Abstract
Adequate support for lactating mothers is crucial to improve the rates of early initiation, exclusive, and continued breastfeeding. Maternal breastfeeding intention and ongoing breastfeeding duration are strongly predicted by their partners' breastfeeding beliefs. Partner support has a significant effect on improving rates of any and exclusive breastfeeding, when compared with professional support, particularly in low‐income populations. This systematic review investigates the effectiveness of breastfeeding interventions targeting fathers in low‐ and middle‐income countries (LMIC). A systematic literature search was undertaken on Medline (EBSCOhost), PsycInfo, CINAHL, and Scopus databases and via manual searching. Inclusion criteria were experimental or quasiexperimental designs targeting fathers from LMIC, which measured either breastfeeding initiation, breastfeeding exclusivity, or duration of breastfeeding as the main outcomes. No time restriction was put in place, and all articles were published in English. The quality of selected papers was assessed using the Joanna Briggs Institute tool. A total of 8 articles were included from 6 interventions: 2 quasiexperimental and 4 randomized control trials. All interventions involved breastfeeding education targeting fathers; 2 were given only to fathers, and 4 delivered to both fathers and mothers. Among these interventions, 2 measured both early initiation and exclusive breastfeeding; one exclusive breastfeeding only; one exclusive breastfeeding, knowledge, and attitudes; one exclusive breastfeeding and knowledge; and one breastfeeding, continued breastfeeding, and awareness. Across all interventions, breastfeeding education showed significant improvement in breastfeeding outcomes in the intervention compared with the control groups. In summary, breastfeeding education interventions targeting fathers in LMIC are effective in improving early initiation of breastfeeding, exclusive breastfeeding, and continued breastfeeding. Thus, breastfeeding promotion should consider the education and involvement of fathers in the intervention.
Keywords: breastfeeding, education, father, intervention, low‐ and middle‐income countries, systematic review
1. INTRODUCTION
Breastfeeding is the optimal way of providing the required nutrients for infants for healthy growth and development (WHO, 2001). The World Health Organization (WHO) recommends breastfeeding initiation within the first hour after birth and continued exclusive breastfeeding for 6 months. At around 6 months of age, complementary foods should be introduced with continued breastfeeding to 2 years (WHO, 2001, 2009). There are multiple benefits conferred by breastfeeding that are dose dependent; children who are breastfed for longer have lower risk of morbidity and mortality primarily from infectious diseases, fewer dental malocclusions, and improved intelligence when compared with children with shorter duration of breastfeeding (Victora et al., 2016). Longer duration of breastfeeding also protects against non‐communicable diseases such as overweight and diabetes in adolescence (Victora et al., 2016). Despite the documented benefits of breastfeeding, only 36% of infants globally are exclusively breastfed for the first 6 months (WHO, 2014). This indicates that a majority of infants remain nonexclusively breastfed and are therefore at higher risk of morbidity and mortality predominantly due to gastrointestinal and respiratory infections (Kramer & Kakuma, 2004).
According to WHO, adequate social and nutritional support to lactating mothers is crucial to improve breastfeeding outcomes (WHO, 2001). Women who get any forms of extra support are more likely to continue breastfeeding. Support from professionals or nonprofessionals (lay/peer support) has significant positive effects on breastfeeding practices of mothers (Renfrew, McCormick, Wade, Quinn, & Dowswell, 2012; Sikorski, Renfrew, Pindoria, & Wade, 2003). The effectiveness of support for breastfeeding depends on who delivers the support. Findings from a meta‐analysis indicated that partner/lay support significantly correlated with duration of breastfeeding compared with professional support (Dennis, 2002). Similarly, systematic reviews reveal the effectiveness of lay support to prevent the cessation of exclusive breastfeeding compared with professional support at 6 months (McFadden, et al., 2017; Renfrew et al., 2012).
Although the mother of the infant has primary responsibility for infant feeding, family members particularly fathers and grandmothers have significant influence (Thuita, Martin, Ndegwa, Bingham, & Mukuria, 2015; USAID, 2011). Fathers have an important supportive role by providing food, financial, and resources, which are critical for the health of the mother and child (Thuita et al., 2015; USAID, 2011). In addition to financial support, fathers can use their breastfeeding knowledge to motivate and assist their partners to breastfeed, and they can help them with child care and housework (Rempel & Rempel, 2011). Two systematic reviews have been conducted on breastfeeding interventions targeting fathers predominantly from high‐income countries (Bar‐Yam & Darby, 1997; Mitchell‐Box & Braun, 2013). These reviews reveal that breastfeeding interventions targeting fathers or partners have a significant effect on breastfeeding outcomes including initiation, exclusivity, and duration. In addition, findings from other research show that fathers' beliefs on whether their partners should breastfeed strongly predict the level of maternal intention to breastfeed (Scott, Landers, Hughes, & Binns, 2001). Mothers who perceive that their partners prefer breastfeeding are less likely to cease breastfeeding at any time, compared with those who perceive that their partner prefers bottle feeding or are ambivalent about how their child is fed (Scott et al., 2001). Maternal intention to breastfeed is a significant factor influencing breastfeeding practice. Maternal breastfeeding intention is strongly predicted by their partners' breastfeeding beliefs more than their own reasons for breastfeeding and previous breastfeeding behaviour (Rempel & Rempel, 2004). On the other hand, although men know the benefits of breastfeeding, they are not directly involved in decisions related to breastfeeding, and they may believe formula feeding is more convenient than breastfeeding (Avery & Magnus, 2011; Henderson, McMillan, Green, & Renfrew, 2011; Mitchell‐Box & Braun, 2012). Fathers' attitudes and beliefs towards exclusive breastfeeding can be improved through educational interventions. Breastfeeding interventions targeting fathers improve knowledge and attitudes towards breastfeeding initiation and exclusivity, and therefore ultimately breastfeeding outcomes (Abbass‐Dick, Stern, Nelson, Watson, & Dennis, 2014; Bich & Cuong, 2017; Maycock et al., 2013; Pisacane, Continisio, Aldinucci, D'Amora, & Continisio, 2005).
