Abstract
A community‐based cross‐sectional study was carried out with 603 children ages 5 and under and 500 of their mothers from 510 households to examine the prevalence of undernutrition and chronic diseases among the Khasis of North‐East India. Anthropometric measurements including Mid‐Upper Arm Circumference, height, and weight were taken. Dry blood spots to estimate haemoglobin and vitamin A were collected from children and women separately by finger prick. Mothers provided data about household socio‐demographic particulars and infant and young child feeding practices. The prevalence in children of underweight was 31%, stunting was 57%, and wasting was 10%. Undernutrition was higher among boys as compared to girls. Nutrient intakes were below recommended levels. The prevalence of anaemia among children ages 1 to 5 years old was 68%, and vitamin A deficiency was 59%, and they were 83% and 48%, respectively, among women. Hypertension was observed in 15% of women, whereas diabetes was less than 1%. Only about 20% of households were food secure, and this was associated with parental literacy, per capita income, and family size. Undernutrition was unacceptably high among the Khasis despite rich food biodiversity. Proper implementation of nutritional intervention programs such as Integrated Child Development Services, Mid Day Meal, and the Public Distribution System will improve the nutrient intake and nutritional status of the population. Additionally, preservation of forest lands and products paired with judicious use of the rich food biodiversity available will promote dietary diversity and ultimately better nutrition and health.
Keywords: biodiversity, children, Khasi, North‐East India, nutritional status, women
“The staple food of the Khasis is rice and dried fish. When rice cannot be obtained or is scarce, millet or Job's tears are used instead. The latter are boiled, and a sort of porridge is obtained, which is eaten either hot or cold according to fancy.” P. R. T. Gurdon, 1863
1. INTRODUCTION
Tribal communities in India comprise an estimated 104 million Indigenous People. North‐East India, inhabited by more than 200 diverse tribes, is considered one of the most culturally diverse regions in the world. The cultural communities of Khasi, Garo, and Jaintia living in the state of Meghalaya are well known for their unique matrilineal and matrilocal cultural patterns. The Khasis are one of the 15 largest tribal cultures in India (Xaxa Committee, 2014) and the predominant tribe inhabiting Ri‐Bhoi and the East, West, and South‐West Khasi Hills districts of Meghalaya. In Khasi society, women are the heads of the household and custodians of wealth. A Khasi woman preserves her clan, her family, and her lineage while holding a position of importance and dignity in the community. The woman of the house makes all major decisions. The youngest daughter inherits the custodianship of intergenerational property and becomes the keeper of the traditional faith. The mother's brother is responsible for upholding the customary practices and judicial roles toward children, including their behavioural discipline (Lyngdoh & Nongknrih, 2015). The maternal uncle's status and role are embedded and intrinsic in the matrilineal structure with women as the head of the household, which ensures preservation of matriarchy among the Khasi society.
Meghalaya is forested terrain with one third of the area (15,657 km2) under forest cover. Shillong is the capital of the state. The West Khasi Hills district is known for its rich biodiversity and has a population of approximately 383,000, predominantly Khasi, people (Census of India, 2011). The district covers 23% of the state and is bordered by the Indian state of Assam to the north and the country of Bangladesh to the south (Figure 1). The district receives extensive rainfall and has diversified forest types that support varied flora and fauna (Mittermeier, Turner, Larsen, Brooks, & Gascon, 2011). Community forests and sacred groves are storehouses of a variety of genetic resources in this unique forest ecosystem (Khan, Khumbongmayum, & Tripathi, 2008). The rest of the land is open agricultural land, which 83% of the population depends on for their livelihood. Both settled (terraced agriculture, or bun) and shifting (slash and burn, or jhum) cultivation are practiced. The principal crops are rice, maize, millets, oilseeds, and pulses. Rice (Oryza sativa Linn.) is the most important food crop, occupying 44% of the total agricultural land, with 40% of it coming from jhum fields. Commercial crops are potato (Solanum tuberosum Linn.), sweet potato (Ipomea batatus Lam.), ginger (Zingiber officinale Rosc.), turmeric (Cucurma domestica Valeton), various oilseeds, black pepper (Piper nigrum Linn.), areca nut (https://en.wikipedia.org/wiki/Areca_catechu), betel (Piper betel) leaves, and several vegetable crops. Typical fruit crops are banana and pineapple, which are grown along with temperate fruits such as plum, pear, and peach (Meghalaya Climate Change Action Plan, Meghalaya State Development Report, and Government of Meghalaya). The natural forests support diverse insects, wild animals, plants, and nontimber forest products that provide nutritious food and income opportunities. The Khasi are known for their broad knowledge and use of this biodiversity, but how much these still form an integral part of their food system needs to be ascertained.
Figure 1.
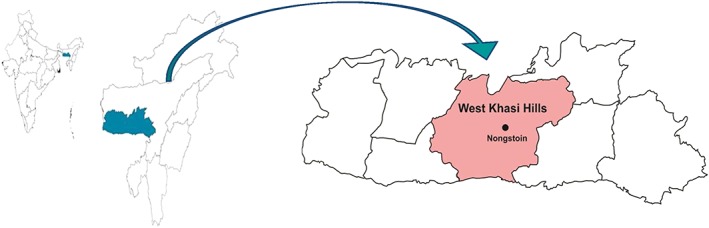
Map of West Khasi Hills in Meghalaya, North‐East India
Nutritional status for the state of Meghalaya, according to the District Level Health Survey of the International Institute for Population Sciences (IIPS; 2014), revealed high rates of childhood undernutrition with 31% underweight, 42% stunting, 17% wasting, and 71% of children under 5 with anaemia. Among the adult population, 5% have a blood glucose (used as a measure of diabetes) higher than 160 mg/dl, and 30% have hypertension (IIPS, 2014). Sporadic studies specific to Khasi women and school girls showed malnutrition among girls and nutrient intakes far below the Indian recommended levels for energy, protein, fat, calcium, iron, and carotene (Agrahar‐Murugkar, 2005; Agrahar‐Murugkar & Pal, 2004). However, there appears to be no information for specific tribal groups of North‐East India, including the Khasis.
The research presented here is part of a larger programme to assess the well‐being, agroecology, and nutritional status of Khasi women and children in the West Khasi Hills district of Meghalaya. The investigation objective is to uncover how gender roles and local food resources might contribute to improving the nutritional status of women and children. The data were gathered to establish the nutritional status in the region and to determine the priorities for food and nutrition education programs using local natural resources. The study was carried out in collaboration with North East Slow Food and Agrobiodiversity Society (NESFAS), Shillong, Meghalaya. Due to space limitations, a summary of key data is presented.
Key messages.
Child undernutrition and micronutrient deficiencies are unacceptably high among the Khasi in West Khasi Hills District, Meghalaya.
