Supplemental Digital Content is available in the text
Keywords: homocysteine, metformin, multivitamin, vitamin B12 deficiency
Abstract
Background:
Metformin can cause serum vitamin B12 deficiency, but studies on the influence of its duration and dose are lacking. We investigated vitamin B12 deficiency in patients with type 2 diabetes using metformin, in conjunction with other related factors.
Method:
This cross-sectional study included 1111 patients with type 2 diabetes who took metformin for at least 6 months. Serum vitamin B12 levels were quantified using a competitive-binding immunoenzymatic assay, and vitamin B12 deficiency was defined as serum B12 <300 pg/mL. Information on metformin use and confounding variables were collected from records or questionnaires and interviews.
Result:
Serum vitamin B12 deficiency occurred in 22.2% of patients (n = 247). After adjusting for confounders, a 1 mg increase in daily metformin dose was associated with a 0.142 pg/mL decrease in vitamin B12 (P < .001). Compared with a daily dose of <1000 mg, the adjusted odds ratios for 1000 to 1500, 1500 to 2000, and ≥2000 mg metformin were 1.72 (P = .080), 3.34 (P < .001), and 8.67 (P < .001), respectively. Vitamin B12 deficiency occurred less often in patients taking multivitamins (odds ratio 0.23; P < .001). After adjusting for confounding factors, there was no correlation between B12 deficiency and duration of metformin use. Serum homocysteine levels showed significant negative correlation with vitamin B12.
Conclusion:
Metformin at ≥1500 mg/d could be a major factor related to vitamin B12 deficiency, whereas concurrent supplementation of multivitamins may potentially protect against the deficiency. Serum homocysteine levels were negatively correlated with vitamin B12 levels, suggesting that B12 deficiency due to metformin use may occur at the tissue level. However, this hypothesis will require further study.
1. Introduction
Metformin as a first-line oral treatment for hyperglycemia in diabetes is generally regarded as having few side effects.[1] However, since Berchtold et al first reported in 1969 that metformin could cause vitamin B12 deficiency by reducing vitamin B12 absorption in the gastrointestinal tract, such findings have been constantly published.[2] It has been reported that an average of 6% to 30% of patients could show vitamin B12 deficiency due to metformin use.[3,4] In addition, some studies have reported that serum vitamin B12 levels were inversely related to the duration and dose of metformin use.[5–8] Since large prospective studies have clarified this relationship recently,[9,10] the 2017 American Diabetes Association treatment guidelines now recommend regular monitoring of vitamin B12 levels in patients with diabetes taking metformin.[11]
Meanwhile, serum vitamin B12 may be an unreliable marker for overall vitamin B12 deficiency because of the variability in measurement methods.[12] Homocysteine is a key component in the one-carbon pathway of methionine metabolism which plays an important role in DNA methylation, and is involved in various intracellular vitamin B12 reactions.[1,13] An increase in homocysteine is known to be related to an increased risk of cardiovascular diseases, cognitive disorders, cancer, chronic kidney disease, and other chronic diseases, and is often caused by vitamin B12 deficiency. Therefore, increased homocysteine levels in patients with serum vitamin B12 deficiency can more accurately predict vitamin B12 deficiency in true tissues.[1,13] Many studies have investigated homocysteine increases in patients taking metformin, but there is still controversy on the conclusions of the studies.[14,15]
Although the clinical significance of metformin-induced vitamin B12 deficiency is controversial, anemia and peripheral nerve damage are typically attributed symptoms.[1,16] If peripheral nerve damage is not adequately treated, diabetic peripheral neuropathy (DPN) may be exacerbated, leading to serious and permanent nerve damage.[17] As such, it is clinically advisable to ensure that B12 deficiency does not develop under metformin treatment.
Comparatively lower amounts of meat are consumed in Asian countries than in Western nations, suggesting a higher risk of vitamin B12 deficiency, but few studies have considered the impact of duration and dose of metformin use in this context. We investigated the prevalence of vitamin B12 deficiency among Korean patients with type 2 diabetes under long-term metformin treatment, and examined how the period and dose of metformin affected B12 deficiency. We further investigated whether metformin-induced B12 deficiency in the serum could indicate tissue deficiency by also measuring serum homocysteine.
2. Method
2.1. Participants
The study protocol conformed to the ethical guidelines of the Declaration of Helsinki and was approved by the institutional review board at Yongin Severance Hospital, Yonsei University College of Medicine, Korea (protocol No. 9-2017-0003), and all participants provided written informed consent. In this cross-sectional study, patients with type 2 diabetes who took metformin for at least 6 months and visited the Yongin Severance Hospital outpatient clinic between June 2017 and April 2018 were considered for enrollment. Patients with a history of gastrectomy, colectomy, inflammatory bowel disease, or pernicious anemia were excluded. We further excluded patients with acute illness characterized as severe infection, cancer or acute coronary syndrome within the last 3 months, as well as serious organ damage characterized by liver cirrhosis, aspartate aminotransferase (AST) or alanine aminotransferase (ALT) ≥3 times the upper limit of the normal range, estimated glomerular filtration rate (GFR) <30 mL/min/1.73 m2, or symptoms of heart failure. Patients with hematological disorders other than anemia, pregnant women, and vegetarian patients were also excluded. Of the 2933 patients with diabetes who visited the outpatient clinic during the study period, 1131 adult patients, who were deemed suitable for the inclusion criteria and agreed to participate in the study, were evaluated again through detailed review of medical records and laboratory tests. In the end, 1111 patients were finally enrolled in the study (Fig. 1). The 1111 patients were between 20 to 85 years of age, with a mean age of 59.5 ± 10.9 years, and 58.1% (645 patients) were male. The mean duration of diabetes was 10.5 ± 6.9 years, and the mean duration of metformin use was 10.1 ± 7.0 years (range of 0.5–45 years), with a mean daily dose of 1339 ± 479 mg.
