Abstract
As evidence grows supporting certain mechanisms of change in psychological treatments and we improve statistical approaches to measuring them, it is important that we also explore how mechanisms and processes are related to each other, and how they together affect treatment outcomes. To answer these questions about interrelating processes and mechanisms, we need to take advantage of frequent assessment and modeling techniques that allow for an examination of the influence of one mechanism on another over time. Within cognitive behavioral therapy, studies have shown support for both decentering, the ability to observe thoughts and feelings as objective events in the mind, and anticipatory processing, the repetitive thinking about upcoming social situations, as potentially related mechanisms of change. Therefore, the current study examined weekly ratings of decentering and a single-item anticipatory processing question to examine the interrelation among these change mechanisms in 59 individuals who received a 12-weeks of Cognitive Behavioral Group Therapy for social anxiety disorder. Overall, these results found that both anticipatory processing and decentering changed over the course therapy for clients. Change in both anticipatory processing and decentering was related to outcome. The bivariate latent difference score analysis showed that anticipatory processing was a leading indicator of change in decentering, but not the reverse, indicating that change in anticipatory processing is leading to change in decentering. It may be that with the focus on cognitive reappraisal in this treatment, that reducing anticipatory processing is freeing up the cognitive resources for decentering to occur.
Keywords: decentering, repetitive negative thinking, anticipatory processing, mechanisms of action, modeling change
In 2007 when Kazdin wrote his seminal paper on mediators and mechanisms of change he observed that “we know well that therapy ‘works,’ … but have little knowledge of why or how it works.” (Kazdin, 2007, p. 2). Since this time, there has been a consistent focus on mechanism research. This has led to a more mature knowledge base of some of the key mechanisms leading to change in psychotherapy. While this has provided a wealth of important information, change in psychotherapy is multifaceted and too often research has focused on a single mechanism. To further capture how and why therapy works, attention should be paid to how potential mechanisms interrelate over time to lead to improved outcomes in psychotherapy. Therefore, this study utilizes bivariate latent difference score analysis to demonstrate one method for examining the interrelation among two potential mechanisms of change (decentering and anticipatory processing) across Cognitive Behavioral Group Therapy for social anxiety disorder.
One hypothesized mechanism of change which has been receiving empirical support is decentering, or the ability to observe thoughts and feelings as objective events in the mind rather than personally identifying with them (Safran & Segal, 1990). According to the metacognitive processes model of decentering (Bernstein et al., 2015), decentering involves meta-awareness, disidentification from internal experiences, and reduced reactivity to thought content. In other words, decentering involves a focus on observing the thinking process rather than a focus on the content of one’s thoughts. This allows for a disidentification from internal experiences where the thought or other internal state is separate from one’s self. The present moment focus on the thought process also reduces one’s emotional reactivity to a particular thought.
Within therapy, decentering has been hypothesized as a mechanism of action in both cognitive behavioral therapies (CBTs) (Beck, Rush, Shaw, & Emery, 1979; Heimberg & Ritter, 2008) as well as acceptance and mindfulness-based therapies (Bishop et al., 2004; Hayes-Skelton, Calloway, Roemer, & Orsillo, 2015). From a CBT perspective, decentering may play a role in cognitive restructuring in that cognitive restructuring involves looking at one’s thoughts from a more objective perspective and then challenging the idea that thoughts are fact by instead seeing thoughts as hypotheses to be tested (Heimberg & Ritter, 2008). Similarly, the process of systematically identifying and examining thoughts (i.e., cognitive reappraisal) may provide disidentification from the anxious thoughts (Beck et al., 1979) which then may allow for decentering. The role of decentering in CBT has been shown empirically in that decentering increases across both CBT (Fresco, Segal, Buis, & Kennedy, 2007) and Mindfulness-Based Cognitive Therapy (MBCT; Teasdale et al., 2002) for depression relapse prevention and changes in decentering predicted changes in symptoms of depression following MBCT (Bieling et al., 2012). In a mixed anxiety and depression sample, the closely related construct of cognitive defusion was a mediator in both cognitive therapy and acceptance and commitment therapy (Forman et al., 2012). Similarly, an initial investigation of the data presented in the current study showed that change in decentering predicted improvement on most outcome measures and those who no longer met criteria for social anxiety disorder at post-treatment had significantly greater change in decentering across therapy and significantly higher decentering scores at post-treatment compared to those who retained a social anxiety disorder diagnosis at post-treatment (Hayes-Skelton & Lee, 2018).
While decentering appears to play a role in CBT in general, as well as CBT for social anxiety specifically, questions remain about how decentering influences outcome. For example, it is not clear whether decentering leads to cognitive changes or instead follows from cognitive changes. The answers to these questions have implications for whether decentering should be a direct therapy target or whether it is a result of other changes. Given that changes in decentering are related to changes in worry in clients with generalized anxiety disorder (Hayes-Skelton et al., 2015), it is possible that decentering influences social anxiety through its relation with the cognitive rumination process that occurs before individuals with social anxiety disorder enter a social situation. This repetitive thinking about social situations before they occur has been termed anticipatory processing.
According to Clark and Wells’s (1995) model of social anxiety, anticipatory processing refers to the review of what might happen in a future social situation, a focus on the anticipatory anxiety, recollections of past failures, negative self-images, and predictions of poor performance. For example, this may look like a future focused worry spiral – “my mind will go blank and I won’t recover and then everyone will laugh at me, why can’t I just do this simple thing.” Of note, this mental review process prior to participating in a social situation is part of many prominent models of social anxiety (i.e., Herbert & Cardaciotto, 2005; Hofmann, 2007; Rapee & Heimberg, 1997). Sometimes this process is also referred to as pre-event rumination (Penney & Abbott, 2014) or pre-event processing (Hodson, McManus, Clark, & Doll, 2008). Anticipatory processing falls under the larger umbrella term of repetitive negative thinking, which is a transdiagnostic construct including post-event processing, worry, and rumination (Arditte, Shaw, & Timpano, 2016). We will use the term anticipatory processing in this paper, but see Wong (2016) for a review of these related constructs.
Individuals high in social anxiety reported more frequent negative thoughts about future social events (i.e., Hinrichsen & Clark, 2003; Vassilopoulos, 2004). Of note, research has supported the connection between social anxiety and the avoidance function, not the preparatory aspects, of anticipatory processing (Mills, Grant, Lechner, & Judah, 2013). At this point, there has been little research examining anticipatory processing in the context of therapy. One study has shown that anticipatory processing is a mediator in CBGT for SAD specifically (Hedman et al., 2013). However, anticipatory processing was not a mediator of outcome in individual CBT in the same study, despite it decreasing across CBT based on Clark and Wells’s (1995) model, speaking to how processes and mechanisms can be treatment specific.
