Abstract
Cognitive models of posttraumatic stress disorder (PTSD) implicate interpretation biases as a maintaining factor of symptoms. Existing measures index symptoms and negative beliefs in PTSD patients, but not threatening interpretation of socially-ambiguous information, which would further inform cognitive models of PTSD. Here we describe the development of a measure of interpretation bias specific to individuals with PTSD. Studies 1 and 2 utilized analog samples to identify the smallest set of items capable of differentiating PTSD-specific interpretation biases. Study 3 utilized a clinical sample to examine the factor structure of the 9-item Interpretation Bias Index for PTSD (IBIP). A bifactor model fit the IBIP best, comprising a general PTSD factor and two subfactors. The IBIP was most strongly related to PTSD symptoms and demonstrated sensitivity and specificity to detecting true PTSD cases. The IBIP has potential clinical utility for tracking interpretation bias in PTSD, or even screening for PTSD diagnoses.
Keywords: PTSD, measure development, maintenance factors, interpretation bias
Upwards of half the general population is estimated to experience a traumatic event (e.g., physical or sexual assault, serious accident or injury) during their lifetime (Frans, Rimmö, Åberg, & Fredrikson, 2005; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Though stress reactions are common following such events, the severity of responses vary across individuals. In some cases, severe stress responses result in posttraumatic stress disorder (PTSD), which is characterized by intrusive thoughts, increased negative cognitions and mood, behavioral avoidance, and alterations in arousal (American Psychiatric Association [APA], 2013). With an estimated 12-month prevalence of 6.8% in the American population (Kessler et al., 2005), research has highlighted a need for understanding the individual mechanisms implicated in determining how these individuals develop PTSD (Bomyea, Risbrough, & Lang, 2012).
Early models developed to explain the maladaptive cognitive processes inherent to anxiety psychopathology highlighted a putative role for identifying threat, activation of networks biased to attend to threat, and elaborative appraisal of situational information as potentially threatening (e.g., Beck & Clark, 1988, 1997). As PTSD was previously categorized as an anxiety disorder (APA, 2000) and is characterized in part by hypervigilance for threat and avoidance behavior, these cognitive models were extended to describe the development and maintenance of PTSD. Initially, a cognitive action theory of PTSD (Chemtob, Roitblat, Hamada, Carlson, & Twentyman, 1988) proposed that individuals with PTSD are susceptible to a positive feedback loop in which trauma-relevant stimuli activate threat-response structures that bias the interpretation of ambiguous information as threatening. As an extension of this, a comprehensive cognitive model (Ehlers & Clark, 2000) posited that individuals who develop PTSD are less able to process or appraise details of their index trauma in an adaptive (i.e., benign or non-threatening) manner, resulting in the tendency to be hypervigilant for potential threat cues, and overgeneralize threatening appraisals to ambiguous social-informational cues. Thus, over-attendance to threat cues influences the over-generalization of threat appraisals for ambiguous cues, which in turn perpetuates an ongoing sense of current threat.
To date, few studies have investigated cognitive appraisals of external stimuli and the degree to which they may be implicated in PTSD. Amir and colleagues (Amir, Coles, & Foa, 2002) used reaction time latencies to a homographs (i.e., words with the same spelling but two potential meanings; e.g., ‘arms’ could mean limbs, or weapons) task to examine the activation and inhibition of potentially threat-relevant stimuli at the automatic and strategic stages of information processing, respectively. Individuals with, as opposed to without, PTSD were faster to respond to threat-meanings of homographs presented during the automatic (i.e., attentional) stage of processing, but slower to respond when homographs were presented during the strategic (i.e., interpretation) stage. In accord with cognitive theories of PTSD, the authors suggest these results evince increased activation of attentional threat structures, and greater difficulty inhibiting threat meanings for ambiguous information. Kimble and colleagues (Kimble, Batterink, Marks, Ross, & Fleming, 2012) found further evidence of difficulty inhibiting threat meanings using a sentence completion tasks. In this study, veterans with PTSD, compared to controls, spontaneously completed more ambiguous sentences (e.g., ‘He was almost hit by a ‘__’) with military trauma-related words (e.g., ‘bullet’) than neutral words (e.g., ‘rock’). Finally, Elwood and colleagues (Elwood, Williams, Olatunji, & Lohr, 2007) utilized video clips of social situations to demonstrate threat interpretations of ambiguous information and an ongoing sense of threat. Compared to controls, victims of interpersonal violence were more likely to perceive positively-valenced scenes as riskier (i.e., more threatening), and threatening scenes as quicker to escalate toward threat.
Though limited, these studies corroborate an important role for interpretation biases in PTSD. Therefore, indexing biased elaborative interpretations of social-informational cues is both promising and important considering: 1) its position as a mechanism in the development and maintenance of PTSD; 2) its proximal relation to similar targets of established cognitive-behavioral therapeutic techniques (i.e., cognitive distortions); and 3) given that this dynamic appraisal process is independent of the more stable, underlying negative beliefs about the self and world that are central to PTSD (Nanney, Constans, Kimbrell, Kramer, & Pyne, 2015). Thus, a straightforward and simple to administer index of interpretation bias in PTSD would benefit researchers and clinicians alike for screening, measurement, and informing potential therapeutic targets.
Although not yet applied to PTSD, the word-sentence association paradigm (WSAP) has proven to be a robust task for assessing benign and threat interpretations of ambiguous situations. In an initial investigation of the WSAP for interpretation biases (Beard & Amir, 2009), socially anxious individuals rated ambiguous sentences (e.g., “Your date has to leave early”) for how related they were to socially threatening (e.g. “bored”) or benign (e.g., “busy”) words. Compared to non-anxious controls, individuals high in social anxiety symptoms were more likely to endorse threat interpretations of the ambiguous scenarios, and less likely to endorse benign interpretations. These results were further replicated in a clinical sample (Amir, Prouvost, & Kuckertz, 2012). Additionally, Hindash and Amir (Hindash & Amir, 2012) demonstrated that dysphoric individuals endorsed threat stimuli as related to ambiguous sentence stems more often and readily than non-dysphoric individuals. Though the tasks utilized in these studies were computer based, others have successfully used the same basic endorsement and rating format to deliver paper-and-pencil based versions of a WSAP. For instance, Kuckertz and colleagues (Kuckertz, Amir, Tobin, & Najmi, 2013) developed a WSAP measure capable of detecting increased threat bias in individuals with elevated obsessive-compulsive symptoms, compared to controls. Taken together, evidence suggests that the WSAP is a simple and effective method for measuring interpretation biases for threatening information, as it relates to an array of psychiatric symptoms.
Interpretation biases are integral to PTSD, and a simplified method for indexing these biases exists; however, we are unaware of any study applying the WSAP to PTSD. The current studies therefore describe the development of a brief implicit measure (i.e., WSAP) designed to specifically index threatening cognitive appraisals of ambiguous information related to PTSD. Study 1 was designed to test and identify a set of WSAP stimuli capable of discriminating individuals high and low in posttraumatic stress symptoms (PTSS). Study 2 was designed to assess the latent structure of these candidate items via exploratory factor analysis, examine the resulting scales in relation to distress-disorder (e.g., worry, depression, and PTSD) symptoms, and test the discriminant validity of this measure among analog distress disorder symptom groups. Study 3 was designed to replicate the results of Study 2 in a clinical sample; testing the factor structure, reliability, discriminant validity, and incremental predictive validity of the most parsimonious number of items capable of demonstrating PTSD-specific interpretation biases.
Study 1: Pilot Study of WSAP items for PTSD
The goal of this study was to identify items that significantly differentiate individuals with low and high levels of PTSD symptoms via a paper-and-pencil WSAP.
Method
Participants and procedures
Participants (N = 82) were drawn from a larger sample (N = 258) of students who opted to participate in a self-report survey for class credit at a Southwestern university. Following data collection, descriptive statistics were calculated for the six-item version of the PCL-C used in this study. In order to identify potential IBIP items that would differentiate low and high-PTSS groups, individuals who scored greater than or equal to one standard deviation above and below the full sample mean. Among the full sample, the total score for the 6-item PCL-C averaged 14.98 (SD = 5.59; range = 6–30). Therefore, the low- (N = 35) and high-PTSS (N = 47) groups included those who scored ≤ 10 or ≥ 20 on the 6-item PCL-C. The mean age of the sample was 19.12 (SD = 1.81). Most participants identified as female (86.4%); further, 36% of the sample identified as Caucasian, 33% Non-white Hispanic, 12% Asian/Pacific Islander, 8% African-American, and 11% ‘Other’. All individuals completed a brief self-report battery, in addition to the WSAP items developed by the first and fourth investigators, via paper and pencil. All procedures were approved by the university’s Institutional Review Board, and in accordance with the Declaration of Helsinki.
Measures
The PTSD CheckList- Civilian Version (PCL-C).
The PCL-C is a 17-item self-report measure of the symptom criteria specified by the DSM-IV for a PTSD diagnosis (Weathers, Litz, Herman, Huska, & Keane, 1993). Participants were asked to indicated how much they had experienced each item (e.g., repeated, disturbing memories, thoughts or images of a stressful experience from the past) during the past month on a 5-point Likert-style scale (1 = not at all to 5 = extremely). In the present investigation, a previously validated (Lang & Stein, 2005) 6-item version (items 1, 4, 7, 10, 14, 15) of the PCL-C was administered. In prior analog samples (Adkins, Weathers, McDevitt-Murphy, & Daniels, 2008) the full PCL-C demonstrated excellent internal consistency (α = .91), and this 6-item version demonstrated good internal consistency in the present sample (α = .83)
The Interpretation Bias Index for PTSD (IBIP).
