Abstract
Few trials have shown that promoting complementary feeding among young children is effective in improving child linear growth in resource‐challenged settings. We designed a community‐based participatory nutrition promotion (CPNP) programme adapting a Positive Deviance/Hearth approach that engaged mothers in 2‐week nutrition sessions using the principles of ‘learning by doing’ around child feeding. We aimed to test the effectiveness of the CPNP for improving child growth in rural Ethiopia. A cluster randomized trial was implemented by adding the CPNP to the existing government nutrition programmes (six clusters) vs. government programmes only (six clusters). A total of 1790 children aged 6 to 12 months (876 in the intervention and 914 in the control areas) were enrolled and assessed on anthropometry every 3 months for a year. Multi‐level mixed‐effect regression analysis of longitudinal outcome data (n = 1475) examined the programme impact on growth, adjusting for clustering and enrollment characteristics. Compared with children 6 to 24 months of age in the control area, those in the intervention area had a greater increase in z scores for length‐for‐age [difference (diff): 0.021 z score/month, 95% CI: 0.008, 0.034] and weight‐for‐length (diff: 0.042 z score/month, 95% CI: 0.024, 0.059). At the end of the 12‐month follow‐up, children in the intervention area showed an 8.1% (P = 0.02) and 6.3% (P = 0.046) lower prevalence of stunting and underweight, respectively, after controlling for differences in the prevalence at enrollment, compared with the control group. A novel CPNP programme was effective in improving child growth and reducing undernutrition in this setting. © 2016 John Wiley & Sons Ltd
Keywords: community‐based participatory nutrition promotion, effectiveness evaluation, childhood stunting, cluster randomized trial, complementary feeding practices, Ethiopia
Introduction
Undernutrition is associated with deaths by preventable diseases in early childhood and with long‐term adverse consequences in later life (Victora et al. 2008). The period of 1000 days from conception to 24 months of age is recognized as the most effective intervention period to mitigate the adverse effects of undernutrition, thus nutrition interventions focus on this period (Bhutta et al. 2013). Enhancing optimal complementary feeding among young children has been shown to be effective in improving child linear growth in underdeveloped settings (Imdad et al. 2011; Bhutta et al. 2013; Lassi et al. 2013). Such strategies have featured multi‐dimensional behavioural change communication activities, including the development of locally acceptable and affordable recipes, intensive group education or individual counselling, use of mass media, involvement of community groups and health care workers, all largely embedded within existing health services (Penny et al. 2005; Shi et al. 2010; Vazir et al. 2013; Lassi et al. 2014).
Ethiopia has a high public health burden of child undernutrition and micronutrient deficiencies: 40.4% of children under 5 years of age are stunted [length/height‐for‐age z score (LAZ/HAZ) < −2], 8.7% are wasted [weight‐for‐length/height z score (WLZ/WHZ) < −2] (Central Statistical Agency, Government of Ethiopia 2014) and ~40% have anaemia with haemoglobin levels below 11.0 g/dL (Central Statistical Agency, Government of Ethiopia, & ICF International 2012). Despite notable improvements in child nutrition in the past two decades, the current nutritional situation in Ethiopia still calls for more effective, contextualized and sustainable intervention strategies that are in line with Ethiopia's National Nutrition Programme (Government of Ethiopia 2013).
In Ethiopia, two types of community‐based nutrition programmes are operational in poor rural districts: the Essential Nutrition Action (ENA) programme and the Community‐based Management of Acute Malnutrition (CMAM) programme. The ENA framework has its focus on improving breastfeeding, complementary feeding and micronutrient deficiencies, and has had positive results (Jennings & Hirbaye 2008; USAID 2008). Despite the achievements of the ENA implementation at the regional level, poor monitoring system and weak capacity of community volunteers (e.g. knowledge and counselling skills) in the ENA framework were often obstacles in addressing undernutrition in some local contexts (Jennings & Hirbaye 2008). The CMAM programme, on the other hand – although promising in treating severe wasting with ready‐to‐use therapeutic foods (Lenters et al. 2013; Deconinck et al. 2008) – has had no prevention programme components and depends entirely on external funding to purchase therapeutic or supplementary foods (UNICEF 2012).
To address the gaps mentioned earlier in the ENA and CMAM programmes, a new programme model – which we refer to in our study as ‘community‐based participatory nutrition promotion (CPNP)’ – was designed by World Vision (WV) Korea and WV Ethiopia. The CPNP, in part adopting a positive deviance theory (Zeitlin et al. 1990), was designed for scale implementation to promote caregivers' behaviour change at household levels and to strengthen community participation and programme ownership. Thus, we hypothesized that this new programme added to the ENA and CMAM programmes – would be more effective in promoting appropriate complementary feeding and hygiene among caregivers thereby improving the growth of children 6 to 24 months of age and reducing child undernutrition. We tested this hypothesis in a cluster randomized effectiveness trial described in this paper. This trial was registered at Current Controlled Trials as ISRCTN 89206590.
Key messages.
Given the high prevalence of undernutrition among young children in Ethiopia, more sustainable and effective nutrition intervention strategies are needed.
A community‐based participatory nutrition programme – which adopted a PD/Hearth approach and was added to existing government programmes – could successfully improve child growth in rural Ethiopia.
This intervention approach is expected to strengthen community health systems and complement the activities of Ethiopia's National Nutrition Programme.
Participants and methods
Study settings
This study was conducted in the Habro and the Melka Bello districts, which represented typical rural Eastern Ethiopian communities with limited development and dependence on mixed crop agriculture and livestock rearing. All 29 rural Kebeles (the smallest administrative unit) in Habro and 20 of 22 rural Kebeles in Melka Bello belonged to the study area. In 2012, the total population of the study area was estimated to be 187 426 in Habro district and 163 287 in Melka Bello district (Population Census Commission, Government of Ethiopia 2008). The study Kebeles had an estimated average total population of 6300 and 416 children 0–24 months of age.
Study design, hypothesis and sample size
This study was designed as a community‐based cluster randomized trial, which evaluated the effectiveness of the CPNP programme added to the existing ENA and CMAM programmes on child nutritional status, compared with the existing programmes only. Because the CPNP programme was publicly implemented in the community, the programme was expected to impact not only enrolled participants but also their neighbours, who may have either observed the CPNP programme or learned about it indirectly from the participants. Furthermore, each individual had a different time point of participation to the CPNP programme that could not be known at the time of enrollment in this trial. For this reason, all children 6 to 12 months of age residing in the two districts were eligible for this study. The main outcomes were monthly change in LAZ, weight‐for‐age (WAZ) and WLZ scores from 6 to 24 months of age, and absolute risk differences in prevalences of stunting (LAZ < −2), underweight (WAZ < −2) and wasting (WLZ < −2) at a 12‐month follow‐up. We hypothesized that, compared with children in the control area, children living in the intervention area would present 0.2 greater mean LAZ scores at the end of a year follow‐up. A total of 2064 children (n = 1032 per group) were required to identify an increase of a 0.2 LAZ in 18–24 months of age children based on an expectation of a −1.7 z score in the control area, accepting a type I (α) error of 5%, power at 0.80, number of clusters at 12, average cluster size at 172, loss to follow‐up at 10% and standard deviation of 0.9 z score (Dupont & Plummer 1998). There was no available intra‐cluster correlation coefficient information for anthropometric indicators in the study area, so we assumed an intra‐cluster correlation coefficient of 0.054, which was estimated based on data from the Demographic and Health Survey reports in 46 developing countries in another study (Fenn et al. 2004).
