Abstract
Perinatal depression is highly prevalent in low‐and‐middle‐income countries and has been linked to poor child health. Suboptimal maternal nutrition may be a risk factor for perinatal depression. In this randomised‐controlled trial conducted in rural Malawi, we set out to test the hypothesis that women taking a fatty acid‐rich lipid‐based nutrient supplement (LNS) would have fewer depressive symptoms postpartum than those taking iron‐folate (IFA) or multiple‐micronutrient (MMN) capsules. Women were recruited from antenatal clinics and randomised to receive LNS or MMN during pregnancy and for 6 months postpartum, or IFA during pregnancy only. Maternal depressive symptoms were measured using validated translations of the Self Reporting Questionnaire (SRQ) and Edinburgh Postnatal Depression Scale (EPDS), antenatally (SRQ only) and at 6 months postpartum (SRQ and EPDS). Analysis was by modified intention to treat. One thousand three hundred and ninety one women were randomised (LNS = 462, MMN = 466, IFA = 463). The groups were similar across a range of baseline variables. At 6 months postpartum, 1078 (77.5%) had SRQ completed; mean (SD) scores were LNS 1.76(2.73), MMN 1.92(2.75), IFA 1.71(2.66), P = 0.541. One thousand and fifty seven (76.0%) had EPDS completed; mean (SD) scores were LNS 5.77(5.53), MMN 5.43(4.97), IFA 5.52(5.18), P = 0.676. There were no statistically significant differences between the groups on SRQ or EPDS scores (continuous or dichotomised) in unadjusted or adjusted models. In conclusion, fortification of maternal diet with LNS compared with MMN or IFA did not reduce postnatal depressive symptoms in this study.
Keywords: low income countries, maternal mental health, nutritional interventions, polyunsaturated fatty acids, pregnancy and nutrition, randomised, controlled trial
Introduction
Ten to twenty per cent of women in low‐and‐middle‐income countries (LMIC) experience significant depression or anxiety during pregnancy or the postnatal period (Fisher et al. 2012). Perinatal depression is distressing, disabling and has a negative impact on child health and development (Stewart 2007; Murray & Cooper 1999). In LMIC, perinatal depression has been associated with low birth weight (Patel & Prince 2006; Rahman et al. 2004; Rondo et al. 2003; Nasreen et al. 2010; Niemi et al. 2013), preterm birth (Rondo et al. 2003; Niemi et al. 2013), breastfeeding difficulties (Hanlon et al. 2009; Patel & Prince 2006; Adewuya et al. 2008), increased infant diarrhoeal episodes (Ross et al. 2011; Rahman et al. 2007; Okronipa et al. 2012) and infant growth impairment (reviewed in Surkan et al. 2011). In Malawi, prevalence estimates for major depressive disorder were 10.7% antenatally (Stewart et al. 2014a) and 14% amongst mothers of children (mean age 10 months) brought to a child health clinic (Stewart et al. 2010).
Maternal nutritional deficiencies remain a major health problem in LMIC (Black et al. 2013). Poor nutrition has been identified as a potential risk factor for depression (Rechenberg & Humphries 2013; Leung & Kaplan 2009). There has been particular interest in nutrition and mood in the perinatal period because of the nutritional stresses associated with pregnancy and lactation, and the implications of perinatal depression for infant development. In observational studies, deficiencies in iron, zinc, B‐vitamins and fatty acids have been associated with perinatal depression (Leung & Kaplan 2009). A number of randomised controlled trials (RCT) in LMIC have investigated the impact of nutritional supplementation upon maternal mental health during the perinatal period. A RCT in South Africa showed that iron supplementation for women with mild anaemia during the first postnatal year reduced depressive symptoms (Beard et al. 2005). Multivitamin supplementation (B‐complex, C and E) demonstrated a protective effect on incidence of depressive symptoms in HIV‐infected women recruited in the second trimester of pregnancy in Tanzania (Smith Fawzi et al. 2007). Multiple micronutrient (MMN) supplements led to fewer depressive symptoms compared with low dose iron and folic acid (IFA) supplementation amongst women in the perinatal period in Bangladesh (Frith et al. 2009). However, in a cluster RCT comparing perinatal MMN to IFA supplementation in Indonesia, there was no effect of MMN supplementation on maternal mood despite an improvement in cognitive function (Prado et al. 2012).
Fatty acids play a critical role in neuronal functioning (Bazinet & Layé 2014). In high‐income settings, epidemiological studies have shown an inverse relationship between depressive symptoms and dietary consumption of omega‐3 polyunsaturated fatty acids (n‐3 PUFA) (Appleton et al. 2010). In addition, depression has been associated with low serum levels of n‐3 PUFA (Lin et al. 2010). A number of intervention studies have investigated the effectiveness of fatty acid supplementation in prevention and treatment of depression, including in the perinatal period; the results of these have been mixed (Bloch & Hannestad 2012). To date there have been no trials of fatty acid supplementation conducted in a low‐income setting.
We set out to investigate the impact of fortification of maternal diet with a fatty acid‐rich nutritional supplement on maternal mood in a rural sub‐Saharan African setting. The International Lipid‐based Nutrient Supplement study group, enrolling mother‐child dyads in Malawi (iLiNS‐DYAD‐M) trial was primarily designed to study the impact on child growth of providing a lipid‐based nutrient supplement (LNS) to mothers during pregnancy and the first six months postpartum, and to the children from 6 to 18 months of age. In this study, our objective was to test the a priori hypothesis that women provided with a LNS would have fewer depressive symptoms postnatally than those provided with IFA or multiple micronutrient capsules.
Key messages.
Perinatal depression is highly prevalent in low‐and‐middle‐income countries and has been linked to poor child health.
Suboptimal maternal nutrition may be a risk factor for perinatal depression.
In this randomised controlled trial conducted in rural Malawi, fortification of maternal diet with a lipid‐based nutrient supplement, compared to iron‐folate or multiple‐micronutrient capsules, did not reduce postnatal depressive symptoms.
Materials and methods
The ILINS‐DYAD‐M trial was conducted in Mangochi District, a predominantly rural area situated at the southern end of Lake Malawi. Key economic activities in the district are subsistence farming, fishing and small‐scale business. The trial methodology is described in full elsewhere (Ashorn et al. 2015a). The trial is registered at the clinical trial registry at the National Institute of Health (USA) under identifier NCT01239693 (https://clinicaltrials.gov/ct2/show/NCT01239693).
Participants were recruited from the population of women attending antenatal clinics in the government‐run Mangochi District Hospital, a part‐private hospital (Malindi) and two government‐run health centres (Lungwena and Namwera).
Inclusion criteria were: pregnancy of no more than 20 completed gestation weeks (confirmed by ultrasound), being resident in the defined catchment area and available during the study period, and giving informed consent (signed or thumb print). Exclusion criteria were: age less than 15 years, a chronic health condition requiring regular medical attention, asthma (formally diagnosed and on treatment), a severe illness requiring referral to hospital or emergency medical care, peanut allergy, history of any serious allergic reaction, significant pregnancy complications at enrollment visit, previous recruitment to the trial (during a previous pregnancy) or current enrollment in another clinical trial.
