Abstract
Point of care ultrasound (POCUS) provides diagnostic information in addition to visual pulse checks during cardiopulmonary resuscitation (CPR). The most commonly used modality—transthoracic echocardiography (TTE)—has unfortunately been repeatedly associated with prolonged pauses in chest compressions, which correlate with worsened neurologic outcomes. Unlike TTE, transesophageal echocardiography (TEE) does not require cessation of compressions for adequate imaging, while also providing the diagnostic benefit of POCUS. To assess a benefit of TEE, we compared the duration of chest compression pauses between TEE, TTE and manual pulse checks on video recordings of CA resuscitations. We analyzed 139 pulse check CPR pauses among 25 patients during CA. TEE provided the shortest mean pulse check duration (9 seconds [95% CI: 5–12]). Mean pulse check duration with TTE was 19 seconds (95% CI: 16–22), and 11 seconds (95% CI: 8–14) with manual checks. ICC between abstractors for a portion of individual and average times was 0.99 and 0.99, respectively (p<0.0001 for both). Our study suggests that pulse check times with TEE are shorter vs TTE for ED POCUS during CA resuscitations, and further emphasizes the need for careful attention to compression pause duration when using TTE for POCUS during ED CA resuscitations.
Introduction
The use of point-of-care ultrasound (POCUS) as a diagnostic adjunct during in hospital cardiopulmonary resuscitation (CPR) is increasing and is suggested in the most recent American Heart Association (AHA) guidelines.1 Commonly employed by emergency physicians, POCUS can identify reversible causes of arrest such as pulmonary embolism and pericardial effusions,5 errors in pulse check and rhythm analysis,6 and cardiac contractility, which itself has been shown to be the best predictor of survival in cases without a shockable rhythm.5 Transthoracic echocardiography (TTE) is the most common POCUS modality during CPR, though it requires the halting of chest compressions to obtain adequate imaging windows, and can be complicated by factors such as an air-filled stomach and body habitus.
Recent studies have demonstrated TTE POCUS interferes with chest compression delivery, leading to significantly prolonged hands-off time compared to manual palpation alone.7,8 This is important, because CPR guidelines emphasize limiting the duration of pauses to less than ten seconds, as these lead to loss of coronary and cerebral perfusion.1–3 Maximizing the ratio of chest compressions to pauses, known as the chest compression fraction, has been shown to result in decreased mortality.4
In contrast to TTE, transesophageal echocardiography (TEE) as a POCUS modality does not interfere with chest compressions and has been shown to provide adequate images in nearly all critically ill patients, conferring practice-changing information more frequently when compared with TTE.9 At our institution, emergency department CPR may be performed with manual palpation pulse checks, with either TTE or TEE. As the benefits of POCUS during CPR can be obtained without pauses in compressions when using TEE, we sought to assess whether the use of TEE resulted in decreased pause duration compared to TTE or manual pulse checks.
Hypothesis
We hypothesized that TEE-guided pulse and rhythm checks would be shorter, on average, than TTE or manual pulse and rhythm checks.
Methods
We performed a retrospective analysis of video recordings obtained routinely for quality improvement purposes during CPR. The analysis and reporting of this data was approved by the Institutional Review Board.
Setting
The University of Utah emergency department (ED) is a level 1 trauma center and tertiary care facility staffed by board-certified emergency medicine faculty and postgraduate year 1–3 emergency medicine residents with an annual volume of approximately 50,000 patients. Motion-activated cameras record video and audio activity in all 4 of our resuscitation rooms. These videos are used for quality improvement and educational purposes in both trauma and medical resuscitations. Resuscitation attempts are typically staffed by an attending physician, one or two emergency medicine residents, 1–2 emergency nurses, and with 1–2 paramedics or EMTs. All emergency physicians are trained and credentialed in the use of TTE POCUS, with a limited number of attending physicians additionally trained to use TEE.
Inclusion and Exclusion Criteria
Adult patients (≥18 years of age) were included who suffered medical or traumatic cardiac arrest with CPR that was video-captured between March 1, 2016 and May 25, 2017. These were consecutive cardiac arrests receiving active resuscitation for which video was available.
Methods of Data Capture
Two trained abstractors, blinded to the study hypothesis, reviewed the digital video recordings of all sequential available CPR attempts and recorded the timing and duration of all pauses in chest compressions until efforts were ceased, either due to return of spontaneous circulation (ROSC) or a declaration of death. Pauses were defined as the time from the last compression until the start of the next compression, and were recorded with precision to 1 second. For all recorded pauses, abstractors documented any interventions concomitantly performed (such as attempts at endotracheal intubation or arterial access), whether TEE or TTE was used at the time of the pause, whether a pulse and/or rhythm check was performed, and whether a shock was delivered. Compressions were not paused for TEE insertion. Any areas of uncertainty were adjudicated by one of the principal investigators. Duplicative cross-abstraction was performed in 10% of cases to determine the agreement between reviewers. Demographics and resuscitation details were abstracted from the electronic medical record and nursing flowsheets.
