Abstract
The burden of undernutrition in South Asia is greater than anywhere else. Policies and programmatic efforts increasingly address health and non‐health determinants of undernutrition. In Nepal, one large‐scale integrated nutrition program, Suaahara, aimed to reduce undernutrition among women and children in the 1,000‐day period, while simultaneously addressing inequities. In this study, we use household‐level process evaluation data (N = 480) to assess levels of exposure to program inputs and levels of knowledge and practices related to health, nutrition, and water, sanitation, and hygiene (WASH). We also assess Suaahara's effect on the differences between disadvantaged (DAG) and non‐disadvantaged households in exposure, knowledge, and practice indicators. All regression models were adjusted for potential confounders at the child‐, maternal‐, and household levels, as well as clustering. We found a higher prevalence of almost all exposure and knowledge indicators and some practice indicators in Suaahara areas versus comparison areas. A higher proportion of DAG households in Suaahara areas reported exposure, were knowledgeable, and practiced optimal behaviors related to nearly all maternal and child health, nutrition, and WASH indicators than DAG households in non‐Suaahara areas and sometimes even than non‐DAG households in Suaahara areas. Moreover, differences in some of these indicators between DAG and non‐DAG households were significantly smaller in Suaahara areas than in comparison areas. These results indicate that large‐scale integrated interventions can influence nutrition‐related knowledge and practices, while simultaneously reducing inequities.
Keywords: equity, Nepal, nutrition, Suaahara
1. INTRODUCTION
Globally, millions of mothers and children suffer from undernutrition and its short‐ and long‐term physical and cognitive consequences (Hoddinott, Alderman, et al., 2013; Hoddinott, Behrman, et al., 2013; Hoddinott et al., 2011). The determinants of undernutrition are complex and include immediate causes such as inadequate food intake and disease, as well as underlying causes of household food insecurity, inadequate care environments, and lack of access to health services and a healthy environment. Poverty, lack of resources and control of resources, poor infrastructure, and unstable political and economic contexts also contribute to malnutrition (UNICEF, 1990).
Currently, efforts to combat undernutrition increasingly focus on the first 1,000 days, the period between conception and a child's second birthday. After this period, physical and mental stunting may be irreversible, thus it constitutes a window of opportunity to prevent undernutrition (Horton & Lo, 2013). While progress has been made in addressing undernutrition, achieving global goals like the World Health Assembly target of reducing stunting by 40% by 2025 seems unlikely without the acceleration of concerted efforts. In addition to reducing the burden of undernutrition, there is also increasing recognition of the need to focus on equity in development, as socioeconomic differences in mortality and morbidity in most countries are widening (Gwatkin et al., 2007; Victora et al., 2003). This is particularly true in developing countries, where it is predicted that it will take much longer to reduce undernutrition in excluded and disadvantaged groups than in majority populations (UNICEF, WHO, and World Bank Group, 2015).
The global nutrition community now emphasizes the need to complement nutrition‐specific interventions (those primarily delivered through health systems) with nutrition‐sensitive interventions that address the diverse underlying determinants of nutritional well‐being. Interventions in education, agriculture, and water, sanitation, and hygiene (WASH), for example, may have both direct and indirect linkages with nutrition. However, there is a dearth of information on how to most effectively design and implement integrated programs at scale; the evidence base for what works is encouraging but limited (Bhutta et al., 2008; Menon et al., 2014; Ruel & Alderman, 2013).
Nowhere in the world is stunting as prevalent as in South Asia (Black et al., 2013), where 65 million children under five are estimated to be stunted (Shekar, Dayton Eberwein, & Kakietek, 2016). In Nepal, remarkable rapid progress has been made since the mid‐1990s to reduce maternal and child undernutrition. However, undernutrition remains a major public health issue: 41% of children under 5 years of age are stunted and 11% wasted (Ministry of Health and Popualation (MOHP) Nepal, 2012). There is increasing evidence that Nepal's progress in education and WASH has played a key role in the nutrition success Nepal has achieved (Crum et al., 2013; Cunningham et al., 2016; Headey & Hoddinott, 2015; Headey, Hoddinott, & Park, 2016). However, there is substantial subnational variation in improvements to date. For example, the prevalence of child stunting is 42% in rural areas, but only 27% in urban areas. More than half of children in the lowest wealth quintile but only one‐fourth of children from the highest wealth quintile are stunted. Child stunting is highest among historically disadvantaged caste groups including Dalits, hill Janajatis, and Muslims, and the prevalence of severe underweight among women is highest among terai madhesi Dalits (Ministry of Health and Popualation (MOHP) Nepal, 2012). Access to resources and services, political representation, and the presence of opportunities is unequal due to both geographic isolation and long‐standing social and economic inequities. To most effectively address persistent undernutrition in Nepal, an explicit focus on overcoming these disparities in the access to and utilization of services is imperative (Anon, 2006; Crum et al., 2013; Devkota, Adhikari, & Upreti, 2016; Devkota & Bennett, 2014).
In 2012, the Government of Nepal (GoN) endorsed a multi‐sectoral nutrition plan (MSNP) to address Nepal's undernutrition problem (Government of Nepal National Planning Commission, 2012; Pokharel et al., 2009). In line with the MSNP, donors and international non‐governmental organizations (NGOs) have in turn funded programs that aim to reduce undernutrition. Suaahara, a United States Agency for International Development‐funded 5‐year (2011–2016) integrated nutrition program (Figure 1), aimed to address the poor nutritional status of women and children residing rurally in 41 of Nepal's 75 districts. Suaahara had a specific focus on social behavior change and communication (SBCC) and gender and social inclusion (GESI), including the targeting of disadvantaged groups (DAGs), that is, those identified as being food insecure and vulnerable due to socioeconomic, cultural, or physical factors. Suaahara integrated its programming across nutrition, health services, family planning, WASH, and agriculture/homestead food production (HFP) with four key objectives: (a) to improve household nutrition, health, and hygiene behaviors; (b) to increase the use of quality nutrition and health services; (c) to increase the production and consumption of diverse and nutritious foods; and (d) to strengthen coordination among nutrition actors (Anon, 2015; Cunningham & Kadiyala, 2013).
Figure 1.
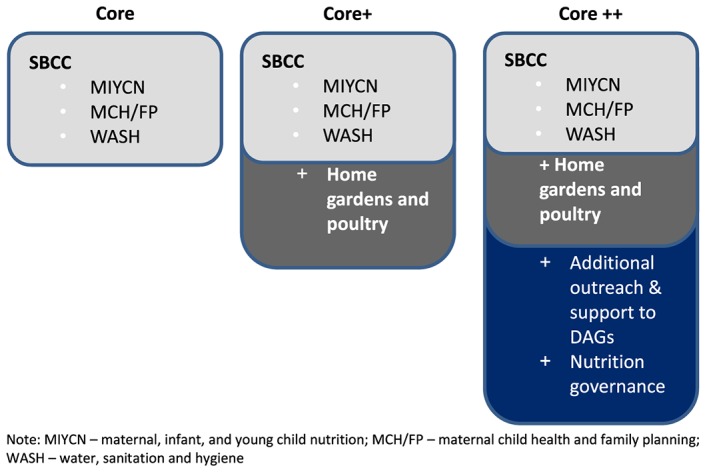
Suaahara's intervention packages. SBCC = social behavior change and communication; DAGs = disadvantaged groups
Suaahara not only facilitated national‐ and district‐level efforts to improve nutrition policies and coordination among stakeholders but also trained and supported a diverse cadre of GoN and NGO health, agriculture, and WASH frontline workers (FLWs) to improve service quality. The GoN's long‐established network of female community health volunteers (FCHVs) served as the primary means of engaging Suaahara's target populations with SBCC activities. FCHVs were to use new knowledge and skills they gained from participating in Suaahara into routine home visits and mothers' group meetings. Suaahara also partnered with district‐level NGOs who hired Suaahara field supervisors (FS) to support government FLWs. Other FLWs involved in Suaahara included the following health, nutrition, WASH, and agriculture‐related individuals and groups: health assistants, assistant health workers, assistant nurse midwifes; traditional healers; agricultural extension workers; livestock extension workers; MOFALD social mobilizers; village development committee (VDC) and WASH committees; citizen awareness centers; VDC nutrition and food security steering committees; ward citizen forums; Suaahara FS; Suaahara HFP mothers' groups; Suaahara peer facilitators; and Suaahara community hygiene and sanitation facilitators.
