Abstract
After decades of global response to iron‐deficiency anemia, lessons learned from antenatal iron‐folic acid (IFA) supplementation can inform new micronutrient supplementation efforts. The World Health Organization recommends calcium supplementation for the prevention of preeclampsia; however, little is documented on how to design programs to integrate calcium into the standard of care. Twenty interviews with pregnant women and 22 interviews with health providers and volunteers in two districts in Ethiopia were conducted to examine how barriers and facilitators to antenatal care, IFA supplementation, and initial reactions to calcium supplements and regimen might influence adherence and inform future programs. Women viewed supplementation positively but cited lack of information on benefits and risks, forgetfulness, and inconsistent IFA supply as challenges. Though knowledge and awareness of anemia and IFA supplements were widespread, preeclampsia was mostly unknown. Some symptoms of preeclampsia were viewed as normal in pregnancy, making it difficult to convey risk to motivate supplement use. Some women viewed co‐consumption of IFA and calcium as potentially harmful and were confused regarding the simultaneous risks of anemia and hypertension, understood as “low” and “high” blood levels in pregnancy. However, most said they would take both IFA and calcium supplements if provided with supplements and counseling on purpose and benefits. Strategies such as social support from families, stronger community‐based counseling, and increased health care provider and community awareness of preeclampsia are critical for women to understand the benefits of supplementation and resolve confusion caused by current descriptors used for anemia and hypertension.
Keywords: adherence barriers, adherence facilitators, antenatal care, calcium supplementation, formative research, iron‐folic acid supplementation
1. INTRODUCTION
Micronutrient deficiencies contribute to maternal morbidity and mortality in low‐ and middle‐income countries where dietary consumption of key micronutrients is often inadequate to meet increased nutritional demands during pregnancy (Hacker, Fung, & King, 2012; Stoltzfus and Dreyfuss, 1998). Globally, iron deficiency is highly prevalent, and anemia affects 32 million pregnant women (Stevens et al., 2013) and contributes to 20% of maternal deaths (World Health Organization, 2016). Hypertensive disorders in pregnancy including preeclampsia are the second highest direct cause of maternal mortality (after hemorrhage), accounting for 10% to 15% of maternal mortality (Duley, 2009) or over 40,000 maternal deaths annually (Khan et al., 2006). Antenatal iron‐folic acid (IFA) and calcium supplementation can prevent iron‐deficiency anemia and preeclampsia, respectively, in populations where dietary intake is low (Hofmeyr, Duley, & Atallah, 2007; Peña‐Rosas, De‐Regil, Garcia‐Casal, & Dowswell, 2015).
The World Health Organization antenatal IFA supplementation guideline (one daily supplement) (World Health Organization, 2012) is a long‐standing policy in many countries, and supplementation is included in standard maternal care (Sanghvi, Harvey, & Wainwright, 2010). Recent guidelines on antenatal calcium supplementation (1.5–2.0 g/day in three doses) to prevent preeclampsia have yet to be widely implemented in country‐wide policies and programs (World Health Organization, 2013). Consumption of both IFA and calcium according to guidelines could require four pill‐taking events daily, although some authors suggest lower‐dose calcium regimens (Omotayo et al., 2016; Hofmeyr, Belizan, & Von Dadelszen, 2014). Complex regimens contribute to poor adherence, as do ineffective provider–patient dialogue, inconsistent access to care, and shortages of product supply, all common in many low‐income settings (Brown & Bussell, 2011; Galloway et al., 2002).
Formative research is critical to ensure that integrated maternal and child interventions are successful across multiple contexts, client subgroups, and preventive and curative methods (Bentley et al., 2014). Despite some studies exploring the influence of micronutrient product type and regimen on adherence and health status (Baxter et al., 2014; Joshi & Gumashta, 2013), there are gaps in knowledge on stakeholder perspectives on regimens that combine calcium and IFA.
Lessons learned from IFA supplementation programs can guide the integration of calcium into antenatal care (ANC) (Martin et al., 2017). Ethiopia's low coverage of timely ANC and high maternal mortality (World Bank Data Indicators [2011–2015], 2016) indicate high need and make it a suitable context for exploring potential challenges. Half of women in Oromia Region did not receive ANC during pregnancy in 2014; most (75%) did not consume iron supplements; 22% were not informed of signs of pregnancy complications (Central Statistical Agency, 2014). Focusing on communities where an earlier intervention had strengthened delivery of IFA supplements and counseling (Micronutrient Initiative, 2016) allowed us to assess perceptions and practices in contexts where women were likely to have actually encountered IFA programming.
To inform policy and program guidance for calcium and IFA supplementation, our primary objectives were to (a) examine practices and beliefs around ANC and IFA; (b) understand knowledge and perceived risks of anemia, preeclampsia, and eclampsia; and (c) explore views on calcium supplements and regimen among pregnant women. In addition, we sought to explore the knowledge, practices, and attitudes of health care providers and community‐based volunteers to provide context for understanding women's views and experiences.
Key messages.
Women have prevention‐focused motivations for attending antenatal care, but late initiation undercuts the preventive benefits of antenatal micronutrient supplementation.
Women were knowledgeable on anemia and iron but desired more detailed information on supplementation and health risks in pregnancy, and providers desired training to be more knowledgeable and offer enhanced services.
An integrated calcium/IFA regimen will likely introduce new challenges, including concerns regarding supplement quantity and co‐administration.
Women were generally receptive to potential calcium supplementation, and antenatal counseling, familial support, and reminders are likely to support adherence.
2. METHODS
2.1. Study setting
The study was conducted in two rural, agricultural districts in Oromia, Ethiopia, each with four primary health care units comprising a health center and five to ten widely distributed health posts. Health center nurses provide a full range of services; health extension workers (HEWs), operating from health posts, focus on preventive care. Local Health Development Army (HDA) volunteers liaise with HEWs to encourage preventive health care‐seeking and health‐promoting behaviors. Traditional birth attendants (TBAs), excluded from the formal Ethiopian health system, play an active role in maternal health (Temesgen, Umer, Buda, & Haregu, 2012).
