in the beginning and during the entire exclusive breastfeeding period. The use of nipple shields was also significantly associated with a shorter duration of exclusive breastfeeding. Among primiparae, an increased risk of breastfeeding cessation before week 17 was seen for both mothers using nipple shields in the beginning and during the entire breastfeeding period, while this was only the case for mothers using it all the time among multiparae. The mothers' own descriptions underlined how early breastfeeding problems led to the use of nipple shields and how it for some helped them through a difficult period. In the following breastfeeding period, mothers described that nipple shields had a tendency to create dependence.
In the present study, more than one fifth of the mothers used a nipple shield in the beginning, and a minor proportion used it during the entire breastfeeding period. This is an increase in the use of nipple shields among Danish mothers compared with studies from 2004 showing a 15% rate (unpublished). The present study also had a higher proportion of users than earlier Scandinavian studies (Ekstrom et al. 2014) and the US studies (Powers & Tapia 2004; Hanna et al. 2013), pointing to the number of breastfeeding women that using a nipple shield during their breastfeeding period may be increasing these years.
In this study, as in other studies (Brigham 1996; Wilson‐Clay 1996; Meier et al. 2000; Hanna et al. 2013; Ekstrom et al. 2014), the primary reason for using nipple shields was found, both in the open and in the closed questions, to be early breastfeeding problems. Knowing that around 30–40% of new mothers experience early breastfeeding problems (Kronborg & Vaeth 2009) and that these are often related to problems with damaged nipples and extreme pain during breastfeeding, the nipple shield has the potential to help mothers through this difficult period. This was confirmed in the present and others studies by mothers describing how they may have stopped breastfeeding if it had not been for the nipple shield (Brigham 1996; Powers & Tapia 2004; Chertok 2009). It underlines the need for the nipple shield in the early period of breastfeeding and how the device can be used as support in a helpful way.
The results also pointed to differences in the characteristics of breastfeeding problems related to the use of nipple shields and duration of exclusive breastfeeding. Damaged nipples and pain were only associated with the use of nipple shields in the beginning of the breastfeeding period and not associated significantly with the duration of exclusive breastfeeding; whereas early breastfeeding problems with latching, mastitis or worries about insufficient milk supply were associated with the use of nipple shields both in the beginning, the entire period and the duration of exclusive breastfeeding. These characteristics may point to groups of mothers who need support in the process of learning to breastfeed beyond being introduced to a nipple shield, taking into account that mothers using a nipple shield more frequently were characterized by being less experienced in breastfeeding and being younger, having a lower education and a higher BMI, all socio‐demographic factors well‐known to be associated with shorter breastfeeding duration (Kronborg & Vaeth 2004; Taylor et al. 2006; Krause et al. 2011). When studies analyzing open descriptions find that mothers did not think the nipple shield helped them (Hanna et al. 2013) or that it complicated breastfeeding (Chertok et al. 2006), it may be because the nipple shield was introduced for reasons that should have been supported in other ways. Pincombe et al. showed in 2008 (Pincombe et al. 2008) that starting use of nipple shields before discharge reduced the chance of breastfeeding. Recently, Ekstrom et al. (2014) have pointed to the results from their longitudinal study showing that the negative association between breastfeeding duration and the use of nipple shields was not explained by the mother or the baby but to a higher degree by the way mothers were introduced to and supported in their use of nipple shields. Health professionals should take into account that introducing a nipple shield may not necessarily be supportive to the inexperienced or insecure mother who has difficulty with latching.
Using the nipple shield all the time tripled the odds for early cessation of exclusive breastfeeding in both primipara and multipara, whereas using a nipple shield in the beginning only increased the risk among primiparae. These results are to the best of our knowledge the first reliable results, building on a large study population and multivariate analysis, showing a shorter duration of exclusive breastfeeding related to the use of nipple shields. The inconclusive results until now on whether the use of nipple shield influence breastfeeding duration may be explained by studies that except for the study from Ekstrom et al. (2014) have not differentiated between exclusive and partial breastfeeding (Brigham 1996; Powers & Tapia 2004; Hanna et al. 2013) or have included mothers who pump or use formula supplementation (Chertok et al. 2006; Chertok 2009). According to Amatayakul et al. (1987) and Auerbach (1990), the nipple shield reduced milk transfer. Although results from these studies are based on relatively small study populations and limited in their research methods by using breastpump (Auerbach 1990) or introducing nipple shield to normally breastfed infants (Amatayakul et al. 1987), it is hard to imagine the use of nipple shields not having any functionary influence on the milk transfer, knowing about the way mothers' milk spurt out of the breast and into the babies' mouth during milk ejections (Ramsay et al. 2004; Ramsay & Hartmann 2005). The ongoing discussion how the uses of nipple shields influence breastfeeding duration may be explained by differences in babies' sucking abilities and mothers' milk release. If the baby has a strong suck or the mother an efficient milk production and a high intention to breastfeed, the use of nipple shields may not influence the exclusive breastfeeding duration in the same way as if the baby, e.g. has a week sucking pattern. Further research is needed to clarify the influence of physiological and psycho‐social factors.
