Abstract
It is recommended that infants from the age of 12 months should be weaned from bottles. However, an overwhelming proportion of young children were still using bottle after the recommended age of bottle‐weaning. This cross‐sectional study examined the association between utensils for milk drinking and food group consumption, growth and socio‐demographic characteristics among young children. Data from the Survey of Infant and Young Child Feeding in Hong Kong were analyzed for 649 children aged 18–48 months old. Dietary outcomes were obtained via 3‐day dietary records, while utensils for milk drinking and socio‐demographic characteristics were collected from a self‐developed questionnaire. Length/height and weight of the children were measured by the nurses. Results showed that daily consumption of formula milk was significantly greater among bottle users or bottle plus cup users than non‐bottle users (p < 0.05). Exclusive bottle users had significantly lower intakes of meat and meat alternatives than bottle plus cup users for the 18 to 24‐month group (p = 0.001) and lower intakes of fruits than non‐bottle users in the 48‐month group (p = 0.015). BMI z‐score was significantly higher for exclusive bottle users than non‐bottle users, even after adjusting for socio‐economic factors and child's age (p = 0.006). The results showed that the milk drinking utensil was associated with the amount of formula milk and food group consumption as well as BMI z‐score. There is a need to actively discourage prolonged bottle use in order to help young children develop good dietary habits. © 2016 John Wiley & Sons Ltd
Keywords: Chinese, diet, growth, milk bottle, nutrition, young child
Introduction
Professional guidelines recommend introducing a cup at 6 months and completing bottle‐weaning by 12 to 18 months to promote feeding skills (American Academy of Pediatrics 2008). Despite these recommendations, various studies document prolonged bottle feeding to be a relatively frequent practice (Kaste & Gift 1995; Hammer et al. 1999; De La Hunty et al. 2000).
Prolonged bottle feeding has been associated with excessive milk intake (Safer et al. 2001; Northstone et al. 2002). Health professionals noticed that a number of feeding problems arise because a child has been filled up on his/her bottle, has no room in the stomach to accommodate other food and also has no interest in trying the food offered (Avery & Baxter 2001). Consequently, inappropriate and extended use of bottle can result in long‐term health problems, including a restricted diet, poor chewing techniques, food refusal, iron deficiency anaemia, failure to thrive and speech problems (Avery & Baxter 2001).
In addition, prolonged bottle feeding is one of the risk factors for overweight. A study of primarily Hispanic children (mean age of 36 months) showed that prolonged bottle use was significantly associated with body mass index (BMI) >95% (Bonuck & Kahn 2002). Each additional month of bottle use by 3‐ to 5‐year‐olds was associated with 3% increased probability of being in a higher BMI group (Bonuck et al. 2004). A large prospective study also found that prolonged bottle use at 24 months of age was associated with increased risk of BMI over 95th percentile at 5.5 years of age, after controlling for socio‐demographic characteristics, maternal obesity, maternal smoking, breastfeeding, age of introduction of solid foods, screen‐viewing time and the child's weight status at birth and at 9 months of age (Gooze et al. 2011). As consuming excess liquids, most often formula milk, through bottles is easy, excess protein intake from formula milk can increase the risk of overweight/obesity (Koletzko et al. 2009; Koletzko et al. 2010).
Indeed, significant associations have been observed between socio‐demographic characteristics and prolonged bottle use, namely poverty, lower parental education, maternal smoking and the number of older siblings (Kaste & Gift 1995; De La Hunty et al. 2000; Northstone et al. 2002). Knowledge of the association between the use of different milk drinking utensils and socio‐demographic characteristics of local children may help better define the target groups of caregivers for intervention.
The American Academy of Pediatrics recommended that children should be encouraged to drink from a cup as they approach their first birthday and they should be weaned from bottles between 12 and 18 months (American Academy of Pediatrics 2008). In the United Kingdom (UK), parents are encouraged to offer drinks in a non‐valved, free‐flowing cup from age 6 months and bottle use is discouraged after the first year (Nice Public Health Guidance 11 2008). In Hong Kong, children are advised to start using a training cup when they are around 9 months old and it is best to wean from bottle to training cup by the 14th month (Oral Health Education Unit & Department of Health Hong Kong SARG 2013). However, findings of a milk consumption survey, which was one of the three sub‐surveys of the Infant and Young Child Feeding Survey (IYCFS) in Hong Kong revealed that adherence to bottle‐weaning guideline is poor (Family Health Service 2012). Of major concern in the results reported in the milk consumption survey is that an overwhelming proportion of the sample were still using a bottle despite being well over the age of 14 months old. There were 95% and 89% of children in the 18‐ and 24‐month groups, respectively, who were using the bottle for milk drinking, while 55% of the 48‐month group still used bottle to drink milk. More importantly, the use of formula, in particular follow‐up formula, was common among them, with 87.7% taking it. However, previous analyses of the milk consumption survey were mainly descriptive and the association between prolonged bottle use and pattern of diet among the studied children has not been examined in details. These situations raised our interest to conduct further analysis to examine such association using the pooled data of the milk consumption survey and the diet and nutrition survey. The diet and nutrition survey was another sub‐survey of the IYCFS with detailed dietary data of the studied children being collected. The survey showed an unbalanced dietary habit among young children in Hong Kong, in which their diet was characterized by low vegetable and fruit consumption, high intake of animal protein‐rich foods and over dependence on formula milk. This report therefore aims to address the following three questions: (1) do children who continue to use bottles consume more milk, in particular formula milk and have lower intakes from other food groups?; (2) do children who continue to use bottles have a greater body mass index than non‐bottle users after adjusting for socio‐demographic factors?; and (3) are there any socio‐demographic characteristics associated with the use of bottle?
Key messages.
Prolonged bottle feeding is common in Hong Kong.
Use of milk bottle was associated with greater consumption of formula milk among 18 to 48‐month‐old children.
Exclusive bottle users had significantly lower consumption of food groups (except milk and alternatives).
Exclusive bottle use was associated with higher BMI z‐score among 48‐month old children after adjusting for socio‐economic factors.
Early bottle‐weaning intervention is essential for care‐givers to help children to develop good dietary habits and to prevent childhood obesity.
