Abstract
Micronutrient powder (MNP) interventions are often integrated within infant and young child feeding (IYCF) programmes to improve micronutrient intake from complementary foods. This review aims to describe country experiences with MNP interventions and their impact on IYCF practices and develop a framework for how MNP may strengthen complementary feeding practices. A literature review and key informant interviews were used to gather data on complementary feeding practices in MNP programme design, implementation, and evaluation. Findings from 11 MNP programmes in different geographic regions reinforced the potential of MNP interventions to add renewed focus and resources to existing IYCF programmes. MNP plays an important role in ensuring adequate micronutrient intake and reducing anaemia in young children. In some programmes, MNP users had improved IYCF practices, such as breastfeeding to 24 months and children receiving complementary foods with adequate consistency, frequency, and diversity. Our framework highlights how behaviour change communication is an essential component for influencing household actions, not only to generate demand and promote correct and sustained MNP use but also raise awareness of IYCF practices. The actions at MNP policy, delivery, and behaviour change communication levels collectively influence household IYCF practices, and formative research and monitoring and evaluation serve to inform programme design and optimize impact. In conclusion, a limited but growing body of evidence suggests that MNP interventions can contribute to improve complementary feeding practices. However, there is scope for improvement even among integrated MNP and IYCF programmes in order to realize the full potential of MNP interventions for IYCF practices.
Keywords: behaviour change communication, complementary feeding, conceptual framework, infant and young child feeding, micronutrient powder
1. INTRODUCTION
The complementary feeding period, generally from 6 to 24 months of age when solid, semisolid, and soft foods are provided in addition to breastfeeding, is a critical phase of child growth and development. Nearly 100,000 child deaths could be averted if complementary feeding interventions, such as nutrition education and provision of additional complementary foods in food insecure populations, were scaled up to 90% coverage (Bhutta et al., 2013). Dietary diversity and consumption of animal‐source foods are associated with reduced stunting in children 6 to 23 months of age (Krasevec, An, Kumapley, Bégin, & Frongillo, 2017), and consumption of a minimum acceptable diet (MAD) with dietary diversity reduces the risk of both stunting and underweight (Marriott, White, Hadden, Davies, & Wallingford, 2012). However, many young children in resource‐poor countries still do not receive optimal complementary feeding practices: only one in six children are fed the MAD, and one in four are given minimum dietary diversity (MDD; White, Bégin, Kumapley, Murray, & Krasevec, 2017). Even when use of locally available foods is optimized, iron and zinc needs are still not met for young children, and other cost‐effective strategies to ensure adequate intake of these nutrients are needed (Osendarp et al., 2016).
There is growing evidence demonstrating the feasibility and effectiveness of complementary feeding interventions and their role in reducing undernutrition in the first 1,000 days of life. Results from efficacy and effectiveness trials and programme evaluations have demonstrated the positive impacts of combined community‐based, mass media, and advocacy approaches in improving breastfeeding and complementary feeding practices (Fabrizio, van Liere, & Pelto, 2014; Lamstein et al., 2014). Despite the gains in the science, few countries are implementing comprehensive, large‐scale complementary feeding programmes, whether nested within broader infant and young child feeding (IYCF) programmes or integrated into other programmes or sectors.
Micronutrient powder (MNP) sachets contain a dry powder with micronutrients that can be added to any semisolid or solid food and were first developed as an alternative to iron syrup for treating nutritional anaemia in young children (Zlotkin et al., 2005). On the basis of a recent review of trial evidence, (De‐Regil, Suchdev, Vist, Walleser, & Pena‐Rosas, 2011), the World Health Organization (WHO, 2016) recommends home fortification of foods with MNP among infants and children 6–23 months of age to reduce iron deficiency and anaemia in young children. Programming guidance for MNP interventions has been provided by the Home Fortification Technical Advisory Group (HF‐TAG, 2011). MNP interventions are currently implemented at national, subnational, or pilot level in at least 50 countries globally (UNICEF, 2015).
In controlled settings, the effect of standard MNP formulations on child growth has been minimal (De‐Regil et al., 2011; Salam, MacPhail, Das, & Bhutta, 2013), except for a recent trial in Bangladesh using an expanded micronutrient formulation among full‐term, low birthweight infants that demonstrated a reduction in stunting at 12 months (Shafique et al., 2016). To effectively improve child growth, and although the optimal MNP composition is being researched, there is a need to concurrently address other complementary feeding and care practices along with promoting MNP use. MNP interventions are often integrated within broader IYCF programmes with the goal of improving micronutrient intake from complementary foods among children 6 months of age and older (HF‐TAG, 2011). The Nutridash 2014 Global Report showed that 74% of MNP interventions were linked with IYCF programmes (UNICEF, 2015).
The purpose of this paper is to review country experiences on how existing MNP interventions impact IYCF practices and to develop a framework on how MNP interventions could strengthen IYCF practices and complementary feeding in particular. The focus of the review is on nonhumanitarian contexts, although reference may be made to unique situations where a modified approach is needed.
Key messages.
Countries scaling up MNP interventions to address micronutrient deficiencies in young children should consider carefully how to integrate this within broader programs that intentionally and simultaneously address other IYCF practices.
MNP delivery through routine health services, community‐based outreach, market‐based models, and other platforms has the potential to increase awareness of important IYCF practices in a broad sense and increase frequency of contact between caregivers and providers of IYCF counselling and support.
The proposed framework highlights how actions at MNP intervention policy, delivery, and BCC levels could collectively influence household IYCF practices; however, program evidence of improved complementary feeding practices among MNP users was limited.
There is a need to develop practical tools for community‐based monitoring of complementary feeding practices and strengthen evaluation of core IYCF indicators by MNP programs.
2. METHODS
A review of existing MNP interventions was conducted with a focus on those that were integrated with IYCF programmes and have documented formative research and/or programme evaluation results. Thirty‐one MNP interventions integrated with infant and young child nutrition programmes in 25 countries were identified in the United Nations Children's Fund (UNICEF) NutriDash 2013 database. Information was requested from UNICEF, government, and implementing partners through a convenience sample of 13 countries that were thought to represent programmes with regional diversity, public/private distribution systems, national scale of implementation, and mature and initial phases. Information was obtained from 11 countries. For each MNP country programme, formative research reports, training and behaviour change communication (BCC) materials, evaluation reports, and peer‐reviewed publications were reviewed. Data were collected on the type of MNP intervention, evidence of integration of IYCF in the MNP intervention (considering integration at policy, training, and monitoring/evaluation levels), how the MNP delivery channel facilitated access to IYCF counselling, whether recommended IYCF practices were included in MNP training and BCC materials, and any documented evidence of improved complementary feeding practices (i.e., timely introduction of complementary foods, continued breastfeeding, appropriate foods, and feeding frequency) among MNP users. To complement the programme data collected, key informant interviews were conducted with technical advisors and MNP programme managers.
On the basis of MNP programme experiences, a theoretical framework was designed to illustrate the potential mechanisms through which MNP interventions could influence and strengthen complementary feeding practices at the household level.
3. OVERVIEW OF COUNTRY PROGRAMMES
Information was gathered from countries with MNP interventions delivered at scale and in the process of scale‐up. Table 1 summarizes the key characteristics of these programmes. No programmes from Latin America region were included due to lack of information available at the time of the review.
Table 1.