Figure 1.
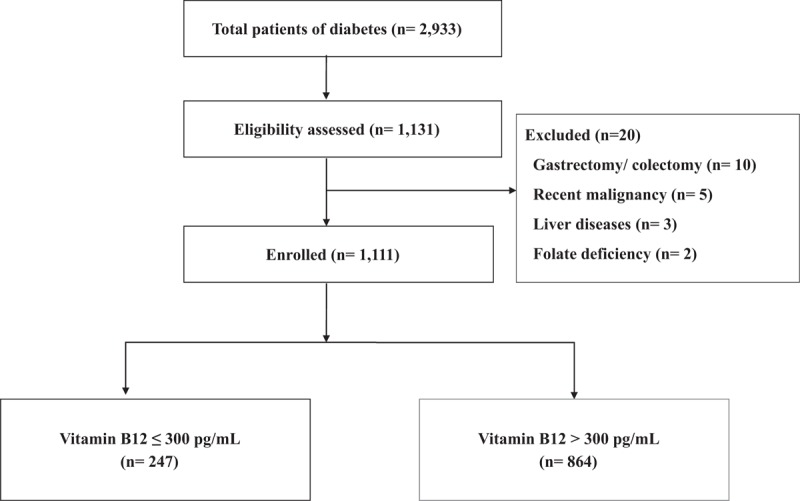
Study flow chart.
2.2. Study methods
Participants underwent basic blood tests at study registration, and also took questionnaires on neuropathy, supplement drug histories, as well as alcohol consumption and smoking habits. The participants’ medical records and past prescriptions were carefully reviewed during the study period by researchers. Blood and urine samples were collected in a fasting state to measure serum vitamin B12, serum folic acid, serum homocysteine, glucose, insulin, glycated hemoglobin (HbA1c), hemoglobin, mean corpuscular volume (MCV), AST, ALT, creatinine, total cholesterol, triglycerides, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and urine albumin-to-creatinine ratios (ACR). Physical examinations of height, weight, and blood pressure were also performed. Hypertension was defined as systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg, or use of any antihypertensive medications. Cardiovascular disease was defined as a history of coronary heart disease, stroke, or peripheral arterial disease confirmed by a specialist. Diabetic retinopathy was noted based on patient records, or in some cases affirmed by a specialist during study registration. Diabetic neuropathy was defined as having been previously diagnosed with DPN, taking relevant medication, or exceeding 2 points in a questionnaire using the Michigan Neuropathy Screening Instrument.[18] Time elapsed since initial diagnosis of diabetes and duration and dose of metformin use were recorded following a review of medical records. If a patient had discontinued metformin use for longer than 6 months, the duration of metformin treatment was counted from when it was resumed. The daily dose of metformin was calculated as the mean dose taken over the last 6 months. Additional drug histories, drinking habits, and smoking habits were collected either from individual questionnaire or from medical records within the last year. Use of multivitamins, calcium supplements, histamine-2 receptor blockers, and proton pump inhibitors was noted if taken continuously for at least 6 months. The average amount of alcohol consumed weekly was calculated, and 98 g per week was used as a guideline threshold limit for moderate drinking.[19]
2.3. Laboratory testing
Vitamin B12 levels were measured by competitive-binding immunoenzymatic assays using an Unicel DxI 800 analyzer (Beckman Coulter, Inc., CA). Assay sensitivity was 50 pg/mL, and inter-assay coefficient of variation was <11.4% at serum concentrations of 88 to 975 pg/mL. In this study, biochemical vitamin B12 deficiency was defined as serum B12 <300 pg/mL, not accompanied by serum folic acid deficiency.[1,20] Based on this distinction, patients were categorized as B12-deficient or normal, and the clinical characteristics of the 2 groups were compared. Serum folic acid deficiency was defined as <4 ng/mL.[1] Anemia was defined as hemoglobin <13 g/dL for men and <12 g/dL for women, based on the World Health Organization guidelines.[21] The homeostasis model of assessment-insulin resistance was calculated using the following equation: fasting glucose (mg/dL) × fasting insulin (μU/mL)/405.[22] Estimated GFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration criteria. Serum homocysteine levels were measured using the chemiluminescent Microparticle Immuno-Assay (Abbott Architec i2000). Elevated homocysteine was defined as >13.7 μmol/L.[8] Albuminuria was defined as urine ACR ≥30 mg/gCr.
2.4. Statistical analysis
SPSS version 23 (IBM, Chicago, IL) was used for statistical analyses. Data are expressed as mean ± standard deviation or frequencies (percentages). Independent t tests for continuous variables and Pearson Chi-squared test for categorical variables were used to compare the vitamin B12 deficiency group and the normal group. Pearson correlation and linear regression analysis were performed to find the linear relationship between the serum vitamin B12 levels and metformin use. Multivariate logistic regression analysis was used to examine the factors related to vitamin B12 deficiency and calculate odds ratios (OR). Area under the curve (AUC) was measured using receiver operator characteristic (ROC) curve analysis, and cut-off values of duration and dose of metformin use were calculated for vitamin B12 deficiency.
