Abstract
Maternal capabilities—qualities of mothers that enable them to leverage skills and resources into child health—hold potential influence over mother's adoption of child caring practices, including infant and young child feeding. We developed a survey (n = 195) that assessed the associations of 4 dimensions of maternal capabilities (social support, psychological health, decision making, and empowerment) with mothers' infant and young child feeding practices and children's nutritional status in Uganda. Maternal responses were converted to categorical subscales and an overall index. Scale reliability coefficients were moderate to strong (α range = 0.49 to 0.80). Mothers with higher social support scores were more likely to feed children according to the minimum meal frequency (odds ratio [OR] [95% confidence interval (CI)] = 1.38 [1.10, 1.73]), dietary diversity (OR [95% CI] = 1.56 [1.15, 2.11]), iron rich foods, (OR [95% CI] = 1.47 [1.14, 1.89]), and minimally acceptable diet (OR [95% CI] = 1.55 [1.10, 2.21]) indicators. Empowerment was associated with a greater likelihood of feeding a minimally diverse and acceptable diet. The maternal capabilities index was significantly associated with feeding the minimum number of times per day (OR [95% CI] = 1.29 [1.03, 1.63]), dietary diversity (OR [95% CI] = 1.44 [1.06, 1.94]), and minimally acceptable diet (OR [95% CI] = 1.43 [1.01, 2.01]). Mothers with higher psychological satisfaction were more likely to have a stunted child (OR [95% CI] = 1.31 [1.06, 1.63]). No other associations between the capabilities scales and child growth were significant. Strengthening social support for mothers and expanding overall maternal capabilities hold potential for addressing important underlying determinants of child feeding in the Ugandan context.
Keywords: dietary diversity, infant and child nutrition, maternal capabilities, sub‐Saharan Africa, women's empowerment
List of abbreviations
- IYCF
infant and young child feeding
- LAZ
length‐for‐age z‐score
- WAZ
weight‐for‐age z‐score
- WLZ
weight‐for‐length z‐score
- WEAI
Women's Empowerment in Agriculture Index
- BMI
body mass index
1. INTRODUCTION
The majority of essential public health interventions that are necessary to support child survival in low‐income countries, including those aimed at improving child feeding and hygiene practices, target mothers (Bhutta et al., 2013; Matare et al., 2015). Caregiver feeding practices of infants and young children present one important set of modifiable behaviours among mothers and are a common target in behaviour change communication interventions. When effectively delivered, appropriate child feeding can reduce undernutrition, mortality, disruption of cognitive development, and earning losses later in life (Stewart, Ionnotti, Dewey, Michaelsen, & Onyango, 2013).
Effective child feeding and nutrition depends on a variety of influences at the societal, household, and individual levels (Black et al., 2013; World Bank‐UNICEF Nutrition, 2002). Although each of these levels exerts some influence over the available resources for feeding, adequate child feeding requires caregivers to execute a set of complex behaviours (e.g., preparing frequent age‐appropriate complementary foods and feeding a child responsively) that need to be sustained over an extended time (WHO, 2008). Engle, Menon, and Haddad (1999) posited the concept of “Resources for Care” to describe the maternal and household‐level supports necessary for mothers to translate knowledge and skills into caregiving actions for child nutrition and child health. These resources include constructs such as maternal knowledge/beliefs; mental health/stress; control of resources/autonomy; workload/time constraints; social support; and maternal/household health and nutritional status (Engle et al., 1999). More recent efforts have been made to expand this “Extended Model of Care” to describe “caregiver capabilities”—factors that influence a caregiver's ability to care for a young child in a way that produces optimal nutrition, health, and development (Zongrone et al., under review).
A growing body of research links specific maternal level constructs with child feeding practices and nutritional status. Several studies indicate that women in low‐income countries who report constraints on their agency, or decision‐making abilities, are more likely to have children that feed less adequately and who are more likely to be malnourished (Cunningham, Ruel, Ferguson, & Uauy, 2015; Cunningham, Ploubidis, et al., 2015; Shroff, Griffiths, Adair, & Bentley, 2009; Shroff, Griffiths, Adair, & Bentley, 2011). Maternal social support is strongly associated with breastfeeding outcomes, and successful breastfeeding interventions often seek to strengthen social support to improve breastfeeding through peer counselling efforts (Rollins et al., 2016; Tylleskär et al., 2011). A robust literature links maternal depression with poorer feeding and growth (Ashaba, Rukundo, Beinempaka, Ntaro, & LeBlanc, 2015; Surkan, Kennedy, Hurley, & Black, 2011; Surkan et al., 2008).
Establishing methods for measuring maternal factors, including caregiver capabilities, and documenting associations between these capabilities are important for at least two reasons. First, it allows us to understand where constraints among caregivers may impair intervention impact; for example, if low decision‐making capabilities limit the dietary diversity a mother is able to provide, this factor can be strengthened through interventions. Second, we can identify vulnerabilities in caregivers that can benefit from intervention supportive.
This study aimed to expand our understanding of the associations between multiple dimensions of caregiver capabilities and child feeding and nutritional status. Using a tool that was developed using formative research in the specific study context, this study (a) assessed four domains of caregiver capabilities and (b) modelled the associations of these capabilities with infant and young child feeding (IYCF) practices and children's nutritional status. The study was conducted in a rural Ugandan District where poor IYCF practices and a high burden of undernutrition have been previously documented (Uganda Bureau of Statistics (UBOS) & ICF International Inc., 2012; Ickes et al., 2017) and where mothers experience multiple constraints to their capabilities to provide care to support children's nutrition and development (Ickes, Heymsfield, Wright, & Charles, 2016).
Key messages.
Most interventions aimed at improving child malnutrition target mothers. This necessitates an understanding of the relationship between maternal capabilities, feeding practices, and child nutrition.
The creation of scales for social support, psychological well‐being, decision‐making, freedom/empowerment, and a composite index of maternal capabilities provide a baseline for adaptation and refinement in further studies that examine the relationship between maternal capabilities and child nutrition and health outcomes.
Although this study did not find significant associations between maternal capabilities and nutritional status, there were consistent associations between capabilities and IYCF practices. Social support and freedom/empowerment were most predictive of improvements in IYCF practices.
2. METHODS
2.1. Participants and setting
The study was conducted in the 261,000‐person Bundibugyo District in western Uganda, situated west of the Rwenzori Mountains and east of the Democratic Republic of Congo. Subsistence farming is the main livelihood. Twenty percent of women receive no education, and the national fertility rate of 6.2 live births per woman. Women in the western region are the youngest in the country to marry (median age at first birth is 17.1 years) and are also the most likely to be in a polygynous marriage with two or more co‐wives (11%). Over one fifth (21.9%) of women in Uganda have experienced sexual violence in their lifetime (UBOS & ICF International, 2017). Mountain regions of Uganda have a substantially higher prevalence of stunting (height‐for‐age z‐score < −2) compared to the national mean (36.5 vs. 28.9%; UBOS & ICF International, 2012; UBOS & ICF International, 2017). Stunting rates also have a sharp education gradient, with a prevalence of 37% among mothers with no education (UBOS & ICF International, 2017).