The IBIP was the primary measure of interest for this pilot development study. Researchers familiar with PTSD sequelae and cognitions prepared a set of 21 ambiguous sentence stems (Table 1), with each of the three DSM-IV PTSD symptom clusters (i.e., re-experiencing, avoidance, hyperarousal) represented by 7 items. Each sentence was presented twice throughout the measure- once with a benign/non-threatening word, and once with a threatening word- for a total of 42 items to which participants responded. Items were structured similar to previously published WSAP paper and pencil measures (e.g., Kuckertz et al., 2013), such that participants are asked to rate on a 5-point Likert-style scale how much they think each word is related to the preceding sentence stem. For instance, if the scenario “You go to the beach” is paired with the word “fun”, an individual would indicate a “1” if they thought that this would not be a fun scenario at all; alternatively, they would indicate a “5” if they thought this would be an extremely fun scenario.
Table 1.
Independent sample t-test for average ratings of 21 WSAP threat items between PTSS groups.
| Item | Sentence Stem | Threat Stimuli | t | p |
|---|---|---|---|---|
| 1 | A past memory suddenly comes to mind* | Scared | 4.26 | <.001 |
| 2 | There is a sudden movement next to you | Injure | 1.91 | .06 |
| 3 | Someone is asking you a question | Irritated | 1.72 | .09 |
| 4 | A stranger behind you in line is close to you* | Agitated | 2.14 | .02 |
| 5 | A friend wants to meet up | Indifferent | 1.18 | .24 |
| 6 | A conversation triggers a memory* | Traumatic | 4.93 | <.001 |
| 7 | You haven’t spent much time with family | Detached | 1.50 | .13 |
| 8 | You are invited to a party* | Avoid | 4.89 | < .001 |
| 9 | You have memories about a place* | Horror | 4.08 | <.001 |
| 10 | You are reminded of a past event* | Distraught | 5.00 | <.001 |
| 11 | Your relative tells you they are getting married | Numb | 1.65 | .10 |
| 12 | You picture a scenario in your mind* | Upset | 4.95 | <.001 |
| 13 | You hear a noise | Danger | 1.18 | .24 |
| 14 | You become frustrated* | Outburst | 5.93 | < .001 |
| 15 | Your friends all want to get together | Distant | 1.70 | .09 |
| 16 | You think of someone you haven’t seen in a while* | Terror | 3.76 | <.001 |
| 17 | You have to read directions second time* | Racing Thoughts | 2.38 | .02 |
| 18 | You think of a face you are familiar with* | Attacker | 2.36 | .02 |
| 19 | You are invited to the movies, but don’t want to go* | Withdrawn | 6.16 | < .001 |
| 20 | You see a picture of you and your family | Disinterest | 1.69 | .10 |
| 21 | You are in a public place* | Over-alert | 4.30 | <.001 |
Note.
Denotes items retained for Study 2; PTSS groups determined by participants scoring +/− 1SD of the full sample mean on 6-item version of the PTSD Check List- Civilian Version.
Data analytic plan
Descriptive statistics were used to provide sample characteristics. As an initial investigation of these items, analyzing group differences among respondents at opposite ends of this distribution provided the sensitivity necessary to detect which IBIP items would be most likely to differentiate individuals in a clinical sample (Study 3). Next, benign and threat averages across the 21-item scales were calculated. Independent sample t-tests were employed to test for differences between high- and low-PTSS groups (i.e., +/− 1 SD of the PCL-C) in: 1) average benign ratings; 2) average threat ratings; and 3) individual threat item ratings. Benjamini-Hochberg corrections were applied to the individual threat item ratings to guard against Type-I error (Benjamini & Hochberg, 1995).
Results
Independent samples t-tests were conducted to assess for differences between the low- and high-PTSS groups on average ratings for IBIP benign and threat stimuli. There were no statistically significant differences between the low- (M = 3.69, SD = .58) and high-PTSS (M = 3.55, SD = .54) groups for benign stimuli rating averages [t(80) = 1.06, p = .29]. However, the high-PTSS group (M = 2.75, SD = .61) rated threat stimuli as significantly more related to ambiguous sentence stems, on average (t[80] = 5.97, p < .001), than the low-PTSS group (M = 2.00, SD = .49).
Because groups only differed significantly on ratings of threat stimuli, independent sample t-tests with Benjamini-Hochberg corrections were employed to assess differences between the low- and high-PTSS groups for the threat word-sentence pairs only. Of the 21 threat items, the high-PTSS group provided higher average ratings than the low-PTSS group (all p’s < .05) on thirteen of them (Table 1).
Study 1 Discussion
The results of Study 1 suggested that the WSAP may can detect interpretation biases for threatening stimuli in individuals with elevated PTSS. Furthermore, there was no evidence to suggest that interpretation of benign stimuli differed as a function of PTSS; thus, in the interest of parsimony, these items did not appear necessary to include in the IBIP. The 13 threat pairs that significantly differed between symptom groups were retained and tested as a more succinct measure of PTSS interpretation bias in Study 2.
Study 2: Factor Structure and Discriminant Validity
The primary goal of Study 2 was to use exploratory factor analysis (EFA) to determine which items should be retained for the interpretation bias measure, and the number of factors on which they load. Empirically, we hypothesized that these items should all load on to a single factor representative of the global PTSD construct. However, as items were designed to reflect interpretations of situations specific to certain symptom clusters (e.g., intrusive memories, hypervigilance), it is possible that several secondary factors exist. The secondary goal was to examine the discriminant validity of the IBIP in an independent sample, extending symptom measures to include those of other distress disorder facets, such as generalized worry and depressive symptoms (Watson, 2005).
Method
Participants and procedures
Participants (N = 202) were those who elected to participate in an online survey of self-report symptom measures for class credit from a larger undergraduate sample (N = 620) at a Southwestern university. The average age of the sample was 19.03 years (SD = 1.49), and the majority (68.7%) identified as female. Of the full sample, 35% identified as Caucasian, 22% Non-White Hispanic, 20% Asian-American/Pacific Islander, 12% African American, 1% Native American, and 10% ‘Other’.
The study was made available through the university’s research participation web portal, where students could register for the study and participate for class credit. To ensure that individuals with elevated PTSS were included, we oversampled by inviting, via email, those who had scored above the suggested conservative PCL-C symptom cut-off for diagnostic screening (≥ 50; Weathers et al., 1993) in an initial screening battery. All participants were required to first provide a digital signature of informed consent, and were awarded class credit for their participation after submitting their responses. All study procedures were approved by the university’s Institutional Review Board and in accord with the Declaration of Helsinki.
Measures
The PTSD CheckList- Civilian Version (PCL-C).
The PCL-C was administered. Although an abbreviated version of the PCL-C was used in Study 1, the complete original 17-item PCL-C was administered to participants in Study 2. The PCL-C demonstrated excellent internal consistency in the current sample (α = .96).
Beck Depression Inventory-II (BDI-II).
The BDI-II is a measure of depression severity, that assesses mood as well as cognitive and physical symptoms of depression (Beck, Steer, & Brown, 1996). Participants were asked to rate each of 21 items on a unique 4-point scale, based on their experiences in the previous 2 weeks. For example, participants responded to loss of pleasure by selecting a response from 0 (I get as much pleasure as I ever did from things I enjoy) to 3 (I can’t get any pleasure from the things I used to enjoy). In prior studies (Steer & Clark, 1997), the BDI-II has demonstrated good internal consistency (a = .89). Internal consistency was excellent in the current sample (α = .91).
Penn State Worry Questionnaire (PSWQ).
The PSWQ is a 16-item measure of pathological worry designed to evaluate the generality, excessiveness, and uncontrollability that are characteristic of generalized anxiety disorder (Meyer, Miller, Metzger, & Borkovec, 1990). Participants were asked to respond to how well each of 16 items (e.g., My worries overwhelm me; I worry all the time) characterize them on a 5-point Likert-style scale (1 = Not at all to 5= Very). In prior studies (Fresco, Heimberg, Mennin, & Turk, 2002), the PSWQ demonstrated good internal consistency (α = .90), as it did in the current sample (α = .88).
Interpretation Bias Index for PTSD (IBIP).
In Study 2, the IBIP consisted of the 13 threat items identified in Study 1 (see Table 3 for complete list) as most capable of detecting interpretation bias differences between those with high and low PTSS. Instructions for responding to these items were identical to those in Study 1. Scores for the IBIP total and subscales were calculated by summing all respective items, with higher scores indicating more threat-interpretation bias. Reliability is discussed below.
Table 3.