Statistical Analysis
All data were entered into an Excel spreadsheet (Microsoft Excel for Mac, version 15.4, Microsoft Corp, Redmond, WA) and analyzed using STATA statistical software (Stata/IC for Mac [64-bit Intel], version 14.2, StataCorp, College Station, TX). To evaluate the independent effect of TEE, TTE, or manual palpation alone on the duration of CPR pause during pulse and rhythm checks, we compared the average duration of pause (primary outcome) associated with the three groups. We used generalized linear mixed models (mixed command in STATA), which account for variability both within and between patients in whom repeated measures are obtained. We excluded pauses during which procedures were performed. Because individual patients had multiple pulse checks using one or more modalities to assess for return of spontaneous circulation, we entered pulse check modality as both a random and fixed effect. Individual arrests were modeled as random effects. (In other words, individual pulse checks were nested within pulse check modality which were nested within individual arrests.) We estimated that 31 pauses would provide 90% power to detect a difference in duration of pause of 5 seconds with an alpha of 0.05, assuming a correlation coefficient of 0.05 between measures and a common standard deviation of 6 seconds. To assess agreement between reviewers, we calculated intraclass correlations coefficients (ICC) on a portion of the data (27%; 31/139) using a two-way random effects model. We considered a p value of <0.05 to be statistically significant and all tests were two tailed.
Results
During the period between March 1, 2016 and May 25, 2017 there were a total of 25 arrests (23 medical, 2 traumatic) providing 208 pauses (139 CPR pauses for analysis and 69 pauses for procedures or other resuscitation activities). Figure 1 shows demographic information, details the resuscitation attempts and outlines the flow of patient data. Among all patients, 88% experienced a prehospital arrest, whereas 12% arrested in the ED. Forty eight percent were male, 32% (8/25) of arrests were witnessed, while 20% (5/25) had bystander CPR. Sixteen percent (4/25) had an initial shockable rhythm, 28% (7/25) had either asystole or PEA as an initial rhythm, and 56% (14/25) had an unknown initial rhythm, while 12% achieved prehospital ROSC. In unadjusted analysis, TTE was associated with in an average pause duration of 18 (SD 8) seconds, TEE 7 (SD 5) seconds, and manual palpation 10 (SD 5) seconds.
Figure 1:
Overview of total cardiac arrest pauses included for analysis.
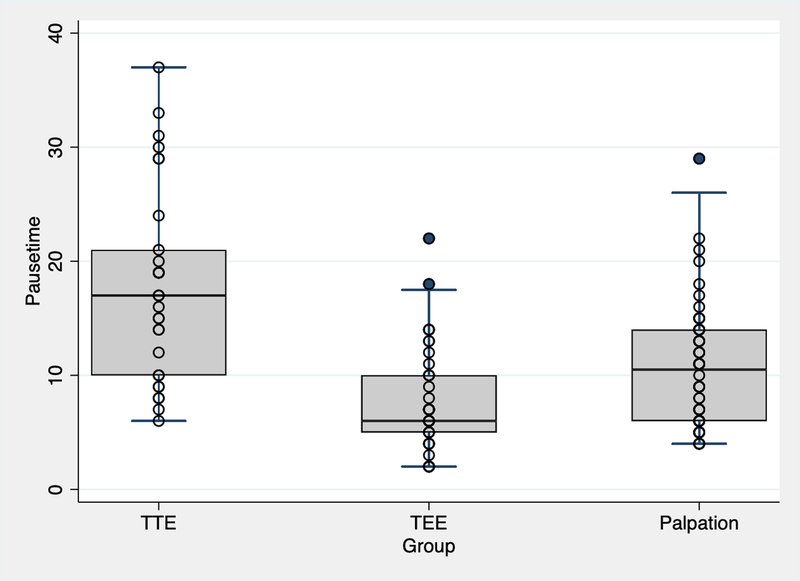
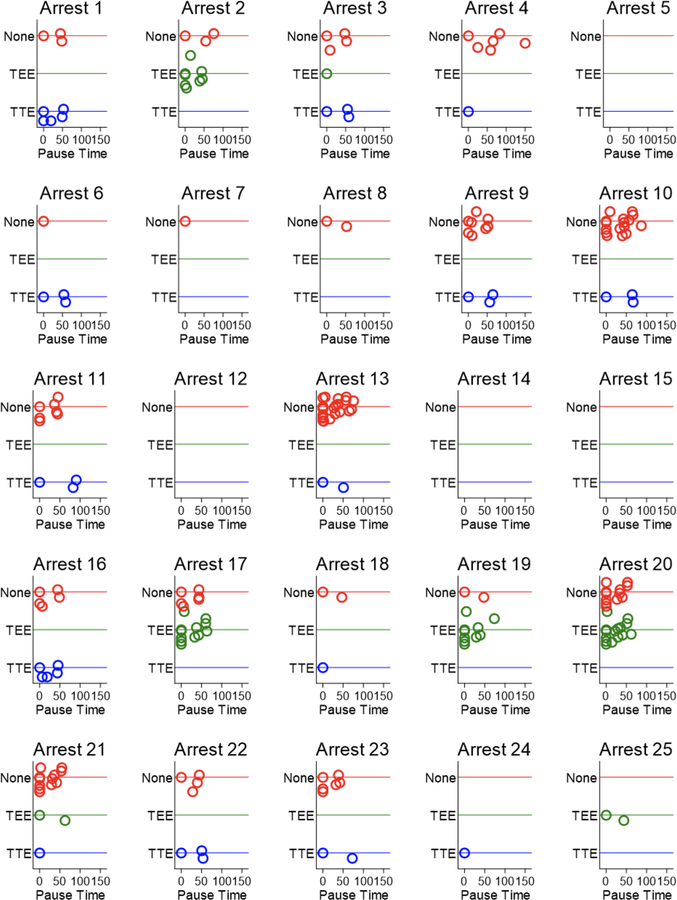