Randomization
We could have a total of 12 clusters for this cluster randomized trial. The number of clusters was determined by feasibility in intervention operation in the study area. All 49 Kebeles in the Habro and Melka Bello districts were first ranked according to the level of socio‐economic condition assessed by the qualitative information of agricultural officers of WV Ethiopia and local governments. Two to six nearby Kebeles that were presumed to share similar socio‐economic living environments were grouped into a cluster, with a total of 12 clusters, six per district. Each cluster was matched to another cluster in the same district based on the similarity of agricultural and wealth information.
Intervention allocation was decided by tossing a coin in the presence of the local authorities; one cluster was randomly decided as an intervention area, and the paired cluster automatically became a control area. Intervention allocation was not blinded among study subjects and community members because of the public nature of the intervention. Borders between the control and the intervention areas were adjacent.
Interventions
In Afan Oromo language, the CPNP was called ‘Sagantaa Shuuro’, which meant ‘Complementary feeding programme’. Some programme elements, such as the 2‐week group nutrition session and utilization of community available and affordable resources, were adapted from the Positive Deviance (PD)/Hearth programme (Child Survival Collaborations and Resources Group 2002). Contrary to the PD/Hearth, CPNP had no community‐specific positive deviant behaviours, yet generally identified PD practices around feeding, caring, hygiene and health‐seeking in similar settings were addressed using a WV's PD/Hearth training manual (http://wvi.org/nutrition/publication/pdhearth-master-trainers-manual). Detail implementation process of the CPNP programme was described in Supplemental file 1. Briefly, group nutrition sessions were led by female operators hired and trained for this programme operation unlike volunteer mothers practising PD behaviours in typical PD/Hearth programmes. The 12‐day nutrition sessions were conducted at the village (‘Ganda’). By and large, 7 to 12 child–mother pairs participated in each nutrition session. The mothers contributed various food ingredients and session materials such as firewood, prepared complementary foods based on recipes developed by WV's nutrition experts through a local market survey, and fed their children on the spot during the 12 days. The mothers discussed feeding, caring, hygiene and health‐seeking messages with the operators. All enrolled children were weighed on the first and 12th day of the sessions, then 1 and 3 months after the last session. The participants had 1 to 2 follow‐up visits by operators during the 2 weeks following the end of the sessions. Once a nutrition session was carried out in a village in a Kebele, the next session was organized in a neighbouring village within the Kebele.
The ENA activity aimed to deliver nutrition messages to all mothers with children under 2 years of age through individual counselling by Health Extension Workers or community volunteers. Adequate breastfeeding and appropriate complementary feeding practices were the main nutrition messages in the ENA counselling (Ethiopia Public Health Training Initiative 2004).
According to the Ethiopia national CMAM protocol (Federal Ministry of Health, Government of Ethiopia 2007), severely wasted children with mid‐upper arm circumferences of less than 11.0 cm but without complications were referred to the nearest health post/health centre and received Plumpy'Nut until their recovery. Through three rounds of corn‐soy blend (CSB) distribution over the project period, only moderately wasted children with mid‐upper arm circumferences of 11.0‐11.9 cm received 8.3 kg of CSB and oil per month for 3 months from their assigned health centre.
The CPNP was launched in August 2012 and implemented through August 2013. ENA and CMAM activities were done during this time in the control and intervention areas.
Data collection procedures
Habro and Melka Bello district health offices prepared a roster of children 0 to 12 months of age in the study area. Health Extension Workers and community volunteers visited households in their Kebele and recorded the relevant information onto the child roster form. The form included Kebele and village name, mother's name, and child's name, birthdate, age and sex. Following data entry of this information, a unique identification number was assigned to each child, out of which 2064 children 3–9 months of age were randomly selected proportional to the population size of each cluster. Data collection was initiated 4 months after the first CPNP nutrition session because of logistical challenges in implementing data collection. The enrollment was done from 20 November 2012 to 19 February 2013, and the last follow‐up data collection was completed on 19 February 2014. Data collection through household visits was carried out at five major time points for a cohort of children 6 to 12 months of age: at enrollment (visit1), 3 months (visit2), 6 months (visit3), 9 months (visit4), and at the 12‐month follow‐up (visit5) (Fig. 1). Thus, the children enrolled at 6 to 12 months of age at visit1 turned 18 to 24 months old at visit5. The CPNP programme was phased out when visit4 started; thus, visit5 was done after the end of the programme.
Figure 1.
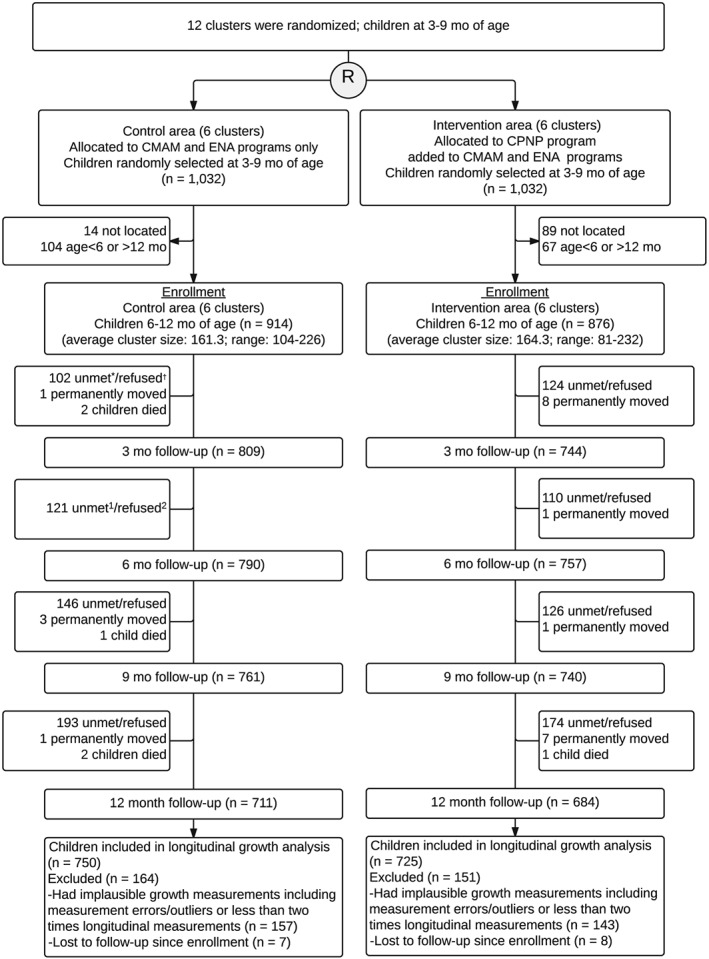
Consort diagram for trial participants from enrollment through 12‐month follow‐up, Habro and Melka Bello districts, Ethiopia. CMAM, community‐based management of acute malnutrition; CPNP, community‐based participatory nutrition promotion; ENA, Essential Nutrition Action. *Unmet: the subject moved out of the area or was not at home at the time of the survey visit. †Refused: the subject decided not to participate at the time of the survey.