While there is empirical support for the role of both anticipatory processing and decentering in treating social anxiety, questions remain regarding how these relate to each other. There are two possibilities for this relation. First, decentering could be a higher order mechanism the follows the cognitive changes in anticipatory processing. When anticipatory processing decreases in that an individual is spending less time engaged in repetitive negative thought prior to an anxiety provoking event, does this then lead them to take the wider, more objective perspective that is characteristic of decentering? This would imply that the beneficial changes in anxiety due to decentering follow decreases in anticipatory processing. Alternately, if changes in decentering precede changes in anticipatory processing, this may imply that it is the broader perspective characteristic of decentering that is allowing the anticipatory processing to decrease. For example, theory from an acceptance-based perspective would suggest that by taking a decentered perspective, one would not become as fixated on the content of one’s cognitive biases, which would then decrease the repetitive worry characteristic of anticipatory processing (Roemer & Orsillo, 2009). While we are not aware of any research specifically looking at the relation between decentering and anticipatory processing, there is some evidence of the relation between decentering and the larger construct of repetitive negative thoughts. For example, several studies have shown a moderate to large negative correlation between decentering and rumination, in both nonclinical samples and a clinical sample diagnosed with an anxiety disorder (Fresco et al., 2007; Kaiser, Andrews-Hanna, Metcalf, & Dimidjian, 2015; Mori, & Tanno, 2015; Naragon-Gainey & DeMarree, 2017). Similarly, when looking at the broader construct of repetitive negative thinking, authors found a moderate negative correlation between repetitive negative thinking and decentering using one (Experiences Questionnaire; Ehring et al., 2011), but not another decentering measure (Toronto Mindfulness Questionnaire; Naragon-Gainey, & DeMarree, 2017). Of note, these differences between the two decentering measures are common (see Naragon-Gainey & DeMarree, 2017).
Therefore, the current study will demonstrate how bivariate latent difference score analysis (BLDS: Ferrer & McArdle, 2003) can be utilized to examine questions about the interrelation and timing of these two change processes by examining weekly ratings of decentering and anticipatory processing across Cognitive Behavioral Group Therapy (CBGT: Heimberg & Becker, 2002) for social anxiety disorder. This method will allow us to examine: 1) whether both anticipatory processing and decentering change over the course of therapy, 2) whether change in each of the potential mechanisms is related to treatment outcome, and 3) the strength and direction of the relation between anticipatory processing and decentering.
Modeling Change with Bivariate Latent Difference Score Analysis
To answer these questions about interrelating mechanisms, we need to take advantage of frequent assessment and modeling techniques that allow for an examination of the influence of one mechanism on another over time. The BLDS modeling will allow us to examine whether changes in anticipatory processing precede changes in decentering or if changes in decentering precede changes in anticipatory processing. Bivariate latent difference score analysis is an analytic method that combines latent growth modeling with cross-lagged regression analyses and factor analysis models of change and latent difference scores in order to account for the latent changes on variables over time. In other words, these models examine change over time in two separate variables (i.e., changes in decentering and anticipatory processing across treatment) as well as examining how change in one variable leads to change in the second variable at a subsequent time point (Grimm, An, McArdle, Zonderman, & Resnick, 2012). This form of modeling, while not strictly causal, does allow us to get closer to asking questions about the temporal ordering of multiple potential mechanisms by examining the effect of change in one variable at a previous time point on the amount of change on a second variable. In other words, models can be developed that examine decentering leading to changes in anticipatory processing and with anticipatory processing leading to changes in decentering.
Methods
Participants
Participants are the 59 individuals who attended at least one of the 12-sessions of cognitive-behavioral group therapy for social anxiety (see Hayes-Skelton & Lee, 2018 for the full outcome results). All participants were: a) individuals with a principal diagnosis of SAD on the ADIS-IV with at least moderate severity (score of 4) on the Clinician’s Severity Rating; b) stable on psychotropic medications for three months (or one month for benzodiazepines) and willing to maintain these levels; c) willing to refrain from other psychosocial treatments for anxiety or mood problems during the course of therapy; d) fluent in English; and e) 18 years or older. Individuals who exhibited symptoms that required more immediate attention such as psychotic symptoms, active suicidal intent, bipolar disorder, or substance dependence were excluded. All participants provided informed consent to participate in the study. The demographic characteristics of participants can be seen in Table 1.
Table 1.
Demographic Characteristics
| Gender n(%) | |
| Female | 34 (57.60%) |
| Male | 25 (42.40%) |
| Mean Age (SD) | 27.90 (10.06) |
| Min/Max | 18.00/60.00 |
| Sexual Orientation n(%) | |
| Heterosexual | 49 (83.10%) |
| Gay/Lesbian | 4 (6.80%) |
| Bisexual | 2 (3.40%) |
| Not listed | 1 (1.70%) |
| Racial/Ethnic Identity n(%) a | |
| White | 30 (50.80%) |
| Asian | 14 (23.70%) |
| Black | 8 (13.60%) |
| Latino/Hispanic | 6 (10.17%) |
| Pacific Islander | 1 (1.70%) |
| Alaskan/Native | 1 (1.70%) |
| Not listed b | 7 (11.86%) |
| Mean Pre-Treatment Clinician’s Severity Ratings (SD) | 5.54 (0.80) |
Participants checked as many racial identities as appliec
Other identities endorsed: White and Korean, African, Don’t identify, East Indian, Latino skin tone, Serbian, Vietnamese and Italian
Measures
Weekly Assessment – Anticipatory Processing (AP) –
The weekly assessment was used to assess clients’ weekly ratings on a number of constructs from their perceived severity of their social anxiety, to avoidance of social situation, to number of out of session exposures that clients completed. For the purpose of the current study, we used the single item from this measure that focused on anticipatory processing. Specifically, this item asked: “Over the past week how often have you gone over in your mind things that you think might go wrong in a social situation before entering the situation?” Participants rated their response on a 0 (“Not at all”) to 8 (“Always”) Likert scale.
Experiences Questionnaire—Decentering Subscale (EQ-Decentering; Fresco et al., 2007)
The EQ is a 20 item self-report measure that assesses decentering and rumination. We used the Decentering subscale (11 items) for the purposes of the current study. This 5-point Likert-type scale ranges from never to all the time. Sample items include: “I can separate myself from my thoughts and feelings” and “I can observe unpleasant feelings without being drawn into them.” Higher scores indicate more decentering. The Decentering subscale has demonstrated good internal consistency in both nonclinical and clinical samples with alpha coefficients of .83 and .84, respectively (Fresco, Moore, et al., 2007; Fresco, Segal, et al., 2007). The EQ was assessed at each session. Internal consistencies in the current sample ranged from .84 (in session 5) to .96 (in session 12).