Materials and methods
Design and study sample
Data of this cross‐sectional study was based on a survey on infant and young child feeding conducted in Hong Kong from February to September 2010. The study has been described in more details in a report (Woo et al. 2012). In brief, the participating families were randomly selected from the registry of 29 Maternal and Child Health Centres (MCHCs) in Hong Kong. Over 90% of babies born to local parents are registered with MCHCs which provide free child health services to children aged 0 to 5. The inclusion criteria for this study: (1) both parents being Chinese; Hong Kong citizens, defined as holders of Hong Kong Identity Card; Cantonese‐speaking; read and write Chinese; (2) the child being born at a gestational age of at least 37 weeks; and (3) parents with children aged 6–48 months. Exclusion criteria included child being suffered from any chronic medical illness or major congenital abnormalities requiring specialist care or long‐term follow up. This survey was approved by the Ethics Committee of the Department of Health. Written informed consent was obtained from all participating parents. A total of 1272 parent–child pairs were included in the data analysis for the original survey, in which respondents' children were divided into age group of 6‐ (n = 177, 13.9%), 9‐ (n = 164, 12.9%), 12‐ (n = 171, 13.4%), 18‐ (n = 233, 18.3%), 24‐ (n = 314, 24.7%) and 48‐month (n = 213, 16.7%). Data of 649 children of 18–48 months were included in the current study.
Children aged 18–48 months were chosen in this study as local recommendation advises parents to wean their children from bottle to training cup by the 14th month (Oral Health Education Unit & Department of Health Hong Kong SARG 2013). In addition, children of this age group are in the process of weaning or transitioning to an adult diet, resulting in increased variety in their diet compared with relying on milk as the major source of nutrition in younger children.
Data collection
Research assistants specially trained for the survey were responsible for data collection. Face to face interview took place in the MCHC at which participating children were registered. A standardized questionnaire was administered by the research staff to collect the socio‐demographic information of the index child and the parents. It included the child's gender, age and number of siblings. Parents' age, education attainment, employment status, whether they were born in Hong Kong, marital status and monthly family income were also collected.
Anthropometric data
Body weight of the child was measured by nurses at the MCHC. Seca electronic scale was used to measure children aged 18 months or above to the nearest 0.1 kg. Supine length was measured for children below 24 months of age using measuring mat of graduation 0.5 cm, while standing height was measured to the nearest 0.1 cm for children aged 24 months or above by Seca 242 measuring rod. Weight, height and BMI were transformed to age‐sex standardized z‐score based on the WHO Child Growth Standard (World Health Organization 2006). The proportion of children with wasting (BMI for age z‐score below −2), normal (BMI for age z‐score ≥ −2 to ≤1), possible risk of overweight (BMI for age z‐score >1 and ≤2) and ‘overweight or obesity’ (BMI for age z‐score over 2) was estimated with reference to the WHO Child Growth Standard.
Dietary assessment
To estimate the dietary intake of a child, 3‐day dietary record forms (2 weekdays and 1 weekend day) were completed (Crawford et al. 1994). Tools such as standard feeding utensils, rubber food model, a ‘food portion size and utensil guide’ and grid and circles of various sizes were provided to standardize the reporting and recording of quantity of food consumed (Woo et al. 2012). A face‐to‐face interview was carried out at the MCHC. The interviewer checked the dietary record completed for the previous day with the participating parent or the caregiver who were familiar with the child's food intake. After the first day dietary record was completed, blank dietary record forms were given to participants in order to record the child's diet in two additional assigned days. A follow‐up phone interview was then arranged, usually within 14 days of the first dietary interview, to collect dietary records of the two additional days. Dietary records of daily food consumption were analyzed using nutritional analysis software CompEat Pro Version 5.8.0 (UK). Food composition of Chinese foods and local foods were also added to the software based on food composition tables from China (Yang et al. 2002; Yang et al. 2004) and the Centre for Food Safety, Hong Kong (Centre for Food Safety 2006).
Utensils for milk drinking
A questionnaire was developed to obtain data regarding the milk consumption behaviour of the children. Parents were requested to report the milk drinking utensils for the children in the preceding 7 days, and available options included milk bottle, cup with a straw, trainer cup and regular cup. Regarding the milk drinking utensils, children were categorized to three different groups, namely bottle users (i.e. exclusive use of milk bottle), bottle plus cup users (i.e. use both milk bottle and cup of any types including cup with a straw, trainer cup or regular cup) and non‐bottle users (i.e. exclusive use of cup of any type).
Perceptions and knowledge about milk
Parents were requested to complete a self‐developed questionnaire with eight statements concerning their opinion on the importance of milk, in particular formula milk as part of children's diet.
Statistical analysis
The total amount of each food and beverage consumed over the three‐day period was summed, and the average amount of each food and beverage per day was calculated. Each food or beverage was assigned major food groups according to the local food pyramid for children of 2–5 years old (Central Health Education 2014). Daily food group consumption was presented by means and standard deviations (SD) or median (interquartile range (IQR)) where appropriate.
Statistical analyses were performed with the statistical package SPSS version 21.0 (SPSS Inc., Illinois, US). Data was checked for normality by descriptive analysis. Differences in daily food group consumption by age group and by utensils for milk drinking were compared using non‐parametric Kruskal Wallis test and Mann–Whitney U test for non‐normally distributed variables and one‐way ANOVA, Bonferroni Post‐hoc tests and independent t‐test for normally distributed variables. Multiple linear regression was used to assess whether bottle milk feeding was associated with BMI z‐score, with adjustment for socio‐demographic factors. Multivariate logistic regression analysis was performed to identify which of the socio‐demographic characteristics were associated with the use of milk bottle (both bottle users and bottle plus cup users were considered as using milk bottle). Categorical independent variables used in the multivariate regression models were child's gender, being first time parents (yes/no), father's or mother's age (<35 years/≥35 years), father's or mother's education level (secondary 3 or less/secondary 4–7/tertiary or above), maternal employment status (full‐time or part‐time employment/unemployed), being a local‐born mother (yes/no), monthly family income (<HK$20 000/HK$20 000 to HK$39 000/HK$40 000 or above) and living with maid (yes/no).
