Abstract
We assessed India's readiness to deliver infant and young child feeding (IYCF) interventions by examining elements related to policy, implementation, financing, and evidence. We based our analysis on review of (a) nutrition policy guidance and program platforms, (b) published literature on interventions to improve IYCF in India, and (c) IYCF program models implemented between 2007 and 2012. We find that Indian policies are well aligned with global technical guidance on counselling interventions. However, guidelines for complementary food supplements (CFS) need to be reexamined. Two national programs with the operational infrastructure to deliver IYCF interventions offer great potential for scale, but more operational guidance, capacity, and monitoring are needed to actively support delivery of IYCF counselling at scale by available frontline workers. Many IYCF implementation efforts to date have experimented with approaches to improve breastfeeding and initiation of complementary feeding but not with improving diet diversity or the quality of food supplements. Financing is currently inadequate to deliver CFS at scale, and governance issues affect the quality and reach of CFS. Available evidence from Indian studies supports the use of counselling strategies to improve breastfeeding practices and initiation of complementary feeding, but limited evidence exists on improving full spectrum of IYCF practices and the impact and operational aspects of CFS in India. We conclude that India is well positioned to support the full spectrum of IYCF using existing policies and delivery platforms, but capacity, financing, and evidence gaps on critical areas of programming can limit impact at scale.
Keywords: complementary food supplements, India, infant and young child feeding, IYCF counselling, policies, programs
1. INTRODUCTION
In the context of the new global goals for development, the momentum to improve nutrition is high and action is imperative. Nutrition has been recognized to be fundamental to achieving the health, education, and economic goals contained in the Millennium Development Goals (von Braun, Swaminathan, & Rosegrant, 2004) and is now well positioned in the Sustainable Development Goals (World Health Organization, 2014) and in the World Health Assembly global nutrition targets (World Health Organization, 2014). Despite rapid progress on reductions in undernutrition, the burden remains high and the poor state of infant and young child feeding (IYCF) is a particularly significant challenge (International Food Policy Research Institute, 2014).
Age‐appropriate IYCF practices include initiation of breastfeeding within an hour after birth, exclusive breastfeeding for the first 6 months, and age‐appropriate complementary feeding practices (i.e., appropriate quality, quantity, frequency, and hygiene). Strong technical guidance exists for improving infant feeding practices (PAHO, 2003; World Health Organization, 2010). Evidence‐based interventions such as individual and group counselling by health professionals and peers (Dyson, McCormick, & Renfrew, 2006; Bhutta et al., 2008) and lay health workers (Lewin et al., 2010) are known to support improvements in breastfeeding, and counselling along with food supplementation in food‐insecure populations is known to support improvements in complementary feeding practices (Imdad, Yakoob, & Bhutta, 2011). Improving these practices can make significant contributions to achieving the new global goals, whether in the realm of reducing child deaths or improving nutritional status, but what is imperative is that countries embrace, scale‐up, and intensify the policy and program actions necessary to support these practices.
India's progress on IYCF is mixed (Figure 1). Despite improvements in early initiation of breastfeeding, current levels remain low (44 percent). Exclusive breastfeeding at 65 percent is encouraging (India–MoWCD, 2015), but only one in two Indian children received complementary foods between 6 and 8 months of age, a decline from 56 percent (IIPS, 2007) a decade ago. Only one in five children received at least four food groups (India–MoWCD, 2015). Finally, food supplements provided to infants and young children by the Integrated Child Development Services (ICDS), a national program, currently reach only up to 50% of children across India (India–MoWCD, 2015). Several small‐scale studies support these survey findings, detailing suboptimal breastfeeding and/or complementary feeding practices throughout India (Khan, Kayina, Agrawal, Gupta, & Kannan, 2012; Mahmood, Srivastava, Shrotriya, & Mishra, 2012; Meshram, Laxmaiah, Venkaiah, & Brahmam, 2012; Meshram et al., 2013; Singhal et al., 2013). Achieving progress on these practices in India, therefore, will require integrating and strengthening IYCF interventions in the context of programs that are already operating at nationwide scale while also strengthening the policy environment to support optimal infant feeding. Our study aims to examine India's readiness to effectively integrate and implement evidence‐based IYCF interventions at scale.
Figure 1.
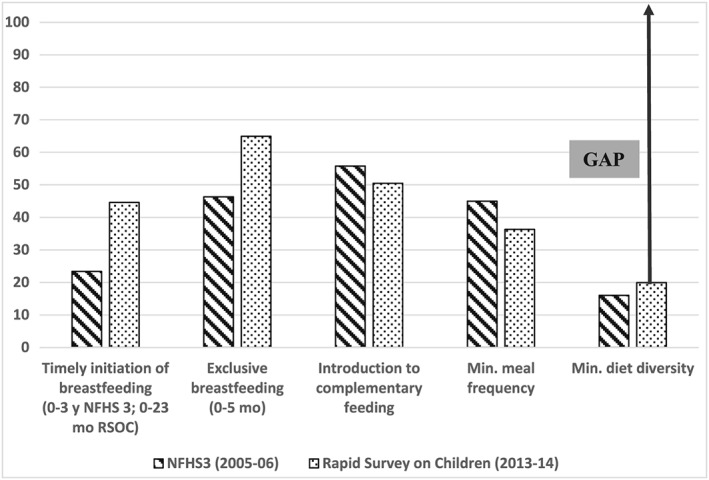
Coverage gap in infant and young child feeding in India
Key Messages.
India has a vision for impact to improve infant and young child feeding (IYCF): a supportive policy environment for most current IYCF interventions and multiple operational platforms exist that can deliver counseling and complementary food supplements.
Indian policies are well aligned with global evidence on counseling interventions. However, current guidelines for complementary food supplements need to be reexamined.
Capacity, finance, and governance gaps are the primary limiting factors in achieving full coverage of IYCF counseling and complementary food supplements.
A significant evidence gap exists in the research evidence base and program experience base on key aspects of improving complementary feeding, for example, improving diet diversity, assessing the combined effects of food supplements, and counselling.
2. MATERIALS AND METHODS
We use a framework for scaling‐up nutrition impact (Gillespie, Menon, & Kennedy, 2015) to analyze India's ability to deliver interventions to improve IYCF practices at scale. Using multiple sources of information, we examined India's vision and policy environment for scaling‐up of the IYCF interventions, availability of intervention delivery platforms, enabling organizational context, catalysts, and champions to drive the effort, and relevant strategies and operational capacities, along with adequate financing and embedded learning mechanisms. We reviewed (a) India's policy intent and program platforms, (b) program implementation experiences, and (c) India‐specific efficacy and effectiveness evidence on IYCF interventions.
To assess policy intent, we conducted a content analysis of India's national nutrition policies (India–MoHFW, 2013; Vir et al., 2014), examining whether currently recommended IYCF interventions (Bhutta et al., 2013) are included in the policies. We accessed these documents directly from government websites. To assess the program platforms available for delivering IYCF interventions at scale, we reviewed relevant national program documents (India‐MoWCD, 2009; India‐MoWCD, 2011) and their operational guidelines (India–MoHFW, 2007; India‐MoWCD, 2010a; India‐MoWCD, 2010b).
To document IYCF implementation experiences, we took two approaches. First, we reviewed programs identified as “best practice” models in two earlier program reviews (Micronutrient Initiative, 2007; IntraHealth International, 2008) that covered programs implemented until 2007. To update this list of programs, we contacted approximately 70 stakeholders (e.g., nongovernment organizations, research institutes, development partners, and individual nutrition champions) in 2012. The call had a 50% response rate. Only those programs that met the pre‐determined criteria of at‐scale implementation (at least at the district level) and had a detailed program description were included in the review. Eighteen programs met these criteria. Program documents were examined to identify which evidence‐based interventions for IYCF were included in the programs and what operational strategies had been used to deliver these interventions.
Information on the capacity needs was drawn from the review of implementation experiences and the published literature. Information on financing and stakeholders was included from other sources (Menon, McDonald, & Chakabarti, 2016; Puri et al., forthcoming).
To assess the availability of evidence on the impact of IYCF interventions in India, we reviewed the published literature on the impact of interventions—counselling and complementary food supplements (CFS)—to improve IYCF in India between 2000 and 2014. We conducted a literature search using Google Scholar and PubMed for the period between 2000 and 2014 (Table 1). Then titles and abstracts were examined for relevance, and full texts of all relevant articles were reviewed to document both the intervention descriptions and impacts of the tested interventions. Additionally, using guidance on evaluation designs (Habicht, Victora, & Vaughan, 1999), we examined the evaluations used in the program implementation experiences, which were then classified to have (a) an adequacy design if the evaluation was a pre‐ or post‐comparison only; (b) a weak plausibility design if there was a comparison group but no baseline data; (c) a strong plausibility design if there was a comparison group, with baseline in both program and comparison areas; or (d) a probability design if the comparison and control groups were randomly assigned.
Table 1.
