Abstract
Socioeconomic inequalities in child undernutrition remain one of the main challenges in Bangladesh. The social determinants of health are mostly responsible for such inequalities across different population groups. However, no study has examined the relative contribution of different social determinants to the socioeconomic inequality in child undernutrition in Bangladesh. Our objective is to measure the extent of socioeconomic‐related inequalities in childhood stunting and identify the key social determinants that potentially explain these inequalities in Bangladesh. We used data for children younger than 5 years of age for this analysis from 2 rounds of Bangladesh Demographic and Health Surveys conducted in 2004 and 2014. We examined the socioeconomic inequality in stunting using the concentration curve and concentration index. We then decomposed the concentration index into the contributions of individual social determinants. We found significant inequality in stunting prevalence. The negative concentration index of stunting indicated that stunting was more concentrated among the poor than among the well‐off. Our results suggest that inequalities in stunting increased between 2004 and 2014. Household economic status, maternal and paternal education, health‐seeking behavior of the mothers, sanitation, fertility, and maternal stature were the major contributors to the disparity in stunting prevalence in Bangladesh. Equity is a critical component of sustainable development goals. Health policymakers should work together across sectors and develop strategies for effective intersectoral actions to adequately address the social determinants of equity and reduce inequalities in stunting and other health outcomes.
Keywords: Bangladesh, decomposition, low‐income countries, socioeconomic factors, stunting, undernutrition
1. INTRODUCTION
Stunting is considered an irreversible outcome of inadequate nutrition and repeated infection during the first 1,000 days of a child's life (Black et al., 2008; Olofin et al., 2013; Victora et al., 2008). It is associated with increased morbidity and mortality and has long‐term effects on individuals including poor cognitive and physical development, reduced productivity, and increased risk of future metabolic disease (Olofin et al., 2013). Additionally, stunted girls are at increased risk for obstetric problems and associated mortality (Martorell & Zongrone, 2012). All of these reduce the capacity of a child to develop to their full potential and contribute to economic development of the country (Prendergast & Humphrey, 2014; Victora et al., 2008).
In 2011, it was estimated that globally, about 165 million children were stunted (Black et al., 2013). By 2020, if current trends continue, 132 million children younger than 5 years will be stunted in Asia and Africa only (de Onis, Blossner, & Borghi, 2012) and 127 million globally by 2025. So despite increased efforts in curbing stunting rates, it will remain a major public health problem in many parts of the world. This would also mean that we would fail to achieve the World Health Assembly global stunting target of 100 million for 2025. In Bangladesh, stunting is a significant public health problem with prevalence in children younger than 5 years at 36% in 2014 (NIPORT & ICF International, 2016).
Typically, in low‐ and middle‐income countries, stunting is more common in low‐socioeconomic groups. Several studies have shown that children from higher socioeconomic status (SES) have lesser risk of stunting compared to their lower SES counterparts (Menezes et al., 2011; Mostafa, 2011; Rahman & Chowdhury, 2007; Said‐Mohamed, Allirot, Sobgui, & Pasquet, 2009; Vella, Tomkins, Borghesi, Migliori, & Oryem, 1994). Inequalities in stunting among different socioeconomic strata of the population remain one of the main challenges for public health throughout the world. It is important that we understand patterns, trends, and causes of inequalities in stunting and other forms of undernutrition and use these insights to guide national level programs to target and deliver interventions to the most vulnerable groups. This equity consideration for all health and nutrition outcomes has been highlighted in the Sustainable Development Goals.
Although inequalities in stunting can result from differential access to food and health care and/or differences in health‐seeking behaviors, there is ample evidence in the literature that suggests other social determinants of health play an important role in determining child nutritional status (Chirande et al., 2015; Fenske, Burns, Hothorn, & Rehfuess, 2013; Ikeda, Irie, & Shibuya, 2013; Keino, Plasqui, Ettyang, & van den Borne, 2014; Tiwari, Ausman, & Agho, 2014). The UNICEF conceptual framework of undernutrition has identified poverty and food insecurity, maternal and child care practices, limited access to health services, poor health environment (water, sanitation, and hygiene), gender inequities, and limited education as the underlying determinants of undernutrition (UNICEF, 2009). The complex interaction between these underlying factors makes it very challenging to control stunting despite being considered as a preventable condition.
In order for us to mitigate increased socioeconomic inequalities in stunting and overall child health, a key step is to first identify those factors that make the greatest contributions towards the observed inequalities. Although the social determinants of stunting are fairly well known in Bangladesh (Fakir & Khan, 2015; Jesmin, Yamamoto, Malik, & Haque, 2011; Mostafa, 2011; Rahman & Chowdhury, 2007) and elsewhere (Correia et al., 2014; Esfarjani, Roustaee, Mohammadi, & Esmaillzadeh, 2013; Fenske et al., 2013; Ikeda et al., 2013; Keino et al., 2014; Rannan‐Eliya et al., 2013; Semali, Tengia‐Kessy, Mmbaga, & Leyna, 2015; Tiwari et al., 2014; Wolde, Berhan, & Chala, 2015), the determinants of socioeconomic inequalities in stunting are less well studied. There is increasing interest in understanding the underlying causes of inequalities in stunting, to know whether determinants of stunting are distributed differently by wealth or socioeconomic status of the households.
There are few studies, which have assessed the levels of socioeconomic inequalities in nutrition using concentration indices. The concentration index quantifies the degree of socioeconomic inequalities in health and nutrition and can also be decomposed into the relative contribution of factors leading to this inequality (O'Donnell, Van Doorslaer, Wagstaff, & Lindelow, 2008). Decomposition analysis is a technique, which allows quantification of the independent contribution of different determinants to a particular outcome and population. It can provide insights on pathways, through which health and nutrition inequalities occur (O'Donnell et al., 2008). However, very few studies have decomposed inequalities in nutrition or stunting in particular (Novignon, Aboagye, Agyemang, & Aryeetey, 2015). Moreover, there is no reported study that has attempted decomposition of health or nutrition inequalities in the Bangladesh context.
We selected stunting as the outcome for our analysis because it is widely regarded as the most important indicator of overall child nutrition, and it reflects the cumulative effects of inadequate nutrition, and/or chronic, or recurrent acute illness during the most important periods of growth and development in early life. It also has long‐term consequences on economic productivity and is associated with increased maternal morbidity and mortality (Prendergast & Humphrey, 2014). This paper aims to identify the factors that potentially explain the socioeconomic‐related inequalities in child stunting in Bangladesh by decomposing those inequalities into relative contributions from a set of known determinants of stunting. This paper will highlight the important contribution of broader economic, physical, and social environmental factors to inequalities in childhood stunting. This will help policymakers to devise appropriate multisector nutrition plan and actions to enhance intersector collaborations to tackle inequalities in stunting.
Key messages.
The socioeconomic‐related inequalities in stunting have increased over time in Bangladesh.
Household wealth status, maternal and paternal schooling, access to health services, shorter birth interval, maternal short stature, and improved sanitation significantly contribute to the socioeconomic inequality in stunting.
Public health interventions directed towards reducing undernutrition should address the broader economic, physical, and social environmental factors as well as access to health care to reduce socioeconomic inequality and achieve equity‐oriented universal health coverage.
