Abstract
To analyze the factors that affecting the help-seeking behavior of bipolar disorder (BD) patients by conducting interviews BD individuals in Hunan province of China.
In 2015, 72,999 people from 123 counties of Hunan province of China were interviewed through multistage stratified random sampling. Twelve items of general health questionnaire (GHQ-12) and abnormal behavioral clue questionnaire were used as screening tools. The Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) (SCID) was used as a diagnostic tool.
Among the 75 BD patients, 36% (27/75) sought help. Compared with help-seekers, non-help-seekers were more likely to be older, divorced, or widowed, mostly illiterate or elementary education, family monthly income at least 3000 ¥, more physically consulted in the past year, able to effective work or study, at a stable illness status. 70.4% help-seekers firstly sought help from a medical institution. The main reasons that patients did not seek help were economic problem, did not know where to seek help, unsatisfied with medical services, afraid of mental health stigma, and other problems, such as traffic inconvenience.
Non-help-seekers were faced with more difficulties in their social functions and social interactions.
Keywords: bipolar disorder, help-seeking behavior, social functions, stigma
1. Introduction
Bipolar disorder (BD), as one of the most severe psychiatric disorders in worldwide, is a chronic disease characterized by changes in mood, energy, and activity and brings burden on socioeconomic development and health care system.[1] The duration of untreated BD is associated with more mood episodes, more suicidal behavior, and a trend towards greater lifetime mood instability.[2] Even between mood episodes, its residual symptoms may disturb circadian cycles, emotional regulations, cognitive functions, psychiatric disorders, and comorbidities.[3–5] The high misdiagnose rate of BD has already become a widespread problem, and it has reached to 36.2% in Africa.[5] In addition, lifetime prevalence of anxiety disorders in BD individuals was 45%.[6] Therefore, it requires to find better diagnosis methods and more appropriate therapeutic strategies for BD patients.
Help-seekers, the key factor in treatment for BD individuals, are referred to people who have been diagnosed with mental disorders and seek help from other professionals. They are divided into 2 groups, drug-receivers who take medication and non-drug-receivers who refuse to take any medication. In Western, it has reported that barriers were mainly related to accessibility and acceptability of health services,[7] as well as the social distance between physicians and patients.[8] Many mental health workers even have set anti-stigma campaigns to decrease stigmatization. However, in China, traditional views have become a major barrier to help-seeking, due to they feel shame and embarrassment when individuals with mental health disorder visiting doctors, or their problems are known by dwellers in their communities. Furthermore, due to lack of mental health institutes and workers, patients cannot be performed with mental health service, especially in the vast rural China.
In this research, the key factors that might affect help-seeking behavior among BD individuals, such as age, sex, living alone, marital and employment status, education level, physical hospitalization, and others, were investigated in Hunan Province of China. Furthermore, we explored the reasons associated with non-help-seeking and key factors with non-drug-receivers. These findings on the help-seeking behavior among BD patients would have great implications on future interventions for BD patients in China.
2. Method
2.1. Sampling method
A cluster sampling method was implemented in 3 stages. Firstly, 123 cities and counties were randomly chosen in Hunan Province of China, then 1 street and 1 town were randomly chosen in each city and county, thus 123 streets and 123 towns were selected. Secondly, in each street and village, 1 neighborhood committee and 1 village were randomly chosen. Thirdly, 150 families in each neighborhood committee and village were randomly selected in 123 neighborhood committees and 123 villages. Finally, a total of 74,370 participants (>15 years old) were selected.
2.2. Training for interview team
This study was approved by the Ethics Committee of Hunan Brain Hospital (2014–01). The written informed consent was obtained from all participants. The interview teams consisted of 2 groups of people. In step 1, the psychiatrists were workers from Centers for Disease Control (CDC) of Hunan Province, Brains Hospital of Hunan Province, and mental health centers in every city and county. They were well trained for basic psychiatry and consistency on every questionnaire in step 1, ensuring they would complete the interview under the unified standard. In step 2, psychiatrists received training programs held by Xiangya Second Hospital and Brains Hospital of Hunan Province. Only those who passed the final tests could become researchers in this study. All researchers received professional training for the interview protocol, administration of the questionnaire, and consistency in using the Chinese version of the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorder (SCID).
2.3. Instruments and recoded measurements
The study was implemented in 2 steps (Fig. 1).
Figure 1.