Intervention and comparator arms
The enrolled women were randomly allocated to one of three study arms; the intervention arm (LNS) or one of two comparator arms (IFA and multiple micronutrients (MMN)). Women in the IFA comparator group received supplementation from enrollment to delivery with one capsule per day containing 60‐mg iron and 400‐µg folic acid, as is recommended in standard antenatal care in Malawi. Participants in the MMN control group received one capsule per day that contained IFA plus 16 additional micronutrients. The LNS daily dose (20 g) was designed to contain the same micronutrients as the MMN capsules, plus 4 additional minerals, protein and fat, optimised to provide high amounts of essential fatty acids thought to be important in pregnancy (Coletta et al. 2010). The fatty acids contained in the supplement were 0.59‐g alpha‐linolenic acid (ALA) (42% of RDA in pregnancy and 45% RDA in lactation) and 4.59 g of linoleic acid (LA) (35% of RDA in pregnancy/lactation). The daily LNS dose also provided 118 kcal of energy. The iron dose for participants in the MMN and LNS groups (20 mg/day) was lower than for those in the IFA group (60 mg), because the MMN and LNS supplementation was continued during the first 6 months postpartum, when the recommended iron intake for lactating women is much lower than the recommended antenatal dose (Arimond et al. 2013). Data collectors delivered supplements fortnightly to each participant. At each visit, the data collectors counted and recovered any supplement doses that were unused.
During the trial period, new international guidance advised that LNS used in the management of acute childhood malnutrition be tested for the presence of Cronobacter sakazakii bacteria, with any untested or infected product being withdrawn. In response to this guidance, distribution of LNS to the iLiNS‐DYAD trial participants was suspended until testing had been completed. During this time (1 to 21 August 2012), 160 pregnant women in the LNS arm missed supplement for a period ranging from 1 to 20 days. Of these women, 127 were provided with IFA capsules instead; the other 33 were not located during the IFA distribution.
The study participants attended antenatal and under‐5 clinics according to the same schedule as all other Malawian pregnant women and infants and received all normal preventive services provided by the national health system. Participants were refunded for any medical costs incurred during the study period.
The IFA and MMN interventions were provided using double‐masked procedures: the capsules appeared identical, and neither participants nor the research team members were aware of the nutrient contents of the capsules. For the group receiving LNS (which was easily distinguished from the capsules), we used single‐masked procedures: the data collectors who administered the postnatal depressive symptom outcome measures were blind to group allocation and the participants were asked not to disclose information about which supplement they were taking. Researchers responsible for the data cleaning remained blind to the trial code until the database was fully cleaned.
Randomisation
Randomisation code lists were generated by an independent statistician. At enrolment participants were randomised to trial arm using allocation codes sealed in opaque envelopes. Full details of the randomisation procedure are described in Ashorn et al. (2015a).
Outcome measures
Maternal depressive symptoms were measured using the Self Reporting Questionnaire (SRQ) and the Edinburgh Postnatal Depression Scale (EPDS). The SRQ was designed by the World Health Organisation as a screen for common mental disorders that could be used internationally and particularly in developing countries (WHO 1994). It consists of 20 questions with yes/no answers exploring symptoms of depression, anxiety and somatic manifestations of distress experienced over the previous 4 weeks. Scores are obtained by totaling the number of yes answers, with higher scores indicating higher number of depressive symptoms (possible score range 0–20). Unlike the SRQ, the EPDS was specifically designed for the postnatal period and excludes somatic items (sleep, appetite, energy or other bodily complaints) that might overlap with physical symptoms typical of the perinatal period (Cox et al. 1987). The EPDS consists of 10 questions asking about frequency of symptoms over the last 7 days, each answered from a choice of 4 options, scored 0–3. Scores are obtained by totaling the individual scores on the 10 items, with higher scores indicating higher number and frequency of depressive symptoms (possible score range 0–30). Both measures were validated in the local population (Stewart et al. 2013).
In this study, we used SRQ and EPDS mean scores as primary outcome measures at 6 months postpartum (SRQ and EPDS). The SRQ and EPDS are best analysed as continuous variables to reduce loss of information (Altman & Royston 2006). We also analysed the proportion of women scoring above SRQ ≥ 8 and SRQ ≥ 5, and EPDS ≥13 and EPDS ≥9 cut‐offs. In the earlier validation study, at a cut‐off score of SRQ ≥8 (a cut‐off commonly chosen in previous studies (Harpham et al. 2003)), the SRQ Chichewa version had sensitivity 50.4%, specificity 88.4% and positive predictive value (PPV) of 41.2% for detection of Diagnostic and Statistical Manual of Mental Disorders 4th edition (DSM‐IV) major depressive episode (Stewart et al. 2013). In the same study, at a cut‐off score of EPDS ≥ 13 (the most commonly chosen cut‐off in previous studies (Cox et al. 2014)), the EPDS Chichewa version had sensitivity 33.7%, specificity 94.9% and PPV 50.0%. The test characteristics of the Chiyao translation of the SRQ and EPDS were similar (unpublished data).
Data collectors were trained in the administration of the SRQ and EPDS by a trilingual clinical psychologist (EU) and given written instructions for later reference. At interview, any participant answering yes to the item about suicidal thoughts was asked further questions regarding suicidal ideation. Any participant reporting active or persistent suicidal ideas was referred to local mental health care services (nurse‐led outpatient clinics). During the study, no participants fulfilled this criterion.
Other variables
We measured the following baseline variables: maternal age, number of years of education completed, number of previous pregnancies, household ownership of a set of assets (combined into an index (with a mean of zero and standard deviation of one) using principal components analysis (Vyas & Kumaranayake 2006)), Household Food Insecurity Access (HFIA, a measure of food insecurity), mid‐upper arm circumference (MUAC), weight, height and BMI at recruitment, HIV status, malarial infection and haemoglobin at recruitment, season of enrolment (divided into quarters: Jan–Mar, Apr–Jun, Jul–Sept, Oct–Dec), gestational age at enrolment, antenatal SRQ score (done within 21 days of enrollment) and Multidimensional Scale of Perceived Social Support (MSPSS) score (a measure of the perception of the adequacy of support from others that was translated and locally validated (Stewart et al. 2014b)).
Ethics statement
The trial was conducted according to Good Clinical Practice guidelines and Helsinki Declaration standards. The study was approved by the College of Medicine Research and Ethics Committee, University of Malawi and the Ethics Committee of Pirkanmaa Hospital District, Finland. An independent data safety and monitoring board monitored the study for suspected serious adverse events and performed 2 interim analyses for safety.
Statistical analysis
All presented analyses were pre‐specified either in the trial protocol or in the statistical analysis plan (http://www.ilins.org/ilins-project-research/data-analysis/iLiNS-DYAD-M%20Statistical%20Analysis%20Plan-%20version%2016.0%20with%20appendices%201-19-%202014-12-20.pdf/at_download/file). Analysis was conducted on the principle of modified intention to treat. All randomly allocated participants were included in the analyses, but participants with missing data on an outcome variable were excluded from the analysis of that outcome and two participants whose group allocation was incorrectly transcribed and assigned during enrollment were included in the group corresponding to the actual intervention they received.