There is a growing body of literature regarding the involvement of fathers in providing breastfeeding support. Previous systematic reviews however have focused on high‐income countries (Bar‐Yam & Darby, 1997; Mitchell‐Box & Braun, 2013), but the role of fathers in infant and young child feeding has not been reviewed in low‐ and middle‐income countries (LMIC). There may be significant differences between high income and LMICs with respect to the role of fathers. In LMIC, the roles of men and women are distinctly different; culturally, men tend to be responsible for providing financial support for food, clothes, and health care. In addition, unlike fathers from high‐income countries, fathers from LMIC rarely accompany their partners to antenatal or postnatal appointments (Thuita et al., 2015). Without receiving adequate information about breastfeeding during the antenatal and postnatal periods (Maycock et al., 2013), their participation and involvement in early infant feeding could also be different. To our knowledge, there is no review of breastfeeding interventions delivered to fathers'/partners' in LMIC. Thus, the aim of this systematic review is to analyse the existing knowledge and summarize the effectiveness of breastfeeding interventions focusing on fathers/partners towards early initiation, exclusivity, and duration of breastfeeding in low‐ to middle‐income countries.
2. METHODS
2.1. Source of information
The systematic literature search was undertaken in February 2017, using Medline (EBSCOhost), PsycInfo, CINAHL, and Scopus bibliographic databases and supplemented with manual searching of the reference lists of retrieved articles. See Box Key messages for the search terms and combinations.
Key messages.
Partners' support has a significant effect on maternal breastfeeding intention, initiation, exclusivity, and duration.
Breastfeeding interventions targeting fathers in LMIC increase the level of early breastfeeding initiation, exclusive breastfeeding, and continued breastfeeding.
Breastfeeding interventions focusing on fathers from LMIC are limited
More research is required to investigate the effectiveness of fathers' involvement in breastfeeding education on breastfeeding outcomes, especially in low‐income countries.
2.2. Eligibility criteria
Inclusion criteria were experimental or quasiexperimental designs targeting fathers from LMIC, which measured either breastfeeding initiation, breastfeeding exclusivity, or duration of breastfeeding as the main outcomes. No time restriction was put in place, and all articles were published in English. Low‐ and middle‐income countries were defined using the World Bank classification of countries based on their gross national income per capita. Breastfeeding interventions targeting fathers/partners, or fathers/partners and mothers, or fathers/partners and any other support group were also targeted.
2.3. Study selection
The search results were exported to Endnote X7 where duplicates were removed. After duplicates were removed, titles and abstracts were reviewed simultaneously. Full‐text assessment was conducted by K. T. and D. G. using the inclusion and exclusion criteria.
2.4. Data extraction and quality assessment
Data, including the publication characteristics, study characteristics, participant characteristics, and study variables and outcomes, were extracted into Excel.
The quality of selected papers was assessed independently by K. G. and D. G. using the Joanna Briggs Institute (JBI) tool for assessing quality of randomized controlled trials, and quasiexperimental studies prior to inclusion in the review. The JBI assessment tool comprises 10‐item and 9‐item checklists for RCTs and quasiexperimental designs, respectively, and it is one of the commonly used tools (The Joanna Briggs Institute, 2017). Disagreements on selection of articles and result of quality assessment were discussed by K. T. and D. G., and decisions were made based on discussion and consensus. Data were synthesized using a narrative method and does not include meta‐analysis due to the heterogeneity of the studies.
Box 1. Search terms
TI ((Breastfeeding OR “infant feeding” OR prenatal OR postnatal OR antenatal) AND (education* OR promotion* OR support* OR program* OR message* OR psychosocial*) AND (father* OR partner* OR parental OR husband OR male OR Spouses) AND (“low income countr*” OR “middle income countr*” OR “developing countr*” OR “low and middle income countr*” OR “low to middle income countr*” OR LMIC*)) OR AB ((Breastfeeding OR “infant feeding” OR prenatal OR postnatal OR antenatal) AND (education* OR promotion* OR support* OR program* OR message* OR psychosocial*) AND (father* OR partner* OR parental OR husband OR male OR Spouses) AND (“low income countr*” OR “middle income countr*” OR “developing countr*” OR “low and middle income countr*” OR “low to middle income countr*” OR LMIC*)) TI: Title, AB: Abstract, LMIC: low and middle income countries.
3. RESULTS
A total of 1,574 articles were found from the databases and additional searching. Out of these, 425 duplicates were removed using Endnote software. Figure 1 illustrates the total number of articles found and the subsequent exclusions.
Figure 1.