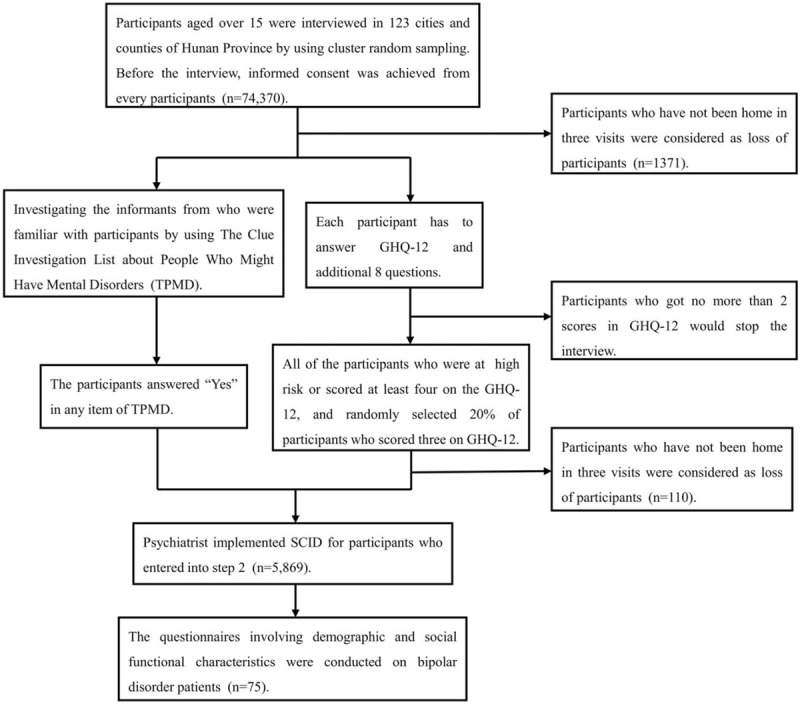
Sample flowchart in this study.
2.3.1. Step 1. Screening
All participant were asked to evaluate their health condition by answering the General Health Questionnaire (GHQ-12), which has been proven to have great validity and reliability as a screening tool for common psychiatric disorders.[9] Furthermore, 8 additional questions were also added to GHQ-12 questionnaire. Two items (choices ranged from “excellent” to “worst”): how they considered their physical and mental health condition. Three items (the choices listed from “never” to “always”): whether they have thought of something repeatedly in the past month; whether they were afraid of being restricted their activity in the past month; and whether they had been extremely anxious or nervous in the past 6 months. Three items (“Yes” or “No”): whether they were in trouble due to a drinking problem; whether they were hospitalized or had sought help due to psychiatric or mental disorders. Anyone who chose “worst,” “always,” or “Yes” would be considered at high risk.
Another questionnaire called the Clue Investigation List about People Who Might Have Mental Disorders (TPMD) was also involved in the step 1. This questionnaire was published by Beijing Ministry of Health Bureau of Disease Prevention and Control, and has been proven to be great valid and reliable in China.[10] Informants (parents, spouse, children, friends, or neighborhood members) who were familiar with participants were asked to answer the 11 questions as follows: once lived in a mental health center, but now at home; locked at home due to mental health disorders; displayed agitation, incomprehensible or unrealistic speech, such as announcing that they could have conversations with invisible people or had supernatural powers; exhibited babbling or violence toward to others without specific reason or due to drinking; talked to himself or herself, laughed without reason, or exhibited a dull or bizarre expression; oddly behaved in public places, such as wearing clothes in abnormal way or wearing no clothes on purpose; extremely skeptical, such as wondering if people around were discussing him/her privately, or plotting to kill him/her; was overly talkative, hyperactive, or officious; was overly quiet or indolent, showing no passion, or spending all day in bed; committed suicide or attempted to hurt oneself; did not go to school, work, or have contact with anyone. The choices were between “Yes” and “No.”
The participants who met the following criteria entered into step 2: scored at least 4 in GHQ-12; considered to be at high risk; the informants answered “Yes” in any item of TPMD. Furthermore, 20% of people who scored 3 on the GHQ-12 would be randomly selected into step 2. Therefore, there were in total of 5869 (5869/72,999, 8.04%) participants entered into step 2.
2.3.2. Step 2. In-depth interview
In this study, the Chinese version of the SCID,[11] that provided by the Department of Psychiatry of Kaohsiung Medical University in Taiwan, was used to generate diagnoses for all participants who entered into step 2. Diagnoses were performed by psychiatrists from the research teams after interviews with participants and their informants. Except 110 participants who could not be contacted in 3 different visits, 5869 participants were interviewed with the SCID. Lastly, 75 (0.10%) participants were diagnosed with BD, and were interviewed with the following questionnaires. Two informants, who were familiar with patients, answered questions instead of those patients who could not answer by themselves. Thus, the 75 participants were divided into help-seekers and non-help-seekers.
Living condition was dichotomized as “Living in city (1)” and “Living in county (0)”; “Living alone (1),” and “Not living alone (0).” Marital status was dichotomized as “currently married (1)” and “currently unmarried (0),” the former included people who were married, remarried, or cohabitated, while the latter were those who were single, separated, divorced, or widowed. Smoking/alcohol drinking was measured by asking whether they had habits of smoking and/or alcohol drinking, and the results were dichotomized as “having smoking/drinking problem (1)” and “not having smoking/drinking problem (0).” Employment status was dichotomized as “currently employed (1)” and “currently unemployed (0),” the former included workers, businessmen, housewives, and students, while the latter were those who were laid off, retired, in pregnancy leave, sick leave or disability. Education level was dichotomized as “Illiteracy and/or elementary school (1)” and “At least junior high school (0).” Health condition was measured by asking them whether they have suffered from any chronic physical disease, such as cardiovascular disease, respiratory disease, and others. The results were dichotomized as “having chronic physical disease (1)” and “Not having physical disease (0).” They also have to answer whether they have been physically hospitalized in the past year (Yes, [1] or No [0]). Medical insurance was dichotomized as “Having medical insurance (1)” and “Not having medical insurance (0).” Monthly family income and annual expenses on inpatients were dichotomized as “Below 3000 ¥ (1)” and “At least 3000 ¥ (2),” and the expenses on outpatient each year in Chinese RMB (¥) were dichotomized as “Below 600 ¥ (1)” and “At least 600 ¥ (2).”