List of key words used for systematic review of literature
| Google Scholar | ||||
|---|---|---|---|---|
| Number of articles found 2000–2012 | Number of relevant articles 2000–2012 | Number of articles found 2012–2014 | Number of relevant articles 2012–2014 | |
| Timely initiation breastfeeding | ||||
| “Breastfeeding initiation*” + “intervention*” + India | 318 | 2 | 331 | 5 |
| “Breastfeeding initiation*” + “counselling*” + “intervention* “ + India | 98 | 0 | 74 | 2 |
| “Breastfeeding initiation*” + “counselling*” + “intervention*” + “community*” + India | 95 | 0 | 72 | 1 |
| “Breastfeeding initiation*” + “counselling*” + “intervention*” + “community*” + “health worker*” + India | 27 | 1 | 18 | 1 |
| Exclusive breastfeeding | ||||
| “Exclusive breastfeeding*” + “intervention*” + “community*” + “counselling*” + India | 593 | 3 | 341 | 5 |
| “Exclusive breastfeeding*” + “intervention*” + “community*” + “counselling*” + “health workers*” + India | 361 | 3 | 139 | 3 |
| “Exclusive breastfeeding*” + “trial*” + “community*” + “counselling*” + India | 493 | 3 | 457 | 3 |
| “Exclusive breastfeeding*” + trial*” + “community*” + “nutrition education*” + India | 223 | 3 | 815 | 3 |
| “Exclusive breastfeeding*” + “trial*” + “community*” + “counselling*” + “health workers*” + India | 284 | 3 | 48 | 3 |
| Complementary feeding | ||||
| “Complementary feeding*” + “initiation*” + “interventions*” + “supplementary nutrition*” + India | 455 | 4 | 313 | 5 |
| “Complementary feeding*” + “initiation*” + “interventions*” + “supplementary nutrition*” + “trials*” + India | 82 | 3 | 113 | 3 |
| “Complementary feeding*” + “initiation*” + “interventions*” + “nutrition education*” + India | 145 | 3 | 88 | 3 |
| “Complementary feeding*” + “nutrition education*” + India | 490 | 6 | 300 | 7 |
| Feeding during illness | ||||
| “Complementary feeding*” + “illness” + India | NA | NA | 1,760 | 1 |
NA = not applicable.
Note. Number of relevant articles for each set of search terms is not mutually exclusive.
3. RESULTS
Our review points to substantial policy intent, nationally available at‐scale implementation platforms and frontline workers but mixed program/operational support and potentially limited financing. On evidence for action on scaling‐up IYCF counselling and CFS, we find a reasonable evidence base of efficacy studies but a poor evaluation base for scaling‐up. Our overall analysis, addressing all elements of the scaling‐up framework, is summarized in Table 2, and the most salient details, stemming from our primary reviews, are discussed below.
Table 2.
Summary of findings on readiness to deliver infant and young child feeding (IYCF) counselling interventions and complementary food supplements (CFS) at scale in India
| Framework element (adapted from Gillespie et al., 2015) | IYCF counselling | CFS |
|---|---|---|
| 1. Vision, goal, and policy context (source: authors review) | The need for IYCF counselling is generally included in policy guidance, but there are no specific stated measurable goals to achieve, thus, diluting the vision. | CFS are included in the stated universalization of the ICDS in the Right to Food legislation. The notion of universalization provides a goal (coverage for all). |
| Policy guidance available and in alignment with global strategy on IYCF. Training modules available for multiple frontline workers, and record‐keeping registers are also available to support adequate home visit‐based counselling. | Policy guidance and legal directives in place to ensure universal access to CFS. | |
| 2. and 3. Intervention and delivery platforms (source: authors review and Vaid, Avula, George, John, & Menon, 2017) | Two major operational platforms exist (the ICDS and NRHM). There is limited ownership by both programs of IYCF counselling, limited role clarity among frontline workers (FLWs), and challenges exist in converging services from the two platforms. | CFS is fully controlled and delivered through one platform (i.e., ICDS) that operates at scale. Although the norms for the CFS (quality, amounts, and nutritional composition) require some revision, the potential for reaching all the children exists (barring issues of leakage, parental choice to use supplements for children, family sharing, etc.). |
| 4. Capacity (source: authors review and Avula et al., 2015) | FLWs are currently available but not adequately trained (as evidenced by knowledge assessments in Avula et al., 2015), but materials are developed, and at the time of writing this paper, different approaches are being explored to train FLWs. Role clarity, adequate supervision, and monitoring are key challenge areas here. | Capacity of local production models to produce high‐quality, safe complementary food supplements is unknown, although models like the one used in Odisha appear to deliver supplements at scale. |
| 5. Financing (source: Menon et al., 2016) | Costing estimates are available, but adequacy of available financing for training and support to FLWs remains unknown. Financial incentives, mass media campaigns, and ICT tools to support counselling will add to costs. | Financing is available and secured. However, adequacy of financing is a challenge, and changes in financing landscape for nutrition (decentralized) raise further issues of state‐level prioritization and adequacy. Furthermore, addressing quality and composition issues will have cost implications that will need careful attention. |
| 6. Governance (source: primary review) | No major governance challenges | Significant governance challenges around procurement, production, and distribution of the CFS, however, which varies by state and which persist despite a court‐appointed monitoring office. |
| 7. Catalysts and leading institutions (Puri et al., forthcoming) | Limited. BPNI and UNICEF have played important roles over the years, but there is no clear coalition or alliance to engage, harmonize actions, and content for counselling. | Right to Food Campaign activists filed legal cases in the context of public interest litigation cases. Core nutrition community has not come together around this component of the nutrition programs. |
| 8. Monitoring, learning, and evaluation (source: Avula et al., 2013) | Adequate evidence exists in the published literature from India to support the use of counselling intervention. Limited documented program implementation experiences in targeting complementary feeding. | Very limited literature in India on the role of CFS (whether and to what extent) in improving complementary feeding practices and nutritional outcomes. Few models of CFS delivery are rigorously evaluated either for cost or operational implications or impact. |
| No denominator‐based monitoring indicators on IYCF, which limits supervision and management. | Monitoring indicators are in place to track reach of the supplements to intended target groups, but in many areas, this is not denominator‐based and simply reports on numbers of women and children given supplements. |
We find that nutrition policies and guidelines/action plans for delivery of nutrition interventions are made across two major ministries—the Ministry of Health and Family Welfare (MHFW) and the Ministry of Women and Child Development (MWCD) and relate to an overall goal of improving nutrition. These policies set overall direction, whereas action plans and guidelines often provide operational and even financial guidance. The goal of achieving universal coverage is clearly articulated for CFS delivery in response to a legal edict issued in 2006 to assure full‐scale availability of food supplements in the ICDS as part of policy efforts to ensure children's right to food (Supreme Court of India, 2001). A similar hard goal is amiss for IYCF counselling.
Overall, Indian policies have evolved over time to align with global recommendations and demonstrate broad support for implementing evidence‐based IYCF interventions (Table 3). The national policies and charters offer a vision and guidance to a government's approach to India's child health and nutrition as well as protection of child rights. As far back as in 1993, the first National Nutrition Policy (India‐MHRD, 1993) highlighted the need for a multisectoral approach to address malnutrition and recommended special focus on IYCF practices to improve child nutrition. The subsequent National Plan of Action for Children in 1995 defined a framework for a multisectoral strategy and specified sectoral goals and objectives to be achieved by 2000. In 2005, an updated National Plan of Action for Children identified 12 priority areas for action and set goals to be achieved by 2010 (India‐MoWCD, 2005). Whereas the 1995 Plan of Action took a sectoral approach, the 2005 Plan of Action took a priority area approach; however, the National Policy for Children, initially adopted in 1974, was the premise for both of these plans.
Table 3.
Evolution of Indian policies and guidelines on infant and young child feeding (IYCF)
| Year | Policy/guidelines/action plans | Elements of the policies/guidelines | Issuing authority |
|---|---|---|---|
| 1983 | National Code for Protection and Promotion of Breastfeeding and introduced measures for reducing marketing of milk powder and infant food substitutes. | Follows the 1981 International Code for Protection and Promotion of Breastfeeding | Government of India |
| Introduced measures to reduce marketing of milk powder and infant food substitutes | |||
| 1992 | Infant Milk Substitutes, Feeding Bottles and Infant Foods (Regulation of Production, Supply & Distribution) Act | Regulates production, supply, and distribution of infant milk substitutes, feeding bottles, and infant foods to protect and promote breastfeeding | Ministry of Law, Justice and Company Affairs, Government of India |
| 1993 | National Nutrition Policy | Recognizes the need for a multi‐sectoral approach to improve nutrition | Department of Women and Child Development |
| Describes multiple programs for addressing malnutrition | Ministry of Human Resource Development | ||
| 1995 | National Plan of Action for Nutrition | Recognizes the need for multi‐sectoral approach and identifies objectives and activities for multiple sectors | Department of Women and Child Development |
| Recommends exclusive breastfeeding up to 4 months and introduction of complementary feeding after 4–6 months | Ministry of Human Resource Development | ||
| 2003 | The Infant Milk Substitutes, Feeding Bottles and Infant Foods (Regulation of Production, Supply and Distribution) Act, 1992 as Amended in 2003 (IMS Act) | Regulates production, supply, and distribution of infant milk substitutes, feeding bottles, and infant foods to protect and promote breastfeeding and ensure the proper use of infant foods. | Government of India |
| 2003 | National Charter for Children | Proclamation of the state to protect the rights of children to ensure their healthy growth and development through combined action of the State, civil society, communities, and families | Department of Women and Child Development |
| Ministry of Human Resource Development | |||
| 2004 | National Guidelines on Infant and Young Child Feeding | Recommends early initiation of breastfeeding, exclusive breastfeeding for up to 6 months and introduction of complementary foods after 6 months, frequent feeding (5–6 times/day), ensuring food hygiene and provides guidance on feeding during illness and feeding in exceptionally difficult | Department of Women and Child Development |
| Ministry of Human Resource Development (Food and Nutrition Board) | |||
| 2005 | National Plan of Action for Children | Recommends a life‐cycle approach to improving nutritional status | Department of Women and Child Development |
| Promotes optimal infant and child feeding practices and strategies to achieve them | Ministry of Human Resource Development | ||
| 2006 | National Guidelines on Infant and Young Child Feeding | IYCF guidelines updated to reflect the WHO/UNICEF global recommendations on breastfeeding and complementary feeding | Food and Nutrition Board |
| Ministry of Women and Child Development | |||
| 2009 | Revised Nutritional and Feeding Norms for Supplementary Nutrition in ICDS Scheme | Recommends a daily food supplement of 500 calorie of energy and 12–15 g of protein per child per day | Ministry of Women and Child Development |
| 2013 | Guidelines for enhancing optimal infant and young child feeding practices | Includes technical guidelines developed by the Indian Academy of Pediatrics in 2010 and the Ministry of Women and Child Development's 2006 national IYCF guidelines | Ministry of Health and Family Welfare |
| Provides planning and implementation guidance for program managers on IYCF practices | |||
| 2013 | National Policy for Children | Affirms government's rights based approach to healthy growth and development of children | Ministry of Women and Child Development (India‐MOWCD, 2013a) |
| Intends to provide guidance to all policies, plans, and programs affecting children. | |||
| One of the topics listed are the right to all essential nutrition services, including IYCF practices. |
The first National Code for protection and promotion of breastfeeding was introduced in 1983, following the International Code to regulate marketing and promotion of breastmilk substitutes. The code was later amended in 1992 and 2003. The amendments to the Code in 2003 reflect advances in marketing techniques and improved technical guidance. The definition of “advertisement” was modified to include “electronic transmission by audio or visual transmission,” healthcare system included pharmacies and drugstores, and the age limit for marketing infant foods was raised from 4 to 6 months and an upper age limit of 2 years.