Between December 2012 and April 2014, the Ethiopia Public Health Institute and Micronutrient Initiative implemented a community‐based program to strengthen antenatal IFA supplementation in Oromia (Micronutrient Initiative, 2016). Facility‐based health care providers and HEWs received training on the national IFA supplementation protocol and adherence monitoring and counseling approaches and improved availability of supplements and behavior change communication materials. Selection of study sites within this program area provided an opportunity to explore factors relevant to the introduction of calcium supplementation into existing antenatal services delivering IFA supplementation.
2.2. Sampling
We purposively selected two primary health care units per district based on geographic distribution and accessibility. In consultation with health center managers, we purposively selected 12 health posts in rural areas and district headquarter towns to obtain diversity in distance from health center, lowland versus highland and rural versus urban residence.
Interviewers conducted 22 in‐depth interviews across participant groups of nurses and HEWs (providers) and HDA volunteers and TBAs (volunteers) in June 2013. Interviewers visited selected health facilities and available providers were asked to participate. Volunteers were recruited through HEWs and interviewed in their homes. Interviewers conducted 20 in‐depth interviews with pregnant women in April 2014 at the nearest health post to their residence. Interviewers coordinated with HEWs familiar with the local population to recruit women who had and had not received ANC in their current pregnancy.
All those approached agreed to participate and gave written informed consent. Cornell University's Institutional Review Board, Jimma University's Institutional Review Board, and the Oromia Regional Health Bureau approved the study.
2.3. Data collection and analysis
A multidisciplinary team of researchers developed semi‐structured interview guides for each participant group on concerns and care‐seeking in pregnancy, provision and quality of ANC services, and perceptions of antenatal micronutrient supplements (Supporting information). Guides were translated into Afan Oromo, back‐translated by an independent translator, and pretested to fit the local context.
Four qualitative researchers conducted and audio‐recorded 1‐ to 2‐hour interviews, transcribed the interviews verbatim, and translated them into English. Research investigators and interviewers reviewed the transcripts for accuracy and completeness.
Three researchers (ZB, GC, and SO) coded transcripts and conducted thematic analysis using qualitative data analysis software ATLAS.ti 7.1. Initially, one researcher conducted iterative rounds of open coding of emergent themes associated with the research questions, guided by grounded theory (Corbin & Strauss, 1990). A second researcher independently coded a subset of transcripts. The team reviewed the coded transcripts to reach consensus on a coding scheme and consistent code definitions, which were then used to code all transcripts. Results were organized in matrices summarizing subthemes and key quotes, which were shared and reviewed to ensure consistency of thematic analysis. Findings were compared across participant groups to explore similarities and differences among women, providers, and volunteers. Peer debriefings were conducted with the broader research team to inform interpretation.
To guide a larger multiphase research project on antenatal calcium and IFA supplementation, a priori we developed a program impact pathway of critical steps that potentially lead to women receiving and consuming antenatal micronutrient supplements. The goal of formative research described here was to identify potential barriers and facilitators of adherence, thus we focused on pregnant women's perspectives, triangulating these results with the perspectives of providers and volunteers when relevant to provide a comprehensive picture of ANC and IFA supplementation. Results are presented in relation to critical steps in the pathway: (a) factors influencing women's participation in ANC; (b) ANC‐based transfer of supplements and information to motivate adherence; (c) women's motivation and likelihood of taking supplements, including knowledge of health risks targeted by supplements; and (d) factors influencing sustained adherence (Figure 1). Steps related to ensuring health facility supplies, staffing, and training were not addressed in this phase of the study.
Figure 1.
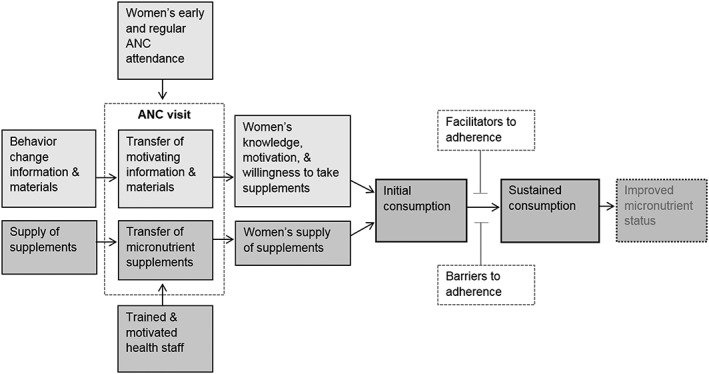
Key steps in a simplified program impact pathway for micronutrient supplementation, from antenatal care (ANC) delivery of supplements and information through supplement consumption to improved micronutrient status
3. RESULTS
3.1. Participant demographics
Characteristics of participating pregnant women are summarized in Table 1. All but one was married and the mean gravidity was 3.6 (range: 1–11). Mean gestational age was 7.1 (range: 4–9) months. Most women were farmers, primarily growing teff, a staple grain.
Table 1.
Demographic profile of Ethiopian pregnant women interviewed on antenatal care and micronutrient supplementation (N = 20)
| n (%) | ||
|---|---|---|
| Age (years) | 17–20 | 4 (20) |
| 21–34 | 14 (85) | |
| 35–45 | 2 (10) | |
| Level of education | No school | 12 (60) |
| Some primary | 3 (15) | |
| Completed primary | 5 (25) | |
| Religion | Orthodox | 15 (75) |
| Protestant | 4 (20) | |
| Traditional | 1 (05) | |
| Number of antenatal visits (current pregnancy) | None | 2 (10) |
| 2 | 6 (30) | |
| 3 | 9 (45) | |
| 4 | 3 (15) | |
| Location of antenatal care | Health center only | 7 (35) |
| Health post only | 6 (30) | |
| Health post and health center | 5 (25) | |
| Gestational age at first antenatal visit | First trimester | 7 (10) |
| Second trimester | 9 (30) | |
| Third trimester | 2 (45) |
Equal numbers of providers and volunteers were included in each district, all female except for one male nurse. Mean age was 26.5 years (range: 20–36) for providers and 45.9 years (range: 37–60) for volunteers. Most HDA volunteers had attended some primary school; most TBAs had no formal education.