BD patients were asked the social function characteristics, such as whether they had committed any illegal acts, including theft, robbery, violence, or murder. They also had to answer: whether they could work or study, and solve problems by themselves or others; whether they had any physical illness and social problems due to alcohol drinking, any social interactions with other people, any dangerous behavior including verbal threatening, screaming, smashing things without reason, hurting oneself, or committing suicide. The answers for these questions were “Yes (1)” or “No (0).” Furthermore, they were also asked whether their mental health condition was better than before, and the answer was dichotomized as “Being better than before (0)” or “No changes/even worse (1).” Their current stage of illness was dichotomized as “Being at stable stage of illness (0)” or “Being at unstable stage of illness (1).”
Help-seekers were asked several questions about the specific details of how they sought help. For example, they were asked: whether they would be hospitalized or receive any drug therapy if necessary, and the answers were dichotomized as “Yes (1)” or “No (0)”; what kind of help they would seek, with choices among “institutes related to mental health services,” “non-psychiatric departments in general hospital,” “community health department,” and “others including relatives or friends.”
As for the non-help-seekers, 11 possible reasons of not seeking help were listed: solving problems by oneself (1) versus not by oneself (0); not knowing (1) versus knowing (0) where to seek help; encountering (1) versus not encountering (0) other problems such as traffic inconvenience; costing too much time (1) versus not costing too much time (0) to visit doctors; too much expenses (1) versus not too much expenses (0); treatment is not working (1) versus working (0); afraid of (1) versus not afraid of others’ judging (0); afraid of (1) versus not afraid of coercive hospitalization (0); not satisfied (1) versus satisfied with medical services (0); afraid of (1) versus not afraid of mental health stigma (0); not necessary (1) versus necessary to receive treatment (0). Any participants could select more than one reason.
2.4. Statistical analysis