The outcome measures (SRQ and EPDS) were administered by data collectors during participant study clinic visits at 6 months postpartum. Data collectors made tracing home visits if a participant did not come for the scheduled visit within 14 days of the appointment. We used outcome data if measured between 22 and 34 weeks following delivery. Data collected outside of these limits were regarded as missing. Occasional missing item values on the SRQ (8 participants) and EPDS (11 participants) were imputed using mean substitution for the same scale and participant. Mean substitution was done if there were <50% missing data points.
Sample size
The sample size was calculated based on the primary study outcomes of birth size and growth at 18 months. Allowing for 20% missing values, with a sample size of 1400 participants the study had 80% power to detect an effect size of 0.24 (difference between groups, divided by the pooled SD) for each continuous outcome. For SRQ and EPDS, this is equivalent to 0.65 and 1.27 points, respectively.
Comparison of continuous SRQ and EPDS scores between the three intervention groups
The group means and standard deviations for SRQ total and EPDS total at 6 month postpartum were tabulated by intervention group. The difference between the three groups was tested with ANOVA and null‐hypothesis of no difference between groups was rejected if P < 0.05.
Comparison of dichotomised SRQ and EPDS scores between the three intervention groups
The proportions of women scoring SRQ ≥5 and ≥8 and EPDS ≥ 9 and ≥13 at 6 month postpartum were tabulated by intervention group. The difference between the three groups was tested with chi‐squared test, and null hypothesis of no differences between groups was tested with global null‐hypothesis rejected if P < 0.05.
Covariate adjustment
In order to adjust for covariates, for the primary continuous outcomes (SRQ total and EPDS total at 6 month postpartum) we constructed linear regression models including antenatal SRQ score, assets score, social support, height, BMI at enrolment, gestational age at enrollment, haemoglobin at enrollment, age, maternal education, number of previous pregnancies, season at enrollment, child sex and twin pregnancy. Categorical variables (study arm and season) were included as dummy variables. Study arm was analysed as two dummy variables, LNS vs. IFA and MMN vs. IFA; season was analysed as three dummy variables, Jan–March, April–June and July–September, with Oct–Dec as reference category. Each regression analysis used multiple imputation with 20 imputations per missing item of data on each covariate using the multivariate normal model based on the relevant dependent variable and all the covariates. We present the mean difference and 95% confidence intervals for the two group comparisons as described above. For the dichotomized outcome measures we adjusted for the same covariates and using multiple imputation for missing data on covariates as described above for the continuous outcome measures. We present odds ratio and 95% confidence intervals for the two group comparisons.
We conducted the main analyses including women who had either singleton or twin deliveries. We repeated the analysis restricting to women who had singleton deliveries. We also conducted a sensitivity analysis that restricted the analysis to the most adherent participants (participants who received and did not return supplements for more than 80% of the antenatal follow‐up days).
Interaction and effect modification
We tested for interaction between the intervention group and variables that could modify the effect of the nutritional intervention on depression outcomes, as per the analysis plan; these were antenatal SRQ score, assets score, social support, height, BMI at enrolment, gestational age at enrollment, haemoglobin at enrollment, age, maternal education, number of previous pregnancies, season at enrollment and child sex. If a statistically significant interaction (P < 0.1) was found, the adjusted analysis was completed as stratified by the respective predictor. All analyses were carried out using SPSS version 22, and Stata version 14.
Results
Between February 2011 and August 2012, 9304 women were approached at the antenatal clinics of the four study sites. Of these, 4449 were excluded and 3470 were not interested in participating (see Fig. 1). 1391 (15.0%) were enrolled to the trial. The flow of participants is shown in Fig. 1. The enrolled participants and those who refused or were not eligible were similar in demographic and socio‐economic characteristics, obstetric history and maternal nutritional status.
Figure 1.
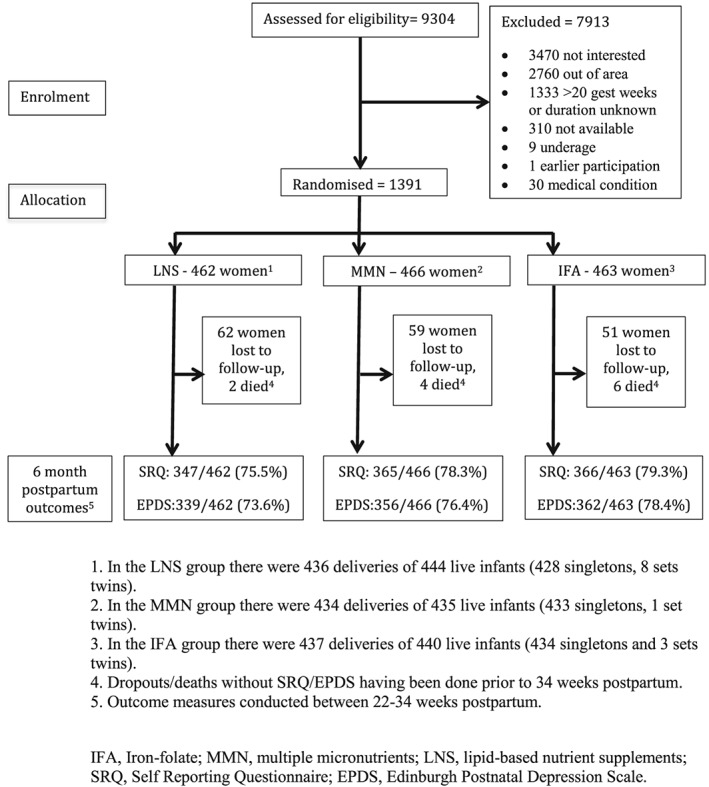
Participant flow.
Participants randomised to each of the three intervention arms (LNS = 462 (33.2%), MMN = 466 (33.5%) and IFA = 463 (33.3%)) were similar across a range of baseline variables (Table 1). Antenatal SRQ was done within 21 days of enrollment for 742/1391 (53.3%) of the participants (LNS = 244/462 (52.8%), MMN = 246/466 (52.8%) and IFA = 252/463 (52.3%)). Statistical testing showed no differences between the groups on any variables. Of the participants, 1078/1391 (77.5%) had data on depressive symptoms for at least one depression outcome. A comparison of those with and without data on depressive symptoms is shown in Table 2. Those without such data were younger, had more years of education and higher assets scores, were later in gestation at enrolment, had had fewer previous pregnancies, were more likely to be primiparous, and had higher BMI and antenatal SRQ scores. There was a trend for more missing data in the LNS arm compared to the other 2 arms but this was not a significant difference (p=0.311).
Table 1.