2.2. Survey development
The survey (Data S1) was developed through formative research conducted in the previous year in the same community, and through a review of literature of relevant scales in low‐income country contexts, with priority given to scales that had been applied in sub‐Saharan Africa (Oxford Poverty and Human Development Initiative, 2015; Samman, 2007; Ibrahim & Alkire, 2007). The formative research sought to determine the events and processes in the community that shaped maternal capabilities in this Uganda District, and to define the relevant caregiver capabilities in this context (Ickes et al., 2016). The survey assessed four domains of maternal capabilities (social support, psychological well‐being, decision making, and freedom/empowerment), as well as IYCF practices and child nutritional status. Nutritional status and IYCF practice measurements were adapted from the 2011 Uganda Demographic and Health Survey and the WHO Indicators for IYCF (UBOS & ICF Macro 2012; WHO, 2008).
2.3. Survey domains of caregiver capabilities
2.3.1. Social support
The 10 questions on the social support scale were assessed using a 5‐point scale. Women were asked to express the level to which they agreed or disagreed with a series of statements about the level of the support they feel is generally available to them. Respondents were given five possible response options that ranged from “strongly agree” to “strongly disagree.” The social support scale primarily assessed instrumental (e.g., help from her family; help from friends; being able to count on others when things go wrong) and emotional support (e.g., whether the mother felt she had a special person that provided her with comfort; support in her feelings; the ability to discuss problems and decisions with her family; and supportive and dependable friends). The social support subscale was adapted from the Duke‐UNC Functional Social Support Questionnaire (Broadhead, Gehlbach, De Gruy, & Kaplan, 1988).
2.3.2. Psychological well‐being
Mothers were asked to rate their level of satisfaction for a variety of attributes: life overall, food, housing, income, health, work, perceived safety (personal and community), freedom from physical violence, education, dignity, their ability to help others, and freedom to express their spiritual beliefs. The scale assessed 16 items using 4‐point Likert‐type scale questions that ranged from very satisfied to not at all satisfied. This subscale was developed based on guidance for developing a personal well‐being index, taken from the OECD Guidelines on Measuring Subjective Well‐being (2013).
2.3.3. Decision making/agency
This scale contained fourteen 5‐point Likert‐type scale items that assessed the respondent's agreement with statements about how her opinions were respected in household and financial decisions; whether she felt confident in her ability to make good choices for her children; whether she felt she had control over her family size; and the timing of conceiving a child. The decision‐making subscale included four questions on health‐related decision making that consisted of four 4‐point Likert‐type scale questions that assessed agreement about the respondent's ability to help their children in the case of a serious health problem, the degree to which her health‐related actions were made to meet the expectations of other people; and their freedom to exert personal agency when making decisions for their personal health. This subscale was taken from the power to/choice component of the Ibrahim and Alkire's proposal for internationally comparable measures of agency empowerment and was designed to measure household decision making and domain‐specific autonomy (2007).
2.3.4. Overall freedom/empowerment
This scale asked mothers to imagine a 10‐step ladder where the first step represented people who are completely without free choice and control over the way their lives turn out and where the highest step represented people with the greatest choice and control over their lives. Using this visual, mothers indicated (a) which step they were on today, (b) the step that they were on 5 years ago, (c) the step their neighbours were on, and (d) the step they will be on in 1 year. Participants were given a score of “0” if they were on Step 3 or below, and “1” if they were on Step 4 or higher for their current position on the ladder. A score of “1” was given if participants projected to be on a higher step than 5 years ago, and “0” if otherwise. A score of “1” was given to respondents who were at the same step or higher than their neighbours, and “0” if otherwise. A score of “1” was given if participants projected to be on a higher step 1 year from now, and “0” if otherwise. This scale also used a single yes/no question to ask mothers whether they felt that they, or others similar to them, could change things in their community if they wanted. The concept for this scale was adapted by Ibrahim and Alkire from Cantril's Self‐Anchoring Striving Scale, which has been applied in a variety of countries and measures judgement and life evaluation (Cantril, 1965; Deaton, 2008; Diener & Ryan, 2009).
2.4. Assessment of IYCF practices and construction of indicators
We constructed the four of the eight core IYCF indicators specified by the World Health Organization: minimum meal frequency; minimum dietary diversity; consumption of iron‐rich or iron‐fortified foods; and feeding a minimally acceptable diet (WHO, 2008). All dietary data were based on caregiver reports of feeding practices in the 24 hr preceding the survey. Children were classified as breastfed if the caregiver reported that the child was breastfed at least once in the 24 hr preceding the survey. Feeding frequency for breastfed children included only nonliquid feeds, whereas feeding frequency for nonbreastfed children included both milk feeds and solid/semisolid feeds. Consumption of any amount of food from each food group was sufficient to be counted. In addition, we constructed the four additional core IYCF indicators (early initiation of breastfeeding; exclusive breastfeeding to 6 months; continued breastfeeding at 1 year; and timely introduction of complementary foods). We report the frequency of feeding according to these indictors but do not include these in regression analysis due to an insufficient sample size of children in the relevant age categories for these variables.
2.5. Child anthropometry assessment
Children were weighed to the nearest 0.1 kg using a lightweight electronic SECA scale, and mothers were weighed using a digital standing scale and measuring tape on a flat surface (a packed clay, cement, or brick entryway) at the caregiver home. Infants (0–11 months) were weighed with their mothers, and then the mother's weight was subtracted to obtain infant weights. Child lengths under 24 months were obtained using the length board on the SECA scale; whereas children 24 months and over were measured while standing, using a wooden measuring board with an affixed tape (Shorr Productions, n.d., Olney, MD). Height/length was measured to the nearest 0.1 cm. Underweight (weight‐for‐age z‐score < −2), stunted (height‐for‐age z‐score < −2), and wasted (weight‐for‐length z‐score < −2) were defined based on the WHO Multicentre Growth Reference Study Standards (WHO, 2008). Adult body mass index (BMI) was assessed as height in meters squared divided by weight in kilograms (Figure 1).
Figure 1.