3. Results
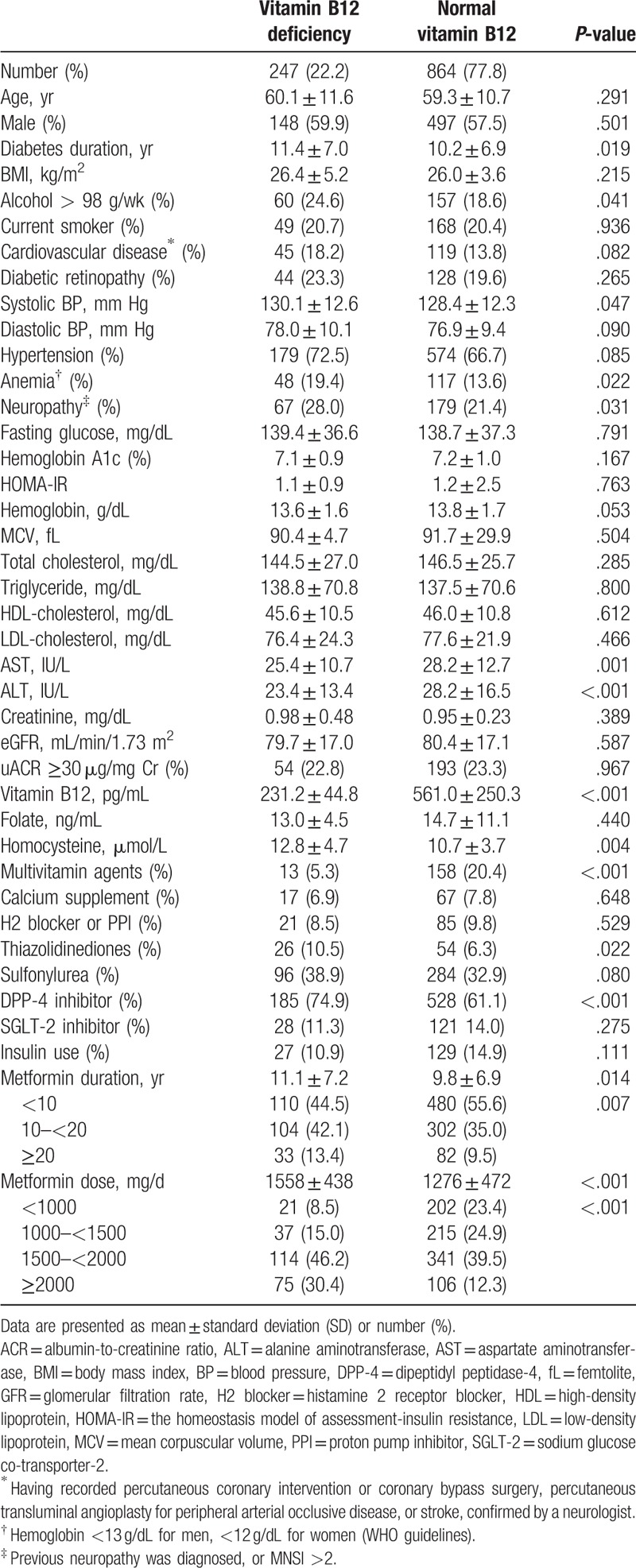
The mean vitamin B12 level in the patient pool was 487.7 ± 260.7 pg/mL. A total of 22.2% (247 patients) showed vitamin B12 deficiency, with a mean vitamin B12 level of 231.2 ± 44.8 pg/mL. In this patient pool, only 1 patient had B12 level <100 pg/mL, and 60 patients (5.4%) had serum B12 levels <200 pg/mL. Their clinical characteristics were compared with the normal-vitamin B12 group (Table 1). Vitamin B12-deficient patients were found to have a longer duration of metformin use (11.1 ± 7.2 years vs 9.8 ± 6.9 years; P = .014) and took a larger dose (1558 ± 438 mg/d vs 1276 ± 472 mg/d; P < .001) than normal patients. Serum homocysteine was found to be significantly greater in the B12-deficient group, at 12.8 ± 4.7 μmol/L versus 10.7 ± 3.7 μmol/L (P = .004). Duration of diabetes, alcohol consumption, anemia, neuropathy, multivitamin supplements (5.3% vs 20.4%; P < .001), systolic blood pressure, AST, ALT, use of dipeptidyl peptidase-4 inhibitors, and use of thiazolidinediones were also significantly different between the 2 groups. There were no differences in age, sex, body mass index, smoking rates, cardiovascular diseases, diabetic retinopathy, fasting glucose, HbA1c, hemoglobin, MCV, lipid profiles, or GFR between the 2 groups.
Table 1.
Clinical characteristics of the study population.
Serum vitamin B12 levels showed a negative correlation with metformin dose (r = −0.300, P < .001), but were not significantly correlated with duration of metformin use (r = 0.030, P = .317), according to Pearson correlation. When daily metformin dose was categorized into 4 groups as <1000, 1000 to 1500, 1500 to 2000, and ≥2000 mg, serum vitamin B12 levels also significantly decreased as metformin dose increased (P < .001; Fig. 2). However, when duration of metformin use was categorized as <10, 10 to 20, and ≥20 years, there was no significant correlation with serum vitamin B12 levels (P = .667). Even after adjusting for multiple confounding factors using linear regression analysis, a 1 mg increase in daily metformin dose was associated with 0.142 pg/mL decrease in vitamin B12 levels (P < .001; Table 2).
Figure 2.