Statistical Product and Service Solutions (SPSS) for Windows (version 18.0, SPSS Inc, IBM, Armonk, NY, USA) was used for data analysis. t-Test or Chi-square test was used to compare differences on continuous or categorical variables across groups. Bivariate correlation analysis was used to explore the factors that were positively or negatively related to reasons for the non-help-seekers. In addition, logistic regression analysis was performed to examine factors related to help-seekers and non-help-seekers, as well as drug-therapy-receivers and non-drug-therapy-receivers. All of the factors were chosen as independent variables. All tests were two-tailed and a P < .05 was considered statistically significant.
3. Results
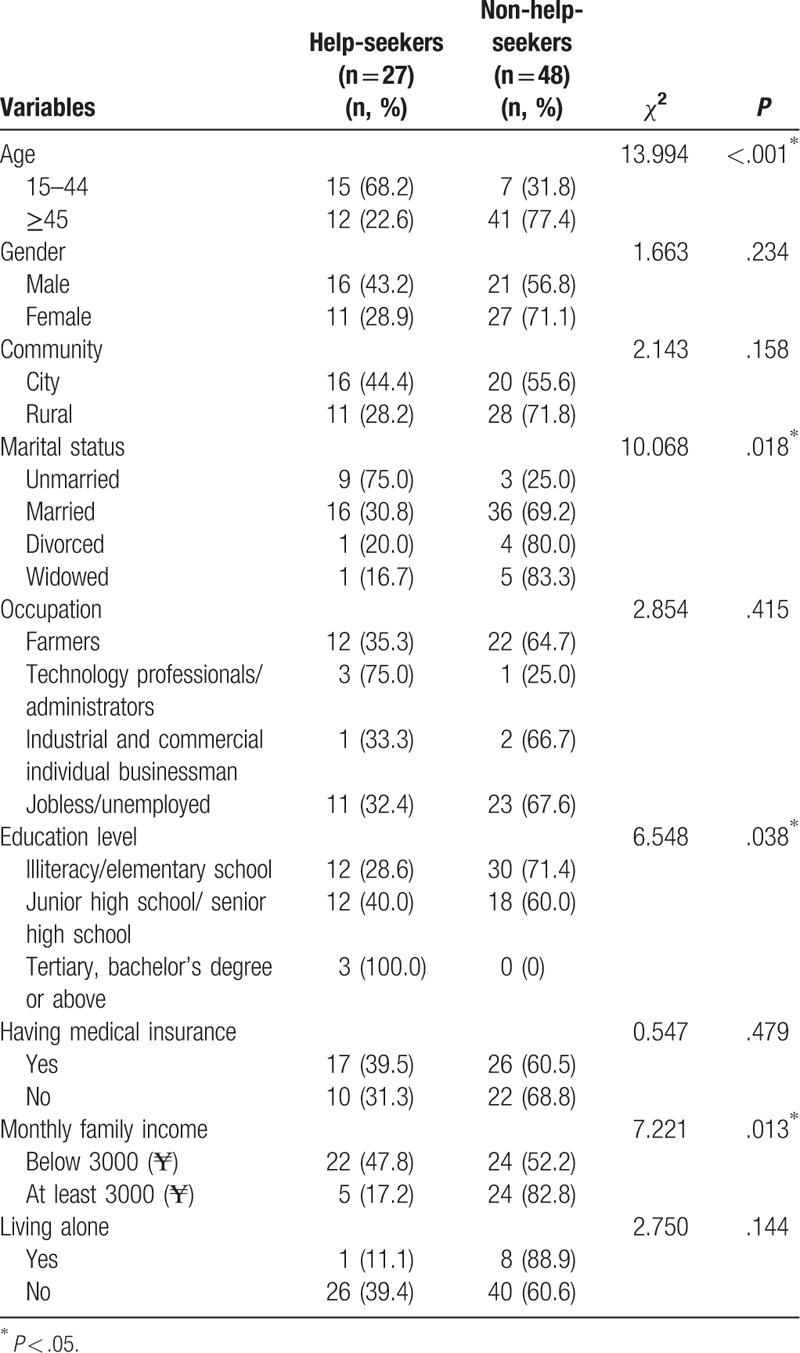
As Fig. 1 shown, a total of 75 (0.10%, 75/72,999) participants, including 37 men and 38 women and aged 53.57 ± 14.11 years, were finally diagnosed with BD. Among them, 27 participants (36%) sought help from others, while 48 participants (64%) did not seek any help. In addition, 36 participants (48.00%) lived in a city, 52 (69.33%) were currently married, 34 participants (45.33%) were farmers, 34 participants (45.33%) were unemployed, 42 participants (56%) were illiterate or only graduated from elementary school, 46 patients’ (61.33%) monthly family income was lower than 3000 ¥, and 43 participants (57.33%) had medical insurance. There were statistically significant differences in terms of age, marital status, education level, and monthly family income between help-seekers and non-help-seekers. Compared with the help-seekers, non-help-seekers were significantly older, divorced or widowed, illiteracy or elementary school cultural level, monthly family income at least 3000 ¥ (Table 1).
Table 1.
Demographic of samples (N = 75): help-seekers and non-help-seekers with bipolar disorder.
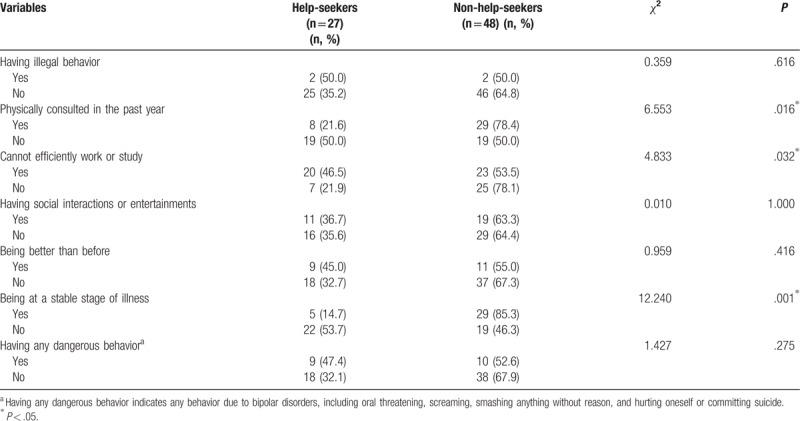
As for social functions, 37 participants (49.33%) consulted physical problem, 43 participants (57.33%) could not efficiently work or study, only 30 participants (40%) had social interactions or entertainment, and 34 participants (45.33%) were at a stable stage of illness, 19 participants (25.33%) had committed dangerous behavior, and 4 participants (5.33%) had illegal behavior. Compared with help-seekers, the non-help-seekers were inclined to efficiently work or study, higher cost of physically consulted in the past year, more likely to not changing/even worse mental health and being at an unstable stage of illness (Table 2).
Table 2.
Social functions of samples (N = 75): help-seekers and non-help-seekers with bipolar disorder.