At the sub‐district level, Suaahara worked at the VDC and ward levels, Nepal's two smallest administrative units. A core package of SBCC activities on maternal, infant, and young child nutrition (MIYCN), maternal and child health and family planning, and WASH was implemented throughout Suaahara districts for all 1,000‐day households. Various platforms were used for SBCC activities: mass media, community mobilization, and interpersonal communication. The mass media platform consisted of a radio program and a complementary call‐in show, titled Bhanchhin Aama (or “Mother knows best”), featuring a positive mother‐in‐law role model who communicated evidence‐based health, nutrition, and WASH information. Billboards, posters, and other visual materials, with similar information, were displayed throughout communities. FLWs who worked with Suaahara also reinforced key messages during community activities such as food demonstrations and key life event celebrations. The interpersonal communication platform consisted of home visits and mothers' groups, where videos, flip charts, card games, counseling wheels, and other tools and materials were used to promote optimal nutrition‐related practices.
Suaahara incorporated an explicit GESI strategy across all program areas. Additional programmatic activities were facilitated for VDCs classified by the GoN into two categories denoting the highest concentration of DAGs. In these areas, material inputs for the construction of toilets and hand washing stations and for HFP were distributed. Suaahara also facilitated nutrition governance activities in these DAG VDCs, such as discussion sessions at community‐level Citizens Awareness Centers (settlement level platforms composed of socioeconomically disadvantaged community members to increase their awareness relating to rights and entitlements and their engagement in VDC budget planning) and linkages between DAG households and their local Ward Citizen Forums (platforms composed of community members to identify the needs of local people and excluded groups in order to recommend priorities for VDC budget planning; UNDP, 2015). Suaahara FS prioritized DAG households for regular home visits to provide counseling, distribute HFP inputs and advice, and assess access to and use of toilets.
As of program end in 2016, Suaahara's monitoring data showed that about 2.4 million people across 1,900 VDCs were reached. The total population of Nepal is 27 million, and there were approximately 11.6 million people in the program's 41 districts. There are 51,470 FCHVs nationally, and all FCHVs in Suaahara districts were trained. This means that Suaahara trained 33,688 FCHVs, and training in key thematic areas was given to additional FLWs: 14,494 in MIYCN, 4,815 in family planning, and 13,475 in WASH. HFP activities reached more than 155,000 households, and an FCHV or a Suaahara FS made a home visit to about 160,000 households.
Suaahara is one of the first nutrition programs globally to operate at scale, use a multi‐sectoral approach, and have an explicit focus on equity. The research presented here aims to assess Suaahara's progress in increasing exposure to nutrition‐related information and services and its potential role in improving nutrition‐related knowledge and practices among pregnant women and mothers of children under 2 years of age in rural Nepal. We also explore Suaahara's potential role in narrowing gaps between DAG and non‐DAG households for these same nutrition‐related exposure, knowledge, and practices. To the best of our knowledge, this is the first process evaluation (PE) to assess not only overall program progress but also equity‐based variation in program coverage and uptake.
Key messages.
Suaahara process evaluation results confirm effective scale (on some/many behaviors) and reach can be obtained in multi‐sectoral nutrition programs, while simultaneously addressing equity gaps.
After only 2 years of full program intervention, large differences were found in exposure, knowledge, and some practices between comparison and intervention groups for maternal and child health and nutrition, as well as WASH.
Progress on difficult to move child nutrition indicators, that is, appropriate sick child feeding, can be made via multi‐sectoral integrated at‐scale interventions.
2. METHODS
2.1. Study design and implementation
For this analysis, we used data from Suaahara's household‐level PE study, conducted in November–December 2014, about 2 years after the program started. A baseline study was conducted in 2012; however, due to differences in sampling methodology at the household‐level, we will not compare our findings to the baseline results. Consistent with other PE studies of nutrition interventions, this mixed‐methods PE was theory‐driven, carried out after a few years of implementation in all target areas, and aimed to assess program delivery and utilization (Mbuya et al., 2015; Robert et al., 2006; Robert et al., 2007).
The household‐level PE study aimed to assess the depth of exposure to the program as well as related knowledge and practices along the pathways to impact, among target beneficiaries in Suaahara areas and a similar population in comparison areas. At baseline, 16 districts were matched into intervention‐comparison pairs based on social, economic, and agroecological characteristics. Among these districts, eight were subsequently purposively selected for the PE: four intervention‐comparison pairs spanning Nepal's three agroecological zones and excluding pairs where a baseline comparison district later became a Suaahara district during program scale‐up. Within each district, we selected the same five rural VDCs, and within each VDC, the same three wards, which were all randomly selected for the baseline survey using probability‐proportional‐to‐size techniques. Enumerators consulted with local FCHVs to construct a list of all pregnant women and mothers of children under 2 years of age in the ward and then classified each into one of four categories: (a) DAG pregnant woman, (b) non‐DAG pregnant woman, (c) DAG mother of a child under 2 years of age, and (d) non‐DAG mother of a child under 2 years of age. FCHVs classified women from disadvantaged castes, living in extreme poverty, and/or food insecure as DAG. Once the listing was complete, enumerators randomly selected one woman per category in each ward. In total, the sample included 472 households (eight non‐respondents) from 120 wards, 40 VDCs, and eight districts.
Twenty local enumerators and supervisors were hired and trained for 2 weeks on interview techniques, study details, and mobile data collection. The training included field practice to test and refine study instruments. Women were interviewed using precoded, structured questionnaires, translated into Nepali. Questions were included on a range of topics: (a) demographics and socio‐economic characteristics; (b) exposure to Suaahara intervention platforms, including FLWs, project information, tools, materials, and key messages; (c) knowledge about nutrition, health, WASH, and family planning; and (d) practices related to nutrition, health, WASH, and family planning. Spot‐check observations were used to examine household construction materials and to assess WASH facilities and practices. Supervisors remained in the field to oversee data collection processes, and data quality controllers visited study areas to ensure the collection of valid and reliable data.
Ethical approval for the study was obtained from the Nepal Health Research Council. All respondents gave their informed consent prior to participating in the survey.
2.2. Data analysis
Data were analyzed using Stata 13 (StataCorp, 2013). Descriptive statistics and bivariate and multivariate regression analyses were conducted to examine differences in prevalence rates for exposure to FLWs; information, tools, and materials; and messages, as well as levels of knowledge and practices between intervention and comparison areas. For equity analyses, we used an interaction term between study arm and DAG status in order to examine how differences between DAG and non‐DAG households in Suaahara areas contrasted with those same differences in comparison areas. In all regression models, we controlled for VDC‐level clustering and reported statistical significance if P < .05. In final multivariate regression models, we also controlled for the following potentially confounding factors: women's age, education, and pregnancy status, as well as household agroecological zone of residency, number of children <5 years, asset ownership, and quality of roof materials.
3. RESULTS
3.1. Characteristics of Suaahara and comparison households
Table 1 presents an overview of study participants (n = 472). Nearly all women were married, and their mean age was 24 years. Among women who were mothers (n = 363), the youngest child was, on average, 17 months. Households had one child under 5 years of age, on average. Close to 90% of the households were Hindu, almost all owned their home and some land, and they owned an average of 7 or 8 out of a possible 22 types of assets included in the questionnaire. The only significant difference among the demographic and socioeconomic characteristics were that in Suaahara areas, women were nearly 1 year older at first pregnancy and more households had improved roof materials (S:97%; C:83%; p < .001).
Table 1.
Sample child, mother, and household characteristics
| Comparison | Intervention | Significancea | |
|---|---|---|---|
| N = 240 | N = 232 | ||
| Mean (SD)/% | Mean (SD)/% | P value | |
| Children (N = 197‐C, 166‐I) | |||
| Age (in months) | 16.9 (14.6) | 16.9 (15.6) | .982 |
| Sex: percent boys | 52.1 | 53.0 | .862 |
| Mother | |||
| Marital status: percent married | 99.6 | 100.0 | N/A |
| Age (in years) | 24.4 (5.1) | 24.3 (4.8) | .813 |
| Age at first pregnancy (in years) | 19.3 (2.6) | 20.1 (2.6)* | .018 |
| Formal schooling (in years) | 4.9 (4.2) | 6.3 (4.3) | .081 |
| Household | |||
| Number of children <5 years | 1.1 (0.8) | 1.0 (0.8) | .299 |
| Religion: percent Hindu | 88.8 | 88.4 | .950 |
| Home: percent owning | 97.9 | 97.8 | .964 |
| Number of bedrooms in the house | 2.6 (1.4) | 2.7 (1.4) | .624 |
| Electricity: percent with access | 66.7 | 82.8 | .129 |
| Floor material: percent improved (observation) | 12.5 | 20.3 | .352 |
| Exterior wall material: percent improved (observation) | 15.0 | 33.6 | .061 |
| Roof material: percent improved (observation) | 83.3 | 97.0*** | .001 |
| Agricultural land: percent owning | 97.1 | 94.8 | .323 |
| Total types of assets owned (range: 0–22) | 7.3 (3.2) | 7.6 (3.0) | .577 |
| Total types of animals owned (range: 0–8) | 3.3 (1.7) | 2.8 (1.5) | .146 |
Note. ANC = antenatal care; FCHV = female community health volunteers; FP = family planning; TT = tetanus toxiod..
