Abstract
The aim of health guidelines is to ensure consistency in the delivery of care to minimise health‐related complications. However, even when good evidence is available, professionals do not necessarily implement it. Following a 2011 survey (Time 1) of staff in a tertiary maternity hospital, a number of service changes were implemented to facilitate best practice delivery of care to pregnant women regarding gestational weight gain (GWG). A (second) staff survey was then undertaken to re‐assess staff knowledge, attitudes and behaviours around the management of GWG in our hospital. This cross‐sectional, prospective online survey was distributed to staff in antenatal clinic. The survey assessed staff awareness of pregnancy‐related weight complications, knowledge and application of specific guidelines, and a guideline adherence score was calculated. Sixty‐nine staff (44.8% response rate) completed the 2014 (Time 2) survey. Just over half (51.9%) stated they were familiar with clinical guidelines regarding weight management in pregnancy. Guideline adherence ranged from 3.7 ± 1.9 to 11.3 ± 1.0 /15 across different professional groups; significant improvements with adherence by dietitians were noted over time. Despite minimal change over time in the overall adherence score, compliance with individual elements of the guideline recommendations comprising the adherence score differed. Improvements in staff practices and attitudes are apparent since the first survey. However, further improvements in guideline awareness and guideline elements are still required to improve the delivery of best practice antenatal GWG care.
Keywords: implementation, guidelines, obesity, overweight, pregnancy, weight gain
Introduction
The aim of an evidence‐derived health service guideline is to manage, and ideally reduce, health‐related risks and to ensure consistency in the delivery of care. The IOM (Institute Of Medicine 2009) and Queensland Health Maternity and Neonatal Clinical Guidelines for Obesity (‘the statewide Obesity guideline’) (Queensland Health 2011) provide advice regarding recommended gestational weight gain (GWG) based on pre‐pregnancy body mass index (BMI). Additionally, the Queensland Health guidelines outline referral practices for care, including specialist support and postpartum advice, with clear links to improved maternal and neonatal outcomes. Summary recommendations from the guidelines are in Fig. 1.
Figure 1.
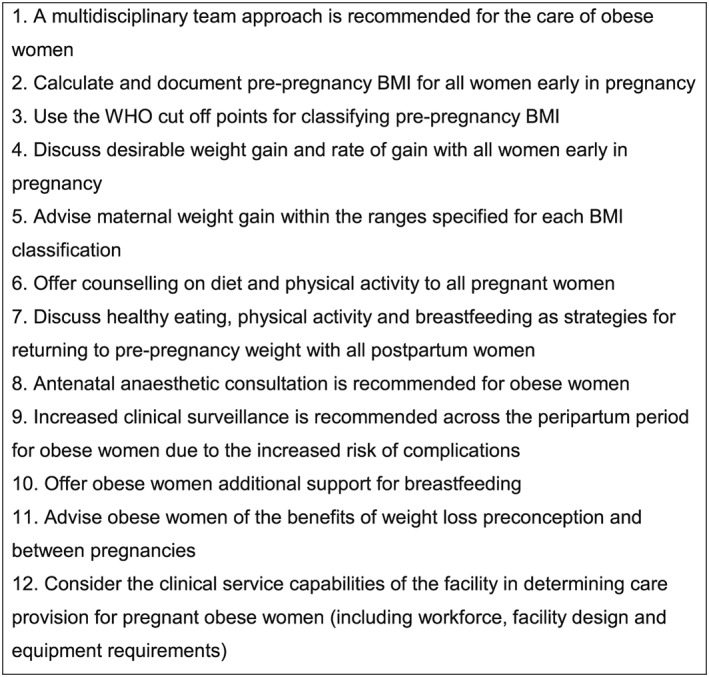
The 12 summary recommendations from the Queensland Health Obesity guidelines.
Pregnant women who gain weight in accordance with the US Institute of Medicine (IOM) guidelines, also adopted for use in Australia (Institute Of Medicine 2009; NHMRC 2013; Royal Australian and New Zealand College Of Obstetricians And Gynaecologists 2013), have the lowest risk of pregnancy and birth‐related complications. Their infants are also at reduced risk of incurring a chronic disease during their adult lives (Institute Of Medicine 2009). However, even when good evidence is available to support behavioural change, maternity professionals do not necessarily adopt it, or disseminate it to women. Initiating discussion on ‘sensitive’ topics such as GWG, especially for overweight/obese (ow/ob) women, is known to be problematic for staff, and there is some evidence that staff who struggle with their own weight management are more reluctant to engage in such discussions (Wilkinson et al. 2013; Wilkinson & Stapleton 2012; Knight‐Agarwal et al. 2014).
Awareness and dissemination of guidelines does not always effect changes in practice, and an evidence‐practice gap may continue to exist (Grol & Wensing 2004). A systematic and theory‐driven process is essential in closing this gap and requires an assessment of influencing factors (barriers/enablers) and an implementation and evaluation plan (French et al. 2012). The use of a framework to underpin the process is highly recommended (Francis et al. 2012).
In 2011 (Time 1), we administered a survey to clinicians working at a tertiary maternity hospital in Brisbane, South East Queensland [the Mater Mothers' Hospital (MMH)] to assess staff knowledge, attitudes and behaviours around the management of GWG (Wilkinson & Stapleton 2012). The results showed that the staff had excellent awareness of the clinical complications related to a high BMI in pregnancy and/or excessive GWG but had poor knowledge of referral criteria, BMI cut‐off points and GWG advice (Wilkinson et al. 2013; Wilkinson & Stapleton 2012). Many staff also reported lacking confidence in their skills for supporting women achieve GWG targets (Wilkinson et al. 2013; Wilkinson & Stapleton 2012).