Standardized factor loadings for the 13 IBIP items in Study 2 and Study 3 confirmatory factor analyses.
| Study | |||||||
|---|---|---|---|---|---|---|---|
| Study 2 (analog EFA) | Study 3 (clinical CFA) | ||||||
| Sentence Stem | Threat Word | Factor | I β | HA β | Factor | I β | HA β |
| 1. A past memory suddenly comes to mind. | Scared | I/HA | .42* | .35* | -- | -- | -- |
| 2. A stranger behind you in line is close to you. | Agitated | HA | −.04 | .68* | HA | -- | .60* |
| 3. You have to read directions a second time. | Racing thoughts | HA | .09 | .47* | HA | -- | .47* |
| 4. You picture a scenario in your mind. | Upset | I/HA | .58* | .22* | -- | -- | -- |
| 5. You have memories about a place. | Horror | I | 1.04* | −.26* | I | .84* | -- |
| 6. You are reminded of a past event. | Distraught | I/HA | .56* | .25* | -- | -- | -- |
| 7. You think of someone you haven’t seen in a while. | Terror | I | .67* | .00 | I | .69* | -- |
| 8. You become frustrated. | Outburst | I/HA | .22* | .35* | -- | -- | -- |
| 9. You are invited to the movies but do not want to go. | Withdrawn | HA | .13 | .56* | HA | -- | .69* |
| 10. A conversation triggers a memory. | Traumatic | I | .79* | .05 | I | .77* | -- |
| 11. You think of a face you are familiar with. | Attacker | 1 | .64* | .01 | 1 | .73* | -- |
| 12. You are invited to a party. | Avoid | HA | −.01 | .68* | HA | -- | .73* |
| 13. You are in a public place. | Over-alert | HA | .07 | .73* | HA | -- | .77* |
Note. IBIP = 9-item Interpretation Bias Index for PTSD; I = 4-item IBIP ‘intrusions’ factor; HA = 5-item IBIP ‘hypervigilance/avoidance’ factor.
p < .01
Data Analytic Plan
Descriptive statistics were used to provide sample characteristics (Table 2). A series of analyses were conducted to assess the latent and psychological properties of the full measure, as well as any subsequent subfactors. First, an EFA with oblique geomin rotation using maximum likelihood was conducted in Mplus version 6.11 (Muthén & Muthén, 2011) for the 13-item IBIP. Oblique geomin rotation is the default in Mplus and allows factors to be correlated with one another, which was appropriate for use with IBIP items given that any resulting factors were expected correlate in a manner similar to PTSD symptom clusters. Decisions about the number of factors to extract were based on the Kaiser-Guttman rule (Kaiser, 1960) and parallel analysis (Hayton, Allen, & Scarpello, 2004). Items were retained if they loaded significantly on a single factor at greater than .4; any items that loaded on multiple factors were retained only if their primary loading was greater than .5, and any secondary loadings were less than .2 (Matsunaga, 2010). Items that did not meet these criteria were flagged for removal and not included in subsequent analyses. Second, the full measure and any subscales revealed through EFA were investigated for internal consistency. Third, discriminant validity was assessed in two ways. Bivariate correlations (Table 2) for the full scale, any subscales, and other distress-disorder measures were calculated and compared using Fisher’s z-tests. Due to the inherent overlap in PTSS and other forms of psychopathology, it was expected that, while the IBIP would positively correlate with other symptom measures (i.e., worry, depression), it would be more strongly related to PTSS. Thus, hierarchical regression models tested the predictive validity of PTSS for IBIP total and subscale scores (Step 2) over and above other distress disorder measures (i.e., worry, depression; Step 1).
Table 2.
Descriptive statistics and bivariate correlations for symptom measures, 9-item IBIP, and IBIP subscales in studies 2 (analog sample) and 3 (clinical sample).
| Measure | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Study 2 | ||||||
| l. IBIP | -- | |||||
| 2. IBIP Intr. fx | .82* | -- | ||||
| 3. IBIP H/A fx | .83* | .45* | -- | |||
| 4. PCL-C | .75* | .61* | .66* | -- | ||
| 5. PSWQ | .64* | .43* | .64* | .66* | -- | |
| 6. BDI-II | .60* | .43* | .55* | .66* | .73* | -- |
| M | 27.63 | 13.79 | 15.49 | 36.47 | 39.61 | 12.65 |
| SD | 10.06 | 5.99 | 4.79 | 16.04 | 12.34 | 9.76 |
| Range | 9–36 | 4–18 | 5–24 | 17–85 | 0–58 | 16–64 |
| Study 3 | ||||||
| l. IBIP total | -- | |||||
| 2. IBIP Intr. fx | .54* | -- | ||||
| 3. IBIP H/A fx | .89* | .52* | -- | |||
| 4. PCL-C | .72* | .67* | .60* | -- | ||
| 5. PSWQ | .39* | .20* | .46* | .39* | -- | |
| 6. BDI-II | .58* | .44* | .56* | .70* | .49* | -- |
| M | 23.74 | 8.58 | 15.16 | 45.60 | 60.48 | 25.76 |
| SD | 8.43 | 4.44 | 5.21 | 16.31 | 13.21 | 12.37 |
| Range | 9–45 | 4–20 | 5–25 | 17–85 | 25–80 | 0–59 |
Note. IBIP = 9-item Interpretation Bias Index for PTSD; IBIP Intr. fx = 4-item IBIP ‘intrusions’ factor; IBIP H/A fx = 5-item IBIP ‘hypervigilance/avoidance’ factor; PCL-C = PTSD Check List- Civilian Version; PSWQ = Penn State Worry Questionnaire; BDI-II = Beck Depression Inventory-II.
p < .001
Results
Factor Structure and Internal Reliability
An EFA with oblique geomin rotation revealed a two-factor solution provided the best fit to the sample data (see Table 3 for item loadings). Based on the Kaiser-Guttman rule of retaining factors with eigenvalues greater than 1, only two of three extracted factors (eigenvalues = 5.83, 1.46, and .87, respectively) met this criteria. Similarly, the eigenvalues of factor 1 and factor 2 exceeded the 95th percentile Eigenvalues from randomly generated data in parallel analysis (1.54 for factor 1, 1.39 for factor 2), though the third did not (1.24). Compared to the one-factor model (χ2[65] = 269.09, p < .001; RMSEA = .125, 95%CI[.109, .140]; CFI = .820; TLI = .784; SRMR = .076), the two-factor model (χ2[53] = 109.58, p < .001; RMSEA = .073, 95%CI[.053, .092]; CFI = .950; TLI = .927; SRMR = .038) provided significantly better fit to the data (Δ χ2[12] = 159.51, p < .001). Thus, tests of factor extraction and model fit converged on a two factor solution.
Four items loaded exclusively on factor 1, which was interpreted as the ‘intrusions’ factor; five items loaded exclusively on factor 2, which was interpreted as the ‘hypervigilance/avoidance’ factor. Four items cross-loaded on both factors and were therefore removed from all subsequent analyses. The two factors were significantly correlated with one another (r = .59, p < .001). Internal reliability for sum-scores of the 9-item IBIP, 4-item ‘intrusions’ subscale, and 5-item ‘hypervigilance/avoidance’ subscale were good (α’s = .84, .85, and .79, respectively).
Discriminant Validity
Zero-order correlations between the 9-item IBIP, 4-item ‘intrusions’ subscale, and 5-item hypervigilance/avoidance subscale, and all symptom measures are presented in Table 2. The 9-item IBIP was more strongly correlated with the PCL-C than the PSWQ (z = 2.23, p < .05) and BDI (z = 2.86, p < .01). Similarly, the 4-item ‘intrusions’ subscale was more strongly correlated with the PCL-C than the PSWQ (z = 2.44, p < .05) and BDI-II (z = 2.45, p < .01). However, the 5-item ‘hypervigilance/avoidance’ subscale was correlated with the PCL-C, PSWQ, and BDI-II at statistically equivalent levels (all p’s > .05).
To more stringently test the discriminant validity of the 9-item IBIP, a hierarchical regression model was employed with 9-item IBIP scores regressed on BDI-II depression symptoms, PSWQ worry symptoms, and PCL-C PTSS (Table 4). The first step accounted for a significant proportion of variance in IBIP total scores (ΔF[2,199] = 80.30, p < .001, Δr2 = .447), as BDI-II and PSWQ scores were both significant predictors (p’s < .001). The addition of PCL-C PTSS in the second step of the model accounted for a significantly larger proportion of variance in IBIP total scores (ΔF[1,198] = 79.81, p < .001, Δr2 = .159). In the second step, BDI-II depression symptoms (p = .34) were no longer a significant predictor of IBIP total scores, although PSWQ worry (p < .01) and PCL-C PTSS (p < .001) were. A similar hierarchical model regressed the 5-item ‘hypervigilance/avoidance’ subscale on PSWQ, BDI-II, and PCL-C scores. The first step accounted for a significant proportion of variance in IBIP ‘hypervigilance/avoidance’ subscale scores (ΔF[2,199] = 73.96, p < .001, Δr2 = .426), as BDI-II (p = .03) and PSWQ scores (p < .001) were both significant predictors. The addition of PCL-C PTSS in the second step of the model accounted for a significantly larger proportion of variance in IBIP ‘hypervigilance/avoidance’ subscale scores (ΔF[1,198] = 34.25, p < .001, Δr2 = .085). In the second step, BDI-II depression symptoms (p = .90) were no longer a significant predictor of IBIP ‘hypervigilance/avoidance’ subscale scores, although PSWQ worry (p < .001) and PCL-C PTSS (p < .001) were. Finally, 4-item ‘intrusions’ subscale scores were regressed on PSWQ, BDI-II, and PCL-C scores in a hierarchical regression model. The first step accounted for a significant proportion of variance in IBIP ‘intrusions’ subscale scores (ΔF[2,199] = 26.46, p < .001, Δr2 = .210), as BDI-II (p = .01) and PSWQ scores (p = .01) were both significant predictors. The addition of PCL-C PTSS in the second step of the model accounted for a significantly larger proportion of variance in IBIP ‘intrusions’ subscale scores (ΔF[1,198] = 49.49, p < .001, Δr2 = .158). In the second step, BDI-II depression symptoms (p = .76) and PSWQ worry (p = .67) were no longer significant predictors, but PCL-C PTSS (p < .001) were.