Overview of country MNP program characteristics included in the review
| Country | Type of programme (local MNP brand) | Organization(s) involved | Distribution mechanism | Target group and MNP regimen |
|---|---|---|---|---|
| Established programmes | ||||
| Bangladesh | MNP + MCHN (Pushtikona, MoniMix) | BRAC, GAIN, Renata, SMC | Community‐based sales of MNP | 6–23 months; on demand |
| Kyrgyz Republic | MNP + MIYCN + ECD (Gulazik) | MOH, UNICEF, CDC | Health services with follow‐up by community‐based volunteers | 6–23 months; 30 sachets every 2 months |
| Mongolia | MNP + IYCF | MOH, ADB | Health service delivery (free) | 6–35 months; 60 sachets every 6 months (use within 2–3 months) |
| Nepal | MNP + IYCF pilot programme (Baal Vita) | UNICEF, MOH | Health facility, community‐based and other urban distribution (all free) | 6–23 months; 60 sachets every 6 months (use daily for 2 months) |
| Philippines | MNP + IYCF + IFA | MOH, UNICEF, EU, HKI (ELNI/MYCNSIA) | Health service delivery, community‐based delivery, CCT (all free) | 6–23 months; 10 sachets per month |
| Early stage programmes | ||||
| Cambodia | MNP scale‐up (2012–15) | MOH, UNICEF, HKI, WVI | Health services & community‐based (free) | 6–23 months; 15 sachets/month for 18 months |
| Lao PDR | MNP + IYCF + WASH (SuperKid) | MOH, UNICEF, UBC | TBD | TBD |
| Cameroon | MNP + IYCF | MOH, UNICEF, UBC | TBD | TBD |
| Madagascar | MNP + IYCF (Zazatomady) | PSI, UNICEF, MOH | Urban: market‐based through private clinics; rural: community‐based | 6–23 months; 90 sachets every 6 months (1 per day) |
| Nigeria | MNP + IYCF | UNICEF, MOH | TBD | TBD |
| MNP + MNCH | Gain, MOH | Health service delivery during MNCH Weeks (free) | 6–59 months; 30 or 60 sachets per distributiona | |
| Rwanda | MNP + IYCF | MOH, UNICEF | Community‐based GMP sessions | 6–23 months; 30 sachets every 3 months |
Note. ADB = Asian Development Bank; BRAC = Building Resources Across Communities; CCT = conditional cash transfer; CDC = Centres for Disease Control; ECD = early childhood development; ELNI = Enhanced Local Nutrition Interventions; EU = European Union; GAIN = Global Alliance for Improved Nutrition; GMP = growth monitoring and promotion; HKI = Helen Keller International; IFA = iron and folic acid; IYCF = infant and young child feeding; MCHN = maternal and child health and nutrition; MIYCN = maternal, infant, and young child nutrition; MNCH = maternal, newborn, and child health; MNP = micronutrient powder; MOH = Ministry of Health; MYCNSIA = Maternal and Young Child Nutrition Security Initiative in Asia; PSI = Population Services International; SMC = social marketing company; TBD = to be determined; UBC = University of British Columbia; UNICEF = United Nations Children's Fund; WASH = water, sanitation, and hygiene; WVI = World Vision International.
Protocol was for 60 sachets per child but was reduced to 30 sachets (and priority given to children 6–23 months) during the December 2013 distribution due to inadequate supplies; 60 sachets per child were given during the March 2014 distribution (Korenromp et al., 2016).
Bangladesh, Kyrgyz Republic, Mongolia, Nepal, and Philippines have integrated MNP interventions within IYCF programmes that are operating at scale and have been evaluated for coverage and effectiveness. In Bangladesh, MNP are sold through a variety of channels including the community‐based networks of Building Resources Across Communities' female community health volunteers (CHV; Shasthya Shebikas), pharmaceutical outlets, and the Social Marketing Company. Scale‐up of MNP in Kyrgyz Republic followed a pilot study (Lundeen et al., 2010) and scale‐up in one province (Serdula et al., 2013); now, MNP are distributed free nationally through the primary health care system to children 6–23 months as an integral component of the maternal, infant, and young child nutrition programme (MOH Kyrgyz Republic, UNICEF and CDC, 2015). In Mongolia, MNP are integrated in maternal and IYCF programmes delivered through primary health care facilities, and recent projects have sought to improve nutrition service quality and coverage and IYCF counselling by health workers (Batjargal et al., 2013). In Nepal, MNP were integrated within IYCF programmes in six districts in 2011 and delivered through female CHV or health facilities in rural areas, and ward offices or health facilities in urban areas (Mirkovic et al., 2016). In the Philippines, a national policy on MNP intervention for children 6–23 months was developed in 2011 and implementation occurs through health stations and service providers that are part of the national health system.
Madagascar, Nigeria, Rwanda, Cameroon, Lao PDR, and Cambodia have completed preparatory phases of formative research and pilot studies of MNP programme implementation and are now in the process of scaling up MNP distribution. In Madagascar, an 18‐month social marketing pilot project (Fortidom) in 2013 tested MNP delivery through sales by private clinic franchises in urban areas and distribution by CHV in rural areas. In Nigeria, home fortification with MNP is being piloted through different delivery mechanisms as well. Benue State first tested free MNP distribution for children 6–59 months during Maternal Newborn and Child Health Weeks in 2013 and 2014 (Korenromp et al., 2016). In Kebbi and Adamawa States, formative research is guiding the design of an integrated IYCF and MNP intervention targeting children 6–23 months (UNICEF Nigeria, 2015). In Rwanda, MNP distribution is now integrated in the Community‐Based Nutrition Protocol as part of monthly community growth monitoring sessions given by community health workers (CHW), following a 1‐year pilot evaluation in six districts (McLean, Michaux & Smith, 2013). The programme has since been scaled up rapidly. Recent formative research has guided the design of an integrated IYCF and MNP programme in Cameroon, with MNP distribution through public health facilities expected to strengthen IYCF counselling and support provided by health workers and CHW. The Lao PDR National Nutrition Policy includes MNP to address anaemia and other micronutrient deficiencies as part of a child nutrition intervention package with IYCF and water, sanitation, and hygiene. Cambodia is working with UNICEF and other non‐governmental organization (NGO) partners to scale up MNP delivery and IYCF counselling and support by village health volunteers to children 6–23 months in 14 provinces, a strategy that achieved higher coverage and compliance compared to delivery through health centres (Kingdom of Cambodia, 2014).
4. FRAMEWORK ON HOW MNP MAY CONTRIBUTE TO IMPROVE CHILD FEEDING PRACTICES
MNP intervention's contribution to improve child feeding practices has not been systematically explored to date. Integration of MNP with IYCF may mutually benefit both programmes, although there is little programmatic evidence of this (Mirkovic et al., 2016). As shown in the framework (Figure 1), the potential for MNP to influence complementary feeding practices is based on multiple programme components, including policy actions, delivery actions, and behaviour change interventions, that work in collective ways to influence household actions with respect to child care and feeding practices. The following sections describe the potential contribution that MNP interventions can make at each level within the framework and provide examples from country programme experiences. A summary of the proposed mechanisms is shown in Table 2.
Figure 1.