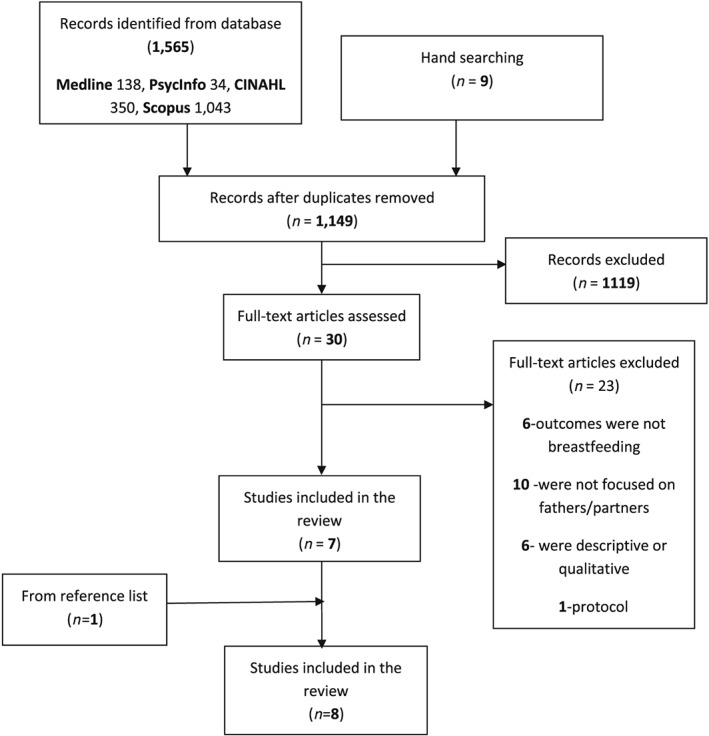
Systematic selection of studies on effectiveness of breastfeeding intervention in low‐ and middle‐income countries focusing on fathers
A total of eight articles are included in this review from six interventions; of these, two were quasiexperimental (Bich et al., 2016; Bich, Hoa, & Målqvist, 2014; Su & Ouyang, 2016) and four were randomized control trials (Özlüses & Çelebioglu, 2014; Raeisi, Shariat, Nayeri, Raji, & Dalili, 2014; Sahip & Turan, 2007; Susin et al., 1999; Susin & Giugliani, 2008). The details of these articles are presented in Table 1. Two articles were from one intervention from Viet Nam (Bich et al., 2014; Bich et al., 2016), two articles from Turkey (Özlüses & Çelebioglu, 2014; Sahip & Turan, 2007), one from Iran (Raeisi et al., 2014), two articles from one intervention from Brazil (Susin et al., 1999; Susin & Giugliani, 2008), and one from China (Su & Ouyang, 2016). Among the six interventions, four interventions were implemented in a hospital setting (Özlüses & Çelebioglu, 2014; Sahip & Turan, 2007; Su & Ouyang, 2016; Susin et al., 1999; Susin & Giugliani, 2008), one in a health facility plus home visit (Bich et al., 2014; Bich et al., 2016), and one in a research centre (Raeisi et al., 2014). Three of the interventions were provided to fathers only (Bich et al., 2014; Bich et al., 2016; Sahip & Turan, 2007), the other three were to fathers and mothers (Özlüses & Çelebioglu, 2014; Su & Ouyang, 2016; Susin et al., 1999; Susin & Giugliani, 2008).
Table 1.
Selected experimental studies of breastfeeding education targeting fathers in LMIC
| Author, year | Design | Setting | Location | Participants | Intervention components | Breastfeeding measure | Data analysis | Breastfeeding outcome |
|---|---|---|---|---|---|---|---|---|
| (Bich et al., 2014; Bich et al., 2016) | Quasiexperimental | Health facility, house visit | Viet Nam | 251 intervention and 241 control couples |
Mass media Counselling Home visits Community |
Maternal report of BF early initiation EBF |
Chi‐square Logistic regression |
Intervention group has higher rate of Early initiated of BF (81.2% vs. 39.6%, p < .001) EBF for the intervention group: At 4 months measured using the 24‐hr recall, no difference, last week recall (21.8% vs. 14.8%, p = .048), since birth (20.6% vs. 11.3%, p = .006) At 6 months: 24‐hr (18% vs. 3%), last week recall (6.6% vs. 1.9%), and since birth recall (6.7% vs. 0.9%) (p < .001) |
| (Özlüses & Çelebioglu, 2014) | Experimental | Hospital | Turkey |
39 mothers and fathers intervention, 39 mothers only intervention, And 39 control group couples |
BF training Education manual |
Maternal report of EBF |
ANOVA Chi‐square |
No significant EBF difference at first and second weeks Couples in the intervention groups show better EBF: First month (82% vs. 87% vs. 33%, p < .001) Second month (69% vs. 76% vs. 30%, p < .001) Fourth month (51% vs. 69% vs. 25%, p = .001) Sixth month (33% vs. 56% vs. 12%, p < .001) |
| (Raeisi et al., 2014) | Intervention | Research Centre | Iran | 50 fathers in the intervention and 50 in the control group | BF training | Maternal report of continued BF | Chi‐square | Intervention group had significantly higher continued BF 6 months (94% vs 76%, p < .01) |
| (Su & Ouyang, 2016) | Quasiexperimental | Hospital | China | 36 couples in the intervention and 36 mothers in the control group | BF education |
Maternal report of EBF Early BF initiation Knowledge Attitude |
t test, Man‐Whitney U test, Chi‐square |
Intervention group showed Better maternal attitude(7.50 vs. 5.17, p = .001), and knowledge (19.75 vs. 14.81, p = .009), EBF at fourth (51.4% vs. 40%, p = .034), and sixth (26.4% vs. 17.6% p = .041) No difference in BF initiation, EBF at 1 month |
| Controlled clinical trial | Hospital | Brazil | 208 control, 197 only mother's intervention, and 196 both mothers and father intervention |
BF education Video discussion Handout |
Maternal report of EBF knowledge |
Kaplan‐Maier, Chi‐square Cox regression Logistic regression |
