Abstract
It is challenging to estimate genetic variant burden across different subtypes of epilepsy. Herein, we used a comparative approach to assess the genetic variant burden and genotype–phenotype correlations in four most common brain lesions in patients with drug-resistant focal epilepsy. Targeted sequencing analysis was performed for a panel of 161 genes with a mean coverage of >400×. Lesional tissue was histopathologically reviewed and dissected from hippocampal sclerosis (n = 15), ganglioglioma (n = 16), dysembryoplastic neuroepithelial tumors (n = 8), and focal cortical dysplasia type II (n = 15). Peripheral blood (n = 12) or surgical tissue samples histopathologically classified as lesion-free (n = 42) were available for comparison. Variants were classified as pathogenic or likely pathogenic according to American College of Medical Genetics and Genomics guidelines. Overall, we identified pathogenic and likely pathogenic variants in 25.9% of patients with a mean coverage of 383×. The highest number of pathogenic/likely pathogenic variants was observed in patients with ganglioglioma (43.75%; all somatic) and dysembryoplastic neuroepithelial tumors (37.5%; all somatic), and in 20% of cases with focal cortical dysplasia type II (13.33% somatic, 6.67% germline). Pathogenic/likely pathogenic positive genes were disorder specific and BRAF V600E the only recurrent pathogenic variant. This study represents a reference for the genetic variant burden across the four most common lesion entities in patients with drug-resistant focal epilepsy. The observed large variability in variant burden by epileptic lesion type calls for whole exome sequencing of histopathologically well-characterized tissue in a diagnostic setting and in research to discover novel disease-associated genes.
Subject terms: Genetic testing, DNA sequencing, Epilepsy
Introduction
Drug-resistant epilepsies due to focal brain lesions represent a huge health burden and challenge for every day clinical practice [1]. Neurosurgical resection strategies have proven helpful in carefully selected patients, especially for magnetic resonance imaging and histopathologically visible brain lesions [2]. The most common types epilepsy-associated brain lesions comprise hippocampal sclerosis (HS) [3], low-grade epilepsy-associated brain tumors (LEAT) [4], such as ganglioglioma (GG) and dysembryoplastic neuroepithelial tumors (DNT), and focal cortical dysplasia type II (FCDII) [5]. Overall, these four types of epilepsy-associated brain lesions account for more than 60% of almost 10,000 patients submitted to epilepsy surgery collected at the European Epilepsy Brain Bank [2].
The genetics of epilepsy-associated brain lesions represent an emerging field. Overall, to date more than 14 genes have been associated with epilepsy-associated brain lesions for FCDII and LEAT [4, 6, 7] and to the best of our knowledge, the burden of somatic gene variants has not been evaluated for HS tissue before. These lesion type specific genetic studies have been successful to different degree with a wide range of diagnostic yield. Somatic variants at low rate mosaicism in brain DNA, with somatic alternate allele fractions (AAF) ranging from 0.9 to 12.6% and activating the PI3K-AKT-mTOR pathway were identified in 25% of FCDII, namely AKT3, MTOR, and PIK3CA [6]. In addition, germline loss-of-function variants in DEPDC5 and NPRL2, also belonging to the PI3K-AKT-mTOR pathway, were identified in FCDII patients. The detection of some of those variants led to a pathophysiology-based therapy in the sense of precision medicine [8] which might be also conceivable for other focal pharmaco-resistant epilepsies in the future.
Somatic variants in BRAF and FGFR1 have been reported to play a major role in LEAT with BRAF V600E in 18–56% [4] and variants in FGFR1 in 58–82% of patients in individual studies [9, 10].
The majority of epileptic brain lesion-associated genes have been discovered in the past 5 years, so few data are available regarding the prevalence of variants and genotype–phenotype correlations. An accurate estimation of the genetic contribution to different brain lesions has proven difficult with most data coming from various studies on specific epilepsy-associated brain lesion subtypes with a large variety in genetic screening approach, study design, and technology. In the present study, we performed a comparative analysis and assessment of pathogenic (P) or likely pathogenic (LP) variants across the four major disease entities associated with drug-resistant epilepsy-associated brain lesions. This study will help to understand the genetic variant burden for specific brain lesions, the contribution of genetic mosaicisms and commonalities in the epilepsy phenotype. Unraveling the genetic variant burden of epilepsy-associated brain lesions will help to find new treatments for current drug-resistant patients.