2. METHODS
2.1. Population and data
We used data for children younger than 5 years of age for this analysis from two rounds of Bangladesh Demographic and Health Surveys (BDHS) conducted in 2004 and 2014. Demographic and Health Surveys are one of the key sources of information on fertility, reproductive health, nutrition, mortality, and HIV/AIDS health behaviors in low‐ and middle‐income countries. In each survey, a nationally representative sample of households is obtained through a two‐stage stratified cluster sampling method. Our analysis used women and children's survey weights to make summary data representative of the Bangladesh population.
BDHS collected anthropometric data for all children younger than 5 years from all households. Trained personnel measured the recumbent length of children aged younger than 24 months and the standing height of older children. Children were included in our analysis if they had no missing values for any anthropometric measurements and have complete information of their mothers. The final sample was composed of 5,911 in 2004 and 6,965 in 2014, for whom complete and credible anthropometric and age data were available.
2.2. Variables
2.2.1. Measurement of stunting
To measure the extent of socioeconomic inequality and the proportions of stunting across different social determinants of health, we used a binary variable that indicated whether or not the child was stunted (i.e., two standard deviations or more below the mean of the WHO reference population; de Onis, Onyango, Borghi, Garza, & Yang, 2006). We used height‐for‐age z‐scores to measure the contribution of each determinant to the socioeconomic‐related inequality of stunting as proposed by Wagstaff and van Doorslaer in a previous study (Wagstaff, van Doorslaer, & Watanabe, 2003).
2.2.2. Socioeconomic indicators
The most direct measures of living standards are income and consumption. As the BDHS does not collect information on household income and expenditure, we have used principal components analysis to construct a wealth index from available information on assets. The wealth index scores originally provided by the BDHS were estimated separately and were not comparable across survey years. Therefore, to compute the household wealth index scores on a single common scale across surveys, we pooled data sets and conducted a principal component analysis on household possession of 12 durable assets and housing materials (Filmer & Pritchett, 2001). We used information on ownership of household assets (such as TVs, radios, bicycles, motorcycles/scooters, tables, chairs, and wardrobes), housing materials (floor, wall, and roof materials), access to utilities (electricity, safe water, and clean energy), and house and land ownership, to construct the household wealth index. We later grouped the wealth index score into quintiles with Quintile 1 representing the poorest segment of the population and Quintile 5, the wealthiest.
2.2.3. Social determinants of health
Social determinants of health that are used in this study are factors with known or plausible links to stunting and thus may be related to inequalities in stunting. We included several variables linked to socioeconomic and material conditions (wealth quintiles, education of the parents, mother's current employment status, and sanitation conditions); geographical area (regions); and indicators of health service utilization (antenatal care by medically trained provider and facility delivery). The demographic variables included were age of mother at the time of the child birth, height of the mother, birth order, and the preceding birth interval. The rationale for this selection has been discussed in a previous study done in Bangladesh by Headey, Hoddinott, Ali, Tesfaye, & Dereje (2015).
All variables were categorical and coded as follows:
Mother's age in years at birth (<20 years, between 21 and 34 years, and between 35 and 49 years).
Mother's height in centimeters was categorized into two groups (≤145 cm and >145 cm).
Birth order was defined as 1, 2, 3 and older than 4.
Preceding birth interval was categorized into four groups (≤24 months, 25–36 months, 37–48 months, and >48 months).
Geographical area was based on the region in which each respondent was residing (Barisal, Chittagong, Dhaka, Khulna, Rajshahi, Sylhet, and Rangpur).
Prenatal care from a medically trained provider cluster (yes or no).
Delivery at a health care facility (yes or no).
Both maternal and paternal education were categorized into four groups of highest level of education received (no education or primary or secondary or tertiary).
Wealth index was categorized quintiles (1–5), with 1 the lowest.
Availability of improved sanitation (yes or no). We have used the definition of improved sanitation as used in BDHS 2014 report (NIPORT & ICF International, 2016).
Current employment status of the mother (yes or no).
2.3. Ethical consideration
All study participants gave informed consent before participation, and all information was collected confidentially. The data are publicly available with all identifier information removed.
2.4. Statistical analysis
We took into account the complex sampling method (i.e., stratification, clustering, and sample weights) in estimating summary statistics for the variables at the population level. We used stata svy command to adjust our analysis for the complex sampling design of BDHS. The absolute differences in prevalence estimates in stunting were expressed as percentages comparing the 2004 and 2014 surveys. In all comparisons, differences were estimated using chi‐square to test the significance of differences at p < .01.
We measured socioeconomic inequality in the prevalence of stunting using the concentration curve and the concentration index. We used stata commands igini and clorenz to measure the concentration indices and to plot the concentration curves. The concentration curve is a plot of the cumulative percentage of stunting on the y axis and cumulative percentage of the population ranked by wealth index on the x axis. The 45° line represents perfect equality. The further the curve is from the line of equality, the higher the degree of health inequality. If the curve lies below the line, the outcome is more concentrated among the higher SES individuals in the population, and if it lies above the line, the outcome is more concentrated among the lower SES individuals in the population (O'Donnell et al., 2008).
The concentration index, which measures the magnitude of inequality, is twice the area between the concentration curve and the line of perfect equality. It is calculated as twice the weighted covariance between the outcome and the fractional rank in the wealth distribution divided by the variable mean (O'Donnell et al., 2008).
Its value can range between −1 and 1. A negative value indicates the concentration of the outcome variable (stunting in our study) in the poorer population or pro‐poor inequality; whereas, a positive value indicates the opposite (pro‐rich inequality). A zero value represents perfect equality. We plotted the curves and developed the concentration index for 2004 and 2014.
We then decomposed the concentration index to understand the relative contribution of different social determinants to the stunting inequality. Wagstaff et al. showed that a linear regression equation relating a dependent health variable to a set of predictor variables can be used to decompose the observed inequality as expressed by concentration index into the contributions of several factors. Each contribution is the product of the sensitivity of the dependent heath variable with respect to that factor and the degree of socioeconomic‐related inequality in that factor. We used Stata version 13.1 (Stata Corp LP, College Station, United States of America) for all statistical analyses. All stata commands for the decomposition analysis have already been published elsewhere (O'Donnell et al., 2008; Wagstaff et al., 2003).
3. RESULTS
3.1. Characteristics of the study population and rate of stunting across different social determinants of health
We present the characteristics of the study population for the two survey period (Table 1). Women's height has increased over the past decade across the country. We also observed major improvement in the use of maternal health services, education, sanitation, and economic status during the same time. Birth order and birth interval also showed significant improvement.
Table 1.