Education and behavioral change communication for better food intake during pregnancy and lactation as well as child feeding practices are needed to improve child undernutrition.
Wild food resources form an indispensible part of Khasi culture suggesting a strong bond with nature.
Community‐based strategies need to be developed to utilize the available wide food biodiversity to effectively improve the Khasi people's food security, nutrition, and health.
The nutritional potential of the Khasi people's food requires further investigation including its compositional analysis.
2. PARTICIPANTS AND METHODS
2.1. Sample design and sample size estimation
A community‐based cross‐sectional study was carried out by adopting a random sampling procedure. Sample size was calculated using 42% prevalence of stunting among children under age 5 in West Khasi Hills (IIPS, 2014), with 5% precision and 95% confidence interval. A sample size of 564 children was required; therefore, 600 households in the district were targeted for nutritional assessment. Twenty villages were selected by a systematic random sampling procedure from the administrative blocks in the district, and in each village, 30 households with at least one index child under 5 were assessed. Data were collected on pretested and precoded questionnaires by local investigators trained by staff of the National Institute of Nutrition (NIN), Hyderabad.
Information collected from mothers included socio‐economic and demographic circumstances, food security, morbidity, dietary recalls and frequency of consumption of selected foods, immunizations and supplements, prenatal and antenatal care, and infant and young child feeding practices. Anthropometric measurements including length/height (up to nearest 1 mm using height/length board) and weight (up to nearest 100 g using SECA weighing scale) were taken on children (Jelliffee & Jelliffee, 1990). Mid‐Upper Arm Circumference, a measure of malnutrition that uses UNICEF tricolour tapes (UNICEF, 2009), was also used. A 1‐day (24‐hr) recall dietary survey was conducted on all persons in the household for every sixth household (Thimmayamma & Rao, 1969).
2.2. Ethical approval
Ethical clearance was given by the Institutional Ethical Committee of the National Institute of Nutrition, Hyderabad. Community consultation and logistics were provided by NESFAS staff from Shillong. After an explanation of the study, adults provided written informed consent in the local language for themselves and for their children. The disposal of biomedical waste (i.e., blood samples after the analysis, needles, and cotton) was carried out according to biomedical waste (management and handling) rules (Ministry of Environment and Forests, 2000).
2.3. Haemoglobin estimation
Blood samples (20 μl) were collected by finger prick using haemoglobin pipette on filter paper (Whatman® #1), and dry blood spot (DBS) samples were prepared. The blood spots were shade dried and transported to NIN for further analysis. The DBS sample was dissolved in a test tube containing 5 ml of Drabkin's solution for 24 hr and was analysed by indirect cyanomethemoglobin method reported by Sari et al. (2001). The criteria recommended by World Health Organization (WHO; 2001) were used to diagnose anaemia among preschool children, adolescent girls, pregnant women, and lactating mothers. The cut‐off value of less than 11 g/dl of haemoglobin for 1‐ to 5‐year‐old children and pregnant women and less than 12 g/dl for adolescent girls and lactating women was considered anaemic.
2.4. Vitamin A estimation
A free falling drop of blood from a finger prick was collected on a precoded special chromatography filter paper (Whatman® #1) to estimate blood vitamin A in a subsample of children and women covered for anthropometry by the DBS method (Craft et al., 2000). Blood vitamin A levels less than 20 μg/dl was considered as vitamin A deficiency.
2.5. Food insecurity evaluation
The Food and Agriculture Organization of the United Nations (FAO) Voices of the Hungry project developed an international measure called the Food Insecurity Experience Scale. This scale uses a set of eight questions on household food‐related behaviours associated with difficulty in accessing food due to resource constraints in the last 12 months (FAO, 2015) and was administered to households covered by 24‐hr dietary recall.
2.6. Quality control
Random quality checks were conducted by NIN scientists by revisiting households to ensure quality data collection. Databases were developed with range and consistency checks.
2.7. Statistical analyses
Descriptive and statistical analysis was carried out with SPSS® for Windows® version 19.0. Chi‐square tests assessed various dependent and independent variables with statistical significance (p ≤ .05). Food insecurity was assessed with the FAO Voices of the Hungry household measure of Food Insecurity Experience Scale using the Rasch model (FAO, 2015).
3. RESULTS
3.1. Coverage particulars
Six hundred three children 5 years old or younger (boys: 316; girls: 277) from 510 households were covered. Five hundred women and 56 men were covered for various investigations. There were 181 mothers with children less than 12 months of age, and 214 mothers with children 12 to 35 months old, who were interviewed on infant and young child feeding practices, immunizations, and supplements (specifically iron, folate, and vitamin A). Blood pressure was measured in 497 women, and blood sugar in 467 women. Dietary intake data of all individuals in 97 households were collected.
3.1.1. Household socio‐economic and demographic summary
Khasi families were found to be primarily nuclear families with an average family size of five. The literacy rate was 77% among women and 67% among men, with 21% of both having completed intermediate schooling (Grade 12) and above. Christianity was the main religion (95%), and the major occupation was labour (50%) or farming (30%). Women worked within the home 76% of the time. The family per capita monthly income was low (median Rs. 1050 ± 860/U.S.$ 16 ± 13). Houses were made of brick or stone walls with tile or asbestos roofs (61%) or mud walls with tile, asbestos, or thatch roofs (35%), and had at least two rooms (46%), or three or four rooms (41%). Safe drinking water was available in 45% of households, and 93% were still using firewood for cooking purposes. Household electricity was present in 84% of households, sanitary latrines were present in 77%, and separate kitchens in 63%. About 51% of Khasi families had cell phones, and 19.2% had televisions. Rice (45.6%) and sugar (90.5%) were received through the public distribution system (PDS, 2014). Ninety‐two percent of households used iodized salt with an iodine level of 7 ppm.
3.1.2. Food and nutrient intake of women and children
Dietary analyses compiled from the 24‐hr recalls were summarized and compared to the Indian recommended daily intake (RDI; Indian Council of Medical Research, 2012), which is a dietary guideline for intake from each food group (Table 1). Dietary data were differentiated for sedentary or moderately active women who were nonpregnant and nonlactating and those who were pregnant or lactating. Children's data were grouped by those who were 1 to 3 years old, 4 to 6 years old, and 7 to 9 years old. Intake of food groups by women in all categories was reasonably similar. For both women and children, cereals and millets as well as roots and tubers provided the greatest intakes (g/day) with more than 50% of individuals exceeding 70% of the RDI, whereas other vegetables were the next most prominent food group. Consumption of green leafy vegetables, milk, and fat was poor, but some fish and meat consumption was observed. Plain rice was consumed by 95% of adults 2 or 3 times per day, and the major edible oil was mustard seed oil. Due to missing nutrient data for many of the local foods, the calculation of nutrient intake from the dietary analysis of the 24‐hr recalls is only estimated. Nutrient intakes showed that all the nutrients were below the Recommended Dietary Allowances for Indians (NIN, 2010) in all the groups. The intakes of vitamin A, iron, and calcium were far below the Recommended Dietary Allowances (Table 2). It is clear that the intakes of both women and children are below acceptable levels for protein‐rich and micronutrient‐rich foods. It appears that when the intakes were analysed in the three age categories by gender, girls consumed more vegetables and meat than boys (NIN & NESFAS, 2016), but there was no evidence or knowledge of feeding priority by Khasi women for girls over boys.