Baseline/antenatala characteristics of the participating women at enrolment, by study group
| Characteristic | LNS | MMN | IFA |
|---|---|---|---|
| No. of participants | 462 | 466 | 463 |
| Maternal age (years) (Mean (SD)) | 25 (6) | 25 (6) | 25 (6) |
| Maternal education (completed years) (Mean (SD)) | 4.0 (3.5) | 4.1 (3.4) | 3.9 (3.4) |
| Household asset score (Mean (SD)) | 0.04 (1.85) | 0.02 (1.78) | −0.03 (1.78) |
| Proportion with severely food insecure households% | 36 | 38 | 35 |
| Gestational age at enrollment (weeks) (Mean (SD)) | 16.9 (2.2) | 16.8 (2.1) | 16.8 (2.1) |
| Number of previous pregnancies (Mean (SD)) | 2.2 (1.7) | 2.1 (1.8) | 2.1 (1.8) |
| Proportion of nulliparous women, % | 22 | 23 | 20 |
| Height, cm (Mean (SD)) | 156.2 (5.7) | 156.0 (5.6) | 156.1 (5.7) |
| Weight, kg (Mean (SD)) | 54.3 (8.4) | 54.0 (8.1) | 53.9 (7.4) |
| MUAC, cm (Mean (SD)) | 26.5 (2.7) | 26.3 (2.8) | 26.4 (2.4) |
| BMI, kg/m2 (Mean (SD)) | 22.3 (3.0) | 22.2 (2.9) | 22.1 (2.6) |
| Proportion of women with a BMI <18.5 kg/m2, % | 6 | 5 | 6 |
| Blood haemoglobin concentration, g/L (Mean (SD)) | 112 (16) | 111 (16) | 111 (17) |
| Proportion of anaemic women (haemoglobin 100 g/L) % | 21 | 20 | 21 |
| Proportion of women with a positive HIV test, % | 14 | 11 | 16 |
| Proportion of women with positive malaria test (RDT) % | 23 | 24 | 23 |
| Antenatal SRQ score (Mean (SD)) | 3.97 (3.30) | 4.20 (3.27) | 4.04 (3.39) |
| Proportion of women scoring SRQ ≥ 8 antenatally2, % | 16 | 16 | 15 |
| MSPSS score antenatally (Mean (SD)) | 37.6 (8.4) | 37.2 (8.0) | 36.5 (8.9) |
IFA, iron‐folate; MMN, multiple micronutrients; LNS, lipid‐based nutrient supplements; SRQ, Self Reporting Questionnaire; MSPSS, Multi‐dimensional Scale of Perceived Social Support.
Most variables were collected pre‐intervention; household characteristics were done within 1‐week of enrolment; SRQ scores were included if done within 21 days of enrolment (n = 742).
Table 2.
Characteristics of participants with at least one outcome point (SRQ or EPDS score) vs. those missing all outcome data.
| Characteristic | Included | Missing | P‐value a |
|---|---|---|---|
| Number and proportion of participants (%) | 1078 (77.5%) | 313 (22.5%) | |
| Maternal age (years) (Mean (SD)) | 25 (6) | 24 (6) | <0.005 |
| Maternal education (completed years) (Mean (SD)) | 3.8 (3.3) | 4.9(3.8) | <0.005 |
| Household asset score (Mean (SD)) | 0.17(1.65) | 0.73 (2.22) | <0.005 |
| Proportion with severely food insecure households % | 35 | 36 | 0.800 |
| Gestational age at enrollment (weeks) (Mean (SD)) | 16.7 (2.1) | 17.1 (2.1) | 0.005 |
| Number of previous pregnancies (Mean (SD)) | 2.3(1.7) | 1.7(1.8) | <0.005 |
| Proportion of nulliparous women, % | 19 | 33 | <0.005 |
| Height, cm (Mean (SD)) | 156.1 (5.6) | 156.0 (5.7) | 0.388 |
| Weight, kg (Mean (SD)) | 53.9 (7.9) | 54.7 (8.2) | 0.136 |
| MUAC, cm (Mean (SD)) | 26.4 (2.6) | 26.4 (2.9) | 0.781 |
| BMI, kg/m2 (Mean (SD)) | 22.1 (2.7) | 22.5 (3.1) | 0.029 |
| Proportion of women with a BMI <18.5 kg/m2, % | 5 | 6 | 0.330 |
| Blood haemoglobin concentration, g/L (Mean (SD)) | 111.9 (16.1) | 110.1(17.1) | 0.085 |
| Proportion of anaemic women (haemoglobin 100 g/L) % | 20 | 24 | 0.094 |
| Proportion of women with a positive HIV test, % | 14 | 12 | 0.255 |
| Proportion of women with positive malaria test (RDT) % | 23 | 25 | 0.331 |
| Antenatal SRQ score (Mean (SD)) b | 3.9 (3.4) | 4.8 (3.1) | 0.003 |
| Proportion of women scoring SRQ ≥ 8 antenatallyb, % | 15 | 18 | 0.289 |
| MSPSS score antenatally (Mean (SD)) | 37.2 (8.3) | 36.6 (9.1) | 0.269 |
| Proportion of women in trial arm (IFA), arm included vs missing % | 79 | 21 | 0.311 |
| Proportion of women in trial arm 2 (MMN), arm included vs missing % | 78 | 22 | |
| Proportion of women in trial arm 3 (LNS), arm included vs missing % | 75 | 25 |
IFA, iron‐folate; MMN, multiple micronutrients; LNS, lipid‐based nutrient supplements; SRQ, Self Reporting Questionnaire; MSPSS, Multi‐dimensional Scale of Perceived Social Support.
Comparison used the t‐test for scored and continuous data, and Chi squared or Fishers exact test for categorical data.
Antenatal SRQ score done within 21 days of enrolment (n = 742).
Table 3 shows 6 months postpartum mean SRQ and EPDS scores for the three groups, and associated P‐values. Table 4 shows the proportions of 6 months postpartum SRQ scores ≥5 and ≥8 and EPDS scores ≥9 and ≥ 13 for the three groups, and associated P‐values.
Table 3.
SRQ and EPDS total scores (continuous outcomes) by intervention group (model with covariates and using multiple imputation for missing data on the covariates)
| Result by study group | Comparison between LNS and IFA group | Comparison between MMN and IFA group | ||||
|---|---|---|---|---|---|---|
| Variable | LNS | MMN | IFA | P‐valuea | Difference in means (95 % CI) b | Difference in means (95 % CI) b |
| 6 months postpartum SRQ score, mean (SD), n | 1.76 (2.73) n = 347 | 1.92 (2.75) n = 365 | 1.71 (2.67) n = 364 | 0.560 | 0.07 (−0.33 to 0.47) | 0.20 (−0.19 to 0.59) |
| 6 months postpartum EPDS score, mean (SD), n | 5.78 (5.53) n = 339 | 5.43 (4.97) n = 356 | 5.54 (5.18) n = 362 | 0.654 | 0.38 (−0.38 to 1.13) | 0.04 (−0.71 to 0.79) |
IFA, iron‐folate; MMN, multiple micronutrients; LNS, lipid‐based nutrient supplements; SRQ, Self Reporting Questionnaire; EPDS, Edinburgh Postnatal Depression Scale; 95% CI = 95% confidence interval.
ANOVA.