Similarly, changes in global technical recommendations influenced national guidance on exclusive breastfeeding. The 1995 National Plan of Action (India‐MoHRD, 1995) recommended exclusive breastfeeding until the first 4 months, which aligned with the global recommendations of that period. The guidelines were revised in the 2005 National Plan of Action, to recommend exclusive breastfeeding until the first 6 months, in alignment with global recommendations (PAHO, 2003).
The national guidelines on IYCF were revised in 2004 and then in 2006 to be congruent with the WHO/UNICEF Global Strategy on IYCF (India–MHRD/FNB, 2006). Most recently, in 2013, the MHFW released operational guidelines for interventions to support optimal IYCF practices (India–MoHFW, 2013) and launched a program to support breastfeeding (Mothers Absolute Affection; Press Information Bureau 2016), bringing into focus the current discourse on the first 1,000 days (Table 3). Thus, IYCF counselling is well recognized as a key aspect of improving IYCF practices.
In India, nutrition counselling interventions were guided by the evolving global evidence; the CFS intervention was initiated primarily to bridge known calorie and protein gaps in the diets of the Indian children in the 1970s. Under the Minimum Needs Programme of the Fifth Five‐Year plan, the Special Nutrition Programme was launched in 1970–1971. It included provision of food supplements to eligible pregnant and lactating mothers and to preschool children, which was later integrated into the ICDS program (India‐MHRD, 1993). The food supplements were intended to provide 300 calories and 10 g of protein to children (India‐MHRD, 1993). Food supplementation along with nutrition education is a recommended intervention for improving IYCF practices among food insecure populations (Imdad et al., 2011), and hence, India's policy, taken along with the existing guidelines for providing counselling, is consistent with the global guidance. In 2009, the MWCD revised the cost and calorific norms to adequately bridge the gap between the recommended dietary allowance and average dietary intake. The recommendation that the reconstitutable blend of cereals, pulses, and other ingredients should provide 500 kcal of energy and 12–15 g of protein per day for children from 6 months to 3 years (India‐MOWCD, 2009), however, is much higher than the World Health Organization's (WHO) recommendations for the macro and micronutrient requirements from the food supplements. The WHO recommends that a breastfed infant in a developing country should receive about 200 kcal per day at 6–8 months of age, 300 kcal per day at 9–11 months, and 550 kcal per day at 12–23 months of age, from all complementary food and the remaining energy from breast milk (PAHO, 2003). The ICDS food supplements provide up to 81 percent of the total energy requirements for a 6–8‐month children and 73 percent for 9–11‐month‐old children, raising questions about the potential for this supplement to displace breastmilk. In this situation, therefore, the intervention exists in policy, but its effectiveness at supporting optimal IYCF practices is likely limited by its calorie‐heavy nutritional composition.
On implementation platforms to deliver counselling and CFS, two major national programs in India, the ICDS program under MWCD with nearly 2 million frontline workers (FLWs) and the National Health Mission (NHM) under MHFW with nearly 900,000 FLWs, are present across most of the country. These form the operational platforms to deliver counselling and CFS. The ICDS FLWs are responsible for delivery of CFS and individual and group counselling to mothers of young children on IYCF practices. The NHM FLWs are expected to provide counselling to mothers of children 0–3 months old. Although primary and supportive roles and responsibilities are outlined for these two cadres of FLWs in national‐level guidance documents (India–MoWCD, 2013b), clear guidelines are not available on how best to achieve full reach to mothers with children under 2 years of age through these two cadres of FLWs.
In addition, several programmatic experiences from India have used diverse approaches for implementing interventions to support IYCF (summarized in Table 4, drawing on detailed reviews in Avula, Kadiyala, Singh, & Menon, 2013). Several of the program models reviewed focused on improving breastfeeding (Table 4). Seventeen programs included interventions to support timely initiation of breastfeeding and exclusive breastfeeding and 15 programs on improving complementary feeding. Fifteen of the programs implemented complementary feeding interventions, but they focused only on timely initiation of complementary feeding. Only seven of the 15 programs promoted age‐appropriate quantity, quality, and safe handling of food.
Table 4.
Summary of program models that delivered infant and young child feeding (IYCF) counselling interventions in India (from Avula et al., 2013)
| Program | Implementer | Implementation states/time period | IYCF practices targeted | Approaches |
|---|---|---|---|---|
| Anchal Se Angan Tak (http://wcd.rajasthan.gov.in/wcdWeb/ASAT.pdf) | UNICEF, in collaboration with Integrated Child Development Services (ICDS) | Rajasthan 2001–2006 | IBF, EBF, ICF, and ACF | ‐Each member of a trained community group of local women adopted 15–20 households to communicate messages. |
| ‐Mass media, puppet shows, and street plays were used to reinforce the messages. | ||||
| ‐Program was monitored at the village and district levels using assessment, analysis, and action approach. | ||||
| Ankur Project (Mavalankar & Raman, n.d.) | Society for Education, Action, and Research in Community Health in collaboration with seven nongovernmental organizations | Maharashtra 2001–2005 | IBF | ‐Trained village health workers (VHWs) counseled mothers during periodic home visits. |
| ‐Meetings were conducted, and social functions were celebrated to raise community awareness. | ||||
| ‐Doctors/nurses supervised VHWs. | ||||
| Baby Friendly Community Health Initiative (Kushwaha, 2010) | Department of Paediatrics, B.R.D. Medical College, Gorakhpur, Uttar Pradesh, in collaboration with the Lalitpur district administration, government of Uttar Pradesh, and UNICEF | Uttar Pradesh2006–2007 | IBF, EBF, ICF, and ACF | ‐A mothers' support group (MSG) of frontline workers (FLWs) and active mothers from village were charged with counselling 10–15 households. |
| ‐ MSGs conducted home visits, held group discussions, and sensitized other community groups. | ||||
| Cell Phone Technology as Community‐Based Intervention (Patel et al., 2012) | Lata Medical Research Foundation | Maharashtra 2009 | IBF, EBF, and ICF | ‐Lactation counselors used mobile phones to provide breastfeeding information to mothers. |
| Community‐Based Maternal and Child Health and Nutrition Project (ORG Centre for Social Research, 2006). | Directorate of Health and Family Welfare of Uttar Pradesh in collaboration with the Directorate of ICDS of Uttar Pradesh, with technical and financial support from UNICEF | Uttar Pradesh 2001–2004 | IBF, EBF, and ICF | ‐Trained village‐level workers counseled during weekly home visits and coordinated with government FLWs. |
| ‐Information was provided in women's groups and village health committees and social functions. | ||||
| Community‐driven Nutrition Behavior Change Campaign for improved pregnant and infant feeding practices through community‐managed Nutrition cum Day Care Centers (Chava L.D. n.d.) | Society for Elimination of Rural Poverty | Andhra Pradesh 2007–present | IBF, EBF, ICF, and ACF | ‐Provide hot‐cooked food three times a day for pregnant and lactating women at the center |
| ‐During nutrition and health days, it was ensured that women attend sessions when government frontline workers provided nutrition and health information. | ||||
| Community Driven and Managed Health, Nutrition and Well‐Being Improvement Program (Sethi, n.d.) | Urban Health Resource Center provided technical support to the State Health and Family Welfare Department, government of Uttar Pradesh, and District Health Department | Uttar Pradesh Madhya Pradesh 005–present | IBF, EBF, ICF, and ACF | ‐Women's health groups were formed to generate awareness, demand for nutrition, and health services and serve as a community resource link to service providers. |
| ‐Women's groups conducted individual and group counselling along with community awareness activities to improve behaviors of pregnant women and to promote optimal child feeding practices. | ||||
| Safe Motherhood and Child Survival (SMCS) (Deepak Foundation, 2011). | Deepak Foundation in collaboration with the Department of Health and Family Welfare, Government of Gujarat | Gujarat (Tribal Vadodara) 2005–2010 | IBF, EBF, and ICF | ‐Deepak Foundation's staff initiated culturally acceptable activities such as generating of horoscopes to elicit community participation. Horoscopes were used to record child details at birth including initiation of breastfeeding, identify low‐birth weight babies and facilitate referrals. |
| ‐Coordination between the government FLWs was facilitated through interdepartmental meetings. | ||||
| ‐Community sensitization and involvement was facilitated through the village health and sanitation committees | ||||
| Community‐Led Initiatives for Child Survival (Garg et al., 2006) | Aga Khan Foundation in collaboration with the Department of Community Medicine, Mahatma Gandhi Institute of Medical Sciences | Maharashtra 2003–2008 | IBF, EBF, and ICF | ‐Adolescent peer educators counseled women on breastfeeding |