3.2. Women's participation in ANC
All participating women knew ANC was available at health centers and health posts. Almost all had attended ANC at least once, usually in the second trimester or later, believing initiation should occur when there is fetal movement. Many women described prevention‐focused motivations for attending ANC: to learn their health status, receive vaccinations, and have “peace of mind.”
Most women preferred receiving ANC at health centers rather than health posts because of greater expertise and consistent availability of nurses providing more comprehensive services, as compared to HEWs (Table 2), and health center incentives for facility‐based delivery (e.g., food, baby clothes, and money). Providers and volunteers concurred. Most HEWs spontaneously reported extensive workload and lack of training as primary challenges for providing maternal care.
I learned about preeclampsia three years ago, but now I forget. There should be a mechanism in place to provide us with training. – HEW, 24 years old, small town
Table 2.
Preference for health center over health post services as reported by participating pregnant women
| Preference | Illustrative quotes | Respondent descriptors |
|---|---|---|
| Sophistication of services | ▪ HCs have a laboratory and medical equipment which is necessary to identify one's health problems. I started ANC visits at the HC because HEWs do not have enough equipment to diagnose and identify my problems. | Multipara, 26 years old, rural |
| Community meetings and incentives | ▪ The HC organizes pregnant mother meetings monthly and always gives us 145 birr (approximately 5.00 USD) at the end of the meeting.
▪ There is porridge and there is coffee. Mothers who deliver their baby at the HC will be pleased. |
Multipara, 27 years old, rural
Multipara, 24 years old, small town |
| Availability and access | ▪ HEWs may not be available but HC staff are always available. Thus, people prefer to visit the HC. Once, the HEW called us for a meeting, but she was absent. We waited for her the whole day and returned home without meeting her. Their messages often do not reach me. | Primipara, 20 years old, small town |
| Knowledge | ▪ HEWs don't have adequate knowledge to tell me about my condition. They tell me what I myself already know, nothing more. They can only take our weight and give us iron tablets.
▪ HEWs cannot identify any problem; hence nobody can get any solution from them. |
Multipara, 28 years old, rural
Multipara, 45 years old, small town |
Note. ANC = antenatal care; HC = health center; HEW = health extension worker.
3.3. ANC‐based transfer of supplements and information
Most women reported taking IFA supplements. Of the women who did not have supplements, two had not attended ANC, two attended ANC but did not receive IFA, and two had not returned for more supplements.
I am over 8 months pregnant and I am using iron only this last month. The health post was out of tablets for so long. I went three different times, but I couldn't get them. – Multipara, 30 years old, rural
Several women suggested home visits to provide supplements, encouragement and advice on how to take them, and follow up. Although HEWs agreed home visits could improve women's adherence, routine visits were limited by lack of staff and high workloads, and they anticipated difficulty carrying IFA supplies. They intended visits to motivate women to visit health posts. All groups mentioned HEWs and HDA volunteers as ideally positioned to mobilize women in the community and link providers and clients.
[HEWs] need to conduct more home visits to educate women. We also need to educate the HDAs so that they motivate women to take the [IFA] tablets. We must show the tablets and explain how women should use them. – HEW, 20 years old, small town
Women taking IFA were knowledgeable about the dosing schedule. Most women said they were told to take IFA with meals to minimize side effects but not given specific information on side effects. One woman was told IFA may cause heartburn; two were told to return to the health post if adverse effects were experienced.
Half of women taking supplements reported their provider had not discussed the benefits of IFA supplementation. Among women who received information on the benefits, most recalled hearing only that IFA was “good” for the mother and developing child.
HEWs don't tell us anything. They take our weight and order us to take the tablets and we don't understand why. They don't tell us the causes of the illness; however I wanted to learn what my problem was. – Multipara, 28 years old, rural
In contrast, all nurses and a few HEWs reported counseling during ANC on specific IFA benefits (e.g., prevention or treatment of “blood deficiency,” and improved fetal physical and cognitive development) and side effects (e.g., heartburn, nausea, and vomiting), including their temporary nature and strategies to reduce them (e.g., take with food).
Despite women's reports of receiving minimal information from providers, when asked about motivations for supplement use, nearly all demonstrated some knowledge, explaining that supplements “fill low blood,” improve mental and physical growth of the baby, and relieve fatigue and light‐headedness.
Likely due to recent IFA program strengthening, providers were knowledgeable about anemia and its symptoms, considering the condition common. Volunteers were aware of anemia symptoms and encouraged women to attend ANC and take IFA supplements.
Women who complain of light‐headedness may have low blood. For example, women may lose orientation, get confused, and fall down. So, for low blood I advise women to go to the health post to get tablets. – TBA, 40 years old, rural
Providers' understanding of preeclampsia and eclampsia varied. Nurses had more extensive knowledge; all identified the clinical manifestation of hypertension and two of four identified proteinuria and described how preeclampsia precedes eclampsia. Two HEWs were unaware of preeclampsia; the rest recognized the term from training. Only a few mentioned hypertension, labor complications, or other symptoms. Volunteers were unaware of the disease.
Nurses reported the importance of measuring blood pressure to identify cases, although they often lacked functional equipment. Nurses and HEWs felt their training and knowledge was inadequate to save the lives of women with preeclampsia, highlighting the value of a preventative supplementation approach. Two HEWs and two nurses had identified patients with high blood pressure in pregnancy and referred them to the nearest higher‐level facility 2–3 hours away. Preeclampsia was not a priority among those who had never witnessed a case.
I can't see [preeclampsia] as an important health issue in this area. Since I haven't encountered any case, I don't think I will encounter it in the future. I would not mention it as a problem. – Nurse, 25 years old, small town
When asked about introducing calcium into ANC services, a particularly important concern for providers and volunteers was training on the new protocol.
We have to receive training about the tablets. Then we can explain the benefits and side effects. We will advise women and teach them… they will understand and then use it. More challenges would be identified once implementation starts, thus it is important to give us prompt solutions to any problems which could occur during implementation. – HEW, 27 years old, small town
3.4. Women's motivation and likelihood of taking supplements
To understand women's motivation to take supplements, we asked about their diet in pregnancy, knowledge, and perceptions of anemia and preeclampsia risks and gathered initial reactions to calcium supplements and regimen.