ANCOVAR adjusting for antenatal SRQ score, assets score, social support, height, BMI at enrolment, gestational age at enrollment, haemoglobin at enrollment, age, maternal education, number of previous pregnancies, season at enrollment and twin pregnancy.
Table 4.
SRQ ≥5, SRQ ≥8 and EPDS ≥9 and ≥13 (dichotomous outcomes) by intervention group. Odds ratio for LNS vs. IFA and MMN vs. IFA are presented with 95% confidence intervals.
| Analyses adjusted for covariates | ||||||
|---|---|---|---|---|---|---|
| Result by study group (unadjusted analyses) | Comparison between LNS and IFA group | Comparison between MMN and IFA group | ||||
| Variable | LNS | MMN | IFA | P‐valuea | Odds ratio (95 % CI) | Odds ratio (95 % CI) |
| 6 months postpartum prevalence of SRQ ≥ 5 | 49/347 (14.1 %) | 55/365 (15.1 %) | 49/366 (13.4 %) | 0.808 | 1.08 (0.70 to 1.68) | 1.15 (0.75 to 1.77) |
| 6 months postpartum prevalence of SRQ ≥ 8 | 24/347 (6.9 %) | 21/365 (5.8 %) | 17/366 (4.6 %) | 0.435 | 1.63 (0.85 to 3.15) | 1.32 (0.68 to 2.58) |
| 6 months postpartum prevalence of EPDS ≥ 9 | 94/339 (27.7 %) | 92/356 (25.8 %) | 113/362 (31.2 %) | 0.281 | 0.87 (0.62 to 1.21) | 0.80 (0.57 to 1.12) |
| 6 months postpartum prevalence of EPDS ≥ 13 | 41/339 (12.1 %) | 37/356 (10.4 %) | 43/362 (11.9 %) | 0.747 | 1.12 (0.70 to 1.80) | 0.93 (0.58 to 1.51) |
IFA, iron‐folate; MMN, multiple micronutrients; LNS, lipid‐based nutrient supplements; SRQ, Self Reporting Questionnaire; EPDS, Edinburgh Postnatal Depression Scale; 95% CI = 95% confidence interval
Chi squared test.
There were no statistically significant differences between the groups for either continuous or dichotomised depressive symptom scores in the unadjusted models. Adjustment for covariates did not alter this finding, either on a complete cases analysis or using multiple imputation for missing values on the covariates.
Neither exclusion of women who gave birth to twins or restricting the analysis to only those mothers who had consumed supplements on >80% of days altered the findings.
Of the variables analysed, only number of previous pregnancies was shown to moderate the relationship between study arm and SRQ score at 6 months in an unadjusted model (P = 0.033). Amongst women with 0–2 previous pregnancies, the mean (SD) SRQ scores at 6 months were LNS: 1.48 (2.29), MMN: 2.02 (2.86) and IFA: 1.44 (2.22), (P = 0.026). Amongst women with >2 previous pregnancies, the mean (SD) SRQ scores at 6 months were LNS: 2.07 (3.14), MMN: 1.78 (2.58) and IFA: 2.13 (3.22) (P = 0.558). This moderating effect was not found in an adjusted model.
Discussion
This study tested the hypothesis that women provided with a LNS would have fewer depressive symptoms postnatally than those provided with IFA or multiple micronutrient capsules in rural Malawi. There was no difference between the groups in mean SRQ and EPDS scores at 6 months postpartum. We did not find that antenatal depressive symptoms or antenatal BMI moderated the effect of the intervention upon postnatal depressive symptoms. The study findings do not support the hypothesis that this formulation of LNS reduces postnatal depressive symptoms in the study area. The adjusted effect sizes for LNS vs. IFA are −0.02 for postpartum SRQ and −0.07 for postpartum EPDS, where a positive effect size means that LNS is better than IFA, and a negative effect size means that LNS is worse than IFA. For LNS vs. MMN the adjusted effect sizes are 0.05 and −0.06, respectively. All these effect sizes are regarded as small.
Mean baseline antenatal SRQ score was similar to that in our earlier study conducted in Mangochi district hospital antenatal clinic (Stewart et al. 2014a). In that study, the weighted prevalence of DSM IV major depressive episode was 10.7%, which is consistent with the prevalence estimate of antenatal depression (11.3%) from a meta‐analysis of studies in sub‐Saharan Africa (Sawyer et al. 2010), and indicates that antenatal depression is a common health problem in the study population. In this study, mean SRQ scores postnatally were lower than those antenatally. This is consistent with prospective cohort studies from Ethiopia (Medhin et al. 2010) and Cote d'Ivoire (Guo et al. 2013) in both of which the prevalence of depressive symptoms dropped between pregnancy and the postnatal period.
Strengths of the study included our use of measures of depressive symptoms that had been validated in the study population (Stewart et al. 2013). Confidence in our finding was increased by our use of two outcome measures, the SRQ and EPDS, and our analysis of scores as both continuous and dichotomised variables. The study sample was large, the trial randomisation procedure was robust, and efforts were made to ensure that the outcome data collectors were masked to allocation. We conducted analysis by modified intention to treat, according to a plan that had been published prior to analysis.
A limitation of the study was the high proportion of missing outcome data. Those with no outcome data differed significantly from those included, and there was a trend for more missing data in the LNS arm compared to the other 2 arms although this was not a significant difference. One reason for the high proportion of missing data was a misunderstanding of study protocol by some data‐collectors who, if they found that the participant was not available when they visited to administer the SRQ/EPDS, did not attempt a repeat visit. Multiple imputation for missing data on covariates did not alter the finding of no significant differences between the 3 groups.
This was the first RCT investigating the effect of fatty acid supplementation on maternal postnatal depressive symptoms in a low income country. Fatty acids play an important role in brain function, in particular the n‐3 PUFAs, docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) (Grosso et al. 2014a; Bazinet & Layé 2014). These are obtained in the diet mainly from oily fish. ALA is the precursor of DHA and EPA and is obtained from plant sources. Less than 10% of ALA is converted into DHA/EPA in adults (Burdge & Calder 2005; Gibson et al. 2011) conversion of ALA to DHA/EPA is competitively inhibited by the n‐6 PUFA, LA. In this study, the fatty acids contained in the supplement were 0.59‐g ALA (42% of RDA in pregnancy and 45% RDA in lactation) and 4.59 g of LA (35% of RDA in pregnancy/lactation). For use as a dietary supplement in LMIC, plant‐based fatty acids have advantages of low cost and local acceptability (Arimond et al. 2013). An earlier trial in Ghana suggested that plant‐based fatty acids, and in particular ALA, played an important role in promoting linear growth in children (Adu‐Afarwuah et al. 2007)
Observational and ecological studies have demonstrated an inverse association between depression and both n‐3 PUFA consumption and plasma levels, including in the perinatal period (Appleton et al. 2010; Lin et al. 2010). Most observational studies investigating fatty acids and depression have focused on DHA/EPA, and there have been few studies of ALA. In a 10‐year cohort study of US women, ALA intake was inversely associated with risk of experiencing a depressive episode with an adjusted risk ratio for 0.5 g per day increment of 0.82 (95% CI 0.71–0.94) (Lucas et al. 2011). This association was stronger in women with low LA intake.