| ‐Community‐based events were held to raise awareness among local leaders, health care providers, and grandparents. | ||||
| Comprehensive Child Survival Program | Launched by the government of Uttar Pradesh and implemented by Catholic Relief Services and Mamta Health Institute for Mother and Child with technical assistance from the Vistaar Project | Uttar Pradesh 2008–2012 | IBF and EBF | ‐Trained government health FLWs counseled women. |
| ‐Trained facilitators worked with health FLWs to improve their knowledge and counselling techniques. | ||||
| ‐Job aids such as frequently asked questions, pictorial flip books, and checklists were developed for the frontline workers. | ||||
| Dular (IntraHealth 2007) | UNICEF, in collaboration with ICDS | Bihar; Jharkand 1999–2005 | IBF, EBF, and ICF | ‐Volunteers assisted government frontline workers in counselling mothers during home visits and spent time with families in teaching new practices. |
| ‐District and block coordination committees were created and trained. | ||||
| Home‐Based Neonatal Care (Bang et al., 2005) | Society for Education, Action, and Research in Community Health | Maharashtra 1993–1998 | IBF, EBF, and ICF | ‐Trained village health workers (VHWs) held group meetings on pregnancy, newborn care, and child feeding once every 4 months and followed‐up with home visits. |
| ‐Traditional birth attendants reinforced VHWs' messages. | ||||
| Kano Parbo Na (Mustaphi, 2005) | UNICEF, in collaboration with ICDS | West Bengal 2001–2005 | EBF, ICF, and ACF | ‐12‐day Nutritional Counselling and Childcare Sessions were organized at the anganwadi centers, where frontline workers trained mothers on infant feeding practices and mothers of well‐nourished children shared their infant feeding experiences. |
| ‐Village committees were formed to hold proactive dialogues between social groups and institutions. | ||||
| Maternal, Newborn and Child Health and Nutrition Practices in Select Districts of Uttar Pradesh and Jharkhand | Government of Uttar Pradesh and government of Jharkhand (Department of Health and Family Welfare and Department of Women and Child Development) with technical assistance from the Vistaar Project | Uttar Pradesh; Jharkhand 2007–2012 | IBF, EBF, ICF, and ACF | ‐Government FLWs were trained during regular monthly meetings and were given counselling guides and flip charts to counsel women. |
| ‐Convergence between the Department of Health and Family Welfare and the Department of Women and Child Development was facilitated through promotion of the use of data and joint reviews of village health and nutrition days. | ||||
| Mother and Child Care Program (Sri Ramkrishna Ashram., 2008). | Welthungerhilfe | West Bengal 2004–2008 | IBF, EBF, and ICF | ‐Awareness camps were organized in communities for mothers and mothers‐in‐law on child feeding. |
| Nutrition Security Innovations in Chhattisgarh (Mitanin Program) (Vir, 2012) | State Health Resource Center | Chhattisgarh 2001–2005 | IBF, EBF, and ICF | ‐Trained voluntary health workers (Mitanin) provided health information to families. |
| ‐Raised community awareness on government programs and entitlements. | ||||
| ‐Sensitized the local governing bodies on local health programs and implementation. | ||||
| Reproductive and Child Health, Nutrition and HIV/AIDS (Care n.d.) | CARE India, in collaboration with ICDS | 9 statesa 2001–2006 | IBF, EBF, ICF, and ACF | ‐Trained FLWs of the government programs and volunteers made home visits during critical periods and provided advice on health and nutrition practices |
| ‐Trained change agents worked with support of the FLWs and community organizations to promote child health and nutrition practices. | ||||
| Sure Start PATH (2012). | PATH | Maharashtra, Uttar Pradesh 2005–2012 | IBF and EBF | ‐Trained health workers communicated messages to women and family members during home visits. |
| ‐Community‐level activities were undertaken to create demand, strengthen linkages between the communities and the health systems |
Andhra Pradesh, Bihar, Chhattisgarh, Jharkhand, Madhya Pradesh, Odisha, Rajasthan, Uttar Pradesh, and West Bengal
Andhra Pradesh, Bihar, Gujarat, Rajasthan, Tamil Nadu, Jharkhand, Madhya Pradesh, Maharashtra, Odisha, Uttar Pradesh, West Bengal, and Chhattisgarh. IBF = initiation of breastfeeding; EBF = exclusive breastfeeding; ICF = introduction of complementary foods; ACF = age‐appropriate complementary feeding
Most programs to support breastfeeding implemented evidence‐based interventions (i.e., individual and/or group counselling to promote breastfeeding using lactation counselors, mothers' groups, village health workers, village health groups, and adolescent groups). The frequency and timing of visits for counselling and operational strategies varied among programs. For complementary feeding support, individual and/or group counselling or a combination of both was the most common intervention; however, one program provided food as well. In addition, some programs used community awareness raising activities (e.g., rallies, wall paintings, and folk media). Similar strategies (e.g., individual and group counselling and community support groups) were identified in a compendium of state success stories (UNICEF, 2013). The focus of the interventions was, again, mainly on the timely introduction of complementary foods (UNICEF, 2013). A more detailed description of intervention strategies used and the features of individual programs is available in Avula et al., 2013.
Among published efficacy and effectiveness studies, we identified 15 intervention studies in India that tested strategies to improve IYCF practices (Table 5). Nearly half of these studies were conducted as randomized‐controlled trials (Bhandari et al., 2001; Bhandari et al., 2004; Bhandari et al., 2005; Kumar et al., 2008; More et al., 2012; Vazir et al., 2013; Gami, Mishra, & Kocher, 2014); others were more mixed in their study design. Targeted IYCF practices in these studies included timely initiation, exclusive breastfeeding, different aspects of complementary feeding, and feeding during illness. The literature is most limited on studies on the impact and implementation of CFS interventions either alone or in combination with counselling.
Table 5.
Status of infant and young child feeding evidence in the peer‐reviewed literature from India
| Topic | Study design | Approaches | Outcomes |
|---|---|---|---|
| Timely initiation of breastfeeding | Kumar et al., 2008; Ahmad et al., 2012; Agrawal et al., 2012; More et al., 2012; Gami et al., 2014; Khan et al., 2013; Vir et al., 2013 | Timely initiation of breastfeeding was promoted through individual and group counselling by trained community health workers (Kumar et al., 2008), trained frontline workers (Agrawal et al., 2012), health staff (Ahmad et al., 2012; Gami et al., 2014), local educated women (More et al., 2012), and trained volunteers (Vir et al., 2013). Information was shared through distribution of educational materials for mothers and families (Khan et al., 2013). | Nearly all studies documented improvements in the initiation of breastfeeding (Khan et al., 2013; Kumar et al., 2008; Ahmad et al., 2012; Agrawal et al., 2012; Gami et al., 2014; Vir et al., 2013). More et al. (2012) did not find improvements in early initiation of breastfeeding. |
| Exclusive breastfeeding | Bhandari et al., 2005; Ahmad et al., 2012; More et al., 2012; Khan et al., 2013; Roy et al., 2013; Vir et al., 2013 | Exclusive breastfeeding was promoted through individual and group counselling by AWWs, ANMs, traditional birth attendants, physicians (Bhandari et al., 2005), health staff (Ahmad et al., 2012), local educated women (More et al., 2012), and trained volunteers (Vir et al., 2013). Information was shared through facilitated women's group meetings (Roy et al., 2013) and distribution of educational materials for mothers and families (Khan et al., 2013). | A majority of studies reported improvements in exclusive breastfeeding (Bhandari et al., 2005; Ahmad et al., 2012; Khan et al., 2013; Roy et al., 2013); and 3) underweight (Vir et al., 2013). Two studies (More et al., 2012; Vir et al. 2013) did not observe improvements in exclusive breastfeeding. |
| Complementary feeding | Bhandari et al., 2001; Sethi et al., 2003; Bhandari et al., 2004; Bhandari et al., 2005; Kilaru et al., 2005; Palwala et al., 2009; Vir et al., 2013; Vazir et al., 2013 | Advice on complementary feeding was given through individual and group counselling by trained workers (Sethi et al., 2003; Kilaru et al., 2005; Palwala et al., 2009), trained village women (Vazir et al., 2013), and physicians (Bhandari et al., 2005). In addition, community awareness‐raising activities such as songs and street plays and group discussions (Sethi et al., 2003) were conducted. | Studies documented improvements in complementary feeding practices including frequency of feeding (Sethi et al., 2003; Kilaru et al., 2005; Palwala et al., 2009), quantity of foods given (Sethi et al., 2003; Palwala et al., 2009; Vazir et al., 2013), and the quality of foods offered to children (Sethi et al., 2003; Bhandari et al., 2004; Bhandari et al., 2005; Kilaru et al., 2005; Palwala et al., 2009; Vazir et al., 2013). |
| Only one study (Bhandari et al., 2001) tested the impact of food supplements combined with nutrition education/behavior change communication. |
AWW = Anganwadi workers; ANM = auxiliary nurse midwives; EBF = exclusive breast feeding.
