Purpose of review
The current article reviews recent literature examining occupational voice use and occupational voice disorders (January 2018–July 2019).
Recent findings
Our understanding of the prevalence of voice disorders and work-related vocal use, vocal load and vocal ergonomics (environmental and person influences) across different occupations is continuing to build. There is encouraging evidence for the value of intervention programs for occupational voice users, particularly of late with performers, teachers and telemarketers. Education and prevention programs are emerging for other ‘at risk’ occupations.
Summary
Occupational health and workforce legislation does not adequately acknowledge and guide educational, preventive and intervention approaches to occupational voice disorders. Voice disorders are prevalent in certain occupations and there is an urgent need for research to support occupational voice health and safety risk measurement, prevention and intervention. Large population-based studies are required with a focus on the health and economic burden of occupational voice disorders.
Keywords: dysphonia, economics, occupational health, occupational voice users, voice
INTRODUCTION
Occupational voice disorder literature is expanding with a call for improved occupational health and safety standards and legislation to protect voice [1,2]. Many occupations have been identified as at-risk for the development of voice disorders as a consequence of their inherent work conditions [3,4▪▪]. While such studies are valuable in identifying ‘who’ is at-risk and in the exploration of possible influences, there is a lack of recent epidemiological information for occupational voice disorders in the general nontreatment-seeking population and what we do have is potentially outdated [5,6,7▪].
Despite the high prevalence of occupational voice disorders, the WHO neglects to itemize voice disorders as a potential occupationally related disease or condition [8]. It is also difficult to determine where voice disorders fit within the existing criteria for work-related disease (communicable and noncommunicable) and injuries (intentional and unintentional). This may in part be due to the multidimensional nature of voice disorders as well as the inherent difficulty in measurement and in establishing an operational definition of vocal injury.
Definitions of work-related voice disorders or vocal injuries may vary across geographical location according to relevant legislation, terminology and context. Yet, any speech pathologist understands the enormity of the occupational voice-user population whereby voice is a critical occupational tool and no voice equals no work today – singers, stage performers, sports coaches, sales assistants, teachers, lecturers, lawyers, telephone operators, call centre workers, receptionists, priests and health professionals. Speech pathologists witness first-hand the extreme financial repercussions of voice disorders as well as the impact on social and professional identity.
There is a longstanding assumption of a causal relationship between heavy voice-use and the development of voice problems. More recent research however, suggests that the relationship is more complex. There are people working in heavy voice-use occupations who do not experience vocal difficulties. Many other environmental and contextual factors (coined voice ergonomics) have been proposed to exert an effect [9▪▪]. There has been a shift toward the exploration of these occupation-specific environmental factors as well as person factors, such as vocal fitness, as determinants of vocal survival in the workplace especially for those with sustained heavy load [10].
The new American Academy of Otolaryngology-Head & Neck Surgery Clinical Practice Guideline: Hoarseness (Dysphonia), estimates the direct health costs of dysphonia in the US up to US$13.5 billion [11]. Overall economic costs from lost work days, however, is in addition and requires more attention. Described 20 years ago within the Australian context, Pemberton et al.[12] estimated teachers’ lost work days due to voice problems averaged 1.3 days/year. This absenteeism was estimated conservatively to cost the Victorian State Government approximately $17 million per annum. More recently, Pemberton [13▪▪] presented to the Australian Government on the impressive outcomes from a large-scale ‘voice care for teachers’ program spanning over 5 years (n ≥ 1500 teachers). In purely economic terms for the employer, a saving of $500 000 (AUD) was estimated due to reduced voice-related sick leave.
This current opinion provides an overview of the articles that have published in the last 18 months (January 2018–July 2019) on the topic of occupational voice. We cover ‘at-risk’ workforce groups, work-related influences on vocal health, risk measurement and intervention, as well as considerations for the future.
Box 1.
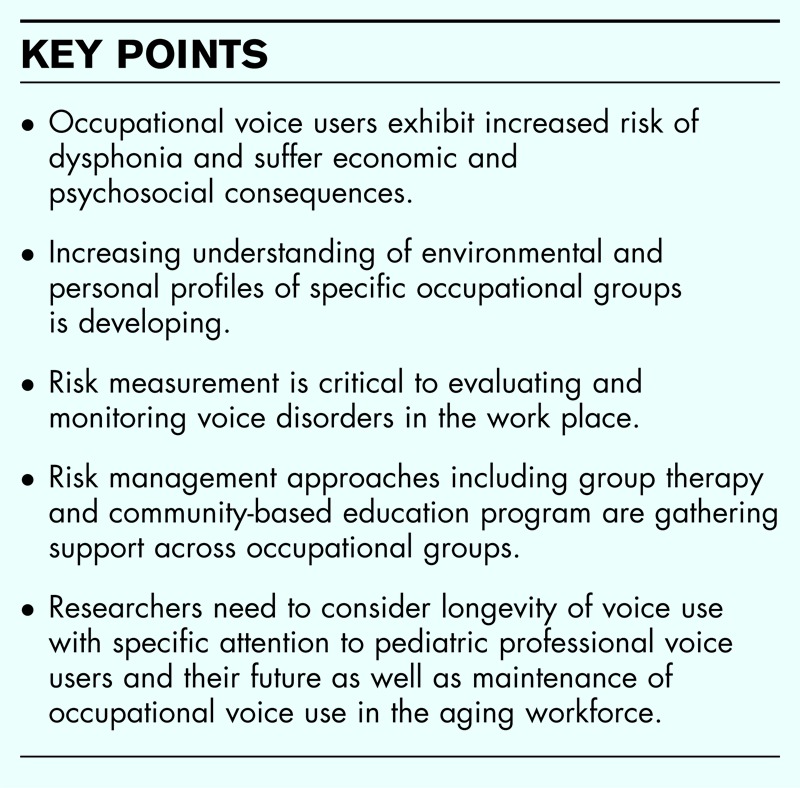
no caption available
OCCUPATIONAL RISK
Risks of vocal harm in those using their voice directly in performance of work duties needs to be understood to provide preventive strategies and early interventions aimed at minimizing development of vocal pathology.
