Abstract
PURPOSE
Coping with symptoms related to cancer treatment is challenging for pediatric patients with cancer and their caregivers. Additionally, caring for pediatric patients requires specialized expertise to incorporate age-appropriate interventions to improve outcomes. Despite the increase in pediatric inpatient integrative medicine (IM) therapies, there is a paucity of knowledge about whether the utilization of IM therapies differs by patient age.
METHODS
We conducted a retrospective analysis on IM utilization among pediatric inpatients between 2008 and 2016 in a tertiary urban cancer center using electronic medical records. Multivariable logistic regression models examined the relationship between age and specific type of IM utilization, adjusting for specific demographic factors.
RESULTS
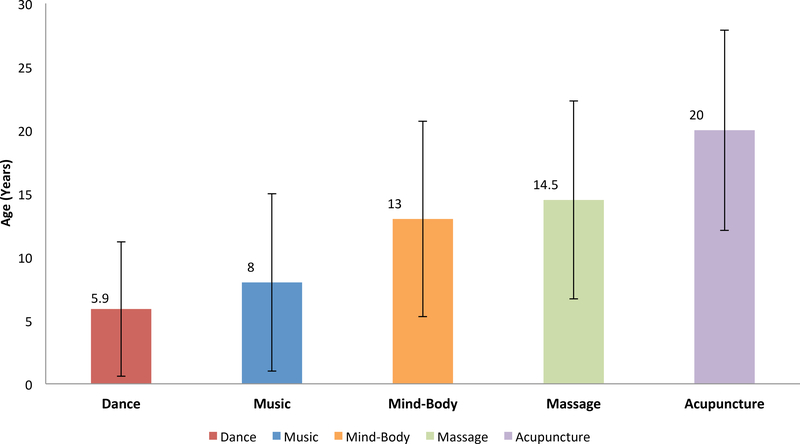
Between 2008 and 2016, the pediatric inpatient IM service had 20,686 visits and treated 1,877 unique patients. A significant age difference (p<0.001) by modality was noted: dance therapy (mean age±standard deviation: 5.9±5.3 years), music therapy (8.0±7.0 years), mind-body therapies (13.0±7.7 years), massage (14.5±7.8 years), and acupuncture (20.0±7.9 years). In multivariable analysis, the association between age and use of specific IM therapies remained significant (p<0.001 for all).
CONCLUSION
Specific types of inpatient IM therapy usage significantly differed by the age of pediatric patients with cancer; therefore, designing and providing age-appropriate IM interventions with consideration for developmental stage are needed to ensure that the most appropriate and effective therapies are provided to children with cancer.
Keywords: Child, Dance Therapy, Integrative Medicine, Music Therapy, Inpatients, Massage, Mind-Body Therapies, Acupuncture, Pediatric Oncology
INTRODUCTION
Cancer is the leading cause of death by disease for children aged 1–19 years in the United States.1 Each year, approximately 15,780 new cases are diagnosed and 1,960 children and adolescents die from cancer.2 Although advances in cancer treatment over the past 40 years have improved the 5-year childhood cancer survival rate from 10% to nearly 90%,3,4 childhood cancer incidence rates have continuously increased since 1975.4,5
Pediatric patients with cancer suffer from a high level of symptom burden related to their cancer, such as pain, fatigue, dyspnea, and insomnia.6 Moreover, invasive medical procedures like bone marrow aspiration, biopsy, and lumbar puncture can cause pain, fear, anxiety, and distress before, during, and after treatment.7 Many pediatric patients with cancer may live with these symptoms for years, even after completion of treatment.6 Furthermore, these symptoms place substantial emotional and physical burdens on patients’ parents and/or caregivers.8 Physical and emotional symptom palliation,9 and the provision of emotional support10 for pediatric patients throughout their procedures and treatments,11 are essential standards in caring for children with cancer and their families.