Most women mentioned the importance of consuming a varied, balanced diet and eating certain foods to provide nutrients for the baby and prevent pregnancy‐related complications.
There was a belief that the baby in the womb does not feed. Now we realize half of the food consumed by mothers goes to the baby. The health and strength of the baby depends on what is consumed by the mother. – Multipara, 26 years old, rural
More than one quarter of women expressed challenges in regularly consuming such foods.
It is possible to prevent blood deficiency by having a balanced diet. The problem is some woman cannot access this diet because of limited funds. – Primipara, 21 years old, rural
All women were aware of anemia, understood as a reduction in blood volume (referred to as “low blood” or “blood deficiency” in either Amharic or Afan Oromo), as opposed to a lack of hemoglobin or weak blood. Women considered anemia to be the most important complication in pregnancy, noting it warranted treatment at a health facility. Most reported having anemia in their current pregnancy; more than half considered it a severe condition that made it difficult to work, and some said it could lead to death if untreated.
Women were familiar with hypertension, understood as “excess blood” or an increase in blood volume but did not relate it to pregnancy. Some women associated high blood pressure with excessive weight gain, eating too much, overconsuming sugar or salt, or anger and tension. Most respondents acknowledged both the infrequency and severity of the condition, several describing it as potentially fatal.
Blood deficiency is better than high blood. If the blood is low, it is possible to fill it up but if it gets high, nothing helps. It can lead to death. – Primipara, 20 years old, small town
Nearly half of women found the notion of low blood and high blood as concurrent health issues to be confusing; several reported they would be apprehensive to take calcium and IFA together (Table 3). Women who understood calcium and IFA supplementation as preventive measures were more accepting of concurrent supplementation.
As you told me, calcium is for prevention of the symptoms even without having the disease. If it is for prevention, it is not confusing. We can take calcium simultaneously with iron. – Multipara, 27 years old, small town
Table 3.
Quotes illustrating how common terms for hypertension and anemia that refer to blood volume may pose a barrier to pregnant women's willingness to consume concurrent calcium and IFA supplements
| Illustrative quotes | Respondent descriptors |
|---|---|
| ▪ It seems they [calcium and iron] have opposite action; I think it is not necessary to take two drugs which have opposite action. | Multipara, 27 years old, rural |
| ▪ They cannot be taken simultaneously. The tablet given for low blood increases blood and the tablet given for high pressure reduces it. | Multipara, 45 years old, small town |
| ▪ Iron increases low blood, calcium reduces high blood, I don't know what average thing could be created in between. I can't imagine what may happen if I took both. | Multipara, 28 years old, rural |
| ▪ One has to take a medication which fits for her own problem. If she has blood deficiency she should take iron. One should not take iron and calcium together. It may lead to death. I have to take a tablet which fits with my problem; I should not take everything coming to me. | Primipara, 20 years old, small town |
| ▪ It is confusing. It is not possible to take both. Iron is used for low blood and calcium is used for high blood. I use only iron and don't use calcium because I have low blood and I don't have high blood. | Primipara, 17 years old, rural |
There was no local term for preeclampsia/eclampsia among pregnant women (or volunteers), and nurses confirmed that women lacked awareness of it. Providers and volunteers used low and high blood terminology during interviews; however, their inability to describe preeclampsia/eclampsia symptomatically could be a significant barrier to motivating utilization of calcium supplements. Most providers suggested counseling on key symptoms or general severity of the condition to motivate women to adhere to calcium.
We have to explain what would happen if they don't take calcium. We have to say they may get edema which also affects their baby, because they don't understand if you say “blood pressure.” – HEW, 24 years old, rural
One‐quarter of women experienced or witnessed others with swelling of the feet or legs in pregnancy, but swelling was attributed to carrying heavy loads, traveling, sitting too long, normal weight gain. Swelling of lower extremities was mostly viewed as normal in pregnancy; only two women felt it warranted treatment, one positing it may be due to dhooftuu (devil attack).
Fewer women knew of swelling of the hands or face in pregnancy. Two women had experienced this condition; one viewed it as serious and deserving of medical attention and had been told delivery was the only solution. Other symptoms not exclusive to preeclampsia (e.g., severe headache, blurred vision, vomiting/nausea) were considered part of pregnancy.
There was almost no awareness of eclampsia or seizures in pregnancy. Several women understood seizures only in relation to epilepsy. Most women, HEWs, and volunteers associated seizures with lack of food intake, nutritional deficiency, and anemia, using the term synonymously with fainting, falling down, and light‐headedness. Some nurses said a cultural belief led women to attribute seizures to “the devil's kick” or “a devil attack.” Only one woman reported knowing a pregnant woman who had lost consciousness after seizing: “People say it is due to pregnancy and it will be cured as the pregnancy ends” (multipara, 31 years old, rural).
Interviewers presented women with calcium supplements, encouraged them to hold, smell, and taste the pills, and described the WHO‐recommended regimen (three supplements daily in addition to IFA) and the purpose and benefits of supplementation. More than half of women reported they would be willing to take calcium in pregnancy as prescribed if advised by a provider. Women who were convinced of the benefits of calcium in preventing potential serious problems in pregnancy did not anticipate difficulties adhering and were less concerned about the quantity of prescribed supplements.
I am willing to take calcium. My child who died because of my delay to seek health care would not have died if I had sought health care on time. Therefore, these tablets will also prevent unnecessary deaths. – Multipara, 31 years old, rural
One‐quarter of women were concerned that taking three or four supplements daily was excessive and could be harmful.
Taking one iron and one calcium per day is possible. But taking three or even two calcium every day would result in an overdose and cause dizziness. It may harm me. – Primipara, 17 years old, rural
A few women expressed concern over pill size; however, most described the supplement as not difficult to swallow.
Providers and volunteers strongly believed that women who were properly counseled and motivated did not face barriers to taking IFA consistently. All women, nurses, and most HEWs thought effective counseling would motivate women to adhere to calcium and IFA.