Eight studies implemented interventions to improve timely initiation of breastfeeding, prevent pre‐lacteal feeding, and promote colostrum feeding (Kumar et al., 2008; Agrawal et al., 2012; Ahmad, Sughra, Kalsoom, Imran, & Hadi, 2012; More et al., 2012; Khan, Khalique, Siddiqui, & Amir, 2013; Roy et al., 2013; Vir, 2013; Gami et al., 2014). Intervention approaches used in these studies included individual or home‐based counselling during antenatal visits or at tertiary‐care settings by trained FLWs including Anganwadi workers (AWW), auxiliary nurse midwives (ANM; Agrawal et al., 2012;), community volunteers (Vir, 2013), local educated women (More et al., 2012), and health staff (Gami et al., 2014). Information was shared during women's group meetings (Roy et al., 2013) and through distribution of information materials on neonatal care and breastfeeding practices (Khan et al., 2013). Six studies that aimed to improve exclusive breastfeeding also included individual and group counselling at routine contact points by multiple health workers such as AWWs, ANMs, traditional birth attendants, and physicians (Bhandari et al., 2005); health staff (Ahmad et al., 2012); local educated women (More et al., 2012); and trained volunteers (Vir, 2013). Information was shared during facilitated women's group meetings too (Roy et al., 2013).
We identified eight studies that tested interventions to improve complementary feeding practices (Bhandari et al., 2001; Sethi, Kashyap, & Seth, 2003; Bhandari et al., 2004; Bhandari et al., 2005; Kilaru, Griffiths, Ganapathy, & Shanti, 2005; Palwala et al., 2009; Vazir et al., 2013; Vir, 2013). Nearly all the studies used individual and group counselling as strategies, which was provided by trained workers (Sethi et al., 2003; Bhandari et al., 2004; Kilaru et al., 2005; Palwala et al., 2009) and trained village women (Vazir et al., 2013). In addition, community awareness‐raising activities, such as village rallies by children, school debates (Bhandari et al., 2004,) and group discussions (Sethi et al., 2003), were used to reinforce complementary feeding messages. Only one study tested the added value of a food supplement; in that study, a milk‐cereal supplement was provided along with nutrition counselling (Bhandari et al., 2001).
Summarizing implementation approaches identified in program experiences and in the published research literature in India, it appears that a major goal focus to date has been on early initiation of breastfeeding, exclusive breastfeeding, and initiation of complementary feeding. Program experiences covering other aspects of complementary feeding were severely limited at the time of preparing this review, as were research studies targeting the full spectrum of complementary feeding. The strategies tested via research studies and implemented in program models were similar and included counselling through multiple channels, community mobilization and awareness raising activities, food preparation techniques and demonstrations, and in just one case, the inclusion of food supplements.
Beyond the vision, delivery platforms, and implementation experiences, capacity and financing to deliver at scale are critical elements of scaling‐up. We did not do a detailed human resources assessment of capacity, but note that the program platforms have available frontline workers (usually one per village from the ICDS and the NHM). Capacity gaps are common in supervision, where there are substantial vacancies in many states (Raykar, Majumder, Laxminarayan, & Menon, 2015) in the health and the ICDS programs. Both the ICDS and the NHM have training guidelines, training materials, and training programs available that address different aspects of IYCF counselling, but these are not currently harmonized on content, or ensure role clarity among the FLWs. For CFS, capacity issues primarily pertain to ensuring quality, safety, and reach of the CFS. Different states in India use different production and distribution modalities (Vaid et al., 2017), and thus, capacity needs to ensure adequate supply, and reach to villages and households will differ by state.
Our review of implementation experiences and the published efficacy literature indicates that efforts to improve capacity were central to supporting the delivery of IYCF counselling interventions. Systems strengthening was a common feature of all these programs; strategies included recruiting new paid staff or volunteers, providing training and materials (such as checklists and flip charts) to assist in service delivery, community mobilization, and improving monitoring and supervision mechanisms. For example, in the Reproductive and Child Health, Nutrition and HIV/AIDS (RACHNA) program, volunteers were trained as change agents and worked with support of the ICDS FLWs to promote IYCF practices (CARE n.d.). All of the FLWs received quick reference guides, flip charts, and home‐visit planners to facilitate counselling. Additionally, the program was regularly reviewed, and the FLWs were supported through capacity building during review meetings and supportive supervision. In the Kano Parbo Na program (Mustaphi, 2005), new monitoring and surveillance tools such as mother and child protection cards, community growth charts, spreadsheet‐based ICDS monthly progress reports, and community service provider–level community mapping sheets were introduced to facilitate relevant data collection and monitoring at multiple levels. In the published literature as well, elements of capacity strengthening were central to achieving impact. Frontline worker training (Kumar et al., 2008), knowledge (Agrawal et al., 2012), strategically timed home visits (Kumar et al., 2008; Vir, 2013), and rapport and trust with the communities (Kumar et al., 2008) were critical for the success of the early initiation of breastfeeding interventions. On issues of capacity, therefore, we conclude that there is recognition of the need for capacity strengthening across the system to support the delivery of IYCF counselling interventions, especially, and that several program experiences exist to guide future direction in this regard. The challenges lie in the context of large‐scale government delivery platforms being able to integrate these capacity strengthening activities.
On financing, Menon and colleagues (2016) have estimated the cost needs for implementing counselling and delivering CFS at scale. Assessing the adequacy of financing is a challenge because current reporting of expenditures by the government preclude intervention‐specific adequacy assessments for counselling. For CFS, however, available expenditure estimates, based on several assumptions, suggest that current financing is inadequate, even under the government's current cost norms per child. Changing the composition, quality standards or production modalities for the CFS will all likely have cost implications that are currently not captured in available estimates.
The governance aspects of these two core interventions—IYCF counselling and CFS—in the context of India's programs pertain primarily to issues of transparency in the production and distribution of CFS. Our study does not tackle this issue directly, but several others have written about this (Saxena & Mander, 2011; Patnaik, 2012). The CFS component of the ICDS program has been fraught with governance and efficiency challenges. Large‐scale production modalities directly contravene the legal guidance from the Supreme Court of India to limit the role of contractors in the production of the CFS, a role that has been associated with high levels of corruption and poor quality CFS in some states (Commissioners to the supreme court of India, 2005). Our review of CFS production modalities (Vaid et al., 2017) highlights the different production modalities that exist across India; each of these modalities raises different governance issues. However, evidence of the safety, quality, acceptance, and nutritional impact of CFS produced via the decentralized modalities is limited despite evidence of high reach of the CFS in states such as Odisha and Chhattisgarh (India–MoWCD, 2015).
A recent network analysis of actors involved in supporting IYCF counselling (Puri et al., forthcoming) highlights the roles of two ministries (MWCD and MHFW), key development partners (UNICEF, notably), and the Breastfeeding Promotion Network of India (BPNI) as critical to support to actions for breastfeeding. The BPNI and UNICEF have both been active proponents of counselling interventions, and BPNI, in particular, has been actively engaged in advocacy around the regulation of marketing of the breastmilk substitutes. In case of CFS, the Right to Food Campaign and the Supreme Court have been the major catalysts in ensuring the universalization of the CFS. Individuals in the Right to Food network have also actively advocated for the universalization of the ICDS services including the CFS. Specifically, the filing of public interest litigations eventually led to the Supreme Court judgments mandating the universalization of the CFS component of the program and decentralized production and distribution models for the CFS.
Learning and evaluation is highlighted as a significant contributor to scaling‐up both in framework (Gillespie et al., 2015) and in successful examples of interventions operating at scale (Sanghvi et al., 2016). Our review of published literature and implementation experiences shows that there is more available evidence on the impact of counselling interventions for supporting timely initiation and exclusive breastfeeding and initiation of complementary feeding than on other aspects of complementary feeding and on the impact and use of CFS (Table 2). For example, nearly all of the studies we identified in the literature review reported improvements in timely initiation of breastfeeding among the intervention groups. Only one study (More et al., 2012) did not find significant improvements in the initiation of breastfeeding between the intervention and comparison groups. Four studies reported improvements in exclusive breastfeeding, whereas two studies (More et al., 2012; Vir, 2013) did not. Low intervention fidelity (More et al., 2012) and strong cultural beliefs (Vir, 2013) could have been the barriers to improving exclusive breastfeeding practices in these two studies.
Studies focused on complementary feeding varied in the types of outcomes they assessed (Table 5). Only one study assessed and found improvements in timely introduction of complementary foods (Vir, 2013). Six studies assessed and reported improvements in atleast one of the aspects of complementary feeding (i.e., frequency, quantity, and quality of foods offered; Table 5) (Sethi et al., 2003; Bhandari et al., 2004; Bhandari et al., 2005; Kilaru et al., 2005; Palwala et al., 2009; Vazir et al., 2013). Only one study tested the added value of a food supplement; in that study, a milk‐cereal supplement was provided along with nutrition counselling, and improvements were observed in energy intake (Bhandari et al., 2001). Although there was a counselling‐only comparison group, all the outcomes were compared with the group that received only visits and no counselling. Therefore, it is not possible to disentangle the added effects of a food supplement from those of counselling.