According to the Quarterly Report on General Household Survey published by the Census and Statistics Department, the median monthly household income in Hong Kong in the year of 2015 was HK$25 000. Therefore, the levels of household income as categorized in the analysis could be relatively regarded as low income family (<HK$20 000), middle‐class family (HK$20 000 to HK$39 999) and high income family (HK$40 000 or above) (Census and Statistics Department 2015). Moreover, unlike in many western countries, family‐friendly policies to promote work–family balance, such as family care leaves and flexible work‐time are not common in Hong Kong. Under such situation, hiring maid has become a popular choice for Hong Kong family (Cheung 2014). Therefore, living with maid is likely to have been a marker for a working mother and/or an affluent family. The level of significance was set as p < 0.05 and two sided.
Results
Sample characteristics
A total of 649 children aged 18–48 months were included in data analysis. The number of children aged 18‐, 24‐ and 48‐month old were 207 (32%), 277 (43%) and 165 (25%) and the mean (95% CI) for age of each age group were 18.4 (18.4–18.4), 24.5 (24.5–24.6) and 49.3 (49.2–49.4) months, respectively. The numbers of girls in the 18‐, 24‐ and 48‐month age groups were 126 (61%), 117 (42%) and 78 (47%), respectively. Characteristics of the children presented as a whole and by categories of bottle milk feeding are shown in Table 1.
Table 1.
Demographics by categories of bottle milk feeding
| Characteristics, n (%) | Overall (n = 649) | Non‐bottle milk feeding (n = 115) | Bottle plus cup milk feeding (n = 86) | Bottle milk feeding only (n = 448) | P a |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 328 (50%) | 63 (54%) | 46 (53%) | 219 (48%) | 0.445 |
| Female | 321 (49%) | 52 (45%) | 40 (46%) | 229 (51%) | |
| Age group (months) | |||||
| 18 | 207 (32%) | 7 (6%) | 16 (19%) | 184 (41%) | <0.001 |
| 24 | 277 (43%) | 31 (27%) | 44 (51%) | 202 (45%) | |
| 48 | 165 (25%) | 77 (67%) | 26 (30%) | 62 (14%) | |
| Paternal age (years) | |||||
| Below 35 | 172 (26%) | 26 (22%) | 26 (30%) | 120 (26%) | 0.466 |
| 35 or above | 477 (73%) | 89 (77%) | 60 (69%) | 328 (73%) | |
| Maternal age (years) | |||||
| Below 35 | 283 (43%) | 38 (33%) | 45 (52%) | 200 (44%) | 0.018 |
| 35 or above | 366 (56%) | 77 (67%) | 41 (47%) | 248 (55%) | |
| Paternal education level | |||||
| Below Form 3 | 123 (19%) | 22 (19%) | 14 (16%) | 87 (19%) | 0.034 |
| Form 4‐7 | 266 (41%) | 42 (36%) | 26 (30%) | 198 (44%) | |
| Tertiary or above | 260 (40%) | 51 (44%) | 46 (53%) | 163 (36%) | |
| Maternal education level | |||||
| Below Form 3 | 107 (16%) | 18 (15%) | 9 (10%) | 80 (17%) | 0.008 |
| Form 4‐7 | 294 (45%) | 53 (46%) | 29 (33%) | 212 (47%) | |
| Tertiary or above | 248 (38%) | 44 (38%) | 48 (55%) | 156 (34%) | |
| Employment status of mother | 0.997 | ||||
| Full‐time or part‐time | 414 (63%) | 73 (63%) | 55 (64%) | 286 (63%) | |
| Unemployed | 235 (36%) | 42 (36%) | 31 (36%) | 162 (36%) | |
| Local born mother | |||||
| Yes | 458 (70%) | 83 (72%) | 58 (67%) | 317 (70%) | 0.758 |
| No | 191 (29%) | 32 (27%) | 28 (32%) | 131 (29%) | |
| Monthly family income (HK$) | |||||
| <$20 000 | 182 (28%) | 39 (33%) | 21 (25%) | 122 (27%) | 0.03 |
| $20 000–39 999 | 265 (40%) | 34 (29%) | 32 (38%) | 199 (44%) | |
| ≥$40 000 | 196 (30%) | 42 (36%) | 31 (36%) | 123 (27%) | |
| Living with maid | |||||
| Yes | 284 (43%) | 53 (46%) | 48 (55%) | 183 (40%) | 0.032 |
| No | 365 (56%) | 62 (53%) | 38 (44%) | 265 (59%) | |
| First time parents | |||||
| Yes | 372 (57%) | 64 (55%) | 55 (64%) | 253 (56%) | 0.354 |
| No | 274 (42%) | 51 (44%) | 30 (35%) | 193 (43%) |
Difference by the categories of bottle milk feeding was tested by Chi‐square test.
Utensils for milk drinking
Overall, milk bottle was used exclusively by 448 (69.0%) children for milk drinking. Although the locally recommended age of stopping milk bottle use was 14 months, 446 (92.1%) and 88 (53.3%) children in the 18 to 24‐month group and 48‐month group, respectively, were still using the bottle for milk drinking.
Food group consumption by age group
The daily food group consumption is shown in Table 2. There were significant differences in daily intakes of all the major food groups between children of 18–24 months and 48 months (p < 0.05). Daily consumption of grains, vegetables, fruits, meat and meat alternatives, non‐formula milk and other dairy products were significantly higher while intake of formula milk was significantly lower among 48‐month‐old children than 18 to 24‐month group. Because of the differences in food group consumption between the two age groups, the analyses were separately done for each age group.
Table 2.
Comparison of food group consumption between 18 and 24‐month children and 48‐month‐old children
| Food group | 18–24 month old (n = 484) | 48 month old (n = 165) | P a |
|---|---|---|---|
| Mean + SD/Median (IQR) | |||
| Milk and alternatives (g) | 468 + 161 | 291 + 177 | <0.001 |
| Fluid milk (ml) | 457 + 162 | 271 + 175 | <0.001 |
| Formula milk (ml)b | 447 + 169 | 228 + 181 | <0.001 |
| Non‐formula milk (ml)c | 0 (0–0) | 0 (0–67) | <0.001 |
| Other dairy products (g)d | 0 (0–10) | 6 (0–33) | <0.001 |
| Grains (g)e | 311 + 147 | 334 + 99 | 0.023 |
| Vegetables (g)f | 58 (30–98) | 74 (56–113) | <0.001 |
| Fruits (g)g | 53 (25–93) | 72 (43–112) | <0.001 |
| Meat and meat alternatives (g)h | 66 + 39 | 104 + 47 | <0.001 |
Group difference was examined by independent t‐test or Mann–Whitney U test where appropriate.