The data collection team comprised a total of two team leaders and 18 enumerators in two districts, all of whom were recruited from their district and trained by study investigators for the anthropometric measurements and household survey. Structured questionnaires were prepared in local language (‘Afan Oromo’), and the data collection tool was pre‐tested in a neighbouring Kebele outside the study area.
After obtaining signed informed consent, the weight and length of the children were measured using standardized procedures every 3 months from the moment of enrollment (visit1) to the 12‐month follow‐up (visit5) (Cogill 2003). A locally designed measuring board was used to measure supine length for children to the nearest 0.1 cm. Weight was measured to the nearest 0.01 kg by a digital scale (model 354, SECA/GERMANY). Both length and weight were recorded two times. At enrollment, using a structured questionnaire, mothers of children were asked about household demographic information, dwelling conditions, household assets, food insecure conditions, social capital, drinking water sources and sanitation facilities. Every 3 months, all mothers were also asked whether they participated in or received each of the three interventions – attended a CPNP nutrition session, received ENA activity/counselling, or received Plumpy'Nut or CSB through the CMAM programme – in the past three months. Every 3 months, the mothers were asked about infant and young child feeding practices in accordance with World Health Organisation (WHO) guidelines (Pan American Health Organization/WHO 2003). At every 6 months, mothers were asked whether they had washed their hands with soap in the past 24 h at critical time points.
Data quality control
Standardization of anthropometric measurements was achieved by taking multiple measurements on non‐study subjects during the training prior to commencement of data collection and by conducting refresher training when necessary. Regular supervision visits by team leaders were made during filed data collection. Collected questionnaires and forms were submitted to team leaders regularly during bi‐weekly team meetings and delivered to the field data management team in the Habro district. All entered data were cross‐checked with another data entry person. Enumerators and the data entry team had no interaction with the intervention implementation staff or government health staff.
Statistical analysis
Child, parental and household characteristics at enrollment between intervention and control areas were compared using linear, logistic and multinomial logistic regression for continuous, binary and categorical variables, respectively, which were adjusted for the clustered study design. Proportion of participation in the ENA and CMAM programmes were computed by summing up all events from visit1 to visit5 divided by the total number of mothers who were interviewed at each visit. The mean percentage difference in programme participation was tested by two‐sample tests of proportions.
Length and weight were used to create indices of LAZ, WAZ and WLZ based on the WHO child growth standards (WHO Multicentre Growth Reference Study Group 2006). At each visit, data with z scores in unacceptable ranges [i.e. LAZ (n = 11) and WAZ (n = 0) below −6 or greater than 6; WLZ (n = 54) below −5 or greater than 5] were treated as missing values. In our study, the missing values were omitted from the statistical analysis while the other values for the same child at the next time point were still retained. For the z scores removed, its corresponding length or weight was replaced as a missing value also, considering it to be the result of measurement error. Child length measure at visit1 was treated as a missing value if an unacceptably high increase (>10 cm) was shown between visit2 and visit1 (n = 29), because more measurement errors were reported during visit1 and data quality improvement was conducted before visit2. All length measures of a total of 242 children were removed as their subsequent length measures were lower than that of prior visits. We computed the growth rate of children (based on length and weight) by sex and age for each enumerator and compared those values to the standard growth rate by sex and age, which was computed using datasets that were used for constructing the WHO growth standards (WHO Multicentre Growth Reference Study Group 2006). This procedure was decided based on our previous experience in identifying measurement errors in linear growth in children. We found that measures from two enumerators almost doubled weight gain rate per month, compared with the growth rate of the standard population, thus all weight measures collected by these two enumerators were treated as missing values (n = 704). During the data cleaning process, of the total number of length (n = 7757) and weight (n = 7776) measures collected from 1790 enrolled children over a year, 18.5% (n = 1432) of length measures and 16.0% (n = 1248) of weight measures were either removed or treated as missing values.
Three‐level mixed‐effects linear regression models estimated the differences in z scores, length and weight between children in the control area vs. intervention area. The repeated anthropometric measures (level1) were nested within children (level2), who were nested within randomized clusters (level3). The models added quadratic terms for child age and accounted for the cluster‐level effect and differences at enrollment (visit1) such as father's education, household wealth index, food security, mobile phone availability and type of nearest health facilities to the house. Fixed‐effects covariates included randomized area (control area vs. intervention area), child age, interaction term between child age and randomized area, sex and variables that differed at visit1. Random intercepts were included at both the individual and cluster levels. The distribution of z scores, length and weight at 6 to 24 months of age was graphically presented by Lowess curves, which were produced from nonparametric, locally weighted regression of the anthropometric outcomes on the range of child age (Cleveland & Devlin 1998). Absolute risk differences between control and intervention areas were derived using mixed‐effects linear regression models in the prevalences of stunting, underweight and wasting during the 12‐month follow‐up, by subtracting the average differences in these outcomes at enrollment from the average differences at 12‐month follow‐up.
Data management and statistical analysis were performed using stata version 12.0 (Stata Corporation, College Station, TX, USA). Statistical significance was set at P < 0.05 with all tests being two tailed.
Ethical review
The study proposal, questionnaires and consent forms were submitted and approved by the Institutional Review Board at Oromia Regional Health Bureau, Addis Ababa, Ethiopia. All mothers of study subject children were provided detailed information about the study verbally at enrollment (visit1) prior to data collection, and only mothers who provided consent were enrolled in this study.
Results
Out of the 2064 randomly selected children from the roster, 914 children from the control and 876 children from the intervention areas were enrolled in the study. Exclusions were related to not finding children/refusal (n = 14 in control and n = 89 in intervention area) or age criteria not being met (n = 104 in control and n = 67 in intervention area). Thus, a total of 1790 child and mother pairs were enrolled at visit1 and followed up every 3 months. The two groups did not differ in children being followed by visit; 78% of children were visited at visit5 (Fig. 1).
The mean (SD) age of enrolled children was 8.7 (1.9) months, the mean (SD) age of fathers and mothers was 32.3 (6.8) years and 26.1 (5.4) years, respectively, and 82.3% of mothers were illiterate (Table 1). More than 90% of the households depended on mixed farming for their livelihood. Child nutritional status, reflected by stunting (20.0% vs. 19.2%), underweight (19.2% vs. 19.2%) and wasting (16.7% vs. 16.9%), was not different by group. Groups did not differ in child age and sex, parents' age, mothers' education, parity, main living sources, religion, and drinking water source and sanitation facilities (Table 1). However, the intervention area had a higher proportion of fathers having any primary education or higher (48.6% vs. 37.8%; P < 0.05), fewer households with severe food insecurity (12.4% vs. 34.7%; P = 0.001), higher availability of mobile phones (30.3% vs. 14.2%; P = 0.003), fewer poor households (34.9% vs. 43.0%; P = 0.05) and greater access to the larger health facilities (P < 0.001) (Table 1).