Descriptive statistics of the cohort at each of the two study period (weighted frequency)
| Variables (2004 and 2014) | 2004 (5,977) | 2014 (7,173) | ||
|---|---|---|---|---|
| N | % | N | % | |
| Mother's age at birth | ||||
| Less than 20 | 1,944 | 33 | 2,258 | 31 |
| Between 21 and 34 | 3,712 | 62 | 4,640 | 65 |
| Between 35 and 49 | 320 | 5 | 274 | 4 |
| Mother's height in cm | ||||
| Less than 147 cm | 1,655 | 28 | 1,679 | 23 |
| Between 147 and 150 cm | 1,515 | 25 | 1,856 | 26 |
| Between 150 and 154 cm | 1,444 | 24 | 1,746 | 24 |
| More than 154 cm | 1,363 | 23 | 1,892 | 26 |
| Birth order | ||||
| 1 | 1,709 | 29 | 2,754 | 38 |
| 2 | 1,538 | 26 | 2,155 | 30 |
| 3 | 1,114 | 19 | 1,174 | 16 |
| >4 | 1,615 | 27 | 1,089 | 15 |
| Birth interval | ||||
| Equal or less than 24 months | 783 | 18 | 566 | 13 |
| Between 25 and 36 months | 1,084 | 25 | 806 | 18 |
| Between 37 and 48 months | 867 | 20 | 662 | 15 |
| More than 48 months | 1,529 | 36 | 2,372 | 54 |
| Child's current age | ||||
| 0 | 1,145 | 19 | 1,407 | 20 |
| 1 | 1,182 | 20 | 1,542 | 21 |
| 2 | 1,205 | 20 | 1,422 | 20 |
| 3 | 1,239 | 21 | 1,402 | 20 |
| 4 | 1,207 | 20 | 1,400 | 20 |
| Region | ||||
| Barisal | 355 | 6 | 1,516 | 21 |
| Chittagong | 1,325 | 22 | 2,517 | 35 |
| Dhaka | 1,834 | 31 | 546 | 8 |
| Khulna | 649 | 11 | 755 | 11 |
| Rajshahi | 1,323 | 22 | 728 | 10 |
| Sylhet | 490 | 8 | 698 | 10 |
| Rangpura | ||||
| Prenatal care from a medically trained provider | ||||
| No | 2,476 | 52 | 1,549 | 39 |
| Yes | 2,307 | 48 | 2,468 | 61 |
| Delivery at a health care facility | ||||
| Home | 5,380 | 90 | 2,693 | 62 |
| Facility | 583 | 10 | 1,672 | 38 |
| Husband's education level | ||||
| No education | 2,388 | 40 | 1,850 | 26 |
| Primary level | 1,638 | 27 | 2,160 | 30 |
| Secondary level | 1,396 | 23 | 2,191 | 31 |
| Tertiary level | 551 | 9 | 970 | 14 |
| Mother's education level | ||||
| No education | 2,236 | 37 | 1,169 | 16 |
| Primary level | 1,875 | 31 | 2,008 | 28 |
| Secondary level | 1,564 | 26 | 3,324 | 46 |
| Tertiary level | 302 | 5 | 671 | 9 |
| Asset quintile—may need to use year wise | ||||
| Lowest | 2,737 | 46 | 457 | 6 |
| Second | 1,417 | 24 | 1,022 | 14 |
| Middle | 1,034 | 17 | 1,550 | 22 |
| Fourth | 701 | 12 | 1,799 | 25 |
| Highest | 88 | 1 | 2,344 | 33 |
| Improved sanitation and/or toilet | ||||
| No | 2,466 | 42 | 2,127 | 33 |
| Yes | 3,393 | 58 | 4,387 | 67 |
| Women currently working | ||||
| No | 4,917 | 82 | 5,291 | 74 |
| Yes | 1,060 | 18 | 1,881 | 26 |
Rangpur was not a separate division in 2004.
Table 2 shows the prevalence of stunting in 2004 and 2014 across different social determinants of health. Stunting rates in children aged 0–59 months dropped from 43% to 36% between 2004 and 2011 (i.e., a 7% absolute reduction, or an average relative reduction of 1.6% per year in 10 years). Between 2004 and 2014, stunting has decreased across all social determinants of health. The reduction in stunting prevalence was greatest in Dhaka and Sylhet divisions (10% point) and lowest in Kuhlna (4% point).
Table 2.
Percentages of stunting in 2004 and 2014 across different social determinants of health
| Proportion (95% CI) | Absolute change (%) | ||
|---|---|---|---|
| 2004 | 2014 | ||
| Mother's agea | |||
| <20 years | 44.9 (42.6, 47.2) | 37.1 (34.2, 40.1) | −8* |
| 21–34 years | 41.4 (39.0, 43.9) | 35.3 (33.4, 37.3) | −6* |
| 35–49 years | 49.9 (43.4, 56.3) | 44.3 (37.7, 50.9) | −6* |
| Mother's height in cm | |||
| ≤145 cm | 61.7 (57.9, 65.5) | 56.5 (52.2, 60.8) | −5* |
| >145 cm | 39.4 (37.5, 41.4) | 33.1 (31.4, 34.9) | −6* |
| Birth order | |||
| First born | 40.1 (37.6, 42.6) | 31.7 (29.3, 34.1) | −8 |
| Second born | 38.8 (36.0, 41.7) | 35.8 (33.0, 38.6) | −3 |
| Third born | 42.2 (38.2, 46.2) | 37.0 (33.3, 40.7) | −5 |
| Fourth or later born | 50.7 (47.8, 53.5) | 47.8 (43.9, 51.7) | −3 |
| Preceding birth interval | |||
| <24 months | 49.8 (45.5, 54.1) | 48.4 (42.9, 53.9) | −1 |
| 25–36 months | 50.8 (47.8, 53.8) | 45.7 (40.8, 50.5) | −5* |
| 37–48 months | 44.1 (40.5, 47.6) | 39.8 (34.8, 44.8) | −4* |
| >48 months | 36.6 (33.4, 39.9) | 34.6 (32.1, 37.0) | −2 |
| Region | |||
| Barisal | 49.0 (44.4, 53.6) | 40.0 (35.5, 44.5) | −9* |
| Chittagong | 46.2 (42.6, 49.9) | 38.0 (34.3, 41.6) | −8* |
| Dhaka | 44.6 (40.7, 48.6) | 34.1 (30.3, 38.0) | −10* |
| Khulna | 32.0 (26.9, 37.2) | 27.9 (24.2, 31.6) | −4* |
| Rajshahi | 40.2 (36.3, 44.1) | 30.9 (27.4, 34.3) | −9* |
| Sylhet | 46.2 (42.1, 50.3) | 36.6 (32.3, 40.8) | −10* |
| Rangpurb | 49.9 (45.8, 53.9) | ||
| Prenatal care from a medically trained provider | |||
| No | 47.2 (44.7, 49.8) | 43.1 (38.8, 47.3) | −4* |
| Yes | 35.1 (33.3, 36.9) | 28.3 (26.1, 30.4) | −7* |
| Delivery at a health facility | |||
| No | 45.1 (43.2, 47.0) | 37.6 (35.2, 40.1) | −7* |
| Yes | 23.7 (20.2, 27.1) | 24.3 (21.5, 27.1) | 1 |
| Husband's education level | |||
| No education | 49.7 (47.1, 52.3) | 48.1 (44.8, 51.5) | −2 |
| Any primary | 44.3 (41.4, 47.2) | 40.6 (38.0, 43.1) | −4* |
| Any secondary | 37.5 (34.5, 40.5) | 29.6 (27.1, 32.2) | −8* |
| Any tertiary | 24.0 (20.2, 27.8) | 18.9 (15.9, 21.8) | −5* |
| Mother's education level | |||
| No education | 50.4 (47.9, 52.9) | 47.5(42.552.5) | −3* |
| Any primary | 45.6 (42.6, 48.6) | 43.9(40.946.9) | −2 |
| Any secondary | 34.7 (32.1, 37.4) | 31.0(29.033.1) | −4* |
| Any tertiary | 15.3 (10.9, 19.7) | 19.7(16.123.2) | 4* |
| Wealth quintile | |||
| Lowest | 54.4 (51.5. 57.3) | 49.4(45.653.2) | −5* |
| Second | 47.0 (43.5, 50.4) | 42.3(39.245.4) | −5* |
| Middle | 42.5 (39.1, 45.9) | 36.2(33.339.1) | −6* |
| Fourth | 39.8 (36.5, 43.0) | 31.3(27.635.0) | −8* |
| Highest | 25.1 (21.9, 28.2) | 19.5(16.622.3) | −6* |
| Improved sanitation | |||
| No | 49.9 (47.4, 52.5) | 45.1(42.148.0) | −5* |
| Yes | 37.7 (35.5, 40.0) | 32.4(30.334.4) | −5* |
| Mother's employment status | |||
| Currently not working | 41.5 (39.4, 43.6) | 34.3(32.536.2) | −7* |
| Currently working | 46.9 (43.8, 50.0) | 41.6(38.145.0) | −5* |
| Overall | 43.0 (41.1, 44.9) | 36.2(34.538.0) | −7* |
Note. CI = confidence interval.
