Abstract
An alternative Community‐based Management of Acute Malnutrition model with community health workers (CHWs) delivering treatment for uncomplicated severe acute malnutrition (SAM) was piloted in Mali. The capacity of the CHWs to evaluate, classify, and treat cases of uncomplicated SAM, to provide nutritional counselling to caretakers of children receiving treatment for SAM, malaria, pneumonia or diarrhoea and to correctly refer cases of complicated SAM, was assessed. This was done using direct observation by trained enumerators of the management of SAM cases using checklists, re‐diagnosing the cases admitted for treatment and reviewing admissions cards and registers. One hundred twenty‐five cases, assessed and treated by the CHWs, were observed. The majority of children were correctly assessed for the presence of major clinical signs (cough, diarrhoea, fever, and vomiting; 97.6%), and similarly most children were checked for the presence of danger signs (95.2%). Mid‐upper arm circumference was correctly assessed in 96.8% of children and oedema was correctly assessed in 78.4% (The composite indicator, which includes all essential tasks to provide high‐quality treatment, was achieved in 79.5% of cases. This paper concludes that well‐trained and supervised CHWs are capable of managing cases of uncomplicated SAM. This suggests that such a strategy is an opportunity to increase access to quality treatment in Mali for SAM cases. However, further evidence is required to ensure that this level of care can be achieved at scale.
Keywords: child nutrition, community health workers (CHWs), Community‐based Management of Acute Malnutrition, quality of care, severe acute malnutrition (SAM)
Abbreviations
- CHW
community health worker
- iCCM
Integrated Community Case Management [of childhood illnesses]
- MAM
moderate acute malnutrition
- SAM
severe acute malnutrition
1. INTRODUCTION
Today, it is estimated that 16 million children younger than 5 years are suffering from severe acute malnutrition (SAM) globally (“WHO | UNICEF‐WHO‐The World Bank,” n.d.). The condition, which increases the risk of mortality nine folds, remains a significant global health challenge and is the cause of half a million deaths each year of children younger than 5 years. (Black et al., 2013) Until 10 years ago, treatment was delivered solely through hospitals, requiring prolonged inpatient stays. Although this approach delivered good clinical outcomes, it only reached 10% of the affected population within the facility catchment area and resulted in a high proportion of cases defaulting from treatment (Collins et al., 2006). In response to this limitation, and enabled by incorporating mid‐upper arm circumference (MUAC) measurement to assess nutritional status and the routine use of ready‐to‐use‐therapeutic food (RUTF) for treatment, an outpatient‐treatment model was developed.
The Community‐based Management of Acute Malnutrition model, formerly known as Community‐based Therapeutic Care, successfully treats SAM cases without medical complications in the home. The model's clinical outcomes match inpatient care, while also reaching a higher proportion of cases (Collins et al., 2006) and has been adopted by Ministries of Health and non‐governmental organisations alike. In 2014, over 3.2 million children were treated across 73 countries using the approach (UNICEF, 2014).
Despite the significant success of the outpatient model in improving the availability of effective treatment for uncomplicated SAM cases, recently available evidence shows that on average treatment services reach less than 40% of affected cases within their target area (Rogers, Myatt, Woodhead, Guerrero, & Alvarez, 2015). The challenge of low coverage is particularly evident in Mali in the Kayes region, where SAM prevalence varied from 1.2–2.4% between 2013 and 2015 (INSTAT, Republic of Mali, 2014) which led to the adoption of the outpatient approach, delivering services through all primary health facilities. Yet despite the geographical availability of services, a recent coverage survey concluded that only 24.5% of all cases in the region have access to services (Begashaw et al., 2014). This low figure suggests that in some contexts the outpatient model at scale is currently unable to meet the needs.