Occupational voice users
Over the last few years, there has been a plethora of articles exploring voice use and voice disorders in specific occupational groups worldwide. Teachers, frequent visitors to the voice clinic, continue to feature heavily in the research [14–33]. International research is now also appearing across a wider range of occupations: radio broadcasters [34], wind instrumentalists [35], fitness instructors [36▪,37], cycling instructors [38▪], university professors [39–41], telemarketers [42], tour guides [43], street vendors [44], Islamic officials [45], scientists exposed to chemical irritants [46] and sports coaches [47]. Teachers with music in their job description are receiving more attention including music theory teachers [48], elementary school music teachers [25,48] and music therapists [49,50]. Joseph et al.[51] wrote an article titled ‘Do young speech pathologists practice what they preach?. They found speech pathologists did not follow the vocal health principles that they provide to others.
Although most articles describe voice disorder prevalence or list vocal symptoms, there is a recent focus on work-related communication and environmental profiles in specific occupations [34,38▪]. A novel and carefully designed observation of indoor cycle instructors found reduced perceived phonatory effort with the addition of amplification but continuing high vocal dose. They hypothesize the loud ambient noise in the indoor cycling arena might cause a Lombard Effect leading to involuntary louder speaking irrespective of amplification [38▪]. These types of studies may lead to useful insights for preventive and rehabilitation programs for specific populations.
Professional voice users
Chitguppi et al.[52] propose a nomenclature for people who rely on their voice for their occupation and suggest such voice users should be split into speaking and nonspeaking voice professionals. This may prove useful for determining relative prevalence figures for work-related voice disorders among each group as current information is confounded by differences in voice use characteristics and work-contexts between singers and nonsinger professionals. Certain studies have used this binary classification to report differences between professional voice users [52–54].
As an alternative construct, professional voice users are distinguished from occupational voice users in a new textbook Voice Ergonomics: Occupational and Professional Voice Care: an excellent resource for voice teams [9▪▪]. The authors define professional voice users as those who have a need for a skillful voice as distinct from occupational voice-users ‘who need a lot of voice and often must use a loud voice’ (such as the teachers and sports coaches described in the previous section). They further separate this group from active voice users who use their voice during a working day but without regularly raised intensity (e.g. telemarketers and health workers) [9▪▪]. This proposed classification system is novel and provides interesting criteria for delineating the different vocal loads, work characteristics and phonatory needs.
The professional vocalist or working vocal artist is perhaps historically one of the most recognized ‘at risk’ professional voice user for the development of phonotraumatic lesions. However, employment-related prevalence figures for singers and actors are confounded by huge heterogeneity across and among these voice users in environmental and person variables such as type of voice use, performance environment, music genre, repertoire, context, vocal expectations and voice training. Other difficulties are the reliance on treatment-seeking populations, the inclusion of amateur performers and that many studies do not specify whether performance is the primary occupation.
Despite the dearth of epidemiologic studies, further valuable insights have been provided over the past 18 months regarding vocal health, voice demands, laryngology findings and treatment options among specific performer groups such as elite award-winning performers [55▪], Broadway singers [56▪▪], opera singers [57], theater singers [58▪], theater actors [59], and singers of specific cultural music styles such as Carnatic [60], Korean classical [61] and Fado singers [62]. Weekly et al.[63▪▪] conducted a global survey of an impressive number of amateur and professional voice-users (n = 1195) on their vocal health practices and included both speaking and nonspeaking voice users. They found a third of respondents did not access medical care due to insurance or financial constraints. This suggests treatment-seeking populations may be an under-representation of the number of working vocalists with voice disorders.
RISK MEASUREMENT AND VOICE ERGONOMICS
Sustained heavy vocal load in the workplace has been long identified as the primary threat to employees’ vocal health [4▪▪,64]. Some studies have now challenged this notion showing, for some voice users, heavy vocal load can have a positive effect on immediate vocal function postloading [10,58▪,59] and may even help build voice strength and endurance [65,66]. Our understanding of ergonomic and person-related influences in the work context is expanding. Further described risks include nonconducive speaking environments and background noise impact [25,26,37,67–69,70▪,71], workload [19], stress and anxiety [28,29,72], posture [22], reduced respiratory [73] or cardiopulmonary function [74▪] and shyness [75]. Table 1 displays ergonomic and person-factor influences on vocal health.
Table 1.
