Abstract
Global efforts to further improve exclusive breastfeeding rates have not been successful, in part because effective scaling‐up frameworks and roadmaps have not been developed. The Becoming Breastfeeding Friendly (BBF) toolbox includes an evidence‐based index, the BBF Index (BBFI), to guide the development and tracking of large scale, well‐coordinated, multisector national breastfeeding promotion programmes. This paper describes the development of the BBFI, which is grounded in the Breastfeeding Gear Model complex adaptive systems framework. The BBFI was developed by the BBF Steering Committee in collaboration with a high‐level Technical Advisory Group following the Delphi consensus methodology. Key benchmarks and definitions were informed by evidence‐based health, nutrition, and newborn survival initiatives identified from the academic and grey literature. The BBFI consists of 8 gears (54 benchmarks): Advocacy (4); Political Will (3); Legislation and Policies (10); Funding and Resources (4); Training and Program Delivery (17); Promotion (3); Research and Evaluation (10); and Coordination, Goals, and Monitoring (3). Scores are generated for 8 gear scores plus a total country score to gauge the scaling‐up enabling environment. The BBFI provides an evidence‐based index to assist countries in (a) assessing their readiness to scale up breastfeeding programmes and (b) tracking scaling‐up progress.
Keywords: breastfeeding, complex adaptive systems, health planning, measurement, nutrition, scaling up
Key messages.
Few tools have been developed for assessing BF promotion, protection, and support, and none are comprehensive nor designed to provide specific guidance to assist countries and policies makers in deciding the next course of action when gaps are found.
The BBF toolbox through the BBFI assesses the national readiness of countries to scale up BF programmes.
The BBFI is an evidence‐based index grounded in the BFGM that tracks large scale, multisector national BF promotion programmes worldwide and assists policymakers to make the data‐driven decisions needed to successfully improve BF outcomes.
1. INTRODUCTION
Breastfeeding (BF) has been identified as a highly feasible and cost‐effective intervention to improve child health and development (Jones, Steketee, Black, Bhutta, & Morris, 2003). The recent Lancet Breastfeeding Series provides strong evidence that BF brings substantial benefits beyond infant survival, on the short as well as long‐term health and development outcomes (Rollins et al., 2016; Victora et al., 2016). BF also benefits women's health (Chowdhury et al., 2015; Victora et al., 2016). All these benefit human capital (Victora et al., 2015) and national development in low‐, middle‐, and high‐income countries (Rollins et al., 2016; Victora et al., 2016). Such evidence supports the recognition of BF as a human right for women and children (Kent, 2006; UN, 2016). Therefore, governments should ensure that all mothers are supported and empowered to follow optimal infant feeding practices, which includes exclusive BF (EBF) for about 6 months and continuing BF, once complementary foods are introduced, for at least 2 years (Kent, 2006; Perez‐Escamilla & Sellen, 2015). Providing affordable and high‐quality programmes that support all women who wish to breastfeed is an excellent investment for society at large and a key step towards achieving the Sustainable Development Goals by 2030 (Rollins et al., 2016).
Efficacious BF interventions delivered across key sectors systems surrounding infants and mothers have been identified, including peer‐counselling (Chapman, More, Anderson, Kojo, & Perez‐Escamilla, 2010), the International Code of Marketing of Breastmilk Substitutes (Rollins et al., 2016), and the Baby‐Friendly Hospital Initiative (Perez‐Escamilla, Martinez, & Segura‐Perez, 2016). Unfortunately, the “real world” effectiveness for many BF interventions has not been fully demonstrated. This is in part because effective scaling‐up frameworks and roadmaps have not been developed. Without them, it is unlikely that successful scaling‐up of optimal BF will be achieved as this effort requires extensive understanding of strategies for implementation, adoption, and sustainability in complex contexts (Reis et al., 2016).
Despite all efforts to improve EBF duration, its prevalence remains low globally. In the last two decades, global EBF rates among infants under 6 months grew slowly from 24.9% in 1993 to 35.7% in 2013 (Victora et al., 2016). In an effort to improve child and maternal health outcomes, EBF was universally endorsed as one of the first‐ever global nutrition targets by the 2012 World Health Assembly (WHA). The WHA target calls to increase the EBF rate in low‐ and middle‐income countries from 37% in 2012 to at least 50% by 2025 (WHO, 2014 2014).
In the current environment with limited resources to achieve the target, it is vital to develop effective evidence‐based tools to assist countries with their efforts to scale up their BF programmes (Shekar, Kakietek, Eberwein, & Walters, 2016). These frameworks need to consider the causal chains of policies and programmes to promote, protect, and support BF, recognizing that they operate in a complex adaptive multilevel systems “universe”(Lutter & Morrow, 2013; Perez‐Escamilla, Curry, Minhas, Taylor, & Bradley, 2012; Rollins et al., 2016; Sinha et al., 2015). Until recently, we still lacked evidence‐based frameworks and models to assist countries to effectively scale up and sustain their BF programmes (Perez‐Escamilla et al., 2012). The objective of this article is to fill this void by detailing the development of an evidence‐based index to assess readiness for and monitoring of the scaling‐up of BF programmes.