In Bangladesh, South Sudan, Angola, Ethiopia, and Malawi, community health workers (CHWs) have effectively delivered SAM treatment alongside other community‐based public health interventions (Keane, 2013; Linneman et al., 2007; Miller et al., 2014; Morgan, Bulten, & Jalipa, 2015; Puett, Coates, Alderman, & Sadler, 2013). These approaches, developed in response to low coverage resulting from similar barriers to access as identified in Mali, have proven to deliver high performance, increasing service coverage and with a good quality of care. In Bangladesh, treatment by CHWs achieved a cure rate of 92%, treatment coverage of 89% and 89.1% of CHWs achieving a minimum of 90% error‐free case management (Puett et al., 2013). In South Sudan, the CHWs achieved a cure rate of 94% and in Ethiopia, 59% of cases of malnutrition were treated correctly (Keane, 2013; Miller et al., 2014). However, the approach required further investigation for its wider applicability. In Mali, there is a comprehensive and established CHW network, managed through a decentralised apolitical and social model (ASACO, Association de Santé Communautaire), which is already used to deliver Integrated Community Case Management (iCCM or SEC, Soins Essentielle dans la communauté in Mali). This equity‐focused strategy promoted by the World Health Organization (WHO) extends the reach of public health services by providing timely and effective treatment of malaria, pneumonia, and diarrhoea. It is able to reach populations with limited access to facility‐based health care and focuses on children younger than 5 years. The iCCM proved an effective strategy in achieving high treatment coverage and delivering high‐quality care for sick children in the community (Dawson et al., 2008; Ghebreyesus et al., 1999), and it has been implemented in Mali since 2012 (de Sousa, Tiedje, Recht, Bjelic, & Hamer, 2012). As part of this package, CHWs are active but only undertaking screening, sharing of key nutrition messages, and referring cases to the health facility for treatment by facility‐based staff.
Between February 2015 and February 2016, the Malian Nutrition Division of the Ministry of Health and Action Against Hunger tested the feasibility of integrating SAM treatment into the iCCM package. The pilot took place in two sectors of Kita district, Kayes Region in Southwest Mali. This observational, clinical prospective multicentre cohort study with an intervention and a control area, compared the CHW (Agent de Santé Communautaire in French) delivered treatment model with the existing outpatient health facility model. The pilot covered seven communes, three in the intervention area (Tambaga, Bougarabaya, and Kobiri) and four in the control (Guenikoro, Kassaro, Dafela, and Sebekoro). In the intervention area, 18 CHWs were trained and equipped to treat uncomplicated SAM cases in the community. The pilot assessed the effectiveness of the treatment, specifically measuring clinical outcomes of children enrolled in the programme, quality of care provided, treatment coverage, and the cost‐effectiveness of the intervention. SAM treatment services, previously available in the health facility prior to the start of the pilot, remained available to the population in the intervention area.
This paper presents the findings of a cross‐sectional study undertaken to assess the technical competence—quality of care—of CHWs managing cases of uncomplicated SAM at the community level. The study aims to assess whether CHWs can offer high‐quality treatment for children with uncomplicated SAM.
Key messages.
Well‐trained and supervised CHWs are capable of managing cases of uncomplicated SAM, including treatment and correct dosing with a high quality of care.
Direct management of SAM cases by CHWs is an opportunity to increase access to quality treatment in Mali for SAM cases and possibly in other contexts.
Resources required for continuous service delivery at community level should be further investigated.
2. PARTICIPANTS AND METHODS
In this study, quality of care is defined as the capacity of the CHWs to evaluate, classify, and treat cases of uncomplicated SAM, to provide nutritional counselling to caretakers of children receiving treatment for SAM, malaria, pneumonia, or diarrhoea and to correctly refer cases of complicated SAM. In Mali, uncomplicated SAM in children younger than 5 years is defined as MUAC < 11.5 cm, Weight for Height z score less than −3, and/or nutritional oedema (Collins et al., 2006).
An evaluation framework was developed, based on the Avedis Donabedian care framework, which defines the criteria assessed in a quality‐of‐care analysis (see Figure 1; Donabedian, 2005). In this cross‐sectional study, only two of the criteria were assessed: performance of specific tasks (technical competence) and interpersonal skills of the CHWs. Interpersonal skills are defined as the way the CHW interacts with the carer and child which is important because it has been shown that if carers do not feel welcome to receive treatment, it could become a barrier to access. (Puett & Guerrero, 2015) Trained observers assessed tasks using a checklist and reclassified cases to confirm their status. Technical competence encompassed the following activities: screening for SAM; diagnosis of SAM; provision of antibiotics, vitamin A, and anti‐parasitic medication; and delivery of RUTF until the child has recovered.
Figure 1.