Ergonomic and person-factor influences on vocal health
| Influence | Examples of potential influences (+ve and −ve) |
| Work environment & vocal demands | |
| Place of most voicing | Mixed, indoor, outdoor, car, retail shop, performance tent |
| Vocal dose | Intensity, frequency and duration of voicing time |
| Manner of voicing for work | Singing (type), speaking, character voice, degree of effort |
| Voicing schedule | Number of hours per day voicing, number of consecutive days, periods of voice rest, shows per week, double shows, weeks on/off |
| Room acoustics | High ceilings, reverberation, background noise, open plan classroom, car noise |
| Use of acoustic support/strategies | Foldback, portable microphone, amplifier, megaphone, bell, clap |
| Posture while voicing | Standing, leaning, habitual chin out, in a harness, dancing, exercising, head tilted (on phone) |
| Air conditions | Humidity, quality, temperature, consistency, dust, pollens, heating, odors, air conditioning and proximity to vents |
| Work stressors | Difficult classroom behavior, production week, high workload, employment status (contract versus permanent) |
| Voice efficiency | Breathy quality, poor phrasing, speaking on residual air, habitual use of hard glottal attacks |
| Routine of work practices for voice | Casual relief teaching, extra fitness classes, parent interviews |
| Manner of voicing for work | Habitual intensity required, use of character voice/s, degree of effort |
| Person factors | |
| General | Age, sex, personality, physical fitness, health, lifestyle, quality of life, job satisfaction and communication style |
| Voice training | Type and relevance to work (singing, speaking), quantity, consistency and recency |
| Vocal fitness | Voice stability, endurance and recovery thresholds, recent vocal activity (e.g. rehearsals, previous show, back from maternity leave) |
| Vocal load outside of work | Involved in choir, part-time bartender, karaoke singing |
| Value attached to voice | Previous elite singer, regularly complimented on husky voice, voice identity incongruent with current voice, and high voice expectations |
A previously unreported proactive Australian voice care program, conducted for performers in a large-scale production known as Santa's Kingdom 2004, showed performance vocal load can be less important than other work-related factors (Phyland, unpublished). Performers (n = 210) involved in this interactive exhibition worked intensively for the 4 weeks prior to Christmas in loud performance/activity stations around a large exhibition space. All underwent vocal screening baselines, vocal health education and end-of-production voice assessments. Significant short-term deterioration in vocal function was found for 151 (72%) of the performers on self-report surveys and perceptual and acoustic evaluation, although there were no ongoing concerns after the production conclusion. Of great interest was the finding that even those with no or little speaking or singing performance (e.g. polar bear characters who were mute and fully suited) still demonstrated significant acute vocal change. Vocal fatigue was attributed by many performers to an intensive work timetable and highly social ‘extra-curricular’ culture, rather than inherent occupational vocal demands.
Although the identification and measurement of ‘at risk’ behaviors and influences has advanced, the measurement of direct positive and negative impact of these factors on the vocal health of workers is not straightforward. Proving causation of work-related voice disorders is perhaps easier for acute injuries (such as vocal hemorrhage) than chronic voice disorders. Undertaking baseline vocal assessments and regular screening are important for tracking potential voice changes and as points for comparison [49,68,71,76–80]. It is important to understand normal fluctuations in vocal function across the working hours and days, and what symptoms (including fatigue), durations and severities constitute critical threshold points for development of voice disorders [41,46,69,80–82]. Assessing vocal dose and calculations of occupational vocal load have received much recent research attention and include tools such as visual analogue scales, dosimetry accumulators, fatigue inventories and the Vocal Fatigue Index [14,38▪,46,48,51,66,67,71,76,78,83,84▪]. A newly validated self-report scale called the Evaluation of the Ability to Voice Easily may hold promise for tracking fluctuations in speaking voice function as perceived by the voice user and for identifying risk thresholds or cut-off points (Phyland, 2019, in press). Some studies have also explored the impact of a voice disorder on work performance in addition to other dimensions of voice-related quality of life [18,70▪,85].
RISK MANAGEMENT, HABILITATION AND REHABILITATION
Despite performers being identified as a high-risk group [86▪▪], employer management, within the entertainment industry in particular, of work-related vocal injuries (such as phonotraumatic lesions) is frequently suboptimal [56▪▪]. The economic, logistic and psychological ramifications of a vocal injury can be dire for both employee and employer with cancelled shows, loss of audience support, and an inappropriate assumption of poor vocal technique leading to a stigma and reduced future employment prospects for the injured performer. Fortunately, with increased understanding of the etiological factors in vocal injuries focus is changing to a commitment to provide prevention and risk management programs across many different voice-user groups [10,87▪▪,88,89▪,90–92].
There is emergence of proactive occupational health practices. It is difficult to get direct evidence of the efficacy of industry-funded programs due to sensitivity of data and methodological limitations in the program designs, as most do not have research as the primary objective. However, voice habilitation and rehabilitation programs, particularly in teachers and performers, feature in the recent international literature, with a favouring of the term vocal health over hygiene to better represent the philosophical underpinnings. Programs include education, vocal screens and audits and specific habilitation approaches, for example, the use of saline nebulizers and amplifiers [30,84▪,86▪▪,89▪,90,91]. Promising improvements have been demonstrated in self-perceived vocal scores, reduction in vocal attrition, and diagnosed or reportable incidents of voice disorders [30,84▪,86▪▪,89▪,90,91]. Melbourne Theatre Company introduced a voice care program which has been in place for 25 years and this model of prevention is presented in Fig. 1.
FIGURE 1.