1.1. Becoming BF Friendly (BBF) toolbox
The BBF toolbox is designed to help policymakers make data‐driven decisions to successfully improve their countries' BF outcomes. The toolbox was designed to guide and empower countries to measure their readiness for scaling‐up their BF programmes and develop a scaling‐up plan accordingly through a three‐step process. First, the BBF Index (BBFI) assesses the national readiness of countries to scale up BF. Second, case studies provide decision‐makers with clear evidence‐based examples to guide the translation of policy recommendation into action. Third, a five‐meeting process is conducted where countries use the BBFI and case studies to develop and disseminate policy recommendations and call to action key multisector stakeholders to collectively advocate for scaling‐up of BF protection, promotion, and support.
The BBFI is based on the BF Gear Model (BFGM) that in turn is grounded in the Assess, Innovate, Develop, Engage, and Devolve (AIDED) complex adaptive systems framework (Perez‐Escamilla et al., 2012). The BFGM stipulates that eight gears—Advocacy; Political Will; Legislation and Policies; Funding and Resources; Training and Program Delivery; Promotion; Research and Evaluation; and Coordination, Goals, and Monitoring—must work in harmony for large‐scale improvement in a country's national BF “engine.” The BFGM is based on the premise that evidence‐based advocacy generates political will to enact policies and legislation that are needed to protect, promote, and support optimal BF practices. These, in turn, generate the necessary resources to implement workforce training and programme delivery, as well as social marketing campaigns. Research and evaluations are conducted to maintain the quality and success of the programmes, and a coordinating master gear keeps the multisectorial programme(s) on track by setting and monitoring goals, facilitating the flow of information across gears, and providing timely feedback on actions needed to improve or sustain the quality of scaled‐up programmes (Perez‐Escamilla et al., 2012).
This paper aims to describe the development of the BBFI. The remaining components of the BBF toolbox (i.e., the case studies and evidence‐based BBF process) will be reported elsewhere.
2. METHODS
2.1. Development of BBFI
The BBFI was developed between August 2015 and January 2016 by the BBF Yale University Steering Committee (BBF‐YSC) formed by BF, maternal/child nutrition, and public health experts in collaboration with a 14‐member Technical Advisory Group (TAG) with collective expertise in policy, evaluation, and behaviour change as well as metric development relevant to scaling‐up of health and nutrition programmes in low‐, middle‐, and high‐income countries. TAG members were academics (Bangladesh, Canada, Ghana, Mexico, UK, and USA), international agency officials (WHO, UNICEF, and PAHO), and senior staff representing international philanthropic and non‐profit organizations (Bill and Melinda Gates Foundation, Alive & Thrive, The Manoff Group, GAIN, and TAHN).
The initial step in developing the BBFI was to identify potential themes and benchmarks to measure each of the eight gears corresponding to the BFGM. A review was conducted through PubMed to identify key metric projects that assessed country‐level readiness for scaling‐up health and nutrition initiatives within the areas of maternal, infant and young child nutrition, and newborn survival. Grey literature searches were also conducted using publication/resource databases and examining websites of international organizations, including the WHO, UNICEF, International Baby Food Action Network (IBFAN), United Nations Standing Committee on Nutrition, the Food and Agricultural Organization, and the World Alliance for Breastfeeding Action (WABA). Additional articles and initiatives were identified in consultation with BF and metric experts as well as through backward searches from article reference lists. Key publications and initiatives were included if they described a tool used for scaling‐up health and nutrition initiatives within the three identified areas. We excluded publications and initiatives that did not provide sufficient information on the tool used (see Figure 1).
Figure 1.
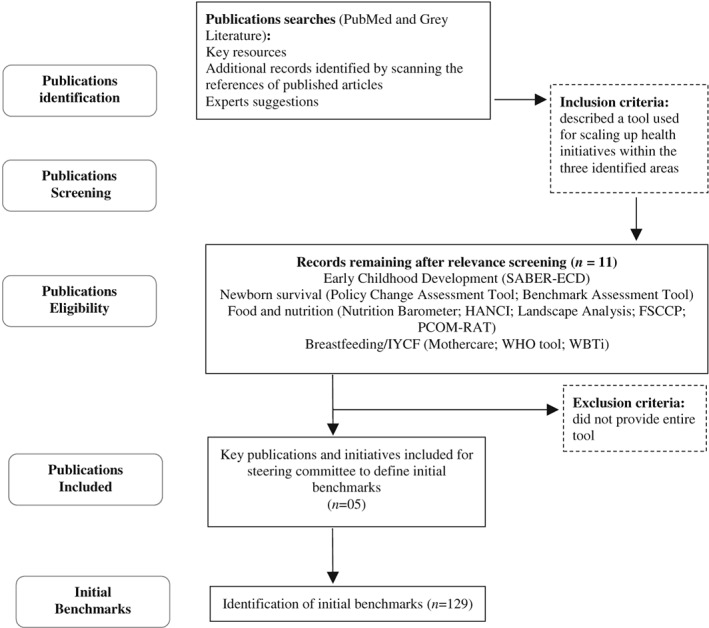
Flow diagram to identify key metrics projects that assessed country‐level readiness of health initiatives within the areas of infant and young child feeding, food and nutrition, and newborn survival
The BBF‐YSC took the lead reviewing key publications and initiatives. A series of consensus meetings were held to (a) identify the publications and initiatives that met the relevant inclusion/exclusion criteria (Darmstadt et al., 2014; Fox, Balarajan, Cheng, & Reich, 2015; IBFAN, 2014; Moran et al., 2012; WABA, 1993; WHO, 2003), (b) propose an operational definition of each of the eight gears, (c) identify themes that reflect key gear components, and (d) identify benchmarks to measure those themes. The BBF‐YSC consensus meetings resulted in the first draft of the BBFI, which included operational definitions of 129 potential benchmarks across the eight gears (see Figure 2).
