Abstract
Studies examining the impact of food insecurity on metabolic markers are limited, specifically in Hispanic youth. This study was a cross-sectional analysis of 218 3rd-5th grade students (83% Hispanic and 49% male). Anthropometrics, blood glucose, insulin, and lipids via fasting blood draw, dietary intake via Block screener, and a 5-item food security scale were collected. HOMA-Insulin Resistance was calculated. Multivariate analyses of covariance were used to examine differences in glucose and insulin indices, adiposity, metabolic and dietary intake variables between categories of food security. Food secure children had greater glycemic control and decreased insulin resistance compared to food insecure children.
Keywords: Glycemic Control, Hispanic/Latino, Food Security, Child, Insulin Resistance
Background
Hispanics represent the nation’s largest ethnic minority comprising 17.6% of the total population and are the fastest growing minority.1 This quickly growing population is disproportionally affected by poverty and food insecurity and is at increased risk for being obesity and developing type 2 diabetes.2–4 Childhood obesity has both immediate and long-term effects on health and well-being. Research has shown that children and adolescents who are obese are likely to be obese as adults.5,6 In 2011–2012, Hispanic children and adolescents had a higher prevalence of obesity (22.4%) compared to non-Hispanic blacks and non-Hispanic white children and adolescents (20.2% and 14.1%, respectively).7 Overweight and obese children and adolescents are at a greater risk of being diagnosed with impaired glucose tolerance, insulin resistance, and T2D.8 The prevalence of children diagnosed with T2D has increased over the past decade with children diagnosed with the disease earlier in their lives.9,10 A Hispanic male born in 2000, has a greater lifetime risk of developing T2D compared to a non-Hispanic white male (45.4% vs. 26.7%).11 Similarly, a Hispanic female also has a greater lifetime risk compared to a non-Hispanic white female (52.5% vs. 31.2%). There is an urgent need to better understanding food insecurity and its effects within this population to lessen the burden of health disparities.
The United States Department of Agriculture (USDA) defines food insecurity as “the limited or uncertain availability of nutritionally adequate and safe foods or limited or uncertain ability to acquire acceptable foods in socially acceptable ways.”12 Four labels are used by the USDA to describe ranges of food security: high food security, marginal food security, low food security, and very low food security. The first two labels describe food security, whereas, the later two describe food insecurity.
While 110.9 million (87.7%) United States (U.S.) households were food secure in 2016, nearly 15.6 million households (12.3%) were food insecure and 6.1 million households (4.9%) experienced very low food security.13 Hispanic households with children are disproportionally affected by food insecurity and have higher rates of food insecurity compared to the national average (11.6% versus 8.0%, respectively).13 Public health programs, federal food assistance programs, and policies are in place to alleviate food insecurity; however, their continued funding and appropriations depend on research highlighting their effectiveness. Further research is needed into the relationship between metabolic disease development and food insecurity to help effectively direct the public health efforts.
Insulin resistance in children can result from both genetic and environmental factors, and is most commonly associated with obesity.14 Hispanic children compared to non-Hispanic whites have greater fasting and post-challenge insulin levels and greater insulin resistance, even when controlling for adiposity.15–18 Limited research exists that focuses the association between insulin resistance and environmental influences such as food insecurity. Parker et al. found that adolescents from very low food secure households were more likely to have abnormal glucose levels compared to adolescents from food secure households; however, no other measures of glycemic control were assessed.19 Studies examining the impact of food insecurity on metabolic markers are limited, specifically in Hispanic youth populations.
The literature has consistently found that food insecurity in children is associated increased risks of anemia20,21, asthma22, aggression and anxiety23, behavioral and cognitive problems23–25, depression26, obesity27,28, oral health problems29, sedentary behaviors30, and overall higher odds of fair or poor health31 compared with their food secure peers. The purpose of this research was to assess the relationship of food insecurity with adiposity, metabolic parameters and dietary intake among a sample of low-income Hispanic/Latino children living in Los Angeles, California. The hypothesis was that Hispanic/Latino children who were food insecure would have lower diet quality, higher weight/adiposity parameters, and elevated metabolic risk compared to their food secure counterparts.
Methods
LA Sprouts
LA Sprouts was a 12-week nutrition, cooking, and gardening intervention targeting obesity reduction in Hispanic/Latino children. Elementary schools were chosen for inclusion in the intervention if they: 1) offered the after-school program “LA’s Best”32, 2) had a student body population with ≥75% Latino, 3) had ≥75% of students participating in the Los Angeles Unified School District (LAUSD) free lunch program, and 4) were within 10 miles of University of Southern California (USC) Health Science Campus, 5) had expressed interest by the school principal and staff in having a school garden/hosting a gardening program, and 6) could make an administrative commitment. Four schools were chosen. A full description of the LA Sprouts intervention design, selection of schools, and primary study results are provided elsewhere.33–35 For this analysis only baseline LA Sprouts data was used. This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Institutional Review Boards of University of Southern California, the University of California Los Angeles, the University of Texas at Austin, Loma Linda University and Los Angeles Unified School District. Written informed consent was obtained from all subject’s parents, and assent from subjects was obtained.