Table 1.
Average consumption of food groups (g/d) by women and children and % RDIa (NPNL sedentary women and children 1–6 years)
| Cereals/millets | Pulses legumes | Green leafy veg. | Other veg. | Roots/tubers | Nuts/oil seeds | Condi./spices | Fruits | Fish | Other flesh foods | Milk and milk prod. | Fats and oils | Sugar/Jaggery | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sedentary | Mean | 419.3 | 14.1 | 24.5 | 49.6 | 95.6 | 0.1 | 2.8 | 3.1 | 18.7 | 51.6 | 9.5 | 6.8 | 20.7 |
| (n = 47) | SD | 121.6 | 31.0 | 48.9 | 71.9 | 68.3 | 0.4 | 3.0 | 11.9 | 55.0 | 58.4 | 29.2 | 8.1 | 8.7 |
| RDI | 410 | 40 | 100 | 40 | 50 | ‐ | ‐ | ‐ | ‐ | ‐ | 100 | 20 | 35 | |
| %RDI | >70 | 89.4 | 19.1 | 14.9 | 42.6 | 83.0 | ‐ | ‐ | ‐ | ‐ | ‐ | 6.4 | 6.4 | 76.6 |
| 1–3 years | Mean | 225.8 | 7.1 | 20.0 | 34.1 | 57.0 | 0.0 | 1.7 | 2.2 | 11.1 | 18.7 | 7.2 | 4.5 | 22.3 |
| (n = 96) | SD | 94.8 | 17.4 | 33.4 | 49.4 | 41.7 | 0.2 | 2.1 | 10.7 | 34.7 | 30.8 | 25.0 | 6.2 | 56.0 |
| RDI | 175 | 35 | 40 | 20 | 10 | ‐ | ‐ | ‐ | ‐ | ‐ | 300 | 25 | 30 | |
| %RDI | ≥70 | 94.8 | 17.4 | 33.4 | 49.4 | 41.7 | 0.2 | 2.1 | 10.7 | 34.7 | 30.8 | 25.0 | 6.2 | 56.0 |
| 4–6 years | Mean | 257.0 | 6.9 | 17.1 | 36.4 | 67.1 | 0.0 | 1.9 | 1.9 | 6.8 | 26.8 | 5.8 | 3.8 | 23.0 |
| (n = 57) | SD | 99.6 | 15.9 | 29.9 | 55.3 | 45.7 | 0.3 | 1.9 | 6.7 | 18.2 | 44.3 | 23.3 | 5.4 | 37.4 |
| RDI | 270 | 35 | 50 | 30 | 20 | ‐ | ‐ | ‐ | ‐ | ‐ | 250 | 25 | 40 | |
| %RDI | ≥70 | 78.9 | 15.8 | 21.1 | 40.4 | 91.2 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 3.5 | 14.0 |
Note. RDI = recommended dietary intakes; NPNL = nonpregnant nonlactating.
ICMR, 1981.
Table 2.
Average daily intake of nutrients and percent RDA of different age and physiological groups
| Particulars | Protein (g) | Total fat (g) | Energy (kcal) | Calcium (mg) | Phosphorus (mg) | Iron (mg) | Vit. A (μg) | Thiamine (mg) | Riboflavin (mg) | Niacin (mg) | Vit. C (mg) | Dietary folate (μg) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1–3 years | (n = 96) | Median | 26.3 | 7.4 | 1040.3 | 117.7 | 501.7 | 5.1 | 43.0 | 0.4 | 0.2 | 6.6 | 16.6 | 33.8 |
| Mean | 29.8 | 9.5 | 1086.8 | 202.3 | 541.7 | 8.5 | 138.0 | 0.4 | 0.2 | 6.9 | 26.0 | 40.6 | ||
| SD | 16.3 | 8.2 | 424.1 | 266.2 | 268.0 | 8.8 | 199.9 | 0.3 | 0.1 | 3.2 | 32.1 | 26.1 | ||
| RDA | 17 | 27 | 1,060 | 600 | ‐ | 9.0 | 400 | 0.5 | 0.6 | 8.0 | 40 | 80 | ||
| >70% RDA | 93.8 | 11.5 | 79.2 | 8.3 | ‐ | 41.7 | 15.6 | 52.1 | 9.4 | 60.4 | 29.2 | 5.2 | ||
| 4–6 years | (n = 57) | Median | 27.3 | 6.9 | 1,116 | 126.2 | 487.5 | 6.8 | 51.6 | 0.4 | 0.2 | 7.3 | 20.8 | 34.7 |
| Mean | 32.7 | 8.3 | 1,182 | 182.5 | 593.5 | 8.6 | 154.9 | 0.5 | 0.3 | 8.3 | 22.2 | 45.9 | ||
| SD | 19.2 | 7.3 | 423 | 188.4 | 306.1 | 7.8 | 209.7 | 0.3 | 0.2 | 4.4 | 15.2 | 32.8 | ||
| RDA | 20 | 25 | 1,350 | 600 | ‐ | 13.0 | 400 | 0.7 | 0.8 | 11.0 | 40 | 100 | ||
| >70% RDA | 93.0 | 7.0 | 70.2 | 10.5 | ‐ | 35.1 | 19.3 | 40.4 | 7.0 | 45.6 | 24.6 | 1.8 | ||
| NPNL women | (n = 47) | Median | 53.7 | 13.6 | 1,797.9 | 221.0 | 1,018.1 | 11.0 | 61.5 | 0.6 | 0.5 | 12.5 | 25.1 | 56.6 |
| Mean | 59.2 | 15.3 | 1,890.2 | 322.8 | 998.1 | 13.8 | 191.2 | 0.7 | 0.5 | 13.1 | 33.4 | 67.9 | ||
| SD | 29.3 | 10.8 | 438.3 | 385.2 | 339.2 | 10.9 | 279.6 | 0.4 | 0.2 | 3.9 | 31.7 | 35.8 | ||
| RDA | 55.0 | 20.0 | 1,900 | 600 | 21.0 | 600 | 1.0 | 1.1 | 12.0 | 40 | 200 | |||
| >70% RDA | 74.5 | 44.7 | 93.6 | 19.1 | ‐ | 19.1 | 14.9 | 38.3 | 8.5 | 95.7 | 42.6 | ‐ | ||
Note. SD = standard deviation; RDA = recommended dietary allowances, NPNL = nonpregnant nonlactating.