Outcome Measures:
Clinician Severity Rating (CSR) –
The CSR is a rating ranging from 0–8, with ratings 4 or greater indicating clinical significance, made by an assessor as part of the Anxiety Disorders Interview Schedule (ADIS-IV; Brown, DiNardo, & Barlow, 1994), a semi-structured diagnostic interview used to diagnose DSM-IV anxiety disorders. For SAD, the ADIS-IV has demonstrated adequate reliability (Brown, DiNardo, Lehmann, & Campbell, 2001). Independent assessors gave the ADIS-IV at pre-treatment and post-treatment assessments. Independent assessors were graduate students, unaware of pre- or post-treatment status, trained in the administration and scoring of the ADIS. To be certified, assessors were required to match a senior interviewer’s diagnoses on three consecutive interviews within one point on the CSR. Diagnoses were also confirmed in a consensus meeting with a doctoral-level psychologist (Dr. Sarah Hayes-Skelton) and by therapists. Additionally, 20% of interviews were scored by a second rater, with an interclass correlation (ICC) between raters on CSR for SAD of .964.
Leibowitz Social Anxiety Scale – Self Report (LSAS-SR: Liebowitz, 1987) is a self-report measure consisting of 24 social situations that are likely to elicit social anxiety. Participants rate both fear and avoidance on 0 to 3 scales. While the LSAS was originally developed as a clinician-administered interview, a self-report version of the LSAS has been developed (Baker, Heinrichs, Kim & Hofmann, 2002; Fresco et al., 2001). Both studies demonstrated that the self-report version is highly correlated with the clinician version, and that the self-report version has high internal consistency and good test-retest reliability of the self-report version. The LSAS demonstrated excellent internal consistency in our sample (Pre: α= .96, Post: α= .97).
Procedures
All study procedures were approved by the University of Massachusetts Boston Internal Review Board. All participants provided informed consent for the study. Participants were enrolled in this study following completion of the ADIS and a phone screen to determine eligibility. Participants received therapy free of charge and were paid $75 for completing the post-treatment assessment. All self-report measures and BATs were completed pre- and post-treatment; additionally, the Weekly Assessment and the EQ was administered before each session.
Cognitive Behavioral Group Therapy (CBGT: Heimberg & Becker, 2002).
Clients received a course of CBGT, which consisted of 12 two and a half hour, weekly sessions, plus an initial engagement session to orient them to the treatment. Each group consisted of four to six clients and two therapists, who were either the first author, a licensed clinical psychologist or advanced doctoral students (n = 9) trained and supervised on a weekly basis by the first author. Additionally, Dr. Heimberg provided an initial training to therapists.
The first three sessions of CBGT focused on psychoeducation and training in Beckian-style cognitive restructuring. By the third session, sessions involved therapist-led cognitive restructuring followed by in-session exposures. Therapists and clients also worked together to design homework exposures that built on the in-session exposures to do between sessions. On average, clients completed 9.22 of the 12 sessions. Overall, sessions were rated as adherent (see Hayes-Skelton & Lee, 2018 for a detailed description of adherence procedures).
Data Analysis
All data were analyzed in Mplus Version 6.12 (Muthén & Muthén, 2010) using full maximum likelihood (ML) estimation procedures. Data were missing for 1.7–37.3% of cases at any time point. With the exception of the Bivariate Latent Difference Score (BLDS) models which were only run without nesting, models were run with and without nesting participants into their treatment groups. However, there were no substantial differences between these models and so for parsimony and consistency with the LDSs, results are reported without nesting.
To test the first hypothesis that clients would experience decrease in anticipatory processing (AP) and an increase in decentering, two separate unconditional linear growth curves were fit to the anticipatory processing (AP) and decentering (EQ) scores that were measures at each session (12 total) over the course of therapy. These analyses provide an estimate of the intercept, here the estimated score at session 1, and the slope, or average rate of change across each session. To test the hypothesis the rate of change in anticipatory processing and decentering would predict symptom change, the CSR and LSAS residualized gain scores were added separately to each of the unconditional models. The residualized gain score provides an estimate of the post-treatment score on the CSR or LSAS accounting for the variance due to the pre-treatment CSR or LSAS score. Next, to test the hypothesis that change in anticipatory processing would be related to change in decentering, a parallel process model was run that simultaneously estimates two unconditional linear growth curves. This allows for an examination of how the intercept and slope of one variable (AP) relates to the intercept and slope of a second variable (EQ). In other words, is change in AP correlated with change in EQ.
Next, to test the hypothesis examining whether changes in decentering would precede changes in anticipatory processing or changes in anticipatory processing would precede changes in decentering, a bivariate latent difference score model (BLDS: Ferrer & McArdle, 2003) was fit to the data to model both the linear change in the AP and the EQ simultaneously and also the component of change that is attributable to the other variable. As described below, within the BLDS framework, nested models can be compared to determine the extent to which various parameters significantly impact the overall fit of the model. In this study, four models were compared: a bidirectional change model where anticipatory processing is a leading indicator of change in decentering and decentering is a leading indicator of anticipatory processing (Model 1), a unidirectional model with anticipatory processing as a leading indicator of change in decentering to examine whether change in anticipatory processing precedes changes in decentering (Model 2), an opposing unidirectional model with decentering as a leading indicator of change in anticipatory processing (Model 3) to examine whether change in decentering precedes changes in anticipatory processing, and a model without the leading indicator relationships between variables (Model 4). Fit statistics such as the chi-square difference tests for nested model comparisons (Satorra & Bentler, 2001) are used to compare the relative fit of the four models. The purpose of the fit statistics here are to compare the fit across these nested models.
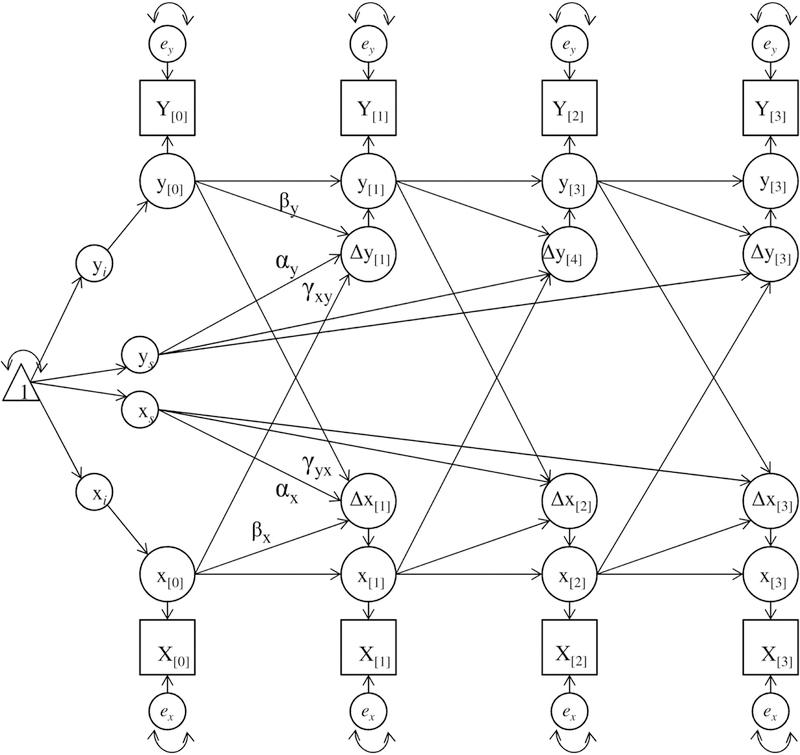
Bivariate Latent Difference Score Models.