Participants
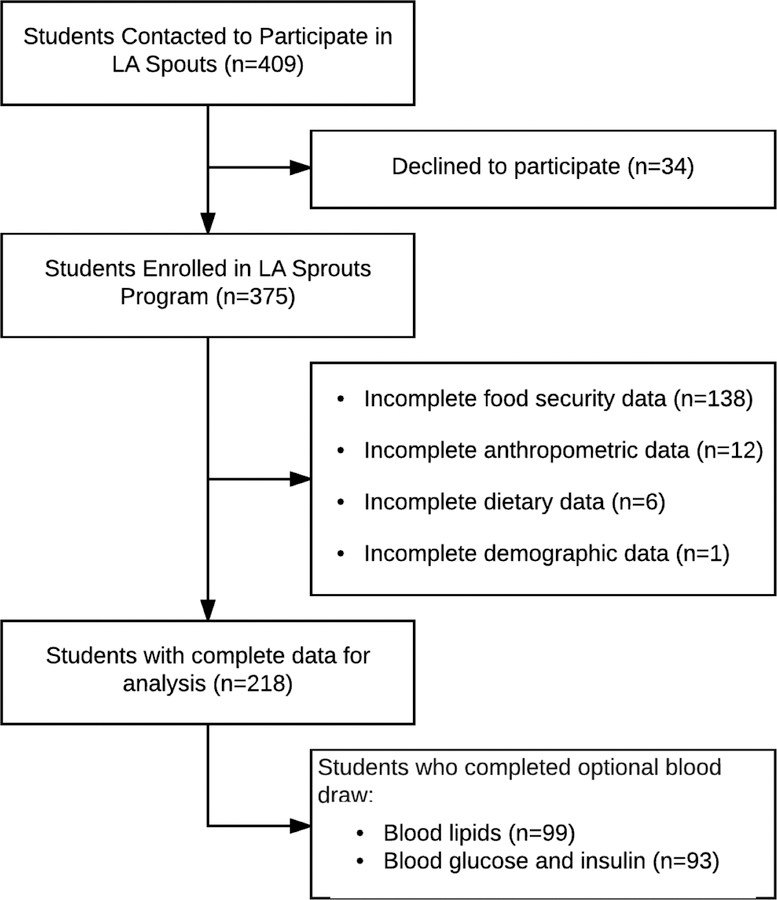
Between 2011 and 2013, all students (n=409) enrolled in LA’s Best after school program at the four participating schools in Los Angeles were contacted to participate in LA Sprouts. Three hundred and seventy five students (92%) agreed to participate. Questionnaire items on food security were added during the second wave of the study, and were collected for 218 students (58%). There were no significant differences among demographic characteristics between waves one and two of the study. An optional fasting blood sample was collected from 99 students (45%). (Figure 1) There were also no statistical demographic differences between children who participated in the fasting blood sample and those who did not.
Figure 1:
Flow of participants for cross-sectional analysis
Anthropometrics and Adiposity
Height was measured with a free-standing stadiometer (Seca, Birmingham, UK) and weight and percent body fat via bioelectrical impedance (Tanita TBF 300A, Arlington Heights, IL, USA). BMI z-scores and corresponding percentiles were determined using Centers for Disease Control and Prevention (CDC) cut-points for age and sex.36 Blood pressure was measured with an automated monitor with appropriate child cuffs (Omron, Schaumberg, IL, USA). Waist circumference was measured using NHANES protocol.37
Child Questionnaire
The questionnaire included items on demographics, socioeconomic status, dietary intake, and food security. Dietary intake was assessed using the Block Kids Food Screener (“Last Week” version). This 41-item screener was developed and adapted from the Block Kids 2004 FFQ (NutritionQuest, Berkeley, CA, USA) and is validated in metropolitan area youth.38 The screener allows for dietary data to be derived into variables reflecting nutrient, specific foods and beverages, and food and beverage group estimates. Dietary variables were grouped by the following food groupings for analysis (meat, poultry, and fish; dairy, whole grains, fruit, vegetables, legumes, French fries, sugar sweetened beverages). French fries were selected as a grouping to differentiate non-fried vegetable consumption from fried vegetable consumption. A bilingual translator was available if students had difficulties reading questionnaire items.
Measurement and Classification of Food Security
Child self-report rather than parent report of child-level food security was used because studies by Fram et al. 2011 and Bernal et al. 2012 have shown that children are aware cognitively, emotionally, and physically of their food insecurity experiences, and are usually in a better position to accurately and reliably report about those experiences.39–41 Further, Fram et al. 2013 found that parent-report of child food insecurity status can result in missing nearly half of children who report themselves as food insecure.40
Child food security experiences were measured using an adaption of the 5-item Child Food Security Assessment (CFSA), which was previously validated for use with children as young as 7 years.30,40 A 5-item scale was used to reduce respondent burden.40 The CFSA was adapted to provide a reference frame of “in the last three months” to match data collection time points of the study. One emotional subdomain item “worry about how hard it is for parents to get enough food” included in the CFSA was removed and replaced with an initiation subdomain item “I tried not to eat a lot so that our food would last”. This change in items was done to include an additional subdomain of child food security experiences. The adapted questionnaire items and response categories are listed in Table 1. The adapted items represent four of six previously conceptualized subdomains of child food insecurity (Q1, emotional awareness; Q2-Q3, physical awareness; Q4, initiation of child food management strategies; Q5, cognitive awareness).41
Table 1.