EBF in mothers and fathers, mothers only, and control groups at fourth month (16.5%, 11.1%, 5.7%, p = .003) Mothers in control group had lower knowledge scores compared with mother only, and mothers' and fathers' intervention groups (5.2%, 15.6%, 27.9%, p < .0001) Knowledge score was higher for fathers in the mother and father intervention compared with fathers in the mother only intervention, and control group (58.3%, 20.6%, and 19.4%, p < .0001) |
|
| (Sahip & Turan, 2007) | Clinical trial | Hospital | Turkey | 102 fathers in the intervention, and 80 in control group |
BF education sessions |
Maternal report of early initiation EBF |
Chi‐square, Student t test, Two‐way ANOVA |
The intervention group showed higher BF initiation (OR = 2·4, 95% CI [1·2, 4·6]), and EBF at 3 months (OR = 3·4, 95% CI [1·7, 6·8]) |
Four of the interventions were tested using the JBI tool for RCTs, three scored 7/10 (Özlüses & Çelebioglu, 2014; Raeisi et al., 2014; Susin et al., 1999; Susin & Giugliani, 2008), and one 6/10 (Sahip & Turan, 2007). Four of the RCTs had similar limitations: Participants who withdrew were not described and were included in the analysis; both group allocators and outcome assessors were not blinded to the treatment allocation (Özlüses & Çelebioglu, 2014; Raeisi et al., 2014; Sahip & Turan, 2007; Susin et al., 1999; Susin & Giugliani, 2008). In addition, in the RCT of Sahip and Turan, assignment to treatment groups was not truly randomized (Sahip & Turan, 2007). The other two were tested using the JBI critical appraisal tool for quasiexperimental studies and scored 8/9 (Su & Ouyang, 2016), and 7/9 (Bich et al., 2014; Bich et al., 2016). The limitations of these quasiexperimental interventions were dissimilarity of participants in each group; difference in care provided between groups other than the intervention or exposure of interest (Bich et al., 2014; Bich et al., 2016); and follow‐up completion and the strategies to deal with loss to follow‐up were not clear (Su & Ouyang, 2016).
3.1. Intervention delivery
The breastfeeding education interventions were delivered by different professionals: paediatricians (Susin et al., 1999; Susin & Giugliani, 2008), physicians (Sahip & Turan, 2007), commune health workers (Bich et al., 2014; Bich et al., 2016), and researchers (Özlüses & Çelebioglu, 2014), with those delivering the intervention unspecified in the remaining two (Raeisi et al., 2014; Su & Ouyang, 2016). The interventions were provided in the form of face‐to‐face breastfeeding education (Özlüses & Çelebioglu, 2014; Raeisi et al., 2014; Sahip & Turan, 2007; Su & Ouyang, 2016), video and discussion (Susin et al., 1999; Susin & Giugliani, 2008), and group counselling, individual counselling, and mass media (Bich et al., 2014; Bich et al., 2016). In addition, the interventions provided printed breastfeeding information such as handouts (Susin et al., 1999; Susin & Giugliani, 2008), brochures (Raeisi et al., 2014), booklets (Su & Ouyang, 2016), and education manuals (Özlüses & Çelebioglu, 2014). The time of intervention delivery was also different across the six interventions. The intervention in Viet Nam (Bich et al., 2014; Bich et al., 2016) was delivered during antenatal and postnatal care. Interventions from Brazil (Susin et al., 1999; Susin & Giugliani, 2008) and Turkey (Özlüses & Çelebioglu, 2014) provided breastfeeding education at hospital during postdelivery. The other three interventions were prenatal breastfeeding trainings delivered at a research centre (Raeisi et al., 2014), workplace (Sahip & Turan, 2007), and university hospital (Su & Ouyang, 2016).
3.2. Breastfeeding outcomes
Except the intervention conducted in Turkey (Özlüses & Çelebioglu, 2014), which has not provided a clear definition of exclusive breastfeeding, all other interventions (Bich et al., 2014; Bich et al., 2016; Raeisi et al., 2014; Sahip & Turan, 2007; Su & Ouyang, 2016; Susin & Giugliani, 2008) have used the WHO breastfeeding definitions (WHO, 2001). WHO defined early breastfeeding initiation as infants put to the breast within 1 hr after birth, and exclusive breastfeeding as providing a child only breastmilk without solid or semi‐solid supplements with the exception of oral rehydration solution, drops or syrups containing vitamins, minerals, and medicines.