Data at the time of the birth of child included in the analysis.
Rangpur was not a separate division in 2004.
p value<.01.
3.2. Measurement of socioeconomic inequalities
Figure 1 shows concentration curves and concentration index of stunting in four survey years. Concentration curves for all periods lie above the diagonal line of 45°, indicating that stunting prevalence is higher in people with lower income than those with higher income. Over time, the curves shift further from the line of equality, reflecting increasing socioeconomic‐related inequalities. The concentration indices for stunting progressively increase from −0.094 (95% confidence interval (CI) [−0.111, −0.077]) in 2004 to −0.164 (95% CI [−0.181, −0.147]) in 2014.
Figure 1.
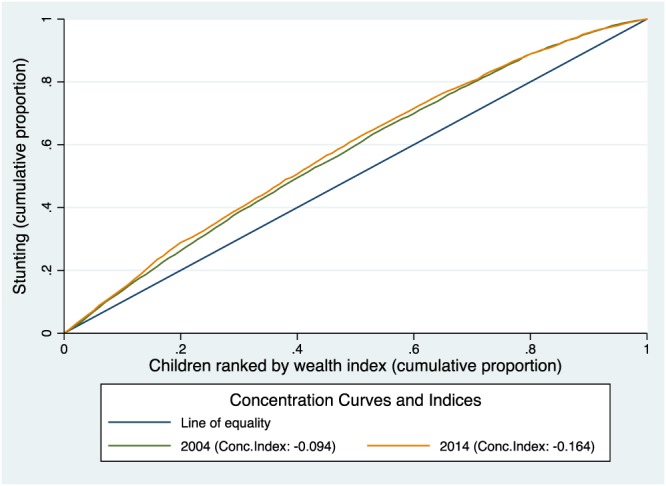
Concentration curves of cumulative stunting by wealth quintile and concentration index of stunting in survey period: 2004 and 2014
3.3. Contribution of the determinants to socioeconomic‐related inequality (decomposition of the concentration index)
We examined the concentration index of each variable included as a determinant in our analysis. The “CI” column of Table 3 presents the degree of socioeconomic inequality (concentration index) in each of the variables separately for 2004 and 2014. We found that children from working mother or from mother who were short in stature, aged 35 or older at the time of birth, and had short‐preceding birth interval were concentrated among the less affluent population. On the other hand, children from mothers who had tertiary level education, prenatal checkup from a medically trained provider, and had her last birth in a facility were concentrated among the better off.
Table 3.
Contribution of factors based on decomposition of concentration index analysis for stunting 2004 and 2014
| 2004 | 2014 | |||||||
|---|---|---|---|---|---|---|---|---|
| Elasticity | Concentration index | Absolute contribution | Percent contribution (%) | Elasticity | Concentration index | Absolute contribution | Percent contribution (%) | |
| Mother's agea | ||||||||
| <20 years | ||||||||
| 21–34 years | 0.021 | 0.017 | 0.000 | 0 | −0.002 | 0.027 | 0.000 | 0 |
| 35–49 years | 0.001 | −0.126 | 0.000 | 0 | 0.004 | −0.103 | 0.000 | 0 |
| Subtotal | 0.000 | 0 | 0.000 | 0 | ||||
| Mother's height in cm | ||||||||
| ≤145 cm | ||||||||
| >145 cm | −0.317 | 0.017 | −0.005 | 5 | −0.295 | 0.022 | −0.006 | 5 |
| Birth order | ||||||||
| First born | ||||||||
| Second born | 0.000 | 0.061 | 0.000 | 0 | −0.018 | 0.043 | −0.001 | 1 |
| Third born | −0.002 | −0.025 | 0.000 | 0 | −0.013 | −0.083 | 0.001 | −1 |
| Fourth or later born | 0.021 | −0.177 | −0.004 | 3 | 0.000 | −0.231 | 0.000 | 0 |
| Subtotal | −0.004 | 3 | 0.000 | 0 | ||||
| Preceding birth interval | ||||||||
| <24 months | ||||||||
| 25–36 months | −0.008 | −0.096 | 0.001 | −1 | 0.006 | −0.087 | −0.001 | 0 |
| 37–48 months | −0.020 | −0.040 | 0.001 | −1 | −0.003 | −0.036 | 0.000 | 0 |
| >48 months | −0.070 | 0.108 | −0.008 | 7 | −0.057 | 0.053 | −0.003 | 2 |
| Subtotal | −0.006 | 5 | −0.003 | 3 | ||||
| Region | ||||||||
| Barisal | ||||||||
| Chittagong | −0.025 | 0.019 | 0.000 | 0 | 0.010 | 0.138 | 0.001 | −1 |
| Dhaka | −0.027 | 0.018 | 0.000 | 0 | −0.003 | 0.198 | −0.001 | 1 |
| Khulna | −0.027 | 0.117 | −0.003 | 3 | 0.002 | 0.028 | 0.000 | 0 |
| Rajshahi | −0.039 | −0.135 | 0.005 | −5 | −0.012 | −0.070 | 0.001 | −1 |
| Sylhet | −0.024 | 0.054 | −0.001 | 1 | 0.001 | −0.208 | 0.000 | 0 |
| Rangpurb | 0.000 | 0.000 | 0.000 | 0 | 0.020 | −0.083 | −0.002 | 1 |
| Subtotal | 0.000 | 0 | 0.000 | 0 | ||||
| Prenatal care from a medically trained provider | ||||||||
| No | ||||||||
| Yes | −0.066 | 0.235 | −0.016 | 14 | −0.063 | 0.149 | −0.009 | 8 |
| Delivery at a health care facility | ||||||||
| No | ||||||||
| Yes | −0.010 | 0.559 | −0.005 | 5 | −0.020 | 0.297 | −0.006 | 5 |
| Husband's education level | ||||||||
| No education | ||||||||
| Any primary | −0.010 | −0.023 | 0.000 | 0 | −0.030 | −0.154 | 0.005 | −4 |
| Any secondary | −0.008 | 0.256 | −0.002 | 2 | −0.021 | 0.190 | −0.004 | 3 |
| Any tertiary | −0.006 | 0.612 | −0.004 | 4 | −0.022 | 0.535 | −0.012 | 9 |
| −0.006 | 5 | −0.011 | 9 | |||||
| Mother's education level | ||||||||
| No education | ||||||||
| Any primary | −0.005 | −0.045 | 0.000 | 0 | −0.019 | −0.243 | 0.005 | −4 |
| Any secondary | −0.028 | 0.315 | −0.009 | 8 | −0.073 | 0.135 | −0.010 | 8 |
| Any tertiary | −0.015 | 0.689 | −0.011 | 9 | −0.046 | 0.564 | −0.026 | 21 |
| −0.019 | 17 | −0.031 | 26 | |||||
| Wealth quintile | ||||||||
| Lowest (Poorest) | ||||||||
| Second | −0.013 | 0.075 | −0.001 | 1 | 0.007 | −0.563 | −0.004 | 3 |
| Middle | −0.017 | 0.394 | −0.007 | 6 | −0.020 | −0.439 | 0.009 | −7 |
| Fourth | −0.015 | 0.680 | −0.010 | 9 | −0.006 | 0.033 | 0.000 | 0 |
| Highest (Wealthiest) | −0.004 | 0.810 | −0.003 | 3 | −0.050 | 0.639 | −0.032 | 26 |
| −0.021 | 18 | −0.028 | 23 | |||||
| Improved sanitation | ||||||||
| No | ||||||||
| Yes | −0.036 | 0.232 | −0.008 | 7 | −0.021 | 0.183 | −0.004 | 3 |
| Mother's employment status | ||||||||
| Currently not working | ||||||||
| Currently working | 0.009 | −0.125 | −0.001 | 1 | 0.030 | −0.101 | −0.003 | 3 |
Note. CI = confidence interval, OR = odds ratio from multivariate hierarchical logistic model.