For the implementation experiences we reviewed, unfortunately, there is little rigorous evidence of impact for most programs. Of the 19 programs reviewed, eight programs only used an adequacy evaluation design, two used strong plausibility evaluation design (Care, n.d., and Bang, Bang, & Reddy, 2005), four used weak plausibility design (Anchal Se Angan Tak; Mustaphi, 2005; IntraHealth, 2007; Kushwaha, 2010), and eight had no documentation of evaluation design. Limited reporting of rigorous evaluations was observed in the cases showcased in Nutrition Moves (UNICEF, 2013).
Overall, although there have been several approaches used to deliver, or support the delivery of, IYCF counselling interventions, few have been evaluated carefully in India. Evidence and implementation experiences are extremely limited on improving diet diversity, on the impact of CFS, and on integrating complementary feeding counselling with CFS.
Finally, our assessments reveal limitations in the programmatic monitoring of the delivery of counselling interventions in both the ICDS and the NHM. The ICDS program has guidelines for monitoring counselling interventions during periodic supervision visits (India–MoWCD, 2010a). However, information on the delivery and coverage of counselling interventions is not included in the routine monthly progress reports of the ICDS. The delivery of CFS through the ICDS is included in the monthly progress reports along with other ICDS services (support to immunization and delivery of preschool education). In both cases, because monitoring is currently not denominator based, either for IYCF counselling or for CFS, it is challenging to accurately monitor the delivery and coverage of IYCF interventions.
4. DISCUSSION
We assessed India's readiness to implement two major IYCF interventions—counselling and the provision of CFS—using a framework for scaling‐up nutrition (Gillespie et al., 2015). On a positive note, we find that India has a vision for impact, multiple operational platforms for delivering interventions, and diverse positive catalysts for change including government, technical agencies, and the judiciary and civil society. Indian policies, to a great extent, are aligned with global technical guidance on IYCF and provide a vision for scaling‐up both counselling and CFS. All states in India include CFS in their programming, which is a highly visible aspect of programming for nutrition. There are, however, challenges in implementing these two interventions. In case of counselling, there is a lack of clear operational guidance and linked monitoring systems for delivering the intervention in addition to capacity gaps related to training and supervision. Furthermore, it is currently not possible to ascertain the adequacy of financing for counselling interventions. In case of CFS intervention, there is a need to revisit policies for CFS composition, production, and distribution to align more appropriately with infant nutritional needs. Although financing for CFS is available and has been increasing over time (Menon et al., 2016), financing gaps still exist that limit full coverage of the CFS. Overall, therefore, our assessment presents a mixed picture of readiness and points to clear areas for improvement.
On the policy front, there has been remarkable progress in evolution of policies to support IYCF, especially for counselling with India rapidly adopting global IYCF strategy directions. However, policy guidance on nutrient composition of the ICDS CFS needs to be reexamined against the WHO's recommendations (Vaid et al., 2017) and evolving changes in India. The early guidelines for the CFS, from the 1970s, were intended to close calorie and protein gaps for a broad age range of children covered under the ICDS. They were developed prior to the emergence of scientific knowledge on the specific nutrient needs for infants and young children (Dewey & Brown, 2003; PAHO, 2003). In the context of the known contributions of breastmilk and complementary foods to infant nutrition, the current CFS guidelines should be revisited. For instance, the high caloric content of the current CFS, along with low nutrient density, suggests that these supplements have the potential to displace breast milk and contribute to poor diet quality. There is an urgent need to revisit, refine, and align the food supplementation guidance strongly with child nutrient needs.
On the operational front, nutrition counselling is one of the least‐focused activities in the ICDS (Gragnolati, Bredenkamp, Gupta, Lee, & Shekar, 2006) and a service for which there is least awareness within the community (India–MoWCD, 2015). Furthermore, there are multiple FLWs (AWWS, ASHAs, and ANMs) assigned with counselling roles. Assuring this role clarity and operational guidance is especially important in an environment where FLWs often have to coordinate multiple activities and deliver multiple interventions to their client populations (Avula et al., 2015), along with content harmonization of IYCF messages between the two ministries implementing the counselling interventions. Our review of implementation experiences highlights that although several operational models for program delivery exist for IYCF counselling, most of them have focused on improving initiation of complementary feeding rather than on the full spectrum of age‐appropriate complementary feeding. Looking forward, specific attention is needed to develop models that can support behaviors related to dietary diversity.
Although, the results of our review of the implementation experiences were limited by the availability of documentation on programs, the ones included cover major program initiatives. Some of the implementation experiences, despite limited evaluations, have informed program and policy decisions and have been incorporated into current programs. For example, ICDS FLW home‐visit planners were modified based on the experiences of RACHNA program (CARE n.d.) to guide timely home visits for counselling by FLWs. At the same time, new implementation experiences are emerging where self‐help groups (Rao, Gray, Metcalfe, & Dutta, 2014) and IYCF counselling centers (Dar, Jha, Sinha, Singh, & Kumar, 2015) are being used to promote appropriate IYCF practices. Such models must be systematically documented and rigorously tested to generate evidence of impact on IYCF practices.
In case of the CFS intervention, it is difficult to ascertain the extent to which counselling approaches have integrated counselling about complementary feeding with appropriate use of the CFS that is distributed alongside. CFS are intended to be added to the daily diet of the children, which in the absence of a strong behavior change communication is likely to lead to inefficiencies in utilizing the food supplement for children or help improve feeding practices. For example, nearly 52% of the mothers reported sharing the food supplements distributed for children under 3 years with other siblings or family members (India–MoWCD, 2015). Furthermore, as communities are well aware of their CFS entitlements, it is likely that irregularities in the distribution of CFS (e.g., poor quality and inadequate quantity) could influence communications between AWWs and families, thus limiting the effectiveness of the counselling intervention. This calls for improving governance around CFS, including plugging production and distribution leakages, and ensuring of quality CFS.
Despite accounting for 25 percent of the total cost required to deliver a full set of nutrition‐specific interventions in India (Chakrabarti & Menon, 2016), the CFS reach less than 50% of children under 3 years (India–MoWCD, 2015). In recent years, program approaches for production and delivery of CFS have expanded, but there is inadequate information on the frequency of distribution, content, and quality of the ICDS food supplements distributed within each of the states, rendering it difficult to assess if the states are meeting the national guidelines (Vaid et al., 2017). There remains a high interstate variability in the implementation and reach of the CFS (India–MoWCD, 2015). Irregular supply and sharing of the product remain to be the barriers to achieving full coverage and use of the CFS (Leyvraz et al., 2016). Given the mandate to universalize the CFS, economic and operational costs, and programmatic gaps in the ICDS, it is imperative to examine the contribution of the food supplementation to the complementary feeding practices in the context of India and its use at the household level.
There appears to be adequate scientific evidence from India to support implementation of counselling‐based IYCF interventions but limited evidence base on the impact of nutrition education combined with CFS. In addition, despite the existence of global evidence, none of the studies in India examined nutrition education combined with a cash transfer.
5. CONCLUSIONS
This study strengthens our understanding of an enabling context for scaling‐up counselling and CFS interventions in India. A strong stated policy intent, program guidance, and the availability of frontline workers can support India to realize the vision of delivering both counselling and CFS interventions at scale. Capacity, finance, and governance challenges, however, continue to limit full coverage of these IYCF interventions. Evidence gaps need to be closed to test specific aspects of counselling and CFS intervention, along with investments in program evaluations, financing research, and strengthening of governance, to support the scale‐up of high‐impact interventions to improve IYCF in India.
SOURCE OF FUNDING
Funding was provided by the Bill & Melinda Gates Foundation, through Partnerships and Opportunities to Strengthen and Harmonize Actions for Nutrition in India (POSHAN), managed by the International Food Policy Research Institute.
CONFLICTS OF INTEREST
Authors declare no conflict of interest.
CONTRIBUTIONS
R. A. and V. O. drafted the manuscript; P. M. guided the development of the manuscript, reviewed, and revised it. S. K. reviewed and revised the manuscript. R. A. revised and finalized the manuscript.
ACKNOWLEDGEMENTS
The authors are thankful to the editors and the anonymous reviewers for helpful suggestions and comments. The authors also acknowledge Kavita Singh for her help with the initial literature and program reviews.