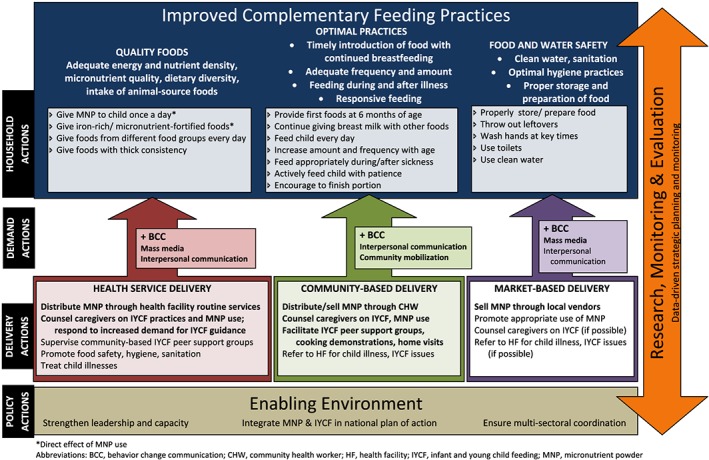
Theoretical framework describing how MNP and IYCF programmes can be integrated to improve complementary feeding practices
Table 2.
Summary of proposed mechanisms for MNP interventions to improve complementary feeding practices
| MNP programme component | Result/outcome |
|---|---|
| Policy and strategy development |
Assessment of nutrition situation and IYCF issues by stakeholders ↑ availability of MNP in the country |
| Formative research |
↑ awareness of context‐specific child feeding knowledge, attitudes and practices Improved design of BCC strategies and messages |
| Training MNP providers |
↑ provider knowledge of context‐specific child feeding issues ↑ access to well‐tested BCC materials, including job aids |
| Community mobilization and orientation to MNP | ↑ awareness among families and community leaders about recommended IYCF practices |
| Health facility delivery of MNP |
↑ access to IYCF counselling (more frequent interaction) ↑ quality of IYCF counselling by health workers ↑ demand for IYCF guidance and support among MNP users |
| Community‐based delivery of MNP |
↑ access to IYCF counselling and support (more frequent interaction, follow‐up) ↑ individualized IYCF counselling from CHWs ↑ demand for IYCF guidance and support among MNP users ↑ hands‐on learning opportunities for caregivers ↑ peer support for recommended IYCF practices |
| Market‐based delivery of MNP | ↑ knowledge among MNP providers/vendors of recommended IYCF practices |
| Monitoring and evaluation |
↑ routine data collection for key IYCF indicators ↑ evidence on effective strategies to improve IYCF |
Note. BCC = behavior change communication; CHW = community health workers; IYCF = infant and young child feeding; MNP = micronutrient powder.
4.1. Enabling environment
The introduction of MNP intervention can provide opportunities to create or strengthen an enabling policy environment for improving complementary feeding practices. Although MNP interventions are primarily used to address the problem of anaemia and micronutrient deficiencies in young children, the very basis for their introduction is usually rooted in a situational analysis of the nutritional status of young children and local IYCF practices. Engaging with multiple stakeholders in government, UN agencies, the private sector, and NGOs in discussions about national and subnational data on the problems of child undernutrition, micronutrient deficiencies, and their contributing factors raises the profile of IYCF practices as a critical component to be addressed. Multistakeholder collaboration can then also be sought in support of national scale‐up and rollout of a home fortification strategy. An example of this is Uganda where the Ministry of Health is supported by Centres for Disease Control and Prevention, SPRING, UNICEF, and World Food Programme to reach national scale of their home fortification programme in a harmonized way.
The potential for MNP interventions to improve complementary feeding practices also may depend on how MNP are registered as a product (e.g., pharmaceutical, food, or nutrition supplement) and the wording of associated legislation to control unethical marketing.
4.2. MNP delivery
The delivery of MNP interventions can also contribute to improve complementary feeding practices through the training provided and increased access to IYCF counselling. MNP training educates providers, users, and their families about the importance of nutrition for child health and optimal feeding practices (HF‐TAG, 2015). Potential improvements to the supply side of IYCF counselling include training MNP providers on context‐specific child feeding issues to be addressed and providing well‐tested, effective BCC materials to support interpersonal counselling efforts (Avula, Frongillo, Arabi, Sharma, & Schultink, 2011). Training packages for health workers and CHVs in Lao PDR and Kyrgyz Republic cover the full range of IYCF topics as well as MNP use. Improved primary health care workers' knowledge about IYCF was observed in Mongolia's evaluation of an MNP programme (Batjargal et al., 2013). MNP delivery may also increase caregiver access to IYCF counselling, as found in Madagascar's pilot project (PSI Research Division, 2014), but this can depend on the delivery mechanism chosen and level of integration with IYCF. Providing MNP can increase caregiver participation in IYCF information sessions (HF‐TAG, 2011), and caregivers may request support for IYCF as they try to use MNP. In India, adding MNP to a young child feeding programme “incentivized caregiver participation and facilitated delivery of program messages” (Avula et al., 2011, p.683).
Delivery of MNP through local health facilities helps motivate caregivers to go on a more frequent basis where they can access IYCF counselling and support. More regular contact with health services is important for complementary feeding practices (Issaka et al., 2015a; Issaka et al., 2015b), because children over 6 months of age often are not brought to clinics unless they are sick. If health care providers are adequately trained in IYCF counselling and support, this MNP delivery mechanism may be considered optimal in terms of providing a credible and trusted source of information for caregivers. Mothers in Niger (Tripp et al., 2011) and Lao PDR (Michaux et al., 2014) preferred MNP delivery through health centres as a trusted source of products and information. However, achieving high coverage through this mechanism depends on the context. In Kyrgyz Republic, primary health care service access is very high and reaches most caregivers of children 6–23 months. In Nepal, MNP coverage was higher in the CHV model, which was more accessible than the health facility model (Jefferds et al., 2015). In Cambodia, MNP coverage through health facilities was lower than the community‐based approach, and some caregivers perceived MNP as a medicine because it was being distributed by health centres, contributing to low compliance (Noij, 2013). Reaching healthy children was also challenging in Mongolia, where MNP was given primarily to children who regularly visited health facilities and were more likely to be weak, malnourished, and prone to illness (Batjargal et al., 2013).
A community‐based delivery mechanism makes both MNP and IYCF counselling and support more accessible to caregivers, especially in rural areas. However, community‐based MNP providers must be trained to promote and support optimal IYCF practices along with appropriate MNP use. Group sessions and home visits ensure more frequent contact with caregivers and opportunities to address issues with MNP use and other child feeding practices. For example, CHV in Cambodia monitor both MNP compliance and recommended IYCF practices (Kingdom of Cambodia, 2014). After a 1‐year pilot MNP project in Rwanda, more caregivers in intervention than comparison areas had talked about complementary feeding with their local CHW (McLean, Michaux, et al., 2013). In Cameroon, caregivers valued cooking demonstrations by CHW for hands‐on learning how to prepare nutritious foods for young children and practicing MNP use (McLean, Suter, et al., 2013). In contrast, issues with the consistency and frequency of MNP delivery by CHV and their credibility among mothers were observed in the Philippines (HKI, 2015) and Bangladesh (Sarma, Uddin, Harbour, & Ahmed, 2016).
Market‐based delivery mechanisms make MNP available for purchase through a variety of access points, including door‐to‐door sales by community vendors (Afsana, Haque, Sobhan, & Shahin, 2014; Suchdev et al., 2010), markets, pharmacies, health centres, or other places where consumers access goods and services (HF‐TAG, 2015). This alternative distribution channel can benefit those that the public health system does not reach but is less likely to provide IYCF counselling and support. In these contexts, it is essential for MNP promotional materials to include messages on recommended IYCF behaviours and demonstrate how MNP are part of a broader breastfeeding and complementary feeding context (Tripp et al., 2011). In Madagascar, where MNP are sold through private clinics in urban areas, training and regular review meetings improved the nutrition knowledge of private sector MNP providers and helped them promote complementary feeding practices along with MNP to their clients (PSI Research Division, 2012). Integration of MNP sales in Bangladesh with a package of intensive IYCF behaviour change interventions implemented by Alive & Thrive did not have either a positive or negative influence on IYCF practices (T Sanghvi, personal communication).