There have been a number of intervention studies investigating DHA/EPA supplements for the prevention and treatment of depression. The results of these studies have been mixed, and there is evidence of publication bias toward positive trials (Bloch & Hannestad 2012). Of six trials that have been conducted in the perinatal period, only one open trial found a beneficial effect of n‐3 PUFA supplementation on maternal mood (Grosso et al. 2014b). In the only intervention trial of ALA supplementation and depression, 2 g/day of ALA had no impact on depression post‐myocardial infarction despite increasing EPA blood concentrations (Giltay et al. 2011). Thus, our negative finding was consistent with the majority of previous studies.
A possible explanation for the negative finding is that, as the LNS in this study was not specifically designed to optimise impact on depression, it may have contained a suboptimal formulation of fatty acids to have a beneficial effect on mood. Previous positive studies have used supplements containing fish‐derived DHA/EPA rather than plant based fatty acids (Grosso et al. 2014b). There is some evidence that supplements that have a high proportion of EPA may be most effective; in a meta‐analysis of depression treatment studies, EPA/DHA supplements containing ≥ 60% EPA, in a dose range of 0.2 to 2.2 g/day of EPA in excess of DHA, were more likely to be effective (Sublette et al. 2011). Thus reformulating the supplement with EPA/DHA (with high EPA:DHA ratio) rather than ALA would be an option.
ALA, however, has advantages in terms of acceptability and cost (Arimond et al. 2013) but, in this study, the ALA dose may have been too low. Only a small proportion of ALA is converted to EPA/DHA, although most of the conversion is to EPA, and the process is more efficient in women than men, particularly in those of reproductive age (Burdge & Calder, 2005). We estimate that, to achieve a dose of 0.2 g/day of EPA, at least 2 g/day ALA would be needed. It is also possible that the ratio of LA:ALA (7.8:1) was too high. Observational studies indicate that diets with a high ratio of n‐6 to n‐3 PUFAs are associated with greater risk of depression (Grosso et al. 2014b), possibly as a result of competitive inhibition of ALA metabolism by LA, and the pro‐inflammatory actions of n‐6 metabolites (cf: the anti‐inflammatory effects of n‐3 metabolites) (Marventano et al. 2015). The LNS used in this study was soy oil‐based; reformulation with canola oil would give an LA:ALA ratio of approximately 2 (Gibson et al. 2011). However, Canola is not widely available in many low‐income countries, and this would have implications for cost and sustainability (Arimond et al. 2013).
Alternatively, the negative result may be explained by the inclusion of all women whether they were depressed or not antenatally. Trials of FA supplementation have tended to show positive results in participants with major depression rather than sub‐syndromal depressive symptoms or in those who are well (where the focus is on prevention of incident depression) (Grosso et al. 2014b). We found no interaction between intervention and antenatal SRQ score ≥ 8, suggesting that this explanation is unlikely. However, SRQ score is only a screening measure for depression; use of a diagnostic interview for depression would have improved our confidence in this analysis but was beyond the resources of the study. Loss to follow‐up is also a limitation as mean antenatal SRQ score was higher for those without outcome data than for those included.
Another possible explanation for the negative result is the relatively high dietary intake of fish in the study population. Keenan et al. (2012) showed that baseline FA status is inversely associated with change in FA status following supplementation. It has been suggested that FA supplements may have a beneficial effect on mood only in individuals with poor fatty acid status (Marangell et al. 2003). There is evidence that n‐3 PUFA intake amongst mothers in Mangochi District is adequate because of the inclusion in the diet of small fishes (‘Usipa’) from Lake Malawi (Jimenez et al. 2015).
A nutritional intervention might reduce symptoms of perinatal depression through (1) a direct effect upon brain physiological processes including neurotransmitter synthesis, membrane function and inflammatory processes; (2) an effect on general nutritional status leading to increased energy, fewer infections, reduced obstetric complications, etc.; or (3) by reducing maternal stress through improving infant health. Caring for a sick infant may be a risk factor for common mental disorder (CMD); in particular, there is an association between infant diarrhoeal episodes and CMD symptoms that may be bidirectional (Rahman et al. 2007). It is of note that, in this study, the intervention had no effect on birth outcome (Ashorn et al. 2015a) or infant growth by 6 months (Ashorn et al. 2015b), so a reduction in carer stress would not be expected, although we did not attempt to directly measure this.
Conclusion
In summary, this study did not provide support for LNS fortification of maternal diet as a strategy for reducing depression postnatally in Malawi. As the LNS used was not specifically formulated to have an impact on maternal mood and had no effect on maternal BMI or child growth, a role for an alternative nutritional intervention for perinatal depression cannot be ruled out and further studies are required.
Source of funding
Supported in part by a grant to the University of California, Davis, from the Bill & Melinda Gates Foundation, with additional funding from the Office of Health, Infectious Diseases and Nutrition, Bureau for Global Health, US Agency for International Development (USAID) under terms of Cooperative Agreement No. AID‐OAA‐A‐12‐00005, through the Food and Nutrition Technical Assistance III Project (FANTA), managed by FHI 360. For data management and statistical analysis, the team received additional support in grants from the Academy of Finland (grant 252075) and the Medical Research Fund of Tampere University Hospital (grant 9M004).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
The authors' responsibilities were as follows: KM, PA, KD, UA, BP, EU, RS, FC and AR designed the research; KM, PA, KD, UA, RS and EU conducted the research; RS and BT analysed data; RS wrote the manuscript, with critical input and comments from all other authors; and RS, PA and KM had primary responsibility for final content. All authors read and approved the final manuscript. The findings and conclusions contained within the article are those of the authors and do not necessarily reflect positions or policies of the Bill & Melinda Gates Foundation, USAID, the US government or the other funders.
Acknowledgements
We thank Kenneth H Brown, Jean Bosco Ouedraogo and Andre ´Briend for advice in trial conceptualization, Mary Arimond for iLiNS Project management, Austrida Gondwe and Thokozani Phiri for supervision of data collection, Seth Adu‐Afarwuah for support in study design and logistics, Mark Manary for making a site monitoring visit, Basho Poelman for his contribution to data cleaning, and Lindsay Allen for helping to define the SQ‐LNS formulation and for input at various stages, Fatima Chitimbe and Aisha Milanzi for their role in training and supervising data collectors in use of depression measures.
Stewart, R. C. , Ashorn, P. , Umar, E. , Dewey, K. G. , Ashorn, U. , Creed, F. , Rahman, A. , Tomenson, B. , Prado, E. L. , and Maleta, K. (2017) The impact of maternal diet fortification with lipid‐based nutrient supplements on postpartum depression in rural Malawi: a randomised‐controlled trial. Maternal & Child Nutrition, 13: 12299. doi: 10.1111/mcn.12299.