Bivariate latent difference score analysis is an analytic method that combines latent growth modeling with cross-lagged regression analyses and factor analysis models of change and latent difference scores (McArdle & Nesselroade, 1994) in order to account for the latent changes on variables over time. In other words, these models examine change over time in a variable (i.e., change in decentering across treatment), the latent growth component (Grimm et al., 2012). By using frequent assessment, change can be examined from one session to the next. Similar to cross-lag regression, the latent difference score component of these models examine change as a combination of the intercept (i.e., decentering score at session 1), plus all of the latent changes that have accumulated up to that point. In other words, the latent difference score for decentering at session 4 is would be influenced by decentering at session 1 as well as the cumulative change in decentering prior to session 4. However, different from cross-lag regression, here change is modeled as a latent variable.
In a bivariate latent difference score model, in addition to the accumulated change on the variable of interest (change through session 5 on decentering), the latent difference scores of a second variable (change through session 4 on anticipatory processing) at the previous time point are also included. In other words, at each occasion a latent variable is modeled which represents change in the true score of each variable (Δx(t) and Δy(t)) as a function of time (t). In this example, x is decentering, y is anticipatory processing, and t is the session number. Each of these latent variables are a function of three components: 1) the linear slope or average rate of change in the given variable (decentering), α; 2) the previous score of the variable of interest (decentering), β; and 3) the score of the other variable (anticipatory processing) at the previous time point, γ. This last one (γ) is typically referred to as the coupling parameter. It is this coupling parameter that represents the influence of one variable on change in the second variable. This coupling parameter is essentially a measure of how much change on the second variable (anticipatory processing) through t-1 predicts change on the first variable (decentering) through t. In this way we are able to get a metric of how change in one variable predicts change in the other or whether anticipatory processing is a leading indicator of change in decentering. In our example, γ would represent the influence of change in anticipatory processing by session t-1 on the latent change in decentering at session t while taking into account the previous score on decentering and the previous amount of change in decentering.
Models can be developed that include coupling parameters in each direction: with decentering leading to changes in anticipatory processing and with anticipatory processing leading to decentering. A model with both of these coupling parameters can then be compared to a model that only has one of the coupling parameters (i.e., only change from decentering to anticipatory processing) to examine the influence of the coupling parameter not included. For example, when the coupling from anticipatory processing to decentering is not included, does this negatively impact the fit of the model compared to the model that has both couplings? If there was a significant change in fit when not including the coupling from anticipatory processing to decentering, then one might conclude that anticipatory processing is a leading indicator of decentering. See supplemental material for a diagram of a bivariate latent difference score model that includes couplings from both variable x to variable y and from y to x. For more information, please see: Grimm et al., (2012); McArdle (2009); and McArdle and Nesselroade (1994).
Results
Preliminary Analyses
First we examined the AP and EQ variables at each time point for skew and kurtosis and for outliers. The EQ values were skewed at several time points, although upon further investigation, this skew was being driven by one outlier who reported low EQ scores at each time point. Results were run with and without this participant included and because they did not meaningfully differ, we are reporting the analyses when this participant was included. The means and standard deviations for the AP and EQ at each time point are presented in Table 2.
Table 2.
Means, standard deviations, and sample size for anticipatory processing (AP) and decentering (EQ) at each session
| Session | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
| AP | ||||||||||||
| Mean | 4.78 | 4.63 | 4.56 | 4.21 | 4.04 | 4.25 | 3.73 | 4.10 | 3.43 | 3.24 | 3.74 | 3.30 |
| SD | 1.82 | 1.84 | 1.88 | 1.72 | 2.02 | 1.50 | 1.63 | 2.04 | 1.77 | 2.03 | 1.95 | 1.86 |
| n | 57 | 53 | 52 | 48 | 43 | 40 | 41 | 42 | 37 | 42 | 42 | 42 |
| EQ | ||||||||||||
| Mean | 31.10 | 30.26 | 30.76 | 31.44 | 32.93 | 33.20 | 32.72 | 32.32 | 33.78 | 34.67 | 34.47 | 36.12 |
| SD | 6.12 | 5.96 | 6.13 | 5.68 | 6.22 | 6.29 | 5.93 | 6.70 | 6.41 | 7.26 | 7.65 | 6.78 |
| n | 58 | 52 | 52 | 48 | 43 | 40 | 41 | 40 | 38 | 41 | 42 | 42 |
Note. AP = Anticipatory processing question of the Weekly Assessment; EQ = decentering subscale of the Experiences Questionnaire.
All clients in this study began treatment with clinically significant social anxiety based on the Clinician Severity Rating (CSR) for social anxiety disorder (mean = 5.54, SD = 0.80, range 4–7). On average, the CSR for social anxiety disorder decreased to below the clinical cutoff by post-treatment (mean = 3.77, SD = 1.23, range 1–6). Similarly, client’s LSAS scores were 121.18 (SD = 25.77) at pre-treatment, indicating a high level of social anxiety. The LSAS scores decreased to 99.69 (SD = 22.98) by post-treatment.
Anticipatory Processing and Decentering Change over Treatment
As a first step, the individual trajectories of anticipatory processing (AP) decentering (EQ) by fitting separate growth curves. For anticipatory processing (AP), the intercept was 4.73 (SE = 0.19) and the slope was −0.13 (SE = 0.02). This slope parameter was significant at Z = - 5.45, p < .001. In other words, clients began treatment with an average AP score of 4.73 which decreased significantly by an average of 0.13 points each session ending treatment at approximately 3.30. For decentering (EQ), the intercept was 30.52 (SE = 0.76) and the slope was 0.49 (SE = 0.07). This slope parameter was significant at Z = 6.83, p < .001. In other words, clients began treatment with an average EQ score of 30.52 which increased significantly by an average of 0.49 points each session ending treatment at approximately 35.91.