Table 4.
Study 2 and 3 linear hierarchical regression analyses with: IBIP full scale scores, ‘intrusions’ subscale and ‘hypervigilance/avoidance’ subscale regressed on distress disorder symptom measures.
| Predictor | Outcome Variable | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| IBIP (full) | I Factor | H/A Factor | |||||||
| Study 2 | β | p | sr2 | β | P | sr2 | β | p | sr2 |
| Step 1 | |||||||||
| BDI-II | .29 | <.001 | .064 | .25 | .01 | .034 | .17 | .03 | .023 |
| PSWQ | .43 | <.001 | .135 | .25 | .01 | .035 | .52 | <.001 | .180 |
| Step 2 | |||||||||
| BDI-II | .07 | .34 | .004 | .03 | .76 | <.001 | .01 | .9 | .001 |
| PSWQ | .22 | <.01 | .047 | .04 | .67 | .001 | .37 | <.001 | .101 |
| PCL-C | .56 | <.001 | .287 | .56 | <.001 | .200 | .41 | <.001 | .147 |
| Study 3 | β | p | sr2 | β | p | sr2 | β | P | sr2 |
| Step 1 | |||||||||
| BDI-II | .51 | <.001 | 231 | .48 | <.001 | .181 | .43 | <.001 | .180 |
| PSWQ | .15 | .01 | .026 | −.03 | .62 | .001 | .27 | <.001 | .080 |
| Step 2 | |||||||||
| BDI-II | .13 | .02 | .018 | .04 | .59 | .001 | .17 | .01 | .022 |
| PSWQ | .13 | <.01 | .031 | −.08 | .14 | .007 | .24 | <.001 | .072 |
| PCL-C | .60 | <.001 | .308 | .67 | <.001 | .295 | .40 | <.001 | .132 |
Note. IBIP = 9-item Interpretation Bias Index for PTSD; I factor = 4-item IBIP ‘intrusions’ factor; H/A factor = 5-item IBIP ‘hypervigilance/avoidance’ factor; BDI-II = Beck Depression Inventory-II; PSWQ = Penn State Worry Questionnaire; PCL-C = PTSD Check List- Civilian Version.
Study 2 Discussion
Study 2 utilized a sample of undergraduates, who provided self-report data relating to PTSS, worry, and depression, to identify the most parsimonious set of items that would be highly specific to indexing interpretation biases in individuals with a PTSD diagnosis. EFA of the 13 threat items selected from Study 1 revealed two factors: one included four items specifically reflective of responses to traumatic reminders (i.e., the ‘intrusions’ factor), and five items reflective of hypervigilance and avoidance (i.e., the ‘hypervigilance/avoidance’ factor). The full IBIP and both subscales demonstrated stronger bivariate correlations with PTSS than worry and depression symptoms, and all IBIP total and subscale scores accounted for a significant increase in the proportion of PTSS variance in hierarchical regression models. However, the 4-item ‘intrusions’ subscale better demonstrated discriminant validity in hierarchical regression analyses, as it was the only one to be significantly predicted by PTSS alone, above and beyond non-significant associations with worry and depression symptoms.
Taken together the results of Study 2 suggest that the IBIP and its subscales are internally reliable measures, and most closely related to PTSS; the ‘intrusions’ subscale in particular. However, these results must be replicated in a clinical sample. Moreover, because there was no support for the hypothesized three-factor model that included a general PTSD interpretation bias on which all IBIP items loaded, it may be warranted to test a bifactor model as a nested competing model of the present two-factor solution. Finally, as cognitive biases are assumed to be a mechanism of PTSD independent of symptoms, it is important to establish the incremental validity of the IBIP in characterizing a clinical diagnosis of PTSD, above and beyond global PTSS. These limitations are the basis for the hypotheses tested in Study 3.
Study 3: Factor Validation, Predictive Validity, and Diagnostic Value
Study 3 sought to build from the exploratory results provided by the analog sample in Study 2. There were four primary aims of study 3.
First, confirmatory factor analysis (CFA) was conducted to test the two-factor model that emerged in Study 2. Additionally, we tested an alternative bifactor model (Chen, Hayes, Carver, Laurenceau, & Zhang, 2012; Reise, 2012) to examine the specificity of the two-factor model. Examining a bifactor model would potentially improve our understanding of the latent structure of the IBIP as well as the ways in which it may be acceptable for use in clinical research. Whereas the conventional CFA approach used to test the two-factor model would force individual items to contribute unique variance to a single factor, a bifactor CFA model would allow the individual IBIP items to share common variance with a latent general PTSD factor (which was hypothesized, but not observed in the Study 2 EFA) as well as unique residual variance with the two subfactors identified by the EFA in Study 2. To a degree, this is akin to acknowledging that individual PTSD symptoms contribute to global severity, but are also a unique component of lower-order symptom clusters. As bifactor modeling would allow us to determine whether individual items contribute unique variance to specific subfactors, it further informs whether any caution should be exercised in interpreting sum-scores of those subfactors. Thus, bifactor modeling has important implications for the use of the IBIP as clinical index of interpretation biases PTSD.
Second, we sought to replicate the discriminant validity of the IBIP and its subscales in relation to PTSS, worry, and depression symptoms. Further, we aimed to extend the discriminant validity by comparing IBIP total and subscale scores across individuals categorized as PTSD diagnosed, trauma exposed, and non-trauma exposed controls. Because interpretation biases are implicated in a PTSD diagnosis, as opposed to trauma exposure, per se (Ehlers & Clark, 2000), those with a diagnosis were hypothesized to score higher on the IBIP than trauma-exposed individuals were not diagnosed with PTSD and non-trauma-exposed controls.
Third, we sought to identify the incremental validity of the IBIP or its subscales in identifying PTSD cases, above and beyond global PTSS. Because interpretation biases are considered an independent mechanism that promote PTSS, scores on the IBIP PTSD subscale were hypothesized to indicate a greater likelihood of PTSD diagnosis, above and beyond global PTSS as measured by the PCL-C. Fourth, since this measure was designed with the intent of indexing the degree to which interpretation bias is present in individuals with a PTSD diagnosis, we were interested in determining a suggested cut-point for identifying clinical-level interpretation bias via a receiver operating curve.
Method
Participants and procedure
Participants (N = 323) were recruited through a community outpatient mental health clinic in the Southeastern United States. The majority (55.5%) identified as female; with 62.9% of the sample identified as Caucasian/White, 23.4% African American, 2.2% Asian/Pacific Islander, 0.9% Native American/American Indian, and 10.3% ‘Other’. Participants ranged in age from 18–79, averaging 33.99 years old (SD = 15.61). The majority of the sample (78.1%) reported a history of trauma exposure. Among trauma-exposed participants, the most prevalent category reported as an individual’s index trauma was sexual assault (26.6%), followed by physical assault (20.6%), serious accidents (14.3%), the sudden death of a loved one (9.5%), combat (8.7%), natural disasters (7.5%), life-threatening illness (5.6%), witnessing or experiencing serious bodily harm or death (e.g., shot, stabbed, or robbed at gun-point; 4.3%), and imprisonment or torture (3.1%). Inclusion criteria stipulated a basic proficiency in English. Individuals were excluded from participation if they displayed evidence of uncontrolled psychotic-spectrum or bipolar disorders, or if current suicide risk was determined to be elevated enough to require immediate hospitalization; however, there were no such cases.
Measures
As in Study 2, PTSD, depression, and worry symptoms were assessed with the PCL-C, BDI-II, and PSWQ, respectively. Each measure demonstrated high levels of internal consistency (α’s = .93, .92, and .92, respectively).
Interpretation Bias Index for PTSD (IBIP).
In Study 3, the IBIP consisted of the 9 items that loaded on the two factors identified by the EFA in Study 2. Each item was again rated on a 1–5 (not at all-extremely) Likert-style scale, with higher ratings indicative of greater threat bias for ambiguous information. Consistent with Study 2, sum-scores for the full measure and subscales were used in all statistical tests of study hypotheses.
Diagnostic interview
The Structured Clinical Interview for DSM-5 – Research Version (SCID-5-RV) was administered to all Study 3 participants to assess diagnostic status (First, Williams, Karg, & Spitzer, 2015). Training for administrators (i.e., clinical psychology graduate students) included reviewing SCID training tapes, observing SCID administrations by trained students, and conducting practice interviews with other trained individuals. Trainees received feedback until they demonstrated high levels of diagnostic reliability. All SCIDs were reviewed with a licensed clinical psychologist to confirm accurate diagnosis. This training process has been used for other research studies in our laboratory, and produced high inter-rater reliability (k = .86; Schmidt, Norr, Allan, Raines, & Capron, 2017). In the present study, the SCID-5-RV was used to determine whether individuals had been exposed to a potentially traumatic event (i.e., Criterion A), and whether they currently met full diagnostic criteria for PTSD.