Food Security Child Questionnaire
| Have these things happened to you in the past 3 months at home with your family? | Yes, many times | Yes, one or two times | No, never |
|---|---|---|---|
| 1. I worried about not having enough to eat | ◯ | ◯ | ◯ |
| 2. I felt hungry because there was not enough food to eat | ◯ | ◯ | ◯ |
| 3. I got really tired because there was not enough food to eat | ◯ | ◯ | ◯ |
| 4. I tried not to eat a lot so that our food would last | ◯ | ◯ | ◯ |
| 5. We couldn’t get the food we wanted because there wasn’t enough money | ◯ | ◯ | ◯ |
The adapted scale was evaluated for agreement in a separate cohort of 166 3rd-5th graders that are part of a baseline data collection for a larger intervention in Fall 2016. Food security classification of the adapted scale compared to the 9-item USDA Self-Administered Food Security Survey Module for Youth42 showed strong agreement (Spearman Correlation rs= 0.52). Additionally, 65 subjects in the above subsample completed the scale an average of 2.7 days later. The scale showed strong test-retest reliability with percent agreement between time 1 and time 2 exceeding 81%.
All participants included in the final analysis had complete food security questionnaire data with no blank or missing responses. Responses to items were coded as follows: 1= Yes, many times; 2= Yes, one or two times; or 3= No, never. A sum of responses was calculated for each student, with higher scores indicative of higher food security. This method of summation is similar to that of the method used with the 9-item USDA Self-Administered Food Security Survey Module for Youth.42 Due to a low number of participants in the high food security category, the USDA’s categories of high food security and marginal food security were collapsed to form one “food secure” category and due to a low number of students in the very low food security category, the categories of very low were collapsed to form one “food insecure” category. The resulting sum was categorized into food insecure (sum 1–10) or food secure (sum of 11–15).
Fasting Blood Samples
An optional fasting blood sample was collected from participants off-campus in the morning before school or on weekends by bilingual, licensed phlebotomists with experience drawing blood in overweight children. Children that elected to participate were asked to not drink or eat anything aside from water, after 8pm the night prior. As an incentive for participation, children received $15 for completing the blood draw. Samples were processed and stored at USC until they were delivered to the Ritchey Lab at USC (glucose and insulin) and the Gower Lab at the University of Alabama (lipids) for analysis. Glucose was assayed using a Yellow Springs Instruments analyzer (Yellow Springs, OH, USA). Total cholesterol, high-density lipoprotein cholesterol (HDL) and triglyceride levels were measured using enzymatic methods on a Stanbio Sirrus analyzer (Stanbio Laboratory, Boerne, TX, USA); low-density lipoprotein (LDL) was calculated using the Friedewald equation.43 Insulin was quantified using an ELISA kit (EMD Millipore, St. Charles, MO, USA). Homeostatic model assessment of insulin resistance (HOMA-IR) was calculated as a measure of insulin resistance at the baseline according to the method described by Matthews et al44. Low HOMA-IR values indicate high insulin sensitivity, whereas high HOMA-IR values indicate low insulin sensitivity (insulin resistance).
Statistical Analysis
Original data was checked to resolve possible measurement errors for participants with standardized residuals >|3|. If errors could not be corrected, it was concluded that the observation was an outlier, and the observation was removed from analyses as described previously.33–35 All variables were examined for normality and data transformations were attempted, but changes were not substantial. Thus, this analysis used the original untransformed data. Given many health outcomes were highly correlated, multivariate analyses of covariance (MANCOVA) were used to examine differences in glucose and insulin indices, adiposity, metabolic and dietary intake variables (dependent variables) between categories of food security (independent variable). The following a priori covariates were included in all models: age (months, continuous), sex, school, and ethnicity (Hispanic/Latino versus non-Hispanic/Latino). BMI percentile (continuous) was an additional covariate in the glucose and insulin indices model, and energy intake (kcal/d) was an additional covariate in the glucose and insulin indices, macronutrient, and food group models. All data was analyzed using SPSS Statistics for Macintosh, Version 24.0 (IBM Corp, Armonk, NY) and an alpha level of p=0.05 was used for significance.
Results
The average sum of responses for the food security questions for food insecure individuals was 8.5 ±1.5 (minimum sum: 5; maximum sum: 10) and the average for food secure individuals was 13.1 ±1.5 (minimum sum: 11; maximum sum: 15). The average sum of responses for both groups was 11.7 ±2.7 (minimum sum: 5; maximum sum: 15). Student characteristics by food-secure or –insecure are shown in Table 2. Compared to food insecure children, food secure children were older and were more likely to be female. MANCOVAs results for differences in adiposity, metabolic parameters and dietary intake between food security groups are presented in Table 3. Food secure children compared to food insecure children had 2.4% lower glucose values (89.9 ±5.9 vs. 92.1 ±6.1mg/dL (5.0 ±0.3 vs. 5.1 ±0.3 mmol/L); p=0.03), 16.6% lower insulin values (8.9 ±7.3 vs. 10.5 ±7.2μU/mL (61.8 ±50.7 vs. 72.9 ±50.0pmol/L); p=0.04) and 17.4% lower HOMA-IR values (2.0 ±1.7 vs. 2.4 ±1.6; p=0.04). Food insecure children had greater insulin resistance compared to their food secure counterparts. Food secure children also had 22.7% lower intakes of French fries (2.0 ±1.3 vs. 2.5 ±1.4 freq.; p=0.04). Food security was not associated with any adiposity measures, lipids, or other dietary variables.