We analysed the 2011 survey results using an ‘implementation science’ methodology (Francis et al. 2012) and identified a number of barriers to guideline adoption (Wilkinson & Stapleton 2012). These barriers included gaps in staff's guideline content knowledge, as well as low reported levels of confidence around delivering some elements of care to ow/ob women, lack of role and delineation and ownership, as well as dietetic resourcing issues. Drawing on the theoretical domains framework (TDF) (Francis et al. 2012), barriers were assigned to the following four discrete ‘domains’: (1) knowledge; (2) skills; (3) professional/social role & identify; and (4) environmental context and resources. Articulating the TDF with the Behaviour Change Wheel (Michie et al. 2011) allowed us to identify evidence‐based interventions to address these barriers that included education of staff (skills‐based) and pregnant women, engaging clinical champions and a review of resources (including staff and equipment) and hospital policies.
The initial changes introduced into the service post the 2011 survey were delivered within existing funding and included increased dietetic time in the antenatal clinic (4 h/day compared with 4 h/week, previously). Additionally, at their ‘booking’ (first) antenatal clinic appointment, women were given a ‘Mater Personalised Pregnancy Weight Tracker’ (‘Weight Tracker’) developed in‐house by Mater Dietitians (http://wellness.mater.org.au/Our-Services/Nutrition-and-Dietetics/Outpatients/The-Mater-Personalised-Pregnancy-Weight-Tracker-©). The Weight Tracker enabled the delivery of GWG support according to the 5As (assess, advise, agree, assist and arrange (Glasgow et al. 2006)). It also advised ideal GWG goals and ranges according to women's pre‐pregnancy BMI and was informed by the IOM GWG guidelines (Institute Of Medicine 2009). Implementation of the Weight Tracker was supported by literature reporting that interventions based on diet and physical activity, in combination with supplementary weight monitoring, appear to be successful in decreasing (excessive) GWG (Streuling et al. 2010; Jeffries et al. 2009). Staff training in using the Weight Tracker was also delivered in regular (non‐mandatory) half‐yearly in services to midwives in the antenatal clinic. Group and individual dietetic appointments for all pregnant women (self‐referred or staff‐referred) included delivery and follow up of the ‘Healthy Start to Pregnancy’ initiative – an evidence‐based behaviour change workshop for pregnant women that focused on dietary intake, physical activity and healthy GWG (Wilkinson & Mcintyre 2012).
To examine possible changes in staff knowledge, attitudes and behaviours with respect to the management of GWG following the implementation of service‐wide strategies to support healthy weight gain, a second (Time 2) survey was undertaken in 2014 in the same study hospital. This paper reports these results and compares them to the results of the first (Time 1) survey in 2011.
Key messages.
Pregnant women who gain weight in accordance with the US Institute of Medicine guidelines have the lowest risk of pregnancy and birth‐related complications. Their infants are also at reduced risk of incurring a chronic disease during their adult lives.
Guidelines aim to ensure consistency in the delivery of care. However, even when good evidence is available, professionals do not necessarily implement it. Only half of the staff in our tertiary maternity centre were familiar with clinical guidelines relating to weight management in pregnancy, and staff exhibited varied adoption of these guidelines.
Evidence‐based strategies targeting known barriers to guideline adoption were used to facilitate implementation of pregnancy weight gain guidelines.
Guideline adherence improved. However, further strategies and initiatives are required to address deficits in specific guideline awareness and elements to improve the delivery of best practice antenatal gestational weight gain care.
Materials and methods
Design and participants
This cross‐sectional study utilised a prospective online survey, adapted for use with permission (Herring et al. 2010). It was distributed to maternity staff (obstetricians, midwives and allied health) involved in delivering care to publically insured women attending a tertiary maternity hospital (MMH) for outpatient antenatal care.
Procedure
Staff were invited, via an email sent by their managers, to complete an online survey, which remained open for 3 weeks over July/August 2014; completion required approximately 10 min. An information sheet was attached to the email invitation, and two reminders were sent, at the end of the first and second weeks, respectively. Participants were informed that survey completion was voluntary and consent was implied by completion and return. The online platform rendered all responses anonymous.
Survey tool
The 15‐item survey assessed staff awareness of pregnancy‐related ow/ob complications, knowledge and application of the statewide Guideline (Queensland Health 2011), as well as knowledge and use of other pertinent guidelines. Practice‐based questions requested information about the clinical care staff provided and their opinions about patients' abilities to manage their GWG, and/or to change their lifestyles and behaviours. Responses were selected from a 4‐point Likert scale from ‘strongly disagree’ to ‘strongly agree’, with options for ‘not advising my patient about this’ and ‘don't know’ for questions about their opinion about the care they provided or from ‘almost never’ to ‘almost always’, and options for ‘this is not appropriate’ and ‘this is not my job’ for questions about practices in a woman's first and 36 week visits. The survey also sought information about the advice staff offered to women and/or if they thought their advice instigated behavioural changes. Staff were also asked about referral patterns to services such as dietetics and anaesthesiology, or for screening procedures, including the early oral glucose tolerance test (OGTT), and the BMI each was undertaken (or if this was ‘not appropriate’ or ‘not my job’). Staff were asked to comment on the resources available to them, including consultation time, training availability and usefulness and which guidelines informed their practice. Staff rated from 1 (does not inform my practice) to 5 (strongly informs my practice), as well as ‘not being aware’ of the guidelines. Additionally, if the staff indicated that they did not use the guidelines it was indicated whether this was because of them being ‘unaware’, ‘unable to access’, ‘not applicable’ or ‘other’. Questions only asked at Time 2 were related to how often women in their care were weighed, the reasons for not weighing and more detailed questions relating to guideline awareness and use.