Data at the time of the birth of child included in the analysis.
Rangpur was not a separate division in 2004.
We then examined the contribution of each determinant to socioeconomic‐related inequality in stunting. The columns under the heading “Absolute contribution” and “percent contribution” in Table 3 present the absolute contribution (in the same units as the concentration index) and relative contributions (adjusted percentage contribution to inequality) of each determinant. The results are summarized in Figures 2 and 3. Among the variables, those with the greatest contributions towards inequality in stunting were economic status of the household and parental education. Household economic status as measured by wealth index was responsible for 17% of the inequality in 2004 and 23% of the inequality in 2014; whereas, parental education explained 26% of the socioeconomic‐related inequality in stunting. Access to health services as measured by prenatal care by a medically trained provider and delivery at a health facility also made a significant contribution to stunting inequality explaining 19% and 13% of the total inequality in 2004 and 2014, respectively. Maternal height and improved sanitation also had significant explanatory role in contributing to the stunting inequality in both the study periods. Other determinants including mother's age, preceding birth interval, birth order, the mother's employment status, and region had minimal or no contribution to the inequality in stunting prevalence. Overall, 81% and 84% of the inequality in stunting was explained by the covariates included in the model in 2004 and 2014, respectively.
Figure 2.
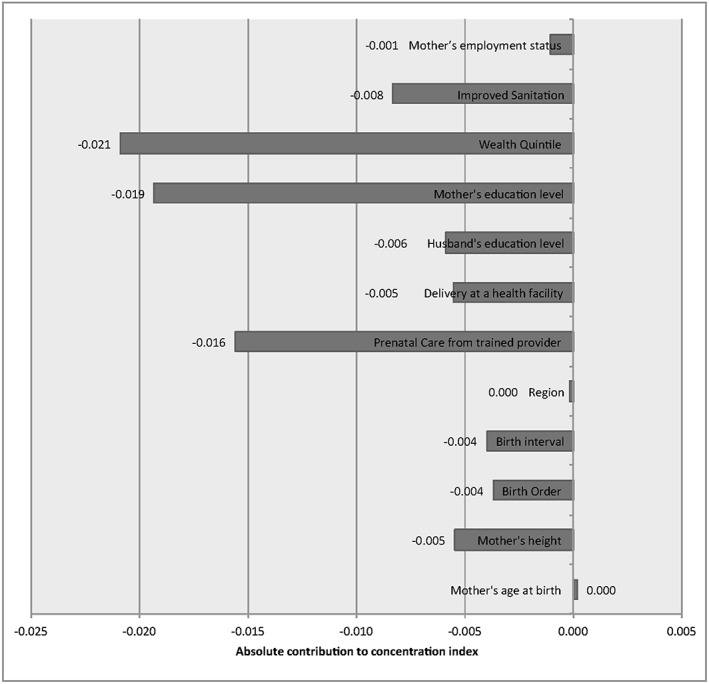
The absolute contribution to concentration indices of socioeconomic‐related inequalities in stunting in Bangladesh by its determinants for the period 2004
Figure 3.
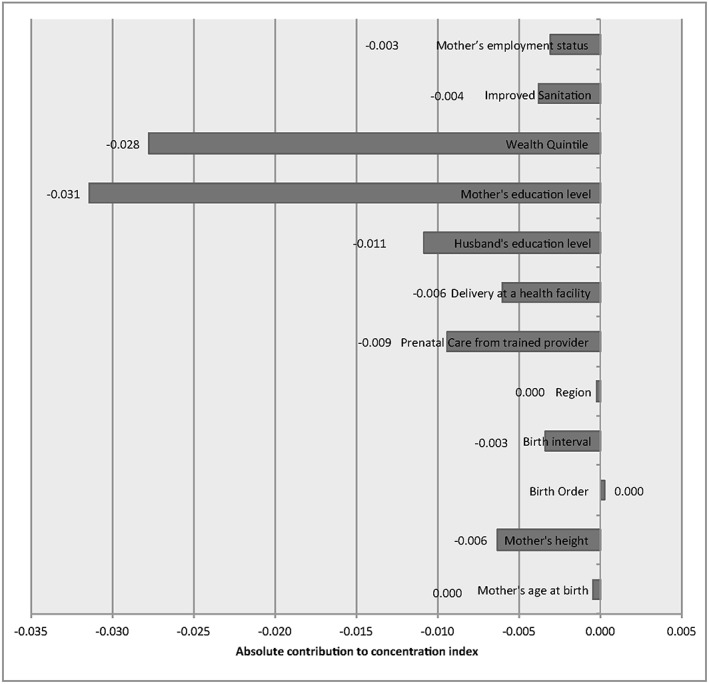
The absolute contribution to concentration indices of socioeconomic‐related inequalities in stunting in Bangladesh by its determinants for the period 2014
4. DISCUSSION
Our decomposition analysis revealed that household wealth status, maternal and paternal schooling, access to health services, shorter birth intervals, maternal short stature, and improved sanitation significantly contributed to the socioeconomic inequality in stunting. The study provides strong evidence that inequalities in stunting are caused by unequal distribution of key socioeconomic determinants between different population groups.