Avula R, Oddo, VM , Kadiyala S, Menon P. Scaling‐up interventions to improve infant and young child feeding in India: What will it take? Matern Child Nutr. 2017;13(S2):e12414 10.1111/mcn.12414
REFERENCES
- Agrawal, P. K. , Agrawal, S. , Ahmed, S. , Darmstadt, G. L. , Williams, E. K. , Rosen, H. , … Baqui, A. H. (2012). Effect of knowledge of community health workers on essential newborn health care: A study from rural India. Health Policy and Planning 27, 115–126. 10.1093/heapol/czr018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad, M. O. , Sughra, U. , Kalsoom, U. , Imran, M. , & Hadi, U. (2012). Effect of antenatal counselling on exclusive breastfeeding. Journal of Ayub Medical College Abbottabad, 24, 116–119. [PubMed] [Google Scholar]
- Anchal Se Angan Tak . Promoting integrated early child development . Retrieved from http://wcd.rajasthan.gov.in/wcdWeb/ASAT.pdf (Accessed on October 14, 2016)
- Avula, R. , Kadiyala, S. , Singh, K. , & Menon, P. (2013). The operational evidence base for delivering direct nutrition interventions in India In IFPRI Discussion Paper 01299). Washington, DC, USA: International Food Policy Research Institute. [Google Scholar]
- Avula, R. , Kim, S. S. , Chakrabarti, S. , Tyagi, P. , Kohli, N. , Kadiyala, S. , & Menon, P. (2015). Delivering for nutrition in Odisha: Insights from a study on the state of essential nutrition interventions In POSHAN report no 7). New Delhi: International Food Policy Research Institute. [Google Scholar]
- Bang, A. T. , Bang, R. A. , & Reddy, H. M. (2005). Home‐based neonatal care: Summary and applications of the field trial in Rural Gadchiroli, India (1993 to 2003). Journal of Perinatology, 25, S3–S10. 10.1038/sj.jp.7211267 [DOI] [PubMed] [Google Scholar]
- Bhandari, N. , Bahl, R. , Nayyar, B. , Khokhar, P. , Rohde, J. E. , & Bhan, M. K. (2001). Food supplementation with encouragement to feed it to infants from 4 to 12 months of age has a small impact on weight gain. Journal of Nutrition, 131, 1946–1951. [DOI] [PubMed] [Google Scholar]
- Bhandari, N. , Mazumder, S. , Bahl, R. , Martines, J. , Black, R. E. , & Bhan, M. K. (2005). Use of multiple opportunities for improving feeding practices in under‐twos within child health programmes. Health Policy and Planning, 20, 328–336. 10.1093/heapol/czi039 [DOI] [PubMed] [Google Scholar]
- Bhandari, N. , Mazumder, S. , Bahl, R. , Martines, J. , Black, R. E. , & Bhan, M. K. (2004). An educational intervention to promote appropriate complementary feeding practices and physical growth in infants and young children in rural Haryana, India. Journal of Nutrition, 134, 2342–2348. [DOI] [PubMed] [Google Scholar]
- Bhutta, Z. A. , Ahmed, T. , Black, R. E. , Cousens, S. , Dewey, K. , Giugliani, E. , … Shekar, M. (2008). What works? Interventions for maternal and child undernutrition and survival. The Lancet, 371, 417–440. [DOI] [PubMed] [Google Scholar]
- Bhutta, Z. A. , Das, J. K. , Rizvi, A. , Gaffey, M. F. , Walker, N. , Horton, S. , … Black, R. E. (2013). Evidence‐based interventions for improvement of maternal and child nutrition: What can be done and at what cost? The Lancet, 382, 452–477. [DOI] [PubMed] [Google Scholar]
- CARE . (n.d). What rachna has done so far: Program description. rachna 2001‐2006. Women and child health at scale. Working Paper Series. Paper 1.
- Chakrabarti, S. , & Menon, P. (2016). Budgeting to deliver for nutrition: Reflections from a costing study on nutrition specific interventions in India. Budget Track, 11, 54–59. [Google Scholar]
- Chava, L. D. (n.d). Community‐driven nutrition behavior change campaign for improved pregnant and infant feeding practices through community‐managed Nutrition cum Day Care Centers (NDCCs).
- Commissioners to the supreme court of India . 2005. Sixth report of the commissioners to the supreme court of India.
- Dar, S. , Jha R., Sinha S., Singh B. B., and Kumar G.. 2015. Implementing IYCF Counselling Centers in Bihar. POSHAN Implementation Note No. 11. New Delhi: International Food Policy Research Institute
- Deepak Foundation . (2011). Safe motherhood and child survival (SMCS).
- Dewey, K. G. , & Brown, K. H. (2003). Food and Nutrition Bulletin, 24(1), 5–28. [DOI] [PubMed] [Google Scholar]
- Dyson, L. , McCormick, F. , & Renfrew, M. J. (2006). Interventions for promoting the initiation of breastfeeding. Evidence‐Based Child Health: A Cochrane Review Journal, 1, 592–616. [DOI] [PubMed] [Google Scholar]
- Gami, N. , Mishra, A. , & Kocher, S. (2014). To Study the effect of counselling on early initiation of breast feeding in the first hour of life. Global Journal of Medical Research, 13, 17–24. [Google Scholar]
- Garg, B. S. , Gupta, S. S. , Datta, S. S. , Boratne, A. , Chaudhuri M., Gandhi A. (2006). Community led initiatives for child survival program (CLICS).
- Gillespie, S. , Menon, P. , & Kennedy, A. L. (2015). Scaling up impact on nutrition: What will it take? Advances in Nutrition, (Bethesda, Md.)6(4), 440–451. 10.3945/an.115.008276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gragnolati, M. , Bredenkamp, C. , Gupta, M. D. , Lee, Y. K. , & Shekar, M. (2006). ICDS and persistent undernutrition: Strategies to enhance the impact. Economic and Political Weekly, 1193–1201. [Google Scholar]
- Habicht, J. P. , Victora, C. G. , & Vaughan, J. P. (1999). Evaluation designs for adequacy, plausibility and probability of public health programme performance and impact. International Journal of Epidemiology, 28, 10–18. [DOI] [PubMed] [Google Scholar]
- Imdad, A. , Yakoob, M. Y. , & Bhutta, Z. A. (2011). Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health, 11, S3–S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- India Ministry of Health and Family Welfare (MoHFW) . (2007). Health nutrition day: Guidelines for AWWs/ASHAs/ANMs/PRIs. Available at: http://www.nrhmmeghalaya.nic.in/guidelines/VHND_Guidelines.pdf (Accessed 6 April 2016).
- India Ministry of Health and Family Welfare (MoHFW) . (2013). Guidelines for enhancing optimal infant and young child feeding practices. Available at: http://www.nrhmorissa.gov.in/writereaddata/Upload/Documents/Guideline%20-%20IYCF.pdf (Accessed 6 April 2016).
- India Ministry of Human Resource Development (MHRD) . (1993). National nutrition policy. Available at: http://wcd.nic.in/fnb/fnb/Publications/FNB%20Booklets/National%20Nutrition%20Policy.pdf (Accessed 6 April 2016).
- India Ministry of Women and Child Development (MoWCD) . (1995). National plan of action on nutrition. Available at: http://www.wcd.nic.in/fnb/fnb/Publications/FNB%20Booklets/national%20Plan%20of%20Action.pdf (Accessed 6 April 2016).
- India Ministry of Women and Child Development (MoWCD) . (2005). National plan of action for children. Available at: http://www.childlineindia.org.in/National-Plan-of-Action-2005.htm (Accessed 6 April 2016).
- India Ministry of Women and Child Development (MoWCD) . (2009). Revised nutritional and feeding norms for supplementary nutrition in ICDS scheme. Available at: http://wcd.nic.in/sites/default/files/AR2009-10.pdf (Accessed 6 April 2016).
- India Ministry of Women and Child Development (MoWCD) . (2010a). Guidelines for monitoring and supervision visits to ICDS blocks and AWCs by officials of the state and central governments. Available at: http://icds-wcd.nic.in/icds/guide/GuidelinesICDSM&E.pdf (Accessed 6 April 2016).
- India Ministry of Women and Child Development (MoWCD) . (2010b). Roles and responsibilities of AWWs. Available at: http://icds-wcd.nic.in/icdsimg/RoleresponseAWWs.pdf Accessed 6 April 2016).
- India Ministry of Women and Child Development (MoWCD) . (2011). Integrated child development services (ICDS) scheme: Framework for development of the State Annual Programme Implementation Plans (APIPs). Available at: http://icds-wcd.nic.in/frameworkapip.pdf (Accessed 6 April 2016).
- India Ministry of Women and Child Development (MoWCD) . (2013a). National policy for children. Available at: http://wcd.nic.in/sites/default/files/npcenglish08072013_0.pdf (Accessed 6 April 2016).
- India Ministry of Women and Child Development (MoWCD) . (2013b). Roles delineation for Frontline workers. A Framework for Convergence of Health & ICDS.
- India Ministry of Women and Child Development (MoWCD) . (2015). Rapid survey on children. http://wcd.nic.in/sites/default/files/India%20fact%20sheet.pdf
- India Ministry of Women and Child Development/Food and Nutrition Board (MoWCD/FNB) . (2006). National guidelines on infant and young child feeding. Available at: http://wcd.nic.in/sites/default/files/infantandyoungchildfeed.pdf (Accessed 6 April 2016).
- International Food Policy Research Institute (2014). Global nutrition report 2014: Actions and accountability to accelerate the world's progress on nutrition. Washington, DC: International Food Policy Research Institute. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IntraHealth International . (2007). Evidence review on complementary feeding. Dular Program.
- IntraHealth International . (2008). Evidence review briefs from the Vistaar project. Available at: http://www.intrahealth.org/page/vistaar-publications#erb (Accessed 6 April 2016).