Data analysis
Data were analysed using spss for Windows version 15 (SPSS, Chicago, Illinois). Descriptive statistics were used to summarise staff characteristics. Means and standard deviations were used to summarise normally distributed continuous data. Categorical data were summarised using frequencies and percentages.
Although the statewide Guideline focuses on obesity, because of the significant and increasing proportion of the maternity population with BMIs above 25 kg m−2, and the strong evidence linking this to excessive GWG (Gunderson 2009; Guelinckx et al. 2008), some questions also related to care delivered to women who were overweight. These were questions relating to opinions about the care they (staff) provided, processes undertaken in a woman's first visit. When presenting results, we specify where data are grouped compared with data that relates exclusively to obesity. A composite guideline adherence score was calculated by summing responses to questions adapted from the 12 key recommendations in the Queensland Health guideline [7] as ‘correct’ or ‘incorrect’. Questions that allowed for double responses (e.g. ‘Offer diet and physical activity counselling to women’) were split for clarity [(1) ‘Offer diet counselling to women’ and (2) ‘Offer physical activity counselling to women’]. Hence, the original 12 recommendations for the care of obese women (from Fig. 1) increased to 15 and to 13 with respect to the care of overweight women. Between group differences were assessed with independent group t‐tests (continuous variables) and independent group Chi‐squared tests or Fisher's Exact tests [categorical, depending on cell size; spss version 16 and STATA version 10.1 (StataCorp. 2007, Stata Statistical Software: Release 10, College Station, TX, USA), respectively]. Assessment of correct BMI cut‐offs used the World Health Organisation classifications of underweight (<18.5 kg m−2), healthy weight (18.5–24.9 kg m−2), overweight (25–29.9 kg m−2) and obese (>30 kg m−2). Answers within 0.1 kg m−2 were considered correct (e.g. to account for a healthy weight range provided as 18.5–25 kg m−2). A ‘rounded’ category was also assessed, with correct answers being within 0.5 kg m−2. Significance was set at P < 0.05. Data from the 2014 survey (Time 2) were compared with data collected in the original 2011 (Time 1) survey (Wilkinson & Stapleton 2012).
Ethical considerations
Ethical approval was obtained from the hospital's Human Research Ethics Committee (HREC/14/MHS/119).
Results
Participant demographics
Sixty‐nine staff completed the Time 2 survey. The overall response rate (44.8%) comprised 21/35 obstetrician/gynaecologists (O and G) (29.4% of sample), 18/69 midwives (33.3%), 2/8 obstetric medicine physicians (3.7%), 9/14 physiotherapists (16.7%) and 4/4 dietitians (7.4%). Staff characteristics are displayed in Table 1.
Table 1.
Response rates by maternity care provider group between the 2011 (Time 1) and 2014 (Time 2) surveys
| n (%) Time 1 (2011) | n (%) Time 2 (2014) | % of staff Time 1 | % of staff Time 2 | |
|---|---|---|---|---|
| Response rate from eligible staff | 68/114 (59.6) | 65/145 (44.8) | ||
| Provider type | ||||
| Obstetrician | 20/40 (29.4) | 21/35 (38.9) | 50 | 60 |
| Obstetric Medicine | — | 2/8 (3.7) | — | 25 |
| Midwife | 35/58 (51.5) | 18/69 (33.3) | 60.3 | 26.1 |
| Physiotherapist | 10/13 (14.7) | 9/14 (16.7) | 76.9 | 64.3 |
| Dietitian | 3/3 (4.4) | 4/4 (7.4) | 100 | 100 |
| Total | ||||
The majority of respondents reported ow (96.3%)/ob (98.2%) as an ‘important/very important’ maternity health issue, with 88.9% (ow) and 94.4% (ob) indicating it was important/very important in their own clinical practice. These findings were similar to the 2011 (Time 1) survey. Most staff recognised the relationship between obesity in pregnancy and a wide range of metabolic, pregnancy/birth‐related and long‐term/chronic maternal and neonatal health sequelae. Approximately one‐third (31.5%) of the study sample had received training in the care of ow/ob pregnant women (compared with 20.2% in 2011, P = 0.3).
Guideline awareness
Just over half (51.9%) of the staff surveyed in 2014 stated they were familiar with clinical guidelines regarding the care of women who were ow/ob. However, only 16.7% reported that the Queensland Health guideline influenced their practice, with 33.3% being unaware of the guideline (Table 2). Approximately one‐quarter of staff reported that their practice was informed by the Weight Tracker, the Australian Dietary Guidelines, the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) guidelines and the MMH Obesity policy (Table 2).
Table 2.