Table 1.
Enrollment characteristics at visit1, Habro and Melka Bello districts, Ethiopia (maximum n = 914 for control area; maximum n = 876 for intervention area)
| Control area | Intervention area | |||
|---|---|---|---|---|
| Child characteristics | n | n (%) | n | n (%) |
| Male sex, % | 914 | 471 (51.5) | 876 | 468 (53.4) |
| Stunting, %† | 620 | 119 (19.2) | 614 | 123 (20.0) |
| Underweight, %‡ | 735 | 141 (19.2) | 713 | 137 (19.2) |
| Wasting, %§ | 614 | 104 (16.9) | 611 | 102 (16.7) |
| n | Mean ± SD | n | Mean ± SD | |
| Age (mo) | 914 | 8.7 ± 1.9 | 876 | 8.8 ± 1.9 |
| Length‐for‐age z score† | 620 | −0.90 ± 1.37 | 614 | −0.87 ± 1.41 |
| Weight‐for‐age z score‡ | 735 | −1.00 ± 1.16 | 713 | −1.00 ± 1.21 |
| Weight‐for‐length z score§ | 614 | −0.62 ± 1.41 | 612 | −0.72 ± 1.38 |
| Parental characteristics | n | n (%) | n | n (%) |
| Mothers who had any primary education or higher, % | 914 | 122 (13.3) | 876 | 170 (19.4) |
| Fathers who had any primary education or higher, %* | 914 | 345 (37.8) | 876 | 426 (48.6) |
| n | Mean ± SD | n | Mean ± SD | |
| Maternal age (years) | 914 | 26.1 ± 5.6 | 876 | 26.0 ± 5.2 |
| Paternal age (years) | 914 | 32.0 ± 6.9 | 874 | 32.7 ± 6.6 |
| No. of parity | 913 | 3.7 ± 2.1 | 868 | 3.7 ± 2.1 |
| Household characteristics | n | n (%) | n | n (%) |
| Muslim religion, % | 911 | 867 (95.2) | 875 | 829 (94.7) |
| Father as a household head, % | 913 | 857 (93.8) | 876 | 857 (97.8) |
| Self‐supporting farming, % | 914 | 821 (89.8) | 872 | 825 (94.6) |
| Household wealth index, %* | ||||
| Poor | 914 | 393 (43.0) | 876 | 306 (34.9) |
| Middle | 386 (42.2) | 339 (38.7) | ||
| Rich | 135 (14.8) | 231 (26.4) | ||
| Availability of mobile phones, %* | 914 | 130 (14.2) | 876 | 265 (30.3) |
| Household food insecurity, %* | ||||
| Food secure | 912 | 180 (19.7) | 876 | 272 (31.1) |
| Mild food insecure | 130 (14.2) | 340 (36.5) | ||
| Moderately food insecure | 286 (31.4) | 154 (20.0) | ||
| Severely food insecure | 316 (34.7) | 110 (12.4) | ||
| Use of protected water sources, %¶ | 914 | 468 (51.3) | 791 | 584 (66.7) |
| None latrine, % | 910 | 246 (26.9) | 871 | 182 (20.8) |
| Inadequate waste disposal, % | 909 | 316 (34.8) | 874 | 242 (27.7) |
| Access to market < 1 h, % | 913 | 239 (26.2) | 871 | 310 (35.6) |
| Nearest health facility, %* | ||||
| Health post | 908 | 420 (46.3) | 868 | 292 (33.6) |
| Health center | 479 (52.8) | 451 (52.0) | ||
| Clinic/Hospital | 9 (1.0) | 20 (14.4) | ||
| District | ||||
| Habro | 914 | 491 (53.7) | 876 | 508 (58.0) |
| Melka Bello | 423 (46.3) | 368 (42.0) | ||
P < 0.05; p‐values were calculated by linear, logistic or multinomial logistic regression accounting for clustering effect.
Missing length measurement (n = 5 in control and n = 9 in intervention area), removed outliers (LAZ < −6 or >6) (n = 9 in control and n = 1 in intervention area) and omitted values through data cleaning process (n = 280 in control and n = 252 in intervention area).
Missing weight measurement (n = 4 in control and n = 2 in intervention area) and omitted values through data cleaning process (n = 175 in control and n = 161 in intervention area).
Missing length measurement (n = 5 in control and n = 9 in intervention area) and weight measurement (n = 4 in control and n = 2 in intervention area), removed outliers (WLZ < −5 or >5) (n = 13 in control and n = 6 in intervention area) and omitted values through data cleaning process (n = 278 in control and n = 248 in intervention area).
Protected water sources include public tap/standpipe, tube well/borehole and protected well.
According to the CPNP programme records, 372 nutrition sessions were held, and 3299 mother–child pairs attended them in the intervention area during the 13 months before the phase out of the programme. Of 876 children in the intervention area, the proportion of CPNP participants was 16.5% (n = 97) at visit1 but increased to 38.9% (n = 340) by visit5 (Table 2). In the control area, 3.3% of the children were reported to have experienced CPNP participation. There was no difference in the proportion of children receiving CSB services (15.1% vs. 16.0%, P = 0.30). By contrast, fewer children received Plumpy'Nut (2.9% vs. 7.7%, P < 0.001), and more mothers were exposed to the ENA activity (21.4% vs. 12.4%, P < 0.001) in the intervention than in the control area.
Table 2.
Programme participation and use of services in CPNP, ENA and CMAM programmes in control and intervention areas, in Habro and Melka Bello districts, Ethiopia (2012–2014)
| Control area | Intervention area | P‐value¶ | |||
|---|---|---|---|---|---|
| n * | n (%) | n * | n (%) | ||
| CPNP | |||||
| Ever participated in the nutrition sessions during 12‐month follow‐up period | 914 | 30 (3.3) | 876 | 340 (38.9) | <0.001 |
| n † | n (%)‡, § | n † | n (%)‡, § | ||
| CMAM | |||||
| Ever received corn‐soy blend in the past 3 months | 3267 | 524 (16.0) | 3107 | 469 (15.1) | 0.30 |
| Ever received Plumpy'Nut in the past 3 months | 3080 | 238 (7.7) | 2916 | 86 (2.9) | <0.001 |
| ENA | |||||
| Ever received ENA counselling at least once a month in the past 3 months | 3987 | 493 (12.4) | 3803 | 813 (21.4) | <0.001 |
n was a total number of mothers enrolled in the study.
n was a total number of mothers surveyed across four visits.
n was a total number of mothers who reported receiving each intervention; questions about receiving Plumpy'Nut were asked at visit2 through visit5; questions about corn‐soy blend were asked at visit1 through visit4; questions about ENA activity exposure were asked from visit1 through visit5. Each of the five visitations (or four visitations for Plumpy'Nut and corn‐soy blend) were conducted 3 months apart.