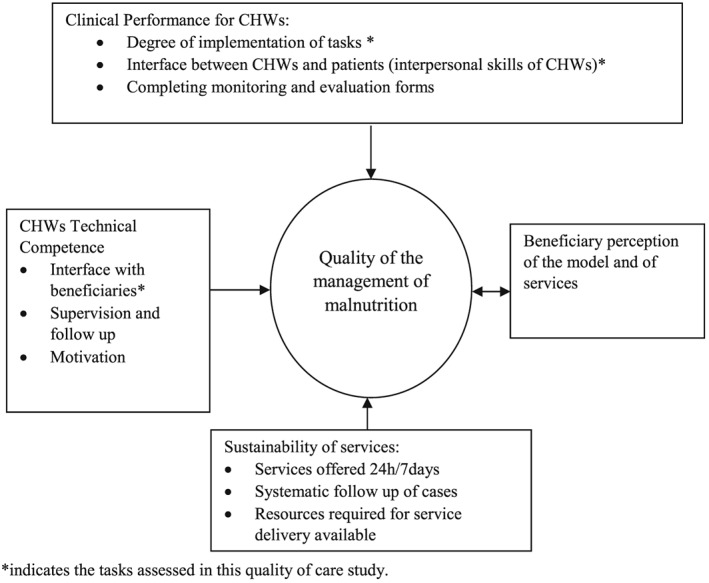
Framework for the management of malnutrition by community health workers (CHWs) in Mali
Other key components of quality of care, including satisfaction of the beneficiaries, programme effectiveness, beneficiary knowledge of services, and availability of services, will be assessed in future research.
The study was conducted during November 2015. Five teams of two observers collected the data over a 2‐week period, and 17 CHWs of the communes of Bougaribaya, Tambaga, and Kobiri in the region of Kita in Mali were evaluated. Observers were health professionals, either medical doctors or nurses whose careers have evolved around malnutrition treatment protocols and received training on data collection during 5 days. The training included two standardisation tests to ensure that all observers reached a level of 90% concordance. The “correct assessment” of cases was defined as such if the case classification matched the observer's; this was done via non‐participating observations made by filling in standardised forms to understand if the CHW is making the technical gestures correctly. After this, the observers review the documents (admission cards) to see if the medical prescriptions, treatment protocols, and reporting reflect the protocol. Observers do not re‐examine cases. They look at the CHWs during the management of cases and then review the prescriptions to verify if they are adequate: for example, dose of albendazole or amount of RUTF. Correct assessment of cases refers to the identification of nutritional status, medical symptoms, or danger signs by the CHWs and its reliability when compared to the classifications made by the observers. Informed consent was obtained from all CHWs and caretakers that participated in the study (see Supplementary Annex II).
The forms and questionnaires used by the observers can be found in Supplementary Annex I. They are different depending on whether it is a new case or a follow‐up visit. Both start with the contextual data of the child, followed by questions around the communication of the CHW with the caretaker, technical competency of anthropometric measurements, conducting the appetite test, and assessing medical signs and symptoms. They end with questions assessing whether the CHWs correctly treated, counselled, and referred the cases. Answers were always coded as “yes,” “no,” or “not applicable (N/A)” and to ensure a sufficient understanding of the quality of care provided, 104 questions were asked for new cases and 95 for follow‐up cases.
Data was entered into EpiData version 3.1 software and analysed with R language software environment for statistical computing (“EpiData Software ‐ http://www.epidata.dk,”, n.d., “R: The R Project for Statistical Computing,”, n.d.). Five dimensions of care were assessed, each with their own indicators. A composite indicator, composed of the essential indicators from each of the five dimensions, was created to produce a summary of quality of care. This composite indicator was considered the minimal essential tasks for the CHW to provide high‐quality treatment for SAM and can be interpreted as the percentage of cases in which all the essential tasks were performed with no errors.
The dimensions included in the indicator are CHW interface with the carer and child; general evaluation of the status of the child, including anthropometrical measures (height, weight, and MUAC), identification of oedema, appetite test, looking for danger signs; classification of the child and referral; treatment (systematic medical and nutritional treatment according to the child's weight); and counselling.
3. RESULTS
Table 1 presents the demographic and socio‐economic characteristics of the CHWs assessed during this study. Seventeen of 18 CHWs working in the study intervention area were assessed, with the remaining CHW unavailable at the time of the assessment. CHWs had a median age of 25 years and were predominantly female (76.5%), and the majority were educated to at least secondary level (82.3%). All were able to read and write as well as work in the French language. All had worked as CHWs in Mali (between 1 and 5 years), the majority had been trained as nurses and midwives (76.5%), and all had a minimum of 2 years of health training and experience. All CHWs lived in the community in which they delivered SAM treatment services and received a salary as per national laws and regulations.
Table 1.