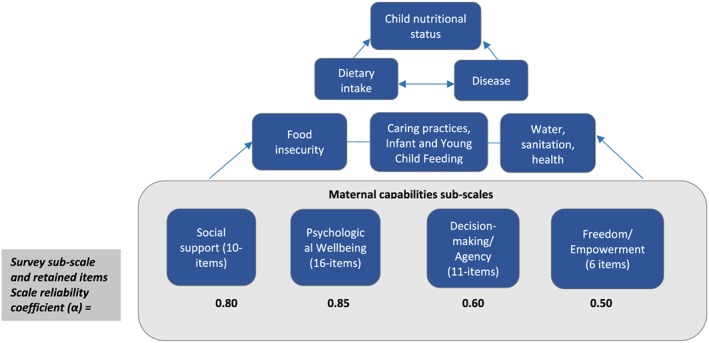
Conceptual framework and scale reliability coefficients for maternal capabilities sub‐scales
2.6. Survey procedures and sample size estimation
The research team visited 10 villages and two peri‐urban centres in the southern portion of Bundibugyo district. We sampled households from three of Bundibugyo's five subcounties: Nyahuka, Busaru, and Ndugutu. These subcounties were selected based on being the primary catchment areas for current community‐based nutrition programs in the district, and relative low socioeconomic status in relation to the more developed Bundibugyo town center. Ndugutu lacks a peri‐urban center, so we selected four villages at random from the eight total villages in the subcounty. In Busaru and Nyahuka, we sampled the only peri‐urban center within each subcounty, and two more remote villages, also selected at random. Given that the Bundibugyo District has been the site of district‐wide nutrition sensitization programs in recent years (e.g., the World Vision Campaign Against Chronic Hunger), the sampling method is unlikely to have introduced selection bias. Further, one purpose of the study was to provide results for the nongovernmental organizations that are active in the subcountries that participated in this study.
We applied the random walk method and set out in two research teams from the village or peri‐urban center (USAID, 2008). We surveyed all caregivers with a child under 24 months, aiming for 65 maternal‐child dyads per subcounty (approximately 195 in total). A total sample size of 195 children provides 92.6% power using a one‐sided test and 96% power using a two‐sided test (α = 0.05) to detect a 20 percentage point difference in the proportion of children who met anthropometric outcomes. The sample of 163 children aged 6 to 23 months was sufficient to detect a 20% difference in the proportion of caregivers who fed according to IYCF practices with over 80% power. Participants were approached at their homes and at health centres by study staff. Inclusion criteria required that the mothers interviewed have a child 3 years or younger for whom they were the primary caretaker. After providing verbal informed consent, interviews were conducted in English through Ugandan translators who reside in the Bundibugyo District, or in the local language, and the mother and the youngest child were weighed and measured. Surveys were conducted between June and July 2014. All surveys were administered in Labwisi or Lukonjo, the two predominant local dialects, depending on caregiver preference, and lasted approximately 40 min.
2.7. Scale development
Survey results were analysed in STATA version 14.0 (College Station, TX). We compiled continuous scales of the summary of responses from each of the survey subscales. Items were selected for the final subscales through sequential elimination of the least reliable items. To accomplish this, we first applied a principal components analysis to each subscale. Scree plots were used to identify the number of substantially important factors in the subscale. Next, using an eigenvalue plot, we identified the main items involved with the most important factors for each scale. Cronbach's alpha was calculated to examine how the elimination of the least reliable items affected the internal consistency of the scale. No items were removed from the social support, psychological health, or freedom/empowerment scales.
Three of the 14 items (comfort with the way husband spends money, acceptability of a husband forcing sex, and feeling a need to act in a way that others insist) were removed from the decision‐making scale to construct an 11‐item scale (Table 1). Following item selection, the score on each subscale was simplified into a 5‐point range that divided the respondents approximately into quintiles. Next, a summary index of caregiver capabilities was calculated through the addition of the four subscales to develop a scale with a range of 4 to 20. Distribution plots of the scales (Data S2) were left unstandardized given the relatively normal distributions of each scale, and to ensure meaningful interpretation of regression results.
Table 1.
Scale properties for maternal capabilities measurement domains
| Scale domain | Items in final scale | Scale range | Mean score (SE) | Cronbach's alpha | Inter‐item covariance |
|---|---|---|---|---|---|
| Social support subscale | 10 | 10 to 50 | 33.8 ± 0.5 | 0.80 | 0.45 |
| Psychological well‐being subscale | 16 | 16 to 64 | 44.7 ± 0.6 | 0.85 | 0.23 |
| Decision‐making subscale | 11 | 11 to 51 | 32.5 ± 0.3 | 0.60 | 0.15 |
| Freedom/empowerment sub‐scale | 5 | 1 to 5 | 2.7 ± 0.08 | 0.49 | 0.03 |
| Summary maternal capabilities composite index | 4 | 4 to 20 | 11.6 ± 0.3 | 0.50 | 0.48 |
2.8. Statistical analysis
Each subscale and an overall composite scale were used in unadjusted logistic and linear regression models to assess the relationship between each subscale of maternal capabilities and IYCF practices and child nutritional status. Due to the exploratory nature of the research question, we did not apply a multiple comparisons adjustment to the significance testing. Results were considered significant if p < .05 for regression results. Multivariable logistic and linear regression models included all mothers with complete anthropometric and survey data. We report adjusted regression results that control for maternal education, distance to water source, becoming pregnant as an adolescent, and the ownership of mobile phones. Model selection began with a larger set of theoretically relevant confounders that were not on the causal path between capabilities and IYCF/anthropometry and were theorized to be associated with both the exposure (maternal capabilities) and the outcomes (feeding practices and nutritional status). We then used a backward selection technique to construct the most parsimonious models.
2.9. Ethical approval
The Ministry of Health at the Mbale Regional Hospital Institutional Review Committee and [redacted for review] approved the study.
3. RESULTS
3.1. Participant characteristics
One hundred ninety‐five mothers were surveyed. No caregivers refused participation. Table 2 describes the demographic characteristics and IYCF practices of the sample. Children were 14.7 (SE = 0.5) months, on average. A large majority of mothers (91.7%) exclusively breastfed their children under 6 months old, whereas 74.4% continued to breastfeed children through 1 year. Between 6 and 12 months, 91.5% of mothers had introduced complementary foods to children's diets. Among children ages 6 to 23 months, fewer than half met their indicator for the minimum meal frequency (40.5%), whereas 22.1% met the minimum dietary diversity indicator, and 15.3% were fed a “minimally acceptable diet.”
Table 2.
Demographic characteristics, feeding practices, and nutritional status of study participants (n = 195)a
| Child age | Percent (number) |
|---|---|
| 0 to 5 months | 6.2% (12) |
| 6 to 11 months | 39.5% (77) |
| 12 to 17 months | 45.1% (88) |
| 18 to 24 months | 9.2% (18) |
| Nutrition status among children 0 to 24 monthsi | |
| Underweight (weight‐for‐age z‐score < −2) | 26.2% (51) |
| Stunted (length‐for‐age z‐score < −2) | 49.7%(97) |
| Wasted (weight‐for‐length z‐score < −2) | 12.8% (25) |
| Sociodemographic factors | |
| Adolescent mother (age at first birth was 16 or younger) | 67.2% (131) |
| Husband of respondent has multiple wives | 38.5% (75) |
| Married/living together with partner | 87.2% (170) |
| Caring for 5 or more children | 45.1% (88) |
| Number of children cared for by mother (mean [SE]) | 4.6 (0.2) |
| Number of biological children per mother (mean [SE]) | 3.3 (0.2) |
| Adolescent mother (age at first birth was 16 or younger) | 67.2% (131) |
| Lives 400 m or more meters from water source | 51.3% (100) |
| Owns a mobile phone | 42.1% (82) |
| Maternal education | |
| None | 19.0% (37) |
| Some primary/complete primary | 72.3% (141) |
| Some secondary and above | 8.7% (17) |
| Feeding practices | |
| Exclusive breastfeeding to 6 months (0 to 6 months, n = 12)b | 91.7% (11) |
| Continued breastfeeding at 1 year (12–18 months, n = 43)c | 74.4% (32) |
| Timely introduction of complementary foods (6–9 months, n = 47)d | 91.5% (43) |
| Fed minimum dietary diversity (6–23 months, n = 163)e | 22.1% (36) |
| Fed iron‐rich foods or iron fortified products (6–23 months, n = 163)f | 9.5% (16) |
| Fed minimum meal frequency (6–23 months, n = 163)g | 40.5% (66) |
| Fed minimally adequate diet (6–23 months, n = 163)h | 15.3% (25) |
Data analysis included all maternal and child dyads with complete dietary intake data among children 0 to 23 months.