3.3. Breastfeeding initiation
Bich & Cuong (2017) found 81.2% of participants initiated breastfeeding within 1 hr after birth in the intervention group and 39.6% in the control group (p < .001). Two studies found that the intervention groups including fathers increased breastfeeding initiation between 2.4 and 7 times (Bich & Cuong, 2017; Sahip & Turan, 2007). This was not supported in another study where there was no difference between intervention and control groups with respect to initiation of breastfeeding (Su & Ouyang, 2016).
3.4. Exclusive breastfeeding
It would appear that interventions that involve fathers improve the rate of exclusive breastfeeding at 3 months (Sahip & Turan, 2007), 4 months (Özlüses & Çelebioglu, 2014; Su & Ouyang, 2016; Susin et al., 1999; Susin & Giugliani, 2008), and 6 months (Bich et al., 2014; Su & Ouyang, 2016), but not at 1 month and below (Özlüses & Çelebioglu, 2014; Su & Ouyang, 2016), when compared with control groups where mothers only received the intervention. At 4 months, mothers had between 4.9% and 11.4% higher rates of exclusive breastfeeding when mothers and fathers received the intervention and 8.8–14.1% at 6 months. Depending on the methods used to determine exclusive breastfeeding, there were significant differences in rates of exclusive breastfeeding using the last week and since birth using recall methods at 4 and 6 months, and at 6 months, only using the 24‐hr recall, but there was no significant difference in breastfeeding exclusivity using the 24‐hr recall at 4 months between the intervention and control groups (Bich et al., 2014).
3.5. Continued breastfeeding
In China, a hospital‐based quasiexperimental study (Su & Ouyang, 2016) showed inclusion of fathers in the intervention decreased breastfeeding discontinuation before 6 months by 20% (HR, 0.80; 95% CI [0.65, 0.98]). Raeisi et al.'s (2014) study from Iran showed that the rate of continued exclusive breastfeeding to 6 months was significantly higher for mothers whose partners were in breastfeeding education training (94%) compared with mothers whose partners were not in the breastfeeding intervention (76%; p < .01).
3.6. Secondary outcomes
3.6.1. Awareness, knowledge, attitude, and support
Breastfeeding interventions improved the level of breastfeeding awareness, knowledge, and attitudes. Fathers who received breastfeeding education showed improved breastfeeding awareness compared with fathers in a control group (103 ± 8.8 vs. 95.7 ± 4.1, p < .0001; Raeisi et al., 2014). Couples receiving antenatal breastfeeding education showed a 7.5% and 4.7% improvement in breastfeeding attitude and knowledge, respectively, compared with the control group (Su & Ouyang, 2016).
The interventions assessed the effect of confounding factors including maternal characteristics, child characteristics, and father characteristics. Although not consistent across multiple studies, mothers with better levels of education, who were not having their first baby (second or higher) and had breastfed their previous child for ≥3 months, had positive effects on improving breastfeeding outcomes (Bich et al., 2014; Susin & Giugliani, 2008). In addition, fathers' and mothers' education level (>8 years) at baseline was associated with improved breastfeeding knowledge after the intervention. Similarly, mothers' participation in prenatal classes and fathers who received advice on breastfeeding during prenatal care had significantly improved knowledge compared with their counterparts (Susin et al., 1999). However, one study (Sahip & Turan, 2007) did not find any effect of confounding factors on breastfeeding outcomes.
4. DISCUSSION
This is the first known systematic literature review exploring breastfeeding interventions targeting fathers in LMIC. Using systematic searching strategies from different bibliographic databases and manual searching, six interventions from LMIC looking at breastfeeding interventions involving fathers were found. A previously conducted systematic review included four interventions, one from LMIC and three from high‐income countries (Mitchell‐Box & Braun, 2013). This indicates that the current systematic review search strategy found additional publications based in LMIC.
The support mothers receive from their partners has a significant effect on their intention to initiate breastfeeding within an hour of birth, breastfeed exclusively, and continue to breastfeed for the recommended timeframe (Bar‐Yam & Darby, 1997; Rempel & Rempel, 2004; Rempel, Rempel, & Moore, 2016; Scott et al., 2001; Thuita et al., 2015). According to the findings of this systematic review, breastfeeding interventions that include fathers (rather than just targeting mothers alone) in LMIC have significantly improved: rates of early breastfeeding initiation (Bich et al., 2016; Sahip & Turan, 2007; Su & Ouyang, 2016), exclusive breastfeeding (Bich et al., 2014; Özlüses & Çelebioglu, 2014; Sahip & Turan, 2007), continued breastfeeding and awareness (Raeisi et al., 2014), and knowledge (Susin et al., 1999). Particularly, interventions with more than one form of education, for instance face‐to‐face breastfeeding education, video, and handout, seem to have a beneficial effect on improving breastfeeding outcomes (Özlüses & Çelebioglu, 2014; Raeisi et al., 2014; Susin et al., 1999; Susin & Giugliani, 2008). Therefore, breastfeeding interventions in LMIC that include fathers will potentially increase breastfeeding initiation, exclusivity, and duration.