Sociodemographic profile of community health workers (CHWs; n = 17)
| Median (Min–max) | n | % | |
|---|---|---|---|
| Age (years) | 25(19–61) | ‐ | ‐ |
| Sex | |||
| Male | 4 | 23.5 | |
| Female | 13 | 76.5 | |
| Marital status | |||
| Single | 6 | 35.3 | |
| Married | 10 | 58.8 | |
| Divorced | 1 | 5.9 | |
| Education level | |||
| Primary | 3 | 17.6 | |
| Secondary | 13 | 76.5 | |
| High | 1 | 5.9 | |
| Education degree | |||
| Midwife | 13 | 76.5 | |
| Health aidea | 3 | 17.6 | |
| Other | 1 | 5.9 | |
| Number of months of training received | 6(3–12) | ‐ | ‐ |
| Number of years worked in the health sector | 3(1–9) | ‐ | ‐ |
| Number of years worked as a CHW | 3(1–5) | ‐ | ‐ |
| Total number of CHWs assessed during the study | 17 | 100 |
Support staff located in the health facility, with minimal health training.
One hundred twenty‐five cases assessed and treated by the CHWs were observed during this quality‐of‐care study. The breakdown of their status is presented in Table 2.
Table 2.
Observed cases
| n | % | ||
|---|---|---|---|
| Age (months) median (min–max) | 14(6–59) | ||
| Sex | |||
| Male | 42 | 33.6 | |
| Female | 83 | 66.4 | |
| New cases | 12 | 9.6 | |
| Follow‐ups | 113 | 90.4 | |
| Total cases | 125 | 100.0 |
The median age of the cases was 14 months, with a range of 6 to 59 months and the majority of cases were female (66.4%). Nearly all (90.4%) were follow‐up cases (they were already receiving treatment from the CHW at the time of the study). SAM prevalence was low in December when this study was undertaken, resulting in 12 new SAM cases (9.6%) entered into the programme during the study period.
All of the CHWs were observed as having an appropriate interface with all of the patients and their carers, defined as greeting the carer on arrival and offering them a seat before beginning the assessment of the child. The outcomes of the observations of the CHW's technical competence are presented in Table 3.
Table 3.
Selected indicators of quality of case management by community health workers (CHWs) in the intervention area of the project in Kita, Mali
| N | % | |
|---|---|---|
| Appropriate interface between CHW and carer | 125 | 100 |
| Assessment | ||
| Child checked for presence of cough, diarrhoea, fever and vomiting | 125 | 97.6 |
| Child assessed correctly for the main danger signsa | 125 | 95.2 |
| Child's respiratory rate counted by the CHWs within ±5 breaths of the gold standard | 125 | 97.6 |
| Nutritional assessment | ||
| Child correctly assessed for oedema | 125 | 78.4 |
| Child's MUAC correctly measured | 125 | 96.8 |
| Child's height correctly measured | 12 | 100.0 |
| Child's appetite test was correctly performed | 36 | 77.8 |
| Child's vaccination status checked against vaccine calendar | 7 | 28.5 |
| Child's vitamin A needs correctly assessed | 21 | 33.3 |
| Classification | ||
| Child correctly classified for pneumonia | 8 | 100.0 |
| Child correctly classified for malaria | 8 | 75.0 |
| Child correctly classified for diarrhoea | 3 | 100.0 |
| Child correctly classified for SAM | 12 | 100.0 |
| Treatment and referral | ||
| Child correctly treated with medical productsb | 56 | 75.0 |
| Child correctly treated with RUTF | 118 | 100.0 |
| Child correctly treated for diarrhoea | 1 | 100.0 |
| Child correctly treated for pneumonia | 6 | 66.6 |
| Child correctly treated for malaria | 4 | 100.0 |
| Counselling | ||
| Caretaker received correct nutritional and feeding advice | 70 | 94.3 |
| Caretaker correctly taught how to give all treatments and appropriate dosages | 12 | 83.3 |
| Cases correctly managed | ||
| Proportion of cases manged with no errorsc | 117 | 79.5 |
Danger signs included: not being able to drink or eat, convulsing, oedema, low consciousness including not responding to external stimuli, anaemia assed by severe palmar pallor, difficulty breathing with chest drawing in or wheezing, spontaneous bleeding, scanty urine in Coca‐Cola colour, and being unable to sit or stand.
Amoxicillin, Albendazole, and vitamin A.
Medical and nutritional treatment as well as nutritional and feeding advice received correctly.
The majority of children were correctly assessed for the presence of cough, diarrhoea, fever, and vomiting (97.6%), and similarly, most children were checked for the presence of the main danger signs (95.2%).