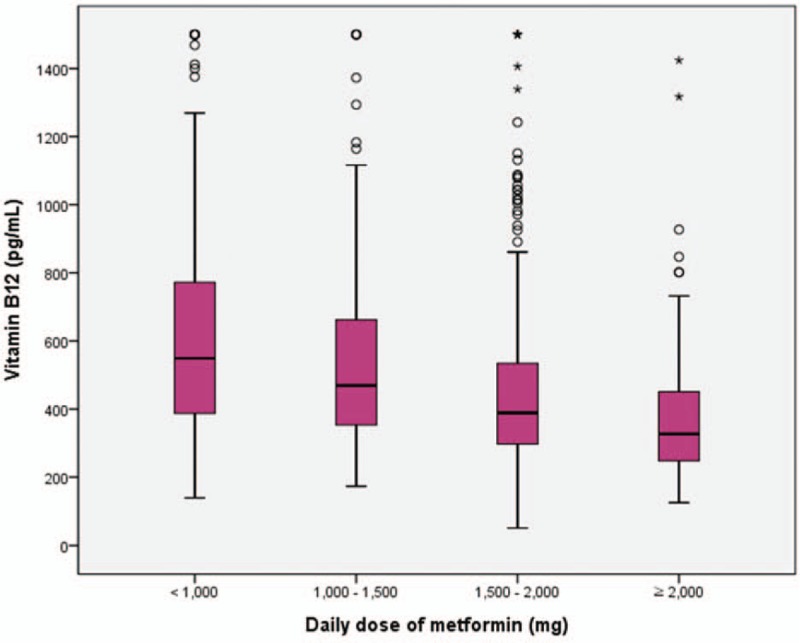
Box plot for serum vitamin B12 level according to different dose of metformin. (P for trend <.001).
Table 2.
Relationship between metformin use and serum vitamin B12 level.
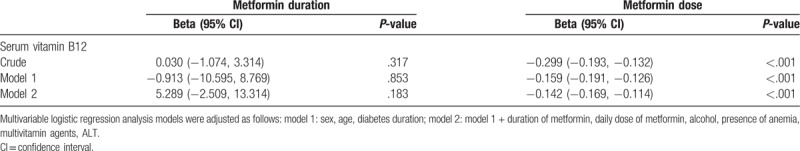
Table 3 identifies the potentially related factors for vitamin B12 deficiency. Age, sex, and other factors found to be significant using univariate logistic regression analysis were then used for multivariate logistic regression analysis. Metformin dose remained the most significant factor related to vitamin B12 deficiency, even after adjusting for age, sex, duration of diabetes, alcohol consumption, anemia, multivitamin supplementation, ALT, and duration of metformin use. The adjusted OR was 3.34 and 8.67 for the 1500 to 2000 mg group and ≥2000 mg group, respectively, compared to the group taking a daily metformin dose <1000 mg. Univariate logistic regression analysis showed that the risk of vitamin B12 deficiency was significantly increased with duration of metformin use, where the 10 to 20 year duration group showed an unadjusted OR of 1.50 (P = .009), and the ≥20 year group showed an unadjusted OR of 1.76 (P = .015) compared to the <10 year group. However, the association was not significant after adjusting for various factors. Other than metformin use, factors influencing vitamin B12 deficiency in patients with type 2 diabetes were alcohol consumption, anemia, multivitamin supplements, and ALT.
Table 3.
Logistic regression for the potentially related factors of vitamin B12 deficiency among patients with type 2 diabetes.
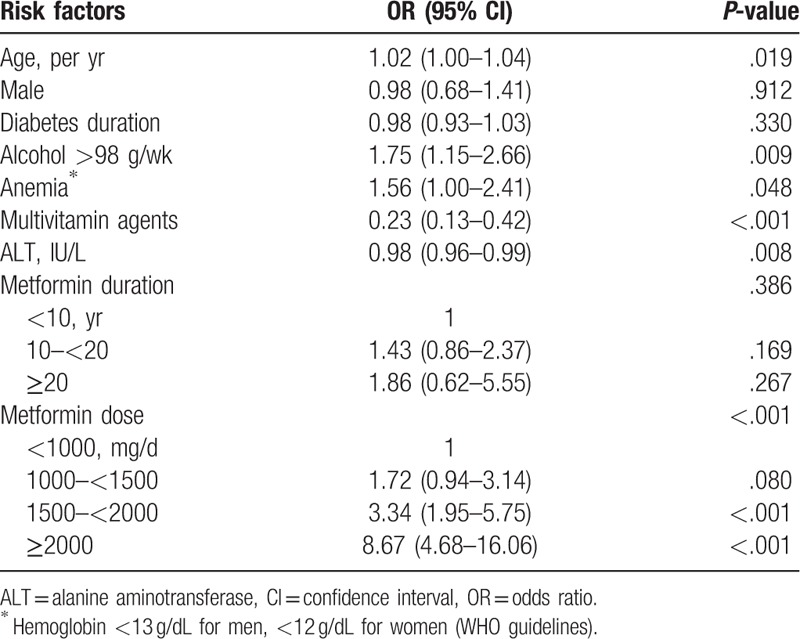
Figure 3 shows the ROC curve for duration and dose of metformin use for vitamin B12 deficiency. AUC for duration of metformin use was 0.56 (95% confidence interval [CI], 0.51–0.60; P = .008), with a cut-off value of 9.5 years (sensitivity 56%, specificity 57%). The AUC for metformin dose was 0.68 (95% CI, 0.64–0.71; P < .001), with a cut-off value of 1425 mg/day (sensitivity 77%, specificity 48%).
Figure 3.