3.1.3. Anthropometry of children and adults
The weight and height growth charts for 595 Khasi children (316 boys, 279 girls) from birth to 5 years are given in Figure 2. The prevalence of low birthweight was 8%. Birthweights were reported as greater than or equal to 2.5 kg for 92% of births in the last 12 months. Data for both weight and height were close to the WHO growth standards (WHO, 2006) in the early months, but growth slows and falls behind the global standard around the third month and continues to decline throughout the measurement period.
Figure 2.
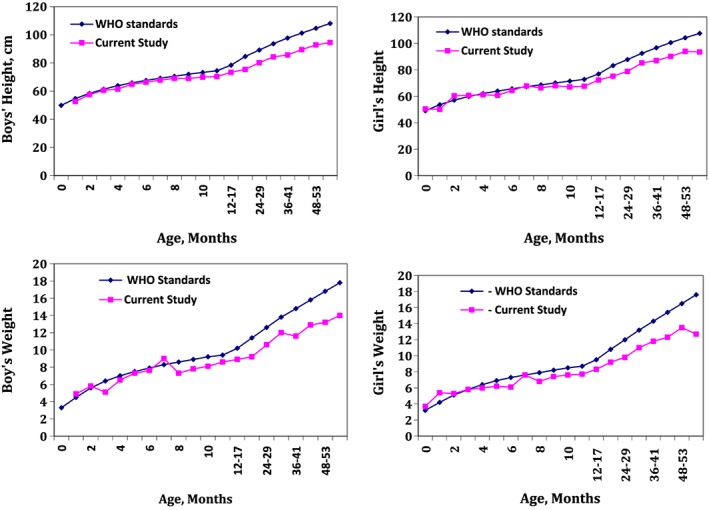
Growth trends of children below 5 years of age n = 595
The prevalence of underweight was 31%, stunting was 56%, and wasting was 10% among Khasi children less than 5 years of age (Figure 3). Underweight was 17%, and stunting was 20% in children less than 12 months of age, which increased to 40% underweight and 77% stunting among 36‐ to 59‐month‐old children. Wasting declines from 15% in the age group under 12 months old to 5% among 36‐ to 59‐month‐old children due to the high rate of stunting. The prevalence of undernutrition was higher among boys than girls. Mid‐Upper Arm Circumference showed that 3% of the children were suffering from severe acute malnutrition; 10% moderate acute malnutrition; 25% were at risk of malnutrition, and 62% were normal (Table 3).
Figure 3.
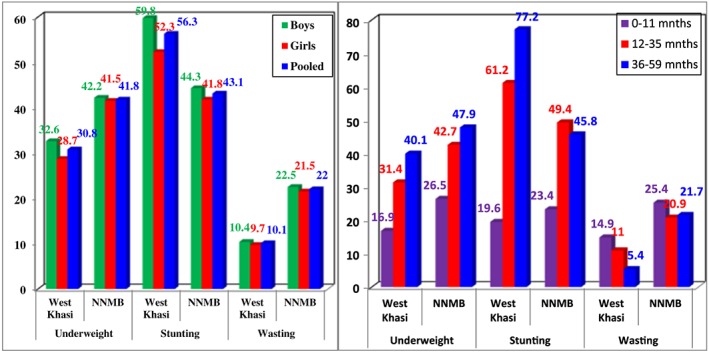
Prevalence (%) of undernutrition among Khasi children <5 years of age, by age groups. Prevalence (%) of undernutrition among Khasi children <5 years of age by gender (n = 595). NNMB = National Nutrition Monitoring Bureau
Table 3.
Distribution (%) of <5‐year‐old children according to MUAC
| MUAC | Khasi (n = 616) | Interpretation |
|---|---|---|
| <11 cm | 2.8 | SAM |
| 11–12.4 cm | 9.9 | MAM |
| 12.5–13.4 cm | 24.8 | At risk |
| ≥ 13.5 cm | 62.5 | Normal |
Note. SAM = severe acute malnutrition; MAM = moderate acute malnutrition; MUAC = Mid‐Upper Arm Circumference.
Clinical examination for nutritional deficiency revealed dental caries being present in 3% of children 12 to 59 months old. Among women, 3% had dental caries and 5% had goitre. Nutritional status among adult women is shown in Figure 4. The prevalence of chronic energy deficiency (body mass index less than 18.5) was 19%, whereas overweight/obesity (body mass index equal to or greater than 25) was observed among 8% women.
Figure 4.
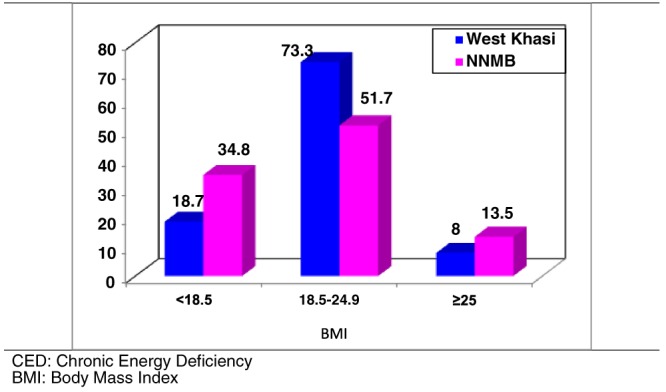
Prevalence (%) of CED and overweight/obesity among adult Khasi women (n = 454) by BMI categories. NNMB = National Nutrition Monitoring Bureau
3.1.4. Prevalence of anaemia, vitamin A deficiency, diabetes, and hypertension
The prevalence of anaemia among 1 to 5‐year‐old children was 68%; pregnant women, 70%; lactating mothers, 86%; and nonpregnant and nonlactating women, 83% (Figure 5). The prevalence of vitamin A deficiency among children and adults is shown in Table 4. Median vitamin A among boys was 20.37 ± 7.8, and that among girls was 19.11 ± 7.08 µg/dl. The prevalence of vitamin A deficiency was 59% among children and was similar in both the genders. The prevalence of vitamin A deficiency was significantly (p < .05) higher among women (47.6%) as compared to men (20%). The prevalence of hypertension was 15%, whereas prevalence of diabetes was 0.7% among adult women (Figure 6).
Figure 5.