Data Analytic Plan
Two CFA’s were conducted in Mplus Version 6.11 (Muthén & Muthén, 2011) to test a two-factor solution and an alternative bifactor model. Each of the nine items were specified to load on a general PTSD interpretation bias factor, as well as their respective subfactors that emerged in Study 2. Following CFA, the full IBIP and its individual subscales were sum-scored in order to examine their bivariate correlations with worry, depression, and PTSD symptom measures. Hierarchical linear regressions were employed to test the discriminant validity of IBIP total, ‘intrusions’ subscale and ‘hypervigilance/arousal’ subscale scores when regressed onto PTSD, worry, and depression symptom measures (Table 4). Mean IBIP total and subscale score differences between non-exposed, trauma exposed without PTSD, and PTSD diagnosed individuals were tested using univariate ANOVA; multiple pairwise comparisons with Bonferroni corrections followed. Logistic regressions were utilized to test the incremental predictive validity of IBIP total and subscale scores above and beyond PCL-C symptoms in identifying positive PTSD diagnoses. Finally, a receiver operating curve (ROC) of IBIP total scores was analyzed to suggest an appropriate clinical cut-off for maximizing its utility in correctly identifying clinically-relevant interpretation biases associated with PTSD diagnoses.
Results
Two-hundred and fifty-seven (80.1%) participants reported at least one prior exposure to a traumatic event. Sixty-four participants (19.9%) presented with a PTSD diagnosis; of these, PTSD was the primary diagnosis for thirty-three participants (10.3%). Twenty-four participants (7.5%) received no diagnoses, 83 (25.9%) received one Axis-I diagnosis, and 214 (66.7%) received 2 or more diagnoses. Overall, the number of total diagnoses ranged from 0–8, with the median number being 2. Descriptive statistics and bivariate correlations for symptom measures are presented in Table 2.
Factor Structure and Internal Reliability
A two-factor CFA was specified, with four items loading on to factor 1 (i.e., ‘intrusions’) and five items loading on factor two (i.e., ‘hypervigilance/avoidance’). The model provided good fit to the data (χ2[26] = 61.79, p < .001; RMSEA = .065, 95% CI[.044, .086]; CFI = .967; TLI = .954; SRMR = .041); although the RMSEA was slightly higher than the desired value of .05, that value was at least included in the 95% CI. All items significantly loaded on their respective factors (all p’s < .001), with standardized estimates on the ‘intrusions’ factor ranging from .69-.84, and .47-.77 on the ‘hypervigilance/avoidance’ factor (see Table 3 for loadings). The two factors were significantly correlated (r = .614, p < .001).
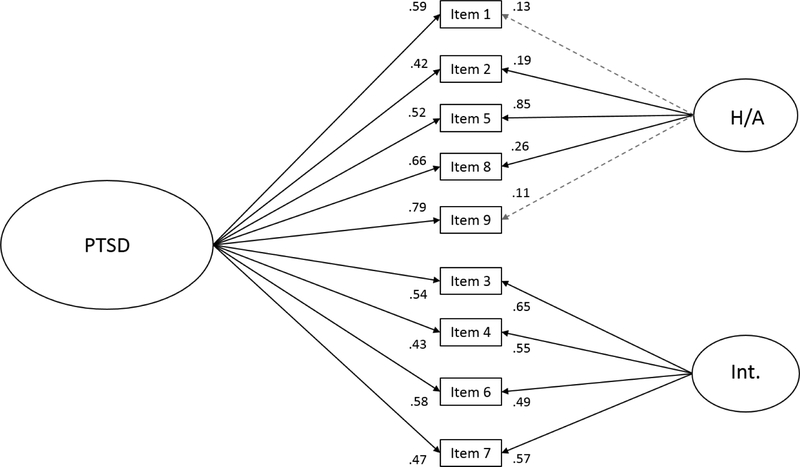
Next, a bifactor model (Figure 1) was tested, which specified all 9 items to load on a general ‘PTSD’ factor, with residual variances for each individual item specified onto their respective subfactors (i.e., 4-item ‘intrusion’ and 5-item ‘hypervigilance/avoidance’ subfactors). This model provided excellent fit to the data (χ2[19] = 34.42, p = .02; RMSEA = .05, 95% CI[.021, .076]; CFI = .986; TLI = .973; SRMR = .027), and fit the data significantly better than the two-factor model specified by the CFA (Δχ2[Δ7] = 27.37, p < .05). All items significantly loaded on the global ‘PTSD’ factor on which they were specified (all p’s < .001), with standardized estimates ranging from .417 – .792. All four items loaded significantly (all p’s < .001) on the ‘intrusions’ subfactor, with standardized estimates ranging from .49-.65. Three items (2, 5, 8) loaded significantly (p’s < .01) on the ‘hypervigilance/avoidance’ factor; however, the loading for IBIP item 1 on the ‘hypervigilance/avoidance’ factor was only marginally significant (p = .05), and the loading for IBIP item 9 (p = .16) did not suggest a significant degree of unique variance in this item was accounted for by this subfactor, after having loaded so strongly (β = .792) on the general ‘PTSD’ factor. Internal reliability for the sum-scored 9-item IBIP, the 4-item ‘intrusions’ subscale, and 5-item ‘hypervigilance/avoidance’ subscale were good (α’s = .85, .84, and .79, respectively).
Figure 1.
Bifactor model of the 9-item IBIP in Study 3. *Note. H/A = hypervigilance/avoidance subfactor; Int. = Intrusions subfactor. Standardized loadings presented.
Discriminant Validity
Bivariate correlations between the 9-item IBIP, 4-item ‘intrusions’ subscale, and 5-item ‘hypervigilance/avoidance’ subscale are presented in Table 2. The 9-item IBIP was more strongly correlated with the PCL-C than the PSWQ (z = 6.18, p < .001) and BDI (z = 3.02, p < .01). Similarly, the 4-item ‘intrusions’ subscale was more strongly correlated with the PCL-C than the PSWQ (z = 7.62, p < .001) and BDI-II (z = 4.13, p < .001). However, the 5-item ‘hypervigilance/avoidance’ subscale was more strongly correlated with the PCL-C than the PSWQ (z = 2.43, p < .01), but not the BDI-II (z = 0.77, p = .22). By comparison, IBIP total and ‘hypervigilance/avoidance’ subscale scores were more strongly correlated with the PSWQ (both p’s < .01) and BDI-II (p’s < .05) than the ‘intrusions’ subscale.
As in Study 2 a hierarchical regression model was employed with 9-item IBIP scores regressed on BDI-II depression symptoms, PSWQ worry symptoms, and PCL-C PTSS (Table 4).1 The first step accounted for a significant proportion of variance in IBIP total scores (ΔF[2,287] = 82.04, p < .001, Δr2 = .364), as BDI-II (p < .01) and PSWQ scores (p = .01) were both significant predictors. The addition of PCL-C PTSS in the second step of the model accounted for a significantly larger proportion of variance in IBIP total scores (ΔF[1,286] = 112.00, p < .001, Δr2 = .179). In the second step, BDI-II depression symptoms (p = .04), PSWQ worry (p = .02) and PCL-C PTSS (p < .001) were all significant predictors of IBIP total scores. A similar hierarchical model regressed the 5-item ‘hypervigilance/avoidance’ subscale on PSWQ, BDI-II, and PCL-C scores. The first step accounted for a significant proportion of variance in IBIP ‘hypervigilance/avoidance’ subscale scores (ΔF[2, 287] = 84.94, p < .001, Δr2 = .372), as BDI-II (p < .001) and PSWQ scores (p < .001) were both significant predictors. The addition of PCL-C PTSS in the second step of the model accounted for a significantly larger proportion of variance in IBIP ‘hypervigilance/avoidance’ subscale scores (ΔF[1, 286] = 40.95,p < .001, Δr2 = .079). In the second step, BDI-II depression symptoms (p = .01), PSWQ worry (p < .001) and PCL-C PTSS (p < .001) were all significant predictors. Finally, 4-item ‘intrusions’ subscale scores were regressed on PSWQ, BDI-II, and PCL-C scores in a hierarchical regression model. The first step accounted for a significant proportion of variance in IBIP ‘intrusions’ subscale scores (ΔF[2, 287] = 39.68, p < .001, Δr2 = .217), wherein BDI-II scores (p < .001) were a significant predictor though PSWQ scores (p = .62) were not. The addition of PCL-C PTSS in the second step of the model accounted for a significantly larger proportion of variance in IBIP ‘intrusions’ subscale scores (ΔF[1, 286] = 118.29, p < .001, Δr2 = .229). In the second step, BDI-II depression symptoms (p = .57) and PSWQ worry (p = .16) were no longer significant predictors, but PCL-C PTSS (p < .001) were.