Assets included stove/gas burner; refrigerator; bed; sofa; cupboard; table/chair; radio; dvd player; cassette/CD player; motorcycle/scooter; bike; tv; mobile phone; small agricultural tools; solar energy panels; machine sprayer for agriculture; hand tube well; low life pump; masonry equipment; carpentry equipment; manual wooden thresher; manual flour mill; animals included the following: poultry; beehives; goat/sheep; cow; buffalo; other cattle; donkey/mule/horse; and pig/boar.
Controlling for village development committee‐level clustering.
P < .05.
P < .01.
P < .001.
3.2. Exposure to Suaahara interventions
Table 2 presents results for exposure to three aspects of Suaahara: (a) frontline workers; (b) information, tools, and materials; and (c) key messages, contrasting women in Suaahara and comparison areas. Women in Suaahara areas, compared with women in comparison areas, reported to have met more regularly with an FLW in the 6 months preceding the survey (S: 4.5; C: 3.1 times; p < .001) and were more likely to report to have received family planning counseling from a health worker (S: 88%; C: 55%; p < .001). The FCHV‐related results varied, although more women in Suaahara areas reported interacting with an FCHV outside of a home visit or health mothers' group meeting (S:87%; C:65%; p < .001), there were no significant differences between study areas on whether an FCHV ever made a home visit and frequency of meeting with an FCHV in the previous 6 months.
Table 2.
Exposure by women to Suaahara's multi‐sectoral interventions
| Comparison | Intervention | Basic Model Significancea | Full Model Significanceb | |
|---|---|---|---|---|
| N = 240 | N = 232 | |||
| Mean (SD)/% | Mean (SD)/% | P value | P value | |
| Frontline workersc | ||||
| Total number of times met with FLWs in the last 6 months | 3.1 (1.6) | 4.5 (2.2)*** | <.001 | .001 |
| Number of times met with FCHV in the last 6 months | 3.9 (3.9) | 4.6 (3.5) | .224 | .699 |
| Home visit by FCHV: percent ever received | 64.6 | 63.8 | .919 | .695 |
| Interaction with FCHV, other than home visit or health mothers' group: percent ever received | 65.4 | 87.1*** | .002 | .001 |
| HTSP counseling by health professional: percent ever received | 54.6 | 87.5*** | <.001 | <.001 |
| Information,d tools, and materials | ||||
| Health: number of information sources in the last 6 months | 2.0 (1.2) | 3.6 (1.5)*** | <.001 | <.001 |
| Nutrition: number of information sources in the last 6 months | 1.6 (1.1) | 3.5 (1.5)*** | <.001 | <.001 |
| FP: number of information sources in the last 6 months | 1.7 (1.3) | 3.2 (1.4)*** | <.001 | <.001 |
| WASH: number of information sources in the last 6 months | 1.3 (1.2) | 3.4 (1.7)*** | <.001 | <.001 |
| Agriculture/HFP: number of information sources in last the 6 months | 0.6 (0.8) | 2.7 (1.7)*** | <.001 | <.001 |
| Health and nutrition: number of tools/materials seene | 0.3 (0.8) | 2.8 (2.5)*** | <.001 | <.001 |
| WASH: number of tools/materials seenf | 0.2 (0.6) | 1.7 (1.8)*** | <.001 | <.001 |
| Key messages | ||||
| Waiting 2 years between each pregnancy: percent heard in last counseling session | 49.6 | 86.2*** | <0.001 | <.001 |
| FP method of woman's choice for 2 years between pregnancies: percent heard in last counseling session | 50.0 | 82.3*** | <0.001 | <.001 |
| Waiting until 20 years of age before trying to become pregnant: percent heard in last counseling session | 22.1 | 72.0*** | <0.001 | <.001 |
| What a pregnant and lactating woman's diet should include (foods, frequency, amount, etc.): percent ever heard | 63.3 | 96.1%*** | <0.001 | <.001 |
| Putting a baby to the breast immediately after birth: percent ever heard | 87.9 | 97.4*** | .001 | <.001 |
| Not putting anything into the child's mouth before breast milk or colostrum: percent ever heard | 65.8 | 78.9*** | .046 | <.001 |
| Feeding only breast milk up to 6 months of age: percent ever heard | 77.9 | 99.6*** | <.001 | .001 |
| Not giving the child any water, liquids, or foods up to 6 months of age: percent ever heard | 60.0 | 89.2*** | <.001 | <.001 |
| Start feeding mashed family foods at 6 months: percent ever heard | 60.0 | 92.7*** | <.001 | <.001 |
| Feeding eggs, fish, and meat (any animal source foods) to children older than 6 months: percent ever heard | 31.7 | 86.6*** | <.001 | <.001 |
| How to feed a child when he or she is sick: percent ever heard | 37.9 | 65.5*** | .001 | <.001 |
| Washing hands with water and soap before feeding the child: percent ever heard | 77.5 | 99.6*** | <.001 | <.001 |
Note. FCHV = female community heath volunteer; FLWs = frontline workers; FP = family planning; HFP = homestead food production; VDC = village development committee; WASH = water, sanitation, and hygiene.
Controlling for VDC‐level clustering.
Controlling for VDC‐level clusering as well as various potential confounders: women's age and education level; household agroecological zone of residency, total number of children <5 years, asset ownership, and roof materials.
FLWs asked about the following: FCHVs; Health assistant/assistant health worker/assistant nurse midwife; traditional healer; agricultural extension worker; livestock extension worker; MOFALD social mobilizer; VDC WASH committee representative; citizen awareness center representative; VDC nutrition and food security steering committee member; ward citizen forum representative; Suaahara field supervisor; Suaahara HFP mothers' group representative; Suaahara peer facilitator; and Suaahara community hygiene and sanitation facilitator.
Potential sources of information asked about include the following: newspaper/magazine; radio/FM; television; brochure/leaflet/poster/banner; FCHV; village model farmer; agriculture/livestock extension worker; village WASH committee member; VDC nutrition and food security steering committee member; social mobilizer; Suaahara field supervisor; ward citizen forum; and citizen awareness center.
Potential health and nutrition tools/material asked about include the following: discussion cards; pictorial books; posters; locally available food; training aid pictures; crop calendar; poultry flip chart; garden‐to‐plate materials; and coop game cards.
Potential WASH tools/material asked about include the following: discussion cards; pictorial books; posters; handwashing demonstration at a handwashing station; WASH DVDs; and PA vial.
Women in Suaahara areas reported having heard information from a greater number of sources for nutrition (S: 3.5; C: 1.6; p < .001), and similar results were found for health, family planning, WASH, and agriculture/HFP. Women in Suaahara areas also reported exposure to more tools and materials both for health and nutrition (S: 2.8; C: 0.3; p < .001) and WASH (S: 1.7; C: 0.2; p < .001). A larger percentage of women in Suaahara areas than in comparison areas recalled having ever been exposed to all eight key MIYCN messages included in the survey, and all of these differences were highly statistically significant (p < .001): maternal diet during pregnancy and lactation; putting a baby to the breast immediately after birth; not putting anything into the child's mouth before breast milk; feeding only breast milk up to 6 months; not giving the child any liquids or foods up to 6 months; starting to feed mashed foods at 6 months; feeding animal source foods to children above 6 months; and how to feed a sick child. A similar pattern was found for WASH and healthy timing and spacing for pregnancy (HTSP) messages.
3.3. Knowledge related to nutrition, health, and water, sanitation, and hygiene
Table 3 presents findings contrasting knowledge levels between women in Suaahara and comparison areas. More women in Suaahara areas had higher knowledge levels about key maternal health and nutrition, and some differences were significant: eating more than usual during pregnancy (S: 96%; C: 79%; p < .001), taking iron/folic acid (IFA) tablets for 180 days during pregnancy (S: 89%; C: 64%; p < .001), and taking 45 IFA tablets during the postpartum period (S: 85%; C: 50% ; p < .001). The difference between groups on knowledge that a pregnant woman needs four ANC visits was only borderline significant.