Although stunting prevalence has declined considerably in Bangladesh, the inequality in stunting prevalence has increased. Over the last 2 decades, the Government of Bangladesh has made substantial investments in nutrition sector. The first major investment on nutrition happened in 1996 when government launched the Bangladesh Integrated Nutrition Program. The next phase was National Nutrition Program, which was carried out from 2006 to 2011. In both phases, a range of community‐based nutrition services were provided through contracted nongovernmental organizations. One of the major critique of this approach was none of these nongovernmental organizations had any links with the main stream health system. As a result, both the programs failed to reach a critical mass of population. Bangladesh Integrated Nutrition Program could only cover approximately 16% of the rural population; whereas, National Nutrition Program covered 34% of the rural population. The current program known as National Nutrition Service (2011–2016) has taken more holistic approach. Under this program, the government is implementing a mainstreamed, comprehensive package of nutrition services as well as trying to develop and strengthen the coordination mechanisms with other sectors to ensure a multisectoral response to malnutrition (Saha, Billah, Menon, El Arifeen, & Mbuya, 2015)
All of these programs took a universal approach, although this was difficult to achieve when implementing these programs. Often access and utilization of such services are determined by education income or gender. So the universal approach usually favors those who are already in better positions. As a result, despite such large investments in nutrition, we see socioeconomic equalities in stunting were increasing over the last decade.
Household wealth accounted for the single largest share of the measured degree of socioeconomic‐related inequalities in stunting. The increase in inequality reflects the more rapid reduction in stunting prevalence in the wealthiest quintile of households compared to the poorest quintile. This is consistent with previous studies that have shown the reduction in stunting prevalence in Bangladesh was not accompanied by improved equity (Khan, Kramer, Khandoker, Prufer‐Kramer, & Islam, 2011; Restrepo‐Mendez, Barros, Black, & Victora, 2015). Several studies have reported a strong association between undernutrition and the economic condition of the households (Brcanski, Jovic‐Vranes, Marinkovic, & Favre, 2014; Fakir & Khan, 2015; Tette et al., 2016). Higher income households spend more money on healthy foods. Household socioeconomic status also influences food choice behaviors and health behaviors, which in turn can have diverse impact on health and nutrition status of the population across different socioeconomic groups. In recent years, Bangladesh has achieved impressive economic growth rates (Headey, Hoddinott, & Park, 2016). However, a substantial level of poverty still exists in the country, and our results indicate that the poor and more disadvantaged section of the population is yet to reap the benefits of the rapid economic progress of the country.
Parental education was found to be a significant contributor to socioeconomic inequality in stunting. Studies have shown that there is a strong association between parent's education and undernutrition (Goli, Doshi, & Perianayagam, 2013; Kumar, Kumari, & Singh, 2015). There are various pathways through which parent's education promotes child nutrition. These include acquisition of health knowledge, adherence to recommended feeding practices for children, and increased control over resources (Abuya, Ciera, & Kimani‐Murage, 2012). Bangladesh has achieved a rapid expansion in education, especially female education. Since the early 1990s, the government has implemented a special stipend program to encourage participation of girls in secondary education (Hasan, Soares Magalhaes, Williams, & Mamun, 2015). However, our analysis showed parents with tertiary level education were disproportionately concentrated among the rich. Therefore, greater investment is needed to reduce inequities in education, particularly for women.
Our analysis showed stunting is more concentrated among mothers of short stature. Several studies have documented the intergenerational effects as measured by height of the mother on stunting (Martorell & Zongrone, 2012; Rachmi, Agho, Li, & Baur, 2016; Ramakrishnan, Martorell, Schroeder, & Flores, 1999). Short maternal stature is associated with child stunting, even after adjusting for socioeconomic status. There are several mechanisms that explain intergenerational effects on stunting including genetic characteristics, epigenetic effects, and adverse “environmental” factors (resulting in synergy of undernutrition and infection) the mother experienced in her early hood (Martorell & Zongrone, 2012). A study using data from 54 countries reported that a 1‐cm increase in maternal height was associated with a decreased risk of stunting, absolute risk difference = 0.0126; relative risk = 0.968; 95% CI [0.967, 0.968] (Ozaltin, Hill, & Subramanian, 2010).
Access to health services is an important factor for child growth (Deshmukh, Sinha, & Dongre, 2013; Semali et al., 2015). Our study showed that together, these account for 17% of the total inequality in stunting. Greater access to health services enhances parental capacities to recognize illnesses early and seek treatment for their children. A previous study has shown that prenatal visit to doctors by mothers significantly improves child's height‐for‐age z‐score (Headey et al., 2015). Our findings also reiterate the importance of greater accessibility of health services for nutrition improvement. In Bangladesh, there has been impressive increase in maternal health care utilization rate. Despite the fact health services in Bangladesh are free of charge, health service utilization are highly concentrated among the rich. It is important that we strengthen our efforts targeting the more vulnerable groups to further increase the uptake of maternal, neonatal, and pediatric health services. These should include awareness‐raising about prenatal and postpartum care, explaining where and how these health services may be accessed, emphasis on the importance of early and appropriate treatment of childhood infectious diseases, risks of adolescent pregnancy, and referral services to other medical services.
A previous study has shown that there is association between child stunting with the high fertility of the mother (Headey et al., 2015). The number of pregnancies and births and the intervals between them had consequences for the mother's health, which ultimately affected the child's birth weight as well as the mother's ability to feed and care for her child (Ikeda et al., 2013). Our study findings also support this notion as the decomposition analysis showed birth order and birth interval together contributed 6% of the socioeconomic inequality in 2004.
Similar to finding of other studies, we found inequalities in access to improved sanitation also contributed to socioeconomic inequality in stunting (Aguayo, Nair, Badgaiyan, & Krishna, 2016; Ikeda et al., 2013; Keino et al., 2014). Unsafe drinking water and poor sanitation make young children susceptible to diarrheal illness. These findings highlight the need for increased attention to water, sanitation, and hygiene issues and actions as part of the approaches to prevent childhood stunting.
4.1. Strengths and limitations of the study
A major strength of our study is our use of nationally representative sample survey data because it gave us the opportunity to examine the regional variations in stunting. The major limitation of the study is the use of an asset‐based wealth index as a proxy indicator for household economic status, because Demographic and Health Surveys data do not collect information on household income or expenditure. A previous study has questioned the appropriateness of wealth index as a proxy for consumption expenditure, because the choice of variable had an important influence on the wealth index, and also such an index does not take into account household size or composition (Howe, Hargreaves, & Huttly, 2008). The household wealth index also fails to capture any recent financial shock or disruptions of income. Despite such limitations, the wealth index constructed by Principal Component Analysis (PCA) has been widely used because of scarcity and reliability (e.g., recall bias and seasonality) of household income expenditure data. Moreover, income and consumption data are both expensive and difficult to collect. The other limitation of the study is related to the decomposition analysis. The decomposition of the concentration index is a useful method to identify factors lying behind socioeconomic inequality, but it cannot provide causal inference.
5. CONCLUSION
Health equity is considered as key component of progressive achievement of universal health coverage Sustainable Development Goals (SDG 3). Reducing persistent health inequalities in chronic undernutrition will require diverse range of nutrition‐specific and nutrition‐sensitive intervention both within and outside the health sector. Nutrition‐specific interventions within the health sector are well known. However, strong evidence will be needed to define the most cost‐effective nutrition‐sensitive interventions with integration of other sectors including agriculture, environment, water and sanitation, finance, infrastructure, social welfare, and education. In the short run, countries like Bangladesh that has very high rates of stunting with significant level of inequality could introduce social safety nets programs with nutrition‐specific goals. The government of Bangladesh has recently introduced a conditional cash transfer to improve maternal and child nutrition. However, there is still no strong evidence whether conditional or unconditional cash transfer work best in a country where health system is still under performing. Further research is needed in this area. This paper provides the foundation for policymakers to facilitate and support multisectoral approaches in tackling undernutrition and achieving equity oriented universal health coverage.