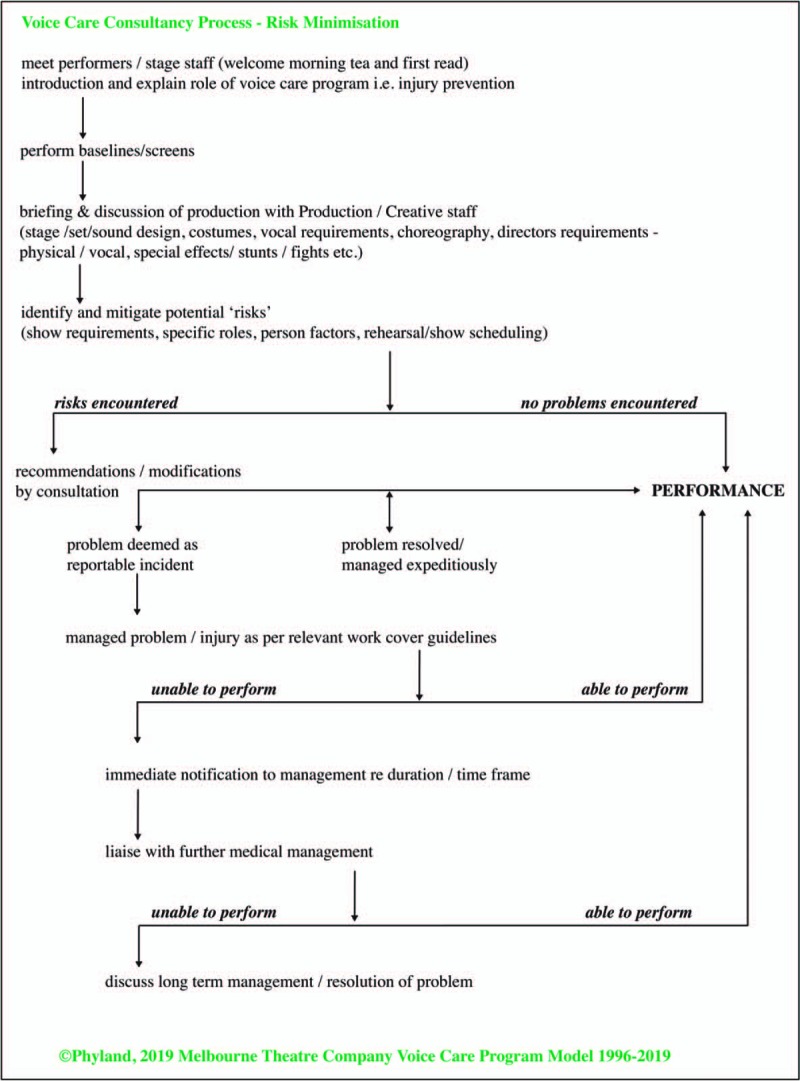
Voice care consultancy process – risk minimization (Voice Medicine Australia).
Research into risk management of work-related vocal ‘injuries’ is thwarted by privacy protection and sensitivity of information related to both the employer and employee. Occupationally induced voice disorders are strongly represented in laryngology clinics and require comprehensive assessment (with stroboscopy as a standard of care) and expert understanding of the occupational context and its’ potential relationship to the development, maintenance and recovery of voice disorders [52,55▪,93▪]. Frequently these occupational voice users will require voice therapy, surgery and expeditious return to work programs [23,52,54,55▪,56▪▪,64,84▪,86▪▪,94,95]. There is a need to further evaluate intervention outcomes, improve understanding of rehabilitation and to develop evidence-based criteria to determine performance fitness in relation to ability to meet vocal requirements (e.g. voice quality, strength, stamina, ease and reliability), across all work-contexts.
CONSIDERATIONS FOR THE FUTURE
Aging workforce
With our understanding of workforce vocal challenges across occupations accumulating, there is a need to also consider other contributions to voice. Allen and Miles [96] provided a comprehensive summary of age-related changes to the voice and current evidence-based interventions as part of a Special Issue on Ageing in Speech, Language and Hearing. Our international trends of an aging workforce imply there will be a need to address the combination of presbyphonia and occupational voice use more frequently in the future. Research into aging and continued occupational voice use is critical for future-proofing our workforce [96,97].
Early onset professional voice use
It is not only adult vocalists that use their voice professionally – child performers also work with their voices especially within the entertainment industry (television, film and the music theater). Many of the shows introduced this century such as Billy Elliot The Musical, Matilda The Musical and School of Rock The Musical feature children as central to the plot and can even involve a greater number of children than adults in the cast (Fig. 2). The associated occupational voice demands can be heavy and there is an urgent need for research investigating the impact of this load on the development of the child performers’ vocal folds and vocal function [98,99]. Unpublished data from Phyland's lab on the outcomes of a voice care program demonstrated child performers (n = 194) working in professional musical theatre productions experienced no negative change in vocal function. Children can be highly resilient in managing heavy vocal load over lengthy production seasons with appropriate and expert vocal care but long term impact needs to be monitored and speech pathologists and laryngologists still need to advocate for optimal conditions for these children still undergoing laryngeal anatomical development.
FIGURE 2.
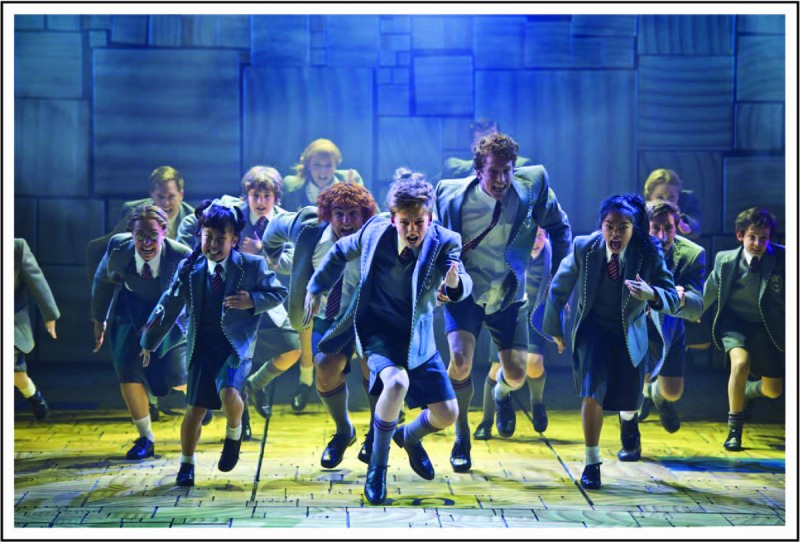
Matilda The Musical original Australian company. Photo: James D. Morgan.