Subjects and methods
Patients included in the study
All patients were retrospectively identified from the epilepsy surgery database of the University Hospital Erlangen, Germany and the University Hospital Tübingen, Germany. The study was approved by the University of Cologne ethical review board. A total of 54 patients fulfilled the following criteria and were included in this study: (1) drug-resistant focal epilepsy; (2) diagnosis of FCDII, GG, DNT, or HS approved by histopathology; (3) availability of a brain lesion paired with adjacent nonlesional brain or blood; (4) patient consented for genetic studies; (5) quality and amount of DNA from extracted brain tissue sufficient for NGS.
Selection of brain tissue samples and DNA extraction
Targeted sequencing of DNA samples obtained from either a brain lesion tissue (n = 55) and adjacent nonlesional brain region (n = 40) or a brain lesion and blood (n = 14) was performed in 15 subjects with FCDII, 15 subjects with GG, eight subjects with DNT, 15 subjects with HS, and one subject with GG and HS (both lesions were analyzed). In the statistical analysis, we counted the patient with two lesions to the group of LEATs since the GG was the patient’s primary lesion. All tissue samples were microscopically reviewed and classified as lesional or nonlesional. Genomic DNA was extracted either from fresh frozen brain (n = 53), formalin-fixed, paraffin-embedded (FFPE) brain tissues (n = 44) or blood (n = 12). The DNeasy Blood and Tissue Kit (Qiagen) was used for DNA extraction from fresh frozen brain samples according to the manufacturer’s protocol. Automated DNA extraction from blood was performed using the chemagic DNA Blood Kit Special (Chemagen/Perkin Elmer). FFPE samples were deparaffinized using xylol followed by DNA extraction using the QIAamp DNA Micro Kit (Qiagen). DNA quality was assessed on a 2% agarose gel.
Gene panel design
A customized gene panel was designed with Agilent’s SureDesign software. The panel targeted 62 PI3K-AKT-mTOR pathway genes (derived from NIH Cancer Genome Anatomy BioCarta pathways project; https://cgap.nci.nih.gov, keyword: “h_mTORPathway”), 50 genes previously associated with epilepsy [11–13], 15 genes associated with malformations of cortical development [14–22], 21 genes associated with brain tumors [9, 23–28] and the 13 most frequently mutated genes in 28 tumor types from Integrative Onco Genomics (https://www.intogen.org/search?). The full gene list is provided in Supplementary Table 1.
Sequencing
Library preparation was conducted using Agilent SureSelect Custom Enrichment Kit, and libraries underwent paired-end sequencing on an Illumina HiSeq 4000 instrument according to manufacturer’s protocol. To increase the average read depth of sequencing from samples with low DNA quality to more than 200×, we performed two independent library preparations and merged the fastq files from both runs.
Bioinformatic analysis
For bioinformatic analysis, we generated analysis-ready bam files using BWA to map reads to the human genome reference build GRCh37 from the 1000 Genomes Project combined with the ensemble build 66 MT-sequence (GCF_000001405.13; http://ftp.1000genomes.ebi.ac.uk/vol1/ftp/technical/reference/README.human_g1k_v37.fasta.txt). GATK version 3.6 [29] was used to mark duplicated reads, perform local realignment, recalibrate the base quality scores and call SNPs and short indels together with Picard, SAM tools version 0.1.18 and Dindel [29–31].
Germline variant calling, quality control, and filtering
We screened our patients for germline and somatic variants. To discover germline variants, we used scripts developed in-house at the Cologne Center for Genomics to filter for variants affecting protein-coding genes. Germline variants were functionally annotated using ANNOVAR’s web interface (wANNOVAR) [32]. Variants were filtered for (1) stop-gain, nonsynosnymous, frameshift, and splicing variants; (2) variants located at a region with a minimal read coverage of 6×; (3) calling consistency in both tissues-pairs with allele balance of ≥25%. Filtering for platform artifacts was performed against an in-house database containing variants from 511 exomes (http://varbank.ccg.uni-koeln.de) from epilepsy patients and by allele frequency filter >10% within our patient cohort. Finally, to enrich for variants of large effect, all variants, which were present in Genome Aggregation Database (gnomAD) [33], were removed.
Somatic variant calling, quality control, and filtering
To discover somatic variants we performed variant calling using MuTect2 [34] and Strelka2 [35] in lesion-free/lesion brain and blood/lesion brain paired data sets. MuTect2 and Strelka2 both use Bayesian approaches; however, they apply different filters and produce different calling results. To select candidate variants of high confidence, we considered only MuTect2/Strelka2 consensus calls. Samples with exceptionally high numbers of variants (>2 standard deviations from the mean) were excluded. We then filtered for stop-gain/loss, nonsynonymous, frameshift, and splicing variants and used ANNOVAR [36] version 2015 to annotate allele frequencies and deleteriousness prediction scores from the dbNSFP database v3.0.