SOURCE OF FUNDING
None.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
TMH designed the study and did the statistical analysis. AH, SEA, and MJD contributed to data interpretation and manuscript writing and have read and approved the final submission.
ACKNOWLEDGMENT
We thank MEASURE DHS for granting permission to use the Bangladesh DHS data.
Huda TM, Hayes A, El Arifeen S, Dibley MJ. Social determinants of inequalities in child undernutrition in Bangladesh: A decomposition analysis. Matern Child Nutr. 2018;14:e12440 10.1111/mcn.12440
REFERENCES
- Abuya, B. A. , Ciera, J. , & Kimani‐Murage, E. (2012). Effect of mother's education on child's nutritional status in the slums of Nairobi. BMC Pediatrics, 12, 80. doi: 10.1186/1471-2431-12-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguayo, V. M. , Nair, R. , Badgaiyan, N. , & Krishna, V. (2016). Determinants of stunting and poor linear growth in children under 2 years of age in India: An in‐depth analysis of Maharashtra's comprehensive nutrition survey. Maternal & Child Nutrition, 12(Suppl 1), 121–140. doi: 10.1111/mcn.12259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black, R. E. , Allen, L. H. , Bhutta, Z. A. , Caulfield, L. E. , de Onis, M. , Ezzati, M. , … Child Undernutrition Study Group . (2008). Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet, 371(9608), 243–260. doi: 10.1016/S0140-6736(07)61690-0 [DOI] [PubMed] [Google Scholar]
- Black, R. E. , Victora, C. G. , Walker, S. P. , Bhutta, Z. A. , Christian, P. , de Onis, M. , … Child Nutrition Study Group . (2013). Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet, 382(9890), 427–451. doi: 10.1016/S0140-6736(13)60937-X [DOI] [PubMed] [Google Scholar]
- Brcanski, J. , Jovic‐Vranes, A. , Marinkovic, J. , & Favre, D. (2014). Social determinants of malnutrition among Serbian children aged <5 years: Ethnic and regional disparities. International Journal of Public Health, 59(5), 697–706. doi: 10.1007/s00038-014-0591-5 [DOI] [PubMed] [Google Scholar]
- Chirande, L. , Charwe, D. , Mbwana, H. , Victor, R. , Kimboka, S. , Issaka, A. I. , … Agho, K. E. (2015). Determinants of stunting and severe stunting among under‐fives in Tanzania: Evidence from the 2010 cross‐sectional household survey. BMC Pediatrics, 15, 165. doi: 10.1186/s12887-015-0482-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correia, L. L. , Silva, A. C. , Campos, J. S. , Andrade, F. M. , Machado, M. M. , Lindsay, A. C. , … Cunha, A. J. (2014). Prevalence and determinants of child undernutrition and stunting in semiarid region of Brazil. Revista de Saúde Pública, 48(1), 19–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Onis, M. , Blossner, M. , & Borghi, E. (2012). Prevalence and trends of stunting among pre‐school children, 1990‐2020. Public Health Nutrition, 15(1), 142–148. doi: 10.1017/S1368980011001315 [DOI] [PubMed] [Google Scholar]
- de Onis, M. , Onyango, A. W. , Borghi, E. , Garza, C. , & Yang, H. (2006). Comparison of the World Health Organization (WHO) Child Growth Standards and the National Center for Health Statistics/WHO international growth reference: Implications for child health programmes. Public Health Nutrition, 9(7), 942–947. [DOI] [PubMed] [Google Scholar]
- Deshmukh, P. R. , Sinha, N. , & Dongre, A. R. (2013). Social determinants of stunting in rural area of Wardha, Central India. Medical Journal Armed Forces India, 69(3), 213–217. doi: 10.1016/j.mjafi.2012.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esfarjani, F. , Roustaee, R. , Mohammadi, F. , & Esmaillzadeh, A. (2013). Determinants of stunting in school‐aged children of Tehran, Iran. International Journal of Preventive Medicine, 4(2), 173–179. [PMC free article] [PubMed] [Google Scholar]
- Fakir, A. M. , & Khan, M. W. (2015). Determinants of malnutrition among urban slum children in Bangladesh. Health Economics Review, 5(1), 59. doi: 10.1186/s13561-015-0059-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenske, N. , Burns, J. , Hothorn, T. , & Rehfuess, E. A. (2013). Understanding child stunting in India: A comprehensive analysis of socio‐economic, nutritional and environmental determinants using additive quantile regression. PloS One, 8(11), e78692. doi: 10.1371/journal.pone.0078692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filmer, D. , & Pritchett, L. H. (2001). Estimating wealth effects without expenditure data—or tears: An application to educational enrollments in states of India. Demography, 38(1), 115–132. [DOI] [PubMed] [Google Scholar]
- Goli, S. , Doshi, R. , & Perianayagam, A. (2013). Pathways of economic inequalities in maternal and child health in urban India: A decomposition analysis. PloS One, 8(3), e58573. doi: 10.1371/journal.pone.0058573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan, M. T. , Soares Magalhaes, R. J. , Williams, G. M. , & Mamun, A. A. (2015). The role of maternal education in the 15‐year trajectory of malnutrition in children under 5 years of age in Bangladesh. Maternal & Child Nutrition. doi: 10.1111/mcn.12178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Headey, D. , Hoddinott, J. , Ali, D. , Tesfaye, R. , & Dereje, M. (2015). The other Asian enigma: Explaining the rapid reduction of undernutrition in Bangladesh. World Development, 66, 749–761. doi: 10.1016/j.worlddev.2014.09.022 [DOI] [Google Scholar]
- Headey, D. , Hoddinott, J. , & Park, S. (2016). Drivers of nutritional change in four South Asian countries: A dynamic observational analysis. Maternal & Child Nutrition, 12(Suppl 1), 210–218. doi: 10.1111/mcn.12274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe, L. D. , Hargreaves, J. R. , & Huttly, S. R. (2008). Issues in the construction of wealth indices for the measurement of socio‐economic position in low‐income countries. Emerging Themes in Epidemiology, 5, 3. doi: 10.1186/1742-7622-5-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda, N. , Irie, Y. , & Shibuya, K. (2013). Determinants of reduced child stunting in Cambodia: Analysis of pooled data from three demographic and health surveys. Bulletin of the World Health Organization, 91(5), 341–349. doi: 10.2471/BLT.12.113381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jesmin, A. , Yamamoto, S. S. , Malik, A. A. , & Haque, M. A. (2011). Prevalence and determinants of chronic malnutrition among preschool children: A cross‐sectional study in Dhaka City, Bangladesh. Journal of Health, Population, and Nutrition, 29(5), 494–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keino, S. , Plasqui, G. , Ettyang, G. , & van den Borne, B. (2014). Determinants of stunting and overweight among young children and adolescents in sub‐Saharan Africa. Food and Nutrition Bulletin, 35(2), 167–178. [DOI] [PubMed] [Google Scholar]
- Khan, M. M. , Kramer, A. , Khandoker, A. , Prufer‐Kramer, L. , & Islam, A. (2011). Trends in sociodemographic and health‐related indicators in Bangladesh, 1993‐2007: Will inequities persist? Bulletin of the World Health Organization, 89(8), 583–593. doi: 10.2471/BLT.11.087429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar, A. , Kumari, D. , & Singh, A. (2015). Increasing socioeconomic inequality in childhood undernutrition in urban India: Trends between 1992‐93, 1998‐99 and 2005‐06. Health Policy and Planning, 30(8), 1003–1016. doi: 10.1093/heapol/czu104 [DOI] [PubMed] [Google Scholar]
- Martorell, R. , & Zongrone, A. (2012). Intergenerational influences on child growth and undernutrition. Paediatric and Perinatal Epidemiology, 26(Suppl 1), 302–314. doi: 10.1111/j.1365-3016.2012.01298.x [DOI] [PubMed] [Google Scholar]
- Menezes, R. C. , Lira, P. I. , Leal, V. S. , Oliveira, J. S. , Santana, S. C. , Sequeira, L. A. , … Batista Filho, M. (2011). Determinants of stunting in children under five in Pernambuco, northeastern Brazil. Revista de Saúde Pública, 45(6), 1079–1087. [DOI] [PubMed] [Google Scholar]
- Mostafa, K. S. (2011). Socio‐economic determinants of severe and moderate stunting among under‐five children of rural Bangladesh. Malaysian Journal of Nutrition, 17(1), 105–118. [PubMed] [Google Scholar]
- NIPORT, M. A. , & ICF International . (2016). Bangladesh Demographic and Health Survey 2014. Retrieved from Dhaka, Bangladesh and Maryland, USA.