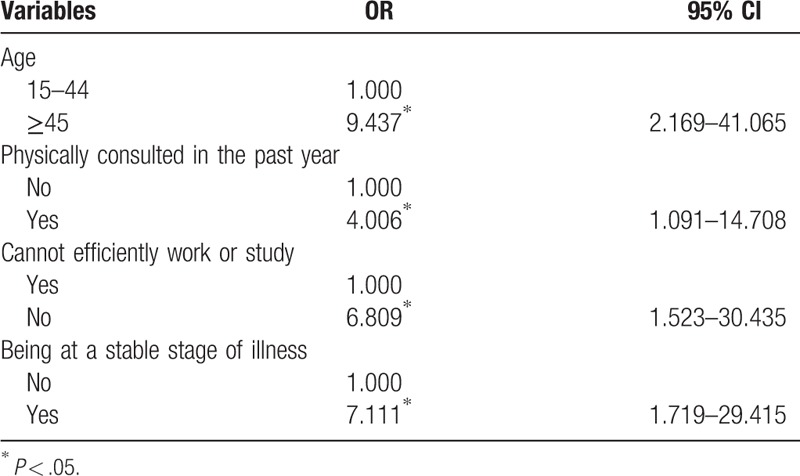
The Table 3 showed the univariate analysis of the influence of help-seeking behavior in BD patients. In addition, a multiple logistic regression model was applied to further explore the reasons that why these patients did not seek help. The single factors that concluded by univariate analysis, including age, marriage, nearly 1 year of medical treatment due to physical diseases, average monthly family income, inability to effectively work and study, disease stage, emotional polarity, and possibly influential covariates between urban and rural occupations, were included in the multivariate analysis. The results showed that being older (odds ratio [OR] = 9.437, 95% confidence interval [CI] = 2.169–41.065), more physically consulted in the past year (OR = 4.006, 95% CI = 1.091–14.708), efficiently work or study (OR = 6.809, 95% CI = 1.523–30.435), and being at a stable stage of illness (OR = 7.111, 95% CI = 1.719–29.415) were risk factors for non-help-seeker (Table 4).
Table 3.
Univariate analysis of the influence of help-seeking behavior in patients with bipolar disorder.
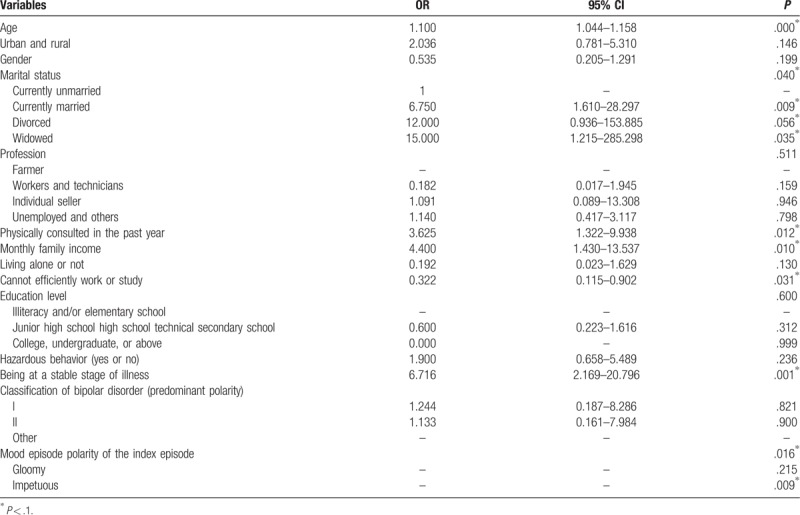
Table 4.
Logistic regressions of risk factors for those bipolar disorder patients who do not seek help (Method: Forward).
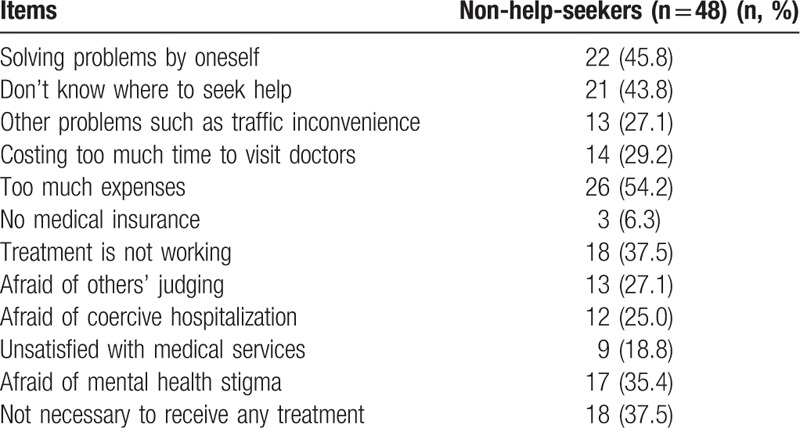
In terms of 27 (36%) BD help-seekers, 6 cases choose general hospital as their help-seeking places, 13 cases choose psychiatry hospital, and 5 cases sought help from relatives or friends. In addition, only 12 cases choose to visit the outpatient department, 7 cases choose to be hospitalized (Table 5). The reasons why patients did not seek help were multiple choice topic. The findings suggested that the reasons of non-help-seekers were as following: 54.2% of them worried about costing too much money when visiting doctors; 45.8% of them choose want to solve problems by oneself; 43.8% of them to choose don’t know where to seek help; 37.5% of them think that they does not need to be treated; 35.4% of them afraid of mental health stigma, and 6.3% of them had no medical insurance (Table 6).
Table 5.
First way to ask for help among help-seekers with bipolar disorder (n = 27).
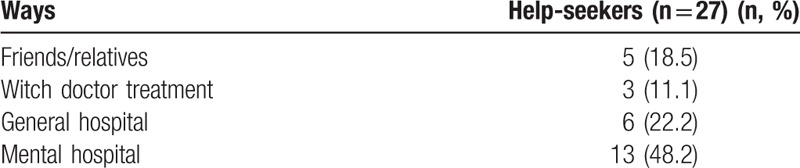
Table 6.