Table 3.
Women's knowledge on key Suaahara‐promoted health, nutrition, and water, sanitation, and hygiene practices
| Comparison | Intervention | Basic Model Significancea | Full Model Significanceb | |
|---|---|---|---|---|
| N = 240 | N = 232 | |||
| Mean (SD)/% | Mean (SD)/% | P value | P value | |
| Maternal health and nutrition: percent reported correctly | ||||
| 4 ANC check‐ups needed for pregnant woman | 68.3 | 81.9 | .015 | .060 |
| 180 days of iron/folic acid tablets need for pregnant woman | 64.2 | 88.8*** | <.001 | <.001 |
| 45 iron/folic acid tablets needed for partpartum woman | 50.0 | 85.3*** | <.001 | <.001 |
| Eating more than usual during pregnancy | 79.2 | 96.1*** | <.001 | <.001 |
| Child health and nutrition: percent reported correctly | ||||
| Being short/small for age as a sign of malnutrition | 12.9 | 51.7*** | <.001 | <.001 |
| Prevention window of opportunity: first 1,000 days (pregnancy or children <2 years) | 47.5 | 81.0*** | <.001 | <.001 |
| Consequences of child malnutrition: mental development, physical development, poor health, or productivity | 79.2 | 96.6*** | <.001 | <.001 |
| Breastfeeding initiation within 1 hr | 72.5 | 91.4*** | <.001 | <.001 |
| Give colostrum to the baby | 87.5 | 95.3** | .018 | .008 |
| Exclusive breastfeeding definition: breast milk and nothing else (not even water) | 16.3 | 68.1*** | <.001 | <.001 |
| Age to introduce water/clear liquids (6–8.9 months) | 67.1 | 93.5*** | <.001 | <.001 |
| Age to introduce milk/milk products (6–8.9 months) | 70.4 | 92.2*** | .001 | <.001 |
| Age to introduce semi‐solid foods (6–8.9 months) | 81.7 | 94.8*** | .001 | <.001 |
| Age to introduce solid foods (6–8.9 months) | 67.9 | 72.0 | .594 | .353 |
| Age to introduce eggs (6–8.9 months) | 57.1 | 74.1** | .028 | .009 |
| Age to introduce animal meat/fish (6–8.9 months) | 40.0 | 67.7** | .001 | .006 |
| For child illness, feed an extra meal daily/more food/more liquids | 18.8 | 53.5*** | <.001 | <.001 |
| For child illness, continue/increase breastfeeding | 12.5 | 41.4*** | <.001 | <.001 |
| WASH: percent reported correctly | ||||
| All five critical times caretaker of a young child should wash hands | 8.3 | 22.0** | .004 | .002 |
| Water treatment: boiling, adding bleach/chlorine, filtering, or SODIS | 90.8 | 97.4* | .013 | .049 |
Note. ANC = antenatal care; FCHV = female community health volunteers; FP = family planning; SODIS =solar disinfection system; TT = tetanus toxoid; VDC = villege development committee; WASH = water, sanitation, and hygiene.
Controlling for VDC‐level clustering.
Controlling for VDC‐level clusering as well as various potential confounders: women's age and education level; household agroecological zone of residency, total number of children <5 years, asset ownership, and roof materials.
P < .05.
P < .01.
P < .001.
More women in Suaahara areas were also knowledgeable regarding all three indicators of child malnutrition causes, prevention opportunities, and consequences, and these differences were highly significant (p < .001). Knowledge on infant and young child feeding (IYCF) was also stronger in Suaahara areas with more women being aware that breast feeding should be initiated within 1 hr of birth (S: 91%; C: 73%; p < .001); the correct definition of exclusive breastfeeding (S: 68%; C: 16%; p < .001); colostrum should be given (S: 95%; C: 88%; p < .001); and various types of complementary foods should be introduced between 6 and 8.9 months. Furthermore, in Suaahara areas, nearly three times the percentage of women than in comparison areas knew that sick children should receive additional food (S: 54%; C: 19%; p < .001) and continued or increased breastfeeding (S: 41%; C: 13%; p < .001). The difference between areas for knowledge on age to introduce solid foods was minimal and not significant.
Women in Suaahara areas were also significantly more likely than their counterparts in comparison areas to know when a young child's caretaker should wash their hands (S: 22%; C: 8%; p < .01) and the appropriate drinking water treatment methods (S: 97%; C: 91%; p < .05).
3.4. Practices related to nutrition, health, and water, sanitation, and hygiene
Table 4 presents findings related to maternal and child health, nutrition, and WASH practices. Differences between study arms for three ANC indicators were insignificant, but more women in Suaahara areas than in comparison areas used FCHVs as a source for ANC services/counseling (S: 70%; C: 53%; p < .001). The prevalence of consuming IFA tables for 180 days during pregnancy (S: 60%; C: 42%; p < .01) and eating more than usual during pregnancy (S: 76%; C: 32%; p < .001) were higher in Suaahara areas than in comparison areas. Consumption of other fruits and vegetables (S: 80%; C: 66%; p < .05), dairy (S: 69%; C: 39%; p < .001), and eggs (S: 17%; C: 11%; p < .01) was also significantly higher in Suaahara areas, but consumption of meats was significantly more common among women in comparison areas (S: 28%; C: 38%; p < .01).
Table 4.
Household practices on key Suaahara‐promoted health, nutrition, and water, sanitation, and hygiene practices
| Comparison | Intervention | Basic Model Significancea | Full Model Significanceb | |
|---|---|---|---|---|
| N = 240 | N = 232 | |||
| Mean (SD)/% | Mean (SD)/% | P value | P value | |
| Maternal health and nutrition: percent reported | ||||
| Received any ANC | 86.3 | 95.3 | .005 | .165 |
| Received ANC from a skilled provider* (among those who received any ANC; N = 207‐C, 222‐I) | 96.1 | 93.7 | .160 | .757 |
| Received four ANC check‐ups* (among mothers who reported; N = 222‐C, 209‐I) | 44.6 | 40.7 | .553 | .318 |
| Iron/Folic acid tablets for 180 days (pregnancy*; among mothers who reported; N = 206‐C, 205‐I) | 41.8 | 60.0** | .023 | .010 |
| FCHV as source of ANC services/counseling | 52.9 | 69.8*** | .011 | <.001 |
| Eating more than usual during pregnancy | 32.1 | 75.9*** | <.001 | <.001 |
| Institutional delivery (hospital, center or post*; N = 196‐C, 164‐I) | 48.5 | 68.3 | .018 | .092 |
| Any delivery assistance* (N = 196‐C, 164‐I) | 95.9 | 100.0 | N/A | N/A |
| Skilled delivery assistance* (N = 196‐C, I64‐I) | 51.5 | 67.1 | .05 | .327 |
| Women's dietary diversity: percent reported consumption in previous 24 hr | ||||
| Starchy staples | 100.0 | 100.0 | N/A | .743 |
| Beans, lentils, and nuts | 88.3 | 88.8 | .908 | .363 |
| Dairy | 39.2 | 68.5*** | <.001 | <.001 |
| Meat | 38.3 | 27.6** | .116 | .002 |
| Eggs | 10.8 | 17.2** | .070 | .017 |
| Dark green leafy vegetables | 62.9 | 75.0 | .216 | .391 |
| Vitamin A rich fruits and vegetables | 25.8 | 16.0 | .136 | .211 |
| Other fruits and vegetables | 65.8 | 79.7** | .058 | .023 |
| Child health and nutrition: percent reported | ||||
| Vitamin A received within 6 weeks post delivery* (N = 197‐C, 166‐I) | 65.0 | 83.7** | .003 | .011 |
| Vitamin A received in last distribution* (N = 197‐C, 166‐I) | 62.4 | 71.1** | .124 | .006 |
| Colostrum given* (among mothers; N = 197‐C, 166‐I) | 74.6 | 94.0*** | <.001 | <.001 |
| Exclusive breastfeeding (0–5.9 m*; N = 53‐C, 43‐I) | 50.9 | 76.7** | .017 | .003 |
| Ever breastfed (0–23.9 m*; N = 148‐C, 129‐I) | 98.7 | 99.2 | .640 | N/A |
| Age‐appropriate breastfeeding (0–23.9 m*; N = 148‐C, 129‐I) | 57.4 | 59.7 | .726 | .392 |
| Minimum dietary diversity (at least four food groups) (6–23.9 m*; N = 95‐C, 86‐I) | 51.6 | 77.9 | .004 | .075 |
| Consumption of iron‐rich foods (6–23.9 m*; N = 95‐C, 86‐I) | 28.4 | 26.7 | .828 | .094 |
| Introduced water/clear liquids at 6–8.9 months (N = 95‐C, 86‐I) | 54.7 | 81.4*** | .001 | <.001 |
| Introduced milk/milk products (excluding breast milk) at 6–8.9 months (N = 95‐C, 86‐I) | 44.2 | 79.1*** | <.001 | .001 |
| Introduced semi‐solid foods at 6–8.9 months (N = 95‐C, 86‐I) | 65.3 | 90.7*** | <.001 | <.001 |
| Introduced solid foods at 6–8.9 months (N = 95‐C, 86‐I) | 62.1 | 72.1 | .247 | .296 |
| Introduced eggs at 6–8.9 months (N = 95‐C, 86‐I) | 34.7 | 66.3*** | .001 | <.001 |
| Introduced animal meat/fish at at 6–8.9 months (N = 95‐C, 86‐I) | 30.5 | 57.0** | .006 | .002 |