- Novignon, J. , Aboagye, E. , Agyemang, O. S. , & Aryeetey, G. (2015). Socioeconomic‐related inequalities in child malnutrition: Evidence from the Ghana multiple indicator cluster survey. Health Economics Review, 5(1), 34. doi: 10.1186/s13561-015-0072-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Donnell, O. , Van Doorslaer, E. , Wagstaff, A. , & Lindelow, M. (2008). Analyzing health equity using household survey data: A guide to techniques and their implementation. World Bank Institute: Washington D. C. [Google Scholar]
- Olofin, I. , McDonald, C. M. , Ezzati, M. , Flaxman, S. , Black, R. E. , Fawzi, W. W. , … Nutrition Impact Model Study . (2013). Associations of suboptimal growth with all‐cause and cause‐specific mortality in children under five years: A pooled analysis of ten prospective studies. PloS One, 8(5), e64636. doi: 10.1371/journal.pone.0064636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozaltin, E. , Hill, K. , & Subramanian, S. V. (2010). Association of maternal stature with offspring mortality, underweight, and stunting in low‐ to middle‐income countries. JAMA, 303(15), 1507–1516. doi: 10.1001/jama.2010.450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prendergast, A. J. , & Humphrey, J. H. (2014). The stunting syndrome in developing countries. Paediatrics and International Child Health, 34(4), 250–265. doi: 10.1179/2046905514Y.0000000158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachmi, C. N. , Agho, K. E. , Li, M. , & Baur, L. A. (2016). Stunting, underweight and overweight in children aged 2.0–4.9 years in Indonesia: Prevalence trends and associated risk factors. PloS One, 11(5), e0154756. doi: 10.1371/journal.pone.0154756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman, A. , & Chowdhury, S. (2007). Determinants of chronic malnutrition among preschool children in Bangladesh. Journal of Biosocial Science, 39(2), 161–173. doi: 10.1017/S0021932006001295 [DOI] [PubMed] [Google Scholar]
- Ramakrishnan, U. , Martorell, R. , Schroeder, D. G. , & Flores, R. (1999). Role of intergenerational effects on linear growth. The Journal of Nutrition, 129(2S Suppl), 544S–549S. [DOI] [PubMed] [Google Scholar]
- Rannan‐Eliya, R. P. , Hossain, S. M. , Anuranga, C. , Wickramasinghe, R. , Jayatissa, R. , & Abeykoon, A. T. (2013). Trends and determinants of childhood stunting and underweight in Sri Lanka. The Ceylon Medical Journal, 58(1), 10–18. doi: 10.4038/cmj.v58i1.5357 [DOI] [PubMed] [Google Scholar]
- Restrepo‐Mendez, M. C. , Barros, A. J. , Black, R. E. , & Victora, C. G. (2015). Time trends in socio‐economic inequalities in stunting prevalence: Analyses of repeated national surveys. Public Health Nutrition, 18(12), 2097–2104. doi: 10.1017/S1368980014002924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha, K. K. , Billah, M. , Menon, P. , El Arifeen, S. , & Mbuya, N. V. N. (2015). Bangladesh National Nutrition Services: Assessment of implementation status. (111 pp.) World Bank Group: Washington, DC. ISBN 978‐1‐4648‐0640‐7, 978‐1‐4648‐0641‐4 [doi: 10.1596/978-1-4648-0640-7]. [DOI] [Google Scholar]
- Said‐Mohamed, R. , Allirot, X. , Sobgui, M. , & Pasquet, P. (2009). Determinants of overweight associated with stunting in preschool children of Yaounde, Cameroon. Annals of Human Biology, 36(2), 146–161. doi: 10.1080/03014460802660526 [DOI] [PubMed] [Google Scholar]
- Semali, I. A. , Tengia‐Kessy, A. , Mmbaga, E. J. , & Leyna, G. (2015). Prevalence and determinants of stunting in under‐five children in central Tanzania: Remaining threats to achieving Millennium Development Goal 4. BMC Public Health, 15, 1153. doi: 10.1186/s12889-015-2507-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tette, E. M. , Sifah, E. K. , Nartey, E. T. , Nuro‐Ameyaw, P. , Tete‐Donkor, P. , & Biritwum, R. B. (2016). Maternal profiles and social determinants of malnutrition and the MDGs: What have we learnt? BMC Public Health, 16(1), 214. doi: 10.1186/s12889-016-2853-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari, R. , Ausman, L. M. , & Agho, K. E. (2014). Determinants of stunting and severe stunting among under‐fives: Evidence from the 2011 Nepal Demographic and Health Survey. BMC Pediatrics, 14, 239. doi: 10.1186/1471-2431-14-239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . (2009). Tracking progress on child and maternal nutrition: A survival and development priority. UNICEF: New York, NY. ISBN: 978‐92‐806‐4482‐1. [Google Scholar]
- Vella, V. , Tomkins, A. , Borghesi, A. , Migliori, G. B. , & Oryem, V. Y. (1994). Determinants of stunting and recovery from stunting in northwest Uganda. International Journal of Epidemiology, 23(4), 782–786. [DOI] [PubMed] [Google Scholar]
- Victora, C. G. , Adair, L. , Fall, C. , Hallal, P. C. , Martorell, R. , Richter, L. , … Child Undernutrition Study Group . (2008). Maternal and child undernutrition: Consequences for adult health and human capital. Lancet, 371(9609), 340–357. doi: 10.1016/S0140-6736(07)61692-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagstaff, A. , van Doorslaer, E. , & Watanabe, N. (2003). On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. Journal of Econometrics, 112(1), 207–223. doi: 10.1016/S0304-4076(02)00161-6 [DOI] [Google Scholar]
- Wolde, M. , Berhan, Y. , & Chala, A. (2015). Determinants of underweight, stunting and wasting among schoolchildren. BMC Public Health, 15, 8. doi: 10.1186/s12889-014-1337-2 [DOI] [PMC free article] [PubMed] [Google Scholar]


