Abstract
Breastfeeding rates among mothers in the Supplemental Nutrition Program for Women, Infants, and Children (WIC) are lower than for other mothers in the United States. The objective of this study was to test the acceptability and feasibility of the Lactation Advice thru Texting Can Help intervention. Mothers were enrolled at 18–30 weeks gestation from two WIC breastfeeding peer counselling (PC) programmes if they intended to breastfeed and had unlimited text messaging, more than fifth‐grade literacy level, and fluency in English or Spanish. Participants were randomized to the control arm (PC support without texting) or the intervention arm (PC support with texting). The two‐way texting intervention provided breastfeeding education and support from peer counsellors. Primary outcomes included early post‐partum (PP) contact and exclusive breastfeeding (EBF) rates at 2 weeks PP. Feasibility outcomes included text messaging engagement and mother's satisfaction with texting platform. Fifty‐eight women were enrolled, 52 of whom were available for intention‐to‐treat analysis (n = 30 texting, n = 22 control). Contact between mothers and PCs within 48 hr of delivery was greater in the texting group (86.6% vs. 27.3%, p < .001). EBF rates at 2 weeks PP among participants in the texting intervention was 50% versus 31.8% in the control arm (p = .197). Intervention group mothers tended to be more likely to meet their breastfeeding goals (p = .06). Participants were highly satisfied with the Lactation Advice thru Texting Can Help intervention, and findings suggest that it may improve early post‐delivery contact and increase EBF rates among mothers enrolled in WIC who receive PC. A large, multicentre trial is feasible and warranted.
Keywords: breastfeeding, breastfeeding support, infant, low income, peer support, newborn feeding behaviours
1. INTRODUCTION
Exclusive breastfeeding is recommended for the first 6 months of life, yet in the United States, adherence is suboptimal and there are inequities by income and race (Johnston, Landers, Noble, Szucs, & Viehmann, 2012). In 2014, in the United States, 79.2% of mothers initiated breastfeeding, but only 18.8% of infants were exclusively breastfed at 6 months of age (CDC, 2014). Among women of lower socioeconomic status who participate in the federal Supplemental Nutrition Program for Women, Infants, and Children (WIC), rates of breastfeeding are even lower (Ryan & Zhou, 2006). The WIC programme provides supplemental foods, health care referrals, and nutrition education for low‐income pregnant, breastfeeding, and non‐breastfeeding post‐partum women and their children under 5 years of age. In fact, in a national sample, one fourth of mothers enrolled in WIC stopped breastfeeding by the end of the second week of life and one half had stopped breastfeeding by the end of the second month (McCann, Baydar, & Williams, 2007). Women who have Medicaid insurance have also been shown to be three times more likely to stop breastfeeding by 2 weeks post‐partum than women who had other insurance (Brand, Kothari, & Stark, 2011). In addition, rates of breastfeeding cessation have been shown to be twice as high in mothers without a high school education or with only a high school diploma than in mothers with any college education. Differences in experiences related to breastfeeding initiation and cessation suggest that targeted and affordable breastfeeding interventions are necessary (Hurley, Black, Papas, & Quigg, 2008).
Barriers to mothers enrolled in WIC initiating or continuing to breastfeed include embarrassment to breastfeed in front of others, time and social constraints when breastfeeding while going to work or school, and lack of social support (Whitacre & Moats, 2011). Furthermore, the lack of preparation for the early post‐partum period, including breastfeeding and expectations of infant behaviour, has been identified as a common reason for mothers' formula requests from WIC during the early post‐partum period (DaMota, Bañuelos, Goldbronn, Vera‐Beccera, & Heinig, 2012). Although traditional breastfeeding peer counselling improves rates of breastfeeding initiation, duration, and exclusivity (Chapman, Morel, Anderson, Damio, & Pérez‐Escamilla, 2010), innovative communication technology may allow peer counselling to be strengthened. WIC breastfeeding peer counsellors are mothers who have personal experience with breastfeeding and are trained to provide basic breastfeeding information and support to other mothers with whom they share various characteristics, such as language, race/ethnicity, and socioeconomic status. They work to reinforce breastfeeding recommendations and promote breastfeeding as an important element in the healthy development of the mother and baby. According to the Institute of Medicine report Updating the USDA National Breastfeeding Campaign, WIC breastfeeding PCs support text messaging for establishing communication and providing support (Whitacre & Moats, 2011). Furthermore, mothers have expressed that text messaging is convenient, especially during the early post‐partum period (Cormick et al., 2012; Perrin, 2012).
Despite PCs and mothers favourably describing communication via text messaging, there are few trials of interventions to test the effectiveness of text messaging used to provide breastfeeding support (Gallegos, Russell‐Bennett, Previte, & Parkinson, 2014; Jiang et al., 2014). Accordingly, we designed and evaluated a pilot texting intervention, “LATCH: Lactation Advice thru Texting Can Help,” a two‐way texting platform used as an adjunct tool for WIC breastfeeding PCs to provide timely peri‐partum breastfeeding support. This study was conducted in preparation for a randomized‐controlled study to clarify several logistical aspects of the intervention such as determining sample size, willingness of participants to be randomized, willingness of participants to interact with the messaging platform, assessing the ability of PCs to respond to participants' concerns via text messages, examining mothers' response to the content of automatic text messages, determining optimal frequency of automatic text messages, and assessing overall acceptability of the texting intervention. Considering how ubiquitous cell phone use and text messaging is and the strong commitment form WIC to support breastfeeding, LATCH is a timely intervention (Pérez‐Escamilla, 2012).
Key messages.
Breastfeeding education and support via two‐way text messaging delivered by peer counsellors is highly feasible among Women, Infants, and Children (WIC) participants.