Figure 2.
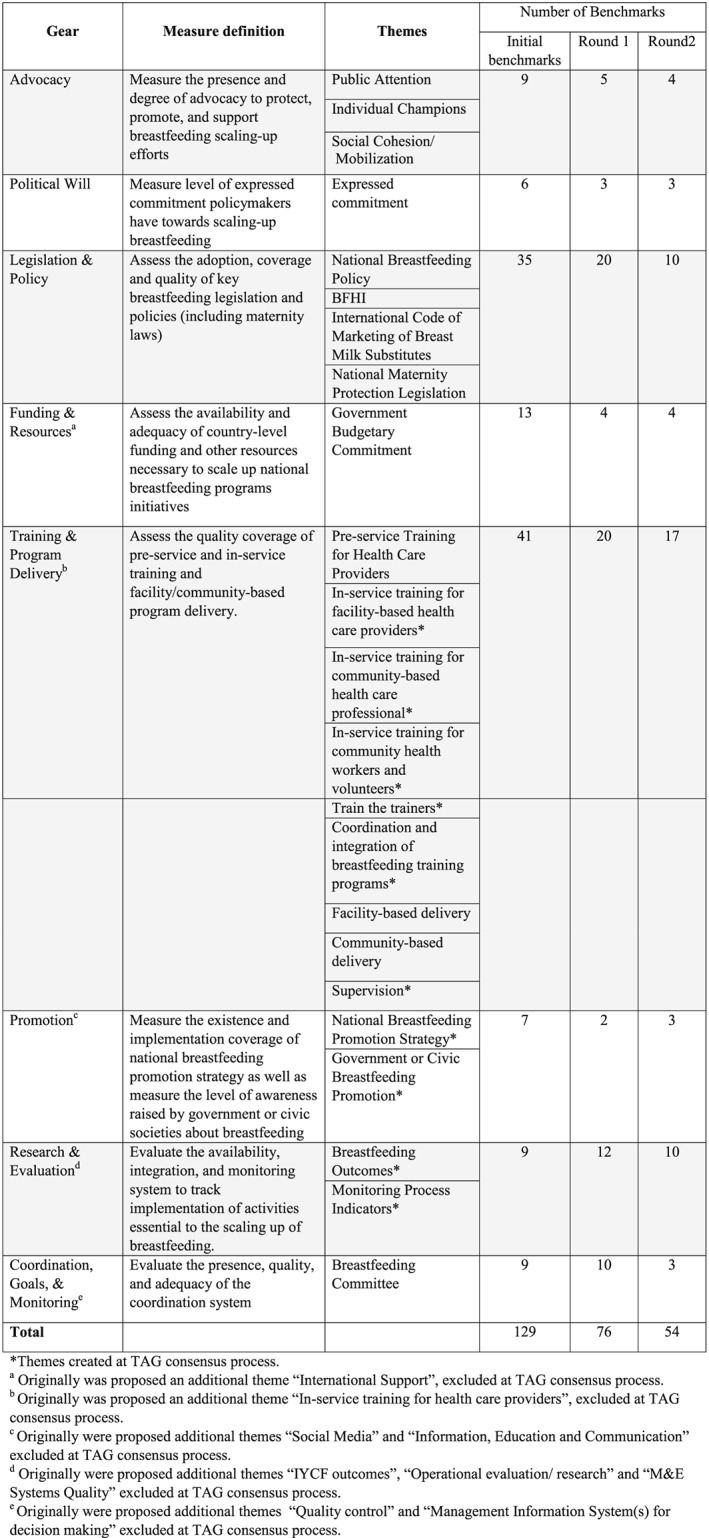
Components of Becoming Breastfeeding Friendly Index (BBFI) toolbox and number of benchmarks per gear for each round of revisions
The first draft of the BBFI was shared with TAG members, and the Delphi consensus methodology (Chia‐Chien Hsu, 2007; Okoli & Pawlowski, 2004) was followed to elicit consensus from them on the suitability of the benchmarks for assessing a country's BF scaling‐up environment.
The Delphi Method of decision‐making is a widely used effective strategy that facilitates efficient group communication to reach consensus on a specific issue using a series of questionnaires delivered via multiple iterations to collect data from a panel of selected experts (Chia‐Chien Hsu, 2007; Okoli & Pawlowski, 2004). This process must be followed after the experts (i.e., TAG members) are carefully selected and provided with detailed “rules” and principles for making decisions during the process to ensure a valid outcome (Okoli & Pawlowski, 2004). The Delphi method begins with identifying a question or issue statement, followed by circulating a questionnaire to the expert panel. After the collection of the initial questionnaire, the data are analysed, summarized, and presented to the panel. Subsequently revising the questionnaire to reflect the previous round's responses, it is distributed again to the expert panel for further feedback. This highly iterative process has been shown to be effective for reaching consensus among stakeholders within a reasonable time. Multiple rounds of questionnaires and revisions are central for the consensus development process (Chia‐Chien Hsu, 2007), allowing participants to reassess their initial judgments if necessary (Okoli & Pawlowski, 2004).