According to the National Center for Complementary and Integrative Health (NCCIH), integrative medicine (IM) brings together conventional and complementary treatments (e.g. acupuncture, massage, and music therapy) in a coordinated approach with the medical team.12 Early evidence indicated that IM therapies may be helpful in the management of cancer-related symptoms for children,13 and a recent systematic review concluded there is good evidence that IM can alleviate symptoms associated with pediatric cancer and treatment, particularly painful procedures.14 Estimates of utilization of IM therapies for symptom management by childhood patients with cancer range from 6% to 91%,15 and evidence suggests that many of these modalities benefit this young population. Specifically, studies have demonstrated that dance therapy’s physical and emotional benefits may reduce cancer-related symptoms like trauma, stress, and fatigue that children with cancer experience as part of the hospitalization process.16,17 Mind-body therapies like meditation, self-hypnosis, guided imagery, and yoga may effectively decrease pain, nausea, and vomiting in children.18–20 Inpatient music therapy has been demonstrated to improve pediatric patients’ states of mind21 and immune systems.22 Massage has been shown to decrease depressed mood, and increase white blood cell and neutrophil counts in pediatric patients with cancer.23,24 Lastly, acupuncture has been shown to reduce chemotherapy-induced nausea and vomiting in children.25
Despite this growing body of evidence indicating that IM therapies may be effective for cancer symptom management, several key barriers to pediatric research exist. According to the American Cancer Society, the rarity of childhood cancer challenges research development in this field by introducing added cost and complexity to the research process.26 Further, age plays an important role in conducting pediatric research since the distribution of the most common cancer types and developmental stages (i.e. motor, social, or mental maturity processes) in childhood vary by age, making eligibility criteria and appropriate assessment complex.26 Consequently, there is a paucity of knowledge about whether IM therapies use differs by patient characteristics like age or developmental stage. This information is important to better understand pediatric integrative oncology and maximize IM’s effectiveness within this population.
Thus, this study’s primary aim was to evaluate the association between age and specific IM modality utilization among pediatric inpatients. As a secondary aim, we evaluated IM modality utilization by other socio-demographic characteristics like sex and race.
METHODS
Study Setting
Since 1999, Memorial Sloan Kettering Cancer Center (MSK), a tertiary urban cancer center, has provided IM therapies including acupuncture, dance therapy, massage, music therapy, and mind-body therapies (breath awareness, meditation, yoga) to help patients with cancer cope with cancer-related symptoms. In the pediatric inpatient setting, IM therapists receive the majority of referrals from physicians, nurses, social workers, and child life specialists. After receiving a referral, IM therapists visit the patient’s room and provide the IM service individually at the bedside. For example, music therapy sessions are conducted at the bedside utilizing live music with guitar, voice, keyboard, and percussion instruments. The music therapist may aim to engage the patient and caregivers through song choice, active listening, singing and playing instruments, instrumental improvisation, song writing, or lyric improvisations. Instruments are disinfected between interactive music therapy sessions. IM therapists also provide dance and mind-body therapy group sessions. Specifically, dance therapists provide different group sessions by patient age. In sessions with infants, toddlers and preschoolers, dance therapists focus on building patients’ attachment relationships with their parents/caregivers using dance, rhythm, and body-to-body physical engagement. With older children and young adults who can participate in dance therapy without their caregiver’s help, dance therapists aim to promote body awareness, self-expression, and socialization through embodied explorations in group dances with other peers. Pediatric inpatients receive all IM services free of charge due to donations from several organizations and MSK’s financial support.
Data Source
The MSK Institutional Database (IDB) provided electronic medical records (EMR) data on all pediatric patients who used an inpatient IM service since the implementation of the database in 2008. This data includes patient ID, date of birth, age at appointment, gender, race, ethnicity, date of appointment, type of modality, visit type description, SEER categories of cancer, tumor site code, and tumor histology code. MSK’s institutional review board approved the retrospective study protocol.
Statistical Analysis
We calculated descriptive statistics as frequencies and percentages and conducted chi-square tests examining demographic characteristics associated with each type of IM modality (i.e. dance, music, mind-body, massage, acupuncture). Multivariable logistic regression analyses were conducted to evaluate the relationship between age at appointment and specific type of IM modality utilization, adjusting for race and gender. The primary outcome was “yes” or “no” for each IM modality. Based on the Centers for Disease Control (CDC) Child Developmental Milestones,27 we created age-at-appointment categories for patients as follows: 0–2 year olds were classified as “Infants and Toddlers,” 3–5 year olds as “Preschoolers,” 6–11 year olds as “Middle Childhood,” 12–17 year olds as “Adolescents,” and those in the 18–39 year range were classified as “Young Adults.” These are chronological age-based stages and cannot reflect baseline or acquired developmental delays or regression sometimes seen in children with serious illnesses. However, we used these age-based milestones as a proxy for developmental stages in this retrospective analysis. For race, patients were grouped as “White,” “Black,” “Asian,” or “Other.” All statistical tests were two-sided with p<0.01 indicating statistical significance (Bonferroni Adjustment) to evaluate the five IM modalities. All analyses were performed using STATA version 12 (STATA Corp, Texas, USA).