Because of the observational cross‐sectional design of this study, we cannot draw any definitive causal conclusion concerning the strong association between use of nipple shield and duration of exclusive breastfeeding. A randomized study by Kramer et al. (2001) did not find an association between the use of pacifier and breastfeeding duration. The authors concluded in that connection that pacifier use might be a marker of breastfeeding difficulties or reduced motivation to breastfeed instead of a true cause of weaning (Kramer et al. 2001). Similarly, the use of a nipple shield may be a marker of breastfeeding difficulties, and although we controlled for potential confounding because of early breastfeeding problems, our measures might not be comprehensive enough to capture all difficulties. Therefore, we cannot rule out that the use of a nipple shield may be a marker of breastfeeding problems that regardless of nipple shield use would have reduced duration of breastfeeding. This issue would be optimally investigated in a randomized trial, but knowing about both the benefits and drawbacks associated with the use of nipple shields, it would, however, be unethical to test the use in such a design.
The present study benefits from a large sample size, including participants from both urban and rural areas, and the study population is suitable as nearly every mother starts breastfeeding in Denmark. Selection bias is unlikely to have influenced the findings in any significant way. The design of the study ensured that every address with a registered newborn received a questionnaire. The response rate of 72% resulted in a study population that closely resembled the Danish background population with respect to ethnicity, multiple and preterm birth and mother's age at delivery (Danish Health and Medicines Authority 2012; Statistics Denmark 2013). Telephone calls to non‐responders supported the findings that different mothers had not returned the questionnaire for various reasons, most often lack of time. In the present study, the study population was reduced to 68% of those eligible because of missing data. We found that the excluded mothers did not differ from the included mothers with respect to socio‐demographic factors, infant factors and the duration of exclusive breastfeeding; but otherwise, we have no knowledge of the behaviour of the non‐responding mothers concerning use of nipple shields.
By using self‐reported data from a questionnaire collected when the infant was 6 months, we got the mothers experiences of the whole exclusive breastfeeding period. The high reported frequency of use of nipple shields indicated the mothers recalled the use of nipple shields just like breastfeeding is usually well recalled by mothers (Natland et al. 2012); but we cannot exclude that the retrospective study design may have caused some recall bias when asking the mothers to recall the early period of breastfeeding. Mothers who have experienced problems later on may be more disposed to look for problems earlier on, and their answers could therefore be dependent on what happened through the course of breastfeeding.
Conclusion
Nipple shields were particularly used in the beginning and by a minor proportion of mothers during the entire breastfeeding period. Primiparae used nipple shields more often than multiparae, and early breastfeeding problems as well as younger age, lower education and higher BMI among mothers and lower gestational age and birthweight among infants were significantly associated with the use of nipple shields in the beginning and the entire breastfeeding period. The use of nipple shields was correlated with a shorter duration of breastfeeding. Among primipara, this was the case for both mothers who used the nipple shield in the beginning and mothers who used it all the time, while among multiparae, the association was only found for mothers who used the nipple shield during the entire breastfeeding period. The mothers' own descriptions underlined how early breastfeeding problems led to the use of nipple shields and how it for some helped them through a difficult period. In the following breastfeeding period, the nipple shields had a tendency to create dependence in some.
Health professionals should be aware that the use of nipple shields may be an easy but not necessarily supportive solution to the inexperienced or insecure mother who has difficulty with latching and need extra support in the early process of learning to breastfeed.
Source of funding
Public Health and Quality Improvement, a non‐profit centre for research and development within the social and public health care system in Central Denmark Region, Denmark, funded this study.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
Work on this study was performed by the authors, and no individuals other than the listed authors contributed. HK, first author of the article, is responsible for the conception and design, collection and interpretation of the data. EF has framed the strategy for data analysis and performed the analysis and interpretation of data. IN and RM have contributed to the interpretation of data. All four authors have contributed to the drafting and editing of the paper and approved the final version submitted for publication.