Staff responses regarding the guidelines (and other resources) that they were aware of and/or informed their practice
| Guideline/resource | Informs practice (%) | Not aware of guideline/ resource (%) |
|---|---|---|
| MMH Personalised Pregnancy Weight tracker | 35.2 | 14.8 |
| Australian Guide to Healthy Eating (Australian Dietary Guidelines) | 29.6 | 18.5 |
| RANZCOG Obesity guidelines | 27.8 | 24.1 |
| MMH Obesity policy | 27.8 | 25.9 |
| Queensland Health Obesity guidelines | 16.7 | 33.3 |
| IOM GWG guidelines | 11.2 | 35.2 |
GWG, gestational weight gain; IOM, Institute of Medicine; MMH, Mater Mother's Hospital; RANZCOG, Royal Australian and New Zealand College of Obstetricians and Gynaecologists.
Guideline adherence
At Time 2, adherence to guidelines (as indicated with the guideline adherence score) rated out of 13 (ow) or 15 (ob) ranged from 4.1 ± 1.5 to 11.8 ± 0.5 (ow) and 3.7 ± 1.9 to 11.3 ± 1.0 (ob) across different professional groups (Table 3). No significant difference was observed in the scores from participants over time for either care of women in overweight or obese BMI categories, except for dietitians between Time 1 and Time 2, with respect to overweight women. Despite minimal changes over time in the overall adherence score (Table 3), individual elements of the guideline recommendations that make up the adherence score showed significant differences (Fig. 2). Significant improvements from Time 1 to 2 were seen in staff calculating pre‐pregnancy BMI (P = 0.001), staff discussing GWG (P = 0.002) and correct advice being provided in these GWG discussions (P = 0.002). Improvements in promoting breastfeeding (P = 0.053) and referrals to a dietitian for postnatal advice (P = 0.07) approached significance.
Table 3.
Queensland Health Obesity [6] guideline adherence scores by maternity care provider group between the 2011 (Time 1) and 2014 (Time 2) surveys
| Guideline adherence | ||||
|---|---|---|---|---|
| Overweight (max/13) Time 1 | Obese (max/15) Time 1 | Overweight (max/13) Time 2 | Obese (max/15) Time 2 | |
| Provider type | ||||
| Obstetrician | 4.6 ± 2.4 | 6.3 ± 3.0 | 4.0 ± 2.6 | 4.8 ± 3.2 |
| Obstetric Medicine | — | 9.5 ± 2.1 | 10.0 ± 4.2 | |
| Midwife | 5.7 ± 3.6 | 6.6 ± 4.1 | 7.2 ± 2.8 | 8.3 ± 2.8 |
| Physiotherapist | 4.1 ± 1.5 | 4.4 ± 1.7 | 4.0 ± 1.7 | 3.7 ± 1.9 |
| Dietitian | 10.3 ± 0.6* | 10.3 ± 0.6 | 11.8 ± 0.5* | 11.3 ± 1.0 |
| Total | 5.3 ± 3.2 | 6.3 ± 3.5 | 5.6 ± 3.4 | 6.4 ± 3.7 |
P = 0.02.
Figure 2.
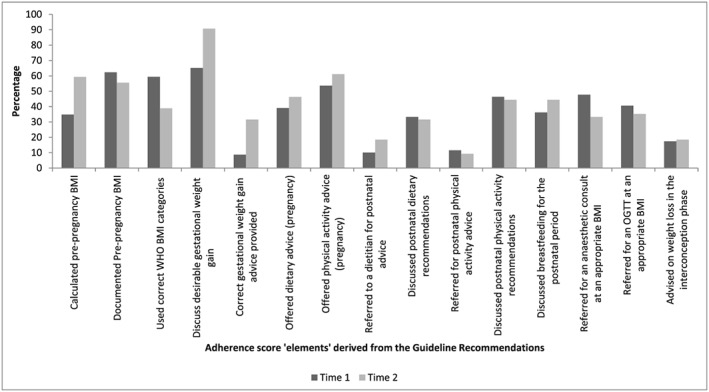
Percentage of correct guideline recommendation elements (that formed the Guideline Adherence score) undertaken by staff at Times 1 (2011) and 2 (2014). Significant improvements from Time 1 to 2 were seen in staff calculating pre‐pregnancy body mass index (BMI) (P = 0.001).
Awareness of BMI category and GWG goals
Significant increases were observed from Time 1 to Time 2 in staff awareness of the World Health Organisation categorisation of BMI with respect to the underweight range (P = 0.03) (Table 4). Greater levels of significance were noted when staff responses were ‘rounded’ (underweight 8.7–63.0% correct, P < 0.001; healthy weight range 14.5–51.9%, P < 0.001). The proportion of staff who provided patients with correct GWG advice increased from Time 1 to 2 for underweight women (P = 0.02) and women in the obese range (P = 0.045). The proportion of staff who reported ‘don't know’, or left their responses blank, decreased for all categories of BMI cut‐offs and GWG advice, except for the BMI cut‐offs for women in the obese category.
Table 4.
Proportion of correct responses to questions regarding BMI categories and pregnancy gestational weight gain
| BMI category and gestational weight gain goal | Proportion of staff who correctly identified cut‐offs for each BMI range [correct (missing/don't know) %] | Proportion of staff who provided correct weight gain advice, per BMI category [correct (missing/don't know) %] | ||
|---|---|---|---|---|
| Time 1 | Time 2 | Time 1 | Time 2 | |
| Underweight | 8.7 (18.8)^ | 25.9 (3.7)^ | 7.2 (49.3)† | 25.9 (35.2)† |
| Healthy weight | 14.5 (17.4) | 27.8 (3.7) | 10.1 (49.3) | 27.8 (18.5) |
| Overweight | 53.6 (15.9) | 57.4 (9.3) | 10.1 (52.2) | 22.2 (31.5) |
| Obese | 59.4 (15.9) | 38.9 (48.1) | 10.1 (52.2)‡ | 31.5 (9.3)‡ |
BMI, body mass index.