As with iron, the most important thing to consider for calcium adherence is the provision of good counseling about it. We also must monitor how she is doing and promote use of reminders. For example, associate taking calcium with three routine meals: breakfast, lunch, and supper. – HEW, 25 years old, rural
3.5. Factors influencing sustained adherence
Most women initially stated they never forgot to take their IFA “because of the importance of the supplements.” Providers and volunteers agreed that adherence rates were high. When probed, more than half of women reported occasionally missing doses because they forgot, were away from home, or were busy with household chores or caring for children. Most women who worked on farms were concerned about the combined calcium and IFA regimen.
We may forget to take calcium if it is taken for a long time continuously. It will be difficult to take on time especially when we go out for work all day. – Multipara, 27 years old, rural
All respondent groups felt that strategies such as keeping IFA supplements visible and taking IFA at mealtimes facilitated sustained adherence. Providers and some volunteers reported counseling women to use visual cues and links with other behaviors, approaches they would also recommend for calcium.
[We] advise her to take iron when she gives food to her child because she never forgets to give meals to her child. – Nurse, 24 years old, small town
I advise them to keep iron in a visible place. The coffee cup is kept in front of all other utensils. So, I advise them to keep the tablets together with the cup. – HDA volunteer, 38 years old, small town
Most women also mentioned social support as a critical adherence facilitator and reported receiving general advice from family members during pregnancy, as well as encouragement and reminders to take IFA.
My family encourages me, especially my elder son who reminds me and brings me the tablet with water. – Multipara, 28 years old, rural
Some providers and volunteers recommended women asking husbands and other family members to help them remember their supplements, and a few advocated educating family members directly.
Children and family members should be notified that a woman is taking tablets so they remind her. The husband should be told to remind his wife because children may not always be home. We also have to tell parents that they should support a mother by reminding her. – HEW, 23 years old, rural
Women noted other challenges of taking IFA but indicated they usually did not affect adherence.
People say iron makes the baby grow faster than necessary. I do not think health professionals would give tablets to women if it harms them. I hesitate to accept what people say may be true. – Multipara, 40 years old, rural
Providers reported more barriers to women's adherence.
[Women] say they experience heartburn, vomiting, and loss of appetite when they take the tablets. Some complain they don't have adequate food as tablets are supposed to be taken with a meal. They wonder how they will take all their tablets without access to adequate food. – Nurse, 26 years old, small town
All participant groups anticipated that adding calcium would increase the challenges women currently face with IFA. A few women said adhering to calcium would depend on not experiencing side effects or on seeing positive effects: “If I don't see clear benefits as I do with IFA, I can't take [calcium]” (multipara, 28 years old, rural).
Most women reported being motivated by relief from previous symptoms.
Iron tablets help very much. I am taking it every morning. Since I started taking it, I am cured from my lightheadedness. – Primipara, 20 years old, small town
An important theme that may be context specific was extremely high levels of trust in providers and government health services. Women were very motivated to adhere to providers' recommendations.
I always confide in health professionals and take what they give me…because they are educated about it. They do not give us something that harms us. – Multipara, 45 years old, small town
HEWs acknowledged that women trusted and accepted their advice; however, most perceived some community resistance, noting that if they received more training, they could offer the detailed knowledge valued by women.
4. DISCUSSION
Micronutrient supplementation in pregnancy is vital for the health and survival of mothers and newborns throughout the world, but effective implementation is challenging. This study explored stakeholders' views on ANC and IFA supplementation and likely implications for calcium supplementation, focusing on several key steps in the program impact pathway for antenatal micronutrient supplementation (Figure 1).
4.1. Women's participation in ANC
Early delivery of community‐based preventive micronutrient supplementation is critical for effective control of pregnancy‐related anemia and hypertension. Women valued preventive ANC, many accessing care through health posts but often not attending early in pregnancy. Prevention‐focused motivations for attending ANC should be leveraged to encourage initiation of ANC by 16 weeks. This, combined with raising awareness among health care providers and community members of the importance of nutrition for mothers and babies, can enable timely introduction of supplements.
HEWs are theoretically well‐positioned to deliver community‐based interventions; they are trusted and their work is linked to increased utilization of ANC services and IFA supplementation (Kok et al., 2015; Medhanyie et al., 2012). However, women's reports of HEW unavailability at health posts undercut the convenience of these posts. HEWs emphasized the challenges in balancing the activities required of them, highlighting that appropriate workload and in‐service trainings are critical to credibility and delivery of high‐quality ANC and routine home‐based monitoring. The importance of training and reasonable workloads has been documented in Ethiopia (Wakabi, 2008; Teklehaimanot, 2007); however, more empirical evidence is needed on how expanded workload impacts community‐based worker performance (Kambarami et al., 2016; Naimoli, Perry, Townsend, Frymus, & Mccaffery, 2015). Incorporating calcium supplementation into ANC will require careful consideration of how to deliver this new intervention without displacing current HEW activities.
4.2. ANC‐based transfer of supplements and information
Despite programmatic efforts to strengthen the supply chain and information about IFA in the study area, a few women faced challenges accessing supplements. IFA supplement shortages are a well‐documented global challenge (Galloway et al., 2002), including in Ethiopia (Ejigu, Woldie, & Kifle, 2013). Integrating calcium supplements will require strengthening of procurement and distribution systems at national and subnational levels.
HEWs and women differed in their views on the extent of IFA counseling provided. Women wanted more detail about how supplementation would affect their health and pregnancy. Consistent with other research from Ethiopia, women with minimal knowledge of anemia and the benefits of IFA had lower acceptance and adoption of IFA supplements (Gebremedhin, Samuel, Mamo, Moges, & Assefa, 2014; Sadore, Gebretsadik, & Hussen, 2015). Further research could explore what information women want and how to help providers respond to questions and reassure women. Strong behavior change communication strategies are essential to increase utilization of IFA and calcium supplements (Martin et al., 2017).
Despite lower satisfaction with HEW services, women expressed strong trust in HEWs to act in their best interests. Patient trust predicts use of preventive services and treatment adherence (Thom, Hall, & Pawlson, 2004), so the HEW–client relationship may facilitate introducing calcium supplements. Trust has enhanced adherence to IFA even in the face of cultural beliefs in Ethiopia that IFA can lead to a larger baby and difficult delivery (Galloway et al., 2002; Taye, Abeje, & Mekonen, 2015).