Figure 2 provides point estimates of generalized linear model-adjusted mean pauses performed using either TEE, TTE, or manual palpitation with 95% confidence intervals (CI). Figure 3 displays a dot plot of the individual pause times for each arrest. Arrests without pauses had time of death called on arrival. Resuscitations guided by TEE were associated with a mean duration of pulse check of 9 seconds (95% CI: 5–12), whereas resuscitations guided by TTE were associated with a mean duration of pulse check of 19 seconds (95% CI: 16–22). Resuscitations using manual pulse checks without ultrasound were associated with a mean duration of 11 seconds (95% CI: 8–14). The difference between TTE and TEE at 10 seconds provided a 95% confidence interval of 5–14. The difference between TTE and manual palpation at 8 seconds provided a 95% confidence interval of 4–11. Finally, TEE and manual palpation at −2 seconds provided a 95% confidence interval of −6 to 2. Calculated ICC between individual and average measurements was 0.99 and 0.99, respectively, suggesting high level of agreement.
Figure 2:
Bar graph of mean compression pause times comparing palpation alone, TTE use, and TEE use.
Figure 3:
Dot plot displaying individual pause times within each arrest.
Discussion
This retrospective analysis of compression pause times during ED CPR compared duration of pauses in compressions for pulse checks when TTE, TEE, or manual palpation alone was used. We found a statistically significant prolongation of compression pause times when TTE was used compared to TEE or manual pulse checks. TEE was similar to manual pulse checks in this study.
Our findings are similar to multiple recent studies that have found an association with TTE use and longer CPR pauses. The two most recent publications demonstrated averages of 17 and 21 seconds with TTE use, similar to our findings of an average of 19 seconds.7,8 While these studies did not look at patient-centered outcomes related to POCUS use in cardiac arrest patients, prolonged pauses in chest compressions are shown to lead to worse outcomes and should be avoided.10,11
Our findings are important in light of the potential conflict between the AHA guidelines to maximize compression fraction during CPR, while obtaining useful diagnostic information with POCUS. We demonstrated that POCUS using TEE resulted a similar duration of pause compared to manual palpation alone, which was significantly shorter compared to POCUS with TTE.
The benefit of POCUS during CPR includes its ability to correct misclassification of rhythm analysis as well as identify reversible causes of cardiac arrest. As was demonstrated in the REASON study, POCUS can successfully identify subsets of patients with PEA arrest with a better prognosis, such as those with evidence of RV strain or pericardial tamponade.5 Unfortunately, studies of POCUS using TTE have consistently demonstrated prolonged pauses in compressions. TEE provides a solution to this dilemma by offering continuous visualization of the heart during both compressions and pauses without interfering with chest compressions. While not demonstrated in this study, TEE has the potential to facilitate shorter compression pause times when compared to manual pulse checks, as if cardiac standstill is clearly visualized during a pause in compressions, providers do not necessarily need to wait the full 10 seconds in order to determine the absence of a pulse.