Assessment of variant pathogenicity
All identified variants were classified following 28 criteria defined by the guidelines of the American College of Medical Genetics and Genomics (ACMG) [37]. The ACMG guidelines classify variants based on criteria using typical types of variant evidence (e.g., population data, computational data, functional data, segregation data), and recommend the use of specific standard terminology—“pathogenic,” “likely pathogenic,” “uncertain significance,” “likely benign,” and “benign”—to describe variants identified in genes that cause Mendelian disorders. We applied the ACMG guidelines on the identified variants using the online tool InterVar [38]. “Pathogenic variants” are defined as dominant acting variants that cause disease. Information about the phenotype and the genetic variants of all patients with VUS, LP, and pathogenic variants were submitted to Leiden Open Variation Database (LOVD; https://databases.lovd.nl/shared/variants) (individuals IDs: 00226318, 00226327, 00226333, 00226335, 00226336, 00226338-00226346, 00234381, 00234387, 00234400). We did not validate low frequency (<5% somatic alternate allele frequency) somatic variants experimentally.
Results
To identify new variants and to elucidate the variant burden in patients with epilepsy-associated brain lesions, we performed targeted sequencing which resulted in a mean gene coverage of 418.44× (SD = 134.53) across the target genes with 96.55% (SD = 6.18) of bases covered at 25× (Supplementary Table 1) and a mean percentage of uniquely mapped reads of 95.13% (SD = 0.51) across the 54 patients (Supplementary Table 2).
Analysis of germline variants
Variant calling and stringent quality control identified 37 germline variants in 26 of 54 (48.2%) patients. However, only one of the 37 germline variants was predicted pathogenic by ACMG guidelines resulting in a germline variant burden of 1.85% in our cohort. The variant was a stop codon introducing missense variant in DEPDC5 (NM_001242896.1:c.4312C>T (p.(Q1438*))) in patient 1 with FCDIIA. We further identified a potentially interesting VUS in patient 2 with HS in MTOR (NM_004958.3:c.5845C>G (p.(P1949A)). Although MTOR is an established disease gene in FCDII, it has not been associated to the related HS before. Since the gene-disorder association has not been clearly established, inheritance data and functional data is lacking, we have to classify the MTOR variant as VUS instead of LP based on the ACMG guidelines.
Somatic variant analysis
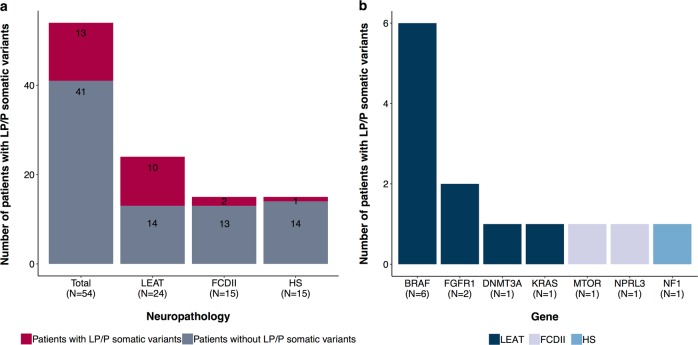
Paired sample analysis identified a total number of 15 exonic somatic variants in 14 of 54 patients (Table 1, Supplementary Table 3), all absent in the control tissues (Supplementary Fig. 1). According to ACMG guidelines, seven of the fifteen variants were classified as LP and six variants as P, resulting in an overall burden of somatic variants of 24.1% in our patient cohort. The two remaining variants had insufficient evidence to be classified as LP or P and were therefore classified as VUS and excluded from the variant burden (Supplementary Table 3). The highest incidence of variants was observed in patients with LEAT (41.67%), compared with FCDII (13.34%) or HS (6.67%; Fig. 1). The somatic AAF of LP or P variants ranged from 2.7 to 37.4% with highest AAFs in tumor tissue (tumor median 16.45%, SD = 11.17 vs FCD/HS median 4.3%, SD = 0.52; Table 1). Seven LP/P variants have been reported previously in either FCDII or DNT; another three LP/P have been reported in a different disease condition (Table 1). Three LP variants were never reported before and extend the spectrum of variants associated with these pathologies (NPRL3 NM_001077350.2:c.682_683dup (p.(S228Rfs*16))) in patient 3 with FCDII; NF1 (NM_000267.3:c.2674del (p.(S892Afs*10))) in patient 2 with HS; BRAF (NM_004333.5:c.1518_1526dup) in patient 14 with GG; Table 1).