Proportion of participation in the ENA and CMAM programmes were computed by summing up all events from visit1 to visit5 (visit1 to visit 4 for corn‐soy blend; visit2 to visit5 for Plumpy'Nut) divided by the total number of mothers who were interviewed at each visit.
The mean percentage difference in programme participation was tested by two‐sample tests of proportions.
CPNP, community‐based participatory nutrition promotion; ENA, Essential Nutrition Action; CMAM, Community‐based Management of Acute Malnutrition.
Z scores, length and weight among study children are presented by visit in Table S1. Out of 1790 subject children, 750 (82.1%, n = 914 in control area) and 725 (82.8%, n = 876 in intervention area) were included in the longitudinal analysis, who had at least two measures at different time points. The mean/proportion values of socio‐demographic variables by treatment group remained similar to that of the original control and intervention groups (n = 1790) (Table S2); however, the significance of fathers' education was attenuated (P > 0.05) with a larger standard error because of the smaller sample size. Differences in anthropometric indices increased with age and were significant by 18–21 months of age and continued up to 24 months of age (Fig. 2). Children in the intervention area had faster growth rate over 6 to 24 months of age compared with children in the control area in terms of length [difference (diff): 0.059 cm/month; 95% CI: 0.027, 0.092; P = 0.001] and weight (diff: 0.031 kg/month; 95% CI: 0.019, 0.042; P < 0.001) (Table 3 and Fig. 2). Growth faltering appeared in both areas, but it was slower in the intervention area as evidenced by the monthly change in LAZ (diff: 0.021 z score/month; 95% CI: 0.008, 0.034). The monthly changes in WAZ (diff: 0.028 z score/month; 95% CI: 0.016, 0.039) and WLZ (diff: 0.042 z score/month; 95% CI: 0.024, 0.059) were also found to be slower favouring children in the intervention area, compared with the control area (all Ps < 0.001). Differences in z scores, length and weight after 12‐month follow‐up, estimated by average marginal effects, were as follows: 0.32 LAZ (95% CI: 0.08, 0.56), 0.34 WAZ (95% CI: 0.06, 0.61), 0.48 WLZ (95% CI: 0.16, 0.81), 0.95 cm in length (95% CI: 0.27, 1.58) and 0.41 kg in weight (95% CI: 0.15, 0.67) (all Ps < 0.001) (Table S3).
Figure 2.
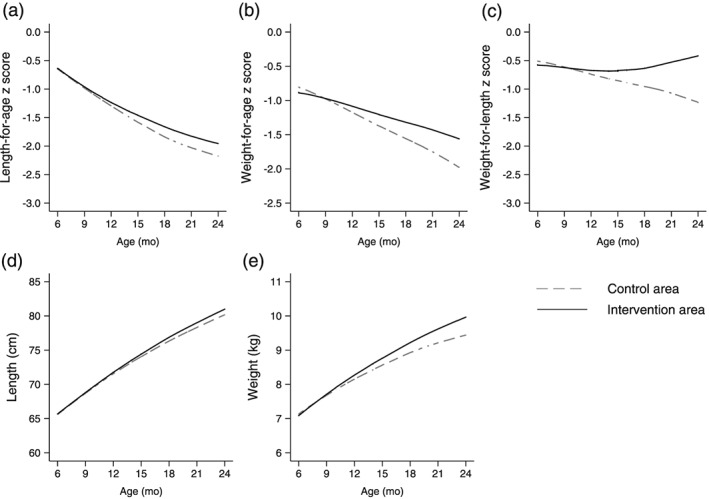
Predicted length‐for‐age z score (A), weight‐for‐age z score (B), weight‐for‐length z score (C), length (D) and weight (E) of children 6 to 24 months of age in control and intervention areas. The graphs were produced by locally weighted regression on the predicted values derived from linear mixed‐effect regression models including age quadratic term (n = 725 children in control area; n = 750 children in intervention area). The Lowess curves had a bandwith of 0.8.
Table 3.
Marginal monthly effects of community‐based participatory nutrition promotion programme on child‐growth outcomes over 6 to 24 months of age in Habro and Melka Bello districts, Ethiopia (2012–2014)
| Control area | Intervention area | Difference (95% CI) in monthly change between control and intervention area‡ | P‐value | |||
|---|---|---|---|---|---|---|
| n * | Monthly change Mean (SE)† | n * | Monthly change Mean (SE)† | |||
| Change in LAZ/month | 3285 | −0.095 (0.004) | 3040 | −0.074 (0.005) | 0.021 (0.008, 0.034) | 0.001 |
| Change in WAZ/month | 3408 | −0.060 (0.004) | 3120 | −0.032 (0.004) | 0.028 (0.016, 0.039) | <0.001 |
| Change in WLZ/month | 3275 | −0.030 (0.006) | 3030 | 0.011 (0.006) | 0.042 (0.024, 0.059) | <0.001 |
| Change in length (cm)/month | 3285 | 0.803 (0.012) | 3040 | 0.862 (0.012) | 0.059 (0.027, 0.092) | <0.001 |
| Change in weight (kg)/month | 3408 | 0.136 (0.004) | 3120 | 0.167 (0.004) | 0.031 (0.019, 0.042) | <0.001 |
n, number of observations (measures) from visit1 to visit5.
Multi‐level mixed‐effects model estimated the monthly change in growth outcomes (SE), adjusting for child age and sex, district location, and data collector who surveyed the household, father's education, household wealth status, household food security, type of nearest health facilities and mobile phone availability.
Differences (95% CI) in monthly change of growth outcomes between control and intervention areas were derived using contrasts of average marginal effects.
LAZ, length‐for‐age z score; WAZ, weight‐for‐age z score; WLZ, weight‐for‐length z score
Absolute risk reduction in the prevalences of stunting, wasting and underweight was computed using a longitudinal panel data at visit1 (enrollment) and visit5 (12‐month follow‐up), adjusting for enrollment status in the aforementioned outcomes, as well as individual‐level and cluster‐level covariates (Table 4). Compared with the control area, children in the intervention area showed an 8.1% (95% CI: 1.1%, 15.1%; P = 0.02) greater decline in the prevalence of stunting and a 6.3% (95% CI: 0.1%, 12.6%; P = 0.046) greater decline in the prevalence of underweight. No statistically significant programme effect was found for the prevalence of wasting (diff: 3.2%; 95% CI:−3.3%, 9.6%; P = 0.34).
Table 4.