3. RESULTS
Two rounds of questionnaires and revisions were circulated before TAG members reached consensus on the final version of the BBFI (see Figure 3). For the first round, eight surveys (corresponding to each of the eight gears and their benchmarks) were constructed and distributed among TAG members via SurveyMonkey® to rank each benchmark for “importance” and “feasibility.” Importance was assessed with the following question: Is this benchmark a critical step along the pathway to implement the scale‐up of national BF programmes? TAG members ranked importance on a 5‐point scale of 0 (no importance) to 4 (very important). Feasibility was assessed with the question: How feasible is it to accurately measure this benchmark in a standardized way across countries? Feasibility was measured on a 5‐point scale from 0 (unfeasible) to 4 (very feasible). TAG members were also able to provide written feedback on the content of the benchmarks and propose new benchmarks. Responses were received within 2 weeks. Average scores for importance and feasibility were calculated for each of the 129 individual benchmarks. Average scores for importance and feasibility were also calculated for each of the eight gears and served as cut‐off points for classifying the benchmarks into one of four groups based on their individual average score: (1) high importance/high feasibility, (2) high importance/low feasibility, (3) low importance/high feasibility, (4) low importance/low feasibility. This classification was used to generate a preliminary ranking for the initial benchmarks (see Figure 4).
Figure 3.
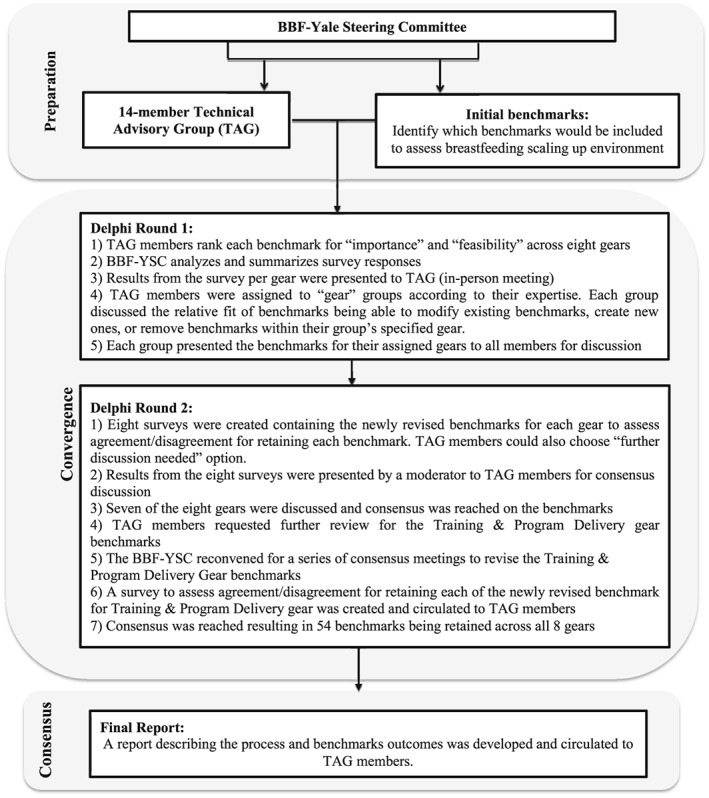
Technical Advisory Group (TAG) members consensus process to develop the final version of the Becoming Breastfeeding Friendly Index (BBFI)
Figure 4.
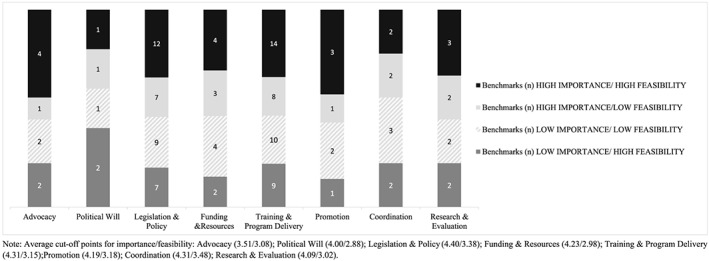
Importance and feasibility ranking for initial benchmarks. Average cut‐off points for importance/feasibility: Advocacy (3.51/3.08); Political Will (4.00/2.88); Legislation and Policy (4.40/3.38); Funding and Resources (4.23/2.98); Training and Program Delivery (4.31/3.15); Promotion (4.19/3.18); Coordination (4.31/3.48); Research and Evaluation (4.09/3.02)
Following the first survey round, 14 TAG members convened at a 3‐day intensive, highly participatory meeting from October 27 to 29, 2015, at Yale University to reach consensus on the final BBFI benchmarks. On the second meeting day, the survey results were presented, by gear, to show TAG members the preliminary rankings of each benchmark. TAG members were assigned to “gear” groups according to their expertise. Within these gear groups, members discussed the relative utility of benchmarks to assess their assigned gear. They were asked to approve or modify existing benchmarks, create new ones, or remove benchmarks within their group's specified gear(s). Subsequently, each gear group presented their set of revised benchmarks to the whole group for discussion as well as consensus, and this process resulted in 76 benchmarks (vs. 129 in the initial round; see Figure 2, Round 1).