Table 2.
Baseline demographic characteristics of between food secure and food insecure participants
| All Study Participants |
|||||
|---|---|---|---|---|---|
| Characteristic | Food Secure (n=143) | Food Insecure (n=75) | P Valuea | ||
| Mean | SD | Mean | SD | ||
| Age (years) | 9.3 | 0.9 | 8.9 | 0.8 | 0.02* |
| n | % | n | % | ||
| Sex | <0.00* | ||||
| Male | 58 | (40.6%) | 49 | (65.3%) | |
| Female | 85 | (59.4%) | 26 | (34.7%) | |
| Race/ethnicity | 0.70 | ||||
| Hispanic or Latino | 117 | (81.8%) | 64 | (85.3%) | |
| Non-Hispanic or Latinob | 26 | (18.2%) | 11 | (14.7) | |
| Body Mass Index (BMI) | |||||
| Normal Weight (<85th Percentile) | 66 | (46.2%) | 31 | (41.3%) | 0.30 |
| Overweight or Obese (≥85th Percentile) | 77 | (53.8%) | 44 | (52.4%) | 0.31 |
| Socioeconomic Factors | |||||
| No English Spoken at Home | 33 | (23.1%) | 21 | (28.0%) | 0.67 |
| No Computer at Home | 39 | (27.2%) | 22 | (29.3%) | 0.78 |
| Mother Doesn’t Own a Car | 52 | (36.3%) | 19 | (25.3%) | 0.07 |
| Eligible for Free Lunch at School | 131 | (91.6%) | 63 | (84.0%) | 0.07 |
P values were calculated using t tests (for continuous variables) and χ2 tests (for categorical variables)
Non-Hispanic White, Non-Hispanic Black, Asian or Pacific Islanders, American Indian or Native American, or parents are from two different ethnicities
Mean values were significantly different between groups: P<0.05
Table 3.
Differences in adiposity, metabolic parameters, and dietary intake between groups based on food security classification
| Variable | Food Secure | Food Insecure | F Value | P Value | ||
|---|---|---|---|---|---|---|
| (Mean) | (SD) | (Mean) | (SD) | |||
| Adipositya (n=218) | n=143 | n=75 | ||||
| Waist Circumference, cm | 70.49 | 10.86 | 72.17 | 12.24 | 2.65 | 0.11 |
| Body Fat (%) | 24.84 | 8.70 | 25.92 | 9.66 | 0.75 | 0.39 |
| BMI z-score | 0.96 | 0.96 | 1.21 | 1.04 | 1.75 | 0.19 |
| BMI percentile | 75.98 | 24.96 | 80.56 | 24.09 | 0.96 | 0.33 |
| Glucose and Insulin Indicesb (n=93) | n=56 | n=37 | ||||
| Glucose (mg/dL)d | 89.86 | 5.93 | 92.08 | 6.11 | 4.66 | 0.03* |
| Insulin (μU/mL)e | 8.85 | 7.31 | 10.45 | 7.23 | 4.21 | 0.04* |
| HOMA-IR | 1.99 | 1.69 | 2.37 | 1.64 | 4.39 | 0.04* |
| Lipidsa (n=99) | n=60 | n=39 | ||||
| Total Cholesterol (mg/dL)f | 151.25 | 24.64 | 159.79 | 34.96 | 1.78 | 0.19 |
| LDL-C (mg/dL)f | 82.03 | 21.98 | 86.14 | 29.58 | 0.36 | 0.55 |
| HDL-C (mg/dL)f | 55.98 | 10.67 | 58.51 | 12.09 | 1.80 | 0.18 |
| Triglycerides (mg/dL)g | 66.20 | 27.71 | 75.69 | 33.14 | 2.26 | 0.14 |
| Macronutrientsc (n=218) | n=143 | n=75 | ||||
| Protein, g/d | 54.91 | 55.30 | 64.77 | 57.58 | 0.26 | 0.61 |
| Carbohydrates, g/d | 148.99 | 134.27 | 169.48 | 122.38 | 0.02 | 0.88 |
| Fat, g/d | 53.38 | 54.87 | 62.06 | 54.48 | 0.23 | 0.63 |
| Saturated Fat, g/d | 18.77 | 18.97 | 21.36 | 18.91 | 1.02 | 0.31 |
| Dietary Fiber, g/d | 11.92 | 10.76 | 13.77 | 11.19 | 0.22 | 0.64 |
| Sugar, g/d | 75.40 | 64.28 | 82.43 | 59.06 | 0.01 | 0.91 |
| Added Sugar, tsp/d | 7.36 | 8.40 | 8.12 | 7.10 | 0.62 | 0.43 |
| Food Groupsc (n=218) | n=143 | n=75 | ||||
| Meat, Poultry, and Fish, OE | 2.83 | 3.40 | 3.63 | 4.20 | 1.33 | 0.25 |
| Dairy, CE | 1.37 | 1.15 | 1.50 | 1.16 | 0.01 | 0.92 |
| Whole Grains, OE | 0.52 | 0.59 | 0.59 | 0.66 | 0.68 | 0.41 |
| Fruit, CE | 1.40 | 1.29 | 1.41 | 1.26 | 0.17 | 0.68 |
| Vegetables, CE | 0.87 | 0.90 | 1.07 | 0.98 | 3.18 | 0.08 |
| French Fries, freq | 1.95 | 1.29 | 2.45 | 1.37 | 4.52 | 0.04* |
| Legumes, CE | 0.12 | 0.20 | 0.17 | 0.24 | 0.35 | 0.56 |
| Sugar Sweetened Beverages, freq | 0.19 | 0.27 | 0.20 | 0.29 | 0.06 | 0.81 |
Abbreviations: G, grams; D, day; Tsp, teaspoon; TBS, tablespoon; CE, cup equivalent; OE, ounce equivalent; Freq, frequency; BMI, Body Mass Index; HOMA-IR, Homeostatic model assessment for insulin resistance
Covariates: age (months), sex, school, and ethnicity/race
Covariates: age (months), sex, school, ethnicity/race, kcal, and BMI percentile
Covariates: age (months), sex, school, ethnicity/race, and kcal
To convert mg/dL glucose to mmol/L, multiply mg/dL glucose by 0.0555. To convert mmol/L glucose to mg/dL, multiply mmol/L by 18.0. Glucose of 89.86 mg/dL = 4.99mmol/L.