As an additional test of the discriminant validity of the 9-item IBIP, a univariate ANOVA was employed to analyze mean score differences among non-trauma-exposed (N = 64), trauma-exposed without a PTSD diagnosis (N = 195), and PTSD diagnosed groups (N = 64). Results revealed a main effect of group (F[2,320] = 45.29, p < .001, = .221). Pairwise comparisons with Bonferroni corrections revealed that 9-item IBIP means were higher among those with a PTSD diagnosis (M = 31.55, SD = 8.07) than both the trauma-exposed no PTSD (M = 22.30, SD = 7.34; p < .001, 95%CI [6.66, 11.83]) and non-trauma-exposed groups (M = 20.33, SD = 7.21; p < .001, 95%CI [8.04, 14.40]). Mean differences were not significantly different among the trauma-exposed no PTSD and non-trauma-exposed groups (p = .20, 95%CI [−4.56, 0.61]).
A similar model was tested with the 5-item ‘hypervigilance/avoidance’ subscale as the dependent variable, revealing a significant, yet smaller, main effect of group (F[2,322] = 16.04, p < .001, = .091). Although Bonferroni-corrected pairwise comparisons remained significant between the PTSD diagnosed (M = 18.31, SD = 5.28) compared to the trauma-exposed no PTSD (M = 14.48, SD = 4.80; p < .001, 95%CI [2.11, 5.56]) and non-trauma-exposed groups (M = 14.11, SD = 5.25; p < .001, 95%CI [2.08, 6.32]), there was no difference between the trauma-exposed no PTSD and non-trauma-exposed groups (p > .99, 95%CI [−2.10, 1.36]). Lastly, a similar model was tested with the 4-item ‘intrusions’ subscale as the dependent variable, revealing a significant main effect of group (F[2,320] = 65.89, p < .001, = .292). Pairwise comparisons with Bonferroni corrections revealed that 4-item ‘intrusions’ subscale means were higher among those with a PTSD diagnosis (M = 13.23, SD = 3.94) than both the trauma-exposed no PTSD (M = 7.83, SD = 3.80; p < .001, 95%CI [4.11, 6.71]) and non-trauma-exposed groups (M = 6.22, SD = 3.41; p < .001, 95%CI [5.42, 8.61]). Mean differences were also significantly greater among the trauma-exposed no PTSD compared to the non-trauma-exposed group (p < .01, 95%CI [.31, 2.91]).
Predictive Validity
To test whether interpretation biases as indexed by IBIP total scores were incremental in differentiating those with and without a PTSD diagnosis beyond global PCL-C PTSD symptoms, total scores from these two scales were entered into a logistic regression predicting a dichotomous (‘yes’ or ‘no’) PTSD diagnosis variable. Greater IBIP scores (AOR = 1.10, p < .001, 95% CI [1.12, 1.28]) were significantly associated with a PTSD diagnosis, above and beyond the significant relationship between greater PCL-C PTSD symptoms (AOR = 1.05, p < .01, 95% CI [1.02, 1.08]). A similar pattern emerged with IBIP ‘intrusions’ subscale scores (AOR = 1.26, p < .001, 95% CI [1.15, 1.37]) and PCL-C scores (AOR = 1.04, p < .01, 95% CI [1.01, 1.07]) in a separate model predicting PTSD diagnostic status. In a third model, IBIP ‘hypervigilance/avoidance’ subscale scores (AOR = 1.04, p = .33, 95% CI [0.96, 1.12]) were not significantly related to PTSD diagnoses above and beyond PCL-C scores (AOR = 1.08, p < .01, 95% CI [1.05, 1.11]).
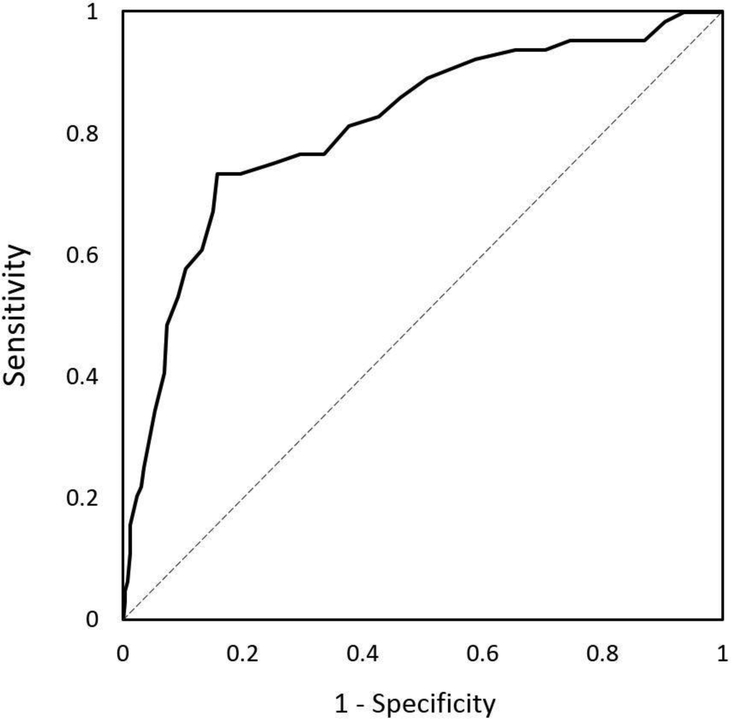
Diagnostic Value
The ROC curve for the 9-item IBIP is presented in Figure 2. The area under the curve was .813 (SE = .032, 95% CI [.750, .875]). Per the maximum calculated value of the Yuden Index, a cut-point of 28.5 on the 9-item IBIP maximizes both the sensitivity (.734) and specificity (.842) of this measure. Using this cut-point in a logistic regression correctly identified 82.1% of cases, including 84.2% of true non-cases (i.e., true negatives) and 73.4% of true PTSD cases (i.e., true positives). Individuals who scored ≥ 29 on the 9-item IBIP were 14.77 times more likely than those below the cut-point to have a PTSD diagnosis (OR = 14.77, p < .001, 95% CI [7.73, 28.21]).
Figure 2.
Receiver operating characteristic (ROC) curve analysis for the 9-item IBIP predicting positive and negative PTSD diagnosis, with scores ≥ 29 suggested as the maximal cut-off for identifying PTSD cases.
Study 3 Discussion
Study 3 utilized a clinical sample to replicate the findings of Study 2, and further suggest the IBIP for use as an index of PTSD-specific interpretation biases and screening for potential PTSD diagnoses. Although the two-factor solution identified in Study 2 was replicated by CFA in Study 3, an alternative bifactor model of the 9-item IBIP provided better fit to the data, which suggests that the full measure is well suited to provide information based on total scores by summing all 9 items. However, because two items did not contribute significant variance to the ‘hypervigilance/avoidance’ subfactor after accounting for variance in the general PTSD factor, caution should be exercised in calculating and interpreting sum scores for this subscale. Alternatively, all four items of the ‘intrusions’ subfactor contributed unique variance to this subfactor after accounting for variance contributed to the general PTSD factor, suggesting that this subscale may be reliably sum scored for use as an index of the tendency for individuals to associate spontaneous thoughts with PTSD-relevant threat. Further, the ‘intrusions’ subscale demonstrated the strongest associations with PCL-C PTSD symptoms in bivariate and regression models, suggesting that these four items may be of particular interest in future research. That the ‘intrusions’ subscale emerged as the strongest predictor of PTSD symptoms is not altogether unexpected, as intrusive reminders of past traumatic events are more uniquely characteristic of PTSD than the broader negative cognitive styles associated with distress disorders, such as looming cognitive style (Reardon & Williams, 2007; Williams, Shahar, Riskind, & Joiner, 2005) or repetitive negative thinking (Ehring & Watkins, 2008). Moreover, one may expect the ‘intrusions’ subfactor to demonstrate a more unique association with PTSD compared to the ‘hypervigilance/avoidance’ subscale, given that the latter includes items referencing difficulty concentrating, agitation, and social avoidance, all of which are common across a number of mental disorders – specifically generalized anxiety disorder and depressive disorders (APA, 2013).
The IBIP demonstrated interpretation biases specific to PTSD, per se, with subscale means higher among diagnosed individuals, compared to non-trauma-exposed and non-diagnosed trauma exposed controls. This is consistent with cognitive models of PTSD, which posit that interpretation biases are pronounced in those who develop PTSD as opposed to individuals who experience a potentially traumatic event but remain relatively free of PTSS. Moreover, results suggested interpretation biases are a meaningful component of PTSD above and beyond its nosological expression (c.f. PCL-C), as 9-item IBIP scores were associated with diagnostic status controlling for PCL-C symptom scores. Finally, Study 3 provided evidence that the 9-item IBIP could be effectively implemented as a screening measure of PTSD among clinical samples, with scores ≥ 29 most likely indicating the presence of a diagnosis.
General Discussion
These studies comprise the development of the IBIP, a brief implicit measure of threat-specific interpretation biases in individuals with PTSD. Following EFA, CFA, and bifactor modelling across analog and clinical samples, nine items emerged as the most parsimonious set capable of indexing PTSD-specific interpretation biases in a clinical population. Furthermore, because this set of items were best fitted to a bifactor model, it appears the IBIP can be sumscored to provide a general measure of PTSD-specific biases, and a lower order subscale score can be derived to reflect interpretation bias specific to intrusive recollections; however, given the non-significant loadings of two items on the hypervigilance/avoidance subfactor, it may not be as suitable for use as a separate subscale, and caution should be exercised. As the IBIP was conceptualized as a multipurpose clinical tool, including screening for and identifying probable PTSD diagnoses, a ROC curve analyses suggested ≥ 28 are most likely to identify individuals with a current PTSD diagnosis.