At the end of the second meeting day, eight surveys containing the 76 newly revised benchmarks, grouped by gear, were distributed via SurveyMonkey® to TAG members to assess their level of agreement/disagreement for retaining each benchmark. There was also a “further discussion needed” option. TAG members responded to the survey on the same day, and at the beginning of the third consultation day, the results were presented by a trained neutral moderator external to the BBF‐YSC to ensure impartiality in the consensus process. Seven of the eight gears were discussed, and consensus about benchmarks and wordings was reached. For the last gear, Training and Program Delivery, TAG members requested the BBF‐YSC further review BF training curriculum guides and propose benchmark changes. In response, the BBF‐YSC revised the Training and Program Delivery gear benchmarks based on the “UNICEF/WHO breastfeeding training curriculum guides for healthcare professionals and community health workers” (WHO & UNICEF, 2012) as well as additional literature (WHO & UNICEF, 2006, 2009). The newly revised benchmarks were circulated via SurveyMonkey® to TAG members 2 months following the TAG meeting, to assess the level of agreement/disagreement for retaining each benchmark and to receive additional feedback. The BBF‐YSC revised the Training and Program Delivery gear benchmarks based on these survey results and feedback, thus ending the second consensus round. The final version of the BBFI consists of eight gears, 23 gear‐related themes, and 54 associated benchmarks (see Figure 2, Round 2). A report describing the process and benchmarks outcomes was developed and circulated to TAG members for their final approval.
Web Appendix S1 describes in full detail the process followed to revise and reach consensus on each one of the final BBFI benchmarks including all benchmarks proposed, deleted, created, or reworded during the consensus process; the rankings and mean scores for importance/feasibility (Round 1); and the percentage of agreement between TAG members to retain benchmarks within each gear (Round 2).
3.1. Development of BBFI score
A scoring algorithm was created to provide a Gear Total Score (GTS) and the BBFI Total Score (BBFI‐TS). The GTS is the country score for each of the eight gears and describes the strength of each gear, whereas the BBFI‐TS represents the overall readiness of a country's environment to scale up BF. The scoring algorithm for the BBFI‐ TS was designed in three steps: (a) scoring the benchmarks; (b) calculating scores for each of the eight gears (GTS); and (c) calculating the BBFI‐TS (see Figure 5).
Figure 5.
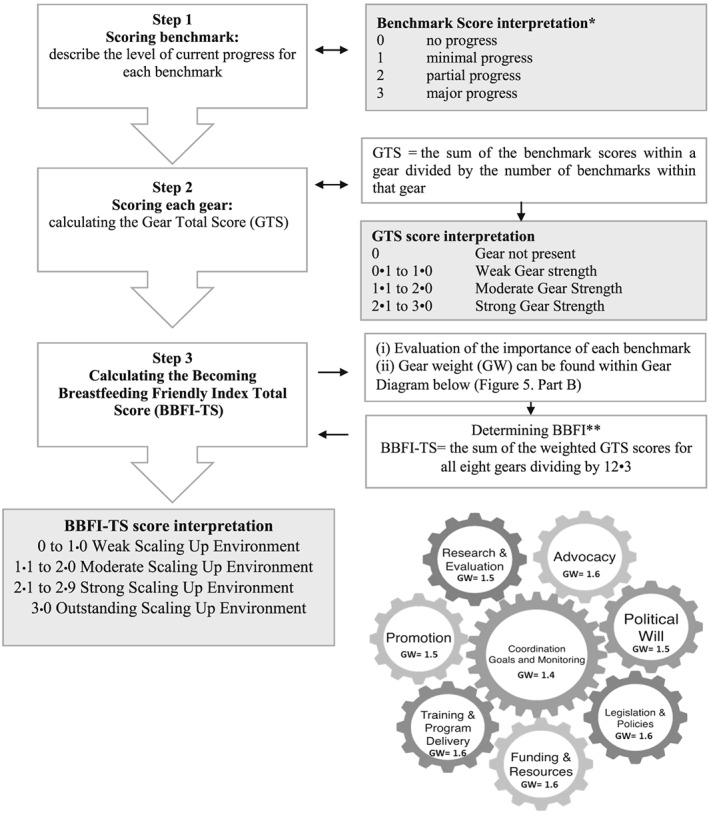
Becoming Breastfeeding Friendly Index (BBFI) scoring steps and score interpretation. BBFI Total Score (BBFI‐TS) formula = [(weighted GTS Advocacy) + (weighted GTS Political Will) + (weighted GTS Legislation and Policies) + (weighted GTS Funding and Resources) + (weighted GTS Training and Program Delivery) + (weighted GTS Promotion) + (weighted GTS Research and Evaluation) + (weighted GTS Coordination, Goals, and Monitoring)]/12.3
3.2. Developing benchmark scores
Each benchmark was scored based on a 4‐point scale similar to those used to assess the scaling‐up of neonatal survival initiatives (Darmstadt et al., 2014). For each benchmark, scoring includes the following: 0 (no progress), 1 (minimal progress), 2 (partial progress), and 3 (major progress) as well as a description of the progress required to achieve for each score (see Figure 5, Step 1).
3.3. Development of GTS
Scoring for each gear was determined by the sum of the benchmark scores within a gear divided by the number of benchmarks within that gear. Because each gear is measured by a different number of benchmarks, GTS allows for standard comparison across gears. GTS indicates the progress of each gear as follows: not present, weak strength, moderate strength, or strong strength (see Figure 5, Step2).