Relation between Change in Anticipatory Processing and Decentering and Treatment Outcome
To test the association between anticipatory processing, decentering, and outcome, we examined separate models for AP and decentering for two separate outcome measures: Clinician Severity Rating (CSR) and Leibowitz Social Anxiety Scale (LSAS). For each model, post-treatment scores were added to the anticipatory processing or decentering models by regressing the residualized gain score for CSR or LSAS on the intercept and slope of the individual growth models. As can be seen in Table 3, decreasing anticipatory processing scores (AP) were associated with lower CSR (r = .44) and LSAS (r = .65) scores. The change in AP is responsible for 43.3% of the change in LSAS and 17.2% of the change in CSR. Similarly, increasing decentering scores were also associated with lower CSR (r = −.33) and LSAS (r = −.47) scores. The change in EQ is responsible for 22.0% of the change in LSAS and 10.8% of the change in CSR.
Table 3.
Predicting Outcome from Growth Parameters for Anticipatory Processing (AP) and Decentering (EQ)
| CSR regressed on Intercept/Slope | LSAS regressed on Intercept/Slope | |||||
|---|---|---|---|---|---|---|
| Est. (SE)a | Z | p | Est. (SE)a | Z | p | |
| AP | ||||||
| Intercept | .14 (.16) | 0.89 | .37 | −.03 (.16) | −0.19 | .85 |
| Slope | .44 (.19) | 2.34 | .02 | .65 (.16) | 3.98 | <.001 |
| EQ | ||||||
| Intercept | −.05 (.15) | −0.32 | .75 | −.16 (.14) | −1.13 | .26 |
| Slope | −.33 (.15) | −2.23 | .03 | −.47 (.14) | −3.36 | .001 |
Note. AP = Anticipatory processing question of the Weekly Assessment; EQ = decentering subscale of the Experiences Questionnaire; CSR = residualized gain score of Clinician Severity Rating post regressed on pre; LSAS = residualized gain score of Leibowitz Social Anxiety Scale - self-report post regressed on pre; Intercept = estimate score at pre-treatment; Slope = unit change for each therapy sessions; Est. = Parameter Estimate; SE = Standard Error; Z = Standardized Z-score. Z > 1.96 is significant at p < .05; Z > 2.58 is significant at p < .01.
Standardized estimates reported.
Relation between Change in Anticipatory Processing and Change in Decentering: Parallel Process Model
In order to examine the relation between change on our two proposed processes, we ran a parallel process model which simultaneously estimated the linear growth curves for anticipatory processing (AP) and decentering (EQ). This allows us to examine the correlations between the parameters. As can be seen in Table 4, there is a moderate correlation between change in anticipatory processing (AP) and change in decentering (EQ) (r = −.41, p = .047). This demonstrates that there is a relation between change on these two variables. Of note, we would not expect the correlations involving the intercepts to be correlated as we conceptualize these variables as mechanisms of change and not predictors of change. In other words, level of AP at pre-treatment does not predict how much change in decentering is experienced over treatment.
Table 4.
Correlations among Growth Parameters for Anticipatory Processing (AP) and Decentering (EQ)
| AP-intercept | AP-slope | EQ-intercept | |
|---|---|---|---|
| AP-intercept | -- | ||
| AP-slope | −.31 | -- | |
| EQ-intercept | .11 | .07 | -- |
| EQ-slope | −.12 | −.41* | −.16 |
Note. AP = Anticipatory processing question from Weekly Assessment; EQ = decentering subscale from the Experiences Questionnaire; Intercept = estimate score at pre-treatment; Slope = unit change for each therapy sessions
p < .05.
Bivariate Latent Difference Score Model
Given that both anticipatory processing and decentering changed significantly over treatment, these changes were related to improved outcome, and change in anticipatory processing was associated with change in decentering, the next step was to further examine the relation between change in anticipatory processing and change in decentering. This will allow us to have a better understanding of how these two mechanisms influence each other over time. To examine the associations between changes in anticipatory processing and changes in decentering, a series of bivariate latent difference score models were fit to the observed data to examine whether change in one process was a leading indicator of change in the other. The model fit of four nested models were compared (see Table 5) to examine the relative fit of the various coupling patterns.
Table 5.
Chi-Square Difference for Alternative Bivariate Latent Difference Score Models
| Index | Model 1: Both | Model 2: | Model 3: | Model 4: |
|---|---|---|---|---|
| Couplings | AP to EQ Only | EQ to AP Only | No Coupling | |
| χ2/df | 873.94/303 | 874.62/304 | 889.37/304 | 889.39/305 |
| p | <.001 | <.001 | <.001 | <.001 |
| ∆χ2/∆df | -- | 0.68/1 | 15.43/1 | 15.45/2 |
| p | .41 | <.001 | <.001 | |
| RMSEA | .18 | .18 | .18 | .18 |
| CI | .16 − .19 | .16 - .19 | .17−.20 | .17−.19 |
| Fit significantly degraded? | -- | No | Yes | Yes |
Note. AP = Anticipatory processing question from the Weekly Assessment; EQ = decentering subscale of the Experiences Questionnaire; RMSEA = root-mean-square error of approximation; CI = confidence interval of the RMSEA. Bold represents the selected model.
First the full bidirectional change model (Model 1), which included couplings from anticipatory processing to decentering and from decentering to anticipatory processing, was run. Next, a more parsimonious model with only the coupling from anticipatory processing to decentering (Model 2) was compared to Model 1 to test whether anticipatory processing would be a leading indicator of change in decentering. The non-significant chi-square difference test (p = .41) indicates that the more parsimonious Model 2 was an equivalent fitting model to the full Model, indicating that the coupling from decentering to anticipatory processing does not significantly add to the model and can be dropped leaving the couplings from anticipatory processing to decentering. Model 3 tested the opposite coupling, the model with only the coupling from decentering leading to anticipatory processing. Comparing this model to Model 1, the chi-square difference test was significant (p < .001), indicating that removing the coupling of anticipatory processing leading to decentering did significantly degrade the model fit and therefore this coupling should be retained, providing evidence that anticipatory processing may be a leading indicator of change in decentering. Finally, the model with no couplings (Model 4) was compared to Model 1 (the base model). As expected, the significant chi-square difference test (p < .001) indicated that removing both couplings significantly degraded the model fit from the base model. Similarly, Model 4 also provided a significant degradation in fit compared to Model 2 (Δχ2/Δdf = 14.77/1, p < .001). Taken together, Model 2, with couplings from anticipatory processing to decentering, was retained as the best fitting, most parsimonious model (see Table 6), indicating that anticipatory processing is a leading indicator of change in decentering, while decentering is not a leading indicator of change in anticipatory processing. Similar to the parallel process model, there was a medium sized correlation between the slopes of AP and EQ, although in this model this correlation did not reach statistical significance.
Table 6.