Table 1.
Likely pathogenic and pathogenic somatic variants identified in patients with epileptic brain lesions
| Patient | Lesion | N | Somatic variant | AAF [%] | Associated disease | ACMG classification | Reference |
|---|---|---|---|---|---|---|---|
| Patient 3 | FCDIIA | 1 | NPRL3 NM_001077350.2:c.682_683dup p.(S228Rfs*16) | 20/443 [4.5] | – | LP | – |
| Patient 5 | FCDIIB | 1 | MTOR NM_004958.3:c.5930C>A p.(T1977K) | 8/240 [3.3] | FCD/HME | P | [42, 45] |
| Patient 6 | DNT | 1 | FGFR1 NM_023110.2:c.1966A>G p.(K656E) | 125/334 [37.4] | DNT | LP | [10] |
| Patient 7 | DNT | 1 | FGFR1 NM_023110.2:c.1966_1968delinsGAC p.(K656D) | 64/212 [30.2] | PA | LP | [46] |
| Patient 8 | DNT | 1 | DNMT3A NM_175629.2:c.2141C>G p.(S714C) | 51/449 [11.4] | AML | LP | [47] |
| Patient 9–13 | GG | 5 | BRAF NM_004333.5:c.1799T>A p.(V600E) | 16/199–474/1337 [8.04–35.5] | PXA/GG/DNT/DIA/DIG | P | [48] |
| Patient 14 | GG | 1 | BRAF NM_004333.5:c.1518_1526dup | 26/318 [8.2] | – | LP | – |
| Patient 15 | HS+GG | 1 | KRAS NM_004985.5:c.40 G>A p.(V14I) | 28/1048 [2.7] | NS/melanoma/carcinoma/neoplasm | LP | [49–52] |
| Patient 2 | HS | 1 | NF1 NM_000267.3:c.2674del p.(S892Afs*10) | 25/569 [4.4] | – | LP | – |
N number of patients carrying the variant, AAF Somatic alternate allele fraction, LP likely pathogenic, P pathogenic according to latest American College of Medical Genetics and Genomics (ACMG) guidelines, FCDII focal cortical dysplasia type II, HME hemimegalencephaly, DNT dysembryoplastic neuroepithelial tumor, NF1 neurofibromatosis type I, PA pilocytic astrocytoma, AML acute myeloid leukemia, PXA pleomorphic xanthoastrocytoma, GG ganglioglioma, DIA desmoplastic infantile astrocytoma, DIG desmoplastic infantile ganglioglioma, NS Noonan syndrome
Fig. 1.
Likely pathogenic and pathogenic somatic variant burden in patients with epilepsy-associated brain lesions. a Number of patients carrying somatic variants in low-grade epilepsy-associated tumors (LEATs), focal cortical dysplasia type II (FCDII) and hippocampal sclerosis (HS). b Genes carrying likely pathogenic or pathogenic somatic variants
The variants observed in FCDII were previously recognized as members of the PI3K-AKT-mTOR pathway (patients 3, 5). All ten variants detected in tumor tissues occurred in known tumor genes (patients 6–15; Table 1; Fig. 1b). The known BRAF p.V600E (NM_004333.5:c.1799T>A) variant was found in 1/3 of the GG patients (patients 9–13). The variant observed in patient 2 with HS affects the tumor gene NF1. NF1 has been reported to interact with the PI3K-AKT-mTOR pathway [39].
Discussion
Up to date, few studies reliably assessed the prevalence of variants and genotype–phenotype correlations in patients with epileptic brain lesions. An accurate estimation is further challenged by the selection of specific lesion subtypes and targeted genes, as well as the spectrum of applied variant discovery technologies. In our current approach including four major epileptogenic brain lesions, we identified LP and pathogenic somatic and germline variants in 41.67% of patients with brain tumors (LEAT), 20% in FCDIIs, and 6.7% in HS. We did not detect variants in 50 established epileptic encephalopathy or genetic generalized epilepsy germline variant-associated genes. Furthermore, we confirmed the genotype–phenotype correlation for LP/P variants in PI3K-AKT-mTOR pathway genes in FCDII patients and oncogenes in LEAT patients. We did not validate the variants experimentally.