Exclusive breastfeeding defined as breastfed by the mother, a wet nurse, or fed expressed breast milk exclusively for the first 5 months of life.
Continued breastfeeding defined as breastfed by the mother, a wet nurse, or fed expressed breast milk from 12 to 15 months of age.
Introduction of complementary foods defined as the introduction of solid, semisolid, or soft food from 6 to 9 months of age. Children with missing dietary diversity data omitted.
Minimum meal frequency defined as two times per day for breastfed infants 6–8 months, three times per day for breastfed children 9–23 months, and four times per day for nonbreastfed children 6–23 months, during the previous 24‐hr period.
Minimum dietary diversity of feeding from four or more of the following food groups during previous 24 hr: grains, roots and tubers; legumes and nuts; dairy products (milk, yogurt, and cheese); flesh foods (meat, fish, poultry, and liver/organ meats); eggs; vitamin A‐rich fruits and vegetables; other fruits and vegetables.
Iron intake includes the ingestion of iron‐rich foods such as flesh foods (meat, fish, and liver) as well as iron‐fortified foods that are specially designed for infants and young children, or is fortified in the home.
Minimum acceptable diet (apart from breast milk) defined for breastfed children as having the minimum dietary diversity and the minimum meal frequency during the previous day. Nonbreastfed children must have been fed at least two milk feeds and be fed the minimum feeding frequency in the previous 24 hr.
Anthropometric indices were calculated using the WHO Multi‐Centre Growth Reference Standards (WHO, 2006).
Approximately half of the children in the sample were stunted (49.7%), whereas 12.8% were wasted and 26.2% were underweight. Most women were married or living with their husbands or partners (87.2%); however, 38.5% reported that their husbands maintained multiple concurrent wives. Nearly one third of mothers were overweight (BMI ≥ 25), and 4.6% were underweight (BMI < 18.5). Mothers were 26.1 (SE = 0.5) years old on average. Two thirds (67.2%) of mothers gave birth to their first child before the age of 18. Only 8.7% of mothers had any secondary education; nearly one fifth (19.0%) reported no formal education.
Correlation between the four binary scales was low to modest. The strongest correlations were between social support and psychological health (0.44), social support and decision making (0.40), and decision making and psychological health (0.35). All other correlations were ±0.24 or below. Histograms of the subscales and overall capabilities scale response ranges are provided in Data S3.
3.2. Social support scale
The mean value (95% confidence interval [CI]) of the 40‐point social support scale was 33.8 (32.7, 34.8), whereas the mean value (95% CI) of the 5‐point quintile scale was 2.9 (2.7, 3.1). The mean score on the 40‐point social support scale was 33.8, and the scale was completed for 192 of 195 mothers (98.5%). Over two thirds of mothers agreed that they know someone who is around when they are in need (68.4%), or who cares about their feelings (70.5%). Fewer mothers agreed that their families were “trying to help them” (53.9%), or that they could discuss their problems (57.5%) or decisions (46.6%) with their families. Although 76.2% of mothers reported having a friend with whom to share joys and sorrows, less than half (49.2%) of mothers indicated that friends were trying to help them, whereas only one third could count on their friends in a time of need.
3.3. Psychological satisfaction scale
The full sample of mothers completed the psychological satisfaction scale (n = 195). Eighty‐one percent of mothers had freedom to express spiritual beliefs, whereas over half (56%) had an ability to help others. Nearly three quarters (72%) expressed an overall sense of safety in their communities and were satisfied with the amount of dignity that they felt (78%); just over half (52%) were satisfied with the amount of freedom they had to make choices. Only 8% of mothers were satisfied with their level of education. The mean value (95% CI) of the 60‐point psychological health scale was 44.7 (43.5, 45.8). When categorized as a 5‐point scale, the mean (95% CI) value was 3.0 (2.8, 3.2).
3.4. Decision‐making scales
The decision‐making capabilities scale assessed general (seven questions) and health‐related decision making (four questions).
3.4.1. General decision making
The majority (59%) of mothers reported that their opinion was respected if their husband disagreed with them about money. Eighty percent indicated that if she and her husband disagreed about how money was spent, he would make the final decision. Over half (56%) of mothers agreed that they wish they could use more of the money that they have on food for their children.
A high proportion (85%) of mothers felt confident in their abilities to make good choices for their children, whereas only 27% of mothers felt free to disagree with their mother‐in‐law if they had a different opinion about how to care for children. Less than two thirds (62%) of mothers felt that they had control over the number of children to have, and 57% had control of when to have another child. A majority (86%) believed it was inappropriate for her husband to beat her.
3.4.2. Health‐related decision making
Fewer than a third (28.2%) of mothers were classified as possessing moderate to high health‐related decision‐making capabilities. A majority (86%) of mothers reported that they did what they considered important if they had a personal health problem, whereas only 33% reported that they were free from seeking approval from others when making a health‐related decision for their child. Only 22% of mothers felt that if their child had a serious health problem, they were free to act independently and not forced to do what a friend or relative insisted. Almost half (46%) of mothers reported that if their child had a serious health problem, they have no other way to help them other than what they do now. When combined into one scale, the mean value for the 44‐point decision‐making scale was 32.5 (32.2, 32.8). When categorized as a 5‐point scale, the mean (95% CI) value for the decision‐making scale was 3.0 (2.8, 3.2).
3.5. Freedom/empowerment scale
A visual 10‐step ladder scale measured overall freedom/empowerment. Mothers who self‐reported a score of Step 3 or below were ranked as possessing “low empowerment” (56.4%); those Step 4 and above were classified as “moderate to high empowerment” (85 mothers, 43.6%). Nearly three quarters (74.4%) placed their neighbours on a higher step than themselves. Compared to 5 years prior, most mothers (76.9%) felt that they were currently either on the same step or higher on the ladder. The 5‐point quintile scale of freedom/empowerment had a mean (95% CI) of 2.7 (2.5, 2.8).