Mothers enrolled in WIC were highly satisfied with the two‐way breastfeeding texting intervention.
The two‐way texting intervention strongly enhanced the chance that mothers could be reached within 48 hr after birth by their peer counsellors.
2. METHODS
2.1. Formative research
Prior to launching this pilot, we held three informal focus groups (two in Spanish and one in English) to help tailor the text messaging for our target population (Kruger & Casey, 2000). Participants (n = 21) included mothers (aged 20–38 years) who had recently participated in the WIC breastfeeding PC programmes at the two sites where we planned to implement the intervention: a hospital‐based primary care centre and a federally qualified community health centre. We created a focus group guide to explore what information could be helpful prenatally to prepare mothers for the post‐partum experience, what information or support could help mothers overcome the challenges of breastfeeding, and logistics surrounding the planned pilot (e.g., frequency of texting, current texting plans, and PC response time; Miles & Huberman, 1994; Patton, 2002). Discussion surrounded on what breastfeeding information would have better prepared the mothers for the immediate post‐partum period, specific difficulties experienced post‐partum, and how text messaging with their PC could help support them. We also polled participants regarding their cell phone plans. All participants had unlimited texting capacity, and all, but one, had an unlimited data plan. A working team was then formed consisting of a PC, two lactation consultants, a maternal–child nutritionist, and two paediatricians. This team used focus group data, along with published literature, to develop a prenatal and post‐partum breastfeeding curriculum via automated text messages. Yale's Human Investigation Committee approved our request for Human Investigation Committee exemption to conduct these focus groups because the focus groups were held informally (no audio recording [just note taking]) and no personal identifiers were recorded.
A literature review identified breastfeeding attitudes and reported barriers to exclusive breastfeeding and key determinants associated with longer duration of exclusive breastfeeding among mothers enrolled in the WIC programme (Bunik et al., 2006; Hannon, Willis, Bishop‐Townsend, Martinez, & Scrimshaw, 2000; Hurley et al., 2008; McCann et al., 2007; Zimmerman & Guttman, 2001). Texts were then tailored to address key breastfeeding barriers and behavioural beliefs. Texting content was timed to coincide and reinforce the WIC breastfeeding PC lessons developed by the Hispanic Health Council, Hartford, Connecticut. See Appendix A for detailed description of texting schedule and Table 1 for a sample of prenatal, peri‐partum, and postnatal text messages.
Table 1.
Sample of automatic Lactation Advice thru Texting Can Help text messages
| Prenatal |
| • Some babies go right to the breast. Sometimes you will need to help them latch on. See video for details: (link to video) |
| • Finding a good breastfeeding position for you and your baby can prevent sore nipples. Here are some pictures: (link to pictures) |
| • Milk changes every day. Over the first few days after delivery, the amount of milk you have will slowly increase. The more you feed, the more you make. |
| Peri‐partum |
| • To make lots of milk, breastfeed often the first few days (at least 8–10 times per day) |
| • Crying is a late sign of hunger. Look for early cues that your baby is hungry. (smacking lips, sucking hands). For more signs see: (link to handout) |
| • Sore nipples are not normal. Holding your baby in a comfortable way while breastfeeding can help. When baby is born, text me and I will show you. |
| Post‐partum |
| Day 1: |
| • Remember to place your baby skin‐to‐skin (baby naked) on your chest for an hour. This will allow baby to get to know you and latch on to breast better. |
| • Your body has already started to make milk. Each day you will make more and more milk. Your baby only needs a little bit at the beginning. |
| • Hi (first name) if you have any questions let me know. I am here to support you. (peer counselor) |
| • While in the hospital, ask nurses for help breastfeeding. They can help you! Any time … day or night! |
| Day 4: |
| • What does your baby's poop look like today? (Answer A, B or C) |
| ◦ A: Yellow, soft |
| ◦ B: Dark brown/black |
| ◦ C: Greenish to yellow |
| • How many times a day is s/he pooping? Text back number. |
| Day 5: |
| • Do you feel your baby is getting enough milk? Respond (A,B, or C) |
| ◦ A: Yes |
| ◦ B: No |
| ◦ C: Not Sure |
| 2 weeks: |
| Planning to back to work soon? Continue to breastfeed. Your baby doesn't need to be trained on bottle yet. I can help you get ready to go back to work. |
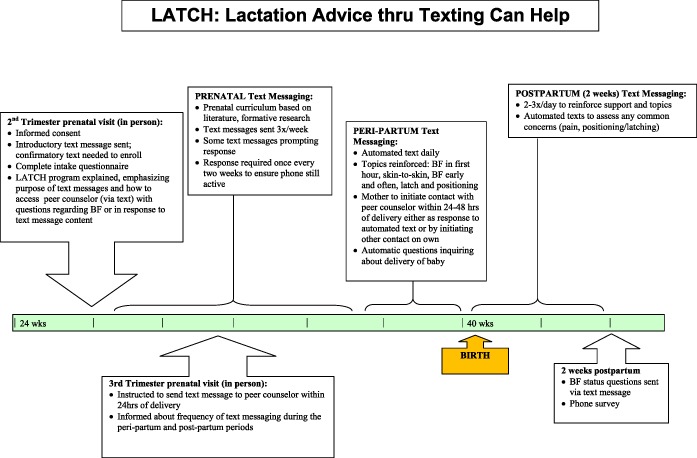
2.2. Texting intervention
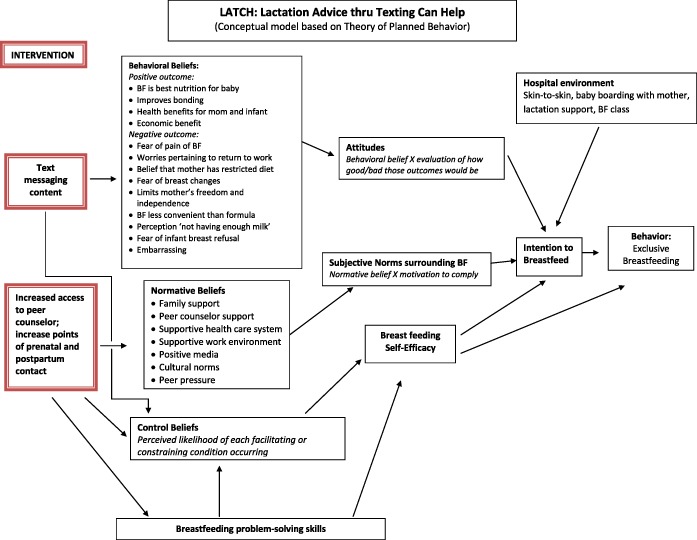
LATCH is a web‐based texting intervention designed to improve breastfeeding rates among mothers receiving WIC. The two‐way texting intervention provided both evidence‐based breastfeeding education through automated texts and a mode for mothers to freely exchange texts with breastfeeding PC. A conceptual model based on the theory of planned behaviour was used to help guide the texting intervention (Appendix B; Ajzen, 1991). In this model, we posited that automatic text messages and increased contact with PCs would have a positive impact on breastfeeding beliefs and problem solving skills that would in turn improve breastfeeding attitudes, intentions, and behaviours.