RESULTS
From 2008 to 2016, MSK’s pediatric inpatient IM service had 20,686 visits and treated 1,877 unique patients. As shown in Table 1, the mean age±standard deviation at appointment was 9.6±7.9 years. Among the 1,877 unique patients, 52% were male and 73% were white. Dance therapy was the most frequently used IM service (n=9,305, 45.0%), followed by massage (n=5,449, 26.3%), music therapy (n=4,704, 22.7%), mind-body therapies (n=912, 4.4%), and acupuncture (n=316, 1.5%). Patients with neuroblastoma used IM therapies the most (n=432, 23.0%), followed by those with leukemia (n=338, 18.0%), soft tissue sarcoma (n=199, 10.6%), and bone/joint cancer (n=190, 10.1%). A significant age-at-appointment difference (p<0.001) was observed by modality for dance therapy (mean age ± SD: 5.9±5.3 years), music therapy (8.0±7.0 years), mind-body therapies (13.0±7.7 years), massage (14.5±7.9 years), and acupuncture (20.0±7.9 years) [Figure 1].
TABLE 1.
Patient characteristics by integrative medicine modality
| Dance (n=1107) | Music (n=793) | Mind-Body (n=296) | Massage (n=848) | Acupuncture (n=60) | Total (n=1877) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % |
| Age at Appointment (years) | ||||||||||||
| Mean (SD) | 5.9 (5.3) | 8.0 (7.0) | 13.0 (7.7) | 14.5 (7.8) | 20.0 (7.9) | 9.6 (7.9) | ||||||
| Median | 4 | 6 | 11 | 15 | 20 | 7 | ||||||
| Age at Appointment Categories | ||||||||||||
| Infants and Toddlers (0–2 years) | 308 | 27.9 | 190 | 24.0 | 6 | 2.0 | 56 | 6.6 | 2 | 3.3 | 367 | 19.6 |
| Preschoolers (3–5 years) | 372 | 33.6 | 204 | 25.7 | 49 | 16.6 | 69 | 8.1 | 1 | 1.7 | 442 | 23.5 |
| Middle Childhood (6–11 years) | 276 | 24.9 | 181 | 22.8 | 95 | 32.1 | 178 | 21.0 | 5 | 8.3 | 407 | 21.7 |
| Adolescents (12–17 years) | 99 | 8.9 | 126 | 15.9 | 69 | 23.3 | 242 | 28.6 | 9 | 15.0 | 313 | 16.7 |
| Young Adults (18–39 years) | 52 | 4.7 | 92 | 11.6 | 77 | 26.0 | 303 | 35.7 | 43 | 71.7 | 348 | 18.5 |
| Race | ||||||||||||
| White | 784 | 70.8 | 527 | 66.5 | 209 | 70.6 | 650 | 76.7 | 45 | 75.0 | 1364 | 72.7 |
| Black | 136 | 12.3 | 119 | 15.0 | 35 | 11.8 | 102 | 12.0 | 2 | 3.3 | 220 | 11.7 |
| Asian | 120 | 10.8 | 89 | 11.2 | 38 | 12.9 | 55 | 6.5 | 10 | 16.7 | 186 | 9.9 |
| Other | 67 | 6.1 | 58 | 7.3 | 14 | 4.7 | 41 | 4.8 | 3 | 5.0 | 107 | 5.7 |
| Gender | ||||||||||||
| Male | 515 | 46.5 | 399 | 50.3 | 172 | 57.1 | 477 | 56.0 | 31 | 50.8 | 978 | 52.1 |
| Female | 592 | 53.5 | 394 | 49.7 | 124 | 42.9 | 371 | 44.0 | 29 | 49.2 | 899 | 47.9 |
| Cancer Type | ||||||||||||
| Bones and Joints | 47 | 4.2 | 61 | 7.7 | 44 | 14.9 | 157 | 18.5 | 19 | 31.7 | 190 | 10.1 |
| Brain and Other Nervous System | 86 | 7.8 | 54 | 6.8 | 11 | 3.7 | 52 | 6.1 | 2 | 3.3 | 140 | 7.6 |
| Digestive System | 42 | 3.8 | 35 | 4.4 | 8 | 2.7 | 27 | 3.2 | 4 | 6.7 | 74 | 3.9 |
| Eye and Orbit | 74 | 6.7 | 29 | 3.6 | 2 | 0.7 | 12 | 1.4 | 0 | 0.0 | 87 | 4.6 |
| Genitourinary System | 39 | 3.5 | 34 | 4.3 | 10 | 3.4 | 26 | 3.1 | 4 | 6.7 | 70 | 3.7 |
| Leukemia | 189 | 17.1 | 213 | 26.9 | 64 | 21.6 | 177 | 20.9 | 7 | 11.7 | 338 | 18.0 |
| Lymphoma | 26 | 2.3 | 37 | 4.7 | 23 | 7.8 | 84 | 9.9 | 1 | 1. | 114 | 6.1 |
| Neuroblastoma | 386 | 34.9 | 137 | 17.3 | 63 | 21.3 | 115 | 13.6 | 5 | 8.3 | 432 | 23.0 |