CONCLUSION
Voice disorders are prevalent in specific occupational groups and there is an urgent need for research to support occupational voice health and risk measurement, prevention and intervention. Our understanding of vocal use, vocal load and vocal ergonomics (environmental and person influences) across different occupational groups is building. There is encouraging evidence supporting intervention programs for occupational voice users with a primary focus on teachers and increasingly including performers. Education and prevention programs are emerging. Large population-based studies are required with a focus on health and economic burden of occupational voice disorders. International occupational health and workforce legislation does not currently adequately acknowledge, prioritise or guide educational and preventive interventions. There is an urgent need to formally identify combined risk factor bundles or environments; quantify the potential threat that voice disorders pose to a safe and healthy workplace; reduce the expression of voice disorders and its concomitant occupational burden; and develop prevention, management and health promotion targeted toward optimal occupational vocal function.
Acknowledgements
Santa's Kingdom, Sam Schwartz-Company Manager, Gary Van Egmond Productions (2004). Matilda The Musical Original Australian Production-Philippa Gowan, General Manager, Louise Withers and Associates.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Arcangeli G, Giorgi G, Mucci N, et al. Emerging and re-emerging organizational features, work transitions and occupational risk factors: the good, the bad, the right. An interdisciplinary perspective. Front Psychol 2018; 9:1533–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sagha Zadeh R, Shepley MM, Owora AH, et al. The importance of specific workplace environment characteristics for maximum health and performance: healthcare workers’ perspective. J Occup Environ Med 2018; 60:e245–e252. [DOI] [PubMed] [Google Scholar]
- 3.Lyberg-Åhlander V, Rydell R, Fredlund P, et al. Prevalence of voice disorders in the general population, based on the Stockholm public health cohort. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 4▪▪.Cutiva LCC. Association between occupational voice use and occurrence of voice disorders: a meta-analysis. Areteé 2018; 18:1–10. [Google Scholar]; A useful systematic review and meta-analysis showing relationship between voice disorders and occupational voice use.
- 5.Verdolini K, Ramig LO. Occupational risks for voice problems. Logoped Phoniatr Vocol 2001; 26:37–46. [PubMed] [Google Scholar]
- 6.Roy N, Merrill RM, Gray SD, Smith EM. Voice disorders in the general population: prevalence, risk factors, and occupational impact. Laryngoscope 2005; 115:1988–1995. [DOI] [PubMed] [Google Scholar]
- 7▪.Bainbridge KE, Roy N, Losonczy KG, et al. Voice disorders and associated risk markers among young adults in the United States. Laryngoscope 2017; 127:2093–2099. [DOI] [PMC free article] [PubMed] [Google Scholar]; Large epidemiological study showing risk factors for voice disorders in young adults.
- 8.Wolf J, Prüss-Ustün A, Ivanov I, Mugdal S. Preventing disease through a healthier and safer workplace. 2018; Geneva, Switzerland: World Health Organization, License: CC BY-NC-SA 3.0 IGO 2019(31/07). [Google Scholar]
- 9▪▪.Sala E, Rantala LM, Simberg S. Voice disorder and voice ergonomics: occupational and professional voice care. 2019; Newcastle upon Tyne, UK: Cambridge Scholars, [Google Scholar]; An essential new resource for voice teams.
- 10.Phyland DJ. Choral singing and vocal health – young choristers are not harming by harmonizing. JAMA Otolaryngol Head Neck Surg 2019; 145:451–452. [DOI] [PubMed] [Google Scholar]
- 11.Stachler RJ, Francis DO, Schwatz SR, et al. American academy of otolaryngology-head & neck surgery clinical practice guideline: hoarseness (dysphonia). Otolaryngol Head Neck Surg 2018; 158:S1–S42. [DOI] [PubMed] [Google Scholar]
- 12.Pemberton C, Oates J, Russell A. Victorian parliamentary enquiry – effective classroom strategies voice injury in teachers: how to minimise occupational risk. 1999. [Google Scholar]
- 13▪▪.Pemberton C. Speech pathology has an important role in efficiently and cost-effectively managing teachers voice problems. Submission to Australian Senate Inquiry: submission 86 2018; 2019(31/07). [Google Scholar]; Impressive outcomes from a 5-year state-wide teacher voice program in Australia.