In addition to providing breastfeeding education, the automated texts were personalized by addressing the mother by name and signed by the PC. These automatic personalized texts were sent out regularly both prenatally and in the immediate post‐partum period to increase PC points of contact with mom via text. Although mothers could respond to the automated text or reach out via text 24 hr a day, mothers were informed that the PC would respond to texts only between 8 a.m. and 5 p.m. Monday–Friday. The web‐based texting platform allowed all text messages to be recorded, and thus, the on‐site lactation consultants and WIC supervisors were able to monitor and supervise all text‐based communication regularly.
In addition, an advisory team (PCs, International Board Certified Lactation Consultants [IBCLCs], a state WIC nutrition coordinator, a paediatrician, and a maternal–child nutritionist) met regularly to review text message conversations between mothers and PCs throughout the study period. Any concerns raised by the PCs or lactation consultants were discussed, and consensus decision making was used to determine how best to respond to different issues raised via text by mothers.
The web‐based texting platform was protected by Secure Sockets Layer encryption, and data stored in the hosted environment met security requirements of the Yale Health Insurance Portability and Accountability Act (HIPPA) Business Associate Agreement. This pilot study was not registered with a clinical trials registry because it was a feasibility study for designing a full trial. The latter is ongoing and was registered under https://connect.yale.edu/owa/redir.aspx?SURL=QzpowGFwUqleJUyY7QbtovYbKm8cEMiM-z77PnHZYptEtn-MaSbTCGgAdAB0AHAAcwA6AC8ALwB1AHIAbABkAGUAZgBlAG4AcwBlAC4AcAByAG8AbwBmAHAAbwBpAG4AdAAuAGMAbwBtAC8AdgAyAC8AdQByAGwAPwB1AD0AaAB0AHQAcAAtADMAQQBfAF8AYwBsAGkAbgBpAGMAYQBsAHQAcgBpAGEAbABzAC4AZwBvAHYAJgBkAD0AQQB3AE0ARgBhAFEAJgBjAD0ALQBkAGcAMgBtADcAegBXAHUAdQBEAFoAMABNAFUAYwBWADcAUwBkAHEAdwAmAHIAPQBFAFoAawBSAG8AbQBUAHIASABVAHgARgA4AEwAdgBFAHAAZwA5AFEAagBZADgAawBpAGYAdgBoAGoAeQB1AFkAagA4AFoAbQBaADUAUwBhAEEAdgBFACYAbQA9AG0AeQBWAFcAUQBUAFEAOQBqAEsANwBTAC0AOQBEAGgAMwAxAEcAegAtAHoASwBTAFYAdgBNAFUANQBYAC0ATABMAGwAdAAzAEUAQgBvADUAUABXAGMAJgBzAD0AUABWAE0AagBsAHUAQQBoAFkAdQBGAHkAYQBrAGgAegBUADQAdgBrAEQATwBpAHoAcABMAGUAQQB4AEgARQBfADIAbwBjAG4ANwB1AHIAOABZAHAASQAmAGUAPQA.&URL=https%3a%2f%2furldefense.proofpoint.com%2fv2%2furl%3fu%3dhttp-3A__clinicaltrials.gov%26d%3dAwMFaQ%26c%3d-dg2m7zWuuDZ0MUcV7Sdqw%26r%3dEZkRomTrHUxF8LvEpg9QjY8kifvhjyuYj8ZmZ5SaAvE%26m%3dmyVWQTQ9jK7S-9Dh31Gz-zKSVvMU5X-LLlt3EBo5PWc%26s%3dPVMjluAhYuFyakhzT4vkDOizpLeAxHE_2ocn7ur8YpI%26e%3d (LATCH; NCT02214849).
2.3. Study design
Pregnant women were recruited and enrolled at 18–30 weeks gestation from local WIC breastfeeding PC programmes at two sites—a hospital‐based primary care centre and a federally qualified community health centre. A small target sample size (60 participants) was chosen as this pilot study was designed to demonstrate intervention feasibility and guide the planning for a larger trial. Inclusion criteria included intention to breastfeed via self‐report, unlimited text message cell phone plan, fifth grade or greater literacy level, and fluency in English or Spanish. Post‐partum exclusions included infant born premature (<37 weeks), >3 days in neonatal intensive care unit, major medical problem affecting breastfeeding, or birthweight <5 lbs. Breastfeeding PCs screened expectant mothers for eligibility and enrolled them in the study. The enrollment process occurred in‐person in the clinic or over the phone. All participants provided verbal informed consent before participating in the study and received a $25 gift card after completion of the 2‐week post‐partum follow‐up survey. Verbal consent was approved by Yale's Human Investigation Committee. An information sheet (at a fifth grade reading level) was provided to each participant. Because participants were recruited at WIC sites, the PCs requested that we seek verbal consent for ease of recruitment. The study was approved by the Yale University Human Research Protection programme.