- International Institute for Population Sciences (IIPS) and Macro International (2007). National Family Health Survey (NFHS‐3), 2005–06: India: Volume I. Mumbai: IIPS. [Google Scholar]
- Khan, A. M. , Kayina, P. , Agrawal, P. , Gupta, A. , & Kannan, A. T. (2012). A study on infant and young child feeding practices among mothers attending an urban health center in East Delhi. Indian Journal of Public Health, 56(4), 301. [DOI] [PubMed] [Google Scholar]
- Khan, M. H. , Khalique, N. , Siddiqui, A. R. , & Amir, A. (2013). Impact of behavior change communication among pregnant women regarding neonatal care. Indian Journal of Public Health, 80, 804–808. [DOI] [PubMed] [Google Scholar]
- Kilaru, A. , Griffiths, P. , Ganapathy, S. , & Shanti, G. (2005). Community‐based nutrition education for improving infant growth in rural Karnataka. Indian Pediatrics, 42, 425. [PubMed] [Google Scholar]
- Kumar, V. , Mohanty, S. , Kumar, A. , Misra, R. P. , Santosham, M. , Awasthi, S. , … Darmstadt, G. L. (2008). Effect of community‐based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: A cluster‐randomized controlled trial. Lancet, 372, 1151–1162. 10.1016/S0140-6736(08)61483-X [DOI] [PubMed] [Google Scholar]
- Kushwaha, K. P. (2010). Universalising delivery of nutrition interventions in district Lalitpur, Uttar Pradesh.
- Lewin, S. , Munabi‐Babigumira, S. , Glenton, C. , Daniels, K. , Bosch‐Capblanch, X. , & van Wyk, B. E. (2010). Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Systematic Review, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyvraz, M. , Wirth, J. P. , Woodruff, B. A. , Sankar, R. , Sodani, P. R. , Sharma, N. D. , & Aaron, G. J. (2016). High coverage and utilization of fortified take‐home rations among children 6–35 months of age provided through the Integrated Child Development Services Program: Findings from a cross‐sectional survey in Telangana, India. PLOSOne, 10.1371/journal.pone.0160814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmood, S. E. , Srivastava, A. , Shrotriya, V. P. , & Mishra, P. (2012). Infant feeding practices in the rural population of north India. Journal of Family & Community Medicine, 19, 130–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mavalankar, D. , Raman, P. (n.d). ANKUR Project. A case study of replication of home based newborn care.
- Menon, P. , McDonald, C. M. , & Chakabarti, S. (2016). Estimating the cost of delivering direct nutrition interventions at scale: national and subnational level insights from India. Maternal & Child Nutrition, 12(Suppl S1), 169–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meshram, I. , Kodavanti, M. , Chitty, G. , Manchala, R. , Kumar, S. , Kakani, S. K. , … Narsimhachary Veera, B. G. (2013). Influence of feeding practices and associated factors on the nutritional status of infants in rural areas of Madhya Pradesh State, India. Asia‐Pacific Journal of Public Health, 27, NP1345–NP1361. 10.1177/1010539513486174 [DOI] [PubMed] [Google Scholar]
- Meshram, I. , Laxmaiah, A. , Venkaiah, K. , & Brahmam, G. (2012). Impact of feeding and breastfeeding practices on the nutritional status of infants in a district of Andhra Pradesh, India. The National Medical Journal of India, 25, 201–206. [PubMed] [Google Scholar]
- Micronutrient Initiative . (2007). Review of “Best Practices” in ICDS: A study conducted for the World Bank. Micronutrient initiative: New Delhi, India. http://wcd.nic.in/issnip/ICDSBESTPRACTICESREVIEWMay2007.pdf
- More, N. S. , Bapat, U. , Das, S. , Alcock, G. , Patil, S. , Porel, M. , … Osrin, D. (2012). Community mobilization in Mumbai slums to improve perinatal care and outcomes: A cluster randomized controlled trial. PLoS Medicine, 9 10.1371/journal.pmed.1001257.e1001257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustaphi, P. (2005). Addressing malnutrition through surveillance and innovative community based strategies. [Google Scholar]
- ORG Centre for Social Research . (2006). Community based maternal & child health nutrition (MCHN) project. [Google Scholar]
- Palwala, M. , Sharma, S. , Udipi, S. A. , Ghugre, P. S. , Kothari, G. , & Sawardekar, P. (2009). Nutritional quality of diets fed to young children in urban slums can be improved by intensive nutrition education. Food & Nutrition Bulletin, 30, 317–326. [DOI] [PubMed] [Google Scholar]
- Pan American Health Organization . (2003). Guiding principles for complementary feeding of breastfed child. Available at: http://www.who.int/nutrition/publications/guiding_principles_compfeeding_breastfed.pdf (Accessed 6 April 2016).
- Patel, A. , Dhande, L. , Sengupta, N. , Umarkar, S. , Pusdekar, Y. , Adware, Ap ., … Borkar, J. (2012). Evaluation of the effectiveness of cell phone technology as community based intervention to improve exclusive breast feeding & reduce infant morbidity rates.
- PATH . (2012). Sure start. www.path.org
- Patnaik B. 2012. Report by principal advisors on Maharashtra contractors in ICDS. http://www.righttofoodindia.org/data/commissioners/November_2012_report_principal_advisor_maharashtra_contractor_icds_31_october_2012.pdf
- Puri, S. , Fernandez, S. , Puranik, A. , Anand, A. , Gaidhane, A. , Zahiruddin, Q.S. , Patel, A. , Uddin, S ., Thow, A. M. (forthcoming). Policy content and stakeholder network analysis for infant and young child feeding in India. [DOI] [PMC free article] [PubMed]
- Rao, S. , Gray, B. , Metcalfe, M. , & Dutta, S . (2014). Leveraging the power of women's groups and financial services to improve knowledge and behaviors for improved child and maternal nutrition. POSHAN Implementation Note 4. New Delhi: International Food Policy Research Institute.
- Raykar, N. , Majumder, M. , Laxminarayan, R. , & Menon, P. (2015). India health report: Nutrition 2015. New Delhi, India: Public Health Foundation of India. [Google Scholar]
- Roy, S. S. , Mahapatra, R. , Rath, S. , Bajpai, A. , Singh, V. , & Nair, N. (2013). Improved neonatal survival after participatory learning and action with women's groups: A prospective study in rural eastern India. Bulletin of the World Health Organization, 91, 426–433. 10.2471/BLT.12.105171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanghvi, T. , Haque, R. , Roy, S. , Afsana, K. , Seidel, R. , Islam, S. , … Baker, J. (2016). Achieving behaviour change at scale: Alive & Thrive's infant and young child feeding programme in Bangladesh. Maternal & child nutrition, 12(S1), 141–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxena, N. C. , & Mander, H. (2011). Issues in the implementation of ICDS in India (Letter to Secretary, Ministry of Women and Child Development from the Commissioners to the Supreme Court in the Right to Food Case. http://www.righttofoodindia.org/data/icds/March_2012_letter_to_secretary_women_and_child_development_sc_commissioners_7_february_2012.pdf
- Supreme Court of India . Civil original jurisdiction. Writ Petition (C) No. 196 of 2001. http://icds-wcd.nic.in/icds/affidivticds.htm
- Sethi, M. V. Community driven & managed health, nutrition & well‐being improvement programme in Agra city (Uttar Pradesh)
- Sethi, M. V. , Kashyap, S. , & Seth, V. (2003). Effect of nutrition education of mothers on infant feeding practices. The Indian Journal of Pediatrics, 70, 463–466. [DOI] [PubMed] [Google Scholar]
- Singhal, P. , Garg, S. , Chopra, H. , Jain, S. , Bajpai, S. , & Kumar, A. (2013). Status of infant and young child feeding practices with special emphasis on breast feeding in an urban area of Meerut. IOSR Journal of Dental and Medical Sciences, 7, 7–11. [Google Scholar]
- Sri Ramkrishna Ashram . (2008). Final report of mother and child care programme.
- United Nations Children's Fund (2013). Nutrition moves. States create promising change in India. New Delhi, India: United Nations Children's Fund. [Google Scholar]
- Vaid, A. , Avula, R. , George, N. R. , John, A. , & Menon, P. (2017). A Review of the Integrated Child Development Services' Supplementary Nutrition Program: Take Home Ration for Children. POSHAN Research Note #7. New Delhi, India: International Food Policy Research Institute. [Google Scholar]
- Vazir, S. , Engle, P. , Balakrishna, N. , Griffiths, P. L. , Johnson, S. L. , & Creed‐Kanashiro, H. (2013). Cluster‐randomized trial on complementary and responsive feeding education to caregivers found improved dietary intake, growth and development among rural Indian toddlers. Maternal & Child Nutrition, 9, 99–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vir, S. , Sreenath, K. C. , Bose, K. , Chauhan, K. , Mathur, S. , & Menon, S. (2014). National policies and strategic plans to tackle undernutrition in India: A review. International Food Policy Research Institute: New Delhi. [Google Scholar]
- Vir, S. (2012). Mitanin initiative and Nutrition Security Innovation (NSI) Chhattisgarh State, India—An evaluation.
- Vir, S. (2013). Community based maternal and child health nutrition project, Uttar Pradesh: An innovative strategy focusing on “at risk” families. Indian Journal of Community Medicine, 38, 234–239. 10.4103/0970-0218.120159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Braun, J. , Swaminathan, M. , & Rosegrant, M. (2004). Agriculture, food security, nutrition and the millennium development goals. Washington DC: International Food Policy Research Institute. [Google Scholar]
- World Health Organization (2010). Indicators for assessing infant and young child feeding practices. Part II: Available at: http://www.who.int/maternal_child_adolescent/documents/9789241599290/en/ Measurement; (Accessed 6 April 2016). [Google Scholar]
- World Health Organization . (2014). Global nutrition targets 2025 Available at: http://www.who.int/nutrition/publications/globaltargets2025_policybrief_overview/en/ (Accessed 6 April 2016).