Effect of community‐based participatory nutrition promotion (CPNP) programme on the prevalences of stunting, underweight, and wasting at 12‐months follow‐up (visit5) in Habro and Melka Bello districts, Ethiopia (2012‐2014)
| Control area | Intervention area | Absolute percentage (%) difference (95% CI)† | P‐value | |||
|---|---|---|---|---|---|---|
| n * | n (%) | n * | n (%) | |||
| Stunting (LAZ < −2) | ||||||
| Enrollment | 620 | 119 (19.2) | 614 | 123 (20.0) | ||
| 12‐month follow‐up | 612 | 300 (49.0) | 513 | 214 (41.7) | −8.1 (−15.1, −1.1) | 0.02 |
| Wasting (WLZ < −2) | ||||||
| Enrollment | 614 | 104 (16.9) | 611 | 102 (16.7) | ||
| 12‐month follow‐up | 611 | 611 (31.8) | 429 | 429 (29.8) | 3.2 (−3.3, 9.6) | 0.34 |
| Underweight (WAZ < −2) | ||||||
| Enrollment | 735 | 141 (19.2) | 713 | 137 (19.2) | ||
| 12‐month follow‐up | 624 | 256 (41.0) | 501 | 168 (33.5) | −6.3 (−12.6, −0.1) | 0.046 |
At enrollment, the total number of children surveyed was 1790 (n = 914 in control and n = 876 in intervention areas), no length measurement (n = 14), no weight measurement (n = 6), removed outliers (n = 10 for LAZ > 6 or < −6, n = 10 for WLZ > 5 or < −5) and treated as missing values through data cleaning process (n = 532 for length, n = 336 for weight); at 12‐month follow‐up, the total number of children surveyed was 1395 (n = 711 in control and n = 684 in intervention area), no length measurement (n = 2), no weight measurement (n = 1), removed outliers (n = 10 for LAZ > 6 or < −6, n = 27 for WLZ > 5 or < −5) and treated as missing values through data cleaning process (n = 258 for length, n = 269 for weight).
Estimated by mixed effect linear regression analysis, adjusting for enrollment status in growth outcomes, child age and sex, father's education, household wealth status, household food security, type of nearest health facilities, mobile phone availability, district location and data collectors who surveyed the households.
Discussion
Using a cluster randomized trial, this study demonstrated that a CPNP programme – added to existing government programmes of ENA and CMAM – could effectively improve child growth in rural Eastern Ethiopia. Specifically, the CPNP programme resulted in significant improvements in LAZ, WAZ and WLZ by 0.02~0.04 z score/month in children aged 6 to 24 months and decline in prevalence of stunting by ~8% and underweight by ~6% at 12‐month follow‐up.
The results of the study were by and large consistent with previous studies on the effect of interventions that promoted complementary feeding through various behavioural change communications. A meta‐analysis of 17 studies showed that the provision of appropriate complementary foods with or without nutritional counselling led to an additional gain of 0.25 kg (±0.18) in weight and 0.54 cm (±0.38) in length in children 6 to 12 months of age, whereas education about complementary feeding resulted in an additional gain of 0.30 kg (±0.26) in weight and 0.49 cm (±0.50) in length (Imdad et al. 2011). In 16 RCTs and quasi‐experimental studies reviewed, education on complementary feeding alone resulted in significant increases in HAZ (standard mean difference, SMD: 0.23, 95% CI: 0.09, 0.36) and WAZ (SMD 0.16, 95% CI: 0.05, 0.27) (Lassi et al. 2013). In view of the aforementioned results, our outcomes with regard to child growth seemed to lie within the reasonable range of values as well as would serve as evidence that behaviour change approaches to improve child feeding practices may be effective in improving linear growth among children living in resource poor settings.
A similar trial in Burkina Faso, which also included components of cluster randomized trial design, behavioural change communication intervention and longitudinal follow‐up of children from 3–12 months of age, decreased wasting by 8.8 percentage point (pp), which was marginally significant, but showed no significant change in stunting (5.9 pp; P = 0.38) or underweight (6.1 pp; P = 0.40) (Olney et al. 2015). Conversely, effects from our study showed a decline in stunting and underweight but not in wasting. Our intervention more directly engaged mothers in performing intended feeding practices until they were adopted for 2 weeks, whereas the Burkina Faso study utilized community health personnel who delivered nutrition messages through home visits, based on an intervention of improving the underlying determinants such as increasing homestead food production. Further studies are needed to explore and compare the intervention mechanisms by which undernutrition by manifestation (e.g. wasting, stunting) is addressed.
Nutrition programmes based on PD/Hearth models have been popularly implemented in developing settings with the advantages of cultural appropriateness, sustainable implementation and community participation (Bolles et al. 2002; Hendrickson et al. 2002; Aubela et al. 2004); however, only a few nutrition programmes that adapted the PD theory were evaluated using robust study design with a control group on child nutritional outcomes (Bisits Bullen 2011). The programmes were effective in improving food consumption and feeding practices; however, they showed no effect on child growth. A trial in Vietnam that examined the impact of a PD/Hearth programme prospectively followed 240 children for 12 months and found no significant difference in growth patterns between intervention and control groups (Schroeder et al. 2002). A study in Haiti also reported no significant differences in nutritional status between study groups (Burkhalter & Northrup 1997). However, our findings would support the effectiveness of PD/Hearth approach if an intervention could be designed using this approach.
The plausibility of the programme impact of CPNP on child growth in the entire intervention area is explained by potential interactions between CPNP participants and non‐participants as follows. First, considerable CPNP programme coverage would make it plausible; of our study children (n = 876) in the intervention area, 38.9% ever attended nutrition sessions (Table 2). A total of 3299 participants in the programme records accounted for ~33.3% of the total population of children aged 0 to 24 months (estimated N = ~9900) residing in the intervention area of the two districts (Population Census Commission, Government of Ethipia 2008). Second, a high propagation of CPNP lessons from the participants to other neighbours was also found; even at visit1, ~45% of study mothers in the intervention area replied ever having a contact with the participants (data not shown). Last, implementation of the CPNP programme resulted in facilitating an existing nutrition programme; overall year‐round higher ENA activity in the intervention area than in the control area (23.4% vs. 15.1%; P < 0.001) was mainly attributed to active participation by CPNP mothers in the intervention area (Table 2). With the present study, implementation, utilization and influence of the CPNP programme and the programme impact on feeding and hygiene practices among caregivers were evaluated elsewhere (under review).