Despite the use of an extensive panel of 161 genes and a careful microscopic preselection of lesional tissue, our LP/P variant burden was at the lower edge of previously published rates of 6–46% in patients with FCDII [6]. This highlights all current challenges in genetic research of brain tissue samples. The affected neuronal (or glial) cell population may be smaller than anticipated and unevenly distributed in a given tissue specimen. This so-called “mutation gradient” could potentially compromise the sensitivity of the somatic variant detection and might miss causal mutations when comparing paired brain lesion tissue with adjacent brain tissue [40, 41]. A single cell approach may help to address these issues [42]. The depth of sequencing, selection of gene panels and stringency to filter and call variants will also need careful consideration to increase the variant detection rate. We propose, therefore, to apply whole exome and ultra-deep sequencing for future research projects in order to further characterize the spectrum of affected genes and to develop a diagnostically meaningful gene panel with a sufficiently high yield of >80%.
Our LP/P variant burden in LEAT was within the broad spectrum of reported findings with a BRAF p.V600E variant described in 18–56% of GG and 0–50% of DNT [4]. Differences in sequencing technologies, but firstly also different histopathological classification schemes of this difficult-to-classify tumor category are likely to play a role [4]. However, targeted development of drugs, such as the approved inhibitor of mutated BRAF V600E, Vemurafenib [43], will open intriguing therapeutic options for personalized medicine in the near future, i.e., pediatric LEAT not amenable for complete surgical resection.
Here, we identify genetic variants potentially involved in the disease etiology of HS. A germline MTOR variant and a somatic loss-of-function variant in NF1 were found in HS patient 2 with automotor and secondary generalized tonic clonic seizures and cognitive impairment (Supplementary Table 4). The combination of a germline and somatic variant suggested a possible role of somatic mosaicism and a second hit mechanism for this disease category although sufficient evidence for the pathogenicity of the MTOR variant is still lacking. NF1 was identified to function as a critical regulator of TSC2 and the PI3K-AKT-mTOR pathway in the absence of growth factors [39]. Hyperactivation of the PI3K-AKT-mTOR pathway has been reported in the sclerotic hippocampus of 13 temporal lobe epilepsy patients [44], supporting both genes as plausible candidates for association with epileptogenic brain lesions what will need further clarification. We did not detect a second pathogenic variant neither germline nor somatic for any of our patients.
In conclusion, we observed a LP/P variant burden of 25.9% in major epileptic brain lesions with gene panel testing. We also identified substantial genetic heterogeneity and specified genotype–phenotype correlations. As of today, genetic testing is already introduced into the integrated phenotype–genotype WHO classification of brain tumors, and is increasingly recognized as valuable basis for personalized therapy. Its use in the arena of epileptology is still lacking behind. However, increasing use of genetic testing in brain tissue obtained from epilepsy surgery will foster our understanding of disease etiologies, and eventually also help to develop biomarker for outcome measures. However, continuous lack of P and LP variants in samples with same histological phenotypes call for advanced technological approaches including deep sequencing at the single-neuronal and glial cell level in the diagnosis of FCD, LEAT, and HS patients.
Supplementary information
Acknowledgements
We thank all participants and their families for participating in this study.
Compliance with ethical standards
Conflict of interest
This study was supported by the UoC Postdoc Grant program at the University of Cologne, Germany, the University Hospital Erlangen, Germany, the Epilepsy Center Frankfurt Rhine-Main, Germany and the University Hospital Tübingen, Germany.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ingmar Blümcke, Phone: +09131 85-26031, Email: ingmar.bluemcke@uk-erlangen.de.
Dennis Lal, Phone: +(216) 444 6701, Email: lald@ccf.org.
Supplementary information
The online version of this article (10.1038/s41431-019-0484-4) contains supplementary material, which is available to authorized users.
References
- 1.WHO. Epilepsy fact sheet 2017. WHO http://www.who.int/mediacentre/factsheets/fs999/en/.