Formula milk included cow‐based, goat‐based and soy‐based formula and special formula.
Non‐formula milk included breast milk, cow's milk, soy milk and other types of milk.
Other dairy products included cheese, yoghurt and ice cream.
Grains included breakfast cereals, breads, noodles and pasta, rice, congee, pastries and crackers.
Vegetables included any types of vegetables, potato, mushroom and seaweeds.
Fruits included fresh, dried and canned fruits.
Meat and meat alternatives include egg, fish and fish products, legumes, meat, poultry, shellfish, soybean and products.
Food group consumption by categories of bottle milk feeding
Among the 18 to 24‐month group of children, bottle users (p < 0.001) or bottle plus cup users (p = 0.001) had significantly higher intake of milk and alternatives than non‐bottle users. In particular, the consumption of formula milk was significantly greater among the bottle users (p < 0.001) and bottle plus cup users (p = 0.001) than non‐bottle users (Table 3). In addition, bottle users had significantly lower intake of meat and meat alternatives than bottle plus cup users (p = 0.001). Consumption of sugar‐containing fluids was significantly lower among bottle milk‐feeding children (p = 0.003). Daily absolute energy and protein intake were not associated with categories of bottle milk feeding. Among non‐bottle users, bottle plus cup users and bottle users, the median (IQR) total daily energy intake (in kcal) were, respectively, 974 (834–1061), 982 (869–1111) and 960 (830–1110) for the 18 to 24‐month group. However, the percent calorie and protein intake from formula milk were significantly greater in bottle or bottle plus cup users than non‐bottle users (p < 0.05, Table 3).
Table 3.
Food group and nutrient intakea by categories of bottle milk feeding in children of 18–24 months old and 48 months old
| Food group and nutrient intake | 18–24 months | 48 months | ||||||
|---|---|---|---|---|---|---|---|---|
| Non‐bottle milk feeding (n = 38) | Bottle plus cup milk feeding (n = 60) | Bottle milk feeding only (n = 386) | p b | Non‐bottle milk feeding (n = 77) | Bottle plus cup milk feeding (n = 26) | Bottle milk feeding only (n = 62) | p b | |
| Milk and alternatives (g) | 333 + 161c, d | 453 + 136 | 484 + 158 | <0.001 | 217 (111–285)c, d | 382 (219–562) | 309 (207–463) | <0.001 |
| Formula milk (ml)f | 290 + 183c, d | 413 + 150e | 467 + 161 | <0.001 | 100 (0–216)c, d | 335 (179–444) | 270 (181–450) | <0.001 |
| Non‐formula milk (ml)g | 0 (0–0) | 0 (0–39)e | 0 (0–0) | <0.001 | 2.0 (0–103)d | 1.3 (0–80) | 0 (0–7) | 0.003 |
| Other dairy products (g)h | 3.9 (0–33)d | 0 (0–27) | 0 (0–6) | 0.005 | 5 (0–29) | 12 (0–48) | 7 (0–33) | 0.340 |
| Other non‐milk fluids (ml) | ||||||||
| Sugar‐containing fluids (ml)i | 41 (0–78)c, d | 0 (0–33) | 0 (0–39) | 0.003 | 60 (0–117) | 29 (0–74) | 67 (0–100) | 0.184 |
| Grains (g) | 309 (209–393) | 282 (211–372) | 282 (193–387) | 0.871 | 337 + 92 | 347 + 124 | 325 + 98 | 0.616 |
| Vegetables (g) | 52 (22–110) | 62 (35–100) | 57 (30–97) | 0.679 | 77 (60–113) | 75 (50–112) | 71 (46–119) | 0.488 |
| Fruits (g) | 62 (19–117) | 65 (32–99) | 53 (24–88) | 0.297 | 79 (55–127)c | 67 (42–102) | 55 (27–105) | 0.041 |
| Meat and meat alternatives (g) | 72 (42–92) | 74 (51–95)e | 55 (36–86) | 0.002 | 111 + 51 | 100 + 35 | 97 + 47 | 0.238 |
| Percent of energy and nutrients from formula milk (%) | ||||||||
| Energy | 21.8 + 14.1c, d | 30.1 + 12.1e | 34.9 + 12.8 | <0.001 | 6.0 (0.0–14.8)c, d | 19.5 (13.2–27.3) | 19.1 (11.0–27.0) | <0.001 |
| Protein | 19.0 (12.8–26.0)d | 24.8 (18.3–32.0)e | 30.4 (23.1–38.8) | <0.001 | 5.5 (0.0–15.8)c, d | 19.1 (10.6–28.4) | 17.2 (11.6–27.7) | <0.001 |
| Iron | 41.7 (32.9–55.8)c, d | 54.6 (43.3–65.1)e | 60.8 (51.3–69.5) | <0.001 | 14.3 (0.0–37.8)c, d | 40.7 (28.9–53.5) | 40.1 (30.1–54.0) | <0.001 |
Presented as mean + SD or median (IQR).
Group difference was examined by one‐way ANOVA or Kruskal Wallis test where appropriate.
For food group with p < 0.05 in ANOVA or Kruskal Wallis Test, Bonferroni Post‐hoc test or Mann–Whitney U test were used, respectively, to compare the amount of food group consumption or percent of energy and nutrients from formula milk between two independent groups of categories of bottle milk feeding of same age.
p < 0.05 (non‐bottle milk feeding vs. bottle plus cup milk feeding).
p < 0.05 (non‐bottle milk feeding vs. bottle milk feeding only).
p < 0.05 (bottle plus cup milk feeding vs. bottle milk feeding only).
Formula milk included cow‐based, goat‐based and soy‐based formula and special formula.
Non‐formula milk included breast milk, cow's milk, soy milk and other types of milk.
Other dairy products included cheese, yoghurt and ice cream.
Included 100% fruit juice, carbonated drinks, baby fruit juice, fruit drinks, honey diluting with water and other beverages (cocoa and other instant powdered drinks, and sports drink).