Overall, the quality of the trials included in this review was good. A majority of the interventions attempted to control for the potential confounding effects of mothers, infants, and father's characteristics at baseline (Bich et al., 2014; Bich et al., 2016; Sahip & Turan, 2007; Su & Ouyang, 2016; Susin et al., 1999; Susin & Giugliani, 2008). The use of multiple education techniques is another strength of these interventions. For instance, Bich and colleagues used video demonstration, group counselling, mass media, individual counselling, and a public event (Bich et al., 2014; Bich et al., 2016). There were, however, a number of limitations. Almost all of them, except the studies in Viet Nam (Bich et al., 2014; Bich et al., 2016), used shorter breastfeeding education within the hospital setting, predominantly during the prenatal, and postdelivery periods. In addition, except for one study (Susin & Giugliani, 2008), none of the interventions blinded the data collectors as to which arm the mother/partner was assigned. Moreover, a majority of the interventions used smaller sample sizes with inadequate power (Özlüses & Çelebioglu, 2014; Raeisi et al., 2014; Sahip & Turan, 2007; Su & Ouyang, 2016). Thus, further randomized control trials with adequate sample sizes are crucial in order to determine the effectiveness of breastfeeding interventions targeting fathers in LMIC.
The systematic review indicated that all of the studies were from middle‐income countries; no intervention studies focused on low‐income countries. According to Abera, Abdulahi, and Wakayo (2017) and Cardoso, Silva, and Marin (2017), involving fathers in breastfeeding support significantly enhances mother's perceptions of breastfeeding and can potentially optimize breastfeeding rates, exclusivity, and duration. Therefore, with the changing role of fathers in low‐income countries, there is a potential opportunity for fathers to maximize the health of their children by supporting their partners using their breastfeeding knowledge to motivate and assist them to breastfeed (Rempel & Rempel, 2011). Data on breastfeeding interventions targeting fathers from low‐income countries are lacking; therefore, future interventions need to target this group.
All these interventions used either health providers working in hospitals or researchers to deliver the breastfeeding education. Findings from a meta‐analysis indicated that lay support significantly correlated with duration of breastfeeding (Dennis, 2002). In the same way, systematic reviews revealed a significant positive treatment effect of lay support on cessation of any breastfeeding, and exclusive breastfeeding compared with professional, or both lay and professional support at 6 months (McFadden et al., 2017; Renfrew et al., 2012).Thus, further research is required to understand the effectiveness of breastfeeding education delivered by peers and targeting fathers in LMIC.
None of the studies identified in this review utilized mHealth techniques. Mobile phone ownership is increasing in low‐income countries, and mobile phones have significant importance in connecting people as landline and broadband connections are not easily accessible (Bastawrous, Hennig, & Livingstone, 2013). In addition, Lee and colleagues show that mothers who received an SMS/phone call breastfeeding intervention were almost twice as likely to initiate breastfeeding early and breastfeed exclusively at 6 months compared with those who were receiving usual care (Lee et al., 2016). Similarly, Flax and colleagues reported that using SMS, call phone, and video interventions to educate mothers in a microfinance group doubled the level of exclusive breastfeeding and early initiation of breastfeeding compared with the standard care (Flax et al., 2014). All of these mHealth approaches have targeted mothers only. Therefore, interventions could incorporate mHealth as a means of promoting breastfeeding to fathers and mothers.
This review of breastfeeding outcomes from interventions targeting fathers in LMIC has strengths and limitations. First, the search strategy was comprehensive and was designed in consultation with a specialist librarian. All possible terms were included in the search strategy under the category of breastfeeding, father, LMIC, and education. In addition, date of publication was not restricted, although a majority were published between 2014 and 2016 (Bich et al., 2014; Bich et al., 2016; Özlüses & Çelebioglu, 2014; Raeisi et al., 2014; Su & Ouyang, 2016). The review process was done by two independent reviewers for both selection of articles and data extraction. Moreover, the quality of these articles was assessed using the JBI RCT and quasiexperimental evaluation tools. However, our search was limited to articles written in English; thus, papers written in other languages were excluded. The other limitation of this review is that a meta‐analysis was not able to be performed to measure the overall intervention effect on breastfeeding outcomes. This was due to multiple factors but primarily due to the diversity of interventions used and outcomes measured. One of the interventions used a broad variety of interventions, others used multiple education types (Bich et al., 2014; Bich et al., 2016), and in some cases, reading material was provided to the control group as well (Özlüses & Çelebioglu, 2014). One intervention provided education to fathers only (Raeisi et al., 2014), and the education duration was different across all interventions.
5. CONCLUSION
It is widely acknowledged that partners' support has a significant effect on maternal breastfeeding intention, exclusivity, and duration. However, in this review, we found only six breastfeeding interventions targeting fathers from predominantly middle‐income countries. Due to the differences in duration of intervention and mix of education types, number of intervention groups, and breastfeeding education delivery mechanisms, a comparison between the interventions was not able to be made. However, all these interventions revealed that breastfeeding interventions targeting fathers in LMIC increased the level of early breastfeeding initiation, exclusive breastfeeding, and continued breastfeeding. Delivery of breastfeeding education through peer fathers and mHealth requires more research in order to understand their effectiveness in improving breastfeeding, as they have been shown to be effective in interventions targeting mothers only. The breastfeeding interventions focusing on fathers from LMIC are limited, and there are no data from low‐income countries. Thus, more research is required to investigate the effectiveness of fathers' involvement in breastfeeding education on breastfeeding outcomes, especially in low‐income countries.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
KT performed the literature searching, selected the papers of interest, performed data extraction, and prepared the manuscript. DG selected the papers of interest, and performed data extraction. OZ and AM gave important contributions for interpretation of data and writing of the manuscript. All authors read and approved the final manuscript.