| Child given more food/liquid during illness* (among mothers reporting child has had diarrhea in last 2 weeks; N = 160‐C, 159‐I) | 28.8 | 41.5*** | .111 | .001 |
| Child's dietary diversity (6–23.9 months of age*; N = 95‐C, 86‐I): percent reported consumption | ||||
| Dietary diversity scores (0–7 food groups) | 3.5 (1.3) | 4.2 (1.3)* | .003 | .049 |
| Grains (cereals and tubers) | 94.7 | 94.2 | .857 | .529 |
| Pulses (legumes and nuts) | 85.3 | 86.1 | .876 | .450 |
| Dairy | 46.3 | 75.6** | .001 | .003 |
| Flesh foods | 24.2 | 22.1 | .774 | .094 |
| Eggs | 6.3 | 24.4** | .001 | .007 |
| Vitamin A rich fruits and vegetables | 56.8 | 79.1 | .018 | .407 |
| Other fruits and vegetables | 35.8 | 43.0 | .419 | .316 |
| WASH: percent reported or observed | ||||
| Handwashing station with water and soap/ash available (observation*; among those with observable handwashing station; N = 239‐C, 232‐I, 471‐A) | 49.6 | 86.6*** | <.001 | <.001 |
| Toilet at household (observation) | 81.7 | 91.4 | .117 | .179 |
| Flush toilet facility (observation*; among those who have a toilet; N = 196‐C, 212‐I, 408‐A) | 68.9 | 88.2 | .040 | .117 |
| Toilet cleanliness (observation*; among those who have a toilet; N = 196‐C, 212‐I, 408‐A) | 19.4 | 68.4*** | <.001 | <.001 |
| Handwashing: all five key times | 59.2 | 57.8 | .902 | .192 |
| Water treatment—boiling, adding bleach/chlorine, filtering, or SODIS | 55.0 | 64.2 | .343 | .285 |
| Drinking water pot covered (observation) | 48.8 | 80.2*** | <.001 | .001 |
| No animal or human feces in house/compound (observation) | 46.7 | 61.6 | .160 | .372 |
Note. ANC = antenatal care; FCHV = female community health volunteer; WASH = water, sanitation, and hygiene; SODIS = solar disinfection system.
All five key times for handwashing assessed include the following: before eating, before feeding a child, before preparing food/cooking, after defecation, and after cleaning a child's bottom of feces; All five key steps for handwashing assessed include the following: running or clean water; soap or ash; rubs hands together at least three times; washes both hands; dries by air or with clean cloth
Controlling for VDC‐level clustering
Controlling for VDC‐level clusering as well as various potential confounders: women's age and education level; household agroecological zone of residency, total number of children <5 years, asset ownership, and roof materials.
P < .05.
P < .01.
P < .001.
All child health and nutrition practices promoted by Suaahara were more prevalent in Suaahara areas than in comparison areas, and many were significant including both vitamin A indicators (p < .01); exclusive breastfeeding (S: 77%; C: 51%; p < .01); and the introduction of five of six types of complementary foods between 6 and 8.9 months of age (p < .001). In Suaahara areas, among children 6–23 months, overall dietary diversity was higher (S: 4.2 food groups; C: 3.5 food groups; p < .05), and more children consumed dairy (S: 76%; C: 46%; p < 0.01) and eggs (S: 24%; C: 6%; p < .001). More women in Suaahara areas than in comparison areas increased feeding of foods/liquids for a young child during illness (S: 42%, C: 29%, p < .001). Differences between study arms, which were not significant, included the following: age‐appropriate breastfeeding, minimum dietary diversity, consumption of iron‐rich foods, and introduction of solid foods at 6 to 8.9 months.
Some household‐level WASH indicators were higher in Suaahara areas than in comparison areas: presence of a hand washing station with water and soap/ash (S: 87%; C: 50%; p < .001); having a clean toilet (S: 68%; C: 19%; p < .001); and keeping the drinking water covered (S: 80%; C: 49%; p < .001). Differences between study arms for all other WASH practice indicators were not significant.
3.5. An equity analysis: exposure to Suaahara and knowledge and practices related to nutrition, health, and water, sanitation, and hygiene among disadvantaged and non‐disadvantaged households
Table 5 presents differences (gaps) in exposure, knowledge, and practices between DAG and non‐DAG households and how these gaps differ between Suaahara and comparison areas. To formally test the significance of these differences in DAG gaps, we calculated an interaction effect for all indicators presented in Tables 2, 3, 4 (results available upon request). Although patterns were similar for most indicators, in the final adjusted models, the interaction term was only significant at the 95% level for indicators included in the table and discussed below.
Table 5.
Exposure, knowledge, and practices on key Suaahara‐promoted health, nutrition, and water, sanitation, and hygiene practices, among disadvantaged and non‐disadvantaged households
| Comparison | Non‐DAG to DAG | Intervention | Non‐DAG to DAG | Interaction term | |||
|---|---|---|---|---|---|---|---|
| DAG (N = 122) | Non‐DAG (N = 118) | Difference | DAG (N = 115) | Non‐DAG (N = 117) | Difference | Significancea | |
| Mean (SD)/% | Mean (SD)/% | Mean/% | Mean (SD)/% | Mean (SD)/% | Mean/% | P value | |
| Exposure to Suaahara | |||||||
| Total number of times met with FLWs in last the 6 months | 2.9 (1.4) | 3.3 (1.7) | 0.4 | 4.5 (2.1) | 4.5 (2.3) | 0.0** | .008 |
| HTSP counseling by health professional: percent ever received | 50.0% | 59.3% | 9.3% | 92.2% | 82.9% | −9.3%*** | <.001 |
| Health: number of information sources in the last 6 months | 1.6 (1.1) | 2.3 (1.3) | 0.7 | 3.5 (1.6) | 3.7 (1.5) | 0.2** | .002 |
| Nutrition: number of information sources in the last 6 months | 1.3 (1.0) | 1.9 (1.2) | 0.6 | 3.3 (1.5) | 3.6 (1.5) | 0.3** | .032 |
| FP: number of information sources in the last 6 months | 1.4 (1.2) | 2.0 (1.4) | 0.6 | 3.1 (1.4) | 3.4 (1.5) | 0.3^ | .097 |
| Health and nutrition: number of tools/materials seen | 0.3 (0.9) | 0.3 (0.7) | 0.0 | 2.6 (2.4) | 3.0 (2.6) | 0.4** | .020 |
| Key message: waiting 2 years between each pregnancy: percent heard in last counseling session | 43.4% | 55.9% | 12.5% | 89.6% | 82.9% | −6.7* | .049 |
| Key message: FP method of woman's choice for 2 years between pregnancies; percent heard in last counseling session | 43.4% | 56.8% | 13.3% | 87.0% | 77.8% | 1.9%* | .011 |
| Key message: not putting anything into the child's mouth before breast milk or colostrum: percent ever heard | 61.5% | 70.3% | 8.8% | 83.5% | 74.4% | −9.1* | .045 |
| Key message: not giving the child any water, other liquids, or other foods up to six months of age: percent ever heard | 52.5% | 67.8% | 15.3% | 93.0% | 85.5% | 5.7%* | .037 |
| Knowledge: percent reported correctly | |||||||
| Knowledge: 180 days of iron/folic acid tablets need for pregnant woman | 58.2% | 70.3% | 12.1% | 81.7% | 95.7% | 14.0%* | .046 |
| Knowledge: 45 iron/folic acid tablets needed for part partum woman | 41.0% | 59.3% | 18.3% | 76.5% | 94.0% | 17.5^ | .096 |
| Knowledge: child malnutrition prevention | 39.3% | 55.9% | 16.6% | 79.1% | 82.9% | 3.8^ | .067 |
| Age to introduce water/clear liquids (6–8.9 months) | 59.8% | 74.6% | 14.7% | 94.8% | 92.3% | −2.5%** | .008 |
| Age to introduce milk/milk products (6–8.9 months) | 63.1% | 78.0% | 14.9% | 93.9% | 90.6% | −3.3%** | .008 |
| For child illness, feed an extra meal daily/more food/more liquids | 14.8% | 22.9% | 8.1% | 56.5% | 50.4% | −6.1%** | .006 |
| Practices: percent reported correctly | |||||||
| FCHV as source of ANC services or counseling | 46.7% | 59.3% | 12.6% | 76.5% | 63.3% | −13.3%** | .006 |
| Eating more than usual during pregnancy | 23.0% | 41.5% | 18.6% | 77.4% | 74.4% | −3.0%** | .004 |
| Dairy: consumed by woman in previous 24 hr | 27.1% | 51.7% | 24.6% | 61.7% | 75.2% | 13.5%^ | .076 |
| Exclusive breastfeeding (0–5.9 m) | 44.8% | 58.3% | 13.5% | 94.7% | 62.5% | −32.2* | .051 |
| Introduced milk/milk products (excluding breast milk) at 6–8.9 months | 30.4% | 57.1% | 26.7% | 81.8% | 76.2% | −5.6^ | .091 |
| Dairy: consumed by children 6–23.9 months | 37.0% | 55.1% | 18.1% | 72.7% | 78.6% | 5.9^ | .062 |
| Other fruits and vegetables consumed by children 6–23.9 months | 39.1% | 32.7% | −6.5% | 29.6% | 57.1% | 27.6%* | .026 |