MUAC was correctly assessed in 96.8% of children, and oedema was correctly assessed in 78.4%. All children were measured correctly for height (100%). Of the 36 that required an appetite test, 77.8% were tested correctly. The evaluation of the immunisation status, according to the national vaccine schedule, was correctly completed for two out of the seven (28.5%) eligible children and the need for vitamin A supplementation correctly assessed in 33.3% of the 21 cases requiring supplementation.
One hundred per cent of diarrhoea and pneumonia cases were correctly classified and 75% of malaria cases. Treatment was correctly provided to all of the diarrhoea and malaria cases (100%) but only 66.6% of pneumonia cases were correctly treated.
Medical treatment with Amoxicillin, Albendazole, and vitamin A for SAM cases was correctly administered by the CHWs in 75.0% of cases while the management of the nutrition treatment with RUTF was correctly administered in all cases (100%) assessed. Essential nutritional counselling was given to 94.3% of caretakers. A demonstration on how to administer the first doses of treatment and information on the correct dosage was correctly provided to 83.3% of caretakers.
Finally, the composite indicator which includes all essential tasks to provide high‐quality treatment for SAM, was achieved by 79.5% of cases. These cases experienced an appropriate interface between the CHW and carer; the child was appropriately assessed for key indicators, correctly classified and treated, and received key counselling.
4. DISCUSSION
This quality‐of‐care study shows that in this context CHWs can manage cases of uncomplicated SAM to a high standard. These findings support existing evidence from Bangladesh, Malawi, and Ethiopia (Amthor, Cole, & Manary, 2009; Linneman et al., 2007; Puett, Coates, Alderman, Sadruddin, & Sadler, 2012) and suggest that the approach should be considered as a non‐inferior delivery method by SAM treatment implementers in similar settings. This study found that 75.9% of SAM cases were screened, treated, and counselled correctly which correlates with findings from Bangladesh where 52.8% of CHWs achieved 100% error‐free management of SAM cases (Puett et al., 2013). In Malawi, 90% of cases treated by community aides recovered suggesting that quality of care was not inferior to facility‐based care (Linneman et al., 2007). However, despite these studies, evidence on the ability of CHWs to correctly treat SAM remains limited.
This study shows that CHWs can accurately assess SAM. A high percentage of cases were correctly classified using MUAC (96.8% of children correctly assessed) reflecting findings in previous studies (Puett et al., 2013). SAM screening was a component of the CHW's iCCM activities prior to the implementation of this pilot, so accurate MUAC measurements are expected. They were less competent assessing oedema correctly, with 78.4% of oedema checks correctly implemented, which is a common weakness of CHWs worldwide (Alvarez, Dent, Browne, Myatt, & Briend, 2016). However, in this context, it can be attributed to the low prevalence of oedema in the intervention area as was shown in the baseline survey implemented at the beginning of the pilot project (no oedema cases where found among 452 children screened), likely reflecting the prioritisation of MUAC measurements over oedema screening. It is also subject to observer bias as CHWs are more likely to measure for oedema if they know it is being assessed. More importantly, the CHWs were able to correctly implement the appetite test, an eight‐step process which is traditionally carried out by medically trained staff. This shows they are capable of taking on this more complex role and led to all cases of SAM assessed in this study being classified correctly. This demonstrates that they are able to undertake all components of the SAM assessment.
CHWs were equally able to assess danger signs and classify diarrhoea, malaria, and pneumonia, with close to 90% of cases classified correctly. It has been shown in multiple contexts that CHWs can correctly assess danger signs and classify malaria, diarrhoea, and pneumonia (Bang et al., 2005; Baqui et al., 2009; Darmstadt et al., 2009) but these results show an improvement on diagnosis rates of iCCM illnesses from other contexts (Miller et al., 2014). Significantly, this study contributes to the evidence‐base that CHWs are able to assess and classify malaria, diarrhoea, and pneumonia and SAM concurrently, indicating that adding SAM to the existing iCCM package is technically feasible.
CHWs are also able to provide the treatment for SAM, although due to the high level of supervision provided during the pilot period, this high level of accuracy may depend on being closely supervised. RUTF was provided correctly to all cases assessed, demonstrating that CHWs were able to identify and provide the correct dosage based on the child's weight. This supports findings from Bangladesh where 96.4% of cases were given the correct dosage of RUTF (Puett et al., 2013). SAM treatment also requires the provision of Amoxicillin, Albendazole, and vitamin A, which varies depending on how long the child has been receiving treatment and on their vaccination history. Only 75% of cases were provided with the correct dosage, suggesting accuracy needs to be improved. The difference in the ability of CHWs to provide the correct dosage of RUTF compared to medical treatment was attributed to the close on‐the‐job support for the former provided to the CHWs by the NGO. This has also been noted as an influencing factor in Ethiopia (Miller et al., 2014). The impact of the level of training or supervision on accuracy of CHW activities was not specifically tested during this pilot and requires further investigation. It is likely that with additional training or supervision, CHW accuracy can be improved; however, further evidence is required.