Limitations
The primary limitation of this study was the retrospective nature, limiting the precision of the pulse check timing obtained from video review. A prospective study with independent time checks would enable more precision. Secondly, the study was only powered to detect differences of 5 seconds, which may be inadequate to distinguish between manual checks and TEE. During the time period included in this study, there were only 4 attending emergency physicians at our institution utilizing TEE in ED cardiac arrest resuscitations and all 4 had ultrasound fellowship training, meaning that if TEE was used then an ultrasound fellowship trained provider was present for the resuscitation. While the provider performing the ultrasound was not the one running the code, their involvement may have influenced compression pause duration. It is possible that a small number of arrests could have a occurred during the study period for which video was not available due to technical failure, but the authors are not aware of any missed cases. Lastly, this is a single study from an academic center and not necessarily generalizable to other practice environments.
Conclusion
In this retrospective analysis of pause duration during ED CPR, pauses during POCUS with TEE were significantly shorter than those utilizing TTE, and comparable to manual pulse check duration. Our findings suggest a potential benefit of TEE for POCUS compared to traditional TTE, and additionally highlight the need for careful attention to pause duration when using TTE during CPR. Larger studies are necessary to investigate the potential impact of the choice of ultrasound modality on patient oriented outcomes.
Acknowledgments
Dr. Tonna was supported by a career development award (K23HL141596) from the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH). This study was also supported, in part, by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, NIH, through grant 5UL1TR001067-02 (formerly 8UL1TR000105 and UL1RR025764).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. None of the funding sources were involved in the design or conduct of the study, collection, management, analysis or interpretation of the data, or preparation, review, or approval of the article.
Footnotes
Conflict of Interest and Sources of Funding
This study was supported, in part, by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 5UL1TR001067–02 (formerly 8UL1TR000105 and UL1RR025764). None of the funding sources were involved in the design or conduct of the study, collection, management, analysis or interpretation of the data, or preparation, review or approval of the manuscript. None of the authors report any conflicts of interest related to this manuscript.
References:
- 1.Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, et al. Part 7: adult advanced cardiovascular life support: 2015 american heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015;132(18 Suppl 2):S444–64 November 3. [DOI] [PubMed] [Google Scholar]
- 2.Soar J, Nolan JP, Böttiger BW, Perkins GD, Lott C, Carli P, et al. European resuscitation council guidelines for resuscitation 2015 section 3. adult advanced life support. Resuscitation 2015;95:100–47. [DOI] [PubMed] [Google Scholar]
- 3.Berg RA, Sanders AB, Kern KB, et al. Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation. 2001;104(20):2465–2470. [DOI] [PubMed] [Google Scholar]
- 4.Christenson J, Andrusiek D, Everson-Stewart S, et al. Chest Compression Fraction Determines Survival in Patients with Out-of-hospital Ventricular Fibrillation. Circulation 2009. September 29; 120(13): 1241–1247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gaspari R et al. Emergency Department Point-Of-Care Ultrasound in Out-Of-Hospital and in-ED Cardiac Arrest. Resuscitation 2016; 109: 33–39 [DOI] [PubMed] [Google Scholar]
- 6.Breitkreutz R, Price S, Steiger HV, et al. Focused echocardiographic evaluation in life support and peri-resuscitation of emergency patients: a prospective trial. Resuscitation 2010. November;81(11):1527–33 [DOI] [PubMed] [Google Scholar]
- 7.His in ‘t Veld M, Allison M, Bostick D, et al. Ultrasound use during cardiopulmonary resuscitation is associated with delays in chest compressions. Resuscitation 119 (2017) 95–98 [DOI] [PubMed] [Google Scholar]
- 8.Point-of-care ultrasound use in patients with cardiac arrest is associated prolonged cardiopulmonary resuscitation pauses: A prospective cohort study. Resuscitation 2018. January;122-65–68 [DOI] [PubMed] [Google Scholar]
- 9.Heidenreich PA, Stainback RF, Redberg RF, et al. Transesophageal echocardiography predicts mortality in critically ill patients with unexplained hypotension. J Am Coll Cardiol1995 Jul;26(1):152–8 [DOI] [PubMed] [Google Scholar]
- 10.Kellum MJ, Kennedy KW, Barney R, Keilhauer FA, Bellino M, Zuercher M, et al. Cardiocerebral resuscitation improves neurologically intact survival of patients with our-of-hospital cardiac arrest. Ann Emerg Med. 52(3)(2008) 244–252 [DOI] [PubMed] [Google Scholar]
- 11.Cheskes S, Schmicker RH, Christenson J, Salcido DD, Rea T, Powell J, et al. Morrison L, and Resuscitation Outcomes Consortium (ROC) Investigators: perishock pause: an independent predictor of survival from out-of-hospital shockable cardiac arrest. Circulation 124(1)(2011) 58–66 [DOI] [PMC free article] [PubMed] [Google Scholar]