Underweight (<18.5 kg m−2: 12.5–18 kg); healthy weight (18.5–24.9 kg m−2: 11.5–16 kg); overweight (25–29.9 kg m−2: 7–11.5 kg); obese (>30 kg m−2: 5–9 kg).
P = 0.03.
P = 0.02.
P = 0.045.
Referral practices
Compliance with BMI‐driven guideline referral criteria varied considerably. A significant improvement was observed in the proportion of staff indicating the correct referral BMI category for OGTT (>30 kg m−2) from Time 1 (10.1%) to Time 2 (35.2%) (P < 0.001). No changes were seen in the correct BMI identification for referring women to a dietitian (>30 kg m−2) from Time 1 (17.3%) to Time 2 (18.6%), or for an anaesthetic review using the Queensland Health guidelines (>35 kg m−2), Time 1 (31.8%) and Time 2 (33.3%), and the MMH guidelines (>40 kg m−2), Time 1 (46.3%) and Time 2 (50.0%).
Practice opinions
Table 5 presents staff perceptions of their effectiveness in advising women about GWG and their influence in effecting behaviour change from Time 1 to 2. Fig. 3 illustrates responses by professional group from the Time 2 survey. Significant improvements in the overall staff scores were noted for three practices considered to be important in supporting healthy GWG in high BMI women: (1) staff feeling they had sufficient knowledge to counsel women; (2) staff believing they had sufficient resources available to support women; and (3) staff believing that women found their advice helpful. High scores at both time points were noted for staff reporting that nutrition and dietetic referrals were readily available and that staff wanted more training.
Table 5.
Overall scores (all professions combined) from Time 1 and Time 2 regarding practice opinions and behaviours that may influence gestational weight gain outcomes
| Overall cohort scores for practice statements | P‐value | ||
|---|---|---|---|
| Time 1 | Time 2 | ||
| My advice influences how much weight my patients gain | 2.7 ± 0.6 | 2.9 ± 0.8 | 0.5 |
| I have enough time to counsel my patients properly about the risks of ow/ob during pregnancy | 2.4 ± 0.9 | 2.5 ± 0.8 | 0.5 |
| I have sufficient knowledge to counsel my ow/ob patients to improve their pregnancy outcomes | 2.5 ± 0.8 | 2.9 ± 1.0 | 0.03 |
| I would like more training about this to help me counsel my ow/ob patients to improve their pregnancy outcomes | 3.5 ± 0.7 | 3.3 ± 0.8 | 0.3 |
| Nutrition and dietetic referrals are available for my ow/ob patients | 3.6 ± 0.8 | 3.8 ± 0.4 | 0.06 |
| Once an ow/ob woman is already pregnant there is not much she can do to change her risks | 1.6 ± 0.7 | 1.5 ± 0.6 | 0.5 |
| My ow/ob patients are motivated to make changes for their health | 2.3 ± 0.8 | 2.4 ± 0.8 | 0.8 |
| My ow/ob patients have the resources they need to make the changes that I recommend | 2.4 ± 0.8 | 2.8 ± 0.8 | 0.03 |
| My ow/ob patients find my advice helpful for weight management during pregnancy | 2.8 ± 0.6 | 3.1 ± 0.6 | 0.04 |
Ow/ob, overweight/obese.
Figure 3.
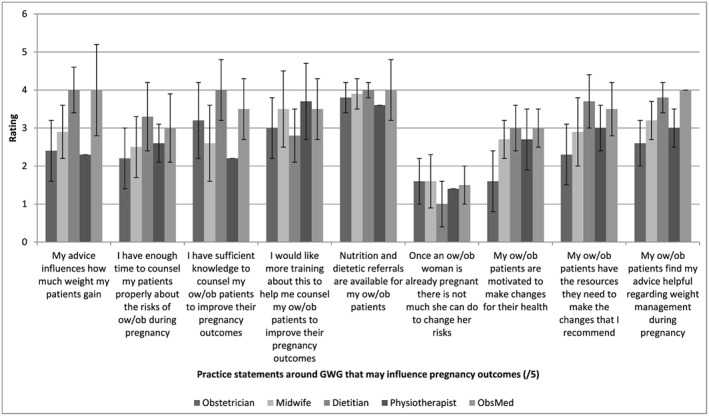
Practice statements by professional group at Time 2 regarding practice opinions and behaviours that may influence gestational weight gain (GWG) outcomes. ow/ob, overweight/obese.
Weighing women and discussing weight gain
Fewer than 15% of respondents (9.3%) reported weighing women at every appointment or at key appointments (e.g. booking, K28, K36) (5.6%). Almost one‐third of respondents (31.5%) reported weighing women only at their booking in appointment, while nearly one‐quarter (24.1%) reported never weighing women. Reasons for not weighing included no scales available (n = 15), no need (n = 12) or no time (n = 9). Half of survey respondents used a BMI of >30 kg m−2 as a threshold to discuss GWG with women while just under one‐quarter (24.1%) discussed GWG only with women whose BMI was >25 kg m−2. Half of the staff surveyed believed their advice influenced GWG, and 42% reported they always offered GWG advice; 51.9% stated they offered advice only to selected women (although which women was not specified). These questions were only asked at Time 2.