3.4. Development of BBFI‐TS
Each gear has a different level of importance (i.e., weight) in the BF scale‐up process (Perez‐Escamilla et al., 2012). The weight of each gear was determined in three steps: (a) evaluating the importance of each benchmark; (b) calculating the gear weight (GW); and (c) calculating the weighted GTS.
To evaluate the importance of each benchmark, a survey containing a list of the 54 final benchmarks, listed without the designation of the gear, was distributed to TAG members who ranked the importance (1 = low, 2 = medium, or 3 = high) of each benchmark for BF scaling‐up. Rankings were then averaged for each benchmark to determine the overall importance of each benchmark. Next, the GW was calculated by grouping benchmarks into their gears and averaging them. Web Appendix S1 describes results of the final benchmark weights and GWs.
For a country to determine their BBFI‐TS, the weighted GTS is calculated first. The weighted GTS for each gear can be determined by multiplying the GWs by each GTS. Subsequently, the BBFI‐TS is calculated by summing the weighted GTS for all eight gears and dividing by the sum of all the GW, which is 12•3. The BBFI‐TS results yield the strength (weak, moderate, strong, or outstanding) of a country's environment to scale up BF (see Figure 5, Step 3).
4. DISCUSSION
The BBFI provides an evidence‐based tool that countries can use to assess their BF scaling‐up environment and meet the WHA goal to increase the rate of EBF in the first 6 months up to at least 50% (WHO, 2014 2014). Although other tools exist to assess BF programmes and initiatives at the country‐level (IBFAN, 2014; WABA, 1993; WHO, 2003), none of these are comprehensive, designed to measure the BF scaling‐up environment, nor provide specific guidance on how to use the data to help countries decide on a course of action(s). Unlike the previous tools, the BBFI is based on a model grounded in a complex adaptive systems framework. The BFGM stipulates that when the specified eight gears fully exist and work harmoniously, the likelihood of success with BF scale‐up is maximized (Perez‐Escamilla et al., 2012). The BBFI measures each of these eight gears using a standardized methodology, which generates both gear scores and a total overall score. This enables countries to determine, which gear(s) needs improvement as well as how they need to be improved, thus distinguishing this index from other available tools.
The BBFI was developed using a strong consensus process driven by experts spanning the fields of BF, political commitment, evaluation metrics, health facility and community programme delivery, and behaviour change communications. The selection of technical advisory experts was purposeful, to allow for expert representation of each gear. The Delphi consensus methodology was key to defining the systematic and scientific process of selecting indicators to include in the BBFI (Chia‐Chien Hsu, 2007; Innes & Booher, 1999; Okoli & Pawlowski, 2004). This process relies on repeated rounds of assessment by the experts to allow them to converge and reach consensus on the final indicators. Evidence has shown the positive impact of using consensus methods to aid in the design and development of objective assessments of valid scaling‐up readiness and progress tools (Bradley et al., 2012; Innes & Booher, 1999; McDaniel, Lanham, & Anderson, 2009). Consensus methods have been used successfully within the nutrition and newborn survival fields to identify benchmarks comprising various assessment tools (Fox et al., 2015; Moran et al., 2012). To our knowledge, this is the first time this methodology has been used to determine the most influential indicators needed for successful BF scale‐up. Thus, in addition to being grounded within a solid theoretical framework, the BBFI is anchored in a strong scientific development process that relied upon transparent participation from experts in the field following a sound consensus methodology.
During the BBFI development process, results showed that the importance of the eight gears was weighed differently by experts, although the range was narrow, suggesting some gears may be slightly important than others in the scaling‐up process. Within the BFGM, a central or master gear is needed to both (a) coordinate the communications and feedback across gears as well as systems levels (i.e., national‐regional‐municipal levels) and (b) to ensure that the engine moves in sync and at the right speed (Perez‐Escamilla et al., 2012). Thus, it would be expected that the Coordination, Goals, and Monitoring Gear would have the highest weighted score, indicating that it is most important in the process. Rather, this gear received the lowest weighted score from the experts compared to the other seven gears. This may indicate that the Coordination, Goals, and Monitoring Gear must always be present (i.e., driving the process) but needs the rest of the gears to be in place for it to be useful. Because the BFGM is analogous to an engine that needs all the gears to work properly, these results can be the first step towards understanding the full pathway as well as the role of the key components for successful BF scale‐up. To generate evidence on different pathways and determinants for successful BF scale‐up, we are currently developing a Program Impact Pathways Analysis, that is, a blueprint to guide future implementation of BBF based on the BBF experience in Ghana and Mexico.
The BBFI addresses previous challenges in measurement and interpretation experienced within other fields (Fox et al., 2015; Moran et al., 2012) by integrating efforts to track the reach and strength of implementation while incorporating some flexibility for countries to decide how to achieve readiness in scale‐up process. This is accomplished through the use of the BFGM framework as the BBFI foundation, which recognizes that the structure of each gear is likely to be similar across countries, but fully acknowledges that the nuts and bolts needed to make each gear function are context‐specific (i.e., path dependence; Perez‐Escamilla et al., 2012). The BBFI enables countries to assess gear strength (i.e., weak, moderate, strong, and outstanding) and target specific investments according to the priority of each country. Given that the strength of each gear can vary across countries, individual countries are able to identify and drive their own paths to scale up and sustain the BF‐friendly environment. This adaptability means that countries can assess and recommend the most critical benchmarks for promotion and sustainable implementation at scale taking into account their own particular contexts (Moran et al., 2012).