- 2.Blumcke I, Spreafico R, Haaker G, Coras R, Kobow K, Bien CG, et al. Histopathological findings in brain tissue obtained during epilepsy surgery. N Engl J Med. 2017;377:1648–56. doi: 10.1056/NEJMoa1703784. [DOI] [PubMed] [Google Scholar]
- 3.Blumcke I, Thom M, Aronica E, Armstrong DD, Bartolomei F, Bernasconi A, et al. International consensus classification of hippocampal sclerosis in temporal lobe epilepsy: a task force report from the ILAE commission on diagnostic methods. Epilepsia. 2013;54:1315–29. doi: 10.1111/epi.12220. [DOI] [PubMed] [Google Scholar]
- 4.Blumcke I, Aronica E, Becker A, Capper D, Coras R, Honavar M, et al. Low-grade epilepsy-associated neuroepithelial tumours—the 2016 WHO classification. Nat Rev Neurol. 2016;12:732–40. doi: 10.1038/nrneurol.2016.173. [DOI] [PubMed] [Google Scholar]
- 5.Blumcke I, Thom M, Aronica E, Armstrong DD, Vinters HV, Palmini A, et al. The clinico-pathological spectrum of focal cortical dysplasias: a consensus classification proposed by an ad hoc Task Force of the ILAE Diagnostic Methods Commission. Epilepsia. 2011;52:158–74. doi: 10.1111/j.1528-1167.2010.02777.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marsan E, Baulac S. Review: mechanistic target of rapamycin (mTOR) pathway, focal cortical dysplasia and epilepsy. Neuropathol Appl Neurobiol. 2018;44:6–17. doi: 10.1111/nan.12463. [DOI] [PubMed] [Google Scholar]
- 7.Pekmezci M, Villanueva-Meyer JE, Goode B, Van Ziffle J, Onodera C, Grenert JP, et al. The genetic landscape of ganglioglioma. Acta Neuropathol Commun. 2018;6:47. doi: 10.1186/s40478-018-0551-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.French JA, Lawson JA, Yapici Z, Ikeda H, Polster T, Nabbout R, et al. Adjunctive everolimus therapy for treatment-resistant focal-onset seizures associated with tuberous sclerosis (EXIST-3): a phase 3, randomised, double-blind, placebo-controlled study. Lancet. 2016;388:2153–63. doi: 10.1016/S0140-6736(16)31419-2. [DOI] [PubMed] [Google Scholar]
- 9.Qaddoumi I, Orisme W, Wen J, Santiago T, Gupta K, Dalton JD, et al. Genetic alterations in uncommon low-grade neuroepithelial tumors: BRAF, FGFR1, and MYB mutations occur at high frequency and align with morphology. Acta Neuropathol. 2016;131:833–45. doi: 10.1007/s00401-016-1539-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rivera B, Gayden T, Carrot-Zhang J, Nadaf J, Boshari T, Faury D, et al. Germline and somatic FGFR1 abnormalities in dysembryoplastic neuroepithelial tumors. Acta Neuropathol. 2016;131:847–63. doi: 10.1007/s00401-016-1549-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Epi PMC. A roadmap for precision medicine in the epilepsies. Lancet Neurol. 2015;14:1219–28. doi: 10.1016/S1474-4422(15)00199-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rolls A, Shechter R, London A, Ziv Y, Ronen A, Levy R, et al. Toll-like receptors modulate adult hippocampal neurogenesis. Nat Cell Biol. 2007;9:1081–8. doi: 10.1038/ncb1629. [DOI] [PubMed] [Google Scholar]
- 13.Fukata Y, Adesnik H, Iwanaga T, Bredt DS, Nicoll RA, Fukata M. Epilepsy-related ligand/receptor complex LGI1 and ADAM22 regulate synaptic transmission. Science. 2006;313:1792–5. doi: 10.1126/science.1129947. [DOI] [PubMed] [Google Scholar]
- 14.Ariani F, Hayek G, Rondinella D, Artuso R, Mencarelli MA, Spanhol-Rosseto A, et al. FOXG1 is responsible for the congenital variant of Rett syndrome. Am J Hum Genet. 2008;83:89–93. doi: 10.1016/j.ajhg.2008.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barkovich AJ, Guerrini R, Kuzniecky RI, Jackson GD, Dobyns WB. A developmental and genetic classification for malformations of cortical development: update 2012. Brain. 2012;135:1348–69. doi: 10.1093/brain/aws019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basel-Vanagaite L, Sarig O, Hershkovitz D, Fuchs-Telem D, Rapaport D, Gat A, et al. RIN2 deficiency results in macrocephaly, alopecia, cutis laxa, and scoliosis: MACS syndrome. Am J Hum Genet. 2009;85:254–63. doi: 10.1016/j.ajhg.2009.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Budny B, Chen W, Omran H, Fliegauf M, Tzschach A, Wisniewska M, et al. A novel X-linked recessive mental retardation syndrome comprising macrocephaly and ciliary dysfunction is allelic to oral-facial-digital type I syndrome. Hum Genet. 2006;120:171–8. doi: 10.1007/s00439-006-0210-5. [DOI] [PubMed] [Google Scholar]