For the 48‐month group, bottle users or bottle plus cup users had significantly greater intake of milk and alternatives than non‐bottle users (p < 0.001). Consumption of formula milk was greater among bottle users than non‐bottle users (p < 0.05) (Table 3). Regarding the consumption of fruits, bottle users had significantly lower intakes than non‐bottle users (p = 0.015). No significant association between consumption of sugar‐containing fluids and categories of bottle milk feeding was found among 48‐month group. Categories of bottle milk feeding were not associated with daily absolute energy and protein intake. Among non‐bottle users, bottle plus cup users and bottle users, the median (IQR) total daily energy intake (in kcal) were, respectively, 1206 (1056–1328), 1254 (1045–1463) and 1135 (1020–1338) for the 48‐month group. However, the percentages of energy and protein intake from formula milk were significantly greater among bottle or bottle plus cup users than non‐bottle users (p < 0.001, Table 3)
Formula milk consumption by parents' perception about milk
Among the 18 to 48‐month groups, formula milk consumption was significantly greater for children of parents who had misconception about milk. For children of parents who agreed/strongly agreed ‘milk is indispensable for the growth and development of a child’ (405 + 196 vs. 314 + 181, p < 0.001), ‘milk should still be major part of a child's diet’ (476 + 179 vs. 356 + 193, p < 0.001), ‘a child must drink milk to obtain adequate calcium’ (417 + 191 vs. 359 + 200, p < 0.001) and ‘follow‐up formulae are more suitable for the 1‐to‐4‐year‐olds than cow milk’ (403 + 182 vs. 346 + 235, p = 0.002), the consumption of formula milk (ml) was significantly greater than those who disagreed/strongly disagreed with the statements (data not shown).
BMI z‐score and categories of bottle milk feeding
Among the 18 to 24‐month children, although not statistically significant, the BMI z‐score of bottle users (mean + SD = 0.21 + 0.93, n = 386) tended to be higher than that of the bottle plus cup users (mean + SD = 0.14 + 0.91, n = 60) and the non‐bottle users (mean + SD = −0.08 + 0.91, n = 38) (p = 0.169). For the 48‐month children, there were significant differences in the BMI z‐score among bottle users (mean + SD = 0.46 + 1.00, n = 62), bottle plus cup users (mean + SD = −0.02 + 0.75, n = 26) and non‐bottle users (mean + SD = 0.04 + 0.89, n = 77) (p = 0.017). However, the risk of overweight and overweight status with reference to the WHO definition was not associated with categories of bottle milk feeding among our study samples (p > 0.05) (Fig. 1). When the two age groups were combined for analysis, the BMI z‐score of the bottle users (mean + SD = 0.25 + 0.95, n = 448) was significantly higher than non‐bottle users (mean + SD = 0.00 + 0.90, n = 115) (p = 0.035), and this association remained significant after adjusting for socio‐demographic factors (B = 0.308, 95% CI = 0.09 to 0.53, p = 0.006, Table 4).
Figure 1.
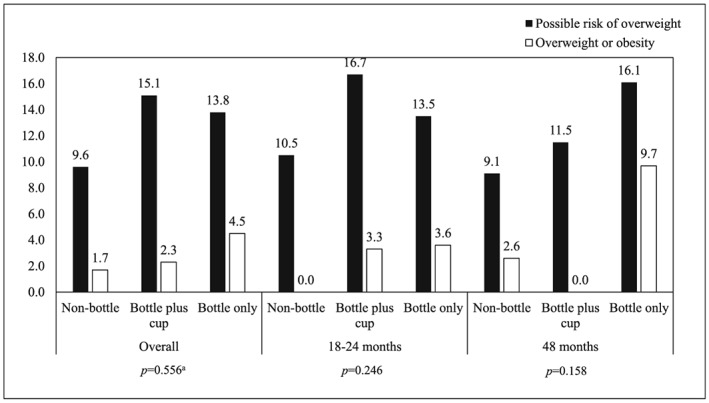
Percentage of possible risk of overweight and overweight or obesity with reference to WHO Child Growth Standard by categories of bottle milk feeding in overall sample, 18 to 24‐month group and 48‐month group. (Possible risk of overweight is defined as BMI for age z‐score >1 and ≤2; Overweight or obesity is defined as BMI for age z‐score over 2) aGroup difference among three categories of utensils for milk drinking was examined by Chi‐square test.
Table 4.
Multiple linear regression analysis of the factors associated with BMI z‐score among 18 and 48‐month children
| Socio‐demographic factors | B | 95% CI | p |
|---|---|---|---|
| Child's characteristics | |||
| Categories of bottle milk feeding (bottle only = 1, non‐bottle = 0) | 0.308 | 0.09–0.53 | 0.006 |
| Categories of bottle milk feeding (bottle plus cup = 1, non‐bottle = 0) | 0.126 | −0.15–0.40 | 0.366 |
| Gender (M = 0, F = 1) | 0.045 | −0.10–0.19 | 0.542 |
| Age (months) | 0.005 | 0.00–0.01 | 0.156 |
| Living with maid (Yes = 0, No = 1) | −0.076 | −0.25–0.10 | 0.397 |
| Being first‐time parents (Yes = 0, No = 1) | −0.132 | −0.30–0.03 | 0.113 |
| Mother's characteristics | |||
| Age (years) (below 35 = 0, 35 or above = 1) | −0.033 | −0.22–0.15 | 0.729 |
| Educational level (Form 1‐3 or less = 0, Form 4‐7 = 1) | 0.021 | −0.23–0.27 | 0.866 |
| Educational level (Form 1‐3 or less = 0, Tertiary = 1) | −0.134 | −0.44–0.18 | 0.397 |
| Employment status (working = 1, unemployed = 0) | −0.091 | −0.28–0.10 | 0.338 |
| Born in Hong Kong (Yes = 0, No = 1) | 0.093 | −0.10–0.28 | 0.319 |
| Father's characteristics | |||
| Age (years) (below 35 = 0, 35 or above = 1) | −0.174 | −0.38–0.04 | 0.105 |
| Educational level (Form 1‐3 or less = 0, Form 4‐7 = 1) | −0.034 | −0.26–0.19 | 0.764 |
| Educational level (Form 1‐3 or less = 0, Tertiary = 1) | −0.095 | −0.37–0.18 | 0.500 |
| Monthly family income | |||
| <$20 000 vs. $20 000–39 999 | −0.097 | −0.32–0.13 | 0.391 |
| <$20 000 vs. ≥$40 000 | −0.098 | −0.38–0.19 | 0.498 |
Socioeconomic factors and categories of bottle milk feeding
Multivariate logistic regression was performed to identify those socio‐demographic factors independently associated with the use of bottle (children who were exclusively bottle‐fed or fed with both bottle and cup were considered as bottle users in logistic regression). Socio‐demographic factors were not associated with use of bottle in 18 to 24‐month children while higher paternal education level was associated with lower risk of bottle use among 48‐month children (OR = 0.202, 95% CI = 0.06 to 0.73, p = 0.015). Because of similar results for the two age groups, results were combined for presentation, with consideration of child's age (Table 5). Overall, only two factors were found to be significant, these were child's age (older child has OR = 0.912 (95% CI: 0.89–0.93) comparing with younger child) and monthly family income (income of $20 000–39 999 has OR = 2.363 (95% CI: 1.14–4.90, p = 0.021) comparing with income below $20 000), which means older children and children from family with income of less than $20 000 were less likely to use bottle.