3.6. Composite index of maternal capabilities
We constructed a composite index from the four component subscales of maternal capabilities (social support, decision making, psychological health, and freedom/empowerment). The scale ranged from 4 to 20, derived from the summation of the four binary scores from each subscale. The mean score (95% CI) was 11.6 (11.1, 12.2). This scale was then divided into a 5‐point index for use in regression models. The overall mean (95% CI) for the five‐category quintile scale for overall empowerment was 2.9 (2.7, 3.1).
3.7. Logistic regression analysis of maternal capabilities scales and IYCF practices
Table 3 reports the associations between maternal capability scales and IYCF practices. Apart from the timely introduction of complementary foods, which was met by nearly all children in the study, mothers with greater social support were more likely to meet the four remaining complementary feeding indicators. For example, each unit increase in social support was associated with a higher odds of feeding the minimum number of times per day (odds ratio [OR] [95% CI] = 1.38 [1.10, 1.73]), the minimum dietary diversity (OR [95% CI] = 1.56 [1.15, 2.11]), and a minimum acceptable diet (OR [95% CI] = 1.55 [1.10, 2.21]). No significant associations were observed between the psychological health or decision‐making subscales. A higher score on the freedom/empowerment subscale was associated with higher odds of feeding the minimum dietary diversity (OR [95% CI] = 1.62 [1.11, 2.36]) and a minimally acceptable diet (OR [95% CI] = 1.65 [1.10, 2.52]).
Table 3.
Adjusted logistic regression coefficients (odds ratios) of predictive power of maternal capabilities scale characteristics on infant and young child feeding practices (n = 163)a , b
| Maternal construct | Fed minimum times per day | Fed minimum dietary diversity | Fed iron rich foods or iron fortified products among children | Fed minimum acceptable diet among children |
|---|---|---|---|---|
| Social support subscale | 1.38 (1.10, 1.73)** | 1.56 (1.15, 2.11)** | 1.47 (1.14, 1.89)** | 1.56 (1.10, 2.21)* |
| Psychological well‐being subscale | 1.12 (0.90, 1.39) | 0.93 (0.71, 1.21) | 1.12 (0.90, 1.41) | 0.90 (0.66, 1.21) |
| Decision‐making subscale | 1.08 (0.87, 1.36) | 1.06 (0.80, 1.41) | 0.97 (0.76, 1.23) | 1.10 (0.79, 1.52) |
| Freedom and empowerment subscale | 1.23 (0.92, 1.64) | 1.62 (1.11, 2.36)* | 1.05 (0.78, 1.43) | 1.65 (1.10, 2.52)* |
| Composite maternal capabilities index | 1.29 (1.03, 1.63)* | 1.44 (1.06, 1.94)* | 1.27 (0.99, 1.63) | 1.43 (1.01, 2.01)* |
Values are odds ratios (95% confidence intervals).
Analysis includes all children 0 to 23 months with complete anthropometric, child feeding data, and maternal capabilities scale survey data (n = 163). Results control for maternal education, distance to water source, becoming pregnant as an adolescent, and ownership of mobile phones.
p < .05,
p < .01.
The overall composite scale of capabilities was significantly associated with multiple IYCF indicators. A higher score on the 5‐point index was associated with higher odds of feeding the minimum meal frequency (OR [95% CI] = 1.29 [1.03, 1.63]), dietary diversity (OR [95% CI] = 1.44 [1.06, 1.94]), and feeding a minimally acceptable diet (OR [95%] = 1.43 [1.01, 2.01]).
3.8. Logistic regression analysis of maternal capabilities scales and anthropometry
Associations between maternal capabilities scales and categorical measures of nutritional status (stunting, wasting, and underweight) are reported in Table 4. A higher score on the psychological satisfaction scale was associated with higher probability of stunting (OR [95% CI] = 1.30 [1.06, 1.63]). All scales except psychological satisfaction showed nonstatistically significant trends towards higher height‐for‐age z‐score, weight‐for‐age z‐score, and weight‐for‐length z‐score when modelled as continuous variables.
Table 4.
Adjusted logistic regression coefficients (odds ratios) of caregiver capabilities scales and child nutritional status (n = 195)a , b
| Maternal construct | Underweight (WAZ < −2) | Stunted (LAZ < −2) | Wasted (WLZ < −2) |
|---|---|---|---|
| Social support subscale | 0.94 (0.74, 1.19) | 0.95 (0.77, 1.18) | 0.95 (0.69, 1.29) |
| Psychological well‐being subscale | 1.00 (0.79, 1.27) | 1.31 (1.06, 1.63)* | 0.88 (0.65, 1.21) |
| Decision‐making subscale | 0.88 (0.69, 1.12) | 1.11 (0.89, 1.39) | 0.94 (0.69, 1.29) |
| Overall freedom and empowerment subscale | 0.80 (0.59, 1.09) | 0.90 (0.69, 1.18) | 0.98 (0.66, 1.45) |
| Composite maternal capabilities index | 0.95 (0.86, 1.04) | 1.02 (0.85, 1.12) | 0.95 (0.84, 1.07) |
Note. LAZ, length‐for‐age z‐score; WAZ = weight‐for‐age z‐score; WLZ = weight‐for‐length z‐score.
Values presented are odds ratios (95% confidence interval).
Results control for maternal education, distance to water source, becoming pregnant as an adolescent, and ownership of mobile phones.
p < .05.
4. DISCUSSION
This study applied a community‐based household survey to measure four dimensions of maternal capabilities in order to establish baseline measures of these constructs in a context of high undernutrition, high fertility among women, and with an early mean age at first pregnancy (UBOS & ICF Macro, 2012). By applying a survey tool that was developed through formative research in the study context, we sought to understand whether these complex, culturally influenced constructs could be measured quantitatively, and whether relationships exist with measurable child feeding indicators and nutritional status.
Our results indicate that complex dimensions of caregiver capabilities can be measured in the study context and that substantial variation in responses to the domains of social support, psychological health, decision making, and freedom/empowerment exist among mothers from the same community. Although our findings suggest limited associations with these dimensions of caregiver capabilities and child nutritional status, we found consistent associations between capabilities and IYCF practices, especially social support and freedom/empowerment. The study context is representative of other settings of rural poverty and with a low relative status of women and is important when interpreting the study findings. It is possible that the overall low opportunity structure places material constraints for which enabled capabilities are insufficient to compensate for with healthful IYCF practices. In this setting, where education among girls remains unacceptably low and where cultural marriage patterns continue to place mothers in vulnerable social positions, tailored social policies and community‐level change are likely necessary to see meaningful benefits to child feeding and nutrition. Further, maternal capabilities represent a set of salient resources for care for just one of many caregivers (e.g., fathers, grandmothers, siblings) that are involved in caring for young children that also need to understood and appropriately supported.