Reasons for non-help-seekers with bipolar disorder (n = 48).
4. Discussion
Many early warning signs of BD, such as sleep deprivation, mania or depression, are easily overlooked by patients and their relatives, which is severely insufficient among Chinese people. In Japan, Koichi et al[12] found the following factors may be positively related to early help-seeking behavior, recognition of early warning signs, consultation with non-professional and professional people, consulting with public mental health workers, and living with family. All above reminding that recognition of warning signs are significant for help-seekers in China and Japan. Therefore, self-awareness of disorders may be improved by accessing to mental health workers, including psychiatrist, public mental health workers, and psychotherapist.
In this study, we found non-help-seekers tend to be older, which may be a potential risk factor. Previously, Webb et al[13] and Coppens et al[14] reported that elders in Western countries had social distance and negative attitudes toward to seeking professional help if they with mentally ill. For Chinese elders, lacking of knowledge about psychiatry and non-psychiatric health care providers difficult identifying psychiatric symptoms should be the most reasons for delaying help-seeking behavior. In addition, prejudice towards mental disease and being ignored or negatively treated by family members were also important barrier factors.[15] These findings demonstrate that older patients should be given more attention and advocated more knowledge about psychiatry when access to mental health services. At the same time, non-psychiatric health care providers may also learn more about how to detect psychiatric symptoms among elders.
An epidemiological research discovered that the social function of non-help-seekers was statistically worse than that in help-seekers according to the Global Assessment of Functioning (GAF).[16] In Western countries, BD may be associated with the highest total number of lost work days and productivity reducing.[17,18] These reminded us the work efficiency and social contact of non-help-seekers could be worse than that of help-seekers, and they might easily be neglect. Even though they could continue to work or study, the low efficiency probable inversely affect the productivity or economic development. What is worse, due to being at an unstable stage of illness, their dangerous acts, such as defacing public facilities or hurting/killing people out of anger, would put public safety at greater risk.
In this study, several possible reasons were found that may explain why BD patients did not seek help. It was more likely to believe that visiting doctors were time-consuming for patients living in county, which might due to unavailable mental health related institutes and professionals. According to a study, the patients lived in rural China no >30 km to mental health related institutes were more inclined to visit doctors.[19] While in Western countries, family practitioners prescribing the same medication as psychiatrists or internal physicians would provide primary care for patients living far away from institutes.[20] However, in China, similar measures could also be taken to solve this problem. The general practitioners working should be promoted to learn more about mental health literacy and psychiatric medication in rural China.
For help-seekers who refuse to receive drug therapy, living in county and being physically hospitalized in the past year were risk factors. In addition, the large expense of medication was another significant reason for poor medication adherence in China, due to psychotropic substances are too expensive for people living in county. In Western countries, they favored psychotherapy instead of medication,[21] and personal stigma was significantly and negatively associated with medication application.[22] Another study also indicated that better medication adherence was associated with greater use of treatment services and positive attitudes of mental health workers.[23] This evidence also illustrates the significance of improving medical insurance system for Chinese mentally ill patients and lessening stigma of mental health workers abroad.
Patients with higher monthly family income would not seek help due to they were afraid of others’ judging or so-called “mental health stigma,” and believed it was not necessary to receive any treatment. Within China, monthly family income will somehow represent the social status, the higher monthly family income, and the higher status in a certain community. In current study, stigma of any psychiatric diagnosis would prevent higher social status patients to seek help from any mental health related institutes. Yang et al[24] have discovered that patients of urban China labeled with “psychiatric diagnosis” and “help-seeking” would engender the greatest social distance, and even prior personal contact could not decrease community stigma. For western individuals, internalized stigma still is a pervasive problem and barrier to seeking help for mentally ill people, especially for patients with suicidal behavior.[25,26] Furthermore, stigma and social relationships dissatisfaction appeared to be risk factors for social isolation of individuals with schizophrenia and mood disorders,[27] which might explain why they refused to seek help. These evidences indicated that for mentally ill patients should be taken lessening stigma measures, especially for patients with higher monthly family income. In addition, non-help-seekers with higher social status were afraid of coercive hospitalization in our study, which may due to unfavorable atmosphere in hospitals and fearing of health workers’ hostilities. Swartz et al[28] discovered that individuals suffering from schizophrenia, fearing of coercive hospitalization were positively related to barriers to seeking help. The findings indicated that mental health workers should improve the understanding of patients and their caregivers about the significance of hospitalization.
Non-help-seekers with physically hospitalization in the past year or chronic physical illness tended to be unsatisfied with medical services, which may due to poor patient–doctor relationships and the stigma of health care workers. Some Western studies reported that mentally ill patients’ perception of participation in the decision process and medication adherence depends on good patient–doctor relationships.[29,30] According to the reports from Canada and Texas, physicians’ “often unintentional stigma” or “inadvertent stigma” in the primary care remains a major barrier to quality care, treatment and recovery, resulting in higher mortality rates of mental patients than average.[31,32] To fight against such stigma among primary care physicians and health workers, Jouet et al[33] have conducted a research about an anti-stigma campaign involving physicians and psychiatric patients. After exchanging their points of view with each other, stigma among physicians was effectively lessened. This action can also be implemented in China to decrease the stigma of Chinese physicians and increase the number of help-seekers.