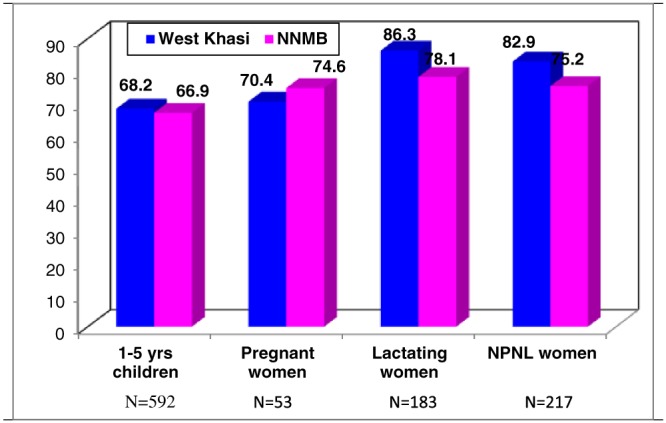
Prevalence of anaemia (%) among different physiological groups. NNMB = National Nutrition Monitoring Bureau; NPNL, nonpregnant and nonlactating
Table 4.
The prevalence of vitamin A deficiency (<20 μg/dl) among Khasi children and adults
| Gender | <20 | ≥20 | Total |
|---|---|---|---|
| 1–5 year children | |||
| Boys | 55 (57.3) | 41 (42.7) | 96 |
| Girls | 61 (60.4) | 40 (39.6) | 101 |
| Total | 116 (58.9) | 81 (41.1) | 197 |
| Adults | |||
| Male | 4 (20.0) | 16 (80.0) | 20 |
| Female | 212 (47.6) | 233 (52.4) | 445 |
| Total | 216 (46.5) | 249 (53.5) | 465 |
Figure 6.
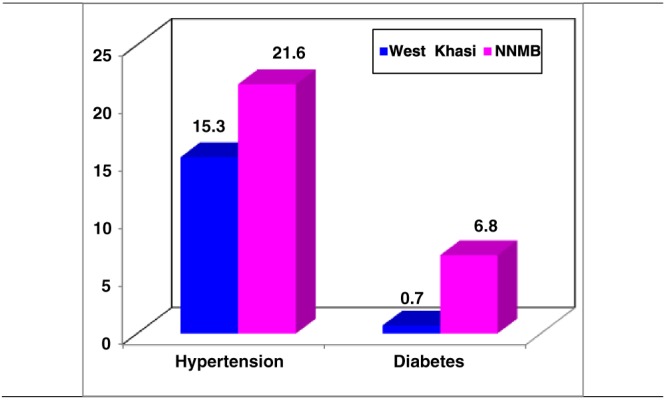
Prevalence (%) of hypertension (n = 497) and diabetes (n = 461) among adult Khasi women. NNMB = National Nutrition Monitoring Bureau
3.1.5. Infant and young child feeding practices.
Most Khasi mothers initiated breastfeeding within 3 hours of birth, regarding colostrum as important for the newborn. Only 15% gave a prelacteal feed such as plain or glucose water. Interviews with mothers revealed that 72% fed only breast milk up to 6 months. Complementary foods were given to 77% of 6‐ to 11‐month‐old infants during this period. Of those receiving complementary feeding, 30% received complementary food before 6 months, and the rest received it at 6 months. The common complementary foods were home‐made cereal‐based semisolids or solids, formula, commercial baby foods, and cow/buffalo milk. The percentage of home‐made complementary foods varied from 65% to 95%, and commercial baby food was recorded at about 16%. Complementary foods before 1 year of age from the household food supply included cereals and millets, pulses, milk products, sugar, vegetables, eggs, roots and tubers, and meat. Most of the mothers reported breastfeeding at least 8 times per day for young infants and continued breastfeeding up to about 2 years. Feeding frequency of at least 4 times per day was observed in 70% of children. More than 80% of children 12 to 24 months were fully immunized, and children 12 to 59 months received at least one dose of vitamin A. About 69% of Khasi children (12 to 59 months) had learned to wash their hands with soap before eating.
3.1.6. Maternal knowledge about feeding during pregnancy
More than 90% of mothers stated that extra food is needed in pregnancy. Despite this, about 57% stated it was difficult to get extra food, but 35% stated that it was not difficult to get more and better food during pregnancy. Regardless, dietary data demonstrated that women and young children had very low intakes and wide variability in the amount (g/day) of iron‐dense foods such as meat (women: 52 to 58 g/day; children 1 to 3 years: 11 to 34 g/day; children 4 to 6 years: 27 to 44 g/day) and pulses/legumes (women: 25 to 49 g/day; children 1 to 3 years: 7 to 17 g/day; children 4 to 6 years: 7 to 15 g/day). The intake of iron‐containing foods was low for pregnant women at 40 to 70 g/day of meat and 9 to 30 g/day of pulses/legumes. Cereals/millets were consumed at or above the RDI by more than 75% of women and children, but micronutrient‐rich green leafy vegetables, meats, and milk were below RDI. Overall, dietary diversity appears to be low, with most of the dietary energy derived from cereals.
3.1.7. Household food insecurity evaluation
Households were classified into different grades of food insecurity per the FAO food insecurity scale (Figure 7). Among the Khasi population, only 19% of households were food secure, whereas 63% were moderately food insecure, and 4% were severely food insecure. The association between food security as a dependent variable and socio‐economic and nutritional status as independent variables is presented in Table 5. The prevalence of chronic energy deficiency was low among those identified as food secure, and the simultaneous prevalence of overweight/obesity was higher among them. The prevalence of food insecurity was higher among the illiterate, those with low per capita income, and those with a family size of nine or more members. However, more than 63% of families of all sizes experienced moderate food insecurity. Similar prevalence distributions of raw scores were also obtained with Rasch model scores, which established reliability and validity of the data (Figure 7).
Figure 7.
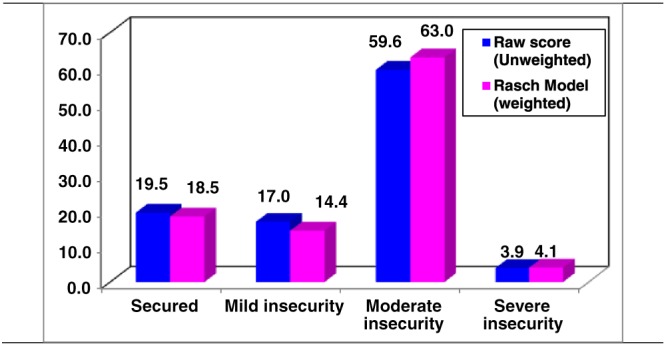
Distribution (%) of food insecurity among Khasi households (n = 472)
Table 5.