Eligible women were randomly assigned in a 1:1 ratio to either the control arm (breastfeeding PC support programme without texting) or the intervention arm (breastfeeding PC support programme with texting intervention). The allocation sequence for randomization, stratified by PC and language, was generated by an independent biostatistician via a computer‐generated random‐number sequence. Immediately after enrollment, the PC contacted the principal investigator (N.H.) who assigned the randomization arm based on allocation sequence. The principal investigator did not have patient contact. Expectant mothers, PCs, and researchers in this pilot trial were not blinded to arm assignments.
PCs completed an intake form at enrollment that included questions regarding demographic factors, breastfeeding experience, breastfeeding goals, and cell phone use. Eligible participants were asked to respond to an introductory text to ensure that their cell phone number was active and to ensure that they were able to respond via text message. The primary outcomes of the study were (a) exclusive breastfeeding at 2 weeks post‐partum, defined as the intake of only breast milk in prior 48 hr—no solids, no water, and no other liquids; (b) contact between mothers and PC within 48 hr of delivery; and (c) met breastfeeding goals. The WIC breastfeeding PC programme defined exclusive breastfeeding as the intake of breast milk alone within the last 48 hr. As such, we aligned our outcome with their programme outcome. Breastfeeding status at 2 weeks post‐partum was chosen due to findings that show women often encounter barriers to breastfeeding following hospital discharge, even after successful initiation, that lead to early discontinuation of breastfeeding within the first 2 weeks post‐partum (Wagner, Chantry, Dewey, & Nommsen‐Rivers, 2013). A research assistant assessed primary outcomes by telephone survey at 2 weeks post‐partum. Breastfeeding status questions were also sent via text (to both the control and intervention groups), and when a mother could not be reached for a phone survey, the texting outcome was used. If there was a discrepancy between phone survey outcome or texting outcome, phone survey outcome was used. If neither the phone survey nor texting outcomes were available, then the 2‐week breastfeeding outcomes from the administrative records of the PC were used. Contact between mothers and PC within 48 hr of delivery was determined via PC contact logs that were routinely documented for all mothers as part of the PC programme. Feasibility outcomes included (a) how often mothers read the automatic text messages, (b) percent of mothers that initiated contact with the PC via text on their own, (c) participant satisfaction, (d) percent of mothers whose cell phone number changed during the intervention, and (e) identifying limitations of the texting platform. The texting platform allowed all texting communication to be stored. These records were then analysed to review the content of PC–mother contacts. Participants in the texting arm also completed an overall satisfaction survey at the end of the study administered by a research assistant over the phone.
We used Stata 12.1 (Stata Corp., College Station, TX, USA) for all quantitative analyses. We compared baseline sociodemographics and breastfeeding‐related factors between the control and intervention arms (using t‐test statistic for continuous variables and χ2 test for categorical variables) to demonstrate between‐group baseline equivalence. Breastfeeding status (exclusive or not) and contact between mothers and PCs were characterized as dichotomous outcomes at 2 weeks for all participants. Contact between the PC and mother within 48 hr of birth was also coded as a binary variable (yes/no). Using an intent‐to‐treat approach, we used χ2 testing to compare the effect of randomization arm on dichotomous outcomes at 2 weeks post‐partum.
We analysed the open‐ended survey questions thematically, following the Editing Analysis Style, which contains both deductive and inductive elements (Crabtree & Miller, 1999). Deductive codes were derived from analysis frameworks based on our literature review on breastfeeding obstacles faced by mothers with low incomes (Bunik et al., 2006; Hannon et al., 2000; Hurley et al., 2008; McCann et al., 2007; Zimmerman & Guttman, 2001). Inductive codes were derived from the survey responses to create new categories and refine framework categories. The principal investigator (N.H.) coded all open‐ended questions with a second coder coding a subset to verify code reliability. Coded survey responses allowed cross‐case comparison and analysis of patterns and themes.
3. RESULTS
Of the 73 women screened for eligibility, nine mothers did not meet inclusion criteria, two mothers did not want to enrol, and four mothers did not respond to the introductory text. Fifty‐eight mothers were enrolled, and 52 were available for intention‐to‐treat analysis (n = 30 texting, n = 22 control; Figure 1). Participants' mean age was 26 years (range 18–41 years); 75% were Hispanic, 17% African American, and 6% White. The two groups were similar in clinical and demographic characteristics (Table 2).
Figure 1.

Eligibility, randomization, and follow‐up
Table 2.