Table 5.
Multivariate logistic regression analysis of the factors associated with the use of milk bottlea among 18 to 48‐month children
| Odds ratio (95% CI) | p | |
|---|---|---|
| Child's sex (female) | 1.164 (0.73–1.86) | 0.528 |
| Child's age | 0.912 (0.90–0.93) | <0.001 |
| Paternal age (35 or above)b | 1.795 (0.86–3.76) | 0.121 |
| Maternal age (35 or above)b | 0.815 (0.42–1.57) | 0.540 |
| Paternal education level (Form 4‐7)c | 1.028 (0.50–2.13) | 0.940 |
| Paternal education level (Tertiary)c | 0.699 (0.29–1.69) | 0.428 |
| Maternal education level (Form 4‐7)c | 0.825 (0.37–1.86) | 0.643 |
| Maternal education level (Tertiary)c | 0.900 (0.33–2.48) | 0.838 |
| Employment status of mother (unemployed) | 0.870 (0.47–1.61) | 0.656 |
| Non‐local born mother | 1.182 (0.65–2.16) | 0.587 |
| Monthly family income ($20 000–39 999)d | 2.363 (1.14–4.90) | 0.021 |
| Monthly family income (≥$40 000)d | 1.254 (0.50–3.14) | 0.628 |
| Not living with maid | 1.170 (0.66–2.06) | 0.587 |
| Non‐first time parents | 0.870 (0.52–1.45) | 0.594 |
The use of milk bottle referred to both the bottle users and the bottle plus cup users.
Compared with paternal or maternal age below 35.
Compared with paternal or maternal education level Form 3 or below.
Compared with monthly family income below $20 000.
Discussion
This report described an association between prolonged bottle use for milk drinking at or beyond 18 months and greater intake of formula milk, lower intake of other food groups (grains, vegetables, fruits, meat and meat alternatives) and higher BMI z‐score, and certain socio‐demographic characteristics were associated with prolonged use of milk bottle.
Bottle milk feeding and food group consumption
Our findings supported those found in previous studies which showed significant association of bottle use and milk consumption (Lampe & Velez 1997; Safer et al. 2001; Northstone et al. 2002). Utensil for milk drinking affects the amount of milk consumed in our samples, with the children who continued to receive bottles (either bottle only or with cup) drinking at least 1.5 times as much formula milk as those who have fully weaned off the bottle. In Northstone's study (Northstone et al. 2002), a significantly greater mean volume of milk was consumed by children of 18 months old who used a bottle (488 ml/day) compared with those who used cup plus bottle (454 ml/day) and cup only (381 ml/day). The finding was similar to that in our survey. However, contrary to our report which found a high popularity of formula milk among 18 to 48‐month‐old children, Northstone showed that cow's milk was the most frequently consumed with 94% having it at least once a day, while only 3.5% had formula milk at 18 months of age (Northstone et al. 2002). The fact that children in our study were still using formula milk even until 48 months old may be explained by parents' misconception about milk as shown in this study. Apart from the misconception, milk formulas are now central to marketing strategies for promoting baby food sales in China and other Asia Pacific countries (Euromonitor International 2011). These formulas are often marketing in a way that confuses consumers by making health claims and marketing ‘convenience’ to time pressed urban parents in Hong Kong (Euromonitor International 2015). These reasons may explain the high consumption of formula milk for Hong Kong children.
Despite the finding of significantly greater milk intake in the bottle users vs. non‐bottle users in our study, the median total caloric intake was not associated with utensils for milk drinking, which is consistent with previous finding (Safer et al. 2001). It also supports the observation of Birch (Birch et al. 1991) that children of this age are capable of self‐regulation. Birch's study showed that the total caloric intake for 2–5 years old children who received energy‐dense items was nearly identical across 2‐day blocks to those received the low‐fat substitutes. Similarly, in our findings, the percentage of energy intake from formula milk was significantly higher in bottle users than non‐bottle users. It appears that the bottle users in our study accommodate the extra calories from formula milk by displacing their appetite for other nutritious food. Therefore, although not statistically significant, in general, our study found that the amount of food group consumption other than milk and alternatives was lower for exclusive bottle users compared with non‐bottle users or bottle plus cup users. Although formula milk could possibly provide an appropriate balance of nutrients for children and its role in limiting the intake of equivalence nutrients from other foods seems to of less concern, the reasons for concern about bottle use should not be limited to nutrient intake and BMI, but also developmental skills and exposure to food variety in early childhood. Transitioning to a varied diet and using a cup at the appropriate time is important for natural developmental skills such as chewing. If chewing is not encouraged, this ability may not develop readily and teaching older infants to chew can be difficult. Moreover, introducing a variety of foods during the early stages of complementary feeding to favour the establishment of preferences for these foods early in childhood is essential for preventing or reducing the risk of diet‐related diseases in adulthood (Paul et al. 2009).
Bottle milk feeding and BMI z‐score
If calories obtained are in excess of the child's needs, this could contribute to weight gain over time (Butte & Ellis 2003; Disantis et al. 2011). In Chinese culture, the society admires caregivers who raise a heavier baby and believes that they are demonstrating high levels of parenting quality and competence. Therefore, caregivers may be affected by normative concept that chubby babies are healthy babies and continue to bottle‐feed children to promote weight gain (Zhang et al. 2013). However, parental use of pressuring feeding practice was positively associated with greater energy intake of the child because of a lack of responsiveness to children's cues of hunger and satiety (Frankel et al. 2012; Thompson et al. 2013). Data on caregivers' feeding styles and the maids' role in child care were not collected in the present study, and the association of these factors with BMI z‐score in Chinese young children deserves further investigation.