Associations between food insecurity with women's BMI and socio‐demographic variables (%)
| Nutritional status | ||||
|---|---|---|---|---|
| Food insecurity | n HH | CED | Normal | Overweight |
| Secured | 83 | 9.6 | 81.9 | 8.4 |
| Mild insecurity | 63 | 28.6 | 66.7 | 4.8 |
| Mod. insecurity | 326 | 10.4 | 86.8 | 2.8 |
| P value | .001 | |||
| Food insecurity | ||||
| Literacy status | Secured | Mild insecurity | Mod. Insecurity | |
| Illiterate | 98 | 9.2 | 6.1 | 84.7 |
| 1st–8th class | 264 | 24.2 | 13.6 | 62.1 |
| 9th and above | 138 | 13.8 | 22.5 | 63.8 |
| P value | .001 | |||
| Per capita income | ||||
| 1st quartile | 137 | 2.9 | 10.9 | 86.1 |
| 2nd quartile | 108 | 11.1 | 21.3 | 67.6 |
| 3rd quartile | 98 | 20.4 | 10.2 | 69.4 |
| 4th quartile | 157 | 35.7 | 15.9 | 48.4 |
| P value | .001 | |||
| Family size | ||||
| 1–4 | 288 | 21.5 | 10.4 | 68.1 |
| 5–8 | 163 | 14.7 | 22.1 | 63.2 |
| ≥9 | 50 | 12.0 | 14.0 | 74.0 |
| P value | .001 | |||
Note. CED = chronic energy deficiency; BMI = body mass index; HH= household.
3.1.8. Food system biodiversity
The current use of food biodiversity was evaluated among 160 households in 15 villages. Focus group discussion (FGD) with community members revealed a wealth of knowledge of food species in the local Khasi food system. In research with Indigenous Peoples' food systems globally, the range of species/varieties reported was 35–387 (Kuhnlein, 2009). Through FGD with the Khasi, the villages reported 372 species of food used during the 2015 assessment period (Table 6). More of these were wild species (225) than were cultivated (147). It is important to note that scientific identifications have not been established for more than two thirds of these food species. The study revealed that several traditional rice landraces are still used by the Khasi; the most common ones being kba bakut, kba sawtdong, and kba bhoi. Yet all the households surveyed were consuming rice obtained from the PDS. Sticky rice (Oryza glutinosa) was used infrequently mainly for snacks. The use of Job's tears (Coix lacryma) and millets is low, with only 3% of the households consuming them intermittently. As many as 13 potato varieties were reportedly grown and consumed by the Khasi, which reveals rich agrobiodiversity. One tuber endemic to the Khasi area is sohphlang (Flemingia vestita), which is normally consumed with the traditional oilseed nei lieh (Perilla frutescens). Such food combinations complement each other and improve nutritional qualities. Small quantities of sweet potato and tapioca are consumed frequently. Thirty‐one wild green leafy vegetables were reported to be edible, but only 10 varieties were consumed by more than 50% of the households once or twice a week, and the others were restricted to a few households. The green vegetable known as jalynniar is not identified scientifically but is collected by 15 villages several times in the month of April and is consumed in approximately 100‐g portions. The consumption of Indigenous vegetables appears to be low, whereas commercially available pulses, such as masoor dal (Lens culinaris), imported from the mainland are consumed by all households. As many as 52 wild fruits and berries were recorded in the Khasi food system, but the actual consumption was limited to only five varieties. The fruit known as sohshang (Eleagnus caudate) is consumed in 16 villages from February to April. All 42 mushrooms recorded were collected from the wild, but the most popular were tit syiar (Clavvulina sp) and tit tyndong (Gomphus floccus), which were consumed once a week during the season by all the households. Small fresh water fish, snails, crabs, small game animals, and insects appear to contribute to dietary protein intake. Chewing kwai (fresh Areca catechu nut in Piper betel leaves with slaked lime/calcium hydroxide) is a common practice among the Khasi, with 81% of women reporting betel use, 27% having it more than 10 times per day and 57% fewer than 10 times. Villagers were able to roughly estimate the amount of each food consumed by one adult in a meal per day and the number of times each food was collected/harvested in the previous year. It is clear that there is a wealth of information on food resources available within the environment and used in the Khasi traditional diet. Another study among the Mizos in Mizoram state listed 279 wild plant foods used as food, of which 35 species are commonly sold in the market, which speaks of the dietary preference for wild edible plants (Kar, Bora, Borthakur, Goswami, & Saharia, 2013). Medhi, Sarma, and Borthakur (2014) also recorded 168 wild plant foods used by the Indigenous People in Dima Hasao district of Assam state. However, though many wild edible plants may be common, there will be many plant foods that are unique to a tribe according to their location and environment.
Table 6.
Khasi food system list by food groups, cultivated or wild, villages using, and number without scientific identification
| Food group | Total # of species | # cultivated | # wild | # with no ID | # of villages using each species/17 |
|---|---|---|---|---|---|
| Rice | 21 | 21 | ‐ | ‐ | 4–17 |
| Maize | 6 | 6 | ‐ | ‐ | 9–17 |
| Millet | 5 | 5 | ‐ | ‐ | 6–14 |
| Pulses/legumes | 13 | 11 | 2 | ‐ | 7–17 |
| Potato | 24 | 22 | 2 | 1 | 7–17 |
| Green leafy veg | 45 | 14 | 31 | 13 | 4–17 |
| Other veg | 19 | 15 | 4 | 6 | 8–17 |
| Fruit/berries | 77 | 24 | 53 | 48 | 6–17 |
| Nuts/oilseeds | 5 | 5 | ‐ | ‐ | 6 |
| Mushrooms | 42 | ‐ | 42 | 34 | 6–17 |
| Spices/condiments | 11 | 9 | 2 | 8 | 12–17 |
| Meat/poultry | 5 | 5 | ‐ | ‐ | 17 |
| Fish/shellfish | 18 | 9 | 9 | 18 | 9–16 |
| Game | 55 | ‐ | 55 | 55 | 6–16 |
| Insects | 26 | 1 | 25 | 26 | 6–13 |
| Total | 372 | 147 | 225 | 209 | N/A |
4. DISCUSSION
The extent of child undernutrition and micronutrient deficiencies among the Khasi is distressing given the paradox of such a wealth of both cultivated and wild food resources available in the district. The dietary intakes obtained from 24‐hr recall do not capture many foods recorded through FGD, such as insects, mushrooms, and small game animals that are good sources of protein. As well, the lack of nutrient composition for most of the foods collected from the wild makes nutrient intake interpretation difficult.