4.3. Women's motivation and likelihood of taking supplements
Anemia knowledge, symptom severity, and feeling better after taking supplements are positively associated with IFA use (Chatterjee & Fernandes, 2014; Souganidis et al., 2012). In contrast to other contexts (Martin et al., 2017; Chatterjee & Fernandes, 2014; Young & Ali, 2005), women in this sample knew about anemia and viewed symptoms as difficult and severe, and their experience of symptomatic relief from IFA motivated adherence. Calcium supplementation does not provide the same type of relief, which a couple women said would affect their willingness to try calcium. Pairing calcium and IFA supplements could enhance acceptability if both become associated with feeling healthier and stronger. Additionally, because women appreciate both the value and the difficulty of obtaining an adequate diet in pregnancy, promoting supplements to address dietary gaps may be motivating.
Relatively low incidence and lack of awareness of preeclampsia/eclampsia present a challenge for increasing women's appreciation of risk. Many providers recommended focusing on the severity of the disease to motivate supplement use.
An unexpected and important emergent theme was confusion regarding the apparent contradiction of simultaneously taking supplements for “low blood” (anemia) and “high blood” (hypertension). Because lay terms for anemia within many contexts refer to blood volume and are accompanied by the belief that IFA consumption increases blood quantity (Alam et al., 2015; Compaore, Gies, Brabin, Tinto, & Brabin, 2014; Galloway et al., 2002), this confusion about taking supplements for too much and too little blood may occur in other settings. Women in our study who understood the preventive purpose of supplementation were more accepting of concurrent supplement consumption and recognized they did not need to be in poor health to benefit from the intervention.
4.4. Factors influencing sustained adherence
Most women were willing to take calcium, although barriers such as side effects, lack of food, supplement size, and concern that multiple daily supplements cause harm (Taye et al., 2015) could affect adherence.
Women reported missing IFA doses due to forgetfulness, workload, or being busy—common reasons for non‐adherence (Gebremedhin et al., 2014). An integrated calcium/IFA regimen with increased dosing events could exacerbate this barrier. Many women felt their schedules were incompatible with taking four supplements daily so simplified regimens should be considered. Few women said side effects constrained their consumption of IFA. Side effects are less often reported with calcium supplementation (Baxter et al., 2014). Even if supplements were begun simultaneously, and side effects from iron were attributed to calcium, these women's reports do not indicate serious interference with adherence.
Participants mentioned visual and behavioral cues as useful IFA adherence strategies. Women received instrumental (reminders, bringing water to take supplements, and completing chores), emotional (encouraging IFA use), and informational (advising them to seek ANC) support from their families. Some providers and volunteers suggested family members be counseled on how to support women to adhere. The importance of family support during supplementation (Tinago, Annang Ingram, Blake, & Frongillo, 2016; Shaw, Golding, & Girard, 2012), and approaches to enhance support could be integrated into behavior change communication materials to promote calcium and IFA adherence (Martin et al., 2017).
4.5. Strengths and limitations
Formative research exploring attitudes and beliefs is a first step in tailoring interventions and is needed in multiple contexts to adapt and adopt interventions. Building on parallel research conducted in Kenya (Martin et al., 2017), this study identified similarities and contrasts between the two settings. Women in both Kenya and Ethiopia complained of lack of access to supplements and information, although availability was much greater in Ethiopia due to recent program strengthening. Side effects of IFA were commonly reported by both groups, but most women said this did not interfere with adherence. The health system contexts differed, with more community outreach in Ethiopia, yet providers strongly desired training on micronutrient supplementation and pregnancy risks in both settings. A few themes that emerged more strongly among women in the Ethiopian context were higher levels of family support and trust in health workers, greater awareness of anemia, and unexpected concerns about concurrent supplementation for both “high blood” and “low blood.”
This purposeful sample was appropriate for in‐depth exploration of women's and providers' perspectives, but small sample size and concentration on a few selected communities limit generalizability of the results. Our primary focus was on women's perspectives; given this and the limited number of providers and volunteers in each community, samples within each cadre of nurses, HEWs, TBAs, and HDA volunteers are particularly small and results must be interpreted with caution. Recruited women reported higher levels of ANC participation and IFA use and adherence than is typical in Ethiopia (Central Statistical Agency, 2014), likely due to recent comprehensive IFA programming in the local area.
Examining these lessons learned from IFA programs can inform the introduction of antenatal calcium supplementation, but further research is needed to explore how attitudes and perceptions related to ANC, IFA, anemia, and preeclampsia influence actual practice. These formative findings guided the design of counseling messages and subsequent household trials research to document women's views after experience with integrated calcium and IFA supplementation. Continued exploration of the influences on implementation and adherence in multiple contexts will facilitate translation of evidence‐based global guidelines on calcium supplementation into effective programs.
5. CONCLUSION
Antenatal IFA supplementation experiences can inform the integration of calcium into ANC. Integration depends on addressing key steps in the program impact pathway including ANC provision and utilization, supplement and information receipt, and adherence barriers and facilitators. Additional challenges for calcium supplementation include quantity of daily supplements, concerns about co‐consumption, and low awareness of preeclampsia. The positive responses to proposed calcium supplementation across respondent groups were encouraging. Women's strong desire for more information on health risks in pregnancy and benefits of antenatal supplements should be addressed through training community‐based providers and volunteers. Communicating the preventive value of ANC, building family support in pregnancy, and strengthening access to IFA and calcium supplements and facility‐ and home‐based support to use them are all critical to address current challenges, expand coverage, and accelerate progress in reducing anemia and preeclampsia.
SOURCE OF FUNDING
Funding for this research was provided by Global Affairs Canada through a grant given to the Micronutrient Initiative (Ottawa Canada).
CONFLICTS OF INTEREST
None declared.