References
- Adewuya A.O., Ola B.O., Aloba O.O., Mapayi B.M. & Okeniyi J.A.O. (2008) Impact of postnatal depression on infants' growth in Nigeria. Journal of Affective Disorders 108 (1–2), 191–193. [DOI] [PubMed] [Google Scholar]
- Adu‐Afarwuah S., Lartey A., Brown K.H., Zlotkin S., Briend A. & Dewey K.G. (2007) A fat‐based supplement containing essential fatty acids increased plasma alpha‐linolenic acid and linear growth of Ghanaian infants. The FASEB Journal. 21, 223.7.17116743 [Google Scholar]
- Altman D.G. & Royston P. (2006) The cost of dichotomising continuous variables. BMJ 332 (7549), 1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appleton K.M., Rogers P.J. & Ness A.R. (2010) Updated systematic review and meta‐analysis of the effects of n‐3 long‐chain polyunsaturated fatty acids on depressed mood. American Journal of Clinical Nutrition 91 (3), 757–770. [DOI] [PubMed] [Google Scholar]
- Arimond M., Zeilani M., Jungjohann S., Brown K.H., Ashorn P., Allen L.H. et al. (2013) Considerations in developing lipid‐based nutrient supplements for prevention of undernutrition: experience from the International Lipid‐Based Nutrient Supplements (iLiNS) Project. Maternal & Child Nutrition Epub ahead of print. 11 (S4), 31–61, December 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashorn P., Alho L., Ashorn U., Cheung Y.B., Dewey K.G., Harjunmaa U. et al. (2015a) The impact of lipid‐based nutrient supplement provision to pregnant women on newborn size in rural Malawi: a randomized controlled trial. American Journal of Clinical Nutrition 101 (2), 387–397. [DOI] [PubMed] [Google Scholar]
- Ashorn P., Alho L., Ashorn U., Cheung Y.B., Dewey K.G., Gondwe A. et al. (2015b) Supplementation of maternal diets during pregnancy and for 6 months postpartum and infant diets thereafter with small‐quantity lipid‐based nutrient supplements does not promote child growth by 18 months of age in rural Malawi: a randomized controlled trial. The Journal of Nutrition 145 (6), 1345–1353. [DOI] [PubMed] [Google Scholar]
- Bazinet R.P. & Layé S. (2014) Polyunsaturated fatty acids and their metabolites in brain function and disease. Nature Reviews Neuroscience 15 (12), 771–785. [DOI] [PubMed] [Google Scholar]
- Beard J.L., Hendricks M.K., Perez E.M., Murray‐Kolb L.E., Berg A., Vernon‐Feagans L. et al. (2005) Maternal iron deficiency anemia affects postpartum emotions and cognition. The Journal of Nutrition 135 (2), 267–272. [DOI] [PubMed] [Google Scholar]
- Black R.E., Victora C.G., Walker S.P., Bhutta Z.A., Christian P., de Onis M. et al. (2013) Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet 382 (9890), 427–451. [DOI] [PubMed] [Google Scholar]
- Bloch M.H. & Hannestad J. (2012) Omega‐3 fatty acids for the treatment of depression: systematic review and meta‐analysis. Molecular Psychiatry 17 (12), 1272–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdge G.C. & Calder P.C. (2005) Conversion of alpha‐linolenic acid to longer‐chain polyunsaturated fatty acids in human adults. Reproduction, Nutrition, Development 45 (5), 581–597. [DOI] [PubMed] [Google Scholar]
- Coletta J.M., Bell S.J. & Roman A.S. (2010) Omega‐3 fatty acids and pregnancy. Reviews in Obstetrics & Gynecology 3 (4), 163–171. [PMC free article] [PubMed] [Google Scholar]
- Cox J., Holden J. & Henshaw C. (2014) Perinatal Mental Health. The Edinburgh Postnatal Depression Scale (EPDS) Manual (2nd Edition). London, UK: RCPsych Publications. [Google Scholar]
- Cox J.L., Holden J.M. & Sagovsky R. (1987) Detection of postnatal depression. Development of the 10‐item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry 150 (6), 782–786. [DOI] [PubMed] [Google Scholar]
- Fisher J., Cabral de Mello M., Patel V., Rahman A., Tran T., Holton S. et al. (2012) Prevalence and determinants of common perinatal mental disorders in women in low‐ and lower‐middle‐income countries: a systematic review. Bulletin of the World Health Organization 90 (2), 139G–149G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frith A.L., Naved R.T., Ekström E.‐C., Rasmussen K.M. & Frongillo E.A. (2009) Micronutrient supplementation affects maternal–infant feeding interactions and maternal distress in Bangladesh. American Journal of Clinical Nutrition 90 (1), 141–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson R.A., Muhlhausler B. & Makrides M. (2011) Conversion of linoleic acid and alpha‐linolenic acid to long‐chain polyunsaturated fatty acids (LCPUFAs), with a focus on pregnancy, lactation and the first 2 years of life. Maternal & Child Nutrition 7 (Suppl. 2), 17–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giltay E.J., Geleijnse J.M. & Kromhout D. (2011) Effects of n‐3 fatty acids on depressive symptoms and dispositional optimism after myocardial infarction. American Journal of Clinical Nutrition 94 (6), 1442–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosso G., Galvano F., Marventano S., Malaguarnera M., Bucolo C., Drago F. et al. (2014a) Omega‐3 fatty acids and depression: scientific evidence and biological mechanisms. Oxidative Medicine and Cellular Longevity 2014 (7430), 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosso G., Pajak A., Marventano S., Castellano S., Galvano F., Bucolo C. et al 2014b. Role of omega‐3 fatty acids in the treatment of depressive disorders: a comprehensive meta‐analysis of randomized clinical trials, Malaga, G. ed PloS one 9(5), e96905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo N., Bindt C., Te Bonle M., Appiah‐Poku J., Hinz R. et al. (2013) Association of antepartum and postpartum depression in Ghanaian and Ivorian women with febrile illness in their offspring: a prospective birth cohort study. American Journal of Epidemiology 178 (9), 1394–1402. [DOI] [PubMed] [Google Scholar]
- Hanlon C.A., Medhin G., Alem A., Tesfaye F., Lakew Z., Worku B. et al. (2009) Impact of antenatal common mental disorders upon perinatal outcomes in Ethiopia: the P‐MaMiE population‐based cohort study. Tropical Medicine & International Health 14 (2), 156–166. [DOI] [PubMed] [Google Scholar]
- Harpham T., Reichenheim M., Oser R., Thomas E., Hamid N., Jaswal S. et al. (2003) Measuring mental health in a cost‐effective manner. Health policy and planning 18 (3), 344–349. [DOI] [PubMed] [Google Scholar]
- Jimenez E.Y., Mangani C., Ashorn P., Harris W.S., Maleta K. & Dewey K.G. (2015) Breast milk from women living near Lake Malawi is high in docosahexaenoic acid and arachidonic acid. Prostaglandins, Leukotrienes, and Essential Fatty Acids 95, 71–78. [DOI] [PubMed] [Google Scholar]
- Keenan A.H., Pedersen T.L., Fillaus K., Larson M.K., Shearer G.C. & Newman J.W. (2012) Basal omega‐3 fatty acid status affects fatty acid and oxylipin responses to high‐dose n3‐HUFA in healthy volunteers. Journal of Lipid Research 53 (8), 1662–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung B.M.Y. & Kaplan B.J. (2009) Perinatal depression: prevalence, risks, and the nutrition link—a review of the literature. Journal of the American Dietetic Association 109 (9), 1566–1575. [DOI] [PubMed] [Google Scholar]