Overall stunting among children less than 5 years of age was 56%, slightly higher than 51% reported by IIPS (2014) in West Khasi Hills district. Stunting among rural Indian children less than 5 years of age is 46% (National Nutrition Monitoring Bureau [NNMB], 2012). Prevalence of underweight in the present study was exactly similar to National Family Health Survey 2015–2016 (NFHS‐4) at 31% for West Khasi Hills but lower than the national average of 42% reported by NNMB (2012). Wasting was 10%, reflecting an acute situation related to lack of food and/or illness. Growth faltering that occurred at an early stage of life could be due to suboptimal young child feeding practices such as delayed or early initiation of complementary feeding, and frequency and quality of breast milk and/or complementary foods. The infant is totally dependent on the mother's diet and body reserves in the first 6 months of life. The knowledge of women on the importance of eating well during pregnancy and for child feeding and their capacity to implement their priorities in a matrilineal and matrilocal society should prevent poor growth of children caused by child undernutrition; however, this was not the case. Other research on the current role of women in Khasi society may help to shed light on this paradox.
It appears that catch‐up growth could not be achieved due to resource poor settings where dietary intake may be consistently inadequate due to low income and high rate of food insecurity. The unacceptably high levels of child undernutrition reflect long‐term nutritional inadequacy. Acute malnutrition is also observed by Mid‐Upper Arm Circumference measure with 13% of children in the severe or moderate categories. According to ethnographic accounts of the mid 1800s, Khasi adults were athletic, well nourished, and short in stature, with males being extremely muscular and women buxom (Gurdon, 1863). Whether genetic make‐up has any influence over the short stature that can be attributed to the high rate of stunting among Khasi children needs further in‐depth study.
Widespread anaemia was noticed among all ages of children and adults. The prevalence is similar to figures reported by NNMB (2003) among rural Indian populations. Anaemia is a well‐known health occurrence in developing countries and has a multifaceted aetiology wherever it occurs. The measurement of haemoglobin as an indicator of iron deficiency anaemia is commonly conducted. Given the poor intake of iron‐rich food groups among both women and children, it is not surprising there is extensive anaemia, but underlying causes include more than nutritional iron intake. They include infection such as Helicobacter pylori and parasitosis; various nutrient deficiencies, including vitamin A, vitamin C, zinc, copper, folate, vitamin E, vitamin B6, vitamin B12, riboflavin, thiamin, and niacin; and ingesting insufficient essential amino acids and fatty acids for erythropoiesis (Jamieson & Kuhnlein, 2008; Jamieson, Kuhnlein, Weiler, & Egeland, 2013).
Considering the low intake of all types of vegetables, it appears that most of the agricultural produce is going to the market instead of being consumed. Greater knowledge of the healthful properties of agrobiodiversity and educational activities at the community level can foster more farming households to better harvest and process for family consumption. Krishi Vigyan Kendra (an agricultural education programme funded by the Indian Council of Agricultural Research) can help bring about such educational activities. Widespread consumption of kwai is expected to add to the vitamin A intake, as betel leaves are known to contain as much as 4500 μg/100 g beta carotene. It will also add to the calcium intake as it contains calcium hydroxide; however, further scientific studies are required to ascertain its accessibility and bioavailability. Subclinical vitamin A deficiency was observed to be very high among the population although no clinical sign of vitamin A deficiency was observed. This may be because of low intake of green leafy vegetables and meat among the population. Although the production and availability of green leafy vegetables, including wild greens, is quite good, the low purchasing capacity and lack of awareness among rural population could be adding to the burden of micronutrient deficiencies.
Intensive agriculture is practiced in about 37% of West Khasi Hills district. Agriculture intensification not only poses serious threats to biodiversity but also exerts negative effects on the food system and health of the Indigenous population. The household food list is remarkable in its breadth and character of diversity in all categories of food groups, but the use of wild food resources is still low as a part of the Khasi diet. Local wild foods contribute to dietary diversity and resilience of the ecosystem. The identification of species needs to be ongoing with local scientific experts, and the nutrient composition of the species must take place in respected laboratories. The robustness of scientific evidence between biodiversity and health can be strengthened if composition data of wild food resources are documented. Using this local food biodiversity to greater advantage will strengthen household food security as well as cultural morale and health and give the communities an opportunity to contribute to the sustainability of their ecosystem. In order for this to happen, the importance of wild food resources to improve food and nutrient security needs more attention from policymakers.
More health and nutrition education to pregnant and lactating mothers needs to be given to communities. Education, together with behaviour change communication, should focus on better food intake during pregnancy and lactation, infant and young child feeding practices (particularly for initiation of breastfeeding and complementary feeding at 6 months and later), and the availability of highly nutritious foods in the local food system. The national Integrated Child Development Services and PDS need to be strengthened so that food supplementation can include local food resources to prevent household food insecurity. Nutrition education and awareness about child growth needs and prevention of chronic diseases such as hypertension, obesity, and diabetes also can be strengthened.
With special attention to the education of women in this unique Khasi society, it can become a global model of how food and nutrition development can take place to reduce childhood stunting, wasting, and overall undernutrition. At the same time, this can prevent the population slide towards overweight and obesity that unfortunately is overcoming the rest of India and other developing countries with the advent of greater economic development.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
DC and RA contributed to The field work and biodiversity assessments, IIM was the field coordinator, KV was statistical consultant, and GN was responsible for dietary and nutritional assessments. PR was overall funding coordinator and leader of the NESFAS team. HVK contributed to the study design and the manuscript drafts, and TL was the overall director of the research. All authors reviewed the manuscript drafts.
PHOTOGRAPHIC SECTION
See Photographic section – Khasi
ACKNOWLEDGMENTS
We express our sincere thanks to The Indigenous Partnership for Agrobiodiversity and Food Sovereignty, Tebtebba, and North East Slow Food and Agrobiodiversity Society (NESFAS) for funding support and cooperation during the study. Our earnest thanks to the entire project staff for their commitment and sincere efforts in completing data collection. We are extremely grateful to the Khasi community, especially mothers of young children, for their unstinting cooperation. Without their participation, the study would not have been completed successfully.
Biography
Thingnganing Longvah is Director of the National Institute of Nutrition (NIN) in Hyderabad, India. After completing his PhD studies in Biochemistry from the North‐Eastern Hill University in Shillong, India, he joined the NIN. He started his career working on the indigenous foods consumed by various tribes of Northeast India. His areas of interest include food biodiversity, indigenous food systems, micronutrients, non‐communicable diseases, and food composition. He has been a Senior Scientist for many years at NIN. Longvah hails from the Tangkhul tribe, one of the indigenous groups in Northeast India. He co‐chairs the Task Force on Traditional, Indigenous, and Cultural Food and Nutrition of the International Union of Nutritional Sciences (IUNS). He is also active in the INFOODS network of IUNS. He is the regional coordinator for SAARCFOODS, and he has recently published the “Indian Food Composition Tables 2017,” with his team. Research with Khasi tribal communities in Meghalaya was carried out with an experienced team of scientists from the NIN, including Daniella Chyne, who is of Khasi heritage.