Our study was limited by several factors. First, the cross‐sectional design limits our ability to draw causal inferences and to establish temporality. Although we assume that capabilities are consistent over time and would precede IYCF practices and nutritional status (e.g., through limiting food purchasing power), it is also possible that poor nutritional status among children may influence caregiver capabilities (e.g., having a malnourished child could reduce psychological satisfaction). Previous experience in the study contexts provides some insight in the potential likely relationship of capabilities constructs preceding poor feeding; however, previous work also noted that an inability to feed children according to caregiver's self‐described expectations may reduce overall satisfaction (Ickes et al., 2016). The questions that assessed maternal capabilities were designed to represent more stable characteristics and asked mothers to report on general life conditions, which should reflect prior history, whereas IYCF practices were measured based on self‐report of the day preceding the survey. Second, comparisons across eight feeding indicators, five scales, and three anthropometric indices raise the possibility of type I error. Given the exploratory nature of this study, we decided against an adjustment for multiple comparisons. Third, the conceptual framework and selected capabilities assessed in this study reflect a nonexhaustive set of maternal‐level factors that may influence caregiving. We examined social support, psychological well‐being, decision making, and freedom/empowerment based from previous work in the study context that provided confidence that these constructs could be (a) measured using scalar methods and (b) would be reasonable constructs to address through future interventions and policies in the study setting and in similar contexts. Additional constructs, such as women's time and physical health, were not evaluated and are both likely to play a role in shaping maternal resources for care.
Despite some limitations, our study improves upon prior literature in at least two ways. First, our composite maternal capabilities scale is related but somewhat distinct from the Women's Empowerment in Agriculture Index and Demographic and Health Survey (DHS) assessments of empowerment and decision making in that we assess social support, psychological health, and a comparison of women's perceived sense of freedom and empowerment. The subscales and composite index developed and evaluated in this study assess these constructs outside of the specific domain of agriculture, with the expectation that this index can stimulate adaptation and refinement in other contexts for assessing mothers that may benefit from additional support within nutrition and health programs and to promote discourse over other downstream approaches that may strengthen capabilities and benefit mothers and children.
4.1. Comparison with other studies
Although the application of the capabilities approach used in this paper does not collectively describe a new construct, our study simultaneously examines multiple, related maternal‐level constructs that are relevant for child care and to create and apply a multidimensional index to assess the predictive power of this measure in relation to IYCF and growth. Our findings underscore the importance of women's social support for promoting the adoption of healthy IYCF practices, with significant positive associations for each of the IYCF indicators assessed and is consistent with a growing literature examines various dimensions of maternal well‐being with IYCF and nutritional status. Social support has been demonstrated to be associated with improved breastfeeding and complementary feeding (Bosire et al., 2016; Mukuria, Martin, Egondi, Bingham, & Thuita, 2016), and a review of women's empowerment and child nutritional status in South Asia concluded that social support is a relatively understudied construct in relation to nutritional status (Cunningham, Reul, et al., 2015). Social support can create an enabled environment for child feeding and access to knowledge and skills for child feeding but may also complicate women's feeding abilities through trade‐offs in workload and time for childcare (Cunningham, Ruel, et al., 2015). For example, a study in Nicaragua found that children of mothers with the most social support were less likely to consume highly processed snacks and/or sugar sweetened beverages but were shorter (Ziaei et al., 2015). Additionally, in cross‐sectional studies conducted in Brazil (Harpham, De Silva, & Tuan, 2006) and Vietnam (Surkan, Ryan, Carvalho Vieira, Berkman, & Peterson, 2007), greater social support among women has been associated with child nutritional status in children under 2 years. These studies assessed the availability of support from key individuals and involvement in community groups (Harpham et al., 2006). Social support is understood to have multiple dimensions (emotional, informational, and practical; Stansfeld, 2006); our instrument placed greater emphasis on emotional and practical support as our objective was to assess more general maternal capabilities.
Although our scale for psychological well‐being focused on life satisfaction, the most well‐studied maternal mental health construct in nutrition‐related studies is depression. We chose to focus on psychological well‐being given the relevance of this construct to the capabilities approach and given the already strong support for maternal depression and child nutrition (Ibrahim & Alkire, 2007). A systematic review of maternal depression and childhood growth in developing countries found robust associations between depression, underweight, and stunting in 17 studies representing 11 countries (Surkan et al., 2011). However, the direction of the causal relationship between maternal depression and child malnutrition is uncertain. Fewer studies measure mediating variables, such as IYCF practices, in the relationship between depression and child nutrition. A cross‐sectional study in Bangladesh found that mothers' depression at 12 months post‐partum was linked to nutritional status and that caregiving practices partially mediated this association (Black, Baqui, Zaman, El Arifeedn, & Black, 2009). Although our scale allowed the investigation of the relationship between positive psychological traits and child nutrition, the relationship was not significant with feeding practices but, was, paradoxically associated with increased likelihood of stunting. This association warrants further exploration; however, we also argue that depression may indeed prove a more meaningful construct that the measure of psychological well‐being.
Decision making was not associated with IYCF outcomes. One potential explanation is that in a context with little available discretionary income, involvement in decision making and access to that income does not improve a mother's situation enough to translate into benefits to children's feeding or nutritional status. A national study using DHS data in Uganda found no association between decision making and IYCF or nutritional status but identified a positive relationship between several other dimensions of women's opportunity structures—maternal education, literacy, and access to antenatal care—and IYCF, and nutritional status (Ickes, Hurst, & Flax, 2015). A similar study in Bangladesh found that mothers who participated in making a range of household decisions were 15% less likely to have a stunted child and 32% less likely to have wasted child (Rahman, Saima, & Goni, 2015).
We observed a significant association between freedom/empowerment and IYCF practices for two indicators. In our study, we assessed empowerment as “freedom,” and used a visual 10‐step ladder scale. This scale appears to have provided a useful method for capturing women's overall sense of freedom, currently and over time, and as compared to their peers. Although we did not observe a significant association between freedom/empowerment and indicators of undernutrition, we hypothesize that the influence of freedom/empowerment on nutritional status may require a sufficient opportunity structure or resources. Freedom alone, in the context of material deprivation, may be insufficient for women to compensate for child growth deficits.
The composite scale was developed to provide a holistic measure of maternal capabilities. The overall scale of maternal capabilities serves multiple functions. First, we aimed to understand whether a global measure of maternal freedoms and abilities to provide care was associated with feeding and nutritional status. Second, the development of this scale may become a model that can be adapted to other contexts to measure caregiver capabilities for a variety of purposes (e.g., screening prior to interventions, as an explanatory variable in path analysis, and general surveillance). This scale was consistently associated with IYCF practices: A one quintile improvement in the scale was associated with a 35% to 45% increase in the likelihood of feeding iron‐rich foods, and in achieving dietary diversity, feeding frequency, overall adequacy indicators.
5. CONCLUSIONS
This study helps to identify certain aspects of caregiver capabilities that may benefit from targeted strengthening through interventions that seek specifically to improve maternal capabilities or through more proximal approaches such as improving education for girls and addressing societal norms that limit women's general capabilities, such as allowing young girls to marry and begin their reproductive lives during adolescence. Improvements in mother's social support and freedom/empowerment appear most predictive of IYCF practices; however, there is some evidence to suggest domain of life satisfaction and decision making are also related to better child feeding.