Characteristics of Lactation Advice thru Texting Can Help study participants
| Control (n = 22) | Texting group (n = 30) | ||
|---|---|---|---|
| Mean (range) | Mean (range) | P‐value | |
| Age (years) | 26.9 (18–41) | 26.4 (18–42) | .786 |
| N (%) | N (%) | ||
| Race | .619 | ||
| Black | 4 (18) | 5 (17) | |
| Hispanic | 16 (73) | 23 (77) | |
| Puerto Rican | 6 | 6 | |
| Non‐Puerto Rican | 10 | 17 | |
| White | 1 (5) | 2 (6) | |
| Other | 1 (5) | 0 (0) | |
| English‐speaking | 14 (63) | 16 (53) | .467 |
| Employment | .415 | ||
| Full‐time | 0 (0) | 2 (7) | |
| Part‐time | 6 (27) | 6 (20) | |
| Unemployed | 16 (73) | 22 (73) | |
| Gestational age at enrollment (weeks) | 28.4 | 29.7 | .64 |
| Gestational age at delivery (weeks) | 37.3 | 41 | .209 |
| Breastfed previously | 13 (59) | 14 (47) | .386 |
| Parity | |||
| Primiparous | 9 (41) | 13 (43) | .302 |
| 1 | 6 (27) | 13 (43) | |
| 2 | 4 (18) | 2 (7) | |
| ≥3 | 3 (14) | 2 (7) | |
| Unlimited texting plan | 22 (100) | 30 (100) | |
| Unlimited data plan | 22 (100) | 28 (93) | .217 |
| Number of times cell phone number change or phone was cut off during study period | .393 | ||
| 0 | 18 (82) | 27 (90) | |
| 1 | 4 (18) | 3 (10) |
The vast majority (92.4%) of the mothers completed the 2‐week post‐partum phone survey. Breastfeeding status for four moms (two controls and two interventions) who could not be reached via phone was determined via responses to evaluation texts or breastfeeding PC programme data as indicated above. There was a 97% concordance rate between breastfeeding status outcomes obtained via breastfeeding PC programme data and the 2‐week post‐partum phone survey.
3.1. Primary outcome measures: impact on infant feeding outcomes and early contact
Although the association did not achieve statistical significance, the exclusive breastfeeding prevalence at 2 weeks post‐partum among participants in the texting intervention was 50% compared with 31.8% in the control arm, p = .197, OR 2.14 (0.68–6.75). Contact between mothers and PCs within 48 hr of delivery was significantly higher in the texting group, 86.6% versus 27.3%, p = <.001, OR 13.3 (3.38–51.05), compared with the control. Mothers in the texting group reported that they were meeting their breastfeeding goals more frequently than mothers in the control arm, 96.1% versus 73.6%, p = .06, OR 8.93 (0.95–84.25). See Table 3.
Table 3.
Outcomes of LATCH texting intervention
| Outcome |
Control N (%)N (%) |
Intervention texting N (%) | OR [95% CI] | P‐value |
|---|---|---|---|---|
| Primary outcomes | ||||
| Exclusive breastfeedinga at 2 weeks post‐partum | 7 (31.8%) | 15 (50%) | 2.14 [0.68, 6.75] | P = .197 |
| Contact with peer counsellor within 48 hr of delivery | 6 (27.3%) | 25 (86.6%) | 13.3 [3.38, 51.05] | P < .001 |
| Met breastfeeding goals | 14 (73.6%) | 25 (96.1%) | 8.93 [0.95, 84.25] | P = .06 |
Note. LATCH = Lactation Advice thru Texting Can Help; OR = odds ratio; CI = confidence interval.
Defined as the intake of only breast milk in prior 48 hr—no solids, no water, and no other liquids.
3.2. Process evaluation
The majority of mothers (83%, n = 25) enrolled in the texting arm noted that they “always” or “very often” read LATCH texts prenatally; 80% (n = 24) always or very often read texts post‐partum. The majority of participants (90%, n = 27) in the texting arm texted an original comment or question during the study period. An original comment or question was defined as a text other than “ok” or “thanks” that raised a specific breastfeeding comment or concern. Many times these comments or questions were sent to the PC immediately after the automatic (auto) text for the day. As many as 77% (n = 23) of moms clicked on at least one web link sent via text during the study period. Five mothers (9.6%) did not have access to internet via their cell phones, and five mothers (9.6%) had their cell phone number changed or cut off at some point during the study period.
On review of text message conversations during an advisory committee meeting, an important issue was broached, related to when to elevate the level of care from a text message conversation to a phone call or an in‐person visit. “Crucial moments” to respond were readily identified as (a) any mention of “milk not flowing” or “no milk,” (b) any indication that feeds are “scheduled” versus “on‐demand,” (c) any supplementation with formula, (d) mother's belief that baby is not “getting enough milk” due to crying, and (e) any mention of nipple or breast pain. PCs were specifically encouraged to switch communication to a phone call in these instances and, if needed, schedule an in‐person visit. In addition, the PCs used the WIC breastfeeding PC programme (WIC Loving Support campaign) guidelines to guide when to refer the mom to a lactation consultant or paediatrician (United States Department of Agriculture Food and Nutrition Services, 2011).
Several limitations of the texting platform were also noted when text message transcripts, brought forth by the PCs and IBCLCS, were reviewed by the advisory committee. Some of the auto‐text messages were sent at moments that were not ideally timed based on mom's interaction with the texting platform. For example, one mother was responding to a text asking “how is breastfeeding going?” She responded with: “It is going great. I need some tips on relieving engorgement if possible.” Before the PC had a chance to respond, another auto‐text came in stating: “Remember to place your baby skin‐to‐skin (baby naked) on your chest for an hour. This will allow baby to get to know you and latch on to the breast better.” This suboptimal timing of texts happened most frequently over weekends or after hours when the PCs were not working. In the majority of cases, the texting conversation would pick up seamlessly once the PC responded to the initial concern. In this case, the mom had sent the initial text about engorgement at 7:12 p.m. The next morning at 9:16 a.m., the PC responded, “Good morning! Are your breasts feeling full? Check out these sites for tips about relieving engorgement: (web site url).”
Switching the mother from the prenatal campaign to the post‐partum campaign did depend on the mother either texting in a specific “opt‐in” word (e.g., “baby born”) or the PC manually switching the mother to the post‐partum campaign once she was aware of the baby's birth. On one occasion, there was a delay (>72 hr) to switching the mother over to the post‐partum campaign because she did not use an opt‐in word and the baby was born over the weekend. In this instance, the PC manually switched the mother to the post‐partum campaign the week following. All other mothers in the texting arm were switched over to the post‐partum texts within 12 hr of delivery.