Parameter Estimates for the Best-Fitting Model with Couplings from Anticipatory Processing (AP) to Decentering (EQ)
| AP | EQ | |
|---|---|---|
| Parameter | Estimate (p) | Estimate (p) |
| Loading α | 1.0 | 1.0 |
| Proportion β | −0.10 (.09) | −0.18 (.007) |
| Coupling γ | -- | −0.90 (.002) |
| (AP→) | ||
| Correlations | ||
| ρis | .24 (.34) | .62 (<.001) |
| ρyi,xi ρyi,xs | .18 (.27) | .59 (<.001) |
| ρys,xi ρys,xs | .005 (.98) | .38 (.06) |
Note. AP = Anticipatory processing question from the Weekly Assessment; EQ = decentering subscale of the Experiences Questionnaire. ρis = AP intercept with AP slope or EQ intercept with EQ slope; ρyi,xi = AP intercept with EQ intercepts; ρyi,xs = AP intercept with EQ slope; ρys,xi = AP slope with EQ intercept; ρys,xs = AP slope with EQ slope.
Discussion
As the field continues to approach questions about how and why treatment works, we need to have methods for examining the relations between interacting mechanisms. This paper demonstrates one approach to examining the interplay of two potential mechanisms of action (decentering and anticipatory processing) across Cognitive Behavioral Group Therapy for social anxiety disorder. As a first step, we were interested in whether these two mechanisms did indeed change over the course of therapy. As was hypothesized, decentering increased and anticipatory processing decreased significantly over the course of therapy. This provides evidence that treatment may be impacting these mechanisms; however, it is important to remember that this is not a controlled design in this study and so the possibility remains that these changes were due to factors other than the treatment itself. Additionally, the reliance on a single item to measure anticipatory processing limits the conclusions that can be made from this study. Nonetheless, it is important to demonstrate that these mechanisms are changing before further examining the interplay between the two mechanisms.
In the next step, we examined whether changes in decentering and anticipatory processing were in fact related to outcome. For a variable to be a mechanism of treatment and not just a facilitative process, it is important to show that it does in fact impact outcome directly. In this study, there were moderate to large associations between two measures of treatment outcome (clinician rated CSR and self-report LSAS) and change in anticipatory processing and decentering. Relatedly, the change in decentering accounted for 10.8% to 22% of the variance in outcome, while anticipatory processing accounted for an even larger 17.2% to 43.3% of the variance in outcome. In other words, the greater the increase in decentering that clients experienced across treatment, the lower their social anxiety scores were at post-treatment. This is similar to what was reported in the previous outcome paper for this study (Hayes-Skelton & Lee, 2018). Consistent with the previous research on anticipatory processing (i.e., Hedman et al., 2013), a decrease in anticipatory processing was associated with lower social anxiety scores at post-treatment following this group CBT. These results support our hypothesis that both changes in anticipatory processing and decentering are related to outcome in this treatment and support further investigation of the interplay of these two mechanisms.
After establishing that anticipatory processing and decentering did change across treatment and that they were both related to outcome in the expected direction, we then examined our primary aim of the paper – the interplay between anticipatory processing and decentering. We used two different methods for examining this question: a parallel process model and a bivariate latent difference score model. The parallel process model is an extension of the linear growth models used to examine whether the proposed mechanisms did change over the course of treatment by estimating the growth parameters for decentering and anticipatory processing simultaneously. This analysis showed that increasing decentering was correlated with decreasing anticipatory processing. This relatively straightforward analysis demonstrates the association between these two processes. As hypothesized, this shows that as anticipatory processing decreases, decentering is increasing indicating that these two processes are related to each other. However, in the parallel process model, change is modeled over the same time periods which does not allow us to address questions about timing or the influence of one variable on the other.
Therefore, we then ran the bivariate latent difference score model which, though still associative, does have an ordering component so that we are better able to evaluate whether change in one of these mechanisms is as leading indicator of change in the other. These models showed that anticipatory processing was a leading indicator of decentering, but not the reverse. This indicates that changes in anticipatory processing predicted subsequent changes in decentering. It may be that as anticipatory processing decreases, the individual spends less time engaged in repetitive negative thoughts and this allows more cognitive resources to be directed towards taking the wider, more objective perspective characteristic of decentering. In support of this hypothesis, Mills and colleagues (2014) suggest that one consequence of anticipatory processing is that it consumes cognitive resources (i.e., Judah, Grant, Mills, & Lechner, 2013) which then results in the individual resorting to more automatic processes to incorporate information (i.e., Teachman, Joormann, Steinman, & Gotlib, 2012). From this perspective, consciously shifting to a more decentered perspective may be difficult until some of the cognitive resources that are being used for anticipatory processing are freed. Future research is needed to determine whether there is a particular threshold that anticipatory processing needs to cross to potentially free up the cognitive resources for decentering to occur. These conclusions differ from what we may interpret if we had found the reverse pattern – that decentering is a leading indicator of anticipatory processing. Being able to differentiate the ordering of these two potential mechanisms allows us to better understand how this CBT treatment may be leading to change for clients and also points us towards future directions for treatment.
This conclusion does not speak to interplay of these mechanisms in other treatments or with other approaches. As Hedman and colleagues (2013) theorize, the emphasis on cognitive restructuring in CBGT places a particularly strong focus on changing anticipatory processing in this treatment approach. Therefore, it is not a surprise that anticipatory processing is a leading indicator in this treatment. More research is needed to see whether anticipatory processing precedes decentering in other treatments, such as acceptance-based approaches. If anticipatory processing precedes change in decentering across treatment approaches, then this would indicate that more of a focus should be placed on what skills lead to these changes in anticipatory processing. Using frequent, brief assessments of anticipatory processing would allow clinicians to monitor whether anticipatory processing is changing and could give an early indicator of potentially poor treatment response.
While the BLDS approach showed that changes in anticipatory processing preceded changes in decentering, this analysis still only focused on two mechanisms. Within this data, the fit statistics were not strong, which is likely an indication that we are not fully capturing the complexity of the pattern of these mechanisms over the course of therapy. For example, these analyses did not show when in therapy these changes were occurring. Given the small sample size, change was modeled in the same way for all clients and the amount of change between each session was constrained to be the same across therapy. With larger samples, these constraints could be relaxed as it is likely that more change is occurring during some phases of therapy than in others. Similarly, with a larger sample it would also be possible to examine whether this pattern of change holds for all clients or whether there are different patterns of change that get obscured when we look at group averages. Additionally, other predictor variables or covariates could be included in this model to more fully capture the change process. For example, if it is not changes in decentering that lead to changes in anticipatory processing, what is it that allows for these changes in anticipatory processing? Future research could model the sequence and interplay of several processes and mechanisms over the course of therapy. Future studies could also examine whether change in anticipatory processing is sufficient for a positive outcome in this treatment or if the positive outcome comes through decentering. Similarly, because of the data available in this study, the focus here was on anticipatory processing; however, future research would benefit from also examining the larger construct of repetitive negative thinking as this would more broadly capture the cognitive processes involved in social anxiety.