Through the BBFI, we are proposing an innovative approach to measuring countries' readiness for BF scaling‐up. This has important implications for influencing global health scaling‐up pathways. The BBFI provides a quantitative index for a baseline assessment, which can be reapplied over time to track changes (improvements/declines) in readiness to scale up. In addition to generating timely information on a country's degree of political commitment to BF, the BBFI can be used in a similar way to tools in other fields (Fox et al., 2015): to raise awareness about the political environment and facilitate the development of political strategies to advance the agenda‐setting process. Therefore, in a global environment with constrained resources (Shekar et al., 2016) and small annual changes in BF outcomes worldwide (Lutter & Morrow, 2013; Victora et al., 2016), the BBFI can be a powerful instrument in different socio‐economic and cultural contexts both in determining how best to sustain BF impacts over a relatively short period of time (i.e.,<3 years) as well as to fill the knowledge gaps for maintaining optimal performance in the long term. This is especially true if the metrics process is accompanied by an evidence‐based decision‐making process on how to translate assessments into concrete actions, as the BBF toolbox provides.
The BBFI and rest of the BBF toolbox components have now been successfully pretested in Mexico and Ghana. Lessons learned will be reported elsewhere. An additional strength of BBFI is that it can be adapted to calculate subnational level scores in countries where the states are relatively autonomous.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
RPE and AHF conceptualized the study and modelling framework. RPE, AHF, KD, MBG, and SM developed the initial set of benchmarks. MBG and GSB developed the scoring algorithm. All authors contributed to the study design, analysis, and writing of the report. GSB developed the manuscript figures.
Supporting information
Appendix S1.
Supporting information
ACKNOWLEDGMENTS
The authors acknowledge the following BBF Technical Advisory Group members for their participation throughout the metric development process: Chessa Lutter, France Begin, Teresita Gonzalez de Cosio, Rukhsana Haider, Sonia Semenic, Marcia Griffiths, Nemat Hajeebhoy, Leslie Curry, Alison Tumilowicz, Ashley Fox, Richmond Aryeetey, Laurence Grummer‐Strawn, and Fiona Clare Dykes.
Pérez‐Escamilla R, Hromi‐Fiedler AJ, Gubert MB, Doucet K, Meyers S, dos Santos Buccini G. Becoming Breastfeeding Friendly Index: Development and application for scaling‐up breastfeeding programmes globally. Matern Child Nutr. 2018;14:e12596 10.1111/mcn.12596
REFERENCES
- Bradley, E. H. , Curry, L. A. , Taylor, L. A. , Pallas, S. W. , Talbert‐Slagle, K. , Yuan, C. , … Perez‐Escamilla, R. (2012). A model for scale up of family health innovations in low‐income and middle‐income settings: A mixed methods study. BMJ Open, 2(4). 10.1136/bmjopen-2012-000987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman, D. , More, K. , Anderson, A. , Kojo, A. , & Perez‐Escamilla, R. (2010). Breastfeeding peer counseling: From efficacy through scale‐up. Journal of Human Lactation, 26(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chia‐Chien Hsu, B. A. S. (2007). The Delphi technique: Making sense of consensus. Practical Assessment, Research & Evaluation, 12(10). [Google Scholar]
- Chowdhury, R. , Sinha, B. , Sankar, M. , Taneja, S. , Bhandari, N. , Rollins, N. , … Martines, J. (2015). Breastfeeding and maternal health outcomes: A systematic review and meta‐analysis. Acta Paediatrica, 104(467), 96–113. 10.1111/apa.13102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darmstadt, G. L. , Kinney, M. V. , Chopra, M. , Cousens, S. , Kak, L. , Paul, V. K. , … Lawn, J. E. (2014). Who has been caring for the baby? The Lancet, 384(9938), 174–188. 10.1016/s0140-6736(14)60458-x [DOI] [PubMed] [Google Scholar]
- Fox, A. M. , Balarajan, Y. , Cheng, C. , & Reich, M. R. (2015). Measuring political commitment and opportunities to advance food and nutrition security: Piloting a rapid assessment tool. Health Policy and Planning, 30(5), 566–578. 10.1093/heapol/czu035 [DOI] [PubMed] [Google Scholar]
- IBFAN (2014). World Breastfeeding Trends Initiative (WBTi) assessment tool: IBFAN (Asia).