- 14.Abou-Rafée M, Zambon F, Badaró F, Behlau M. Vocal fatigue in dysphonic teachers who seek treatment. Codas 2019; 31:e20180120. [DOI] [PubMed] [Google Scholar]
- 15.Albustan SA, Marie BS, Natour YS, Darawsheh WB. Kuwaiti teachers’ perceptions of voice handicap. J Voice 2018; 32:319–324. [DOI] [PubMed] [Google Scholar]
- 16.Chowdhury K, Dawar H. Impact of classroom determinants on psychosocial aspects of voice among school teachers of Indore, India: a preliminary survey. Indian J Otolaryngol Head Neck Surg 2018; 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Sousa E, Goel HC, Fernandes VLG. Study of voice disorders among school teachers in Goa. Indian J Otolaryngol Head Neck Surg 2018; 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greve K, Bryn EK, Simberg S. Voice disorders and impact of voice handicap in Norwegian student teachers. J Voice 2018. [DOI] [PubMed] [Google Scholar]
- 19.Lee YR, Kim HR, Lee S. Effect of teacher's working conditions on voice disorder in Korea: a nationwide survey. Ann Occup Environ Med 2018; 30:43–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Munier C, Brockmann-Bauser M, Laukkanen AM, et al. Relationship between laryngeal signs and symptoms, acoustic measures, and quality of life in Finnish primary and kindergarten school teachers. J Voice 2019; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 21.Nusseck M, Spahn C, Echternach M, et al. Vocal health, voice self-concept and quality of life in German school teachers. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 22.Rantala L, Sala E, Kankare E. Teachers’ working postures and their effects on the voice. Folia Phoniatr Logop 2018; 70:24–36. [DOI] [PubMed] [Google Scholar]
- 23.Rinsky-Halivni L, Klebanov M, Lerman Y, Paltiel O. Adherence to voice therapy recommendations is associated with preserved fitness-for-work among teachers with occupational voice disorders. J Voice 2017; 31:386.e19–386.e26. [DOI] [PubMed] [Google Scholar]
- 24.Sathyanarayan M, Boominathan P, Nallamuthu A. Vocal health practices among school teachers: a study from Chennai, India. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 25.Colombia University, New York, Stephenson KJ. Teacher views on teacher voice: elementary music teacher perceptions of voice use in the workplace (doctoral dissertation). 2018. [Google Scholar]
- 26.University of Kansas, USA, Teters C. An investigation into environmental sound levels and vocal behaviors of female secondary school choir teachers: a collective case study. 2018. [Google Scholar]
- 27.Phadke KV, Abo-Hasseba A, Švec JG, Geneid A. Influence of noise resulting from the location and conditions of classrooms and schools in Upper Egypt on teachers’ voices. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 28.Gomes KO, Lima VHA, de Sousa DS, et al. Overview of occupational diseases caused by mental stress most frequently observed in Brazilian teachers: a review. Int Neuropsychiatr Dis 2018; 11:1–11. [Google Scholar]
- 29.Vertanen-Greis H, Löyttyniemi E, Uitti J. Voice disorders are associated with stress among teachers: a cross-sectional study in Finland. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 30.Meier B, Beushausen U. Long-term effects of a voice training program to prevent voice disorders in teachers. J Voice 2019; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 31.Menon UK, Raj M, Antony L, et al. Prevalence of voice disorders in school teachers in a district in South India. J Voice 2019; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 32.Cha S, Byeon H. A systematic review on voice characteristics and risk factors of voice disorder of Korea teachers. J Korea Convergence Soc 2018; 9:149–154. [Google Scholar]
- 33.Phadke KV, Laukkanen AM, Ilomäki I, et al. Cepstral and perceptual investigations in female teachers with functionally healthy voice. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 34.Cantor-Cutiva LC, Bottalico P, Hunter E. Work-related communicative profile of radio broadcasters: a case study. Logoped Phoniatr Vocol 2018; 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cappellaro J, Beber BC. Vocal tract discomfort and voice-related quality of life in wind instrumentalists. J Voice 2018; 32:314–318. [DOI] [PubMed] [Google Scholar]
- 36▪.Aiken PJ, Rumbach AF. Keeping the voice fit in the group fitness industry: a qualitative study to determine what instructors want in a voice education program. J Voice 2018; 32:256.e25–256.e34. [DOI] [PubMed] [Google Scholar]; Insightful qualitative study asking fitness industry employees what they want from a voice program.
- 37.Estes C, Sadoughi B, Coleman R, et al. Phonotraumatic injury in fitness instructors: risk factors, diagnoses, and treatment methods. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 38▪.Allison LH, Sandage MJ, Weaver AJ. Vocal dose for rhythm-based indoor cycling instructors: with and without amplification. J Voice 2019; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]; Well designed study observing the occupation-specific challenges of indoor cycling instructors.
- 39.Gomes NR, Teixeira LC, de Medeiros AM. Vocal symptoms in University professors: their association with vocal resources and with work environment. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 40.Kyriakou K, Petinou K, Phinikettos I. Risk and prevalence of self-perceived voice disorders in male and female university professors. J Environ Health Sci 2018; 4:26–33. [Google Scholar]
- 41.Korn GP, Park SW, de Lima Pontes AA, Pontes P. Vocal symptoms and associated risk factors between male and female university teachers. Int Arch Otorhinolaryngol 2018; 22:271–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fuentes-López E, Fuente A, Contreras KV. Inadequate vocal hygiene habits associated with the presence of self-reported voice symptoms in telemarketers. Logoped Phoniatr Vocol 2019; 44:105–114. [DOI] [PubMed] [Google Scholar]
- 43.Sanssené C, Bardi J, Welby-Gieusse M. Prevalence and risk factors of voice disorders in French tour guides. J Voice 2019; 33:66–72. [DOI] [PubMed] [Google Scholar]
- 44.Natour YS, Darawsheh WB, Bashiti S, et al. A study of VHI scores and acoustic features in street vendors as occupational voice users. J Commun Disord 2018; 71:11–21. [DOI] [PubMed] [Google Scholar]
- 45.Büyükatalay ZC, Gökmen MF, Yıldırım S, Dursun G. Voice disorders in Islamic religious officials: is it any different than those of the teachers, and other well known professional voice users? J Voice 2019; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 46.Hoode A, Mathew L, Thomas AA. Vocal fatigue inventory measures in individuals exposed to laboratory chemicals. Lang India 2019; 19:12–20. [Google Scholar]
- 47.Bučević A, Bonetti A, Bonetti L. The voice quality of sports coaches. Logopedija 2018; 8:1–5. [Google Scholar]
- 48.Schiller IS, Morsomme D, Remacle A. Voice use among music theory teachers: a voice dosimetry and self-assessment study. J Voice 2018; 32:578–584. [DOI] [PubMed] [Google Scholar]
- 49.Brunkan MC. Preservice music teacher voice use, vocal health, and voice function before and during student teaching. J Music Teach Educ 2018; 27:80–93. [Google Scholar]
- 50.Waldon EG, Isetti D. Voice disorders and related risk factors among music therapists: survey findings and strategies for voice care. Music Ther Perspect 2018; 37:37–44. [Google Scholar]
- 51.Joseph BE, Joseph AM, Jacob TM. Vocal fatigue – do young speech-language pathologists practice what they preach? J Voice 2019; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 52.Chitguppi C, Raj A, Meher R, Rathore PK. Speaking and nonspeaking voice professionals: who has the better voice? J Voice 2018; 32:45–50. [DOI] [PubMed] [Google Scholar]
- 53.Chitguppi C, Raj A, Meher R, Rathore PK. Is the voice of professional voice users with no vocal cord lesions similar to that of non professional voice users. J Voice 2018; 33:66–72. [DOI] [PubMed] [Google Scholar]
- 54.Sheikhany A, Atef A, Refaat O, Al Ali A. Impact of voice disorders and microlaryngeal surgery on psychological profiles of Arabic-speaking professional and nonprofessional voice users. Egypt J Otolaryngol 2019; 35:182–188. [Google Scholar]
- 55▪.Zeitels SM. The art and craft of phonomicrosurgery in Grammy award-winning elite performers. Ann Otol Rhinol Laryngol 2019; 128:7S–24S. [DOI] [PubMed] [Google Scholar]; Timely study in terms of increasing public interest in vocal health of elite performers.