| Soft Tissue including Heart | 82 | 7.4 | 72 | 9.1 | 29 | 9.8 | 114 | 13.4 | 13 | 21.7 | 199 | 10.6 |
| Other | 44 | 4.0 | 28 | 3.5 | 17 | 5.7 | 39 | 4.6 | 3 | 5.0 | 79 | 4.2 |
| Unknown Primary | 92 | 8.3 | 93 | 11.7 | 25 | 8.4 | 45 | 5.3 | 2 | 3.3 | 154 | 8.2 |
FIGURE 1. Patients’ mean age by integrative medicine modality.
This figure shows a significant age difference (p<0.001) by modality: dance therapy (mean age±standard deviation: 5.9±5.3 years), music therapy (8.0±7.0 years), mind-body therapies (13.0±7.7 years), massage (14.5±7.8 years), and acupuncture (20.0±7.9 years).
Table 2 shows the estimates from multivariable modeling of the relationship between age-at-appointment and specific type of inpatient IM modality after adjusting for race and gender. Specifically, in the adjusted models for dance and music therapy, as patients’ age group increased, the odds for using each modality type decreased linearly. Infants and toddlers had 39 times higher odds of using dance therapy (adjusted odds ratio (AOR) 38.96, 95% Confidence Interval (CI) 25.34, 59.88, p<0.001) and three times higher odds of using music therapy (AOR 3.20, 95% CI 2.32, 4.40, p<0.001) compared to young adults. For mind-body, massage, and acupuncture, the odds of modality use were significantly higher as the patients’ age group increased. Infants and toddlers had lower odds of using mind-body therapies (AOR 0.19, 95% CI 0.11, 0.32, p<0.001), massage (AOR 0.03, 95% CI 0.02, 0.05, p<0.001), and acupuncture (AOR 0.03, 95% CI 0.01, 0.15, p<0.001) compared to young adults.
TABLE 2.
Multivariate analysis for the relationship between patient characteristics and specific integrative medicine modality utilization
| Dance | Music | Mind-Body | Massage | Acupuncture | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | AOR | 95% CI | P-value | AOR | 95% CI | P-value | AOR | 95% CI | P-value | AOR | 95% CI | P-value | AOR | 95% CI | P-value |
| Age at Appointment Categories | |||||||||||||||
| Young Adults | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Adolescents | 2.86 | 1.93 – 4.25 | <0.001 | 1.81 | 1.3 – 2.53 | <0.001 | 0.95 | 0.65 – 1.39 | 0.80 | 0.49 | 0.33 – 0.73 | <0.001 | 0.25 | 0.12 – 0.51 | <0.001 |
| Middle Childhood | 14.32 | 9.82 – 20.88 | <0.001 | 1.99 | 1.46 – 2.73 | <0.001 | 0.97 | 0.68 – 1.39 | 0.89 | 0.12 | 0.08 – 0.17 | <0.001 | 0.09 | 0.03 – 0.23 | <0.001 |
| Preschoolers | 34.34 | 22.94 – 51.41 | <0.001 | 2.76 | 2.03 – 3.76 | <0.001 | 0.58 | 0.40 – 0.85 | 0.01 | 0.03 | 0.02 – 0.05 | <0.001 | 0.02 | 0.00 – 0.11 | <0.001 |
| Infants and Toddlers | 38.96 | 25.34 – 59.88 | <0.001 | 3.20 | 2.32 – 4.40 | <0.001 | 0.19 | 0.11 – 0.32 | <0.001 | 0.03 | 0.02 – 0.05 | <0.001 | 0.03 | 0.01 – 0.15 | <0.001 |
| Race | |||||||||||||||
| White | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Black | 1.39 | 0.97 – 1.99 | 0.07 | 1.91 | 1.42 – 2.56 | <0.001 | 1.02 | 0.69 – 1.52 | 0.91 | 0.81 | 0.57 – 1.15 | 0.23 | 0.28 | 0.07 – 1.17 | 0.08 |
| Asian | 1.01 | 0.68 – 1.49 | 0.96 | 1.34 | 0.98 – 1.83 | 0.07 | 1.69 | 1.13 – 2.51 | 0.01 | 0.49 | 0.33 – 0.73 | <0.001 | 2.37 | 1.12 – 5.03 | 0.03 |
| Other | 0.83 | 0.50 – 1.36 | 0.46 | 1.70 | 1.14 – 2.55 | 0.01 | 1.02 | 0.56 – 1.85 | 0.95 | 0.89 | 0.54 – 1.46 | 0.64 | 1.18 | 0.34 – 4.04 | 0.80 |
| Gender | |||||||||||||||