Together, these studies add to the existing literature to further highlight the role of interpretation biases as an important component of cognitive processes in PTSD. First, these studies corroborate the positive relationship between threatening interpretation biases and elevated PTSS (Amir et al., 2002; Elwood et al., 2007; Kimble et al., 2012). Second, these studies provide evidence that an implicit measure can reliably index PTSD-specific interpretation biases, which will help with future efforts to delineate the temporal place of interpretation biases in the development of PTSD (cf. Nanney et al., 2015). A recent study by Nanney and colleagues (Nanney et al., 2015) suggested that threat appraisal processes (i.e., interpretation biases) are independent of resultant appraisal products (i.e., cognitions or beliefs) for military service members. This led the authors to suggest that individuals who are predisposed to interpret ambiguous social cues as threatening may be more likely to develop posttraumatic negative beliefs about the self or world, thereby influencing the development of PTSS. It bears mentioning, however, that like this study, that of Nanney and colleagues was conducted during a single session, therefore obscuring many inferences about the temporal relationship between interpretations, beliefs, and symptom development in PTSD. As future research seeks to further disentangle the relationship between these mechanisms in the development of PTSD, having an independent and brief paper measure to index PTSD-specific interpretation biases such as the IBIP will be important.
Given the putative location and mechanistic function of interpretation biases in PTSD, the IBIP also provides clinical utility. First, as a putative mechanism of PTSS development (Ehlers & Clark, 2000), it has been suggested that a threat-oriented interpretation bias may be similarly a vulnerability factor for developing PTSD (Nanney et al., 2015). Though no such data were collected in the present studies, the IBIP may be useful as a screening measure among trauma-exposed individuals for the potential to develop PTSS in the hours, days, or weeks following the index event. Early identification with the IBIP could allow for intervention, providing an opportunity to thwart PTSS development. Second, given the performance of the IBIP in ROC curve analyses, it appears to function as a brief screening tool for individuals currently meeting diagnostic criteria for PTSD, among whom threat-oriented interpretation biases are already evident. Third, within the context of treatment, the IBIP may prove useful for measuring changes in this specific maintenance factor of PTSD. Because it is so brief, the IBIP could be used in place of, or in conjunction with, additional self-report measures of PTSD maintenance factors (i.e., the Posttraumatic Cognitions Inventory [PTCI; (Foa, Ehlers, Clark, Tolin, & Orsillo, 1999)]) throughout the course of treatment. This may be preferable given the feasibility of administering the IBIP, which at nine items is substantially shorter than the PTCI, which has 33 items.
Finally, as evidence mounts for the role of interpretation biases in the development and maintenance of PTSD, adjunct therapeutic tools designed specifically to target negatively biased processing seemingly hold more utility. Computerized interventions such as cognitive bias modification for interpretations (Salemink, Kindt, Rienties, & van den Hout, 2014), attention bias modification (Kuckertz et al., 2014), attention control training (Badura-Brack et al., 2015), and interference control training (Bomyea, Stein, & Lang, 2015) have all demonstrated various levels of efficacy in altering PTSD maintenance factors and symptoms. Adjunct to gold-standard cognitive behavioral treatments for PTSD, these interventions could provide additional therapeutic benefits via mechanism-specific strategies.
The present studies are not without limitations. Studies 1 and 2 were conducted in analog samples. Though Study 1 utilized abbreviated, albeit validated, subset of PCL-C items, Study 2 built off this by including full symptom measures for all distress-disorder symptoms. The PCL-C was used to index PTSS in all of these studies, as opposed to the PCL-5, for which some items were removed or added, and wording changed. We therefore do not have any data to speak to the relationships between the IBIP and the PCL-5; however, current diagnoses of PTSD in Study 3 were determined based on clinical interview using the SCID-5-RV, suggesting the IBIP is still suited for screening and measurement of current PTSD cases based on its present nosology. The IBIP should be evaluated for integrity within and across various index traumas. At face value, some items on the IBIP appear specific to traumas related to interpersonal violence and sexual assault; however, if interpretation biases indeed generalize to social-informational cues unrelated to the index trauma as hypothesized (Ehlers & Clark, 2000), the IBIP may still serve its purpose in individuals with unrelated index traumas (i.e., combat exposure), albeit not until these cognitive biases are further developed.
Although we detected significant effects in support of most hypotheses, and observed adequate model fit in our factor analytic models, replication of the latent structure of the IBIP may be warranted. Post-hoc power analysis of model fit was conducted with R statistical software (Preacher & Coffman 2006), which allows us to determine the power to detect the effects in each of the factor models. Tests of not close fit were carried out based on moderate fit (RMSEA > .06 and < .08) and good fit (RMSEA < .05) criteria (MacCallum, Browne, Sugawara, 1996). For the two-factor model identified in Study 2, the results for good fit indicated the two-factor model to be slightly underpowered (.71), though the test of moderate fit indicated adequate to maximum power (.91–1.00). Thus, we were sufficiently powered to detect the effect which we observed (RMSEA = .065). We also conducted these test for the bifactor model in Study 3. The results for good fit indicated the bifactor model to be underpowered (.59), though the test of moderate fit indicated adequate to maximum power (.82-.99). Thus, we can conclude that if our models did not provide good fit we were powered to detect that; further, concerns that we may have been slightly underpowered to detect close goodness of fit may be partially allayed given the replicability of the IBIP factor structure. Still, further replication of the bifactor structure appears warranted.
Additional studies intended to examine the IBIP’s sensitivity to change and temporal stability will be necessary to determine whether the IBIP is appropriate for use in clinical settings as a predictor of symptom development or treatment indicator, respectively. Although we eliminated the benign stimuli from the IBIP noted in Study 1, future studies may wish to test these stimuli for differences among a clinical sample. However, prior research suggests interpretation biases for construct-relevant stimuli are specific to overestimation of threat rather than a lack of ability to appropriately estimate the benign nature of neutral stimuli (Dillon, Allan, Cougle, & Fincham, 2016; Kuzkertz et al., 2013), which is consistent with the results observed in Study 1. Future research should also compare the performance of the IBIP directly against the PTCI, in relation to mechanisms for change in severity of PTSS. Though the processes supposedly indexed by the IBIP are suggested to stand independent of the products indexed by the PTCI (Nanney et al., 2015), these studies did not address that specific question. It will be important that future research distinguishes that the IBIP predicts unique variance in PTSD symptoms above and beyond posttraumatic beliefs, and further demonstrate temporal precedence of biased interpretations in the development or amelioration of posttraumatic beliefs and stress symptoms.
Considering the above limitations, these studies underscore the importance of interpretation biases in PTSD. In addition to corroborating a threat-oriented interpretation style among individuals with elevated PTSS, the IBIP proved capable of discriminating positive from negative cases of PTSD. Therefore, like other PTSD symptom measures, the IBIP has potential as a brief and multi-functional assessment tool for the prediction, screening, and categorization of PTSD in both research and clinical practice. The IBIP appears to be a promising tool for delineating the role of biased interpretation processes in the development of posttraumatic beliefs and symptoms.
Acknowledgments
Conflict of Interest: JB has received research grants from the National Institute of Mental Health. NS has received research grants from the Military Suicide Research Consortium, an effort supported by the Office of the Assistant Secretary of Defense for Health Affairs. NA was formerly a part owner of Cognitive Retraining Technologies, LLC, and has an interest in royalty income generated by the marketing of anxiety relief products by this entity. AN declares that he has no conflicts of interest. JT declares that he has no conflicts of interest.
This work was supported in part by the National Institute of Mental Health (Award No. T32 MH93311) and by the Military Suicide Research Consortium (MSRC), an effort supported by the Office of the Assistant Secretary of Defense for Health Affairs (Award No. W81XH-16-2-0003). Opinions, interpretations, and recommendations are those of the authors and are not necessarily endorsed by the U.S. Government, MSRC, or Department of Defense. Funding sources had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report, or in the decision to submit the article for publication.
Dr. Amir was formerly a part owner of Cognitive Retraining Technologies, LLC (“CRT”), a company that marketed anxiety relief products. Dr. Amir’s ownership interest in CRT was extinguished on January 29, 2016, when CRT was acquired by another entity. Dr. Amir has an interest in royalty income generated by the marketing of anxiety relief products by this entity.
Footnotes
All other authors report no financial relationships with commercial interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
As an alternative demonstration of discriminant validity, separate hierarchical regression models tested the incremental effect of IBIP total and subscale scores in predicting PSWQ, BDI-II, and PCL-C scores. A similar pattern of results emerged, wherein after controlling for the other two symptom measures in the first step, the IBIP total and ‘hypervigilance/avoidance’ subscale scores contributed the largest amount of additional variance to PCL-C, PSWQ, and BDI-II scores, respectively, but the IBIP ‘intrusions’ subscale contributed unique variance only to PCL-C scores.