There is sufficient evidence that CHWs are able to safely treat malaria, pneumonia, diarrhoea, and other pathologies in the community, yet this study contributes to the growing evidence base that they are also able to manage uncomplicated SAM (Amthor et al., 2009; Linneman et al., 2007; Miller et al., 2014; Puett et al., 2013). Nevertheless, the challenge is managing them concurrently. This pilot did not assess this specifically although in this study, 61% of these cases treated concurrently by the CHWs were treated correctly, indicating it was possible. However, the sample size for malaria and pneumonia cases was small (n = 5), so drawing concrete conclusions is challenging and further evidence is required. In Bangladesh, CHWs providing similar services, diarrhoea and pneumonia identification, classification and treatment, maintained quality of care when SAM treatment was added to the package (Puett et al., 2012). These CHWs were motivated by the addition yet worked significantly more hours than those only providing diarrhoea and pneumonia treatment, negatively impacting their personal lives. This reflects the well‐evidenced challenge of maintaining CHW effectiveness with a high workload while achieving sustainable programme scale up (Haines et al., 2007; Jaskiewicz & Tulenko, 2012). As with all CHW interventions, workload, supervision, training, and attrition will influence quality of care and require a careful balance.
This study indicates that CHWs are able to effectively classify and treat SAM in the community, although there are some limitations which affected this pilot. First, the sample size of CHWs is small due to the fact that the intervention was only piloted in small catchment areas and the prevalence of SAM was low during the assessment, meaning there was also a small sample of cases. Second, the assessment of quality of care was restricted to CHW‐managed SAM cases and did not compare with the quality of care provided at the health centre. Third, this analysis does not include feedback from the community on the acceptability of CHW delivered services which will strengthen the conclusions since the importance of the two components in the quality of care varies in different contexts and they interact and influence each other. Additionally, observer bias is a well‐documented challenge in quality‐of‐care assessments as CHWs are likely to perform better when observed closely. Finally, CHW motivation increased during the assessment period due to being at the end of the pilot phase. Additional evidence on the quality of care in the treatment of SAM by CHWs when delivered at scale and with reduced levels of supervision from NGO partners is needed before these results are extrapolated to other contexts.
5. CONCLUSION
The results from this study allow us to conclude that well‐trained and supervised CHWs are capable of identifying and managing cases of uncomplicated SAM. The quality of the management of such cases is satisfactory with 79.5% and treated without significant errors. This suggests that such a strategy is an opportunity to increase access to quality treatment in Mali for SAM cases.
Direct observation with re‐examination is a rigorous method for assessing quality of care (Cardemil, Gilroy, Callaghan‐Koru, Nsona, & Bryce, 2012), and there are already multiple studies demonstrating that CHWs can deliver a high quality of care and are able to identify and refer complications. Yet, quality of care is just one component of the service delivered at the community. There are additional benefits from decentralising treatment of SAM into a standard community‐based protocol: increased awareness and coverage and better community access and sensitisation (Guerrero, Myatt, & Collins, 2010).
Despite this, further evidence is required to identify best practice for the scale up of these decentralised models. Specifically, whether comparable levels of quality of care can be achieved when services are delivered at scale. The extent to which training and supervision impacts this quality of care and whether adding SAM treatment to the iCCM package affects the quality of care of the existing treatments. This study has shown that although deficiencies can be found in specific tasks that require close monitoring and additional measurements, the quality of care appears comparable to the care provided at facility level.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
Supporting information
Supporting info item
ACKNOWLEDGMENTS
The authors would like to thank all partners and colleagues who contributed to this process including colleagues at ACF Mali, the Ministries of Health of Mali, University of Bamako and non‐governmental organisations. The authors would also like to thank Dr Fatoumata Yarro and Dr Sylla Oumarou for their technical support during the implementation this survey project and Chloe Puett for her guidance.
CONTRIBUTIONS
JLA and FA design and developed the protocol. FA conducted the field work, extracted data, and implemented the analyses. JLA and ER verified and conducted further analyses and drafted the manuscript with input from SG and FA. SG supervised the whole process. All authors provided input and approved the manuscript.