The literature on the links between maternal level factors and child nutrition behaviours and growth varies substantially by measurement and definitions of constructs, study design, and the context in question (Carlson, Kordas, & Murray‐Kolb, 2014). This broad variation indicates that measuring capabilities in the context of interventions may similarly produce a range of results. However, evidence‐based, theory‐driven measurement tools developed through formative research in the context in which they are to be use are likely to provide the most precise and relevant measures of caregiver capabilities. (Martin et al., 2017; Matare et al., 2015). A better understanding of the relevant capabilities in multiple contexts holds potential for highlighting additional and possibly previously underutilized pathways by which IYCF practices and child nutrition can be improved. Efforts to improve these capabilities for mothers are likely to benefit mothers independently of their nutritional caregiving practices. This study highlights a great need for both improving IYCF, child nutrition, and the varied capabilities of mothers in this rural context of Uganda, which have important health consequences for mothers and children.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
Supporting information
Data S1. Maternal Capacities Survey.
Data S2. Screeplot of Eigen values after PCA for Social Support Scale. Screeplot of Eigen values after PCA for Psychological Health Scale. Screeplot of Eigen values after PCA for Decision‐making Scale. Screeplot of Eigen values after PCA for Freedom/Empowerment Scale.
Data S3.
Online Supplemental Figure S1. Histogram of maternal Social Support sub‐scale.
Online Supplemental Figure S2. Histogram of maternal Psychological Wellbeing sub‐scale.
Online Supplemental Figure S3. Histogram of maternal Decision‐making capabilities sub‐scale (=195).
Online Supplemental Figure S4. Histogram of Freedom/empowerment sub‐scale.
Online Supplemental Figure S5. Histogram of Maternal Capabilities composite index.
ACKNOWLEDGMENTS
This study was supported by a Reves Center International Faculty Research Fellowship and a Faculty Research Grant and a Borgenicht Foundation Grant for Health Sciences Research from the College of William and Mary.
Ickes SB, Wu M, Mandel MP, Roberts AC. Associations between social support, psychological well‐being, decision making, empowerment, infant and young child feeding, and nutritional status in Ugandan children ages 0 to 24 months. Matern Child Nutr. 2018;14:e12483 10.1111/mcn.12483
REFERENCES
- Ashaba, S. , Rukundo, G. Z. , Beinempaka, F. , Ntaro, M. , & LeBlanc, J. C. (2015). Maternal depression and malnutrition in children in southwest Uganda: A case control study. BMC Public Health, 15, 1303–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhutta, Z. A. , Das, J. K. , Rizvi, A. , Gaffey, M. F. , Walker, N. , Horton, S. , … Black, R. E. (2013). Evidence‐based interventions for improvement of maternal and child nutrition: What can be done and at what cost? The Lancet., 382, 452–477. [DOI] [PubMed] [Google Scholar]
- Black, M. M. , Baqui, A. H. , Zaman, K. , El Arifeedn, S. , & Black, R. E. (2009). Maternal depressive symptoms and infant growth in rural Bangladesh. The American Journal of Clinical Nutrition, 89, 951S–957S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black, R. E. , Alderman, G. , Bhutta, Z. A. , Gillespie, S. , Haddad, L. , Horton, S. , … Webb, P. (2013). Maternal and child nutrition: Building momentum for impact. The Lancet, 382, 372–375. [DOI] [PubMed] [Google Scholar]
- Bosire, R. , Betz, B. , Aluiso, A. , Hughes, J. P. , Nduati, R. , Kiari, J. , … Farquahr, C. (2016). High rates of exclusive breastfeeding in both arms of a peer counseling study promoting EBF among HIV‐infected Kenyan women. Breastfeeding Med, 11, 53–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broadhead, W. , Gehlbach, S. H. , De Gruy, F. V. , & Kaplan, B. H. (1988). The Duke‐UNC Functional Social Support Questionnaire: Measurement of social support in family medicine patients. Medical Care, 709–723. [DOI] [PubMed] [Google Scholar]
- Cantril, H. (1965). The pattern of human concerns. New Brunswick, NJ: Rutgers University Press. [Google Scholar]
- Carlson, G. J. , Kordas, K. , & Murray‐Kolb, L. E. (2014). Associations between women's autonomy and child nutritional status: A review of the literature. Maternal and Child Nutrition, 11, 1–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham, K. , Ruel, M. , Ferguson, E. , & Uauy, R. (2015). Women's empowerment and child nutritional status in South Asia: A synthesis of the literature. Maternal & Child Nutrition, 11, 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham, K. , Ploubidis, G. B. , Menon, P. , Ruel, M. , Kadiyala, S. , Uauy, R. , & Ferguson, E. (2015). Women's empowerment in agriculture and child nutritional status in rural Nepal. Public Health Nutrition, 18, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deaton, A. (2008). Income, aging, health and wellbeing around the world: Evidence from the Gallup World Poll. Journal of Economic Perspectives, 22, 53–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener, E. , & Ryan, K. (2009). Subjective well‐being: A general overview. South African Journal of Psychology, 39(4), 391–406. [Google Scholar]
- Engle, P. L. , Menon, P. , & Haddad, L. (1999). Care and nutrition: Concepts and measurement. World Development, 27, 1309–1337. [Google Scholar]
- Harpham, T. , De Silva, M. J. , & Tuan, T. (2006). Maternal social capital and child health in Vietnam. J Epidemiology Community Heath., 60, 865–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim, S. , & Alkire, S. (2007). Agency and empowerment: A proposal for internationally comparable indicators of agency and empowerment. Oxford Development Studies, 35(4), 379–403. [Google Scholar]
- Ickes, S. B. , Hurst, T. E. , & Flax, V. F. (2015). Maternal literacy, facility birth, and education are positively associated with better infant and young child feeding practices and nutritional status among Ugandan children. Journal of Nutrition, 145, 2578–2586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ickes, S. B. , Heymsfield, G. , Wright, T. W. , & Charles, B. C. (2016). “Generally the young mom suffers much:” Socio‐cultural factors and life events that shape maternal and child nutrition decisions in western Uganda. Maternal and Child Nutrition. 10.1111/mcn.12365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ickes, S. B. , Baguma, C. , Brahe, C. A. , Myhre, J. A. , Bentley, M. E. , Adair, L. S. , & Ammerman, A. S. (2017). Maternal participation in a nutrition education program in Uganda is associated with improved infant and young child feeding practices and feeding knowledge: a post‐program comparison study. BMC Nutrition, 3(32). 10.1186/s40795-017-0140-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin, S. L. , Birhanu, Z. , Omotayo, M. O. , Kebede, Y. , Pelto, G. H. , Stoltzfus, R. J. , & Dickin, K. L. (2017). “I can't answer what you're asking me. Let me go please.” Cognitive interviewing to assess social support measures in Ethiopia and Kenya. Field Methods. Retrieved from http://journals.sagepub.com/doi/abs/10.1177/1525822X17703393 [Google Scholar]
- Matare, C. , Mbuya, M. N. , Pelto, G. , Dickin, K. L. , & Stoltzfus, R. J. , Sanitation, Hygiene, Infant Nutrition Efficacy (SHINE) Trial Team . (2015). Assessing maternal capabilities in the SHINE trial: Highlighting a hidden link in the causal pathway to child Health. Clinical Infectious Diseases. 2015; 15(S7), S745–S751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukuria, A. G. , Martin, S. L. , Egondi, T. , Bingham, A. , & Thuita, F. M. (2016). Role of social support in improving infant feeding practices in western Kenya: A quasi‐experimental study. Global Health Science and Practice., 4, 55–72. 10.9745/GHSP-D-15-00197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organisation for Economic Co‐operation and Development (OECD) . (2013). OECD guidelines on measuring subjective well‐being. Paris: OECD Publishing; Available http://at/: http://dx.doi.org/10.1787/9789264191655‐en [PubMed] [Google Scholar]
- Oxford Poverty and Human Development Initiative . (2015). http://www.ophi.org.uk/research/missingdimensions/survey-modules/. Retrieved May 1, 2014.