- Innes, J. E. , & Booher, D. E. (1999). Consensus building and complex adaptive systems: A framework for evaluating collaborative planning. Journal of the American Planning Association, 65(4), 412–423. [Google Scholar]
- Jones, G. , Steketee, R. W. , Black, R. E. , Bhutta, Z. A. , & Morris, S. S. (2003). How many child deaths can we prevent this year? The Lancet, 362(9377), 65–71. 10.1016/s0140-6736(03)13811-1 [DOI] [PubMed] [Google Scholar]
- Kent, G. (2006). Child feeding and human rights. International Breastfeeding Journal, 1, 27 10.1186/1746-4358-1-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutter, C. K. , & Morrow, A. L. (2013). Protection, promotion, and support and global trends in breastfeeding. Advances in Nutrition, 4(2), 213–219. 10.3945/an.112.003111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDaniel, R. R. Jr. , Lanham, H. J. , & Anderson, R. A. (2009). Implications of complex adaptive systems theory for the design of research on health care organizations. Health Care Management Review, 34(2), 191–199. 10.1097/HMR.0b013e31819c8b38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran, A. C. , Kerber, K. , Pfitzer, A. , Morrissey, C. S. , Marsh, D. R. , Oot, D. A. , … Shiffman, J. (2012). Benchmarks to measure readiness to integrate and scale up newborn survival interventions. Health Policy and Planning, 27(Suppl 3), iii29–iii39. 10.1093/heapol/czs046 [DOI] [PubMed] [Google Scholar]
- Okoli, C. , & Pawlowski, S. D. (2004). The Delphi method as a research tool: An example, design considerations and applications. Information Management, 42(1), 15–29. 10.1016/j.im.2003.11.002 [DOI] [Google Scholar]
- Perez‐Escamilla, R. , Curry, L. , Minhas, D. , Taylor, L. , & Bradley, E. (2012). Scaling up of breastfeeding promotion programs in low‐ and middle‐income countries: The “breastfeeding gear” model. Advances in Nutrition, 3(6), 790–800. 10.3945/an.112.002873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez‐Escamilla, R. , Martinez, J. L. , & Segura‐Perez, S. (2016). Impact of the Baby‐friendly Hospital Initiative on breastfeeding and child health outcomes: A systematic review. Maternal & Child Nutrition, 12(3), 402–417. 10.1111/mcn.12294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez‐Escamilla, R. , & Sellen, D. (2015). Equity in breastfeeding: Where do we go from here? Journal of Human Lactation, 31(1), 12–14. 10.1177/0890334414561062 [DOI] [PubMed] [Google Scholar]
- Reis, R. S. , Salvo, D. , Ogilvie, D. , Lambert, E. V. , Goenka, S. , & Brownson, R. C. (2016). Scaling up physical activity interventions worldwide: Stepping up to larger and smarter approaches to get people moving. The Lancet, 388(10051), 1337–1348. 10.1016/s0140-6736(16)30728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollins, N. C. , Bhandari, N. , Hajeebhoy, N. , Horton, S. , Lutter, C. K. , Martines, J. C. , … Victora, C. G. (2016). Why invest, and what it will take to improve breastfeeding practices? The Lancet, 387(10017), 491–504. 10.1016/s0140-6736(15)01044-2 [DOI] [PubMed] [Google Scholar]
- Shekar, M. , Kakietek, J. , Eberwein, J. , & Walters, D. (2016). An investment framework for nutrition In Reaching the global targets for stunting, anemia, breastfeeding, and wasting. World Bank: Group. [Google Scholar]
- Sinha, B. , Chowdhury, R. , Sankar, M. J. , Martines, J. , Taneja, S. , Mazumder, S. , … Bhandari, N. (2015). Interventions to improve breastfeeding outcomes: A systematic review and meta‐analysis. Acta Paediatrica, 104(467), 114–134. 10.1111/apa.13127 [DOI] [PubMed] [Google Scholar]
- UN . (2016). Joint statement by the United Nations Special Rapporteurs on the Right to Food, Right to Health, the Working Group on Discrimination against Women in law and in practice, and the Committee on the Rights of the Child in support of increased efforts to promote, support and protect breast‐feeding. from http%3A%2F%2Fwww.ohchr.org%2FEN%2FNewsEvents%2FPages%2FDisplayNews.aspx%3FNewsID%3D20871%26amp%3BLangID%3DE%2523sthash.NbpPVEPz.dpuf
- Victora, C. G. , Bahl, R. , Barros, A. J. D. , França, G. V. A. , Horton, S. , Krasevec, J. , … Rollins, N. C. (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. The Lancet, 387(10017), 475–490. 10.1016/s0140-6736(15)01024-7 [DOI] [PubMed] [Google Scholar]
- Victora, C. G. , Horta, B. L. , de Mola, C. L. , Quevedo, L. , Pinheiro, R. T. , Gigante, D. P. , … Barros, F. C. (2015). Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: A prospective birth cohort study from Brazil. The Lancet Global Health, 3(4), e199–e205. 10.1016/s2214-109x(15)70002-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WABA . (1993). The global participatory action research (GLOPAR) project. World Alliance for Breastfeeding Action. [Google Scholar]
- WHO (2003). Infant and young child feeding: A tool for assessing national practices, policies and programmes. World Health Organization. [Google Scholar]
- WHO (2014, 2014). Global nutrition targets 2025: Policy brief series (WHO/NMH/NHD/14.2). Geneva: World Health Organization; http://apps.who.int/iris/bitstream/10665/149018/1/WHO_NMH_NHD_14.2_eng.pdf?ua=1 [Google Scholar]
- WHO , & UNICEF . (2006). Infant young child feeding counselling: An integrated course. http://www.who.int/nutrition/publications/infantfeeding/9789241594745/en/
- WHO , & UNICEF . (2009). Baby‐friendly hospital initiative: revised, updated and expanded for integrated care. Section 3, Breastfeeding promotion and support in a baby‐friendly hospital: a 20‐hour course for maternity staff. https://www.unicef.org/nutrition/files/BFHI_2009_s3.1and2.pdf [PubMed]
- WHO , & UNICEF . (2012). The Community Infant and Young Child Feeding Counseling Package. https://www.unicef.org/nutrition/files/Planning_Guide_October_2012.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1.
Supporting information