In our study, the use of a bottle at 18–24 months of age was not associated with BMI z‐score. However, exclusive bottle users had significantly higher BMI z‐score compared with non‐bottle users for 48‐month group. When the two age groups were combined for analysis, BMI z‐score of the bottle users was significantly higher than non‐bottle users, even after controlling socio‐demographic factors. The trend is consistent with previous studies, which demonstrated that the later the age of bottle‐weaning, the greater the child's risk of overweight or obesity in multivariate analysis (Bonuck et al. 2004; Gooze et al. 2011). However, our study was limited by the lack of data on whether fluids except milk, such as fruit juice, instant powdered drinks and carbonated drinks, were given from bottle or cup because this factor may also influence the study outcomes
Use of bottle for milk drinking and socio‐demographic characteristics
Previous work in developed countries showed that socio‐demographic features of parents were associated with prolonged bottle‐feeding in toddlers (Kaste & Gift 1995; Hammer et al. 1999; De La Hunty et al. 2000). These included poverty, urban residence and low parental educational attainment (Kaste & Gift 1995). A study of middle‐class, well‐educated mothers reported that those returning to work during the first 3 months postpartum weaned later from the bottle than women returning to work later or not at all in the first 2 years (Hammer et al. 1999). A national survey in the United Kingdom found that mothers of children at 14 months who reported using feeding bottles were more likely to be younger, from manual social classes and left schools prematurely (De La Hunty et al. 2000). However, employment status, educational level and age of mother were not associated with prolonged bottle‐feeding in our sample. Interestingly, our study showed that children of family with lower monthly income (below $20 000) were less likely to be fed by bottle compared with children of family with higher income ($20 000–$39 999). The reason might be that economically affluent families can afford to buy milk formula (Mazumder & Hossain 2012) compared with low income families. The findings of significant association of bottle use with paternal education level and family income among the 48‐month group but not the 18 to 24‐month group may also suggest that health‐care professional should consider potential target groups, the appropriate intervening period, focus and content of the program when planning bottle‐weaning intervention.
Limitations
Certain study limitations should be noted. First, the group who use bottle plus cup were not questioned as to how frequently the bottle and the cup were used, and whether bottle use was common prior to bed time was not known. Second, only data on the drinking utensils for milk consumption were available in the study. Whether non‐milk fluids were given from bottle or cup is not known as this data was not collected in the study. Self‐regulation is more commonly seen in breastfed babies and less common if caregivers bottle‐feed the children instead of letting them self‐feed from the bottles. However, the questions on how long the group has been breastfed and how the bottles were used were not investigated in the present study. In addition, the cross‐sectional design of the study limits our ability to draw a causal inference.
Conclusions
In conclusion, our study found that the utensil for milk drinking affected the amount of formula milk consumed. The consumption of food groups other than milk and alternatives was lower for exclusive bottle users compared with non‐bottle users or bottle plus cup users. Among the 48‐month group, exclusive bottle use was associated with higher BMI z‐score. Given that it can be difficult to remove a bottle from an older child as well‐established habits are hard to break, and the long‐term consequences of childhood obesity, it is essential for care‐givers to plan and provide bottle‐weaning intervention in a timely manner.
Source of funding
The work was supported by the Centre for Nutritional Studies, The Chinese University of Hong Kong. None of the authors had a conflict of interest.
Conflicts of interest
The authors declare that they have no conflict of interest.
Contributions
SY carried out the statistical analysis, interpretation of findings and writing the manuscript. RC contributed to the analysis plan, interpretation of findings and revising the manuscript for important intellectual content. LL involved in data management, and revised the manuscript for important intellectual content. SL and JW contributed to the study design and revised the manuscript for important intellectual content. All authors read the manuscript and approved the final submission.
Acknowledgment
We would like to thank all participating families. Special thanks are given to all research colleagues of the Family Health Service of the Department of Health for their involvement in the study.
Yeung, S. , Chan, R. , Li, L. , Leung, S. , and Woo, J. (2017) Bottle milk feeding and its association with food group consumption, growth and socio‐demographic characteristics in Chinese young children. Maternal & Child Nutrition, 13: e12341. doi: 10.1111/mcn.12341.
References
- American Academy of Pediatrics (2008) Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, Third edn. American Academy of Pediatrics: Elk Grove Village, IL. [Google Scholar]
- Avery A. & Baxter A. (2001) ‘Change to cup’: an audit to determine parental awareness and practices in changing from bottle to cup. Journal of Human Nutrition and Dietetics 14, 217–223. [DOI] [PubMed] [Google Scholar]
- Birch L.L., Johnson S.L., Andresen G., Peters J.C. & Schulte M.C. (1991) The variability of young children's energy intake. New England Journal of Medicine 324, 232–235. [DOI] [PubMed] [Google Scholar]
- Bonuck K., Kahn R. & Schechter C. (2004) Is late bottle‐weaning associated with overweight in young children? Analysis of NHANES III data. Clinical Pediatrics (Phila) 43, 535–540. [DOI] [PubMed] [Google Scholar]
- Bonuck K.A. & Kahn R. (2002) Prolonged bottle use and its association with iron deficiency anemia and overweight: a preliminary study. Clinical Pediatrics (Phila) 41, 603–607. [DOI] [PubMed] [Google Scholar]
- Butte N.F. & Ellis K.J. (2003) Comment on “Obesity and the environment: where do we go from here?”. Science 301, 598; author reply 598. [DOI] [PubMed] [Google Scholar]
- Cheung A.K.L. (2014) Hiring domestic help and family well‐being in Hong Kong: a propensity score matching analysis. Journal of Comparative Family Studies 45, 475–495. [Google Scholar]
- Central Health Education (2014) Healthy eating food Pyramid for Children 2–5 years old [Online]. Hong Kong SAR: Department of Health. Available at: http://www.cheu.gov.hk/files/her/exn_nutp_027bp.pdf [Accessed 1 December 2014].