To convert μU/mL insulin to pmol/L, multiply μU/mL insulin by 6.945. To convert pmol/L insulin to μU/mL, multiply pmol/L by 6.95. Insulin of 8.85 μU/mL = 61.46 pmol/L.
To convert mg/dL cholesterol to mmol/L, multiply mg/dL by 0.0259. To convert mmol/L cholesterol to mg/dL, multiply mmol/L by 38.6. Cholesterol of 151.25 mg/dL = 3.92 mmol/L.
To convert mg/dL triglycerides to mmol/L, multiply mg/dL by 0.0113. To convert mmol/L triglyceride to mg/dL, multiply mmol/L by 88.6. Triglyceride of 66.20 mg/dL = 0.75 mmol/L.
Mean values were significantly different between groups: P<0.05
Discussion
To our knowledge, this is the first study to find an association between child self-reported food insecurity and lower glycemic control in Hispanic/Latino children. This study found that food secure children compared to food insecure children had lower glucose and insulin values and lower insulin resistance. Intakes of French fries were found to be higher in food insecure children compared to their food secure peers. Food security was not associated with adiposity measures, blood lipids, or other dietary variables. While the glucose and insulin values for food secure and food insecure children were within normal ranges, children who reported being food insecure had mean values that were closer to pre-diabetic levels. Given the elevated risk for development of T2D in Hispanic/Latino populations11, even slightly elevated physiological values for glucose and insulin in a youth population warrant public health significance.
Food insecure individuals often rely on coping strategies to manage periods of food deprivation or restriction. A primary strategy is “feast-famine” - a behavioral and physiological response to cyclical food restriction described by Dinour et al.45 During this cyclical pathway, individuals experience periods of food deprivation or restriction when food is limited and overconsumption when food is plentiful. This can lead to disordered eating behaviors such as food hiding, binge eating, and night-time eating.46 Additionally, this pathway has been mechanistically linked with the development of metabolic problems as it results in an increase in body fat, decrease in lean muscle mass, and quicker weight gain during response to refeeding.47,48 Irregular meal frequency has been associated with decreased insulin sensitivity, leading to a higher insulin response to a meal.49 Additional research is needed to assess the relationship between irregular eating patterns in food insecure children and development of metabolic diseases. Furthermore, the quality of dietary intake when food is plentiful in food insecure individuals could affect glycemic control.
Los Angeles County (LA County) serves as a critical region for the study of food insecurity in Hispanic individuals. The Hispanic population of LA County exceeds that of any other county in the U.S.1 In 2014, LA County had the highest number of food insecure individuals compared to any other county.50 It is estimated that 22.8% of the child population in California (536,000 children) are food insecure. Areas in east, central and south LA have limited access to supermarkets and grocery stores for the purchase of affordable, nutrient dense foods making the region a food dessert.51 Individuals often shop at fast food outlets and corner or convenience stores close to a home; these types of stores are associated with having a detrimental affect on a child’s fruit and vegetable intake.52 Fresh fruits and vegetables are replaced with inexpensive, energy dense carbohydrates and processed foods, which can increase glycemic load and may increase the risk for insulin resistance.53–55
The dietary intake of most children, especially low-income children, in general falls far short of national recommendations, with approximately one in five low-income children not meeting any of the dietary recommendations.56–58 This study found no associations of dietary variables with food insecurity, with the exception of French fries. The assessment of dietary variables is limited by the sensitivity of the food frequency screener used in this study. It is possible that had a more sensitive diet measure been used, there would have been more significant associations with other food groups. Overall, the dietary intake results of this study are similar to those from an epidemiologic study using NHANES data, which found that neither poverty nor food insecurity was associated with nutritional outcomes (measured by the Health Eating Index) among 5,254 school age children (6–17 years).59 Additionally, while not significant, this study found that more food secure individuals were eligible for free lunch and reduced lunch at their schools compared to their food insecure peers. This difference in participation could be random variation of the data or indicative that federal nutrition assistance programs may have gaps in servicing all low-income and food insecure children. Additional research is needed using more sensitive diet measures to assess the relationships between food security and diet quality in low-income Hispanic/Latino children.