Contextual factors determine whether one or more of the above delivery mechanisms is most likely to achieve the desired reach; evidence regarding programme effectiveness, sustainability, and potential for scale‐up should also be considered (Olney, Rawat, & Ruel, 2012). Other potential delivery mechanisms for MNP distribution include integrating MNP interventions with social safety net programmes (HF‐TAG, 2011) or with agricultural support, such as in Mongolia (Batjargal et al., 2013) and Nepal (Osei et al., 2015). MNP delivery to young children in refugee camps and emergency contexts has been successfully implemented with a positive impact on child nutritional status (Rah et al., 2012). The potential for MNP interventions to improve complementary feeding practices in these settings has not been studied.
4.3. Behaviour change interventions
MNP programme effectiveness requires that the product be used for an extended period of time and often requires changes in child feeding practices (HF‐TAG, 2015). No matter what delivery mechanism is used, all programs must develop and deliver strategic behaviour change interventions in order to generate demand, ensure continued high coverage, reinforce appropriate use of MNP, and influence child‐feeding practices in the target population. Local formative research findings are useful for developing the program impact pathway and identifying simple and clear key messages that target specific child feeding practices that providers can understand and promote. Broad dissemination of IYCF messages through mass media and visual aids helps to increase awareness of recommended feeding practices and reinforces the interpersonal communication efforts of health care providers at facility and community levels. Customizing the MNP packaging and branding strategy for market‐based delivery models are also opportunities for including specific IYCF messages.
4.4. Research, monitoring, and evaluation
Formative research, monitoring, and evaluation are shown as cross‐cutting in the framework, providing data to inform strategic planning and implementation. Formative research during the MNP program design phase enhances understanding about child‐feeding knowledge, attitudes, and practices of caregivers (HF‐TAG, 2015) and identifies the potential barriers and facilitating factors associated with behaviour change around complementary feeding and MNP use. This informs the development of key messages and the design of context‐specific and effective BCC strategies, including IYCF counselling materials that resonate with caregivers (Bentley et al., 2014). Routine monitoring by MNP providers may increase their awareness of caregiver concerns with child‐feeding practices and contribute to improve IYCF counselling and support. However, we did not find specific examples of this purported pathway, and more research is therefore needed. Evaluation of MNP program outcomes and impact helps to build the evidence base for effective strategies to improve complementary feeding practices, both nationally and internationally. The HF‐TAG (2013) sample logic model for integrated IYCF and MNP projects includes complementary feeding indicators (MMF, MDD, and MAD), which are collected through periodic surveys. However, no IYCF indicators that can be monitored on a regular basis are provided.
4.5. Household actions
A supportive policy environment and effective MNP delivery mechanism, complemented by strategic behaviour change interventions, all contribute to influencing household level actions, the primary locus of child care and feeding practices. As shown in Figure 1, the promotion and use of MNP have the theoretical potential to help caregivers adopt recommended complementary feeding practices (PAHO/WHO, 2003; Stewart, Iannotti, Dewey, Michaelsen, & Onyango, 2013), as summarized in Table 3 and discussed here under three broad themes–quality foods, optimal feeding practices, and food and water safety.
Table 3.
Summary of potential effects of MNP programmes on complementary feeding practices
| Recommended practice | Potential effect of MNP programme |
|---|---|
| Quality foods | |
| Micronutrient‐rich foods | • increased intake of iron‐rich and micronutrient‐fortified foods |
| Dietary diversity | • increased minimum dietary diversity among MNP consumers |
| Energy density |
• increased consistency of first foods (do not add MNP to liquids) • increased energy density of foods • increased nutrient density of foods |
| Optimal feeding practices | |
| Introduce foods at 6 months |
• promotion of exclusive breastfeeding for first 6 months • increased incentive for caregivers to start giving solid/semisolidfoods at appropriate age (MNP targets children ≥6 months) |
| Continued breastfeeding | • promotion of continued breastfeeding (no negative effect) |
| Responsive feeding |
• active feeding of child; encouraged to finish portion with MNP • increased attention by caregiver to child while eating |
| Frequency of feeding |
• daily feeding of foods, especially among children 6–8 months • higher meal frequency (evidence is mixed) • increased appetite, resulting in increased intake and meal frequency |
| Feeding during/after illness | • encouragement to feed sick child |
| Food and water safety | |
| Clean water | • increased use of clean water to prepare child foods |
| Personal hygiene | • more frequent handwashing by caregiver at key times |
| Food storage and preparation | • increase in disposal of child's leftover food |
4.5.1. Quality foods
Because traditional complementary foods are often of low nutritional quality, there is a need to improve the energy and nutrient density, diversity, and micronutrient content of these foods. Addition of MNP to complementary foods directly contributes to increased child intake of iron and up to 15 other micronutrients, depending on the formulation, and can be an affordable way for families to help children fully meet their micronutrient needs (Baldi et al., 2013). Increasing intake of other locally available micronutrient‐rich foods, such as animal source foods, requires addressing cultural and socioeconomic barriers and including this as a priority behaviour in training and BCC efforts (Allen, 2012; Sanghvi, Jimerson, Hajeebhoy, Zewale, & Nguyen, 2013). There were few examples found of MNP programs and BCC materials that directly addressed this.
MNP interventions also could be a catalyst to motivate caregivers to prepare food of adequate consistency and improve the energy and nutrient density of traditional porridges (McLean, Suter, et al., 2013). Promoting foods with adequate consistency is essential because MNP tends to dissolve in liquids, and this may change the colour or taste of the food, making it less acceptable. A summary of formative research from six countries showed that the type and consistency of first foods given to infants ranged widely and that following MNP acceptability trials in each country, there was an overall improvement in the consistency of foods given to young children (Michaux et al., 2014). Short MNP intervention trials in Cameroon (McLean, Suter, et al., 2013) and Timor‐Leste (Osei et al., 2014) also showed a positive effect of MNP use on the consistency of porridge prepared.
Evidence of improved diversity of foods given to children benefiting from MNP interventions is limited. A 2013 national survey in Kyrgyz Republic showed increased MDD (from 75% to 87%) in children 6–29 months (MOH Kyrgyz Republic, UNICEF, & CDC, 2015). Preliminary data from Madagascar indicate that the proportion of children 6–23 months receiving foods with MDD increased from 11% to 47% (Ramalanjaona et al., 2014). In Nepal, children who had consumed 30–60 MNP sachets were more than twice as likely to have met the dietary diversity recommendation (Mirkovic et al., 2016). After a 1‐year MNP pilot in Rwanda, caregivers were adding MNP to a variety of foods including beans, green leafy vegetables, Irish potatoes, and other root vegetables, consistent with BCC messages (McLean, Michaux, et al., 2013). In Cameroon, researchers specifically focused on dietary diversity as they worked with caregivers to develop local, culturally acceptable food vehicles for MNP (McLean, Suter, et al., 2013).