| Male | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Female | 1.99 | 1.58 – 2.52 | <0.001 | 1.07 | 0.88 – 1.29 | 0.50 | 0.78 | 0.6 – 1.01 | 0.06 | 0.73 | 0.59 – 0.92 | 0.01 | 1.20 | 0.70 – 2.05 | 0.51 |
In terms of race and gender, black patients had almost twice the odds of using music therapy compared to white patients (AOR=1.91, 95% CI 1.42, 2.56, p<0.001). Asians had higher odds of using acupuncture (AOR=2.37, 95% CI 1.12, 5.03, p=0.03) and mind-body therapies (AOR 1.69, 95% CI 1.13, 2.51, p=0.01) and lower odds of using massage (AOR 0.49, 95% CI 0.33, 0.73, p<0.001) compared to whites. Compared to males, females had significantly higher odds of using dance therapy (AOR 1.99, 95% CI 1.58, 2.52, p<0.001) and lower odds of using massage (AOR 0.73, 95% CI 0.59, 0.92, p=0.01).
DISCUSSION
In this study, we identified over 20,000 pediatric inpatient IM treatments among 1,877 unique patients, the largest cohort reported to date. Age differed substantially among different types of IM approaches – the youngest patients were more likely to receive dance and music therapy while adolescents and young adults were more likely to receive mind-body therapies, massage, and acupuncture. Patient’s biological and psychological development status affects their engagement with the IM therapy and potential outcomes. Therefore, age is an important factor when determining appropriate treatments.26,28 Our results highlight the need for cancer centers to consider a range of IM options to appeal to patients of different ages and developmental stages when building inpatient IM services for pediatric patients or when conducting pediatric IM intervention research.
In line with previous research, our results confirm older age is associated with acupuncture and massage use in pediatric patients.29,30 This same pattern of specific therapy utilization by age also appears to follow pediatric patients with cancer into survivorship.31 Interestingly, even though the benefits of acupuncture for cancer symptom management are well known,32–34 the acupuncture utilization rate among younger pediatric patients (1.5%) was limited in our study. Reasons for this may be due to the fact that many young children are more likely to fear needles, are unable to sit/lie still for an adequate period of time, or are less likely to request acupuncture services compared to young adults. These results coincide with a questionnaire-based study in which Tsao et al. examined treatment preferences for IM in children with chronic pain; they reported that older children were more likely than younger children to use acupuncture and massage.29 However, in contrast to our study, they did not find a significant age difference in mind-body therapies and creative arts therapy use. Analysis of our data revealed that younger children (0–11 years) comprised the largest proportion of patients who used creative arts therapy (86.4% of dance therapy patients and 72.5% of music therapy patients), and that utilization of these therapies was significantly correlated with age even after adjusting for gender and race. This disparate finding may be because Tsao et al. examined a narrower age range (8–18 years) than our study population (0–39 years).