Chyne DAL, Meshram II, Rajendran A, et al. Nutritional status, food insecurity, and biodiversity among the Khasi in Meghalaya, North‐East India. Matern Child Nutr. 2017;13(S3):e12557 10.1111/mcn.12557
REFERENCES
- Agrahar‐Murugkar, D. (2005). Nutritional status of Khasi school girls in Meghalaya. Nutrition, 21, 425–431. [DOI] [PubMed] [Google Scholar]
- Agrahar‐Murugkar, D. , & Pal, P. P. (2004). Intake of nutrients and food sources of nutrients among the Khasi tribal women of India. Nutrition, 20, 268–273. [DOI] [PubMed] [Google Scholar]
- Census of India (2011). New Delhi: Office of the Registrar General of India and Census Commissioner, India.
- Craft, N. E. , Haitema, T. , Brindle, L. K. , Yamini, S. , Humphrey, J. H. , & West, K. P. (2000). Retinol analysis in dried blood spots by HPLC. The Journal of Nutrition, 130, 882–885. [DOI] [PubMed] [Google Scholar]
- Expert Group of ICMR. (1981). Recommended Dietary Intakes for Indians. New Delhi: Indian Council of Medical Research.
- Food and Agricultural Organization (2015). Voices of the hungry, food insecurity experience scale. Rome: Food and Agriculture Organization of the United Nations. [Google Scholar]
- Gurdon, P. R. T. (1863). The Khasis. New Delhi: Akansha Publishing House. (Reprinted 2010) [Google Scholar]
- Indian Council of Medical Research (2012). Recommended dietary intakes (RDI) for Indians. Hyderabad, India: National Institute of Nutrition. [Google Scholar]
- International Institute for Population Sciences (2014). District Level Household and Facility Survey (DLHS‐4), 2012–13: India. Meghalaya: Mumbai. [Google Scholar]
- Jamieson, J. A. , & Kuhnlein, H. V. (2008). The paradox of anemia with high meat intake: A review of the multifactorial etiology of anemia in the Inuit of North America. Nutrition Reviews, 66, 256–271. [DOI] [PubMed] [Google Scholar]
- Jamieson, J. A. , Kuhnlein, H. V. , Weiler, H. A. , & Egeland, G. M. (2013). Higher n3‐fatty acid status is associated with lower risk of iron depletion among food insecure Canadian Inuit women. BMC Public Health, 13, 289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jelliffee, D. B. , & Jelliffee, E. P. (1990). Community nutritional assessment. Oxford: Oxford University Press. [Google Scholar]
- Kar, A. , Bora, D. , Borthakur, S. K. , Goswami, N. K. , & Saharia, D. (2013). Wild edible plant resources used by the Mizos of Mizoram, India. Kathmandu University journal of Science, Engineering and Technology, 9(1), 106–126. [Google Scholar]
- Khan, M. L. , Khumbongmayum, A. D. , & Tripathi, R. S. (2008). The sacred groves and their significance in conserving biodiversity: An overview. International Journal of Ecology and Environmental Sciences, 34, 277–291. [Google Scholar]
- Kuhnlein, H. V. (2009). Introduction: Why are indigenous peoples' food systems important and why do they need documentation? In Kuhnlein H. V., Erasmus B., & Spigelski D. (Eds.), Indigenous peoples' food systems: The many dimensions of culture, diversity and environment for nutrition and health (pp. 1–7). Rome: United Nations Food and Agriculture Organization. [Google Scholar]
- Lyngdoh, A. Q. , & Nongknrih, A. K. (2015). Mother's brother in matrilineal societies: A study of Khasi matriliny. The NEHU Journal, 1, 33–46. [Google Scholar]
- Medhi, P. , Sarma, A. , & Borthakur, S. K. (2014). Wild edible plants from Dima Hasao district of Assam, India. Pleione, 8(1), 133–148. [Google Scholar]
- Ministry of Environment and Forests (2000). Biomedical waste (management and handling) rules 1998, Ministry of Environment and Forests. New Delhi: Government of India. [Google Scholar]
- Mittermeier, R. A. , Turner, W. R. , Larsen, F. W. , Brooks, T. M. , & Gascon, C. (2011). Global biodiversity conservation: The critical role of hotspots In Biodiversity hotspots (pp. 3–22)Springer Berlin Heidelberg. [Google Scholar]
- National Institute of Nutrition (2010). Nutrient requirements and recommended dietary allowances for Indians. Hyderabad, India: National Institute of Nutrition, ICMR. [Google Scholar]
- National Institute of Nutrition and Northeast Slow Food and Agrobiodiversity Society (2016). Food biodiversity and nutritional studies among the Khasis in West Khasi Hills district, Meghalaya. Report No 1. Hyderabad, India: National Institute of Nutrition, ICMR. [Google Scholar]
- National Nutrition Monitoring Bureau (2003). Prevalence of micronutrient deficiencies. Report no. 22. Hyderabad, India: National Institute of Nutrition, Indian Council of Medical Research. [Google Scholar]
- National Nutrition Monitoring Bureau (2012). Diet and nutritional status of rural population, prevalence of hypertension and diabetes among adults and infant and young child feeding practices. Technical report No. 26. Hyderabad, India: National Institute of Nutrition (ICMR). [Google Scholar]
- Public Distribution System (2014). Public distribution system and food security. Planning Commission of India. Chapter 8, http://planningcommission.gov.in/plans/mta/mta-9702/mta-ch8.pdf.
- Sari, M. , Pee, S. D. , Martini, E. , Herman, S. , Sugiatmi, Bloem, M. W. , & Yip, R. (2001). Estimating the prevalence of anemia: A comparison of three methods. Bulletin of the World Health Organization, 79, 506–511. [PMC free article] [PubMed] [Google Scholar]
- Thimmayamma, B. V. S. , & Rao, D. H. (1969). A comparative study of the oral questionnaire method with actual observation of the dietary intake of pre‐school children. Indian Journal of Nutrition and Dietetics, 6, 177–181. [Google Scholar]
- The United Nations Children's Fund. (2009). Mid‐Upper Arm Circumference Meas. Tapes. Tech. Bull. No.13, Revision. 2. Retrieved from https://supply.unicef.org/unicef_b2c/mimes/catalog/images/Mid_Upper_Arm_Circumference_Measuring_Tapes.pdf
- World Health Organization (2001). Iron deficiency anaemia: Assessment, prevention, and control: A guide for programme managers. Geneva: World Health Organization. [Google Scholar]
- World Health Organization (2006). Length/height‐for‐age, weight‐for‐age, weight‐for‐length, weight‐for‐height and body mass index‐for‐age: Methods and development.
- Xaxa Committee (2014). Report of the high‐level committee on socio‐economic health and educational status of the tribals of India. New Delhi: Ministry of Tribal Affairs, Government of India. [Google Scholar]