CONTRIBUTIONS
KLD conceptualized the research. KLD, ZB, GMC, and SLM designed the study; GM and ZB coordinated data collection and ensured data integrity; ZB, GMC, and SEO analyzed the data, with all authors involved in data interpretation; ZB, GMC, and KLD drafted the manuscript. All coauthors critically revised the manuscript and approved the final version.
Supporting information
Supporting info item
ACKNOWLEDGEMENTS
We acknowledge critical scientific input from Prof. Rebecca Stoltzfus and Dr. Lanre Omotayo of Cornell University. We thank the participants who contributed their time, trust, and viewpoints to the study and local administrators, health staff, and community members who supported and facilitated field work. We acknowledge the data collection team, including Yohannes Kebede, Mamusha Aman, and Garumma Tolu of Jimma University. Gretchen Seim (University of Wisconsin, Madison) provided technical field assistance during data collection and drafted a report of initial findings; Salma Mutwafy and Edgar Akuffo‐Addo of Cornell University supported data analysis and helped to summarize key themes. Teri Gilleland Scott participated in technical editing of the manuscript.
Birhanu Z, Chapleau GM, Ortolano SE, Mamo G, Martin SL, Dickin KL. Ethiopian women's perspectives on antenatal care and iron‐folic acid supplementation: Insights for translating global antenatal calcium guidelines into practice. Matern Child Nutr. 2018;14(S1):e12424 10.1111/mcn.12424.
REFERENCES
- Alam, A. , Rasheed, S. , Khan, N. , Sharmin, T. , Huda, T. M. , Arifeen, S. E. , & Dibley, M. J. (2015). How can formative research inform the design of an iron‐folic acid supplementation intervention starting in first trimester of pregnancy in Bangladesh? BMC Public Health, 15, 374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter, J. A. , Roth, D. E. , Al Mahmud, A. , Ahmed, T. , Islam, M. , & Zlotkin, S. H. (2014). Tablets are preferred and more acceptable than powdered prenatal calcium supplements among pregnant women in Dhaka, Bangladesh. The Journal of Nutrition, 144, 1106–1112. [DOI] [PubMed] [Google Scholar]
- Bentley, M. E. , Johnson, S. L. , Wasser, H. , Creed‐Kanashiro, H. , Shroff, M. , Fernandez Rao, S. , & Cunningham, M. (2014). Formative research methods for designing culturally appropriate, integrated child nutrition and development interventions: an overview. Annals of the New York Academy of Sciences, 1308, 54–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, M. T. , & Bussell, J. K. (2011). Medication adherence: WHO cares? Mayo Clinic Proceedings, 86, 304–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Central Statistical Agency (2014). Ethiopia Mini Demographic and Health Survey 2014. Ethiopia: Addis Ababa. [Google Scholar]
- Chatterjee, N. , & Fernandes, G. (2014). ‘This is normal during pregnancy’: A qualitative study of anaemia‐related perceptions and practices among pregnant women in Mumbai, India. Midwifery, 30, e56–e63. [DOI] [PubMed] [Google Scholar]
- Compaore, A. , Gies, S. , Brabin, B. , Tinto, H. , & Brabin, L. (2014). “There is iron and iron...” Burkinabè women's perceptions of iron supplementation: A qualitative study. Maternal and Child Health Journal, 18, 1976–1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbin, J. M. , & Strauss, A. (1990). Grounded theory research: Procedures, canons, and evaluative criteria. Qualitative Sociology, 13, 3–21. [Google Scholar]
- Duley, L. (2009). The global impact of pre‐eclampsia and eclampsia. Seminars in Perinatology, 33, 130–137. [DOI] [PubMed] [Google Scholar]
- Ejigu, T. , Woldie, M. , & Kifle, Y. (2013). Quality of antenatal care services at public health facilities of Bahir‐Dar special zone, Northwest Ethiopia. BMC Health Services Research, 13, 443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galloway, R. , Dusch, E. , Elder, L. , Achadi, E. , Grajeda, R. , Hurtado, E. , … Stephen, C. (2002). Women's perceptions of iron deficiency and anemia prevention and control in eight developing countries. Social Science & Medicine, 55, 529–544. [DOI] [PubMed] [Google Scholar]
- Gebremedhin, S. , Samuel, A. , Mamo, G. , Moges, T. , & Assefa, T. (2014). Coverage, compliance and factors associated with utilization of iron supplementation during pregnancy in eight rural districts of Ethiopia: A cross‐sectional study. BMC Public Health, 14, 607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacker, A. N. , Fung, E. B. , & King, J. C. (2012). Role of calcium during pregnancy: Maternal and fetal needs. Nutrition Reviews, 70, 397–409. [DOI] [PubMed] [Google Scholar]
- Hofmeyr, G. J. , Belizan, J. M. , & Von Dadelszen, P. (2014). Low‐dose calcium supplementation for preventing pre‐eclampsia: A systematic review and commentary. BJOG: An International Journal of Obstetrics & Gynaecology, 121, 951–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmeyr, G. J. , Duley, L. , & Atallah, A. (2007). Dietary calcium supplementation for prevention of pre‐eclampsia and related problems: a systematic review and commentary. BJOG: An International Journal of Obstetrics & Gynaecology, 114, 933–943. [DOI] [PubMed] [Google Scholar]
- Joshi, M. , & Gumashta, R. (2013). Weekly iron folate supplementation in adolescent girls—An effective nutritional measure for the management of iron deficiency anaemia. Global Journal of Health Science, 5, 188–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kambarami, R. A. , Mbuya, M. N. , Pelletier, D. , Fundira, D. , Tavengwa, N. V. , & Stoltzfus, R. J. (2016). Factors associated with community health worker performance differ by task in a multi‐tasked setting in rural Zimbabwe. Global Health: Science and Practice, 4, 238–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan, K. S. , Wojdyla, D. , Say, L. , Gülmezoglu, A. M. , & Van Look, P. F. (2006). WHO analysis of causes of maternal death: A systematic review. The Lancet, 367, 1066–1074. [DOI] [PubMed] [Google Scholar]