Our findings confirm that younger children are more likely to use creative art therapies, like dance therapy (mean age 5.9 years) and music therapy (mean age 8.0 years). Previous studies have demonstrated that infants and toddlers who have received treatment for cancer tend to withdraw, digress in developmental milestones, and exhibit increased anxiety;35 therefore, dance and music therapy may be particularly suitable early interventions for these young patients. Furthermore, since dance therapy is movement- and body-focused, including extensive nonverbal communication, it may provide necessary support and reinforce secure attachment relationships between young patients and their parents as they participate in the therapy together.16 Music therapy can also enhance young patients’ ability to stay emotionally and socially engaged because it encourages them to contribute to the musical experience by singing or playing an instrument with their music therapist and/or parents.21 Further, since these therapies engage both the child and parents, they may enhance the parents’ abilities to cope with their own emotional distress from caring for their seriously ill child. Parent and child well-being have been closely linked in psychosocial outcomes research for both groups; parental coping is highly correlated to a child’s physical and emotional well-being, and a child’s adjustment to treatment is affected, in turn, by parental coping. Recognizing these important connections, providing support to parents in pediatric oncology settings has recently been recognized as an essential standard of psychosocial care for children with cancer and their families.36
Our study results demonstrate that as children with cancer get older, they begin using individualized therapies such as acupuncture, massage, and mind-body therapies more than group dance/music therapies. This may be because, in their early teenage years, children begin to develop mastery over their physical bodies (a developmental milestone that illness can disrupt), understand abstract ideas, and move toward a more mature sense of self.37 We found that early teenagers (mean age 13.0 years) most frequently used mind-body therapies, including breath awareness, meditation, and yoga. Development of the above-mentioned qualities, and sufficient cognitive ability, are necessary for engaging meaningfully with and deriving benefit from mind-body therapies.38 Further, massage and acupuncture require patients to be still and relax their bodies, which is likely why both therapies were used in older age groups (mean age 14.5 years for massage and 20.0 years for acupuncture).
Our findings underscore an interesting gap in existing literature. Despite the acceptability and high utilization of IM services across ages, developmental stages, genders, and races shown here, IM interventions have been largely missed as standard supportive care interventions for pediatric patients undergoing cancer treatment. Notably, the recently published “Standards of Psychosocial Care for Children with Cancer and Their Families” is a milestone in the development and improvement of psychosocial and supportive care programs for children with cancer and the research that informs them.39 However, IM is mentioned only as it applies to “procedural support” (providing distraction and relaxation to children before or during medical procedures).11 These standards were based on existing evidence and expert consensus, reflecting a lack of research clarifying the multidimensional benefits children and their families may gain from IM beyond procedural support. Such benefits may include clinically observed relaxation, distress reduction, and improvements in self-regulation, body image, and functioning for both young children and their parents.
We acknowledge several study limitations. First, this is a single-center study, limiting its generalizability because the patients are not representative of the entire population. Second, since most IM visits were initiated based on referrals from clinicians, clinician referral bias might confound the relationship between IM modality utilization and patient characteristics. Third, the rates of IM therapies delivered are reflective of programs with specific funding and should not be interpreted as “popularity” or a true reflection of patient demand. Lastly, we obtained data for this retrospective study directly from patients’ electronic medical charts, limiting our ability to examine other factors that may be associated with IM therapy use like patient/parent beliefs and real-time feedback regarding IM therapies and/or patients’ current symptoms.
In this retrospective study of over 1,800 pediatric and young adult cancer patients (ages 0–39 years), the largest pediatric oncology cohort treated with IM therapies reported to date, we found that patient age significantly impacted utilization of specific IM therapies, even after adjusting for other demographic factors. Younger children frequently used dance and music therapy, while adolescents and young adults were more likely to use individual therapies such as acupuncture, massage, and mind-body therapies. Our study highlights the importance of implementing a range of IM interventions with consideration for developmental appropriateness and patient/parent preference to ensure that the most suitable and effective therapies are available to help pediatric patients with cancer and their parents cope with the cancer experience.
Acknowledgments
This research is funded in part by grants from the National Cancer Institute / National Institutes of Health (P30-CA008748) and the National Center for Advancing Translational Sciences / National Institutes of Health (KL2TR002385), Gabrielle’s Angel Foundation for Cancer Research, Ukulele Kids Club, The Andrea Rizzo Foundation, Lydian Asset Foundation, Julien’s Project Ladybug Fund, Rabinovitz Fund, Robert Fund, Viennese Opera Ball, and by The Byrne Fund and the Translational Research and Integrative Medicine Fund at the Memorial Sloan Kettering Cancer Center. This content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
The authors would like to thank the patients, oncologists, nurses, and clinical staff for their contributions to this study. The authors would also like to thank Christina Seluzicki for her editorial contributions.