Another explanation for our findings is that food insecurity may be linked to high stress levels, which can increase cortisol levels. Higher levels of cortisol have been implicated in greater total and visceral adipose tissue (VAT), metabolic syndrome and insulin resistance.60–63 However, the current study utilized waist circumference as a proxy for VAT and found that food insecurity was not linked to waist circumference. Further research is needed to determine if food insecurity promotes a high stress response in the body and moderates the relationship between specific fat depots, such as VAT and insulin sensitivity using more sophisticated methods.
There are several limitations to consider in interpretation of these results. While, an association between food insecurity and lower glycemic control in a population of Hispanic/Latino youth was observed, this study was a cross-sectional and observational analysis and causal relationships cannot be inferred. Additionally, this study utilized a validated scale to determine food security classification, a strength of this study; however, validation was retrospectively completed in a separate cohort of Hispanic elementary aged students from the cohort used in this study. Another limitation is that the dietary screener only included 41 items, may not be representative of usual or seasonal variations in diet as it only asked about intake in the past week, requires the ability to judge individual portion sizes, and could result in under or over-estimation of different food/beverage items. Future studies should utilize more precise measure of dietary intake such as multiple day 24-hour dietary recalls, that account for greater variability in intake. Another limitation is the relatively small sample size (n=93) of subjects with metabolic data. Additionally, the population analyzed was a primarily homogenous sample of low-income, Hispanic/Latino youth and the results may not be generalizable to children of different socioeconomic statuses, ethnicities, or ages. However, if these results were seen in this homogenous sample, it is possible that a similar impact of food insecurity on glycemic control would be observed in a sample that included a more diverse socioeconomic and racial/ethnic population. Further research is warranted, as it remains unclear whether the decreased glycemic control observed in this study is a result of food insecurity or an overall insecure environment in this population.
Conclusion
Early adolescence serves as a valuable point of child development to identify factors that may be linked with decreased metabolic health. The U.S. federal nutrition programs provide a food safety net that protects against hunger, improves nutrition, and promotes health. Child nutrition programs such as the U.S. National School Lunch Program (NSLP), School Breakfast Program (SBP), and the Child and Adult Care Food Program (CACFP) operate in school, daycare, and after school settings providing nutritious meals and snacks for school aged children.64 With threatened cuts to appropriations for federal food assistance programs, further research into the role these programs play in shielding low-income and food insecure children from metabolic disease risk is warranted. This is particularly important in minority populations such as Hispanics/Latinos as metabolic diseases like T2D disproportionally affect them. This study found an association between food insecurity and glycemic control among a sample of low-income Hispanic/Latino children; however, further research is needed. To fully understand how food security impacts health outcomes like glycemic control over time and how changes to food security status can affect health outcomes longitudinal studies and interventions are warranted.
Acknowledgments
Funding/Financial Disclosures: This study was supported by funding from the NIH (grant number 5R21DK094066). A Community Benefit grant from the Keck School of Medicine at USC provided funding to build the school gardens.
Footnotes
Conflict of Interest Disclosures: The authors whose names are listed on this manuscript report no details of affiliation or involvement in an organization or entity with a financial or non-financial interest in the subject matter or materials discussed in this manuscript.
References
- 1.United States Census Bureau. Annual Estimates of the Resident Population by Sex, Race, and Hispanic Origin for the United States, States, and Counties: April 1, 2010 to July 1, 2015.
- 2.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2015. ERR-215, US Department of Agriculture, Economic Research Service; 2016. [Google Scholar]
- 3.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA 2015;314(10):1021–1029. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. Journal of the American Medical Association 2016;315(21):2292–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freedman D, Khan L, Serdula M, Dietz W, Srinivasan S, Berenson G. Inter-relationships among childhood BMI, childhood height, and adult obesity: the Bogalusa Heart Study. Int J Obes 2004;28(1):10–16. [DOI] [PubMed] [Google Scholar]
- 6.Guo S, Huang C, Maynard L, et al. Body mass index during childhood, adolescence and young adulthood in relation to adult overweight and adiposity: the Fels Longitudinal Study. Int J Obes Relat Metab Disord 2000;24(12):1628–1635. [DOI] [PubMed] [Google Scholar]
- 7.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311(8):806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goran MI, Ball GD, Cruz ML. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. J Clin Endocrinol Metab 2003;88(4):1417–1427. [DOI] [PubMed] [Google Scholar]