Non-help-seekers who lived alone inclined to solving problems by themselves, worrying about as traffic inconvenience, too much expenses, others’ judging and coercive hospitalization and other problems. In rural China, especially solitary elders, have lower family income and no companion, resulting in lower quality of life and loss of family support. Thus, they are susceptible to suffering from mental disorders. Mentally ill patients lived alone still had negative attitude toward seeking professional help.[14]
This research had some limitations. Firstly, the control groups were not included, such as help-seekers with schizophrenia, major depressive disorder, or without any mental disorders. Secondly, the samples were confined to Hunan Province in China, and further research could be done in different provinces within China or even across different cultures. Finally, intervention and psycho-education for non-help-seekers could be done in follow-up research. In conclusion, non-help-seekers were faced with more difficulties in their social functions and social interactions. Therefore, additional measures, such as lessening mental health stigma and increasing the number of mental health workers and access to mental health services, should be urgently taken.
Acknowledgments
The authors are grateful for the researchers and psychiatrists for their involvement in data collection.
Author contributions
Conceptualization: Xiaosong Li.
Data curation: Lihong Tan.
Formal analysis: Xuhui Zhou.
Investigation: Xiaosong Li.
Methodology: Jing Ma.
Software: Yan Chen.
Validation: Huiying Wang.
Visualization: Jing Guo.
Writing – original draft: Dongxin Wang.
Writing – review & editing: Xuejun Liu.
Footnotes
Abbreviations: BD = bipolar disorder, CDC = Centers for Disease Control, DSM-IV = Diagnostic and Statistical Manual of Mental Disorders-IV, GAF = global assessment of functioning, GHQ-12 = 12 items of general health questionnaire, SCID = Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders-IV, SPSS = Statistical Product and Service Solutions, TPMD = the Clue Investigation List about People Who Might Have Mental Disorders.
How to cite this article: Wang D, Ma J, Tan L, Chen Y, Zhou X, Wang H, Guo J, Li X, Liu X. Characteristics of help-seeking behavior among bipolar disorder patients. Medicine. 2019;98:46(e17687).
XL and XL have equally contributed to this paper and thus shared the co-corresponding authorship.
This study was supported by the Application Research of collaborative network construction for clinical research on mental disorders (NO. 2015BAI13B02) and the Major Special Projects of Hunan Province (NO. S2018GCZCZX0036).
The authors have no conflicts of interest to disclose.
References
- [1].Abdul Pari AA, Simon J, Wolstenholme J, et al. Economic evaluations in bipolar disorder: a systematic review and critical appraisal. Bipolar Disord 2014;16:557–82. [DOI] [PubMed] [Google Scholar]
- [2].Drancourt N, Etain B, Lajnef M, et al. Duration of untreated bipolar disorder: missed opportunities on the long road to optimal treatment. Acta Psychiatr Scand 2013;127:136–44. [DOI] [PubMed] [Google Scholar]
- [3].Abreu T, Braganca M. The bipolarity of light and dark: a review on Bipolar Disorder and circadian cycles. J Affective Disord 2015;185:219–29. [DOI] [PubMed] [Google Scholar]
- [4].Costa Lda S, Alencar AP, Nascimento Neto PJ, et al. Risk factors for suicide in bipolar disorder: a systematic review. J Affect Disord 2015;170:237–54. [DOI] [PubMed] [Google Scholar]
- [5].Vannucchi G, Masi G, Toni C, et al. Bipolar disorder in adults with Aspergers Syndrome: a systematic review. J Affect Disord 2014;168:151–60. [DOI] [PubMed] [Google Scholar]
- [6].Pavlova B, Perlis RH, Alda M, et al. Lifetime prevalence of anxiety disorders in people with bipolar disorder: a systematic review and meta-analysis. Lancet Psychiatry 2015;2:710–7. [DOI] [PubMed] [Google Scholar]
- [7].Umubyeyi A, Mogren I, Ntaganira J, et al. Help-seeking behaviours, barriers to care and self-efficacy for seeking mental health care: a population-based study in Rwanda. Soc Psychiatry Psychiatr Epidemiol 2016;51:81–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Corrigan PW, Mittal D, Reaves CM, et al. Mental health stigma and primary health care decisions. Psychiatry Res 2014;218:35–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Gelaye B, Tadesse MG, Lohsoonthorn V, et al. Psychometric properties and factor structure of the General Health Questionnaire as a screening tool for anxiety and depressive symptoms in a multi-national study of young adults. J Affect Disord 2015;187:197–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Control Tmohbodpa. Severe mental disorder treatment management specification. Beijing Ministry of Health Bureau of Disease Prevention And Control; 2012. [Google Scholar]