- 18.Hevner RF. The cerebral cortex malformation in thanatophoric dysplasia: neuropathology and pathogenesis. Acta Neuropathol. 2005;110:208–21. doi: 10.1007/s00401-005-1059-8. [DOI] [PubMed] [Google Scholar]
- 19.Lin YX, Lin K, Liu XX, Kang DZ, Ye ZX, Wang XF, et al. PI3K-AKT pathway polymerase chain reaction (PCR) array analysis of epilepsy induced by type II focal cortical dysplasia. Genet Mol Res. 2015;14:9994–10000. doi: 10.4238/2015.August.21.5. [DOI] [PubMed] [Google Scholar]
- 20.Lopez-Hernandez T, Sirisi S, Capdevila-Nortes X, Montolio M, Fernandez-Duenas V, Scheper GC, et al. Molecular mechanisms of MLC1 and GLIALCAM mutations in megalencephalic leukoencephalopathy with subcortical cysts. Hum Mol Genet. 2011;20:3266–77. doi: 10.1093/hmg/ddr238. [DOI] [PubMed] [Google Scholar]
- 21.Matsuda T, Murao N, Katano Y, Juliandi B, Kohyama J, Akira S, et al. TLR9 signalling in microglia attenuates seizure-induced aberrant neurogenesis in the adult hippocampus. Nat Commun. 2015;6:6514. doi: 10.1038/ncomms7514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lecourtois M, Poirier K, Friocourt G, Jaglin X, Goldenberg A, Saugier-Veber P, et al. Human lissencephaly with cerebellar hypoplasia due to mutations in TUBA1A: expansion of the foetal neuropathological phenotype. Acta Neuropathol. 2010;119:779–89. doi: 10.1007/s00401-010-0684-z. [DOI] [PubMed] [Google Scholar]
- 23.Fassunke J, Majores M, Tresch A, Niehusmann P, Grote A, Schoch S, et al. Array analysis of epilepsy-associated gangliogliomas reveals expression patterns related to aberrant development of neuronal precursors. Brain. 2008;131:3034–50. doi: 10.1093/brain/awn233. [DOI] [PubMed] [Google Scholar]
- 24.Appin CL, Brat DJ. Molecular pathways in gliomagenesis and their relevance to neuropathologic diagnosis. Adv Anat Pathol. 2015;22:50–8. doi: 10.1097/PAP.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 25.Chappe C, Padovani L, Scavarda D, Forest F, Nanni-Metellus I, Loundou A, et al. Dysembryoplastic neuroepithelial tumors share with pleomorphic xanthoastrocytomas and gangliogliomas BRAF(V600E) mutation and expression. Brain Pathol. 2013;23:574–83. doi: 10.1111/bpa.12048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoischen A, Ehrler M, Fassunke J, Simon M, Baudis M, Landwehr C, et al. Comprehensive characterization of genomic aberrations in gangliogliomas by CGH, array-based CGH and interphase FISH. Brain Pathol. 2008;18:326–37. doi: 10.1111/j.1750-3639.2008.00122.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yamada S, Kipp BR, Voss JS, Giannini C, Raghunathan A. Combined “Infiltrating Astrocytoma/Pleomorphic Xanthoastrocytoma” Harboring IDH1 R132H and BRAF V600E Mutations. Am J Surg Pathol. 2016;40:279–84. doi: 10.1097/PAS.0000000000000515. [DOI] [PubMed] [Google Scholar]
- 28.Li X, Wei J, Liu Y, Li P, Fan L, Wang Y, et al. Primary astrocytic tumours and paired recurrences have similar biological features in IDH1, TP53 and TERTp mutation and MGMT, ATRX Loss. Sci Rep. 2017;7:13038. doi: 10.1038/s41598-017-13272-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McKenna A, Hanna M, Banks E, Sivachenko A, Cibulskis K, Kernytsky A, et al. The genome analysis toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010;20:1297–303. doi: 10.1101/gr.107524.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, et al. The sequence alignment/map format and SAMtools. Bioinformatics. 2009;25:2078–9. doi: 10.1093/bioinformatics/btp352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Albers CA, Lunter G, MacArthur DG, McVean G, Ouwehand WH, Durbin R. Dindel: accurate indel calls from short-read data. Genome Res. 2011;21:961–73. doi: 10.1101/gr.112326.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang H, Wang K. Genomic variant annotation and prioritization with ANNOVAR and wANNOVAR. Nat Protoc. 2015;10:1556–66. doi: 10.1038/nprot.2015.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016;536:285–91. doi: 10.1038/nature19057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cibulskis K, Lawrence MS, Carter SL, Sivachenko A, Jaffe D, Sougnez C, et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat Biotechnol. 2013;31:213–9. doi: 10.1038/nbt.2514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim S, Scheffler K, Halpern AL, Bekritsky MA, Noh E, Kallberg M, et al. Strelka2: fast and accurate calling of germline and somatic variants. Nat Methods. 2018;15:591–4. doi: 10.1038/s41592-018-0051-x. [DOI] [PubMed] [Google Scholar]