4.5.2. Optimal feeding practices
Promotion of MNP use can improve timely introduction of complementary foods because it encourages the introduction of food at the age of 6 months. This was observed in Bangladesh (Zlotkin et al., 2005), Mongolia (Batjargal et al., 2013), and Nepal (Mirkovic et al., 2016). BCC materials and MNP sachet package design can also encourage continued breastfeeding while giving MNP (HF‐TAG, 2015). MNP use in research and programmatic settings did not reduce rates of continued breastfeeding among caregivers using MNP (Bilukha, Howard, Wilkinson, Bamrah, & Husain, 2011; Mirkovic et al., 2016; Ramalanjaona et al., 2014; Samadpour, Long, Hayatbakhsh, & Marks, 2011).
MNP interventions promote active and responsive feeding practices, in part to ensure the child eats the entire portion of food mixed with the MNP within 30 minutes in order to prevent colour or taste changes in the food (Michaux et al., 2014). Responsive feeding is especially important in contexts where young children are malnourished and may need active encouragement to eat due to a poor appetite (WHO/UNICEF, 2005). However, a potential increased risk of forced‐feeding young children due to the caregiver's fear of wasting the unfinished MNP sachet was observed in Bangladesh (Pelto et al., 2015). MNP program emphasis on feeding children with a spoon may also discourage local practices of hand‐feeding by caregivers or self‐feeding by the child, which can help to overcome time barriers expressed by caregivers (Affleck & Pelto, 2012). A strict focus on the child eating from a separate dish may also undermine important social and cultural values of sharing the family meal from a common dish.
Recommending daily use of MNP may promote higher meal frequency in contexts where caregivers give complementary foods occasionally to young children. Although MNP interventions focus on adding one sachet to one meal for the child in a day, BCC materials can provide guidance on the importance of regular meals and snacks for young children (McLean, Suter, et al., 2013). Program evidence is mixed on this topic. Children in Nepal who had consumed 30–60 MNP sachets were twice as likely to meet MMF recommendations (Mirkovic et al., 2016). An increase in feeding frequency was also observed in MNP program areas in Mongolia (Batjargal et al., 2013) and Kyrgyz Republic (MOH Kyrgyz Republic, UNICEF and CDC, 2015) but not in Madagascar (PSI Research Division, 2014) or Rwanda (Micronutrient Project (UBC), 2013). The effect of flexible schedules for MNP use on giving children semisolid food on a daily basis has not been assessed.
MNP program evaluations have shown an increase in the proportion of children fed a MAD: this indicator increased from 51% in 2009 to 67% in 2013 (p < .05) among children 6–23 months in Kyrgyz Republic where MNP coverage was 74% in 2013 (MOH Kyrgyz Republic, UNICEF and CDC, 2015). Children in Nepal who consumed 30–60 sachets from the last batch obtained were also twice more likely to meet recommendations for MAD compared to children who consumed no MNP (Mirkovic et al., 2016).
If MNP use addresses underlying nutrient deficiencies, this may improve a child's appetite and contribute to an increased amount of food consumed and the frequency of meals and snacks provided. Loss of appetite in young children is a central concern to caregivers in Bangladesh (Pelto et al., 2015) and Nigeria (UNICEF Nigeria, 2015). Caregivers participating in MNP pilot programs frequently report an observable increase in the child's appetite (Angdembe, Choudhury, Haque, & Ahmed, 2015; Bilukha et al., 2011; Jefferds et al., 2010; Osei et al., 2014; Tripp et al., 2011; UNICEF Nigeria, 2015). Encouraging caregivers to feed their child using a separate bowl can also help to increase their awareness about how much food the child consumes during each meal (McLean, Suter, et al., 2013).
Child feeding practices during and after child illness are also critical, particularly in contexts where food restriction for sick children is common. Although program guidance states that MNP should not be given to any child suffering from malaria, severe acute malnutrition, or severe anaemia (HF‐TAG, 2015), BCC materials can address the need for encouraging a sick child to eat. For example, the Rwanda MNP counselling reference guide encourages caregivers to continue feeding sick children with complementary foods prepared with the MNP, along with continued breastfeeding, explaining that the added vitamins and minerals will help to fight the infection and promote quick recovery.
4.5.3. Food and water safety
Safe preparation and storage of complementary foods and promotion of personal hygiene practices (e.g., handwashing with soap before preparing food and feeding the child) are directly addressed in many MNP interventions. Caregivers are instructed to add the MNP to a very small amount of food and discard any leftover, even if MNP was added, in order to avoid bacterial contamination of food that may be stored by the caregiver and given to the child later in the day, as reported in some MNP trials (Osei et al., 2014; UNICEF Nigeria, 2015). Evidence of a direct impact of MNP interventions on the safe preparation of foods and caregiver hygiene practices is limited. Caregiver hand‐washing practices were similar between intervention and comparison areas in Rwanda (McLean, Michaux, et al., 2013).
5. DISCUSSION
This review has identified many opportunities to improve complementary feeding practices in the process of designing and implementing MNP interventions. Countries scaling up MNP delivery to address micronutrient deficiencies in young children should consider carefully how to integrate this within broader programs that intentionally and simultaneously address other IYCF practices. Given the role of BCC approaches to improve complementary feeding practices (Sanghvi, Seidel, Baker, & Jimerson, 2017), it would be important that BCC for MNP targeted to caregivers also reinforce other key IYCF messages for improving child nutrition in that context. For example, given that adequate frequency of feeding is often a problem, MNP promotional materials can include guidance on the recommended number of times to feed a child each day, according to age, even though MNP is only given once in the day. Examples of training and BCC materials that integrate MNP and IYCF key messages exist that could be replicated by future programs (Mirkovic et al., 2016; Nguyen et al., 2016; UNICEF, 2012).
High‐quality formative research on local IYCF practices is being done as part of MNP program design, but there is still a gap in using these findings to develop the program impact pathway and translating them into IYCF program design recommendations. Research to date has focused primarily on MNP‐related issues, such as appropriate local food vehicles for MNP use, and could place more emphasis on identifying the key barriers and facilitators to caregivers providing locally available nutrient‐rich foods to young children (e.g., iron‐rich foods). Conducting dual purpose research and using the data to design interventions that promote both MNP use and optimal IYCF practices are recommended.
Experiences reviewed here have shown that MNP providers, including CHWs, tend to place more emphasis on assisting caregivers with appropriate MNP use than other IYCF practices. Training, monitoring, and supervision should reinforce proactive follow‐up of all targeted IYCF practices at both health facility and household levels.
A lack of field‐friendly monitoring indicators for child care and feeding practices was also consistently observed. Although many programs utilize large numbers of CHW for MNP delivery and home visits that include IYCF counselling and support, their field monitoring tools focus on MNP coverage and adherence. Changes in core IYCF indicators, including MMF, MDD, and MAD in children 6–23 months, are only assessed by program evaluation or nationally representative surveys. However, there are many caregiver actions associated with optimal IYCF practices that are directly promoted as part of MNP interventions and could be monitored on a more regular basis. The recent manual for developing and implementing monitoring systems for home fortification interventions will be helpful in strengthening monitoring and evaluation efforts (HF‐TAG, 2013).