ABBREVIATIONS KEY
- IM
Integrative medicine
- NCCIH
National Center for Complementary and Integrative Health
- MSK
Memorial Sloan Kettering Cancer Center
- IDB
Institutional database
- EMR
Electronic medical record
- CDC
Centers for Disease Control
- AOR
Adjusted odds ratio
- CI
Confidence interva
Footnotes
CONFLICT OF INTEREST STATEMENT: None declared.
REFERENCES
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7–30. [DOI] [PubMed] [Google Scholar]
- 2.Ward E, DeSantis C, Robbins A, Kohler B, Jemal A. Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin. 2014;64(2):83–103. [DOI] [PubMed] [Google Scholar]
- 3.Ries LAG, Smith MA, Gurney J, et al. Cancer incidence and survival among children and adolescents: United States SEER Program 1975–1995. 1999. [Google Scholar]
- 4.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67(1):7–30. [DOI] [PubMed] [Google Scholar]
- 5.Hudson MM, Meyer WH, Pui C-H. Progress born from a legacy of collaboration. J Clin Oncol. 2015;33(27):2935–2937. [DOI] [PubMed] [Google Scholar]
- 6.Pai AL, Kazak AE. Pediatric medical traumatic stress in pediatric oncology: family systems interventions. Curr Opin Pediatr. 2006;18(5):558–562. [DOI] [PubMed] [Google Scholar]
- 7.Kuppenheimer WG, Brown RT. Painful procedures in pediatric cancer. A comparison of interventions. Clin Psychol Rev. 2002;22(5):753–786. [DOI] [PubMed] [Google Scholar]
- 8.Steele RG, Long A, Reddy KA, Luhr M, Phipps S. Changes in maternal distress and child-rearing strategies across treatment for pediatric cancer. J Pediatr Psychol. 2003;28(7):447–452. [DOI] [PubMed] [Google Scholar]
- 9.Weaver MS, Heinze KE, Kelly KP, et al. Palliative care as a standard of care in pediatric oncology. Pediatr Blood Cancer. 2015;62 Suppl 5:S829–S833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steele AC, Mullins LL, Mullins AJ, Muriel AC. Psychosocial interventions and therapeutic support as a standard of care in pediatric oncology. Pediatr Blood Cancer. 2015;62 Suppl 5:S585–S618. [DOI] [PubMed] [Google Scholar]
- 11.Flowers SR, Birnie KA. Procedural preparation and support as a standard of care in pediatric oncology. Pediatr Blood Cancer. 2015;62 Suppl 5:S694–S723. [DOI] [PubMed] [Google Scholar]
- 12.NCCIH. Complementary, Alternative, or Integrative Health: What’s In a Name? 2016; https://nccih.nih.gov/health/integrative-health-integrative. Accessed July 07, 2016.
- 13.Kelly KM. Complementary and alternative medical therapies for children with cancer. Eur J Cancer. 2004;40(14):2041–2046. [DOI] [PubMed] [Google Scholar]
- 14.Thrane S Effectiveness of integrative modalities for pain and anxiety in children and adolescents with cancer: a systematic review. J Pediatr Oncol Nurs. 2013;30(6):320–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bishop FL, Prescott P, Chan YK, Saville J, von Elm E, Lewith GT. Prevalence of complementary medicine use in pediatric cancer: a systematic review. Pediatrics. 2010;125(4):768–776. [DOI] [PubMed] [Google Scholar]
- 16.Cohen SO, Walco GA. Dance/movement therapy for children and adolescents with cancer. Cancer Pract. 1999;7(1):34–42. [DOI] [PubMed] [Google Scholar]
- 17.Mendelsohn J Dance/movement therapy with hospitalized children. Am J Dance Ther. 1999;21(2):65–80. [Google Scholar]
- 18.Redd WH, Montgomery GH, DuHamel KN. Behavioral intervention for cancer treatment side effects. J Natl Cancer Inst. 2001;93(11):810–823. [DOI] [PubMed] [Google Scholar]
- 19.Galantino ML, Galbavy R, Quinn L. Therapeutic effects of yoga for children: a systematic review of the literature. Pediatr Phys Ther. 2008;20(1):66–80. [DOI] [PubMed] [Google Scholar]
- 20.Carlson LE, Bultz BD. Mind-body interventions in oncology. Curr Treat Options Oncol. 2008;9(2–3):127–134. [DOI] [PubMed] [Google Scholar]
- 21.Barrera ME, Rykov MH, Doyle SL. The effects of interactive music therapy on hospitalized children with cancer: a pilot study. Psychooncology. 2002;11(5):379–388. [DOI] [PubMed] [Google Scholar]