Alvarez Morán JL, Alé FGB, Rogers E, Guerrero S. Quality of care for treatment of uncomplicated severe acute malnutrition delivered by community health workers in a rural area of Mali. Matern Child Nutr. 2018;14:e12449 10.1111/mcn.12449
REFERENCES
- Alvarez, J. L. , Dent, N. , Browne, L. , Myatt, M. , Briend, A . (2016). Putting child kwashiorkor on the map. Retrieved from http://www.cmamforum.org/Pool/Resources/Putting-Kwashiorkor-on-the-Map.pdf
- Amthor, R. E. , Cole, S. M. , & Manary, M. J. (2009). The use of home‐based therapy with ready‐to‐use therapeutic food to treat malnutrition in a rural area during a food crisis. Journal of the American Dietetic Association, 109(3), 464–467. 10.1016/j.jada.2008.11.028 [DOI] [PubMed] [Google Scholar]
- Bang, A. T. , Bang, R. A. , Stoll, B. J. , Baitule, S. B. , Reddy, H. M. , & Deshmukh, M. D. (2005). Is home‐based diagnosis and treatment of neonatal sepsis feasible and effective? Seven years of intervention in the Gadchiroli field trial (1996 to 2003). Journal of Perinatology: Official Journal of the California Perinatal Association, 25(Suppl 1), S62–S71. 10.1038/sj.jp.7211273 [DOI] [PubMed] [Google Scholar]
- Baqui, A. H. , Arifeen, S. E. , Williams, E. K. , Ahmed, S. , Mannan, I. , Rahman, S. M. , … Darmstadt, G. L. (2009). Effectiveness of home‐based management of newborn infections by community health workers in rural Bangladesh. The Pediatric Infectious Disease Journal, 28(4), 304–310. 10.1097/INF.0b013e31819069e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begashaw, M. , Alvarez, J. L. , Woodhead, S. , Perez Bernabe, B. , Malian Nutrition Division of the Ministry of Health and UNICEF . (2014). Simplified Lot Quality Assurance Sampling Evaluation of Access and Coverage (SLEAC) Survey, Republic of Mali, Final Report. Retrieved from http://www.coverage-monitoring.org/wp-content/uploads/2015/07/Mali_-April-2014_-SLEAC-English-version.pdf
- Black, R. E. , Victora, C. G. , Walker, S. P. , Bhutta, Z. A. , Christian, P. , de Onis, M. , … Maternal and Child Nutrition Study Group . (2013). Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet (London, England), 382(9890), 427–451. 10.1016/S0140-6736(13)60937-X [DOI] [PubMed] [Google Scholar]
- Cardemil, C. V. , Gilroy, K. E. , Callaghan‐Koru, J. A. , Nsona, H. , & Bryce, J. (2012). Comparison of methods for assessing quality of care for community case management of sick children: An application with community health workers in Malawi. American Journal of Tropical Medicine and Hygiene, 87(5 Suppl), 127–136. 10.4269/ajtmh.2012.12-0389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins, S. , Dent, N. , Binns, P. , Bahwere, P. , Sadler, K. , & Hallam, A. (2006). Management of severe acute malnutrition in children. Lancet (London, England), 368(9551), 1992–2000. 10.1016/S0140-6736(06)69443-9 [DOI] [PubMed] [Google Scholar]
- Darmstadt, G. L. , Baqui, A. H. , Choi, Y. , Bari, S. , Rahman, S. M. , Mannan, I. , … Bangladesh Projahnmo‐2 (Mirzapur) Study Group . (2009). Validation of community health workers' assessment of neonatal illness in rural Bangladesh. Bulletin of the World Health Organization, 87(1), 12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson, P. , Pradhan, Y. , Houston, R. , Karki, S. , Poudel, D. , & Hodgins, S. (2008). From research to national expansion: 20 years' experience of community‐based management of childhood pneumonia in Nepal. Bulletin of the World Health Organization, 86(5), 339–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donabedian, A. (2005). Evaluating the quality of medical care. 1966. The Milbank Quarterly, 83(4), 691–729. 10.1111/j.1468-0009.2005.00397.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- EpiData Software ‐ http://www.epidata.dk . (n.d.). Retrieved August 30, 2016, from http://www.epidata.dk/
- Ghebreyesus, T. A. , Witten, K. H. , Getachew, A. , O'Neill, K. , Bosman, A. , & Teklehaimanot, A. (1999). Community‐based malaria control in Tigray, northern Ethiopia. Parassitologia, 41(1–3), 367–371. [PubMed] [Google Scholar]