| Handwashing station with water and soap/ash available (observation*; among those with observable handwashing station; N = 239‐C, 232‐I, 471‐A) | 38.5% | 61.0% | 22.5% | 84.4% | 88.9% | 4.5%^ | .055 |
Note. DAG = disadvantaged group; FCHV = female community health volunteers; FLSs = frontline workers; FP = family planning; HTSP =healthy timing and spacing for pregnancy; WASH = water, sanitation, and hygiene.
Potential sources of information asked about include the following: newspaper/magazine; radio/FM; television; brochure/leaflet/poster/banner; FCHV; village model farmer; agriculture/livestock extension worker; village WASH committee member; VDC nutrition and food security steering commmittee member; social mobilizer; Suaahara field supervisor; ward citizen forum; citizen awareness center; potential health and nutrition tools/material asked about include: discussion cards; pictorial books; posters; locally available food; training aid pictures; crop calendar; poultry flip chart; garden‐to‐plate materials; coop game cards; All five key times for handwashing assessed include: before eating, before feeding a child, before preparing food/cooking, after defecation, and after cleaning a child's bottom of feces.
Controlling for VDC‐level clusering as well as various potential confounders: women's age and education level; household agroecological zone of residency, total number of children <5 years, asset ownership, and roof materials.
P < .10.
P < .05.
P < .01.
P < .001.
Gaps between DAG and non‐DAG households in intervention areas were smaller than those in comparison areas for number of information sources exposed to for health (S: 0.2; C: 0.7, p < .01), nutrition (S: 0.3; C: 0.6, p < .01), and family planning (S: 0.3; C: 0.6; p < .001). In comparison areas, there was no gap in exposure to health and nutrition tools and materials, but the levels of exposure for both DAGs and non‐DAGs in Suaahara areas were nearly three times higher (S: 0.4; C: 0.0; p < .05). The DAG/non‐DAG gap was narrower in Suaahara areas for number of FLW meet‐ups in the 6 months prior to the survey (S: 0.0; C: 0.4; p < .01). DAGs in Suaahara areas also reported greater exposure than DAGs in comparison areas, and the DAG/non‐DAG gap in Suaahara areas was narrower and sometimes showing even greater exposure among DAG households than non‐DAG households, for having ever received counseling on HTSP (S: −9%; C: 9%; p < .001) and for exposure to two key messages: heard in the last counseling session about waiting 2 years between pregnancies (S: −7%; C: 13%; p < 0.05) using a family planning method of the woman's choice for 2 years between pregnancies (S: 2%; C: 13%; p < .01) and ever heard to not give the child any water, other liquids, or other foods up to 6 months of age (S: 6%; C: 15%; p < .05).
Furthermore, DAGs in Suaahara areas were more likely to report accurate knowledge for some key maternal and child health and nutrition knowledge variables than DAGs in comparison areas, and the gap between DAG and non‐DAG households in Suaahara areas was much smaller than in comparison areas. However, there were only a few knowledge variables for which the interaction term was significant in adjusted models. These included the percentage aware that pregnant women need to take IFA tablets for 180 days; in this case, the gap was slightly bigger in Suaahara areas, but the percentage of both DAGs and non‐DAGs with this knowledge was more than 20% higher for each group in Suaahara areas than in comparison areas (S: 14%; C: 12%; p < .05). Differences between DAGs and non‐DAGs were also smaller in Suaahara areas for the following: appropriate age for introduction of water and clear liquids (S: −3%; C: 15%; p < .01) and milk and milk products (S: −3%; C:15%; p < .01), as well as knowledge that a sick child should be fed more (S: −6%; C: 8%; p < .01).
The interaction term was significant in fully adjusted models for the following maternal health and nutrition practice indicators: seeking ANC‐related services or counseling from FCHVs (S: −13%; C: 13%; p < .01), eating more during pregnancy (S: −3%; C: 19%; p < 0.01), and exclusive breastfeeding for children under 6 months (S: −32%; C: 14%; p < 0.05). There was one variable for which the significant interaction term favored the comparison areas. Consumption of “other fruits and vegetables” was higher among DAG children in comparison areas than in Suaahara areas, but higher among non‐DAGs in Suaahara areas than in comparison areas. The DAG/non‐DAG gap was much smaller (actually in favor of DAGs) in comparison areas for this one feeding practice (S: 28%; C: −7%; p < .05).
4. DISCUSSION AND CONCLUSIONS
These results provide encouraging evidence that an integrated intervention with multiple delivery platforms can address exposure, knowledge, and practice barriers to nutritional well‐being among mothers and children under 2 years of age. Large significant differences were observed between intervention and comparison groups after only 2 years of program implementation. In Suaahara areas, the prevalence was higher for almost all exposure and knowledge indicators and some practice indicators for maternal and child health and nutrition and WASH. Although our data did not allow for direct comparison and estimation of effects, major differences between Suaahara and comparison areas were not evident in the baseline survey (Cunningham & Kadiyala, 2013). Our equity analysis showed that a greater percentage of DAG households in Suaahara areas was exposed to nutrition information than in comparison areas. DAG households in Suaahara areas were also more knowledgeable about nutrition and more likely to practice almost all of the behaviors promoted by Suaahara. Finally, the gaps between DAG and non‐DAG households were significantly smaller in Suaahara areas than in comparison areas for many of the same exposure, knowledge, and practice indicators. This examination of several steps along Suaahara's implementation pathways, and the equity analysis, exemplifies the possibilities of using detailed PE studies to assess programs (Mbuya et al., 2015).
New evidence points out that if reductions in stunting in South Asia are to be achieved, progress is needed in child diets and nutrition in the first 1,000 days, maternal diet and nutrition during pregnancy and lactation, and WASH (Aguayo & Menon, 2016)—three areas in which we focus our analysis. The magnitude of the differences between intervention and comparison areas varied across selected indicators. This is likely due, at least in part, to Suaahara's gradual roll‐out of key themes per year, resulting in the emphasis of certain desired behavior changes for a longer total period of time than others. Unsurprisingly, most knowledge differences between intervention and comparison areas are larger than the practice differences. This may reflect that additional time is needed for knowledge to translate into certain behaviors, or that for some behaviors, translation from knowledge into practice may require addressing other constraints, for instance, those related to income, social norms, and self‐efficacy, as well as availability, affordability and accessibility of foods or health, and nutrition and family planning products or services (Adhikari, 2016; Affleck & Pelto, 2012; Yates et al., 2012). Finally, one result was surprising—that 38% of women in comparison areas and only 28% of women in Suaahara areas reported to consume meat. This could be due to unmeasured caste and ethnic differences or unidentified socioeconomic differences. However, given that consumption of meat was much higher in Suaahara areas (69% vs. 39%), as was consumption of all other nutritious foods, it is quite likely that it is due to Suaahara's promotion of dairy as an alternative animal source food if eggs or meat are too costly and programmatic emphasis on consuming as many diverse foods as possible. With scarce resources, households in Suaahara areas may have opted to consume dairy plus other nutrient‐rich foods rather than just meat. Without qualitative research, these reasons remain hypothetical and in need of further research to understand household decision‐making.