The strengths of our study included the use of a cluster randomized study design, prospective and longitudinal data collection on a large scale, and the use of a statistical approach to account for correlation within individual children and geographical clusters. There were a few limitations in this study. First, our anthropometric measurements had considerable measurement error despite continually checking for data quality and conducting refresher trainings. However, we improved the data by systematically identifying and excluding suspicious data (18.5% of length and 16.0% of weight measures) through sensitivity analysis. Prior to the aforementioned procedures, the average monthly growth rate in length and weight appeared faster than our current growth rates among study participants, and the differences in main outcomes were greater than current findings. Utilization of data collected at any two or more time points could maximize the amount of data in the analysis set, thus mitigating the weakness, which resulted from a considerable loss of anthropometric measures. Second, allocation of the intervention to the matched clusters was made randomly, but, by chance, imbalances in favour of the intervention area were found in a few enrollment characteristics at visit1 between randomized areas. The intervention clusters were in the vicinity of a main road in the district or passed through by the road. Closer adjacency to the main road would lead to better socio‐economic status in the intervention area. Third, this study had no true baseline because the first data collection was conducted 4 months after the CPNP nutrition sessions started within the communities. However, there was no significant difference in anthropometric measurements and indicators at enrollment and even to 9 months follow‐up until CPNP almost phased out. If the study children had true baselines prior to the CPNP implementation and were followed thereafter, the effect sizes on anthropometric outcomes would be less than the values presented in our study. Fourth, the intervention allocation and data collection procedures were not blinded to subject mothers and interviewers by the nature of the intervention of the CPNP. Some mothers knew of the existence of the CPNP programme in their community, but they still did not know that the purpose of this study was to evaluate the intervention impact. Interviewers were constantly reminded to collect accurate data with neutral attitudes regardless of intervention allocation. Fifth, it remains a possibility that any unmeasured confounding variables could have increased or decreased the current programme effect sizes. Additionally, CPNP participants were found in the control area with 3.3% of mothers. Because the borders between clusters were not regulated, mothers living on the borders of clusters would have had opportunities to attend the nutrition session. We assumed that 3.3% contamination would decrease the programme effect.
In conclusion, this study showed that a CPNP programme could improve child growth when the approach is taken to promote complementary feeding practices and incorporated within the existing government nutrition programmes in rural Ethiopia. These research findings will help spur community participatory approaches in nutritional interventions and perhaps aid in strengthening the community health systems. Finally adopting this type of a programme is likely to complement the work of Ethiopia's National Nutrition Programme, and aid in the development of nutrition strategies of non‐government organisations in the country.
Source of funding
This project was supported by World Vision Korea (project # E197814) and Korea International Cooperation Agency (KOICA). The funding agencies had no role in the design of the study, data collection and analysis, or presentation of the results.
Conflicts of interest
Yunhee Kang and Parul Christian had no conflict of interest related to the study. Sungtae Kim is an employee of World Vision Korea. Sisay Sinamo is an employee of World Vision International.
Contributions
YK, SK, SS and PC designed the research and prepared the proposal; YK conducted the research; SK supported overall research procedure; YK and PC analyzed and interpreted data and wrote the manuscript; SK and SS contributed to the writing of the manuscript; and YK had primary responsibility for the final content of the manuscript. All authors read and approved the final manuscript.
Supporting information
Supplemental File 1. Details of the community‐based participatory nutrition promotion (CPNP) program
Table S1. Anthropometric measurements in control and intervention area over 12‐mo follow‐up by visit Habro and Melka Bello districts Ethiopia (2012‐2014)
Table S2. Enrollment characteristics at visit1 among children who were included in the longitudinal analysis, Habro and Melka Bello districts, Ethiopia (maximum n = 750 for control area; maximum n = 725 for intervention area)
Table S3. Marginal effects of community‐based participatory nutrition promotion (CPNP) program on growth outcomes at 12‐mo follow‐up in Habro and Melka Bello districts, Ethiopia (2012‐2014)
Supporting info item
Supporting info item
Supporting info item
Supporting info item
Acknowledgements
We are grateful to all participating children and their caretakers in Habro and Melka Bello districts for their contribution to this study. We also acknowledge our partners, World Vision Korea, World Vision Ethiopia and Wholistic Interest Through Health (WITH), for their operational support. We appreciate the field support by Ethiopia Integrated Nutrition Project (EINP) team including Lemma Debela, Tadesse Abera, Imiru Waqjira and Eunjoo Yang. We thank Keith West (Johns Hopkins School of Public Health), David Paige (Johns Hopkins School of Public Health) and Bridget Aidam (World Vision International) for reviewing this manuscript. We also acknowledge Martin Blair and Jane Kim for their editing assistance.
Kang Y., Kim S., Sinamo S., and Christian P. (2017) Effectiveness of a community‐based nutrition programme to improve child growth in rural Ethiopia: a cluster randomized trial, Maternal & Child Nutrition, 13, e12349. doi: 10.1111/mcn.12349.
References
- Aubela J., Toure I. & Diagne M. (2004) Senegalese grandmothers promote improved maternal and child nutrition practices: the guardians of tradition are not averse to change. Social Science & Medicine 59, 945–959. [DOI] [PubMed] [Google Scholar]
- Bhutta Z.A., Das J.K., Rizvi A., Gaffey M.F., Walker N., Horton S. et al. (2013) Evidence‐based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet 382, 452–477. [DOI] [PubMed] [Google Scholar]
- Bisits Bullen P.A. (2011) The positive deviance/hearth approach to reducing child malnutrition: systematic review. Tropical Medicine and International Health 16, 1354–1366. [DOI] [PubMed] [Google Scholar]
- Bolles K., Speraw C., Berggren G. & Lafontant J.G. (2002) Ti Foyer (hearth) community‐based nutrition activities informed by the positive deviance approach in Leongane, Haiti: A programmatic description. Food and Nutrition Bulletin 23 (suppl4), S9–S15. [PubMed] [Google Scholar]
- Burkhalter B.R. & Northrup R.S. (1997) Hearth program at the hoˆpital Albert Schweitzer in Haiti In: Hearth Nutrition Model: Applications in Haiti, Vietnam, and Bangladesh (eds Wollinka O., Keeley E., Burkhalter B.R. & Bahir N.). Agency for International Development and World Relief Corporation by the Basic Support for Institutionalizing Child Survival (BASICS) Project: Arlington, U.S. [Google Scholar]
- Central Statistical Agency, Government of Ethiopia (2014) Ethiopia Mini Demographic and Health Survey 2014. Central Statistical Agency: Addis Ababa, Ethiopia. [Google Scholar]
- Central Statistical Agency, Government of Ethiopia & ICF International (2012) Ethiopia Demographic and Health Survey 2011. Central Statistical Agency and ICF International: Addis Ababa, Ethiopia and Calverton, Maryland, USA. [Google Scholar]