- Rahman, M. , Saima, U. , & Goni, A. (2015). Impact of maternal household decision‐making autonomy on child nutritional status in Bangladesh. Asia‐Pacific Journal of Public Health, 27, 509–520. [DOI] [PubMed] [Google Scholar]
- Rollins, N. , Bhandari, N. , Hajeebhoy, N. , Horton, S. , Lutter, C. , Martines, J. , … Victora, C. (2016). Why invest, and what will it take to improve breastfeeding practices? Lancet, 387, 491–504. [DOI] [PubMed] [Google Scholar]
- Samman, E. (2007). Psychological and subjective wellbeing: A proposal for internationally comparable indicators. Oxford Development Studies., 35, 459–486. [Google Scholar]
- Shorr Productions . (n.d.). Available at http://www.weighandmeasure.com. Olney, MD. (Accessed 1 September 2016).
- Shroff, M. , Griffiths, P. , Adair, L. , & Bentley, M. (2009). Maternal autonomy is inversely related to child stunting in Andhra Pradesh. India. Matern Child Nutr., 5, 64–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shroff, M. , Griffiths, P. , Adair, L. , & Bentley, M. (2011). Does maternal autonomy influence feeding practices and infant growth in rural India? Social Science & Medicine, 73, 447–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stansfeld, S. A. (2006). Social support and social cohesion In Marmot M., & Wilkinson R. (Eds.), Social determinants of health (pp. 148–171). New York: Oxford University Press; 10.1093/acprof:oso/9780198565895.003.08 [DOI] [Google Scholar]
- Stewart, C. P. , Ionnotti, L. , Dewey, K. G. , Michaelsen, K. F. , & Onyango, A. W. (2013). Contextualizing complementary feeding in a broader framework for stunting prevention. Maternal Child Nutr., (Suppl 2), 27–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surkan, P. J. , Ryan, L. M. , Carvalho Vieira, L. M. , Berkman, L. F. , & Peterson, K. E. (2007). Maternal social and psychological conditions and physical growth in low‐income children in Piaui, Northeast Brazil. Social Science & Medicine, 64, 375–388. [DOI] [PubMed] [Google Scholar]
- Surkan, P. J. , Kawachi, I. , Ryan, L. M. , Berkman, L. F. , Carvalho, V. L. M. , & Peterson, K. E. (2008). Maternal depressive symptoms, parenting self‐efficacy, and child growth. American Journal of Public Health, 98, 125–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surkan, P. J. , Kennedy, C. E. , Hurley, K. M. , & Black, M. M. (2011). Maternal depression and early childhood growth in developing countries: Systematic review and meta‐analysis. Bulletin of the World Health Organization, 89, 608–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tylleskär, T. , Jackson, D. , Meda, N. , Engebretston, I. , Chopra, M. , Diallo, A. , … PROMISE‐EBF Study Group . (2011). Exclusive breastfeeding promotion by peer counsellors in sub‐Saharan Africa (PROMISE‐EBF): A cluster‐randomised trial. Lancet, 378, 420–427. [DOI] [PubMed] [Google Scholar]
- Uganda Bureau of Statistics (UBOS) and ICF International Inc . (2012). Uganda Demographic and Health Survey 2011. Kampala, Uganda: UBOS and Calverton, Maryland: ICF International Inc.
- Uganda Bureau of Statistics (UBOS) and ICF International Inc . (2017). Uganda Demographic and Health Survey 2016: Key Indicators Report. Kampala, Uganda: UBOS and Rockville, Maryland: ICF International Inc.
- United States Agency for International Development (USAID) . (2008). Manual for the implementation of USAID poverty assessment tools. College Park, MD.
- World Bank‐UNICEF Nutrition . (2002). Toward a common understanding of malnutrition: Assessing the contributions of the UNICEF framework. D.C.: Washington. [Google Scholar]
- World Health Organization . (2006). WHO child growth standards: Length/height for age, weight‐for‐age, weight‐for‐length, weight‐for‐height and body mass index‐for‐age, methods and development. Geneva, Switzerland: World Health Organization. [Google Scholar]
- World Health Organization . (2008). World Health Organization indicators for assessing infant and young child feeding practices: Part 1: Definitions. World Health Organization: Geneva (Switzerland). Available from: http://www.who.int/maternal_child_adolescent/documents/9789241596664/en/
- Ziaei, S. , Contreras, M. , Zelaya Blandon, E. , Persson, L. A. , Hjern, A. , & Ekstrom, E. C. (2015). Women's autonomy and social support and their associations with infant and young child feeding and nutritional status: community‐based survey in rural Nicaragua. Public Health Nutrition, 18, 1979–1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zongrone, A. , Martin, S. , Matare, C. , Dickin, K. , Young, S. , Pelto, G. , … Stoltzfus, R. (Under review). Caregiver capabilities: A conceptual framework for health and nutrition program implementation and research.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Maternal Capacities Survey.
Data S2. Screeplot of Eigen values after PCA for Social Support Scale. Screeplot of Eigen values after PCA for Psychological Health Scale. Screeplot of Eigen values after PCA for Decision‐making Scale. Screeplot of Eigen values after PCA for Freedom/Empowerment Scale.
Data S3.
Online Supplemental Figure S1. Histogram of maternal Social Support sub‐scale.
Online Supplemental Figure S2. Histogram of maternal Psychological Wellbeing sub‐scale.
Online Supplemental Figure S3. Histogram of maternal Decision‐making capabilities sub‐scale (=195).
Online Supplemental Figure S4. Histogram of Freedom/empowerment sub‐scale.
Online Supplemental Figure S5. Histogram of Maternal Capabilities composite index.