Providing dietary and physical activity advice
Almost half of respondents reported that they always (24.1%) or usually (22.2%) offered dietary advice to overweight and obese women. Dietary advice included avoiding fast food or takeaways (64.8%) and sugar‐sweetened drinks (59.3%), eating regular meals (55.6%), using the MMH's ‘Healthy eating during pregnancy’ booklet (55.6%), eating breakfast daily (46.3%) and following/using the Weight Tracker (42.6%).
A large proportion of respondents were familiar with the Physiotherapy referral process (70.4%) and knew about locally available ‘Physiotherapy Exercise in Pregnancy’ classes (61.1%). Only one‐third of staff surveyed (33.3%) were aware of the Australian National Physical Activity Guidelines (Commonwealth Department of Health and Aged Care 1999); however, 46.3% were familiar with the RANZCOG guidelines for safe exercise in pregnancy and even more (55.6%) knew that physical activity guidelines changed for women diagnosed with pelvic girdle pain or pelvic organ prolapse. Over half of the staff surveyed reported that they asked women about their current levels of physical activity, if they were ow/ob (50%), and discussed the benefits of physical activity with women who were overweight (59.2%) or obese (55.5%). Fewer staff (40.8%) reported that they discussed safety guidelines for specific exercise with ow/ob women or recommended appropriate options for safe exercise if women were overweight (46.3%) or obese (48.2%).
Discussion
Improvements in staff knowledge, attitudes and behaviours regarding the management of GWG have been observed in our tertiary maternity hospital since the first survey was conducted in 2011 (Wilkinson & Stapleton 2012). Elements of care essential to best practice management of GWG, such as documenting pre‐pregnancy BMI and discussing and correctly advising women about GWG goals, showed significant change in a positive direction. The previous (high) guideline adherence shown by the dietitians in the first (2011) survey increased significantly (in the small cohort surveyed). Additionally, the basic dietary and physical activity advice provided by many of the staff was in line with the recommendations. However, despite these improvements, adherence scores of 50% or less were noted for many of the statewide Guideline steps for the delivery of best practice.
The service changes implemented were informed by and then introduced after analysis of data from the first survey identified barriers to best practice to support women achieving healthy GWG, with a specific focus on overweight and obese women (Wilkinson & Stapleton 2012). It can be difficult to identify specific interventions responsible for improvements, which may occur when a suite of changes are implemented concurrently. Michie (2014) noted that interventions based on environmental restructuring, restriction (of processes or practices), enablement, incentivisation and/or coercion were more effective than relying on an individual's choice to facilitate decision‐making behaviours (i.e. the delivery of best practice) becoming automatic (Michie 2014). The resourcing changes (e.g. increased availability of dietitians in the antenatal clinic and the use and promotion of the Weight Tracker) may have facilitated the improvements observed in guideline adherence. This may have been enabled through more time available to fulfil requirements of delivering evidence‐based care and by also allowing staff to feel there were dietetic referrals available. Additionally, it is possible that the use of the Weight Tracker by staff to guide the GWG advice they offered to women may have helped to trigger the changes observed.
The significant improvements in staff advising women on (correct) GWG goals per BMI category, as well as the reduction in staff reporting ‘not knowing’ GWG goals, are promising. The provision of GWG guidelines by health professionals, and knowledge regarding appropriate GWG, is predictive of meeting GWG guidelines (Cogswell et al. 1999; Tovar et al. 2011). A recent study has shown that having health providers offer IOM GWG recommendations increased the likelihood of women setting a GWG goal that aligns with the recommendations (vs. no goal) (OR = 5.3, 95% CI: 1.5, 18.6), which in turn was predictive of women gaining weight within IOM guideline ranges (Tovar et al. 2011).
As noted, many of the statewide Guideline steps for the delivery of best practice had low adherence. Further, there was overall low awareness of guidelines or resources pertaining to the management of GWG. Interestingly, the guideline with the lowest rating for awareness and/or informing clinicians' practice was the IOM guideline (Institute Of Medicine 2009), which informs the content of other GWG‐related guidelines (NHMRC 2013; Royal Australian and New Zealand College Of Obstetricians And Gynaecologists 2013; Queensland Health 2011), the MMH Obesity policy and tools such as the Weight Tracker. While respondents may have integrated elements of all the guidelines into their practice without necessarily being aware of the source, it is important that staff are aware of the guidelines (and their full content) to facilitate comprehensive evidence‐based care delivery.
Results from this study will direct the refinement of further interventions at the study site, which will aim to continue improving guideline adherence. Barriers to guideline adherence identified in both surveys included gaps in GWG knowledge, inconsistent weighing and monitoring practices and staff confidence in their own capabilities in delivering care to these women. Barriers also existed regarding supporting women in preparation for the postnatal period, although referrals and advice for diet, physical activity and breastfeeding did show a trend of increasing in the most recent survey. Enablers that may facilitate the adoption of future interventions include staff believing that women find their advice helpful, women having the resources and motivation to effect behaviour change and that they did not consider it was too late to change, sufficient dietetic referrals available and staff willingness to participate in further training in delivering best practice care for achieving healthy GWG. Further, enablers that were identified included an active hospital‐based service improvement and research culture at both clinical and managerial levels, as well as the availability of specialist maternal health dietitians and physiotherapists.