3.3. Participant satisfaction
All mothers enrolled in the texting arm who completed the satisfaction survey (91%, n = 27) stated that they would recommend this texting programme to a friend. Themes that emerged through analysis of the open‐ended satisfaction survey questions included how the texting programme (a) helped to improve breastfeeding knowledge, (b) helped to prepare moms for breastfeeding, (c) provided additional needed support, (d) created ease of communication via texting, and (e) became a modality for mothers to readily ask for advice or support at any time. In addition, text messages were particularly useful for primiparous women or mothers who had not breastfed their previous children (see Table 4). Despite PCs only responding to text messages at 8 a.m.–5 p.m. Monday–Friday, all mothers noted that they were able to reach the PC when needed. Only one mother noted that “there was a time when she needed help but did not get it.” In response to this question, this mother specifically noted her desire for the PC to make a home visit that was not part of that clinic's WIC breastfeeding PC programme. The one suggestion offered to improve the texting programme was to include more pictures and video links.
Table 4.
Mothers' perceptions of Lactation Advice thru Texting Can Help programme
| Helps to improve breastfeeding knowledge |
| • “The random texts had good information. Sometimes you want to ask a question and they've already sent you the answer without having to ask.” |
| • “Even though I have two other kids, I still learned so much from the program. There is so much I didn't know.” |
| • “I was getting the information that I needed about breastfeeding for the first time.” |
| • “Many people don't have knowledge or experience breastfeeding and this texting program really helps.” |
| • “Beginning moms don't know much about breastfeeding and this program was really helpful.” |
| • “Good program for women. Helps them feel comfortable and less in the dark about breastfeeding.” |
| • “There are things, depending on what country you're from, that people believe about breastfeeding that aren't true. This program really clarified things for me.” |
| • “It let me know a lot about breastfeeding. There were so many different topics. It was a lot of good information that they gave.” |
| • “I liked that she would send me images and good advice through text.” |
| • “I liked the information that I got when I got home from the hospital.” |
| Helps to prepare mothers for breastfeeding |
| • “It really helps prepare you for breastfeeding. It really helped me a lot.” |
| • “They told me how to prepare for breastfeeding.” |
| • “Everything helped. How to know different things and what to look for in feeding the baby. It was very helpful.” |
| Provides additional support and help |
| • “It's very helpful especially for me because I didn't breast feed my first child. At first I was unsure because it's difficult, but this program really gave me the support and help I needed.” |
| • “I liked everything, because with my first baby I gave up and wasn't happy about it. With this one I'm very happy with their help. I learned a lot.” |
| • “I already recommended it to my brother's girlfriend who is pregnant with her first child. I recommended both WIC and the texting program because they have been so helpful to me. This is my first child and I really didn't have anyone to ask or turn to, so his program has really helped me so much.” |
| • “As a new mom, it can be tough. With help, the peer counselor helps you get used to the new schedule. I felt the program was excellent with the texting.” |
| • “Because it helps a lot and sometimes moms give up, but this program really helps.” |
| • “Honestly, it helped me the whole time. With every aspect.” |
| • “I like the way they support us and give us advice, and if I didn't understand the text they would send me the video.” |
| • “I like the questions and the way they check the status of the baby.” |
| Ease and convenience of communication via text |
| • “It helped me a lot and just having someone to text with is amazing. Breastfeeding can be very stressful.” |
| • “Convenient for mothers on the go.” |
| • “I liked that you could text anytime. It made it a lot easier.” |
| • “The convenience. I didn't have to leave the house. The information was right there.” |
| • “I liked the convenience and it was very informative.” |
| • “I liked all the tips she sent through text.” |
| Texting allowed mothers to ask for help or advice at any time of the day or night (Although peer counselors would respond only during business hours, there was a perception that support was available 24/7 for some mothers.): |
| • “It's 24 hour help when you need it. That's great for a new mom.” |
| • “I liked being able to ask a question and get an answer or explanation when I needed it.” |
| • “I liked being able to ask a question anytime and actually get a response.” |
| • “She was there 24/7 if I needed her and answered my questions right away when I texted her.” |
| • “I like that when I had a question I had a quick response, and the texts that give advice about asking the nurses for help in the hospital were great.” |
| Areas for improvement: |
| • “Fewer texts especially in the morning.” |
| • “Maybe more pictures and videos. Especially those that are like tutorials.” |
| • “Having someone available to answer during the night and not have to wait until morning to get a response.” |
| • “Having more information on different things instead of repeating info.” |
4. DISCUSSION
Breastfeeding is a learned skill, and it can be challenging for many mothers who intend to breastfeed their infants (Burns, Schmied, Sheehan, & Fenwick, 2010; Williamson, Leeming, Lyttle, & Johnson, 2012). Many unanticipated breastfeeding concerns arise within the first 2 weeks post‐partum, which are associated with the cessation of breastfeeding (Brand et al., 2011).
This pilot demonstrated that the LATCH intervention helped mothers reach their breastfeeding PCs within 48 hr of delivery. Mothers eager to breastfeed their infants are often reliant on health workers for advice regarding breastfeeding. The support from health care workers may not always be readily available, especially within the first 2 weeks post‐partum. This immediate post‐partum support is critical and can help prevent many breastfeeding complications (Koskinen, Aho, Hannula, & Kaunonen, 2014; Patel & Patel, 2015).