- Child Survival Collaborations and Resources Group (2002) Positive Deviance / Hearth: A Resource Guide for Sustainably Rehabilitating Malnourished Children. CORE Incorporated: Washington, D.C.. [Google Scholar]
- Cleveland W.S. & Devlin S.J. (1998) Locally weighted regression—an approach to regression‐analysis by local fitting. Journal of American Statistical Association 83, 596–610. [Google Scholar]
- Cogill B. (2003) Anthropometric Indicators Measurement Guide, Revised edn. Food and Nutrition Technical Assistance (FANTA) Project, FHI360: Washington, D.C. [Google Scholar]
- Deconinck H., Swindale A., Grant F. & Navarro‐Colorado C. (2008) Review of Community‐based Management of Acute Malnutrition (CMAM) in the Post‐emergency Context: Synthesis of Lessons on Integration of CMAM into National Health Systems. Food and Nutrition Technical Assistance (FANTA) Project, FHI 360: Washington, D.C. [Google Scholar]
- Dupont W.D. & Plummer W.D. Jr. (1998) Power and sample size calculations for studies involving linear regression. Controlled Clinical Trials 19, 589–601. [DOI] [PubMed] [Google Scholar]
- Ethiopia Public Health Training Initiative (2004) Trainer's guide. Using the Essential Nutrition Actions to Improve the Nutrition of Women and Children in Ethiopia, including under Situations of Emergencies and HIV & AIDS. The LINKAGES Project/AED. Available at: http://files.ennonline.net/attachments/96/trainers-guide.pdf/ (Accessed 23 November 2012)
- Federal Ministry of Health, Government of Ethiopia (2007) Protocol for the management of severe acute malnutrition. Available at: http://files.ennonline.net/attachments/897/ethiopia-sam-guideline-march-2007.pdf/ (Accessed 23 October 2013)
- Fenn B., Morris S.S. & Frost C. (2004) Do childhood growth indicators in developing countries cluster? Implications for intervention strategies. Public Health Nutrition 7, 829–834. [DOI] [PubMed] [Google Scholar]
- Government of Ethiopia (2013) National Nutrition Programme (June 2013‐June 2015). Available at: http://www.unicef.org/ethiopia/National_Nutrition_Programme.pdf/ (Accessed 12 January 2014)
- Hendrickson J.L., Dearden K., Pachon H., An N.H., Schroeder D.G. & Marsh D.R. (2002) Empowerment in rural Viet Nam: exploring changes in mothers and health volunteers in the context of an integrated nutrition project. Food and Nutrition Bulletin 23 (suppl4), S83–S91. [PubMed] [Google Scholar]
- Imdad A., Yakoob M.Y. & Bhutta Z.A. (2011) Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health 11 (Suppl3):S25 (Epub ahead of print; DOI: 10.1186/1471-2458-11-S3-S25). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings J. & Hirbaye M.B. (2008) Review of Incorporation of Essential Nutrition Actions into Public Health Programs in Ethiopia. Food and Nutrition Technical Assistance (FANTA) Project, FHI360: Washington, D.C. [Google Scholar]
- Lassi Z.S., Das J.K., Zahid G., Imdad A. & Bhutta Z.A. (2013) Impact of education and provision of complementary feeding on growth and morbidity in children less than 2 years of age in developing countries: a systematic review. BMC Public Health 13 (Suppl3):S13 (Epub ahead of print; DOI: 10.1186/1471-2458-13-S3-S13). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassi Z.S., Mallick D., Das J.K., Mal L., Salam R.A. & Bhutta Z.A. (2014) Essential interventions for child health. Reproductive Health 11 (Suppl1):S4. (Epub ahead of print; DOI: 10.1186/1742-4755-11-S1-S4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenters L.M., Wazny K., Webb P., Ahmed T. & Bhutta Z.A. (2013) Treatment of severe and moderate acute malnutrition in low‐ and middle‐income settings: a systematic review, meta‐analysis and Delphi process. BMC Public Health 13 (Suppl3):S23 (Epub ahead of print; DOI: 10.1186/1471-2458-13-S3-S23). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olney D.K., Pedehombga A., Ruel M.T. & Dillon A. (2015) A 2‐year integrated agriculture and nutrition and health behavior change communication program targeted to women in Burkina Faso reduces anemia, wasting, and diarrhea in children 3‐12.9 months of age at baseline: a cluster‐randomized controlled trial. Journal of Nutrition 145, 1317–1324. [DOI] [PubMed] [Google Scholar]
- Pan American Health Organization/WHO (2003) Guiding Principles for Complementary Feeding of the Breastfed Child. Pan American Health Organization, World Health Organization: Washington D.C. [Google Scholar]
- Penny M.E., Creed‐Kanashiro H.M., Robert R.C., Narro M.R., Caulfield L.E. & Black R.E. (2005) Effectiveness of an educational intervention delivered through the health services to improve nutrition in young children: a cluster‐randomised controlled trial. Lancet 365, 1863–1872. [DOI] [PubMed] [Google Scholar]
- Population Census Commission, Government of Ethipia (2008) The 2007 Population and Housing Census of Ethiopia: Statistical Report for Oromiya Region; Part V: Population Size of Kebeles. Ethiopian Population Sensus Commission: Addis Ababa, Ethiopia/. [Google Scholar]
- Schroeder D.G., Pachón H., Dearden K.A., Ha T.T., Lang T.T. & Marsh D.R. (2002) An integrated child nutrition intervention improved growth of younger, more malnourished children in northern Viet Nam. Food and Nutrition Bulletin 23 (suppl4), S53–S61. [PubMed] [Google Scholar]
- Shi L., Zhang J., Wang Y., Caulfield L.E. & Guyer B. (2010) Effectiveness of an educational intervention on complementary feeding practices and growth in rural China: a cluster randomised controlled trial. Public Health Nutrition 13, 556–565. [DOI] [PubMed] [Google Scholar]
- UNICEF (2012) Evaluation of Community Management of Acute Malnutrition (CMAM): Global Synthesis Report. United Nations Children's Fund: New York. [Google Scholar]
- USAID (2008) End‐line Household Survey Results. Southern Nations, Nationalities, and People Region. Essential Service for Health in Ethiopia/US Agency for International Development: Addis Ababa, Ethiopia: Available at: http://www.jsi.com/JSIInternet/Inc/Common/_download_pub.cfm?id=13205&lid=3/ (Accessed 20 January 2014) [Google Scholar]
- Vazir S., Engle P., Balakrishna N., Griffiths P.L., Johnson S.L., Creed‐Kanashiro H. et al. (2013) Cluster‐randomized trial on complementary and responsive feeding education to caregivers found improved dietary intake, growth and development among rural Indian toddlers. Maternal and Child Nutrition 9, 99–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora C.G., Adair L., Fall C., Hallal P.C., Martorell R., Richter L. et al. (2008) Maternal and child undernutrition: consequences for adult health and human capital. Lancet 371, 340–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Multicentre Growth Reference Study Group (2006) WHO Child Growth Standards based on length/height, weight and age. Acta Paediatrica. Supplement 450, 76–85. [DOI] [PubMed] [Google Scholar]
- Zeitlin M., Ghassemi H. & Mansour M. (1990) Positive Deviance in Child Nutrition: With Emphasis on Psychosocial and Behavioral Aspects and Implications for Development. The United Nations University: Tokyo, Japan. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental File 1. Details of the community‐based participatory nutrition promotion (CPNP) program
Table S1. Anthropometric measurements in control and intervention area over 12‐mo follow‐up by visit Habro and Melka Bello districts Ethiopia (2012‐2014)
Table S2. Enrollment characteristics at visit1 among children who were included in the longitudinal analysis, Habro and Melka Bello districts, Ethiopia (maximum n = 750 for control area; maximum n = 725 for intervention area)
Table S3. Marginal effects of community‐based participatory nutrition promotion (CPNP) program on growth outcomes at 12‐mo follow‐up in Habro and Melka Bello districts, Ethiopia (2012‐2014)
Supporting info item
Supporting info item
Supporting info item
Supporting info item