This study adds to the evidence base that achieving nutrition‐related behavior change at scale is possible with intensive interventions. For instance, progress in IYCF indicators is consistent with evidence from the Alive & Thrive program in Bangladesh, which documented significant progress in several breastfeeding and complementary feeding indicators (Sanghvi et al., 2016). Suaahara activities, once fully rolled‐out, took place in more than half of Nepal's 75 districts and within each district, included all households with a woman in the 1,000‐day period. The time‐intensive nature of full programmatic roll‐out in a staged manner and using context‐specific approaches per district should not be minimized. For at‐scale implementation to be possible, investments in time and human resources are required. The Suaahara PE data shows high levels of program coverage and utilization with at‐scale implementation. Suaahara's combination of nutrition‐specific and nutrition‐sensitive approaches, and explicit focus on social inclusion, enabled Suaahara to tackle multiple determinants of under nutrition at once, in line with current regional recommendations (Vir, 2016). Furthermore, Suaahara's approach of using FLWs from the same communities likely contributed to the communities' engagement with programmatic activities. For example, the fact that FCHVs are highly respected and a valued source of health information has been theorized to be an important factor in the success of other programs that used this cadre to deliver child health and nutrition services (Thapa, 2014).
Our results show that an integrated at‐scale nutrition program can reduce inequities in health‐ and nutrition‐related knowledge and practices. This is consistent with evidence that increasing the coverage of interventions helps to ameliorate disparities in health related to socioeconomic status (Victora et al., 2012). Few nutrition programs globally have attempted to operate with such wide geographic coverage, and even fewer have explicitly focused on equity, but there is an increasing call for large‐scale nutrition programs to close equity gaps for vulnerable populations (Aguayo & Menon, 2016). In addition to operating at scale, Suaahara's explicit targeting and GESI approach to program implementation allowed FLWs to provide appropriate support and follow‐up so that support of situation‐specific knowledge and optimal practices for both advantaged and disadvantaged women could be maximized. Other data also suggest that rapid increases in program coverage accompanied by purposeful targetting can reduce inequalities (Victora et al., 2003). Nepal's successful vitamin A distribution was also at scale and with explicit attention to coverage barriers related to equity (Thapa, 2014). Although similarities can be seen in scale and equity focus, the vitamin A campaign was a single health sector intervention, whereas Suaahara involved a package of multi‐sectoral interventions. Therefore, in addition to challenges relating to Nepal's difficult terrain, extreme topographical differences, weak infrastructure, tremendous cultural and linguistic diversity, and long‐standing inequities which all initiatives must face, Suaahara was also challenged by political instability, weak governance, limited capacity of government functionaries, particularly outside of the health sector, for development of nutrition‐related services, and coordination at all levels and across sectors.
There were several study limitations that should be noted. First, the cross‐sectional nature of this study makes causal inferences impossible. However, for this PE analysis, we used fully adjusted models including an interaction term to estimate the effect of Suaahara on reducing inequalities. Suaahara's PE involved careful matching of intervention and comparison districts, ensuring that there were no similar large‐scale nutrition programs, and using random sampling at the VDC and ward level. In the last several years, scientists have emphasized the need for rigorous PE studies to generate evidence on both the design of complex programs and meaningful findings on program implementation and uptake (Mbuya et al., 2015; Menon, Rawat, & Ruel, 2013). Second, the household‐level sampling relied on FCHVs to accurately identify DAG households, which may have introduced bias and misclassification. However, FCHVs are long‐standing community leaders, known to be familiar with households' socioeconomic and cultural status in their own wards. Furthermore, our study is novel in our explicit sampling approach: our sample provides group‐specific estimates, thereby facilitating equity analysis in Suaahara and non‐Suaahara areas. The statistical significance of the interaction term exhibits heterogeneity based on the model implemented, perhaps in part due to lack of statistical power for some models; however, the direction of the impact is consistent across specification, providing evidence of an effective program and robust results.
Several critical questions remain, and further research is needed to determine whether these results are specific to this context, or are also applicable to similar settings in South Asia or other low‐ and middle‐income countries. It would also be interesting to know which program components are most responsible for differences seen between intervention and comparison areas. Finally, whether and how these changes in nutrition‐related knowledge and practices translate into changes in nutritional status should be investigated. With greater global focus on multi‐sectoral nutrition interventions, answering these additional research questions is urgent and requires commitment by development partners in rigorous evaluation studies.
The Suaahara experience is instructive both for Nepal and for the global context, as it provides evidence that complex integrated programs can work to reduce health‐ and nutrition‐related inequities, even while operating at scale. Given that Nepal's current policy environment is supportive of addressing food and nutrition insecurity, as seen in the MSNP, Zero Hunger Challenge, Food and Nutrition Security Plan of Action, and increased interest and communittment by the GoN and development partners alike, Nepal is uniquely positioned to scale‐up the implementation of both nutrition‐specific and nutrition‐sensitive interventions to further address the problem of persistent undernutrition, in a way that benefits all sections of Nepalese society. Development partners and the GoN should use findings from Suaahara in the design and implementation of emerging initiatives to address inequities in health and nutrition, which would also be consistent with the recently endorsed sustainable development goals.
SOURCE OF FUNDING
Suaahara I, funded by the United States Agency for International Development (USAID) Cooperative Agreement AID‐367‐A‐11‐00004, provided financial support for this survey and analysis. This study is made possible by the generous support of the American people through USAID. The contents are the responsibility of the authors and do not necessarily reflect the views of USAID or the United States Government.
CONFLICTS OF INTEREST
K C was an independent research consultant during Suaahara I, but is now employed by Suaahara II. All other authors worked for one of the non‐governmental organizations involved with Suaahara I.
CONTRIBUTIONS
K C designed the study, conducted the statistical analyses, and prepared the first draft of the manuscript. A S, P P, K L, S A, R K, B G, and C U provided revisions and additional text to manuscript drafts. K C prepared the final manuscript and all authors read and approved the final version for submission.
ACKNOWLEDGMENTS
We extend our sincere thanks to Valley Research Group for data collection. Most of all, we thank the survey respondents for their time and the FCHVs and Suaahara field supervisors for their time and commitment in helping carry out this study in their communities. We also acknowledge contributions made by colleagues at Save the Children, Helen Keller International, Johns Hopkins University Bloomberg School of Public Health Center for Communication Programs, JHPIEGO, Nepal Technical Assistance Group, Nepal Water for Health, and Nutrition, and Nutrition Promotion and Consultancy Service. Finally, we are grateful to Kalyani Raghunathan, Suman Chakrabati, and Hazel Malapit for providing statistical input for the analysis.
Cunningham K, Singh A, Pandey Rana P, et al. Suaahara in Nepal: An at‐scale, multi‐sectoral nutrition program influences knowledge and practices while enhancing equity. Matern Child Nutr. 2017;13:e12415 10.1111/mcn.12415
[Correction added on 22 May 2017, after first online publication: The city and state of affiliation 4 has been corrected in this current version]
REFERENCES
- Adhikari, R. (2016). Effect of Women's autonomy on maternal health service utilization in Nepal: A cross sectional study. BMC Women's Health, 16(1), 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Affleck, W. , & Pelto, G. (2012). Caregivers' responses to an intervention to improve young child feeding behaviors in rural Bangladesh: A mixed method study of the facilitators and barriers to change. Social Science and Medicine, 75(4), 651–658. [DOI] [PubMed] [Google Scholar]
- Aguayo, V. , & Menon, P. (2016). Stop stunting: improving child feeding, women's nutrition and household sanitation in South Asia. Maternal & Child Nutrition, 12(Sppl. 1), 3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anon . (2015). SUAAHARA: Process evaluation results from frontline worker and household surveys,
- Anon. (2006). Unequal citizens: Gender, caste and ethnic exclusion in Nepal. Kathmandu. United States Agency for International Development, http://pdf.usaid.gov/pdf_docs/PA00KWXG.pdf.