Findings suggest that the text messaging intervention may improve breastfeeding rates among mothers enrolled in WIC who receive PC. Although this pilot was underpowered, a higher percentage of mothers in the texting intervention (50%) were exclusively breastfeeding at 2 weeks post‐partum compared to mothers in the control arm (17%, p = .197). Mothers found the texting intervention helpful and were more likely to report that they had met their breastfeeding goals. All mothers who received the intervention noted that they would recommend this intervention to a friend. Texting was noted to be informative and “convenient for mothers on the go.” Although PCs only responded to texts during business hours, mothers noted that they felt supported and that they appreciated the ability to text a question “at any time.”
Other studies have also found that text‐based messaging helps improve breastfeeding rates (Gallegos et al., 2014). The unique aspect of this pilot is that the two‐way text messaging platform allowed for the mother to text back specific concerns or questions that may have been raised by the automatic text messaging schedule. The PC then had the ability to respond directly to specific concerns that the mother raises, adding video links as needed.
The timing of the automatic texting schedule allowed for important breastfeeding issues to be raised automatically with mothers at key moments prenatally and post‐partum. Past studies have noted that the lack of preparation for what to expect during the early post‐partum period led mothers to request formula while in the hospital (DaMota et al., 2012). In these past studies, the decision to formula feed fell into the following categories: (a) lack of preparation for the process of breastfeeding, (b) inadequate preparation for newborn care (the need for rest and unrealistic expectations about infant behaviour), and (c) formula as a solution to breastfeeding problems. The automatic texting schedule specifically addressed these concerns. The automatic texts were also personalized using the mother's first name and signed by the PC. These personalized, interactive text messages were successful in eliciting text message conversations between the PC and mother.
Eighty percent of the study participants are considered “millennials” or part of Generation Y that includes individuals born from the early 1980s to the early 2000s. Texting has been shown to play a critical role in communications within this generation (Seppanen, 2012; Thurman, 2013).
Our findings support that text messaging can be used effectively to engage members of this generation. Furthermore, consistent text messaging also helped to foster the perception of constant support and the ability for mothers to reach out for help and advice readily.
This web‐based platform (which recorded all text messages) also allowed IBCLCs to supervise text message conversations exchanged between PC and mother. This level of supervision is often not possible when texts are exchanged phone‐to‐phone alone. Access to these text conversations allowed lactation consultants to engage in multiple case‐based teaching moments to review breastfeeding concepts with the breastfeeding PCs. There were also instances when lactation consultants were made aware of gaps in PC knowledge, and these cases helped to initiate more training on specific topics. Lastly, the web‐based platform allowed lactation consultants to respond to mothers' texts when the PCs were off duty or out of town.
Consideration for modifications to be made in future studies include (a) implementing weekend coverage so that texts sent by mothers over the weekend could be responded to more readily, (b) developing an algorithm of when to switch the text message conversation to a phone call or an in‐person visit, (c) incorporating more educational pictures and videos, (d) expanding the texting curriculum and texting support to 3 months post‐partum, and (e) using the World Health Organization's definition of exclusive breastfeeding that notes the “intake of only breast milk (no other food or water)” within the prior 24 hr.
4.1. Limitations
It is important to note that this was a pilot study that was designed to inform feasibility and identify modification needed in the design of a larger, hypothesis testing study. This study was limited to one city with a relatively small population (100,000k), and participants had to be either English or Spanish speaking. Although this study suggests improved exclusive breastfeeding rates related to texting intervention, the study was underpowered to detect statistical significance. In addition, the research assistant who conducted the follow‐up interviews was not blinded to group allocation because she was collecting feasibility data regarding the texting intervention itself. Future LATCH studies should consider blinding the interviewers to group allocation.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
NH, RP‐E, and MR conceived and designed the study. NR, VB, LG, TJ, CO, and MG acquired the data. NH and RP‐E analysed and/or interpreted the data. NH drafted the manuscript. RP‐E, MR, and MG critically revised the manuscript for important intellectual content.
ACKNOWLEDGMENTS
The authors would like to thank the WIC breastfeeding PCs (Digna Lemus, Diana Bone, and Lucille Lester) for their efforts and contributions in the design and implementation of this intervention. In addition, the authors would like to thank Marilyn Lonczak and Caroline Cooke from the Connecticut WIC Program for their continuous support and active participation throughout the study.
APPENDIX A.
A.1.
APPENDIX B.
B.1.