Concerns with unintended negative consequences of MNP promotion on IYCF practices, such as caregivers introducing foods with MNP earlier than 6 months due to the promised positive effects or modifying feeding practices in a negative way (e.g., choosing not to purchase and give animal source foods) due to the perception that the MNP will provide all the nutrients the child needs, were rarely documented. When introducing a new “product” to improve nutrient intake in young children, it is important to avoid undermining existing efforts to improve the availability and affordability of quality local foods (WHO, 2008). As another potential unintended negative consequence, evidence of increased forced feeding has been found in Bangladesh (Pelto et al., 2015). Adverse side effects associated with MNP use, including increased diarrhoea (Soofi et al., 2013) and adverse effects on the gut microbiome and intestinal inflammation (Jaeggi et al., 2015) may negatively impact child feeding practices, dietary intake, and nutrient absorption. Additional research is needed to explore whether there are real risks of MNP promotion for optimal IYCF practices. In addition to well‐designed research trials, post hoc analysis of program evaluation data on IYCF practices looking at groups with different MNP adherence levels may also be useful in exploring these indirect effects (Mirkovic et al., 2016).
5.1. Limitations of current review
This was not a systematic review but included information in peer‐reviewed publications and the “grey” literature (unpublished reports by governments, multilaterals, and NGOs) on IYCF outcomes as measured by MNP programs. We limited the scope to MNP interventions delivered in stable and relatively food‐secure development contexts; therefore, our findings are not generalizable to food insecure and humanitarian settings. Many of the programs included were pilot efforts where intensity of program oversight and monitoring is likely higher and may result in better outcomes than in national‐scale programs. Program evaluations were often based on before‐and‐after study designs without a comparison or control group, making it impossible to attribute the changes observed solely to the intervention. Thus, the proposed framework is primarily theoretical, as there was sparse evidence to support or contradict the proposed impact pathways. Although stronger evaluation designs are recommended, it will be difficult to identify the specific role of MNP promotion in changes in IYCF practices in contexts where an integrated approach is effectively delivered.
6. CONCLUSION
There is a limited but growing body of evidence to suggest that the implementation of MNP interventions, often integrated with programs seeking to improve IYCF, can contribute to improve complementary feeding practices. MNP interventions play an important role in ensuring adequate micronutrient intake and reducing anaemia in young children. Building on a supportive policy environment and complemented by strategic and integrated BCC efforts, MNP delivery through routine health services, community‐based outreach, market‐based models, and other platforms has the potential to increase awareness of important IYCF practices in a broad sense and increase frequency of contact between caregivers and providers of IYCF counselling and support. With regular follow‐up at the household level and use of hands‐on methods for teaching caregivers about ways to prepare foods and feed them to their young children, MNP interventions have the potential to add renewed focus and resources to existing IYCF programs. However, this can only be achieved when MNP intervention design, implementation, monitoring, and evaluation activities are fully introduced as part of IYCF programming.
CONFLICTS OF INTEREST
FB, RK, and RS are staff members of UNICEF. KS worked as a consultant for UNICEF. The opinions and statements in this article are those of the authors and may not reflect official UNICEF policies. The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
FB, RK, and RS conceived the study. KS collected the data, designed the framework and wrote the draft manuscript. All authors critically revised the manuscript and approved the final version.
ACKNOWLEDGEMENTS
This review paper was commissioned by the Nutrition Section at UNICEF, with guidance and input from the Infant and Young Child Feeding and the Micronutrient teams. Information on country programs was graciously provided by UNICEF country staff: Arnaud Laillou (Cambodia), Annette Imohe (Nigeria), Munkhjargal Luvsanjamba (Mongolia), Aashima Garg (Philippines), Pradiumna Dahal (Nepal), Cholpon Imanalieva (Kyrgyz Republic), Simeon Nanama (Madagascar), Ireen Akhter Chowdhury (Bangladesh), Maria Elena Ugaz (Peru), Josephine Kayumba (Rwanda), and Ines Lezama (Cameroon). We also appreciate helpful comments on earlier drafts from Dominic Schofield (GAIN), Saskia dePee (WFP), and Tina Sanghvi (Alive & Thrive, FHI Solutions). FB, RK, and RS are UNICEF staff members.
Siekmans K, Bégin F, Situma R, Kupka R. The potential role of micronutrient powders to improve complementary feeding practices. Matern Child Nutr. 2017;13(S2):e12464 10.1111/mcn.12464
REFERENCES
- Affleck, W. , & Pelto, G. (2012). Caregivers' responses to an intervention to improve young child feeding behaviors in rural Bangladesh: A mixed method study of the facilitators and barriers to change. Social Science & Medicine, 75, 651–658. [DOI] [PubMed] [Google Scholar]
- Afsana, K. , Haque, M. R. , Sobhan, S. , & Shahin, S. A. (2014). BRAC's experience in scaling‐up MNP in Bangladesh. Asia Pacific Journal of Clinical Nutrition, 23, 377–384. [DOI] [PubMed] [Google Scholar]
- Allen, L. H. (2012). Global dietary patterns and diets in childhood: Implications for health outcomes. Annals of Nutrition & Metabolism, 61(Suppl 1), 29–37. [DOI] [PubMed] [Google Scholar]
- Angdembe, M. R. , Choudhury, N. , Haque, M. R. , & Ahmed, T. (2015). Adherence to multiple micronutrient powder among young children in rural Bangladesh: A cross‐sectional study. BMC Public Health, 15, 440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avula, R. , Frongillo, E. A. , Arabi, M. , Sharma, S. , & Schultink, W. (2011). Enhancements to nutrition program in Indian integrated child development services increased growth and energy intake of children. The Journal of Nutrition, 141, 680–684. [DOI] [PubMed] [Google Scholar]
- Baldi, G. , Martini, E. , Catharina, M. , Muslimatun, S. , Fahmida, U. , Jahari, A. B. , … de Pee, S. (2013). Cost of the Diet (CoD) tool: First results from Indonesia and applications for policy discussion on food and nutrition security. Food and Nutrition Bulletin, 34, S35–S42. [DOI] [PubMed] [Google Scholar]
- Batjargal, J. , Gereljargal, B. , Bolormaa, N. , Tserendolgor, U. , Otgonjargal, D. , Enkhtungalag, B. , … Tserenlkham, B. (2013). Evaluation of outcomes of the project “reducing persistent chronic malnutrition in children” JFPR 9131: Survey report. Ulaanbaatar, Mongolia: Ministry of Health (Government of Mongolia), National Center of Public Health, Asian Development Bank. [Google Scholar]
- Bentley, M. E. , Johnson, S. L. , Wasser, H. , Creed‐Kanashiro, H. , Shroff, M. , Fernandez Rao, S. , & Cunningham, M. (2014). Formative research methods for designing culturally appropriate, integrated child nutrition and development interventions: An overview. Annals of the New York Academy of Sciences, 1308, 54–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhutta, Z. A. , Das, J. K. , Rizvi, A. , Gaffey, M. F. , Walker, N. , Horton, S. , … Maternal and Child Nutrition Study Group . (2013). Evidence‐based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet, 382, 452–477. [DOI] [PubMed] [Google Scholar]