- 9.D’Adamo E, Caprio S. Type 2 diabetes in youth: epidemiology and pathophysiology. Diabetes Care 2011;34:S161–S165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dabelea D, Mayer-Davis EJ, Saydah S, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 2014;311(17):1778–1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Narayan KV, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA 2003;290(14):1884–1890. [DOI] [PubMed] [Google Scholar]
- 12.Anderson SA. Core indicators of nutritional state for difficult-to-sample populations. J Nutr 1990;120(11):1559–1600. [DOI] [PubMed] [Google Scholar]
- 13.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2016. ERR-237, USDA, Economic Research Service; 2017. [Google Scholar]
- 14.Hannon TS, Rao G, Arslanian SA. Childhood obesity and type 2 diabetes mellitus. Pediatrics 2005;116(2):473–480. [DOI] [PubMed] [Google Scholar]
- 15.Goran MI, Bergman RN, Cruz ML, Watanabe R. Insulin resistance and associated compensatory responses in African-American and Hispanic children. Diabetes Care 2002;25(12):2184–2190. [DOI] [PubMed] [Google Scholar]
- 16.Haffner SM, Miettinen H, Gaskill SP, Stern MP. Decreased insulin secretion and increased insulin resistance are independently related to the 7-year risk of NIDDM in Mexican-Americans. Diabetes 1995;44:1386–1391. [DOI] [PubMed] [Google Scholar]
- 17.Haffner SM, Saad MF, Rewers M, et al. Increased insulin resistance and insulin secretion in nondiabetic African-Americans and Hispanics compared with non-Hispanic whites: the Insulin Resistance Atherosclerosis Study. Diabetes 1996;45(6):742–748. [DOI] [PubMed] [Google Scholar]
- 18.Haffner SM, Stern MP, Mitchell BD, Hazuda HP, Patterson JK. Incidence of type II diabetes in Mexican Americans predicted by fasting insulin and glucose levels, obesity, and body-fat distribution. Diabetes 1990;39(3):283–288. [DOI] [PubMed] [Google Scholar]
- 19.Parker ED, Widome R, Nettleton JA, Pereira MA. Food security and metabolic syndrome in US adults and adolescents: findings from the National Health and Nutrition Examination Survey, 1999–2006. Ann Epidemiol 2010;20(5):364–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eicher-Miller HA, Mason AC, Weaver CM, McCabe GP, Boushey CJ. Food insecurity is associated with iron deficiency anemia in US adolescents. Am J Clin Nutr 2009;90(5):1358–1371. [DOI] [PubMed] [Google Scholar]
- 21.Skalicky A, Meyers AF, Adams WG, Yang Z, Cook JT, Frank DA. Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Matern Child Health J 2006;10(2):177–185. [DOI] [PubMed] [Google Scholar]
- 22.Kirkpatrick SI, McIntyre L, Potestio ML. Child hunger and long-term adverse consequences for health. Arch Pediatr Adolesc Med 2010;164(8):754–762. [DOI] [PubMed] [Google Scholar]
- 23.Whitaker RC, Phillips SM, Orzol SM. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics 2006;118(3):e859–868. [DOI] [PubMed] [Google Scholar]
- 24.Huang J, Oshima KMM, Kim Y. Does food insecurity affect parental characteristics and child behavior? Testing mediation effects. Soc Serv Rev 2010;84(3):381–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Howard LL. Does food insecurity at home affect non-cognitive performance at school? A longitudinal analysis of elementary student classroom behavior. Econ Educ Rev 2011;30(1):157–176. [Google Scholar]
- 26.Melchior M, Chastang J-F, Falissard B, et al. Food insecurity and children’s mental health: a prospective birth cohort study. PloS One 2012;7(12):e52615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaur J, Lamb MM, Ogden CL. The association between food insecurity and obesity in children—the National Health and Nutrition Examination Survey. J Acad Nutr Diet 2015;115(5):751–758. [DOI] [PubMed] [Google Scholar]
- 28.Casey PH, Simpson PM, Gossett JM, et al. The association of child and household food insecurity with childhood overweight status. Pediatrics 2006;118(5):e1406–e1413. [DOI] [PubMed] [Google Scholar]
- 29.Chi DL, Masterson EE, Carle AC, Mancl LA, Coldwell SE. Socioeconomic status, food security, and dental caries in US children: mediation analyses of data from the National Health and Nutrition Examination Survey, 2007–2008. Am J Public Health 2014;104(5):860–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fram MS, Ritchie LD, Rosen N, Frongillo EA. Child experience of food insecurity is associated with child diet and physical activity. J Nutr 2015;145(3):499–504. [DOI] [PubMed] [Google Scholar]
- 31.Cook JT, Black M, Chilton M, et al. Are food insecurity’s health impacts underestimated in the US population? Marginal food security also predicts adverse health outcomes in young US children and mothers. Adv Nutr 2013;4(1):51–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.LA’s Best. http://www.lasbest.org/.
- 33.Davis JN, Martinez LC, Spruijt-Metz D, Gatto NM. LA Sprouts: A 12-week gardening, nutrition, and cooking randomized control trial improves determinants of dietary behaviors. J Nutr Educ Behav 2016;48(1):2–11. e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gatto N, Martinez L, Spruijt‐Metz D, Davis J. LA Sprouts randomized controlled nutrition, cooking and gardening programme reduces obesity and metabolic risk in Hispanic/Latino youth. Pediatr Obes 2017;12(1):28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martinez LC, Gatto NM, Spruijt-Metz D, Davis JN. Design and methodology of the LA Sprouts nutrition, cooking and gardening program for Latino youth: a randomized controlled intervention. Contemp Clin Trials 2015;42:219–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000. CDC growth charts for the United States: methods and development. Vital Health Stat 11 2002(246):1–190. [PubMed] [Google Scholar]
- 37.National Center for Health Statistics. National Health and Nutrition Examination Survey (NHANES): Anthropometry Procedures Manual 2007 2007.