- 56▪▪.Bradshaw N, Coopeer AL. Medical privacy and the professional singer: injury stigma, disclosure, and professional ramifications on Broadway. J Singing 2018; 74:513–520. [Google Scholar]; Critical review of the risks, financial challenges and stigma for professional singers for anyone working with singers.
- 57.Pizzorni N, Schindler A, Sozzi M, et al. The vocal score profile in Verdi's characters. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 58▪.Pacheco C, Behlau M. Immediate impact of vocal demand on musical theater singers in Brazil. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]; Well designed study of vocal demand in singers.
- 59.Martin E, Battaglini C. Health status of live theater actors. Med Probl Perform Art 2019; 34:108–117. [DOI] [PubMed] [Google Scholar]
- 60.Devadas U, Kumar PC, Maruthy S. Prevalence of and risk factors for self-reported voice problems among Carnatic singers. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 61.Kan H, Ki S, Yo J. Voice hygiene habits and the characteristics of Korean Voice-Related Quality of Life (K-VRQOL) among classical singers. Phon Speech Sci 2018; 10:49–59. [Google Scholar]
- 62.Pestana PM, Vaz-Freitas S, Manso MC. Prevalence, characterization, and impact of voice disorders in Fado singers. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 63▪▪.Weekly EM, Carroll LM, Korovin GS, Fleming RA. Vocal health survey among amateur and professional voice users. J Voice 2018; 32:474–478. [DOI] [PubMed] [Google Scholar]; Large study of vocal health in amateur and professional voice users.
- 64.Zabret M, Hočevar Boltežar I, Šereg Bahar M. The importance of the occupational vocal load for the occurrence and treatment of organic voice disorders. Zdr Varst 2018; 57:17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.LeBorgne W, Rosenberg M. Application of exercise physiology principles for vocal athletes during vocal injury recovery and performance maximization. Perspect ASHA Spec Interest Groups 2018; 3:88–96. [Google Scholar]
- 66.Sandage MJ. Muscle fatigue physiology applied to management of voice fatigue. Perspect ASHA Spec Interest Groups 2018; 3:7–11. [Google Scholar]
- 67.Patrizia OM, Fabio LC, Sergio I, Raffaele M, Lucia L, Claudia G, Ergonomics and acoustics in music education. Proceedings of the 20th Congress of the International Ergonomics Association (IEA 2018). Eds Bagnara, S., Tartaglia, R., Albolino, S., Alexander, T., Fujita, Y. Springer Nature 2019. [Google Scholar]
- 68.Ryan S, Swartz D. Solving the acoustic issue in physical education settings. Int J Phys Educ Fitness Sports 2018; 7:11–16. [Google Scholar]
- 69.Remacle A, Garnier M, Gerber S, et al. Vocal change patterns during a teaching day: inter-and intra-subject variability. J Voice 2018; 32:57–63. [DOI] [PubMed] [Google Scholar]
- 70▪.Portela AS, Granqvist S, Ternström S, Södersten M. Vocal behavior in environmental noise: comparisons between work and leisure conditions in women with work-related voice disorders and matched controls. J Voice 2018; 32:126–223. [DOI] [PubMed] [Google Scholar]; Useful study for considering environmental risk factors for clients.
- 71.Rollins MK, Leishman TW, Whiting JK, et al. Effects of added absorption on the vocal exertions of talkers in a reverberant room. J Acoust Soc Am 2019; 145:775–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gomes VEFI, da Costa Batista D, Lopes LW, et al. Symptoms and vocal risk factors in individuals with high and low anxiety. Folia Phoniatr Logop 2019; 71:7–15. [DOI] [PubMed] [Google Scholar]
- 73.Hunter EJ, Maxfield L, Graetzer S. The effect of pulmonary function on the incidence of vocal fatigue among teachers. J Voice 2019; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74▪.Omodara OO, Mshelia PP, Madaki AA, Saleh MIA. Comparative study of cardiopulmonary functions in trained male athletes and singers – a pilot study. J Adv Med Pharm Sci 2018; 16:1–8. [Google Scholar]; Highlights the importance of physical fitness in sustained voice production and recovery.