Harari N, Rosenthal MS, Bozzi V, et al. Feasibility and acceptability of a text message intervention used as an adjunct tool by WIC breastfeeding peer counsellors: The LATCH pilot. Matern Child Nutr. 2018;14:e12488 10.1111/mcn.12488
REFERENCES
- Ajzen, I. (1991). The theory of planned behavior. Organizational Behavio and Human Decision., 50, 179–211. [Google Scholar]
- Brand, E. , Kothari, C. , & Stark, M. A. (2011). Factors related to breastfeeding discontinuation between hospital discharge and 2 weeks postpartum. The Journal of Perinatal Education, 20(1), 36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunik, M. , Clark, L. , Zimmer, L. M. , Jimenez, L. M. , O'Connor, M. E. , Crane, L. A. , & Kempe, A. (2006). Early infant feeding decisions in low‐income Latinas. Breastfeeding Medicine, 1(4), 225–235. [DOI] [PubMed] [Google Scholar]
- Burns, E. , Schmied, V. , Sheehan, A. , & Fenwick, J. (2010). A meta‐ethnographic synthesis of women's experience of breastfeeding. Maternal Child Nutrition, 6(3), 201–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control . (2014). Division of Nutrition, Physical Activity and Obesity. Breastfeeding Report Card. Retrieved from: http://www.cdc.gov/breastfeeding/pdf/2014breastfeedingreportcard.pdf
- Chapman, D. J. , Morel, K. , Anderson, A. K. , Damio, G. , & Pérez‐Escamilla, R. (2010). Breastfeeding peer counseling: From efficacy through scale‐up. Journal of Human Lactation, 26(3), 314–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cormick, G. , Kim, N. A. , Rodgers, A. , Gibbons, L. , Buekens, P. M. , Belizán, J. M. , & Althabe, F. (2012). Interest of pregnant women in the use of SMS (short message service) text messages for the improvement of perinatal and postnatal care. Reproductive Health, 9, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crabtree, B. , & Miller, W. (1999). Doing qualitative research (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- DaMota, K. , Bañuelos, J. , Goldbronn, J. , Vera‐Beccera, L. E. , & Heinig, M. J. (2012). Maternal request for in‐hospital supplementation of healthy breastfed infants among low‐income women. Journal of Human Lactation., 28(4), 476–482. [DOI] [PubMed] [Google Scholar]
- Gallegos, D. , Russell‐Bennett, R. , Previte, J. , & Parkinson, J. (2014). Can a text message a week improve breastfeeding? BMC PregnancyChildbirth, 14(1), 374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannon, P. R. , Willis, S. K. , Bishop‐Townsend, V. , Martinez, I. M. , & Scrimshaw, S. C. (2000). African‐American and Latina adolescent mothers' infant feeding decisions and breastfeeding practices: A qualitative study. Journal of Adolescent Health, 26(6), 399–407. [DOI] [PubMed] [Google Scholar]
- Hurley, K. M. , Black, M. M. , Papas, M. A. , & Quigg, A. M. (2008). Variation in breastfeeding behaviours, perceptions, and experiences by race/ethnicity among a low‐income statewide sample of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) participants in the United States. Maternal Child Nutrition, 4(2), 95–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang, H. , Li, M. , Wen, L. M. , Hu, Q. , Yang, D. , He, G. , … Qian, X. (2014). Effect of short message service on infant feeding practice: Findings from a community‐based study in Shanghai, China. JAMA Pediatrics., 168(5), 471–478. [DOI] [PubMed] [Google Scholar]
- Johnston, M. , Landers, S. , Noble, L. , Szucs, K. , & Viehmann, L. (2012). Breastfeeding and the use of human milk. Pediatrics, 129(3), e827–e841. [DOI] [PubMed] [Google Scholar]
- Koskinen, K. S. , Aho, A. L. , Hannula, L. , & Kaunonen, M. (2014). Maternity hospital practices and breast feeding self‐efficacy in Finnish primiparous and multiparous women during the immediate postpartum period. Midwifery, 30(4), 464–470. [DOI] [PubMed] [Google Scholar]
- Kruger, R. A. , & Casey, M. A. (2000). Focus groups: A practical guide for applied research (3rd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- McCann, M. F. , Baydar, N. , & Williams, R. L. (2007). Breastfeeding attitudes and reported problems in a national sample of WIC participants. Journal of Human Lactation., 23(4), 314–324. [DOI] [PubMed] [Google Scholar]
- Miles, M. B. , & Huberman, A. M. (1994). Qualitative data analysis: An expanded sourcebook (2nd ed.). Thousand Oaks: Sage Publications. [Google Scholar]
- Patel, S. , & Patel, S. (2015). The effectiveness of lactation consultants and lactation counselors on breastfeeding outcomes. Journal of Human Lactation, 32(3), 530–541. [DOI] [PubMed] [Google Scholar]
- Patton, M. (2002). Qualitative research and evaluation methods. Thousand Oaks, CA: Sage. [Google Scholar]
- Pérez‐Escamilla, R. (2012). Breastfeeding social marketing: Lessons learned from USDA's “Loving Support” campaign. Breastfeeding Medicine, 7(5), 358–363. [DOI] [PubMed] [Google Scholar]
- Perrin, M. (2012). Supporting breastfeeding with new technologies. Lactation Matters, the ILCA blog. http://lactationmatters.org/2012/01/31/supporting-breastfeeding-with-new-technologies/
- Ryan, A. S. , & Zhou, W. (2006). Lower breastfeeding rates persist among the Special Supplemental Nutrition Program for Women, Infants, and Children participants, 1978–2003. Pediatrics, 117(4), 1136–1146. [DOI] [PubMed] [Google Scholar]
- Seppanen, S. (2012). The millennial generation research review . U.S. Chamber of Commerce Foundation Retrieved from https://www.uschamberfoundation.org/sites/default/files/article/foundation/MillennialGeneration.pdf
- Thurman, S . (2013). NSHSS Scholar 2013 Millennial Career Survey Results. The emerging workforce: Generational trends . Retrieved from https://www.nshss.org/media/1583/nshss-career-survey-2013.pdf
- United States Department of Agriculture Food and Nutrition Services . (2011). Loving Support© peer counseling curriculum. https://lovingsupport.fns.usda.gov/content/downloads
- Wagner, E. A. , Chantry, C. J. , Dewey, K. G. , & Nommsen‐Rivers, L. A. (2013). Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics, 132(4), e865–e875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitacre, P. T. , & Moats, S. (2011). Updating the USDA National Breastfeeding Campaign: Workshop summary. IOM (Institute of Medicine). Washington, DC: The National Academies Press. [Google Scholar]
- Williamson, I. , Leeming, D. , Lyttle, S. , & Johnson, S. (2012). ‘It should be the most natural thing in the world’: Exploring first‐time mothers' breastfeeding difficulties in the UK using audio‐diaries and interviews. Maternal Child Nutrition, 8(4), 434–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman, D. R. , & Guttman, N. (2001). “Breast is best”: Knowledge among low‐income mothers is not enough. Journal of Human Lactation, 17(1), 14–19. [DOI] [PubMed] [Google Scholar]