- [11].Lyu J, Zhang J. Characteristics of schizophrenia suicides compared with suicides by other diagnosed psychiatric disorders and those without a psychiatric disorder. Schizophr Res 2014;155:59–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Koichi R, Miyamoto Y, Akiyama M, et al. Awareness of early warning signs and help-seeking behaviours among patients with schizophrenia who utilize social rehabilitation facilities in Japan. J Psychiatr Ment Health Nurs 2009;16:694–702. [DOI] [PubMed] [Google Scholar]
- [13].Webb AK, Jacobs-Lawson JM, Waddell EL. Older adults’ perceptions of mentally ill older adults. Aging Ment Health 2009;13:838–46. [DOI] [PubMed] [Google Scholar]
- [14].Coppens E, Van Audenhove C, Scheerder G, et al. Public attitudes toward depression and help-seeking in four European countries baseline survey prior to the OSPI-Europe intervention. J Affect Disord 2013;150:320–9. [DOI] [PubMed] [Google Scholar]
- [15].Ly Y, Li Z, Han M, et al. Reasons for delay in seeking for mental health care among Chinese elderly people with depressive disorder. Chinese Nurs Manag 2015;15:433–6. [Google Scholar]
- [16].Kondo N, Sakai M, Kuroda Y, et al. General condition of hikikomori (prolonged social withdrawal) in Japan: psychiatric diagnosis and outcome in mental health welfare centres. Int J Soc Psychiatry 2013;59:79–86. [DOI] [PubMed] [Google Scholar]
- [17].de Graaf R, Tuithof M, van Dorsselaer S, et al. Comparing the effects on work performance of mental and physical disorders. Soc Psychiatry Psychiatr Epidemiol 2012;47:1873–83. [DOI] [PubMed] [Google Scholar]
- [18].Kafali N, Cook B, Wang S, et al. Impact of mental disorders on employment and receipt of public assistance: an instrumental variables approach. J Mental Health Policy Econ 2015;18:137–45. [PubMed] [Google Scholar]
- [19].Zhang QW, Xiao SY, Zhou L, et al. Treatment status and related factors among patients with schizophrenia in a rural Chinses community. Chinese Mental Health J 2010;24:241–9. [Google Scholar]
- [20].Harman JS, Veazie PJ, Lyness JM. Primary care physician office visits for depression by older Americans. J Gen Internal Med 2006;21:926–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Riedel-Heller SG, Matschinger H, Angermeyer MC. Mental disorders–who and what might help? Help-seeking and treatment preferences of the lay public. Soc Psychiatry Psychiatr Epidemiol 2005;40:167–74. [DOI] [PubMed] [Google Scholar]
- [22].Eisenberg D, Downs MF, Golberstein E, et al. Stigma and help seeking for mental health among college students. Med Care Res Rev 2009;66:522–41. [DOI] [PubMed] [Google Scholar]
- [23].Robertson AG, Swanson JW, Van Dorn RA, et al. Treatment participation and medication adherence: effects on criminal justice costs of persons with mental illness. Psychiatr Serv 2014;65:1189–91. [DOI] [PubMed] [Google Scholar]
- [24].Yang LH, Lo G, WonPat-Borja AJ, et al. Effects of labeling and interpersonal contact upon attitudes towards schizophrenia: implications for reducing mental illness stigma in urban China. Soc Psychiatry Psychiatr Epidemiol 2012;47:1459–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Reynders A, Kerkhof AJ, Molenberghs G, et al. Help-seeking, stigma and attitudes of people with and without a suicidal past. A comparison between a low and a high suicide rate country. J Affect Disord 2015;178:5–11. [DOI] [PubMed] [Google Scholar]
- [26].Tanskanen S, Morant N, Hinton M, et al. Service user and carer experiences of seeking help for a first episode of psychosis: a UK qualitative study. BMC Psychiatry 2011;11:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Oliveira SE, Esteves F, Carvalho H. Clinical profiles of stigma experiences, self-esteem and social relationships among people with schizophrenia, depressive, and bipolar disorders. Psychiatry Res 2015;229:167–73. [DOI] [PubMed] [Google Scholar]
- [28].Swartz MS, Swanson JW, Hannon MJ. Does fear of coercion keep people away from mental health treatment? Evidence from a survey of persons with schizophrenia and mental health professionals. Behav Sci Law 2003;21:459–72. [DOI] [PubMed] [Google Scholar]
- [29].Loos S, Neumann P, Arnold K, et al. [Shared decision-making in the treatment of people with severe mental illness: a focus group study]. Psychiatr Prax 2013;40:23–9. [DOI] [PubMed] [Google Scholar]
- [30].Jaeger S, Weisshaupt S, Flammer E, et al. Control beliefs, therapeutic relationship, and adherence in schizophrenia outpatients: a cross-sectional study. Am J Health Behav 2014;38:914–23. [DOI] [PubMed] [Google Scholar]
- [31].Pellegrini C. Mental illness stigma in health care settings a barrier to care. CMAJ 2014;186:E17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Baker SE, Pearson RM, Glenn JE. Inadvertent stigmatization of mental disorders in a primary care setting. Texas Med 2015;111:66–70. [PubMed] [Google Scholar]
- [33].Jouet E, Moineville M, Favriel S, et al. [A mental health awareness anti-stigma program including user-trainers has a significant impact on knowledge, beliefs and attitudes of job centre professionals in Paris]. Encephale 2014;40:136–42. [DOI] [PubMed] [Google Scholar]