- Bilukha, O. , Howard, C. , Wilkinson, C. , Bamrah, S. , & Husain, F. (2011). Effects of multimicronutrient home fortification on anemia and growth in Bhutanese refugee children. Food and Nutrition Bulletin, 32, 264–276. [DOI] [PubMed] [Google Scholar]
- De‐Regil, L. M. , Suchdev, P. S. , Vist, G. E. , Walleser, S. , & Pena‐Rosas, J. P. (2011). Home fortification of foods with multiple micronutrient powders for health and nutrition in children under two years of age. Cochrane Database of Systematic Reviews, (9), CD008959. [DOI] [PubMed] [Google Scholar]
- Fabrizio, C. S. , van Liere, M. , & Pelto, G. (2014). Identifying determinants of effective complementary feeding behaviour change interventions in developing countries. Maternal & Child Nutrition, 10, 575–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HF‐TAG (2011). Programmatic guidance brief on use of micronutrient powders (MNP) for home fortification. Geneva: Home Fortification Technical Advisory Group. [Google Scholar]
- HF‐TAG (2013). A manual for developing and implementing monitoring systems for home fortification interventions. Geneva: Home Fortification Technical Advisory Group. [Google Scholar]
- HF‐TAG (2015). Planning for program implementation of home fortification with micronutrient powders (MNP): A step‐by‐step manual (version 1). Geneva: Home Fortification Technical Advisory Group. [Google Scholar]
- HKI (2015). Process evaluation: Enhancing local nutrition interventions (ELNI) project for maternal and young child nutrition security (MYCNSIA). Manila, Philippines: Helen Keller International. [Google Scholar]
- Issaka, A. I. , Agho, K. E. , Page, A. , Burns, P. , Stevens, G. J. , & Dibley, M. J. (2015a). Determinants of suboptimal complementary feeding practices among children aged 6–23 months in four anglophone West African countries. Maternal & Child Nutrition, 11, 14–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Issaka, A. I. , Agho, K. E. , Page, A. , Burns, P. , Stevens, G. J. , & Dibley, M. J. (2015b). Determinants of suboptimal complementary feeding practices among children aged 6–23 months in seven francophone West African countries. Maternal & Child Nutrition, 11, 31–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaeggi, T. , Kortman, G. A. , Moretti, D. , Chassard, C. , Holding, P. , Dostal, A. , … Zimmermann, M. B. (2015). Iron fortification adversely affects the gut microbiome, increases pathogen abundance and induces intestinal inflammation in Kenyan infants. Gut, 64, 731–742. [DOI] [PubMed] [Google Scholar]
- Jefferds, M. E. , Mirkovic, K. R. , Subedi, G. R. , Mebrahtu, S. , Dahal, P. , & Perrine, C. G. (2015). Predictors of micronutrient powder sachet coverage in Nepal. Maternal & Child Nutrition, 11(Suppl 4), 77–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferds, M. E. , Ogange, L. , Owuor, M. , Cruz, K. , Person, B. , Obure, A. , … Ruth, L. J. (2010). Formative research exploring acceptability, utilization, and promotion in order to develop a micronutrient powder (Sprinkles) intervention among Luo families in western Kenya. Food and Nutrition Bulletin, 31, S179–S185. [DOI] [PubMed] [Google Scholar]
- Kingdom of Cambodia (2014). 2014 National Nutrition Report. Phnom Penh, Cambodia: Kingdom of Cambodia and UNICEF. [Google Scholar]
- Korenromp, E. L. , Adeosun, O. , Adegoke, F. , Akerele, A. , Anger, C. , Ohajinwa, C. , … Aminu, F. (2016). Micronutrient powder distribution through maternal, neonatal and child health weeks in Nigeria: Process evaluation of feasibility and use. Public Health Nutrition, 19, 1882–1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krasevec, J. , An, X. , Kumapley, R. , Bégin, F. , & Frongillo, E. A. (2017). Diet quality and risk of stunting among infants and young children in low‐ and middle‐income countries. Maternal & Child Nutrition, 13(Suppl 2): e12430 10.1111/mcn.12430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamstein, S. , Stillman, T. , Koniz‐Booher, P. , Aakesson, A. , Collaiezzi, B. , Williams, T. , … Anson, A. (2014). Evidence of effective approaches to social and behavior change communication for preventing and reducing stunting and anemia: Report from a systematic literature review. Arlington, VA: USAID/Strengthening Partnerships, Results, and Innovations in Nutrition Globally (SPRING) Project. [Google Scholar]
- Lundeen, E. , Schueth, T. , Toktobaev, N. , Zlotkin, S. , Hyder, S. M. , & Houser, R. (2010). Daily use of Sprinkles micronutrient powder for 2 months reduces anemia among children 6 to 36 months of age in the Kyrgyz Republic: A cluster‐randomized trial. Food and Nutrition Bulletin, 31, 446–460. [DOI] [PubMed] [Google Scholar]
- Marriott, B. P. , White, A. , Hadden, L. , Davies, J. C. , & Wallingford, J. C. (2012). World Health Organization (WHO) infant and young child feeding indicators: Associations with growth measures in 14 low‐income countries. Maternal & Child Nutrition, 8, 354–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean, J. , Michaux, K. , & Smith, L . (2013). The implementation of home fortification and nutrition education to combat anaemia and micronutrient deficiencies among children 6–23 months in Rwanda: Endline report. Vancouver, Canada: Micronutrient Project (University of British Columbia). [Google Scholar]
- McLean, J. , Suter, M. , Foley, J. , Mitch, N. , Norburn, D. , Norris, H. , & Daly, Z. (2013). Formative research for the development of a home fortification programme for young children in Cameroon. Vancouver, Canada: Micronutrient Project (University of British Columbia). [Google Scholar]
- Michaux, K. , Anema, A. , Green, T. , Smith, L. , McLean, J. , Omwega, A. , … Ahimbisibwei, M. (2014). Home fortification with micronutrient powders: Lessons learned from formative research across six countries. Sight and Life, 28, 26–35. [Google Scholar]
- Mirkovic, K. R. , Perrine, C. G. , Subedi, G. R. , Mebrahtu, S. , Dahal, P. , & Jefferds, M. E. (2016). Micronutrient powder use and infant and young child feeding practices in an integrated program. Asia Pacific Journal of Clinical Nutrition, 25, 350–355. [DOI] [PubMed] [Google Scholar]
- MOH Kyrgyz Republic, UNICEF & CDC (2015). Follow‐up survey of nutritional status in children 6–29 months of age, Kyrgyz Republic 2013. Bishkek, Kyrgyz Republic: Ministry of Health of the Kyrgyz Republic, National Statistics Committee of the Kyrgyz Republic, UNICEF‐Kyrgyzstan, U.S. Centers for Disease Control and Prevention. [Google Scholar]
- Nguyen, M. , Poonawala, A. , Leyvraz, M. , Berger, J. , Schofield, D. , Nga, T. T. , … Wieringa, F. T. (2016). A delivery model for home fortification of complementary foods with micronutrient powders: Innovation in the context of Vietnamese health system strengthening. Nutrients, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noij, F. (2013). Support to the distribution and use of micronutrient powders in Cambodia: Learnings from the MDG‐F supported joint programme on children, food security and nutrition 2010–2013. Phnom Penh, Cambodia: MDG Achievement Fund. [Google Scholar]
- Olney, D. K. , Rawat, R. , & Ruel, M. T. (2012). Identifying potential programs and platforms to deliver multiple micronutrient interventions. The Journal of Nutrition, 142, 178S–185S. [DOI] [PubMed] [Google Scholar]