Emergent themes from this study, plus current literature, will be used to formulate a service‐wide policy on the management of GWG. Interventions will be operationalised as skills‐based training, engagement of clinical champions, recording of weight (at agreed pregnancy milestones) and additional resources (the availability of extra scales within consulting rooms). The training content aims will be to specifically target the barriers outlined earlier and will be informed by the implementation science literature to facilitate skill development and behaviour change, as well as to incorporate findings from many studies regarding qualitative experiences of staff and women in providing GWG care.
The importance of a service‐wide approach has been identified in a number of studies, which have highlighted that communication must be consistent across health care professionals, with ‘weight (being) everyone's business’, and should promote healthy GWG to women of all BMIs (Willcox et al. 2012; Furness et al. 2011; Bick 2015). This should be reinforced/introduced through training that takes a systematic approach (Olander et al. 2010; Furness et al. 2011; Heslehurst et al. 2012). Although studies have shown that some staff consider GWG to be a sensitive topic, many are also deeply concerned about the physiological impact of inappropriate GWG (Knight‐Agarwal et al. 2014; Willcox et al. 2012; Heslehurst et al. 2012; Furness et al. 2011). It will also be highlighted that women find receiving advice from their midwives helpful and report feeling that if GWG is not discussed with them that it must not be important (Olander et al. 2010).
In developing the service wide approach, consideration will be given to appropriate evidence‐based strategies, particularly around recording of women's weight measurements and discussion of weight. Interestingly, a recent quality improvement activity in a New South Wales rural referral hospital aiming to implement and evaluate a clinical care pathway for women with a BMI >35 kg m−2 found women did not take up the offer of self‐weighing prior to or during clinic attendance (Fealy et al. 2014). An attempt at ‘avoiding’ potentially difficult processes and conversations was not effective. Strategies to develop rapport with women and to decrease staff's concerns, particularly around discussion of weight and obtaining and recording women's weight measurements, are likely to be more effective. The knowledge that words such as ‘weight’ and ‘BMI’ are more likely to be positively received than references to ‘fat’ and/or (morbidly) ‘obese’ (Wadden & Didie 2003; Thomas et al. 2008) will be incorporated into staff training to facilitate this process.
Strengths of this study include its strong theoretical underpinnings of assessment of barriers (Francis et al. 2012), as well as selection of evidence‐based interventions to target the identified barriers. However, we also acknowledge a number of limitations, including a lower than desirable response rate and the reliance on managers to forward emails to their staff groups. A comparable number of staff completed the survey at both time points, but the relatively lower response rate was because of a wider email circulation (i.e. larger denominator). Additionally, compared with the 2011 study, fewer midwifery staff completed the survey. This may reflect lower interest or ease of access to emails by midwifery staff. Midwifery survey engagement was an acknowledged barrier in 2011 and, despite the provision of a pen‐and‐paper survey in 2014, no midwife utilised this survey method. A nested longitudinal cohort analysis was also planned, but because of staff turnover and rotation through clinical areas, fewer than 10 staff completed the survey at both time points preventing this analysis.
It is also acknowledged that the survey questions assessed intention rather than actual behaviour in the delivery of care around this clinical issue. Future research will monitor direct outcomes related to guideline recommendations, such as correct recording of weight, GWG goals and calculation of pre‐pregnancy BMI, referral rates, as well as actual and overall GWG identification.
Conclusions
Implementation of initiatives to address identified barriers to guideline adherence can improve staff practices and attitudes to support healthy GWG. However, further strategies and initiatives are required to address deficits in specific guideline awareness and elements to improve the delivery of best practice antenatal GWG care.
Source of funding
Nil funding was received for undertaking this study.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
SW conceived the study, and SW and HS developed the study. SW analysed the data, and all authors interpreted the data. SW drafted the manuscript, and all authors provided significant critical input into the manuscript.
Acknowledgements
Dr Shelley Wilkinson is supported by the Queensland Health Research Fellowship (2015–2018).
Wilkinson, S. A. , Donaldson, E. , Beckmann, M. , and Stapleton, H. (2017) Service‐wide management of healthy gestational weight gain following an implementation science approach. Maternal & Child Nutrition, 13: e12266. doi: 10.1111/mcn.12266.