While this study had a small sample size, because of the frequency of assessments, we were able to successfully capture these more complex models. From a design perspective, it is important to have these regular assessments to examine questions about the timing and influence of change. However, the frequent assessments have to be balanced against participant burden. In this case, a single item was used to capture anticipatory processing; however, this approach has several limitations. For example, while the item does have face validity, it is a single item of a complex construct. This item has also not been previously validated and so conclusions should be interpreted tentatively.
With all of these limitations aside, these analyses allowed us to move beyond questions about whether a single mechanism changes over time and whether it is related to outcome by also allowing us to examine how two mechanisms relate to each other. Here we found that changes in anticipatory processing were a leading indicator of changes in decentering. While this finding needs to be replicated, particularly given that anticipatory processing was measured with a single item, and also examined in other treatment approaches, it does inform treatment. For example, within this cognitive behavioral approach, one may not expect decentering to happen until some changes are occurring in anticipatory processing. While changes in decentering may be an indication that the client is moving towards a positive treatment outcome, within this treatment, these changes may be secondary to the cognitive changes reflected in anticipatory processing. Clinically, this supports continued focus on targeting the anticipatory rumination of social anxiety directly as it may be that the beneficial changes seen in decentering are following the decreases in rumination. Consistent with a CBT model, it is likely the cognitive restructuring exercises and the new learning from exposure exercises that is leading to the changes in anticipatory processing; however, further research is needed to fully understand what processes or mechanisms lead to changes in anticipatory processing to more fully capture the sequence of change across CBT for social anxiety.
Supplementary Material
Figure 1.
A bivariate latent difference score model including couplings in both directions. Y[t] and X[t] = observed scores at time t. y[t] and x[t] = latent true scores at time t. Δy[t] and Δx[t] = latent change scores at t. yi and xi = initial scores. ys and xs = slopes. Triangle = constant. α = slope parameter (= 1). β = autoproportional parameter. γ = coupling parameter.
Highlights.
Study examined the relation between decentering and anticipatory processing over CBGT
Bivariate Latent Difference Score models were used to examine these mechanisms
Anticipatory processing was a leading indicator of decentering, but not the reverse
Reducing anticipatory processing may free up cognitive resources for decentering
Acknowledgments
Disclosure Statement
Author Note: This work was supported by National Institute of Mental Health Grant No. MH085060 awarded to the first author. The authors thank the large team that made this project possible. Finally, we would like to thank the clients, without their openness and courage this work would not be possible.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Arditte KA, Shaw AM, & Timpano KR (2016). Repetitive negative thinking: A transdiagnostic correlate of affective disorders. Journal of Social and Clinical Psychology, 35, 181–201. doi: 10.1521/jscp.2016.35.3.181 [DOI] [Google Scholar]
- Baker SL, Heinrichs N, Kim HJ, & Hofmann SG (2002). The Liebowitz social anxiety scale as a self-report instrument: A preliminary psychometric analysis. Behaviour Research and Therapy, 40, 701–715. doi: 10.1016/S0005-7967(01)00060-2 [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, & Emery G (1979). Cognitive therapy of depression New York, NY: Guilford Press. [Google Scholar]
- Bernstein A, Hadash Y, Lichtash Y, Tanay G, Shepherd K, & Fresco DM (2015). Decentering and related constructs: A critical review and metacognitive processes model. Perspectives on Psychological Science, 10, 599–617. doi: 10.1177/1745691615594577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bieling PJ, Hawley LL, Bloch RT, Corcoran KM, Levitan RD, Young LT, … Segal ZV (2012). Treatment-specific changes in decentering following mindfulness-based cognitive therapy versus antidepressant medication or placebo for prevention of depressive relapse. Journal of Consulting and Clinical Psychology, 80, 365–372. doi: 10.1037/a0027483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, … Devins G (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11, 230–241. doi: 10.1093/clipsy.bph077 [DOI] [Google Scholar]
- Brown TA, DiNardo PA, & Barlow DH (1994). Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV) San Antonio, TX: Psychological Corporation. [Google Scholar]
- Brown TA, DiNardo PA, Lehmann CL & Campbell LA (2001). Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology, 110, 49–58. doi: 10.1037/0021-843X.110.1.49 [DOI] [PubMed] [Google Scholar]
- Brown M, & Stopa L (2007). Does anticipation help or hinder performance in a subsequent speech? Behavioural and Cognitive Psychotherapy, 35(2), 133–147. doi: 10.1017/S1352465806003481 [DOI] [Google Scholar]
- Clark DM, & Wells AA (1995). A cognitive model of social phobia. In Heimberg RG, Liebowitz MR, Hope DA, & Schneier FR (Eds.), Social Phobia: Diagnosis, assessment, and treatment (pp. 69–93). New York, NY: Guilford Press. [Google Scholar]
- Ehring T, Zetsche U, Weidacker K, Wahl K, Schofeld S, & Ehlers A (2011). The Perseverative Thinking Questionnaire: Validation of a content-independent measure of repetitive negative thinking. Journal of Behavior Therapy and Experimental Psychiatry, 42, 225–232. doi: 10.1016/j.jbtep.2010.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer E, & McArdle JJ (2003). Alternative structural models for multivariate longitudinal data analysis. Structural Equation Modeling, 10, 493–524. doi: 10.1207/S15328007SEM1004_1 [DOI] [Google Scholar]
- Forman EM, Chapman JE, Herbert JD, Goetter EM, Yuen EK, & Moitra E (2012). Using session-by-session measurement to compare mechanisms of action for acceptance and commitment therapy and cognitive therapy. Behavior therapy, 43(2), 341–354. 10.1016/j.beth.2011.07.004 [DOI] [PubMed] [Google Scholar]
- Fresco DM, Moore MT, van Dulmen MH, Segal ZV, Ma SH, Teasdale JD, & Williams JMG (2007). Initial psychometric properties of the Experiences Questionnaire: Validation of a self-report measure of decentering. Behavior Therapy, 38, 234–246. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Segal ZV, Buis T, & Kennedy S (2007). Relationship of posttreatment decentering and cognitive reactivity to relapse in major depression. Journal of Consulting and Clinical Psychology, 75, 447–455. doi: 10.1037/0022-006X.75.3.447 [DOI] [PubMed] [Google Scholar]