Acknowledgements
We would like to thank health visitor and current PhD student at the Department of Public Health, Section for Nursing, Aarhus University, Denmark, Ingeborg Kristensen who provided support in several parts of the study and was involved in data collection. Moreover, we would like to thank the Public Health and Quality Improvement, a non‐profit centre for research and development within the social and health care systems in Central Denmark Region. Data collection was financed by the non‐profit centre where Ingeborg Kristensen was employed at the time of the study.
Kronborg H., Foverskov E., Nilsson I., and Maastrup R. (2017) Why do mothers use nipple shields and how does this influence duration of exclusive breastfeeding?, Maternal & Child Nutrition, 13, e12251. doi: 10.1111/mcn.12251.
References
- Amatayakul K., Vutyavanich T., Tanthayaphinant O., Tovanabutra S., Yutabootr Y. & Drewett R.F. (1987) Serum prolactin and cortisol levels after suckling for varying periods of time and the effect of a nipple shield. Acta Obstetricia et Gynecologica Scandinavica 66, 47–51. [DOI] [PubMed] [Google Scholar]
- Auerbach K.G. (1990) The effect of nipple shields on maternal milk volume. Journal of Obstetric, Gynecologic, and Neonatal Nursing 19, 419–427. [DOI] [PubMed] [Google Scholar]
- Brigham M. (1996) Mothers' reports of the outcome of nipple shield use. Journal of Human Lactation 12, 291–297. [DOI] [PubMed] [Google Scholar]
- Chertok I.R., Schneider J. & Blackburn S. (2006) A pilot study of maternal and term infant outcomes associated with ultrathin nipple shield use. Journal of Obstetric, Gynecologic, and Neonatal Nursing 35, 265–272. [DOI] [PubMed] [Google Scholar]
- Chertok I.R.A. (2009) Reexamination of ultra‐thin nipple shield use, infant growth and maternal satisfaction. Journal of Clinical Nursing 18, 2949–2955. [DOI] [PubMed] [Google Scholar]
- Danish Health and Medicines Authority (2012) [Number and analysis: birth statistics 2011]. Copenhagen. Available at: http://www.ssi.dk/Sundhedsdataogit/~/media/Indhold/DK%20-%20dansk/Sundhedsdata%20og%20it/NSF/Analyser%20og%20rapporter/TalOgAnalyser/2012/F%C3%B8dselsstatistik%202011.ashx. (Accessed 4 May 2015)
- Ekstrom A., Abrahamsson H., Eriksson R.M. & Martensson B.L. (2014) Women's use of nipple shields – their influence on breastfeeding duration after a process‐oriented education for health professionals. Breastfeeding Medicine 9, 458–466. [DOI] [PubMed] [Google Scholar]
- Elo S. & Kyngas H. (2008) The qualitative content analysis process. Journal of Advanced Nursing 62, 107–115. [DOI] [PubMed] [Google Scholar]
- Graneheim U.H. & Lundman B. (2004) Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse EducationToday 24, 105–112. [DOI] [PubMed] [Google Scholar]
- Hanna S., Wilson M. & Norwood S. (2013) A description of breast‐feeding outcomes among U.S. mothers using nipple shields. Midwifery 29, 616–621. [DOI] [PubMed] [Google Scholar]
- Kramer M.S., Barr R.G., Dagenais S., Yang H., Jones P., Ciofani L. et al. (2001) Pacifier use, early weaning, and cry/fuss behavior: a randomized controlled trial. JAMA 18, 322–326. [DOI] [PubMed] [Google Scholar]
- Krause K.M., Lovelady C.A. & Ostbye T. (2011) Predictors of breastfeeding in overweight and obese women: data from Active Mothers Postpartum (AMP). Maternal and Child Health Journal 15, 367–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronborg H. & Vaeth M. (2004) The influence of psychosocial factors on the duration of breastfeeding. Scandinavian Journal of Public Health 32, 210–216. [DOI] [PubMed] [Google Scholar]
- Kronborg H. & Vaeth M. (2009) How are effective breastfeeding technique and pacifier use related to breastfeeding problems and breastfeeding duration? Birth 36, 34–42. [DOI] [PubMed] [Google Scholar]