References
- Bick D. (2015) The challenge of obesity during pregnancy: when to intervene and what could work? Midwifery 31, 655–656. [DOI] [PubMed] [Google Scholar]
- Cogswell M.E., Scanlon K.S., Fein S.B. & Schieve L.A. (1999) Medically advised, mother's personal target, and actual weight gain during pregnancy. Obstetrics And Gynecology 94, 616–622. [DOI] [PubMed] [Google Scholar]
- Commonwealth Department of Health and Aged Care (1999) National Physical Activity Guidelines for Australians. DHAC: Canberra. [Google Scholar]
- Fealy, S. , Hure, A. J. , Browne, G. & Prince, C. 2014. Developing a clinical care pathway for obese pregnant women: a quality improvement project. Women and Birth 27, e67–e71. Available at: 10.1016/j.wombi.2014.09.001. (Accessed 25 January 2015). [DOI] [PubMed] [Google Scholar]
- Francis J.J., O'Connor D. & Curran J. (2012) Theories of behaviour change synthesised into a set of theoretical groupings: introducing a thematic series on the theoretical domains framework. Implementation Science 7, 35. doi: 10.1186/1748-5908-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French S.D., Green S.E., O'connor D.A., Mckenzie J.E., Francis J.J., Michie S. et al. (2012) Developing theory‐informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implementation Science 7, 38. doi: 10.1186/1748-5908-7-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furness P., Mcseveny K., Arden M., Garland C., Dearden A. & Soltani H. (2011) Maternal obesity support services: a qualitative study of the perspectives of women and midwives. BMC Pregnancy and Childbirth 11, 69. doi: 10.1186/1471-2393-11-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow R.E., Emont S. & Miller D.C. (2006) Assessing delivery of the ‘5As’ for patient‐centered counseling. Health Promotion International 21, 245–255. [DOI] [PubMed] [Google Scholar]
- Grol R. & Wensing M. (2004) What drives change? Barriers to and incentives for achieving evidence‐based practice. Medical Journal Australia 180, s57–60. [DOI] [PubMed] [Google Scholar]
- Guelinckx I., Devlieger R., Beckers K. & Vansant G. (2008) Maternal obesity: pregnancy complications, gestational weight gain and nutrition. Obesity Reviews 9, 140–150. [DOI] [PubMed] [Google Scholar]
- Gunderson E.P. (2009) Childbearing and obesity in women: weight before, during and after pregnancy. Obstetrics & Gynecology Clinics of North America 36, 317–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herring S., Platek D., Elliott P., Riley L., Stuebe A. & Oken E. (2010) Addressing obesity in pregnancy: what do obstetric providers recommend? Women's Health 19, 65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heslehurst, N. , Russell, S. , Mccormack, S. , Sedgewick, G. & Rankin, J. 2012. Midwives perspectives of their training and education requirements in maternal obesity: a qualitative study. Midwifery 29 (7), 736–744. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (2009) Weight Gain During Pregnancy: Reexamining the Guidelines. The National Academies Press: D.C., Washington. [PubMed] [Google Scholar]
- Jeffries K., Shub A., Walker S.P., Hiscock R. & Permezel M. (2009) Reducing excessive weight gain in pregnancy: a randomised controlled trial. Medical Journal of Australia 191, 429–433. [DOI] [PubMed] [Google Scholar]
- Knight‐Agarwal C.R., Kaur M., Williams L.T., Davey R. & Davis D. (2014) The views and attitudes of health professionals providing antenatal care to women with a high BMI: a qualitative research study. Women and Birth 27, 138–144. [DOI] [PubMed] [Google Scholar]
- Michie S. (2014) Implementation science: understanding behaviour change and maintenance. BMC Health Services Research 14 (Suppl 2), 09. doi: 10.1186/1472-6963-14-S2-O9. [DOI] [Google Scholar]
- Michie S., Van Stralen M.M. & West R. (2011) The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Science 6: 42 doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHMRC (2013) Australian Dietary Guidelines: Eat for Health. National Health and Medical Research Council: Canberra. [Google Scholar]
- Olander E., Atkinson L., Edmunds J. & French D. (2010) The views of pre‐ and post‐natal women and health professionals regarding gestational weight gain: an exploratory study. Sexual & Reproductive Health 2, 43–48. [DOI] [PubMed] [Google Scholar]
- Queensland Health 2011. Obesity (Statewide Maternity and Neonatal Clinical Guideline) [Online]. Brisbane: Queensland Health. Available at: http://www.health.qld.gov.au/cpic/documents/mguideg_obesityv4.0.pdf [Accessed 15 June 2011].
- Royal Australian and New Zealand College of Obstetricians and Gynaecologists 2013. Management of Obesity in Pregnancy (College Statement, C‐Obs 49). Available at: http://www.ranzcog.edu.au/doc/management-of-obesity-in-pregnancy.html [Accessed 20 January 2015]. [Google Scholar]
- Streuling I., Beyerlein A. & Von Kries R. (2010) Can gestational weight gain be modified by increasing physical activity and diet counselling? A meta‐analysis of intervention trials. American Journal of Clinical Nutrition 92, 678–687. [DOI] [PubMed] [Google Scholar]
- Thomas S., Hyde J., Karunaratne A., Herbert D. & Komesaroff P. (2008) Being ‘fat’ in today's world: a qualitative study of the lived experiences of people with obesity in Australia. Health Expectations 11, 321–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tovar A., Guthrie L.B., Platek D., Stuebe A., Herring S.J. & Oken E. (2011) Modifiable predictors associated with having a gestational weight gain goal. Matern Child Hlth J 15, 1119–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadden T. & Didie E. (2003) What's in a name? Patients' preferred terms for describing obesity. Obesity Research 11, 1140–1145. [DOI] [PubMed] [Google Scholar]
- Wilkinson S. & Mcintyre H. (2012) Evaluation of the healthy start to pregnancy early antenatal health promotion workshop: a randomized controlled trial. BMC Pregnancy & Childbirth 12, 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson S., Poad D. & Stapleton H. (2013) Maternal overweight and obesity. A survey of clinicians' characteristics and attitudes, and their responses to their pregnant clients. BMC Pregnancy and Childbirth 13, 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson S. & Stapleton H. (2012) Overweight and obesity in pregnancy: the evidence‐practice gap in staff knowledge, attitudes and practices The Australian and New . Zealand Journal of Obstetrics and Gynaecology 52, 588–592. [DOI] [PubMed] [Google Scholar]
- Willcox J., Campbell K., Van Der Plight P., Hoban E., Pidd D. & Wilkinson S. (2012) Excess gestational weight gain: an exploration of midwives' views, attitudes and practice. BMC Pregnancy & Childbirth 12, 102. [DOI] [PMC free article] [PubMed] [Google Scholar]