- Grimm KJ, An Y, McArdle JJ, Zonderman AB, & Resnick SM (2012). Recent changes leading to subsequent changes: Extensions of multivariate latent difference score models. Structural Equation Modeling, 19, 268–292. doi: 10.1080/10705511.2012.659627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes-Skelton SA, Calloway A, Roemer L, & Orsillo SM (2015). Decentering as a common mechanism across two therapies for generalized anxiety disorder. Journal of Consulting and Clinical Psychology, 83, 395–404. doi: 10.1016/j.beth.2006.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes-Skelton SA, & Lee CS (2018). Changes in decentering across Cognitive Behavioral Group Therapy for social anxiety disorder. Behavior Therapy, 49, 809–822. doi: 10.1016/j.beth.2018.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedman E, Mörtberg E, Hesser H, Clark DM, Lekander M, Andersson E, & Ljótsson B (2013). Mediators in psychological treatment of social anxiety disorder: Individual cognitive therapy compared to cognitive behavioral group therapy. Behaviour Research and Therapy, 51, 696–705. doi: 10.1016/j.brat.2013.07.006 [DOI] [PubMed] [Google Scholar]
- Heimberg RG, & Becker RE (2002). Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies New York, NY: The Guilford Press. [Google Scholar]
- Heimberg RG, & Ritter MR (2008). Cognitive behavioral therapy and acceptance and commitment therapy for the anxiety disorders: two approaches with much to offer. Clinical Psychology: Science and Practice, 15, 296–298. doi: 10.1111/j.1468-2850.2008.00140.x [DOI] [Google Scholar]
- Herbert JD, & Cardaciotto LA (2005). An acceptance and mindfulness-based perspective on social anxiety disorder. In Acceptance and mindfulness-based approaches to anxiety (pp. 189–212). New York, NY: Springer. doi: 10.1007/0-387-25989-9_8 [DOI] [Google Scholar]
- Herbert JD, Forman EM, Kaye JL, Gershkovich M, Goetter E, Yuen EK, … Marando-Blanck S (2018). Randomized controlled trial of acceptance and commitment therapy versus traditional cognitive behavioral therapy for social anxiety disorder: Symptomatic and behavioral outcomes. Journal of Contextual Behavioral Science, 9, 88–96. doi: 10.1016/j.jcbs.2018.07.008 [DOI] [Google Scholar]
- Hinrichsen H, & Clark DM (2003). Anticipatory processing in social anxiety: Two pilot studies. Journal of Behaviour Therapy and Experimental Psychiatry, 34, 205–218. doi: 10.1016/S0005-7916(03)00050-8 [DOI] [PubMed] [Google Scholar]
- Hodson KJ, McManus FV, Clark DM, & Doll H (2008). Can Clark and Wells’ (1995) cognitive model of social phobia be applied to young people? Behavioural and Cognitive Psychotherapy, 363, 449–461. doi: 10.1017/S1352465808004487 [DOI] [Google Scholar]
- Hofmann SG (2007). Cognitive factors that maintain social anxiety disorder: A comprehensive model and its treatment implications. Cognitive Behaviour Therapy, 36, 193–209. doi: 10.1080/16506070701421313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judah MR, Grant DM, Mills AC, & Lechner WV (2013). The neural correlates of impaired attentional control in social anxiety: An ERP study of inhibition and shifting. Emotion, 13, 1096–1106. doi: 10.1037/a0033531 [DOI] [PubMed] [Google Scholar]
- Kaiser RH, Andrews-Hanna JR, Metcalf CA, & Dimidjian S (2015). Dwell or decenter? Rumination and decentering predict working memory updating after interpersonal criticism. Cognitive Therapy and Research, 39, 744–753. doi: 10.1007/s10608-015-9697-1 [DOI] [Google Scholar]
- Kazdin AE (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432 [DOI] [PubMed] [Google Scholar]
- Liebowitz MR (1987). Social phobia. Modern Problems of Pharmacopsychiatry, 22, 141–173. [DOI] [PubMed] [Google Scholar]
- McArdle JJ (2009). Latent variable modeling of differences and changes with longitudinal data. Annual Review of Psychology, 60, 577–605. doi: 10.1146/annurev.psych.60.110707.163612 [DOI] [PubMed] [Google Scholar]
- McArdle JJ, & Nesselroade JR (1994). Using multivariate data to structure developmental change (pp. 223–267). In Cohen SH & Reese HW (eds). Life-span developmental psychology: Methodological contributions Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Mills AC, Grant DM, Lechner WV, & Judah MR (2013). Psychometric properties of the anticipatory social behaviours questionnaire. Journal of Psychopathology and Behavioral Assessment, 35, 346–355. doi: 10.1007/s10862-013-9339-4 [DOI] [Google Scholar]
- Mills AC, Grant DM, Lechner WV, & Judah MR (2014). Consequences of anticipatory processing on cognitive symptoms of social anxiety. Anxiety, Stress, and Coping, 27, 394–409. doi: 10.1080/10615806.2013.866229 [DOI] [PubMed] [Google Scholar]
- Mori M, & Tanno Y (2015). Mediating role of decentering in the associations between self-reflection, self-rumination, and depressive symptoms. Psychology, 6, 613. doi: 10.4236/psych.2015.65059 [DOI] [Google Scholar]
- Muthén LK, & Muthén B (2010). Mplus user’s guide (6th ed.). Los Angeles: Muthén & Muthén. doi: 10.1177/1094428105284949 [DOI] [Google Scholar]
- Naragon-Gainey K, & DeMarree KG (2017). Structure and validity of measures of decentering and defusion. Psychological Assessment, 29, 935. doi: 10.1037/pas0000405 [DOI] [PubMed] [Google Scholar]
- Penney ES, & Abbott MJ (2014). Anticipatory and post-event rumination in social anxiety disorder: A review of the theoretical and empirical literature. Behaviour Change, 31, 79–101. [Google Scholar]
- Rapee RM, & Heimberg RG (1997). A cognitive-behavioral model of anxiety in social phobia. Behavior Research and Therapy, 35, 741–756. doi: 10.1016/S0005-7967(97)000223 [DOI] [PubMed] [Google Scholar]
- Roemer L, & Orsillo SM (2009). Mindfulness- and acceptance-based behavioral therapies in practice New York: Guilford Press. [DOI] [PubMed] [Google Scholar]
- Safran JD, & Segal ZV (1990). Interpersonal process in cognitive therapy New York: Basic Books. [Google Scholar]
- Satorra A, & Bentler PM (2001). A scaled difference chi-square test statistic for moment structure analysis. Psychometrika, 66, 507–514. doi: 10.1007/BF02296192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teachman BA, Joormann J, Steinman SA, & Gotlib IH (2012). Automaticity in anxiety disorders and major depressive disorder. Clinical Psychology Review, 32, 575–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, & Segal ZV (2002). Metacognitive awareness and prevention of relapse in depression: Empirical evidence. Journal of Consulting and Clinical Psychology, 70(2), 275. doi: 10.1037//0022-006X.70.2.275 [DOI] [PubMed] [Google Scholar]
- Vassilopoulos SP (2004). Anticipatory processing in social anxiety. Behavioural and Cognitive Psychotherapy, 32, 303–311. doi: 10.1017/S1352465804001377 [DOI] [Google Scholar]
- Wong QJJ (2016). Anticipatory processing and post-event processing in social anxiety disorder: An update on the literature. Australian Psychologist, 51, 105–113. doi: 10.1111/ap.12189 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.