References
- Adkins JW, Weathers FW, McDevitt-Murphy M, & Daniels JB (2008). Psychometric properties of seven self-report measures of posttraumatic stress disorder in college students with mixed civilian trauma exposure. Journal of Anxiety Disorders, 22(8), 1393–1402. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders (4th ed, text rev.). Washington, DC. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed). Washington, DC. [Google Scholar]
- Amir N, Coles ME, & Foa EB (2002). Automatic and strategic activation and inhibition of threat-relevant information in posttraumatic stress disorder. Cognitive Therapy and Research, 26(5), 645–655. [Google Scholar]
- Amir N, Prouvost C, & Kuckertz JM (2012). Lack of a Benign Interpretation Bias in Social Anxiety Disorder. Cognitive Behaviour Therapy, 41(2), 119–129. doi: 10.1080/16506073.2012.662655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badura-Brack AS, Naim R, Ryan TJ, Levy O, Abend R, Khanna MM, … Bar-Haim Y. (2015). Effect of attention training on attention bias variability and PTSD symptoms: randomized controlled trials in Israeli and US combat veterans. American Journal of Psychiatry, 172(12), 1233–1241. doi: 10.1176/appi.ajp.2015.14121578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard C, & Amir N (2009). Interpretation in social anxiety: When meaning precedes ambiguity. Cognitive Therapy and Research, 33(4), 406–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, & Clark DA (1988). Anxiety and depression: An information processing perspective. Anxiety Research, 1(1), 23–36. [Google Scholar]
- Beck AT, & Clark DA (1997). An information processing model of anxiety: Automatic and strategic processes. Behaviour Research and Therapy, 35(1), 49–58. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck depression inventory-II. San Antonio, TX, 78204–72498. [Google Scholar]
- Benjamini Y, & Hochberg Y (1995). Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society. Series B (Methodological), 57(1), 289–300. [Google Scholar]
- Bomyea J, Risbrough V, & Lang AJ (2012). A consideration of select pre-trauma factors as key vulnerabilities in PTSD. Clinical Psychology Review, 32(7), 630–641. doi: 10.1016/j.cpr.2012.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bomyea J, Stein MB, & Lang AJ (2015). Interference control training for PTSD: A randomized controlled trial of a novel computer-based intervention. Journal of Anxiety Disorders, 34, 33–42. doi: 10.1016/j.janxdis.2015.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chemtob C, Roitblat HL, Hamada RS, Carlson JG, & Twentyman CT (1988). A cognitive action theory of post-traumatic stress disorder. Journal of Anxiety Disorders, 2(3), 253–275. doi: 10.1016/0887-6185(88)90006-0 [DOI] [Google Scholar]
- Chen FF, Hayes A, Carver CS, Laurenceau J-P, & Zhang Z (2012). Modeling General and Specific Variance in Multifaceted Constructs: A Comparison of the Bifactor Model to Other Approaches. Journal of Personality, 80(1), 219–251. doi: 10.1111/j.1467-6494.2011.00739.x [DOI] [PubMed] [Google Scholar]
- Dillon KH, Allan NP, Cougle JR, & Fincham FD (2016). Measuring hostile interpretation bias: the WSAP-hostility scale. Assessment, 23(6), 707–719. doi: 10.1177/1073191115599052 [DOI] [PubMed] [Google Scholar]
- Ehlers A, & Clark DM (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. doi: 10.1016/S0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- Ehring T, & Watkins ER (2008). Repetitive negative thinking as a transdiagnostic process. International Journal of Cognitive Therapy, 1(3), 192–205. doi: ijct.2008.1.3.192 [Google Scholar]
- Elwood LS, Williams NL, Olatunji BO, & Lohr JM (2007). Interpretation biases in victims and non-victims of interpersonal trauma and their relation to symptom development. Journal of Anxiety Disorders, 21(4), 554–567. doi: 10.1016/j.janxdis.2006.08.006 [DOI] [PubMed] [Google Scholar]
- First MB, Williams JBW, Karg RS, & Spitzer RL (2015). Structured Clinical Interview for DSM-5—Research Version (SCID-5-RV). Arlington, VA: American Psychiatric Association. [Google Scholar]
- Foa EB, Ehlers A, Clark DM, Tolin DF, & Orsillo SM (1999). The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment, 11(3), 303–314. doi: 10.1037/1040-3590.11.3.303 [DOI] [Google Scholar]
- Frans Ö, Rimmö PA, Åberg L, & Fredrikson M (2005). Trauma exposure and post-traumatic stress disorder in the general population. Acta Psychiatrica Scandinavica, 111(4), 291–290. doi: 10.1111/j.1600-0447.2004.00463.x [DOI] [PubMed] [Google Scholar]
- Fresco DM, Heimberg RG, Mennin DS, & Turk CL (2002). Confirmatory factor analysis of the Penn State Worry Questionnaire. Behaviour Research and Therapy, 40(3), 313–323. doi: 10.1016/S0005-7967(00)00113-3 [DOI] [PubMed] [Google Scholar]
- Hayton JC, Allen DG, & Scarpello V (2004). Factor Retention Decisions in Exploratory Factor Analysis: a Tutorial on Parallel Analysis. Organizational Research Methods, 7(2), 191–205. doi: doi: 10.1177/1094428104263675 [DOI] [Google Scholar]
- Hindash AHC, & Amir N (2012). Negative interpretation bias in individuals with depressive symptoms. Cognitive Therapy and Research, 36(5), 502–511. [Google Scholar]
- Kaiser HF (1960). The application of electronic computers to factor analysis. Educational and Psychological Measurement, 20, 141–151. doi: 10.1177/001316446002000116 [DOI] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). LIfetime prevalence and age-of-onset distributions of dsm-iv disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62(6), 593–602. doi: 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). POsttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry, 52(12), 1048–1060. doi: 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Kimble M, Batterink L, Marks E, Ross C, & Fleming K (2012). Negative expectancies in posttraumatic stress disorder: Neurophysiological (N400) and behavioral evidence. Journal of Psychiatric Research, 46(7), 849–855. doi: 10.1016/j.jpsychires.2012.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuckertz JM, Amir N, Boffa JW, Warren CK, Rindt SEM, Norman S, … McLay R. (2014). The effectiveness of an attention bias modification program as an adjunctive treatment for Post-Traumatic Stress Disorder. Behaviour Research and Therapy, 63, 25–35. doi: 10.1016/j.brat.2014.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuckertz JM, Amir N, Tobin AC, & Najmi S (2013). Interpretation of Ambiguity in Individuals with Obsessive-Compulsive Symptoms. Cognitive Therapy and Research, 37(2), 232–241. doi: 10.1007/s10608-012-9478-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, & Sugawara HM (1996). Power analysis and determination of sample size for covariance structure modeling. Psychological Methods, 1(2), 130. [Google Scholar]
- Matsunaga M (2010). How to factor-analyze your data right: do’s, don’ts, and how-to’s. International Journal of Psychological Research, 3(1), 97–110. [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, & Borkovec TD (1990). Development and validation of the Penn State worry questionnaire. Behaviour Research and Therapy, 28(6), 487–495. doi: 10.1016/0005-7967(90)90135-6 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2011). Mplus User’s Guide. Sixth Edition Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nanney JT, Constans JI, Kimbrell TA, Kramer TL, & Pyne JM (2015). Differentiating between appraisal process and product in cognitive theories of posttraumatic stress. Psychological Trauma: Theory, Research, Practice, and Policy, 7(4), 372–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Coffman DL (2006). Computing power and minimum sample size for RMSEA. [Computer software]. Available from http://quantpsy.org.
- Reardon JM, & Williams NL (2007). The specificity of cognitive vulnerabilities to emotional disorders: Anxiety sensitivity, looming vulnerability and explanatory style. Journal of Anxiety Disorders, 21(5), 625–643. doi: j.janxdis.2006.09.013 [DOI] [PubMed] [Google Scholar]
- Reise SP (2012). The Rediscovery of Bifactor Measurement Models. Multivariate Behavioral Research, 47(5), 667–696. doi: 10.1080/00273171.2012.715555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salemink E, Kindt M, Rienties H, & van den Hout M (2014). Internet-based Cognitive Bias Modification of Interpretations in patients with anxiety disorders: A randomised controlled trial. Journal of Behavior Therapy and Experimental Psychiatry, 45(1), 186–195. doi: 10.1016/j.jbtep.2013.10.005 [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Norr AM, Allan NP, Raines AM, & Capron DW (2017). A Randomized Clinical Trial Targeting Anxiety Sensitivity for Patients With Suicidal Ideation. Journal of Consulting and Clinical Psychology, 85(6), 596–610. doi: 10.1037/ccp0000195 [DOI] [PubMed] [Google Scholar]
- Steer RA, & Clark DA (1997). Psychometric characteristics of the Beck Depression Inventory-II with college students. Measurement and Evaluation in Counseling and Development, 30(3), 128. [Google Scholar]
- Watson D (2005). Rethinking the mood and anxiety disorders: a quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology, 114(4), 522–536. doi: 10.1037/0021-843X.114.4.522 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, & Keane TM (1993). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the annual convention of the international society for traumatic stress studies. [Google Scholar]
- Williams NL, Shahar G, Riskind JH, & Joiner TE Jr. (2005). The looming maladaptive style predicts shared variance in anxiety disorder symptoms: Further support for a cognitive model of vulnerability to anxiety. Journal of Anxiety Disorders, 19(2), 157–175. doi: .janxdis.2004.01.003 [DOI] [PubMed] [Google Scholar]