ACKNOWLEDGMENT
We thank Peter Sondergeld, Liaison Librarian–Health Faculty at QUT for the help in designing the search strategy.
Tadesse K, Zelenko O, Mulugeta A, Gallegos D. Effectiveness of breastfeeding interventions delivered to fathers in low‐ and middle‐income countries: A systematic review. Matern Child Nutr. 2018;14:e12612 10.1111/mcn.12612
REFERENCES
- Abbass‐Dick, J. , Stern, S. B. , Nelson, L. E. , Watson, W. , & Dennis, C.‐L. (2014). Coparenting breastfeeding support and exclusive breastfeeding: A randomized controlled trial. Pediatrics. [DOI] [PubMed] [Google Scholar]
- Abera, M. , Abdulahi, M. , & Wakayo, T. (2017). Fathers' involvement in breast feeding practices and associated factors among households having children less than six months in Southern Ethiopia: A cross sectional study. Pediatrics and Therapeutics, 7(1). 10.4172/2161-0665.1000306 [DOI] [Google Scholar]
- Avery, A. B. , & Magnus, J. H. (2011). Expectant fathers' and mothers' perceptions of breastfeeding and formula feeding: A focus group study in three US cities. Journal of Human Lactation, 27(2), 147–154. 10.1177/0890334410395753 [DOI] [PubMed] [Google Scholar]
- Bar‐Yam, N. B. , & Darby, L. (1997). Fathers and breastfeeding: A review of the literature. Journal of Human Lactation, 13(1), 45–50. [DOI] [PubMed] [Google Scholar]
- Bastawrous, A. , Hennig, B. , & Livingstone, I. (2013). mHealth possibilities in a changing world. Distribution of global cell phone subscriptions. JMTM, 2(1), 22–25. 10.7309/jmtm.78 [DOI] [Google Scholar]
- Bich, T. H. , & Cuong, N. M. (2017). Changes in knowledge, attitude and involvement of fathers in supporting exclusive breastfeeding: A community‐based intervention study in a rural area of Vietnam. International Journal of Public Health, 62(Suppl 1), 17–26. 10.1007/s00038-016-0882-0 [DOI] [PubMed] [Google Scholar]
- Bich, T. H. , Hoa, D. T. , Ha, N. T. , Vui, L. T. , Nghia, D. T. , & Målqvist, M. (2016). Father's involvement and its effect on early breastfeeding practices in Viet Nam. Maternal & Child Nutrition, 12(4), 768–777. 10.1111/mcn.12207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bich, T. H. , Hoa, D. T. P. , & Målqvist, M. (2014). Fathers as supporters for improved exclusive breastfeeding in Viet Nam. Maternal and Child Health Journal, 18(6), 1444–1453. 10.1007/s10995-013-1384-9 [DOI] [PubMed] [Google Scholar]
- Cardoso, A. , Silva, A. , & Marin, H. (2017). Fathers 'to be' knowledge about breastfeeding. International Journal of Pregnancy & Child Birth, 2(3). 10.15406/ipcb2017.02.00023 [DOI] [Google Scholar]
- Dennis, C. L. (2002). Breastfeeding initiation and duration: A 1990‐2000 literature review. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 31(1), 12–32. [DOI] [PubMed] [Google Scholar]
- Flax, V. L. , Negerie, M. , Ibrahim, A. U. , Leatherman, S. , Daza, E. J. , & Bentley, M. E. (2014). Integrating group counseling, cell phone messaging, and participant‐generated songs and dramas into a microcredit program increases Nigerian women's adherence to international breastfeeding recommendations. The Journal of Nutrition, 144(7), 1120–1124. 10.3945/jn.113.190124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson, L. , McMillan, B. , Green, J. M. , & Renfrew, M. J. (2011). Men and infant feeding: perceptions of embarrassment, sexuality, and social conduct in white low‐income British men. Birth, 38(1), 61–70. 10.1111/j.1523-536X.2010.00442.x [DOI] [PubMed] [Google Scholar]
- Kramer, M. S. , & Kakuma, R. (2004). The optimal duration of exclusive breastfeeding: A systematic review. Advances in Experimental Medicine and Biology, 554, 63–77. [DOI] [PubMed] [Google Scholar]
- Lee, S. H. , Nurmatov, U. B. , Nwaru, B. I. , Mukherjee, M. , Grant, L. , & Pagliari, C. (2016). Effectiveness of mHealth interventions for maternal, newborn and child health in low– and middle–income countries: Systematic review and meta–analysis. Journal of Global Health, 6(1). 010401. doi: 10.7189/jogh.06.010401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maycock, B. , Binns, C. W. , Dhaliwal, S. , Tohotoa, J. , Hauck, Y. , Burns, S. , & Howat, P. (2013). Education and support for fathers improves breastfeeding rates: a randomized controlled trial. Journal of Human Lactation, 29(4), 484–490. 10.1177/0890334413484387 [DOI] [PubMed] [Google Scholar]
- McFadden, A. , Gavine, A. , Renfrew, M. J. , Wade, A. , Buchanan, P. , Taylor, J. L. , … MacGillivray, S. (2017). Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database of Systematic Reviews, (2). 10.1002/14651858.CD001141.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell‐Box, K. , & Braun, K. (2013). Impact of male‐partner‐focused interventions on breastfeeding initiation, exclusivity, and continuation. Journal of Human Lactation, 29(4), 473–479. 10.1177/0890334413491833 [DOI] [PubMed] [Google Scholar]