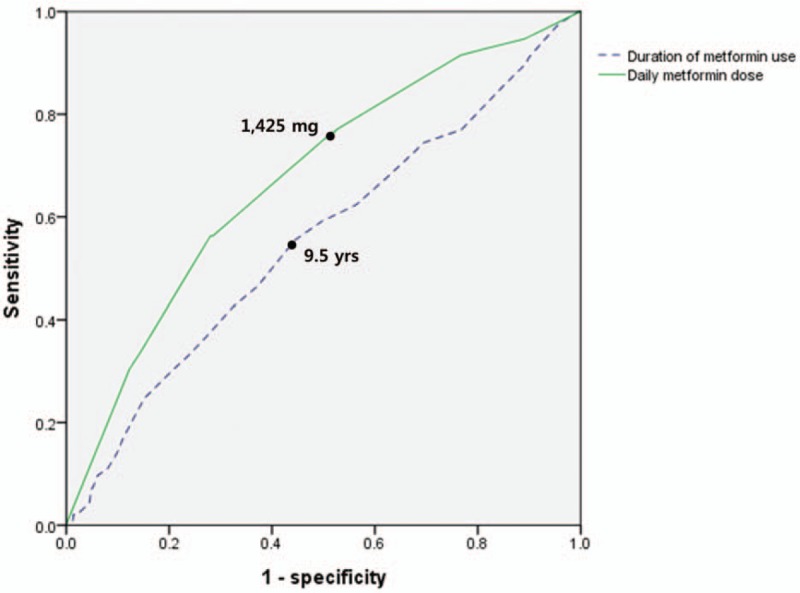
Receiver operator characteristic curve analysis for period of metformin use and daily metformin dose related to vitamin B12 deficiency.
Lastly, we investigated the relationship between serum vitamin B12 levels and homocysteine levels in all patients. In multivariate linear regression analysis, serum vitamin B12 levels showed a significant negative correlation with homocysteine levels even after adjusting for various confounders, such as age, sex, duration of diabetes, alcohol consumption, smoking, anemia, GFR, multivitamin supplementation (beta, −13.140, P = .001). No direct relationship was found between homocysteine levels and the duration or dose of metformin. In the vitamin B12-deficient group, 49% showed elevated homocysteine levels, whereas in the normal group, only 18% showed elevated homocysteine levels. The 121 patients who showed elevated homocysteine levels in vitamin B12-deficient group were separately subjected to baseline characteristics analysis and multivariate logistic regression analysis, assumed as another criterion for vitamin B12 deficiency (Supplemental Tables 1 and 2).
4. Discussion
Our findings indicate a prevalence of vitamin B12 deficiency of 22.2% in patients with type 2 diabetes taking long-term metformin, with larger daily doses significantly associated with vitamin B12 deficiency. Factors other than metformin dose associated with vitamin B12 deficiency were age, alcohol consumption, anemia, multivitamin supplements, and ALT levels. Unexpectedly, the duration of metformin use did not show significant association with vitamin B12 deficiency. Serum homocysteine levels showed a significant negative correlation with serum vitamin B12 levels as well as significant differences between the vitamin B12-deficient and normal groups. In the vitamin B12-deficient group, 49% of patients showed concurrently elevated homocysteine levels, suggesting true tissue deficiency.
The “golden standard” for defining vitamin B12 deficiency is not yet established, since there are various methods for measuring serum vitamin B12, corresponding normal values, and research results. One study reporting lower specificity showed that 60% of patients had symptoms of vitamin B12 deficiency when B12 level was <200 pg/mL, and 90% at <100 pg/mL.[23] In general; however, serum vitamin B12 levels can be interpreted as follows: >300 pg/mL, B12 deficiency is unlikely (probability of 1%–5%); 200 to 300 pg/mL, B12 deficiency possible (probability of 5%–15%); <200 pg/mL, consistent with B12 deficiency (specificity of 90%–100%).[1,20,24] On this basis, biochemical vitamin B12 deficiency was defined as serum B12 <300 pg/mL, not accompanied by serum folic acid deficiency, in this study.[1,20] In other studies, it was recommended that other metabolites, such as homocysteine or methylmalonic acid (MMA), be measured together since it is difficult to define true vitamin B12 deficiency as serum vitamin B12 levels alone.[25,26] If homocysteine and MMA are elevated along with the low vitamin B12 values, it is explained that they have 85% to 98% sensitivities.[20,26] Although MMA values were not measured, serum homocysteine values were measured in this study. Therefore, the definition of vitamin B12 deficiency was secondarily defined as vitamin B12 <300 pg/mL and homocysteine >13.7 μmol/L,[8] and once again analysis was performed. There was no difference in overall results, both when 247 patients with only low serum vitamin B12 levels were defined as vitamin B12 deficiency, and 121 patients with low vitamin B12 and high homocysteine values were defined as vitamin B12 deficiency.
The prevalence of vitamin B12 deficiency after metformin use has been reported to be 6% to 30%, varying with race, standard values of vitamin B12, and metformin usage.[3–10] A large prospective study reported a 20.3% prevalence of vitamin B12 deficiency after 9.5 years of metformin use,[10] and a large dataset provided by the National Health and Nutrition Examination Survey showed a 22% prevalence when vitamin B12 deficiency was defined as levels below 300 pg/mL.[3] A recent study of 799 patients by the College of Medicine of the Catholic University of Korea showed a lower prevalence of vitamin B12 deficiency (9.5%) and higher mean B12 levels (662.5 ± 246.7 pg/mL) than in the present study. The reasons for the difference may include differences in testing methods, differences in alcohol consumption, and differences in the doses of metformin use.[6] Some studies have focused on the impact of the duration and doses of metformin on vitamin B12 deficiency. In the previously mentioned study, both the duration and daily dose of metformin were significantly associated with vitamin B12 deficiency, with cut-off values of 4 years and 1100 mg/d, respectively.[6] In another study, metformin dose had a negative relationship with vitamin B12 levels, and an increase of 1 mg in the daily metformin dose was associated with a 0.042 pg/mL decrease in vitamin B12 levels, but the duration of metformin use did not show significant effects.[5] Similarly, several further studies have reported that daily dose is a more strongly associated with vitamin B12 deficiency than duration.[27,28] Our findings indicate that a 1 mg/d increase in metformin dose decreased vitamin B12 levels by 0.142 pg/mL, but the duration of use did not have significant effects. Altogether, the results of these studies and our study indicate that it is important to account for metformin dose in recommendations for screening for vitamin B12 deficiency, and not just the duration of metformin use.