- 38.Hunsberger M, O’Malley J, Block T, Norris JC. Relative validation of Block Kids Food Screener for dietary assessment in children and adolescents. Matern Child Nutr 2015;11(2):260–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bernal J, Frongillo EA, Herrera H, Rivera J. Children live, feel, and respond to experiences of food insecurity that compromise their development and weight status in peri-urban Venezuela. J Nutr 2012;142. [DOI] [PubMed] [Google Scholar]
- 40.Fram MS, Frongillo EA, Draper CL, Fishbein EM. Development and validation of a child report assessment of child food insecurity and comparison to parent report assessment. J Hunger Environ Nutr 2013;8(2):128–145. [Google Scholar]
- 41.Fram MS, Frongillo EA, Jones SJ, et al. Children are aware of food insecurity and take responsibility for managing food resources. J Nutr 2011;141(6):1114–1119. [DOI] [PubMed] [Google Scholar]
- 42.United States Department of Agriculture Economic Research Service: Self-administered food security survey module for children ages 12 years and older http://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/survey-tools.aspx.
- 43.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972;18(6):499–502. [PubMed] [Google Scholar]
- 44.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28(7):412–419. [DOI] [PubMed] [Google Scholar]
- 45.Dinour LM, Bergen D, Yeh M-C. The food insecurity–obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc 2007;107(11):1952–1961. [DOI] [PubMed] [Google Scholar]
- 46.Tester JM, Lang TC, Laraia BA. Disordered eating behaviours and food insecurity: A qualitative study about children with obesity in low-income households. Obes Res Clin Pract 2015;10(5):544–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dietz WH. Does hunger cause obesity? Pediatrics 1995;95(5):766–767. [PubMed] [Google Scholar]
- 48.Metallinos-Katsaras E, Must A, Gorman K. A longitudinal study of food insecurity on obesity in preschool children. J Acad Nutr Diet 2012;112(12):1949–1958. [DOI] [PubMed] [Google Scholar]
- 49.Farshchi H, Taylor M, Macdonald I. Regular meal frequency creates more appropriate insulin sensitivity and lipid profiles compared with irregular meal frequency in healthy lean women. Eur J Clin Nutr 2004;58(7):1071–1077. [DOI] [PubMed] [Google Scholar]
- 50.Gundersen C, Waxman E, Engelhard E, Satoh A, Chawla N. Map the Meal Gap 2014: Food Insecurity Estimates at the County Level Chicago, IL: Feeding America;2014. [Google Scholar]
- 51.Bassford N, Galloway-Gilliam L, Flynn G, Community Health Councils Inc. Food desert to food oasis: Promoting grocery store development in South Los Angeles Los Angeles, CA: Community Health Councils, Inc; 2010. [Google Scholar]
- 52.Timperio A, Ball K, Roberts R, Campbell K, Andrianopoulos N, Crawford D. Children’s fruit and vegetable intake: associations with the neighbourhood food environment. Prev Med 2008;46(4):331–335. [DOI] [PubMed] [Google Scholar]
- 53.Gross LS, Li L, Ford ES, Liu S. Increased consumption of refined carbohydrates and the epidemic of type 2 diabetes in the United States: an ecologic assessment. Am J Clin Nutr 2004;79(5):774–779. [DOI] [PubMed] [Google Scholar]
- 54.Kendall A, Olson CM, Frongillo EA. Relationship of hunger and food insecurity to food availability and consumption. J Am Diet Assoc 1996;96(10):1019–1024. [DOI] [PubMed] [Google Scholar]
- 55.Willett W, Manson J, Liu S. Glycemic index, glycemic load, and risk of type 2 diabetes. Am J Clin Nutr 2002;76(1):274s–280s. [DOI] [PubMed] [Google Scholar]
- 56.Brady LM, Lindquist CH, Herd SL, Goran MI. Comparison of children’s dietary intake patterns with US dietary guidelines. Br J Nutr 2000;84(03):361–367. [PubMed] [Google Scholar]
- 57.Devaney B, Kim M, Carriquiry A, Camano-Garcia G. Assessing the Nutrient Intakes of Vulnerable Subgroups Princeton, NJ: Mathematica Policy Research, Inc;2005. [Google Scholar]
- 58.Patrick H, Nicklas TA. A review of family and social determinants of children’s eating patterns and diet quality. J Am Coll Nutr 2005;24(2):83–92. [DOI] [PubMed] [Google Scholar]
- 59.Bhattacharya J, Currie J, Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. J Health Econ 2004;23(4):839–862. [DOI] [PubMed] [Google Scholar]
- 60.Adam TC, Hasson RE, Ventura EE, et al. Cortisol is negatively associated with insulin sensitivity in overweight Latino youth. J Clin Endocrinol Metab 2010;95(10):4729–4735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Björntorp P Hormonal regulation of visceraladipose tissue. Growth Horm IGF Res 1998;8:15–17. [DOI] [PubMed] [Google Scholar]
- 62.Duclos M, Pereira PM, Barat P, Gatta B, Roger P. Increased cortisol bioavailability, abdominal obesity, and the metabolic syndrome in obese women. Obesity Research 2005;13(7):1157–1166. [DOI] [PubMed] [Google Scholar]
- 63.Kidambi S, Kotchen JM, Grim CE, et al. Association of adrenal steroids with hypertension and the metabolic syndrome in blacks. Hypertension 2007;49(3):704–711. [DOI] [PubMed] [Google Scholar]
- 64.US Department of Agriculture Food and Nutrition Service. Child Nutrition Programs 2017; https://www.nutrition.gov/food-assistance-programs/child-nutrition-programs.