- 22.Marwick C Leaving concert hall for clinic, therapists now test music’s’ charms’. JAMA. 1996;275(4):267–268. [PubMed] [Google Scholar]
- 23.Field T, Cullen C, Diego M, et al. Leukemia immune changes following massage therapy. J Bodyw Mov Ther. 2001;5(4):271–274. [Google Scholar]
- 24.Beider S, Moyer CA. Randomized controlled trials of pediatric massage: a review. Evid Based Complement Alternat Med. 2007;4(1):23–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reindl TK, Geilen W, Hartmann R, et al. Acupuncture against chemotherapy-induced nausea and vomiting in pediatric oncology. Support Care Cancer. 2006;14(2):172–176. [DOI] [PubMed] [Google Scholar]
- 26.Adamson P, Arons D, Baumberger J, Fleury M, Hoffman R, Leach D. Translating Discovery into Cures for Children with Cancer: Childhood Cancer Research Landscape Report. 2016. [Google Scholar]
- 27.Centers for Disease Control and Prevention (CDC). Child developmental: Middle childhood (6–8 years of age). January 3, 2017:https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/middle.html. Accessed July 28, 2017.
- 28.Williams K, Thomson D, Seto I, et al. Standard 6: age groups for pediatric trials. Pediatrics. 2012;129 (Supplement 3):S153–S160. [DOI] [PubMed] [Google Scholar]
- 29.Tsao JC, Meldrum M, Kim SC, Jacob MC, Zeltzer LK. Treatment preferences for CAM in children with chronic pain. Evid Based Complement Alternat Med. 2007;4(3):367–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chokshi SK, Ladas EJ, Taromina K, et al. Predictors of acupuncture use among children and adolescents with cancer. Pediatr Blood Cancer. 2017;64(7):e26424. [DOI] [PubMed] [Google Scholar]
- 31.Ndao DH, Ladas EJ, Bao Y, et al. Use of complementary and alternative medicine among children, adolescent, and young adult cancer survivors: a survey study. J Pediatr Hematol Oncol. 2013;35(4):281–288. [DOI] [PubMed] [Google Scholar]
- 32.Mao JJ, Farrar JT, Bruner D, et al. Electroacupuncture for fatigue, sleep, and psychological distress in breast cancer patients with aromatase inhibitor-related arthralgia: a randomized trial. Cancer. 2014;120(23):3744–3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mao JJ, Bowman MA, Xie SX, Bruner D, DeMichele A, Farrar JT. Electroacupuncture versus gabapentin for hot flashes among breast cancer survivors: A randomized placebo-controlled trial. J Clin Oncol. 2015;33(31):3615–3620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crew KD, Capodice JL, Greenlee H, et al. Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor-associated joint symptoms in women with early-stage breast cancer. J Clin Oncol. 2010;28(7):1154–1160. [DOI] [PubMed] [Google Scholar]
- 35.NIH. NIH study links childhood cancer to delays in developmental milestones. 2012; News release; Available at: https://www.nih.gov/news-events/news-releases/nih-study-links-childhood-cancer-delays-developmental-milestones. Accessed July 28, 2017. [Google Scholar]
- 36.Kearney JA, Salley CG, Muriel AC. Standards of psychosocial care for parents of children with cancer. Pediatr Blood Cancer. 2015;62(S5):S632–S683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kleigman RM, Stanton BF, St. Geme JW, Schor NF. Adolescent development Nelson Textbook of Pediatrics. Vol chap 110 Philadelphia, PA: Elsevier; 2016. [Google Scholar]
- 38.Eldridge C, Kennedy R. Nonpharmacologic techniques for distress reduction during emergency medical care: a review. Clin Pediatr Emerg Med. 2010;11(4):244–250. [Google Scholar]
- 39.Wiener L, Kazak AE, Noll RB, Patenaude AF, Kupst MJ. Standards for the psychosocial care of children with cancer and their families: an introduction to the special issue. Pediatr Blood Cancer. 2015;62(S5):S419–S424. [DOI] [PMC free article] [PubMed] [Google Scholar]