- Kok, M. C. , Kea, Z. A. , Datiko, D. G. , Broerse, J. E. W. , Dieleman, M. , Taegtmeyer, M. , & Tulloch, O. (2015). A qualitative assessment of health extension workers' relationships with the community and health sector in Ethiopia: Opportunities for enhancing maternal health performance. Human Resources for Health, 13, 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin, S. L. , Seim, G. L. , Wawire, S. , Chapleau, G. M. , Young, S. L. , & Dickin, K. L. (2017). Translating formative research findings into a behaviour change strategy to promote antenatal calcium and iron and folic acid supplementation in Western Kenya. Maternal & Child Nutrition, 13, 1 10.1111/mcn.12233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medhanyie, A. , Spigt, M. , Kifle, Y. , Schaay, N. , Sanders, D. , Blanco, R. , … Berhane, Y. (2012). The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: A cross sectional study. BMC Health Services Research, 12, 352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micronutrient Initiative (2016). What we do: Why iron? Results [Online]. Ottawa: Micronutrient Initiative; Retrieved from http://www.micronutrient.org/what-we-do/by-micronutrient/iron/ [Accessed Nov 16, 2016]. [Google Scholar]
- Naimoli, J. F. , Perry, H. B. , Townsend, J. W. , Frymus, D. E. , & Mccaffery, J. A. (2015). Strategic partnering to improve community health worker programming and performance: Features of a community‐health system integrated approach. Human Resources for Health, 13, 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omotayo, M. O. , Dickin, K. L. , O'Brien, K. O. , Neufeld, L. M. , De Regil, L. M. , & Stoltzfus, R. J. (2016). Calcium supplementation to prevent preeclampsia: translating guidelines into practice in low‐income countries. Advances in Nutrition: An International Review Journal, 7, 275–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peña‐Rosas, J. P. , De‐Regil, L. M. , Garcia‐Casal, M. N. , & Dowswell, T. (2015). Daily oral iron supplementation during pregnancy. The Cochrane Database of Systematic Reviews, 7, CD004736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadore, A. , Gebretsadik, L. , & Hussen, M. (2015). Compliance with iron‐folate supplement and associated factors among antenatal care attendant mothers in Misha District, South Ethiopia: Community based cross‐sectional study. Journal of Environmental and Public Health, 2015, 781973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanghvi, T. G. , Harvey, P. W. , & Wainwright, E. (2010). Maternal iron‐folic acid supplementation programs: Evidence of impact and implementation. Food and Nutrition Bulletin, 31, S100–S107. [DOI] [PubMed] [Google Scholar]
- Shaw, A. , Golding, L. , & Girard, A. W. (2012). Alternative approaches to decreasing maternal anemia: Identifying the need for social marketing strategies to promote iron‐folic acid supplementation in the Peruvian highlands. International Journal of Nonprofit and Voluntary Sector Marketing, 17, 325–333. [Google Scholar]
- Souganidis, E. S. , Sun, K. , De Pee, S. , Kraemer, K. , Rah, J.‐H. , Moench‐Pfanner, R. , … Semba, R. D. (2012). Relationship of maternal knowledge of anemia with maternal and child anemia and health‐related behaviors targeted at anemia among families in Indonesia. Maternal and Child Health Journal, 16, 1913–1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens, G. A. , Finucane, M. M. , De‐Regil, L. M. , Paciorek, C. J. , Flaxman, S. R. , Branca, F. , … Ezzati, M. (2013). Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non‐pregnant women for 1995‐2011: A systematic analysis of population‐representative data. The Lancet Global Health, 1, 70001–70009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoltzfus, R. J. , & Dreyfuss, M. L. (1998). Guidelines for the use of iron supplements to prevent and treat iron deficiency anemia. ILSI Press: Washington, DC. [Google Scholar]
- Taye, B. , Abeje, G. , & Mekonen, A. (2015). Factors associated with compliance of prenatal iron folate supplementation among women in Mecha District, Western Amhara: A cross‐sectional study. The Pan African Medical Journal, 20, 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teklehaimanot, A. (2007). Study of the working conditions for health extension workers in Ethiopia. Ethiopian Journal of Health Development, 21, 246–259. [Google Scholar]
- Temesgen, T. M. , Umer, J. Y. , Buda, D. S. , & Haregu, T. N. (2012). Contribution of traditional birth attendants to the formal health system in Ethiopia: The case of Afar Region. The Pan African Medical Journal, 13, 15. [PMC free article] [PubMed] [Google Scholar]
- Thom, D. H. , Hall, M. A. , & Pawlson, L. G. (2004). Measuring patients' trust in physicians when assessing quality of care. Health Affairs, 23, 124–132. [DOI] [PubMed] [Google Scholar]
- Tinago, C. B. , Annang Ingram, L. , Blake, C. E. , & Frongillo, E. A. (2016). Individual and structural environmental influences on utilization of iron and folic acid supplementation among pregnant women in Harare, Zimbabwe. Maternal & Child Nutrition, 10.1111/mcn.12350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakabi, W. (2008). Extension workers drive Ethiopia's primary health care. The Lancet, 372, 880. [DOI] [PubMed] [Google Scholar]
- World Bank Data Indicators (2011‐2015) . (2016) Maternal mortality ratio (modeled estimate, per 100,000 live births). Retrieved from http://data.worldbank.org/indicator/SH.STA.MMRT (Accessed 28 August 2016). Pregnant women receiving prenatal care (%). Retrieved from http://data.worldbank.org/indicator/SH.STA.ANVC.ZS (Accessed 28 August 2016).
- World Health Organization (2012). Guideline: Daily iron and folic acid supplementation in pregnant women. Geneva: World Health Organization. [PubMed] [Google Scholar]
- World Health Organization (2013). Guideline: Calcium supplementation in pregnant women. Geneva: World Health Organization. [PubMed] [Google Scholar]
- World Health Organization (2016). Micronutrient deficiencies: Iron deficiency anemia [Online]. Geneva: World Health Organization; Retrieved from http://www.who.int/nutrition/topics/ida/en/ [Accessed Nov 16, 2016]. [Google Scholar]
- Young, S. L. , & Ali, S. M. (2005). Linking traditional treatments of maternal anaemia to iron supplement use: An ethnographic case study from Pemba Island, Zanzibar. Maternal & Child Nutrition, 1, 51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting info item