Vitamin B12 is involved in the activity of methylmalonyl-CoA mutase and the pathway for methionine synthase in cells. Intracellular vitamin B12 deficiency interferes with both of these pathways and increases MMA and homocysteine, which are biochemical indicators of metabolic efficacy.[13,17] Therefore, if a decrease in serum vitamin B12 levels is not accompanied by an increase in MMA and homocysteine levels, this could be interpreted as a simple plasma decrease of vitamin B12 levels, rather than a true tissue deficiency. In fact, some studies have reported that decreases in vitamin B12 after metformin treatment were only plasma decreases, without an increase in homocysteine levels.[29–31] Leung et al suggested that metformin only reducted the level of non-functional plasma B12, the part bound to haptocorrin, and not the active part bound to transcobalamin.[31] According to Greibe's study, plasma vitamin B12 decreased by 22% in rats treated with metformin, whereas the total vitamin B12 in tissues and organs did not decrease, and B12 accumulation in the liver was observed.[29] However, other studies have found that patients taking metformin had decreased vitamin B12 levels as well as increased homocysteine levels, suggesting true tissue deficiency, and a consensus has not yet been reached.[9] In the present study, serum homocysteine levels showed significant negative correlation with serum B12 levels as well as significant differences between the vitamin B12-deficient and normal groups. In addition, 49% of patients in the vitamin B12-deficient group showed concurrently elevated homocysteine levels, whereas in the normal group, only 18% showed elevated homocysteine levels. This result supports the hypothesis that vitamin B12 decreases due to metformin use indicate a decrease at the tissue level. Of course, measurement of additional markers, such as holotranscobalamin, MMA, red blood cell-B12, and plasma concentrations of methylation indices may provide a more comprehensive assessment of true deficiency, but are beyond the scope of this study.[32] A large prospective study measuring more functional markers is needed to ensure support for this hypothesis.
The clinical significance of vitamin B12 deficiency lies in megaloblastic anemia and neuropathy.[1,16,17] In this study, anemia was a significant factor related to B12 deficiency, even after adjusting for other confounders; but in other studies, there were few patients with typical megaloblastic anemia (MCV >100 fL).[6] In all, 13 patients showed MCV >100 fL, and only 1 was vitamin B12-deficient. This may be because various factors, such as age and nutrition, play parts in vitamin B12 deficiency, along with other factors, such as iron deficiency anemia and anemia due to chronic disease. This result is supported by other studies which found that 30% of patients, even those with anemia due to vitamin B12 deficiency, had normal MCVs.[33–35] Since this study followed a cross-sectional design, we cannot judge the causal relationship, but our results indicate vitamin B12 deficiency affected anemia.
Neuropathy due to metformin-induced vitamin B12 deficiency has been studied and reported numerous times, but causal relationships remain unclear. As has been recently reported, vitamin B12 deficiency due to metformin use maybe not related to neuropathy if it is a simple plasma deficiency.[17] Differences in the prevalence of neuropathy between the B12-deficient group and the normal group in this study were statistically significant, but there was no significant relationship between vitamin B12 deficiency and neuropathy after adjusting for various factors. Although it is nearly impossible to clinically distinguish neuropathy caused by vitamin B12 deficiency from diabetic neuropathy, neuropathy should still be closely monitored, since early diagnosis and treatment improve prognosis.[1]
The mechanism by which metformin reduces serum vitamin B12 levels has not been elucidated, but the most likely hypothesis is that metformin interferes with calcium-dependent membrane action responsible for vitamin B12 intrinsic factor absorption in the terminal ileum.[36] Few studies have investigated whether such absorption difficulties caused by metformin could be improved by supplementation of multivitamins, which usually contain small amounts of vitamin B12 at 2 to 30 ug/d. A recent review paper recommended the use of vitamin supplements for patients on long-term metformin treatment to prevent decreases in vitamin B12, albeit without direct evidence.[37] Moreover, a retrospective study showed that among metformin users, multivitamin use was associated with lower prevalence of vitamin B12 deficiency (adjusted OR = 0.14; 95% CI = 0.04, 0.54) compared to those not using multivitamins.[38] However, in most other studies that investigated the supplementation with multivitamins, no significant influence on vitamin B12 deficiency was observed.[3,6,28] In the present study, the mean vitamin B12 level in patients taking multivitamin was 715.1 ± 340.4 pg/mL, and that in patients who did not take multivitamin was 410.8 ± 173.4 pg/mL (P < .001). After adjusting for various confounders, our findings indicate that multivitamin supplementation was significantly associated with lower prevalence of vitamin B12 deficiency and a reduced OR of developing a deficiency. We suggest that results with such a meaningful difference were derived, as the study investigated and compared patients whose records showed that they had regularly consumed vitamin supplements for more than 6 months. However, the lack of a detailed grasp of the vitamin B12 dose contained in multivitamin is one of the major limitations of our study. Further well-designed studies should be conducted to confirm the validity of multivitamin use for preventing B12 deficiency.