- Osei, A. , Septiari, A. , Suryantan, J. , Hossain, M. M. , Chiwile, F. , Sari, M. , … Faillace, S. (2014). Using formative research to inform the design of a home fortification with micronutrient powders (MNP) Program in Aileu District, Timor‐Leste. Food and Nutrition Bulletin, 35, 68–82. [DOI] [PubMed] [Google Scholar]
- Osei, A. K. , Pandey, P. , Spiro, D. , Adhikari, D. , Haselow, N. , De Morais, C. , … Davis, D. (2015). Adding multiple micronutrient powders to a homestead food production programme yields marginally significant benefit on anaemia reduction among young children in Nepal. Maternal & Child Nutrition, 11(Suppl 4), 188–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osendarp, S. J. , Broersen, B. , van Liere, M. J. , De‐Regil, L. M. , Bahirathan, L. , Klassen, E. , & Neufeld, L. M. (2016). Complementary feeding diets made of local foods can be optimized, but additional interventions will be needed to meet iron and zinc requirements in 6‐ to 23‐month‐old children in low‐ and middle‐income countries. Food and Nutrition Bulletin, 37, 544–570. [DOI] [PubMed] [Google Scholar]
- PAHO/WHO (2003). Guiding principles for complementary feeding of the breastfed child. Washington, DC: Pan American Health Organization/World Health Organization. [Google Scholar]
- Pelto, G. , Lee, J. , Akhter, S. , Porqueddu, T. , Thuy‐Co Hoang, C. , Anwar, I. , & Akhter, R. (2015). Summary report: Infant and young child feeding and home fortification in rural Bangladesh––Perspectives from a focused ethnographic study. Geneva: GAIN, icddr,b, Valid International. [Google Scholar]
- Rah, J. H. , dePee, S. , Kraemer, K. , Steiger, G. , Bloem, M. W. , Spiegel, P. , … Bilukha, O. (2012). Program experience with micronutrient powders and current evidence. The Journal of Nutrition, 142, 191S–196S. [DOI] [PubMed] [Google Scholar]
- Ramalanjaona, N. , Rakotonirina, S. , Tucker Brown, A. , Reerink, I. , Peterson, J. , & Irena, A. (2014). Scaling up micronutrient interventions: Bridging the gap between theory and implementation. Poster session presented at the Micronutrient Forum Global Conference, Addis Ababa, Ethiopia. [Google Scholar]
- Research Division, P. S. I. (2012). Evaluating knowledge, practices and motivation related to infant and young child feeding among top Reseau providers in three urban sites, and selected public sector providers in one rural site of Madagascar, baseline study 2012. Washington, DC: Population Services International. [Google Scholar]
- Research Division, P. S. I. (2014). Madagascar (2014): Household survey on nutrition evaluating exclusive breastfeeding practices among infants between 0 and 5 months and complimentary feeding practices and anemia among infants and young children between 6 and 23 months of age: Endline study 2014 in Vavatenina and Fenerive‐Est districts. Washington, DC: Population Services International. [Google Scholar]
- Salam, R. A. , MacPhail, C. , Das, J. K. , & Bhutta, Z. A. (2013). Effectiveness of micronutrient powders (MNP) in women and children. BMC Public Health, 13(Suppl 3), S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samadpour, K. , Long, K. Z. , Hayatbakhsh, R. , & Marks, G. C. (2011). Randomised comparison of the effects of Sprinkles and Foodlets with the currently recommended supplement (Drops) on micronutrient status and growth in Iranian children. European Journal of Clinical Nutrition, 65, 1287–1294. [DOI] [PubMed] [Google Scholar]
- Sanghvi, T. , Jimerson, A. , Hajeebhoy, N. , Zewale, M. , & Nguyen, G. H. (2013). Tailoring communication strategies to improve infant and young child feeding practices in different country settings. Food and Nutrition Bulletin, 34, S169–S180. [DOI] [PubMed] [Google Scholar]
- Sanghvi, T. , Seidel, R. , Baker, J. , & Jimerson, A. (2017). Using behavior change approaches to improve complementary feeding practices. Maternal & Child Nutrition, 13(Suppl 2): e12406 10.1111/mcn.12406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarma, H. , Uddin, M. F. , Harbour, C. , & Ahmed, T. (2016). Factors influencing child feeding practices related to home fortification with micronutrient powder among caregivers of under‐5 children in Bangladesh. Food and Nutrition Bulletin, 0379572116645916. [DOI] [PubMed] [Google Scholar]
- Serdula, M. K. , Lundeen, E. , Nichols, E. K. , Imanalieva, C. , Minbaev, M. , Mamyrbaeva, T. , … the Kyrgyz Republic Working Group (2013). Effects of a large‐scale micronutrient powder and young child feeding education program on the micronutrient status of children 6‐24 months of age in the Kyrgyz Republic. European Journal of Clinical Nutrition, 67, 703–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafique, S. , Sellen, D. W. , Lou, W. , Jalal, C. S. , Jolly, S. P. , & Zlotkin, S. H. (2016). Mineral‐ and vitamin‐enhanced micronutrient powder reduces stunting in full‐term low‐birth‐weight infants receiving nutrition, health, and hygiene education: A 2 × 2 factorial, cluster‐randomized trial in Bangladesh. The American Journal of Clinical Nutrition, 103, 1357–1369. [DOI] [PubMed] [Google Scholar]
- Soofi, S. , Cousens, S. , Iqbal, S. P. , Akhund, T. , Khan, J. , Ahmed, I. , … Bhutta, Z. A. (2013). Effect of provision of daily zinc and iron with several micronutrients on growth and morbidity among young children in Pakistan: A cluster‐randomised trial. Lancet, 382, 29–40. [DOI] [PubMed] [Google Scholar]
- Stewart, C. P. , Iannotti, L. , Dewey, K. G. , Michaelsen, K. F. , & Onyango, A. W. (2013). Contextualising complementary feeding in a broader framework for stunting prevention. Maternal & Child Nutrition, 9(Suppl 2), 27–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchdev, P. S. , Ruth, L. , Obure, A. , Were, V. , Ochieng, C. , Ogange, L. , … Jefferds, M. E. (2010). Monitoring the marketing, distribution, and use of Sprinkles micronutrient powders in rural western Kenya. Food and Nutrition Bulletin, 31, S168–S178. [DOI] [PubMed] [Google Scholar]
- Tripp, K. , Perrine, C. G. , de Campos, P. , Knieriemen, M. , Hartz, R. , Ali, F. , … Kupka, R. (2011). Formative research for the development of a market‐based home fortification programme for young children in Niger. Maternal & Child Nutrition, 7(Suppl 3), 82–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF (2012). UNICEF infant and young child feeding––Counseling cards for community workers. New York: UNICEF. [Google Scholar]
- UNICEF (2015). Nutridash 2014: Global report. New York: UNICEF. [Google Scholar]
- UNICEF Nigeria (2015). Formative research for IYCF & MNP programming in Nigeria: Summary of key findings. Abuja, Nigeria: UNICEF Nigeria. [Google Scholar]
- White, J. M. , Bégin, F. , Kumapley, R. , Murray, C. , & Krasevec, J. (2017). Complementary feeding practices: Current global and regional estimates. Maternal & Child Nutrition, 13(Suppl 2): e12505 10.1111/mcn.12505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2008). Strengthening action to improve feeding of infants and young children 6–23 months of age in nutrition and child health programmes: Report of proceedings, Geneva, 6–9 October 2008. Geneva: World Health Organization. [Google Scholar]
- WHO (2016). WHO guideline: Use of multiple micronutrient powders for point‐of‐use fortification of foods consumed by infants and young children aged 6–23 months and children aged 2–12 years. Geneva: World Health Organization. [PubMed] [Google Scholar]
- WHO/UNICEF (2005). IMCI handbook: Integrated management of childhood illness. Geneva: World Health Organization. [Google Scholar]
- Zlotkin, S. H. , Schauer, C. , Christofides, A. , Sharieff, W. , Tondeur, M. C. , & Hyder, S. M. (2005). Micronutrient Sprinkles to control childhood anaemia. PLoS Medicine, 2, e1. [DOI] [PMC free article] [PubMed] [Google Scholar]