- Census and Statistics Department (2015). Quarterly Report on General Household Survey, Second Quarter 2015 [Online]. Hong Kong SAR: Census and Statistics Department. Available at: http://www.statistics.gov.hk/pub/B10500012015QQ04B0100.pdf [Accessed 29 April 2016]
- Centre for Food Safety (2006) Nutrient information inquiry [Online]. Hong Kong SAR: Centre for Food Safety. Available at: http://www.cfs.gov.hk/english/notices/notices.html [Accessed 3 January 2011].
- Crawford P.B., Obarzanek E., Morrison J. & Sabry Z.I. (1994) Comparative advantage of 3‐day food records over 24‐hour recall and 5‐day food frequency validated by observation of 9‐ and 10‐year‐old girls. Journal of the American Dietetic Association 94, 626–630. [DOI] [PubMed] [Google Scholar]
- De La Hunty A., Lader D. & Clarke P.C. (2000) What British children are eating and drinking at age 12–18 months. Journal of Human Nutrition and Dietetics 13, 83–86. [Google Scholar]
- Disantis K.I., Hodges E.A., Johnson S.L. & Fisher J.O. (2011) The role of responsive feeding in overweight during infancy and toddlerhood: a systematic review. International Journal of Obesity 35, 480–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Euromonitor International (2011) Safety First: Global Baby Food Opportunities and Challenges to 2015. Euromonitor International: London and Chicago. [Google Scholar]
- Euromonitor International (2015) Global Baby Food Overview: Key Categories, Countries and Trends. Euromonitor International: London and Chicago. [Google Scholar]
- Family Health Service (2012) A Survey of Infant and Young Child Feeding in Hong Kong: Milk Consumption [Online]. Family Health Service, The Department of Health, HKSAR. Available at: http://www.fhs.gov.hk/english/archive/files/reports/Survey_IYCF_milkconsumption_1904.pdf (Accessed 18 Mar 2015)
- Frankel L.A., Hughes S.O., O'Connor T.M., Power T.G., Fisher J.O. & Hazen N.L. (2012) Parental influences on children's self‐regulation of energy intake: insights from developmental literature on emotion regulation. Journal of Obesity 2012, 327259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gooze R.A., Anderson S.E. & Whitaker R.C. (2011) Prolonged bottle use and obesity at 5.5 years of age in US children. Journal of Pediatrics 159, 431–436. [DOI] [PubMed] [Google Scholar]
- Hammer L.D., Bryson S. & Agras W.S. (1999) Development of feeding practices during the first 5 years of life. Archives of Pediatrics and Adolescent Medicine 153, 189–194. [DOI] [PubMed] [Google Scholar]
- Kaste L.M. & Gift H.C. (1995) Inappropriate infant bottle‐feeding—status of the healthy people 2000 objective. Archives of Pediatrics and Adolescent Medicine 149, 786–791. [DOI] [PubMed] [Google Scholar]
- Koletzko B., Schiess S., Brands B., Hailie G., Demmelmair H., Von Kries R. et al. (2010) Infant feeding practice and later obesity risk. Indications for early metabolic programming. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 53, 666–673. [DOI] [PubMed] [Google Scholar]
- Koletzko B., Von Kries R., Closa R., Escribano J., Scaglioni S., Giovannini M. et al. (2009) Lower protein in infant formula is associated with lower weight up to age 2 y: a randomized clinical trial. American Journal of Clinical Nutrition 89, 1836–1845. [DOI] [PubMed] [Google Scholar]
- Lampe J.B. & Velez N. (1997) The effect of prolonged bottle feeding on cow's milk intake and iron stores at 18 months of age. Clinical Pediatrics 36, 569–572. [DOI] [PubMed] [Google Scholar]
- Mazumder M.S. & Hossain M.K. (2012) Duration of breastfeeding and its determinant in Bangladesh. International Journal of Natural Sciences 2, 49–53. [Google Scholar]
- Nice Public Health Guidance 11 (2008). Maternal and Child Nutrition [Online]. Available at: http://www.nice.org.uk/guidance/PH11 [Accessed 7‐Jan 2016].
- Northstone K., Rogers I., Emmett P. & Team A.S. (2002) Drinks consumed by 18‐month‐old children: are current recommendations being followed? European Journal of Clinical Nutrition 56, 236–244. [DOI] [PubMed] [Google Scholar]
- Oral Health Education Unit & Department of Health Hong Kong SARG (2013). Tooth Club. Oral Care for Infants [Online]. Department of Health Hong Kong SAR. Available at: http://www.toothclub.gov.hk/en/pnc/en_pnc_2_1_1_3.html#start (accessed 3 Mar 2015)
- Paul I.M., Bartok C.J., Downs D.S., Stifter C.A., Ventura A.K. & Birch L.L. (2009) Opportunities for the primary prevention of obesity during infancy. Advances in Pediatrics 56, 107–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safer D.L., Bryson S., Agras W.S. & Hammer L.D. (2001) Prolonged bottle feeding in a cohort of children: does it affect caloric intake and dietary composition? Clinical Pediatrics 40, 481–487. [DOI] [PubMed] [Google Scholar]
- Thompson A.L., Adair L.S. & Bentley M.E. (2013) Pressuring and restrictive feeding styles influence infant feeding and size among a low‐income African–American sample. Obesity (Silver Spring) 21, 562–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo J., Chan R., Li L. & Luk W.Y. (2012) A Survey of Infant and Young Child Feeding in Hong Kong: Diet and Nutrient Intake. HKSAR: Department of Medicine and Therapeutics, The Chinese University of Hong Kong & Family Health Service, The Department of Health, HKSAR. Available at: http://www.fhs.gov.hk/english/archive/files/reports/Survey_IYCF_Dietnutrient%20intake.pdf
- World Health Organization (2006) WHO Child Growth Standards based on length/height, weight and age. Acta Paediatrica. Supplement 450, 76–85. [DOI] [PubMed] [Google Scholar]
- Yang Y., Wang G. & Pan X. (2002) China Food Composition 2002. University Medical Press: Peking. [Google Scholar]
- Yang Y., Wang G. & Pan X. (2004) China Food Composition 2004. University Medical Press: Peking. [Google Scholar]
- Zhang J., Himes J.H., Guo Y., Jiang J., Yang L., Lu Q. et al. (2013) Birth weight, growth and feeding pattern in early infancy predict overweight/obesity status at two years of age: a birth cohort study of Chinese infants. PLoS One 8, e64542. [DOI] [PMC free article] [PubMed] [Google Scholar]