- Guerrero, S. , Myatt, M. , & Collins, S. (2010). Determinants of coverage in community‐based therapeutic care programmes: Towards a joint quantitative and qualitative analysis. Disasters, 34(2), 571–585. 10.1111/j.1467-7717.2009.01144.x [DOI] [PubMed] [Google Scholar]
- Haines, A. , Sanders, D. , Lehmann, U. , Rowe, A. K. , Lawn, J. E. , Jan, S. , … Bhutta, Z. (2007). Achieving child survival goals: Potential contribution of community health workers. Lancet (London, England), 369(9579), 2121–2131. 10.1016/S0140-6736(07)60325-0 [DOI] [PubMed] [Google Scholar]
- INSTAT, Republic of Mali . (2014). Enquête nutritionnelle et de mortalité rétrospective, Mali. Retrieved from http://mail.cnom.sante.gov.ml/docs/Rapport_final%20SMART-2014_Mali.pdf
- Jaskiewicz, W. , & Tulenko, K. (2012). Increasing community health worker productivity and effectiveness: a review of the influence of the work environment. Human Resources for Health, 10, 38 10.1186/1478-4491-10-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane, E. (2013). Integrating severe acute malnutrition into the management of childhood diseases at community level in South Sudan. Malaria Consortium Learning Paper Series: Retrieved from http://www.malariaconsortium.org/pages/learning-papers.htm
- Linneman, Z. , Matilsky, D. , Ndekha, M. , Manary, M. J. , Maleta, K. , & Manary, M. J. (2007). A large‐scale operational study of home‐based therapy with ready‐to‐use therapeutic food in childhood malnutrition in Malawi. Maternal & Child Nutrition, 3(3), 206–215. 10.1111/j.1740-8709.2007.00095.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, N. P. , Amouzou, A. , Tafesse, M. , Hazel, E. , Legesse, H. , Degefie, T. , … Bryce, J. (2014). Integrated community case management of childhood illness in Ethiopia: Implementation strength and quality of care. The American Journal of Tropical Medicine and Hygiene, 91(2), 424–434. 10.4269/ajtmh.13-0751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan, S. , Bulten, R. , Jalipa, H. (2015). Community case management approach to SAM treatment in Angola | ENN. Field Exchange, 49 Retrieved from http://www.ennonline.net/fex/49/angola
- Puett, C. , & Guerrero, S. (2015). Barriers to access for severe acute malnutrition treatment services in Pakistan and Ethiopia: A comparative qualitative analysis. Public Health Nutrition, 18(10), 1873–1882. 10.1017/S1368980014002444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puett, C. , Coates, J. , Alderman, H. , Sadruddin, S. , & Sadler, K. (2012). Does greater workload lead to reduced quality of preventive and curative care among community health workers in Bangladesh? Food and Nutrition Bulletin, 33(4), 273–287. [DOI] [PubMed] [Google Scholar]
- Puett, C. , Coates, J. , Alderman, H. , & Sadler, K. (2013). Quality of care for severe acute malnutrition delivered by community health workers in southern Bangladesh. Maternal & Child Nutrition, 9(1), 130–142. 10.1111/j.1740-8709.2012.00409.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- R: The R Project for Statistical Computing . (n.d.). Retrieved August 30, 2016, from https://www.r-project.org/
- Rogers, E. , Myatt, M. , Woodhead, S. , Guerrero, S. , & Alvarez, J. L. (2015). Coverage of community‐based management of severe acute malnutrition programmes in twenty‐one countries, 2012‐2013. PloS One, 10(6) e0128666. 10.1371/journal.pone.0128666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Sousa, A. , Tiedje, K. E. , Recht, J. , Bjelic, I. , & Hamer, D. H. (2012). Community case management of childhood illnesses: Policy and implementation in Countdown to 2015 countries. Bulletin of the World Health Organization, 90(3), 183–190. 10.2471/BLT.11.093989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . (2014). Nutridash 2014: Global report on the pilot year. Retrieved from http://www.cmamforum.org/Pool/Resources/UNICEF-NutriDash2014-Final-Report.pdf
- WHO | UNICEF‐WHO‐The World Bank: Joint child malnutrition estimates ‐ Levels and trends . (n.d.). Retrieved August 26, 2016, from http://www.who.int/entity/nutgrowthdb/estimates/en/index.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting info item