- Mitchell‐Box, K. , & Braun, K. L. (2012). Fathers' thoughts on breastfeeding and implications for a theory‐based intervention. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 41(6), E41–E50. 10.1111/j.1552-6909.2012.01399.x [DOI] [PubMed] [Google Scholar]
- Özlüses, E. , & Çelebioglu, A. (2014). Educating fathers to improve breastfeeding rates and paternal‐infant attachment. Indian Pediatrics, 51(8), 654–657. 10.1007/s13312-014-0471-3 [DOI] [PubMed] [Google Scholar]
- Pisacane, A. , Continisio, G. I. , Aldinucci, M. , D'Amora, S. , & Continisio, P. (2005). A controlled trial of the father's role in breastfeeding promotion. Pediatrics, 116(4), e494–e498. 10.1542/peds.2005-0479 [DOI] [PubMed] [Google Scholar]
- Raeisi, K. , Shariat, M. , Nayeri, F. , Raji, F. , & Dalili, H. (2014). A single center study of the effects of trained fathers' participation in constant breastfeeding. Acta Medica Iranica, 52(9), 694–696. [PubMed] [Google Scholar]
- Rempel, L. , & Rempel, J. (2004). Partner influence on health behavior decision‐making: Increasing breastfeeding duration. Journal of Social and Personal Relationships, 21(1), 92–111. 10.1177/0265407504039841 [DOI] [Google Scholar]
- Rempel, L. , & Rempel, J. (2011). The breastfeeding team: The role of involved fathers in the breastfeeding family. Journal of Human Lactation, 27(2), 115–121. 10.1177/0890334410390045 [DOI] [PubMed] [Google Scholar]
- Rempel, L. , Rempel, J. , & Moore, K. (2016). Relationships between types of father breastfeeding support and breastfeeding outcomes. Maternal & Child Nutrition, 13 10.1111/mcn.12337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renfrew, M. J. , McCormick, F. M. , Wade, A. , Quinn, B. , & Dowswell, T. (2012). Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev, (5). Cd001141. doi: 10.1002/14651858.CD001141.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahip, Y. , & Turan, J. M. (2007). Education for expectant fathers in workplaces in Turkey. Journal of Biosocial Science, 39(6), 843–860. 10.1017/s0021932007002088 [DOI] [PubMed] [Google Scholar]
- Scott, J. A. , Landers, M. C. , Hughes, R. M. , & Binns, C. W. (2001). Factors associated with breastfeeding at discharge and duration of breastfeeding. Journal of Paediatrics and Child Health, 37(3), 254–261. [DOI] [PubMed] [Google Scholar]
- Sikorski, J. , Renfrew, M. J. , Pindoria, S. , & Wade, A. (2003). Support for breastfeeding mothers: A systematic review. Paediatric and Perinatal Epidemiology, 17(4), 407–417. [DOI] [PubMed] [Google Scholar]
- Su, M. , & Ouyang, Y.‐Q. (2016). Father's role in breastfeeding promotion: Lessons from a quasi‐experimental trial in China. Breastfeeding Medicine, 11(3), 144–149. 10.1089/bfm.2015.0144 [DOI] [PubMed] [Google Scholar]
- Susin, L. , & Giugliani, E. (2008). Inclusion of fathers in an intervention to promote breastfeeding: Impact on breastfeeding rates. Journal of Human Lactation, 24(4), 386–392. 10.1177/0890334408323545 [DOI] [PubMed] [Google Scholar]
- Susin, L. , Giugliani, E. , Kummer, S. , Maciel, M. , Simon, C. , & Silveira, L. (1999). Does parental breastfeeding knowledge increase breastfeeding rates? Birth, 26(3), 149–156. [DOI] [PubMed] [Google Scholar]
- The Joanna Briggs Institute . (2017). Critical Appraisal Tools. Retrieved February 2017, from http://joannabriggs.org/research/critical-appraisal-tools.html
- Thuita, F. , Martin, S. , Ndegwa, K. , Bingham, A. , & Mukuria, A. (2015). Engaging fathers and grandmothers to improve maternal and child dietary practices: Planning a community‐based study in Western Kenya. ajfand, 15(5). [Google Scholar]
- USAID (2011). The roles and influence of grandmothers and men. Washington, DC. [Google Scholar]
- Victora, C. G. , Bahl, R. , Barros, A. J. D. , França, G. V. A. , Horton, S. , Krasevec, J. , … Rollins, N. C. (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet, 387(10017), 475–490. [DOI] [PubMed] [Google Scholar]
- WHO . (2001). Global strategy for infant and young child feeding. The optimal duration of exclusive breastfeeding Geneva: World Health Organization. [Google Scholar]
- WHO . (2009). Model chapter for textbooks for medical students and allied health professionals. Infant and young child feeding Geneva: WHO. [PubMed] [Google Scholar]
- WHO . (2014). Exclusive breastfeeding under 6 months: Global Health Observatory data repository. Retrieved 12/09, 2016, from http://apps.who.int/gho/data/view.main.NUT1710?lang=en