- 75.Gimenez SRML, Madazio G, Zambon F, Behlau M. Analysis of shyness on vocal handicap perceived in school teachers. Codas 2019; 31:e20180149. [DOI] [PubMed] [Google Scholar]
- 76.Singapore, Mahalakshmi P, Dhawan R, Bharadwaj K, Ray MK. Mahalakshmi P, Dhawan R, Bharadwaj K, Ray MK. Development of a system for quantitative assessment of vocal loading. Development of a system for quantitative assessment of vocal loading 2018; Springer, 615–623. [Google Scholar]
- 77.Morawska J, Niebudek-Bogusz E, Wiktorowicz J, Sliwinska-Kowalska M. Screening value of V-RQOL in the evaluation of occupational voice disorders. Med Pr 2018; 69:119–128. [DOI] [PubMed] [Google Scholar]
- 78.Xue C, Kang J, Hedberg C. Dynamically monitoring vocal fatigue and recovery using aerodynamic, acoustic, and subjective self-rating measurements. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 79.Nix J, Roy N. McPherson G, Welch G. Voice health and vocal education. Oxford Handbooks, Vocal, instrumental, and ensemble learning and teaching: an Oxford handbook of music education. Newcastle upon Tyne, UK: 2018. [Google Scholar]
- 80.Ulozaite-Staniene N, Petrauskas T, Šaferis V, Uloza V. Exploring the feasibility of the combination of acoustic voice quality index and glottal function index for voice pathology screening. Eur Arch Otorhinolaryngol 2019; 276:1737–1745. [DOI] [PubMed] [Google Scholar]
- 81.McKenna VS, Diaz-Cadiz ME, Shembel AC, et al. The relationship between physiological mechanisms and the self-perception of vocal effort. J Speech Lang Hearing Res 2019; 62:815–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pellicani AD, Fontes AR, Santos FF, et al. Fundamental frequency and formants before and after prolonged voice use in teachers. J Voice 2018; 32:177–184. [DOI] [PubMed] [Google Scholar]
- 83.Moghtader M, Soltani M, Mehravar M, et al. The relationship between vocal fatigue index and voice handicap index in university professors with and without voice complaint. J Voice 2019; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 84▪.Sandage MJ, Hoch M. Training considerations for recital performance: framing vocal dose in a fatigue resistance training model. J Singing 2019; 75:395–400. [Google Scholar]; Important study highlighting shift toward preventive approaches.
- 85.Lia L, De SF, Mannocci A, et al. A cross sectional study on the vocal handicap index applied to a sample of teachers in nurseries and primary school. Ann Ig 2019; 31:230–235. [DOI] [PubMed] [Google Scholar]
- 86▪▪.Kwok M, Eslick GD. The impact of vocal and laryngeal pathologies among professional singers: a meta-analysis. J Voice 2019; 33:58–65. [DOI] [PubMed] [Google Scholar]; A must-read systematic review and meta-analysis for all those working with professional singers.
- 87▪▪.Masson ML, de Araújo TM. Protective strategies against dysphonia in teachers: preliminary results comparing voice amplification and 0.9% NaCl nebulization. J Voice 2018; 32:257.e1–257.e10. [DOI] [PubMed] [Google Scholar]; Positive outcome study for prevention programs for teachers.
- 88.Paniagua MS, Pérez CJ, Calle-Alonso F, Salazar C. An acoustic-signal-based preventive program for university lecturers’ vocal health. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 89▪.Pomaville F, Tekerlek K, Radford A. The effectiveness of vocal hygiene education for decreasing at-risk vocal behaviors in vocal performers. J Voice 2019; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]; Positive outcome study for prevention programs for vocal performers.
- 90.Rangarathnam B, Paramby T, McCullough GH. Prologues to a bad voice: effect of vocal hygiene knowledge and training on voice quality following stage performance. J Voice 2018; 32:300–306. [DOI] [PubMed] [Google Scholar]
- 91.Sundram ER, Norsa’Adah B, Mohamad H, et al. The effectiveness of a voice care program among primary school teachers in Northeastern Malaysia. Oman Med J 2019; 34:49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Vainio KL. Unlocking US teachers’ vocal potential by raising awareness about the body-mind interconnectedness in voice pilates training. Eur J Soc Behav Sci 2018; 22:2652–2666. [Google Scholar]
- 93▪.Caffier PP, Nasr AI, Rendon MDM, et al. Common vocal effects and partial glottal vibration in professional nonclassical singers. J Voice 2018; 32:340–346. [DOI] [PubMed] [Google Scholar]; Interesting study on potential implications of vibratory characteristics for vocal health in one singing genre.
- 94.Kaneko M, Sugiyama Y, Mukudai S, Hirano S. Effect of voice therapy using semi-occluded vocal tract exercises in singers and nonsingers with dysphonia. J Voice 2019; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 95.Ouyoung L, Villegas BC, Liu C, et al. Effects of resonance voice therapy on hormone-related vocal disorders in professional singers: a pilot study. clinical medicine insights: ear, nose and throat. Clin Med Insights Ear Nose Throat 2018; 11:1179550618786934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Allen J, Miles A. Walking the thin white line – managing voice in the older adult. Speech Lang Hearing 2019; 22:25–31. [Google Scholar]
- 97.Ziegler A, Hapner ER. Vocal dose in older adults with presbyphonia: an analytic, cross-sectional study. J Voice 2018; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 98.Phyland DJ. The aspiring young singer. In: McMurray JS, Hoffman MR, Braden MN, editors. Multidisciplinary management of pediatric voice and swallowing disorders. 2019. Springer International. [Google Scholar]
- 99.Edwin R. Celebrity pedagogy. J Singing 2018; 75:61–62. [Google Scholar]