- Bhutta, Z. A. , Tahmeed, A. , Cousens, S. , Dewey, K. , Giugliani, E. , Haider, B. A. , … for the Maternal and Child Undernutrition Study Group . (2008). What works? Interventions for maternal and child undernutrition and survival. Lancet, 371(9610), pp.417–40. [DOI] [PubMed] [Google Scholar]
- Black, R. E. , Victora, C. G. , Walker, S. P. , Bhutta, Z. A. , Christian, P. , de Onis, M. , … Maternal and Child Nutrition Study Group . (2013). Maternal and child undernutrition and overweight in low‐income and middle‐income countries. The Lancet, 382(9890), 427–451. [DOI] [PubMed] [Google Scholar]
- Crum, J. , Mason, J. , Pokharel, R. , Hutchinson, P. , Mebrahtu, S. & Dahal, P . (2013). Trends and determinants of maternal and child nutrition in Nepal: Further analysis of the Nepal Demographic and Health Surveys, 1996–2011 ., Kathmandu.
- Cunningham, K. , Singh, A. , Headey, D. , Pandey Rana, P. & Karmacharya, C . (2016). Reaching hew heights: 20 years of nutrition progress in Nepal In Pandya‐lorch R., Yosef S., & Gillespie S. (Eds.), Nourishing Millions. (pp. 115–124). Washington D.C: International Food Policy Research Institute (IFPRI). [Google Scholar]
- Cunningham, K. & Kadiyala, S. (2013). Suaahara baseline survey report. pp. 1–135.
- Devkota, M. D. , Adhikari, R. K. , & Upreti, S. R. (2016). Stunting in Nepal: Looking back, looking ahead. Maternal & Child Nutrition, 12, 257–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devkota, S. & Bennett, D. (2014). Gender equality and social inclusion for food‐ and nutrition‐security in Nepal, Washington D.C.
- Government of Nepal National Planning Commission . (2012). Multi‐sectoral nutrition plan: For accelerating the reduction of maternal and child under‐nutrition in Nepal.
- Gwatkin, D.R. , Rutstein, S. , Johnson, K. , Suliman, E. , Wagstaff, A. , & Amouzou, A . (2007). Socio‐Economic differences in health, nutrition and population within developing countries: An overview, [PubMed]
- Headey, D. , & Hoddinott, J. (2015). Understanding the rapid reduction of undernutrition in Nepal, 2001–2011. PloS One, 10(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Headey, D. , Hoddinott, J. , & Park, S. (2016). Drivers of nutritional change in four South Asian countries: A dynamic observational analysis. Maternal & Child Nutrition, 12, 210–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoddinott, J. , Behrman, J. R. , Maluccio, J. A. , Melgar, P. , Quisumbing, A. R. , Ramirez‐Zea, M. , … Martorell, R . (2013). Adult consequences of growth failure in early childhood. American Journal of Clinical Nutrition, 98, 1170–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoddinott, J. , Maluccio, J. , Behrman, J. R. , Martorell, R. , Melgar, P. , Quisumbing, A. R. , … Yount, K. M . (2011). The consequences of early childhood growth failure over the life course, Washington D.C. [DOI] [PMC free article] [PubMed]
- Hoddinott, J. , Alderman, H. , Behrman, J. R. , Haddad, L. , & Horton, S. (2013). The economic rationale for investing in stunting reduction. Maternal & Child Nutrition, 9(Suppl 2), 69–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horton, R. , & Lo, S. (2013). Nutrition: A quintessential sustainable development goal. The Lancet, 6736(13), 9–10. [DOI] [PubMed] [Google Scholar]
- Mbuya, M. N. N. , Jones, A. , Ntozini, R. , Humphrey, J. H. , Moulton, L. H. , Stoltzfus, R. J. , … for the Sanitation Hygiene Infant Nutrition Efficacy (SHINE) Trial Teama . (2015). Theory‐driven process evaluation of the SHINE trial using a program impact pathway approach. Clinical Infectious Diseases, 61(Suppl 7), S752–S758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon, P. , Covic, N. , Harrigan, P. B. , Horton, S. E. , Kazi, N. M. , Lamstein, S. , … Pelletier, D. (2014). Strengthening implementation and utilization of nutrition interventions through research: A framework and research agenda. Annals of the New York Academy of Sciences. [DOI] [PubMed]
- Menon, P. , Rawat, R. , & Ruel, M. (2013). Bringing rigor to evaluations of large‐scale programs to improve infant and young child feeding and nutrition: The evaluation designs for the Alive & Thrive initiative. Food and Nutrition Bulletin, 34(3), 195–211. [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Popualation (MOHP) Nepal . (2012). Nepal Demographic and Health Survey 2011, Kathmandu; Calverton.
- Pokharel, R. J. , Houston, R. , Harvey, P. , Bishwakarma, R. , Adhikari, J. , Dev Pant, K. , … Gartoulla, R . (2009). Nepal nutrition assessment and gap analysis, 1–81.
- Robert, R. C. , Gittelsohn, J. , Creed‐Kanashiro, H. M. , Penny, M. E. , Caulfield, L. E. , Narro, M. R. , … Black, R. E. (2007). Implementation examined in a health center‐delivered, educational intervention that improved infant growth in Trujillo, Peru: Successes and challenges. Health Education Research, 22(3), 318–331. [DOI] [PubMed] [Google Scholar]
- Robert, R. C. , Gittelsohn, J. , Creed‐Kanashiro, H. M. , Penny, M. E. , Caulfield, L. E. , Narro, M. R. , & Black, R. E. (2006). Process evaluation determines the pathway of success for a health center‐delivered, nutrition education intervention for infants in Trujillo, Peru. Journal of Nutrition, 136, 634–641. [DOI] [PubMed] [Google Scholar]
- Ruel, M. T. , & Alderman, H. (2013). Nutrition‐sensitive interventions and programmes: How can they help to accelerate progress in improving maternal and child nutrition? The Lancet, 382(9890), 536–551. [DOI] [PubMed] [Google Scholar]
- Sanghvi, T. , Haque, R. , Roy, S. , Afsana, K. , Seidel, R. , Islam, S. , … Baker, J. (2016). Achieving behaviour change at scale: Alive & Thrive's infant and young child feeding programme in Bangladesh. Maternal & Child Nutrition, 12(1), 141–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shekar, M. , Dayton Eberwein, J. , & Kakietek, J. (2016). The costs of stunting in South Asia and the benefits of public investments in nutrition. Maternal & Child Nutrition, 12, 186–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp . (2013). Stata Statistical Software: Release 13.
- Thapa, S. (2014). High and equitable coverage of vitamin A supplementation program in Nepal. Journal of Community Medicine & Health Education, 4(1). [Google Scholar]
- UNDP . (2015). Local Governance and Community Development Programme (LGCDP), (July 2015).
- UNICEF . (1990). A UNICEF policy review strategy for improved nutrition of children and women in developing countries, New York, NY.
- UNICEF WHO and World Bank Group . (2015). Levels and trends in child malnutrition: UNICEF‐WHO‐World Bank joint child malnutrition estimates. New York, NY; Geneva; Washington DC. [Google Scholar]
- Victora, C. G. , Wagstaff, A. , Schellenberg, J. A. , Gwatkin, D. , Claeson, M. , & Habicht, J‐P. (2003). Applying an equity lens to child health and mortality: More of the same is not enough. The Lancet, 362, 233–241. [DOI] [PubMed] [Google Scholar]
- Victora, C. G. , Barros, A. J. D. , Axelson, H. , Bhutta, Z. A. , Chopra, M. , Franca, G. V. A. , … Boerma, J. T. (2012). How changes in coverage affect equity in maternal and child health interventions in 35 Countdown to 2015 countries: an analysis of national surveys. Lancet, 380(9848), 1149–1156. [DOI] [PubMed] [Google Scholar]
- Vir, S. C. (2016). Improving women's nutrition imperative for rapid reduction of childhood stunting in South Asia: coupling of nutrition specific interventions with nutrition sensitive measures essential. Maternal & Child Nutrition, 12, 72–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yates, B. C. , Pullen, C. H. , Santo, J. B. , Boeckner, L. , Hageman, P. A. , Dizona, P. J. , & Walker, S. N. (2012). The influence of cognitive‐perceptual variables on patterns of change over time in rural midlife and older women's healthy eating. Social Science and Medicine, 75(4), 659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]