The strength of this study lies in the large sample population, especially of Asian people on whom little research has been conducted. We also observed the effect of duration and dose of metformin on vitamin B12 deficiency; moreover, this study examined more related factors (neuropathy symptoms, homocysteine levels, multivitamin use, etc) than did previous studies. We further defined vitamin B12 deficiency as a group with both serum vitamin B deficiency and homocysteine elevation, and compared it to the group lacking only serum vitamin B12 additionally. However, this study had several limitations in addition to a number of aforementioned issues. First, the cross-sectional study approach could not probe the causal relationship between various factors and vitamin B12 deficiency. Second, it is possible that our record was insufficient to capture an accurate representation of patients with a very long period of metformin use, or who had changed their hospital. Therefore, information on the duration of metformin use was dependent on patients’ memories, and the information could have been inaccurate. Third, daily metformin doses were determined by calculating the average of the most recent 6 months, and did not cover the entire duration of metformin use. Because this study was not prospective, there was insufficient information to accurately calculate the cumulative dose during the total period of metformin use. Fourth, animal foods such as meat, fish, and dairy products are rich in vitamin B12. Therefore, to reduce the confounding parameters, patients’ diets should be investigated. However, we could not obtain detailed information on the matter, and only ascertained whether a patient was a vegetarian or not. Lastly, our study relied only on subjective symptoms of the patients for diagnosis of neuropathy, without conducting dedicated neurological examinations that could give objective results; as such, this may have led to an increase in false-negative results.
5. Conclusion
We found that the use of metformin at doses equal to or greater than 1500 mg/d is a major factor related to the development of vitamin B12 deficiency, and that concurrent supplementation of multivitamins may potentially protect against this. Serum homocysteine levels were negatively correlated with vitamin B12 levels, suggesting that the B12 deficiency observed due to use of metformin occurred at the tissue level, but this hypothesis needs further study.
Acknowledgment
The authors thank Editage writers for editing the English text of a draft of this manuscript.
Author contributions
Conceptualization: Jiwoon Kim, Jong Suk Park.
Data curation: Jiwoon Kim.
Formal analysis: Hye Sun Lee.
Investigation: Jiwoon Kim, Jong Suk Park.
Methodology: Jiwoon Kim, Hye Sun Lee, Jong Suk Park.
Resources: Chul Woo Ahn.
Supervision: Chul Woo Ahn, Sungsoon Fang, Jong Suk Park.
Validation: Sungsoon Fang.
Writing – original draft: Jiwoon Kim.
Writing – review and editing: Chul Woo Ahn, Sungsoon Fang, Jong Suk Park.
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: ALT = alanine aminotransferase, AST = aspartate aminotransferase, AUC = area under the curve, CI = confidence interval, DPN = diabetic peripheral neuropathy, GFR = glomerular filtration rate, HbA1c = glycated hemoglobin, MCV = mean corpuscular volume, OR = odds ratio, ROC = receiver operator characteristic.
How to cite this article: Kim J, Ahn CW, Fang S, Lee HS, Park JS. Association between metformin dose and vitamin B12 deficiency in patients with type 2 diabetes. Medicine. 2019;98:46(e17918).
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Mazokopakis EE, Starakis IK. Recommendations for diagnosis and management of metformin-induced vitamin B12 (Cbl) deficiency. Diabetes Res Clin Pract 2012;97:359–67. [DOI] [PubMed] [Google Scholar]
- [2].Berchtold P, Bolli P, Arbenz U, et al. Disturbance of intestinal absorption following metformin therapy (observations on the mode of action of biguanides. Diabetologia 1969;5:405–12. [DOI] [PubMed] [Google Scholar]
- [3].Reinstatler L, Qi YP, Williamson RS, et al. Association of biochemical B(1)(2) deficiency with metformin therapy and vitamin B(1)(2) supplements: the National Health and Nutrition Examination Survey, 1999-2006. Diabetes Care 2012;35:327–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kos E, Liszek MJ, Emanuele MA, et al. Effect of metformin therapy on vitamin D and vitamin B(1)(2) levels in patients with type 2 diabetes mellitus. Endocr Pract 2012;18:179–84. [DOI] [PubMed] [Google Scholar]
- [5].Beulens JW, Hart HE, Kuijs R, et al. Influence of duration and dose of metformin on cobalamin deficiency in type 2 diabetes patients using metformin. Acta Diabetol 2015;52:47–53. [DOI] [PubMed] [Google Scholar]
- [6].Ko SH, Ko SH, Ahn YB, et al. Association of vitamin B12 deficiency and metformin use in patients with type 2 diabetes. J Korean Med Sci 2014;29:965–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Sato Y, Ouchi K, Funase Y, et al. Relationship between metformin use, vitamin B12 deficiency, hyperhomocysteinemia and vascular complications in patients with type 2 diabetes. Endocr J 2013;60:1275–80. [DOI] [PubMed] [Google Scholar]
- [8].Wile DJ, Toth C. Association of metformin, elevated homocysteine, and methylmalonic acid levels and clinically worsened diabetic peripheral neuropathy. Diabetes Care 2010;33:156–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].de Jager J, Kooy A, Lehert P, et al. Long term treatment with metformin in patients with type 2 diabetes and risk of vitamin B-12 deficiency: randomised placebo controlled trial. BMJ 2010;340:c2181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Aroda VR, Edelstein SL, Goldberg RB, et al. Long-term metformin use and vitamin b12 deficiency in the diabetes prevention program outcomes study. J Clin Endocrinol Metab 2016;101:1754–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].American Diabetes Association. Pharmacologic approaches to glycemic treatment. Diabetes Care 2017;40:S64–74. [DOI] [PubMed] [Google Scholar]