- Kronborg H., Vaeth M. & Kristensen I. (2012) The effect of early postpartum home visits by health visitors: a natural experiment. Public Health Nursing 29, 289–301. [DOI] [PubMed] [Google Scholar]
- Kronborg H., Vaeth M., Olsen J., Iversen L. & Harder I. (2007) Effect of early postnatal breastfeeding support: a cluster‐randomized community based trial. Acta Paediatrica 96, 1064–1070. [DOI] [PubMed] [Google Scholar]
- McClellan H.L., Hepworth A.R., Kent J.C., Garbin C.P., Williams T.M., Hartmann P.E. et al. (2012) Breastfeeding frequency, milk volume, and duration in mother–infant dyads with persistent nipple pain. Breastfeeding Medicine 7, 275–281. [DOI] [PubMed] [Google Scholar]
- McKechnie A.C. & Eglash A. (2010) Nipple shields: a review of the literature. Breastfeeding Medicine 5, 309–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier P.P., Brown L.P., Hurst N.M., Spatz D.L., Engstrom J.L., Boruck L.C. et al. (2000) Nipple shields for preterm infants: effect on milk transfer and duration of breastfeeding. Journal of Human Lactation 16, 106–114. [DOI] [PubMed] [Google Scholar]
- Natland S.T., Andersen L.F., Nilsen T.I., Forsmo S. & Jacobsen G.W. (2012) Maternal recall of breastfeeding duration twenty years after delivery. BMC Medical Research Methodology 12, 179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pincombe J., Baghurst P., Antoniou G., Peat B., Henderson A. & Reddin E. (2008) Baby Friendly Hospital Initiative practices and breast feeding duration in a cohort of first‐time mothers in Adelaide, Australia. Midwifery 24, 55–61. [DOI] [PubMed] [Google Scholar]
- Powers D. & Tapia V.B. (2004) Women's experiences using a nipple shield. Journal of Human Lactation 20, 327–334. [DOI] [PubMed] [Google Scholar]
- Ramsay D.T. & Hartmann P.E. (2005) Milk removal from the breast. Breastfeeding Review 13, 5–7. [PubMed] [Google Scholar]
- Ramsay D.T., Kent J.C., Owens R.A. & Hartmann P.E. (2004) Ultrasound imaging of milk ejection in the breast of lactating women. Pediatrics 113, 361–367. [DOI] [PubMed] [Google Scholar]
- Riordan J. (2005) Breastfeeding and Human Lactation, 3rd edn, pp 200 Jones and Bartlett Publisher: Boston. [Google Scholar]
- Taylor J.S., Risica P.M., Gelle L., Kirtania U. & Cabral H.J. (2006) Duration of breastfeeding among first‐time mothers in the United States: results of a national survey. Acta Paediatrica 95, 980–984. [DOI] [PubMed] [Google Scholar]
- Wagner E.A., Chantry C.J., Dewey K.G. & Nommsen‐Rivers L.A. (2013) Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics 132, e865–e875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, UNICEF (2009) Data Baby‐friendly Hospital Initiative: revised, updated and expanded for integrated care. Section 1: background and implementation. WHO Library Cataloguing‐in‐Publication, the World Health Organization, UNICEF and Wellstart International. Available at: http://whqlibdoc.who.int/publications/2009/9789241594967_eng.pdf?ua=1&ua=1 (Accessed 4 May 2015).
- World Health Organization (1991) Indicators for assessing breastfeeding practices. World Health Organization, Division of Child Health and Development, Geneva. Available at: http://www.who.int/maternal_child_adolescent/documents/cdd_ser_91_14/en/ (Accessed 4 May 2015).
- Wilson‐Clay B. (1996) Clinical use of silicone nipple shields. Journal of Human Lactation 12, 279–285. [DOI] [PubMed] [Google Scholar]
- Woolridge M.W., Baum J.D. & Drewett R.F. (1980) Effect of a traditional and of a new nipple shield on sucking patterns and milk flow. Early Human Development 4, 357–364. [DOI] [PubMed] [Google Scholar]
- StataCorp (2011) Stata Statistical Software: Release 12. StataCorp LP: College Station, TX. [Google Scholar]
- Statistics Denmark . (2013) Immigrants in Denmark. Available at: http://www.dst.dk/pukora/epub/upload/17961/indv2013.pdf. (Accessed 4 May 2015).