- Lin P.‐Y., Huang S.‐Y. & Su K.‐P. (2010) A meta‐analytic review of polyunsaturated fatty acid compositions in patients with depression. Biological Psychiatry 68 (2), 140–147. [DOI] [PubMed] [Google Scholar]
- Lucas M., Mirzaei F., O'Reilly E.J., Pan A., Willett W.C., Kawachi I. et al. (2011) Dietary intake of n‐3 and n‐6 fatty acids and the risk of clinical depression in women: a 10‐y prospective follow‐up study. The American Journal of Clinical Nutrition 93 (6), 1337–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marangell L.B., Martinez J.M., Zboyan H.A., Kertz B., Kim H.F.S. & Puryear L.J. (2003) A double‐blind, placebo‐controlled study of the omega‐3 fatty acid docosahexaenoic acid in the treatment of major depression. The American Journal of Psychiatry 160 (5), 996–998. [DOI] [PubMed] [Google Scholar]
- Marventano S., Kolacz P., Castellano S., Galvano F., Buscemi S., Mistretta A. et al. (2015) A review of recent evidence in human studies of n‐3 and n‐6 PUFA intake on cardiovascular disease, cancer, and depressive disorders: does the ratio really matter? International Journal of Food Sciences and Nutrition 66 (6), 611–622. [DOI] [PubMed] [Google Scholar]
- Medhin G., Hanlon C.A., Dewey M., Alem A., Tesfaye F., Lakew Z. et al. (2010) The effect of maternal common mental disorders on infant undernutrition in Butajira, Ethiopia: the P‐MaMiE study. BMC Psychiatry 10, 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray L. & Cooper P.J. 1999. Postpartum depression and child development. [DOI] [PubMed]
- Nasreen H.E., Kabir Z.N., Forsell Y. & Edhborg M. (2010) Low birth weight in offspring of women with depressive and anxiety symptoms during pregnancy: results from a population based study in Bangladesh. BMC public health 10, 515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niemi M., Falkenberg T., Petzold M., Chuc N.T.K. & Patel V. (2013) Symptoms of antenatal common mental disorders, preterm birth and low birthweight: a prospective cohort study in a semi‐rural district of Vietnam. Tropical Medicine & International Health 18 (6), 687–695. [DOI] [PubMed] [Google Scholar]
- Okronipa H.E.T., Marquis G.S., Lartey A., Brakohiapa L., Perez‐Escamilla R. & Mazur R.E. (2012) Postnatal depression symptoms are associated with increased diarrhea among infants of HIV‐positive Ghanaian mothers. AIDS and behavior 16 (8), 2216–2225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V. & Prince M. (2006) Maternal psychological morbidity and low birth weight in India. The British Journal of Psychiatry 188, 284–285. [DOI] [PubMed] [Google Scholar]
- Prado E.L., Ullman M.T., Muadz H., Alcock K.J., Shankar A.H. & SUMMIT Study Group (2012) The effect of maternal multiple micronutrient supplementation on cognition and mood during pregnancy and postpartum in Indonesia: a randomized trial. PloS one 7 (3), e32519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A., Bunn J., Lovel H. & Creed F. (2007) Maternal depression increases infant risk of diarrhoeal illness: a cohort study. Archives of Disease in Childhood 92 (1), 24–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A., Iqbal Z., Bunn J., Lovel H. & Harrington R. (2004) Impact of maternal depression on infant nutritional status and illness: a cohort study. Archives of General Psychiatry 61 (9), 946. [DOI] [PubMed] [Google Scholar]
- Rechenberg K. & Humphries D. (2013) Nutritional interventions in depression and perinatal depression. The Yale Journal of Biology and Medicine 86 (2), 127–137. [PMC free article] [PubMed] [Google Scholar]
- Rondo P.H.C., Ferreira R.F., Nogueira F., Ribeiro M.C.N., Lobert H. & Artes R. (2003) Maternal psychological stress and distress as predictors of low birth weight, prematurity and intrauterine growth retardation. European Journal of Clinical Nutrition 57 (2), 266–272. [DOI] [PubMed] [Google Scholar]
- Ross J., Hanlon C.A., Medhin G., Alem A., Tesfaye F., Worku B. et al. (2011) Perinatal mental distress and infant morbidity in Ethiopia: a cohort study. Archives of Disease in Childhood Fetal and Neonatal edition 96 (1), F59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer A., Ayers S. & Smith H. (2010) Pre‐ and postnatal psychological wellbeing in Africa: a systematic review. Journal of Affective Disorders 123 (1–3), 17–29. [DOI] [PubMed] [Google Scholar]
- Smith Fawzi M.C., Kaaya S.F., Mbwambo J., Msamanga G.I., Antelman G., Wei R. et al. (2007) Multivitamin supplementation in HIV‐positive pregnant women: impact on depression and quality of life in a resource‐poor setting. HIV Medicine 8 (4), 203–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart R.C. (2007) Maternal depression and infant growth: a review of recent evidence. Maternal & Child nutrition 3 (2), 94–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart R.C., Bunn J., Vokhiwa M., Umar E., Kauye F., Fitzgerald M. et al. (2010) Common mental disorder and associated factors amongst women with young infants in rural Malawi. Social Psychiatry and Psychiatric Epidemiology 45 (5), 551–559. [DOI] [PubMed] [Google Scholar]
- Stewart R.C., Umar E., Tomenson B. & Creed F. (2013) Validation of screening tools for antenatal depression in Malawi—a comparison of the Edinburgh Postnatal Depression Scale and Self Reporting Questionnaire. Journal of Affective Disorders 150 (3), 1041–1047. [DOI] [PubMed] [Google Scholar]
- Stewart R.C., Umar E., Tomenson B. & Creed F. (2014a) A cross‐sectional study of antenatal depression and associated factors in Malawi. Archives of Women's Mental Health 17 (2), 145–154. [DOI] [PubMed] [Google Scholar]
- Stewart R.C., Umar E., Tomenson B. & Creed F. (2014b) Validation of the multi‐dimensional scale of perceived social support (MSPSS) and the relationship between social support, intimate partner violence and antenatal depression in Malawi. BMC Psychiatry 14, 180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sublette M.E., Ellis S.P., Geant A.L. & Mann J.J. (2011) Meta‐analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. The Journal of Clinical Psychiatry 72 (12), 1577–1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surkan P.J., Kennedy C.E., Hurley K.M. & Black M.M. (2011) Maternal depression and early childhood growth in developing countries: systematic review and meta‐analysis. Bulletin of the World Health Organization 89 (8), 608–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyas S. & Kumaranayake L. (2006) Construction socio‐economic status indices: how to use principal components analysis. Health Policy and Planning 21 (6), 459–468. [DOI] [PubMed] [Google Scholar]
- WHO 1994. A User's Guide To The Self Reporting Questionnaire (SRQ).