- [12].Ahmed MA. Metformin and vitamin B12 deficiency: where do we stand? J Pharm Pharm Sci 2016;19:382–98. [DOI] [PubMed] [Google Scholar]
- [13].Tefferi A, Pruthi RK. The biochemical basis of cobalamin deficiency. Mayo Clin Proc 1994;69:181–6. [DOI] [PubMed] [Google Scholar]
- [14].Carlsen SM, Kjotrod S, Vanky E, et al. Homocysteine levels are unaffected by metformin treatment in both nonpregnant and pregnant women with polycystic ovary syndrome. Acta Obstet Gynecol Scand 2007;86:145–50. [DOI] [PubMed] [Google Scholar]
- [15].Zhang Q, Li S, Li L, et al. Metformin treatment and homocysteine: a systematic review and meta-analysis of randomized controlled trials. Nutrients 2016;8:E798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Andres E, Noel E, Goichot B. Metformin-associated vitamin B12 deficiency. Arch Intern Med 2002;162:2251–2. [DOI] [PubMed] [Google Scholar]
- [17].Ahmed MA, Muntingh GL, Rheeder P. Perspectives on peripheral neuropathy as a consequence of metformin-induced vitamin B12 deficiency in T2DM. Int J Endocrinol 2017;2017:2452853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Feldman EL, Stevens MJ, Thomas PK, et al. A practical two-step quantitative clinical and electrophysiological assessment for the diagnosis and staging of diabetic neuropathy. Diabetes Care 1994;17:1281–9. [DOI] [PubMed] [Google Scholar]
- [19].Diane Publishing, Allen JP, Columbus M. Assessing Alcohol Problems: A Guide for Clinicians and Researchers. 1997. [Google Scholar]
- [20].Snow CF. Laboratory diagnosis of vitamin B12 and folate deficiency: a guide for the primary care physician. Arch Intern Med 1999;159:1289–98. [DOI] [PubMed] [Google Scholar]
- [21].WHO/UNICEF/UNU. Iron deficiency anaemia: assessment, prevention, and control, a guide for programme managers. Geneva: World Health Organization; 2001. [Google Scholar]
- [22].Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–9. [DOI] [PubMed] [Google Scholar]
- [23].Stabler SP, Allen RH, Savage DG, et al. Clinical spectrum and diagnosis of cobalamin deficiency. Blood 1990;76:871–81. [PubMed] [Google Scholar]
- [24].Lindenbaum J, Savage DG, Stabler SP, et al. Diagnosis of cobalamin deficiency: II. Relative sensitivities of serum cobalamin, methylmalonic acid, and total homocysteine concentrations. Am J Hematol 1990;34:99–107. [DOI] [PubMed] [Google Scholar]
- [25].Norman EJ, Morrison JA. Screening elderly populations for cobalamin (vitamin B12) deficiency using the urinary methylmalonic acid assay by gas chromatography mass spectrometry. Am J Med 1993;94:589–94. [DOI] [PubMed] [Google Scholar]
- [26].Savage DG, Lindenbaum J, Stabler SP, et al. Sensitivity of serum methylmalonic acid and total homocysteine determinations for diagnosing cobalamin and folate deficiencies. Am J Med 1994;96:239–46. [DOI] [PubMed] [Google Scholar]
- [27].Ting RZ, Szeto CC, Chan MH, et al. Risk factors of vitamin B(12) deficiency in patients receiving metformin. Arch Intern Med 2006;166:1975–9. [DOI] [PubMed] [Google Scholar]
- [28].de Groot-Kamphuis DM, van Dijk PR, Groenier KH, et al. Vitamin B12 deficiency and the lack of its consequences in type 2 diabetes patients using metformin. Neth J Med 2013;71:386–90. [PubMed] [Google Scholar]
- [29].Greibe E, Trolle B, Bor MV, et al. Metformin lowers serum cobalamin without changing other markers of cobalamin status: a study on women with polycystic ovary syndrome. Nutrients 2013;5:2475–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Greibe E, Miller JW, Foutouhi SH, et al. Metformin increases liver accumulation of vitamin B12 – an experimental study in rats. Biochimie 2013;95:1062–5. [DOI] [PubMed] [Google Scholar]
- [31].Leung S, Mattman A, Snyder F, et al. Metformin induces reductions in plasma cobalamin and haptocorrin bound cobalamin levels in elderly diabetic patients. Clin Biochem 2010;43:759–60. [DOI] [PubMed] [Google Scholar]
- [32].Obeid R, Jung J, Falk J, et al. Serum vitamin B12 not reflecting vitamin B12 status in patients with type 2 diabetes. Biochimie 2013;95:1056–61. [DOI] [PubMed] [Google Scholar]
- [33].Lindenbaum J, Healton EB, Savage DG, et al. Neuropsychiatric disorders caused by cobalamin deficiency in the absence of anemia or macrocytosis. N Engl J Med 1988;318:1720–8. [DOI] [PubMed] [Google Scholar]
- [34].Wickramasinghe SN. Diagnosis of megaloblastic anaemias. Blood Rev 2006;20:299–318. [DOI] [PubMed] [Google Scholar]
- [35].Chan CW, Liu SY, Kho CS, et al. Diagnostic clues to megaloblastic anaemia without macrocytosis. Int J Lab Hematol 2007;29:163–71. [DOI] [PubMed] [Google Scholar]
- [36].Bauman WA, Shaw S, Jayatilleke E, et al. Increased intake of calcium reverses vitamin B12 malabsorption induced by metformin. Diabetes Care 2000;23:1227–31. [DOI] [PubMed] [Google Scholar]
- [37].Valdes-Ramos R, Guadarrama-Lopez AL, Martinez-Carrillo BE, et al. Vitamins and type 2 diabetes mellitus. Endocr Metab Immune Disord Drug Targets 2015;15:54–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Kancherla V, Garn JV, Zakai NA, et al. Multivitamin use and serum vitamin B12 concentrations in older-adult metformin users in REGARDS, 2003–2007. PLoS One 2016;11:e0160802. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