- 36.Wang K, Li M, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 2010;38:e164. doi: 10.1093/nar/gkq603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24. doi: 10.1038/gim.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li Q, Wang K. InterVar: clinical interpretation of genetic variants by the 2015 ACMG-AMP guidelines. Am J Hum Genet. 2017;100:267–80. doi: 10.1016/j.ajhg.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Johannessen CM, Reczek EE, James MF, Brems H, Legius E, Cichowski K. The NF1 tumor suppressor critically regulates TSC2 and mTOR. Proc Natl Acad Sci USA. 2005;102:8573–8. doi: 10.1073/pnas.0503224102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mirzaa GM, Campbell CD, Solovieff N, Goold CP, Jansen LA, Menon S, et al. Association of MTOR mutations with developmental brain disorders, including megalencephaly, focal cortical dysplasia, and pigmentary mosaicism. JAMA Neurol. 2016;73:836–45. doi: 10.1001/jamaneurol.2016.0363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ribierre T, Deleuze C, Bacq A, Baldassari S, Marsan E, Chipaux M, et al. Second-hit mosaic mutation in mTORC1 repressor DEPDC5 causes focal cortical dysplasia-associated epilepsy. J Clin Investig. 2018;128:2452–8. doi: 10.1172/JCI99384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.D’Gama AM, Woodworth MB, Hossain AA, Bizzotto S, Hatem NE, LaCoursiere CM, et al. Somatic mutations activating the mtor pathway in dorsal telencephalic progenitors cause a continuum of cortical dysplasias. Cell Rep. 2017;21:3754–66. doi: 10.1016/j.celrep.2017.11.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.del Bufalo F, Carai A, Figa-Talamanca L, Pettorini B, Mallucci C, Giangaspero F, et al. Response of recurrent BRAFV600E mutated ganglioglioma to Vemurafenib as single agent. J Transl Med. 2014;12:356. doi: 10.1186/s12967-014-0356-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sha LZ, Xing XL, Zhang D, Yao Y, Dou WC, Jin LR, et al. Mapping the spatio-temporal pattern of the mammalian target of rapamycin (mTOR) activation in temporal lobe epilepsy. PLoS One. 2012;7:e39152. doi: 10.1371/journal.pone.0039152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lim JS, Kim WI, Kang HC, Kim SH, Park AH, Park EK, et al. Brain somatic mutations in MTOR cause focal cortical dysplasia type II leading to intractable epilepsy. Nat Med. 2015;21:395–400. doi: 10.1038/nm.3824. [DOI] [PubMed] [Google Scholar]
- 46.Jones DT, Hutter B, Jager N, Korshunov A, Kool M, Warnatz HJ, et al. Recurrent somatic alterations of FGFR1 and NTRK2 in pilocytic astrocytoma. Nat Genet. 2013;45:927–32. doi: 10.1038/ng.2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Russler-Germain DA, Spencer DH, Young MA, Lamprecht TL, Miller CA, Fulton R, et al. The R882H DNMT3A mutation associated with AML dominantly inhibits wild-type DNMT3A by blocking its ability to form active tetramers. Cancer Cell. 2014;25:442–54. doi: 10.1016/j.ccr.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dahiya S, Emnett RJ, Haydon DH, Leonard JR, Phillips JJ, Perry A, et al. BRAF-V600E mutation in pediatric and adult glioblastoma. Neuro Oncol. 2014;16:318–9. doi: 10.1093/neuonc/not146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Irving J, Matheson E, Minto L, Blair H, Case M, Halsey C, et al. Ras pathway mutations are prevalent in relapsed childhood acute lymphoblastic leukemia and confer sensitivity to MEK inhibition. Blood. 2014;124:3420–30. doi: 10.1182/blood-2014-04-531871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McConechy MK, Ding J, Cheang MC, Wiegand K, Senz J, Tone A, et al. Use of mutation profiles to refine the classification of endometrial carcinomas. J Pathol. 2012;228:20–30. doi: 10.1002/path.4056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schubbert S, Zenker M, Rowe SL, Boll S, Klein C, Bollag G, et al. Germline KRAS mutations cause Noonan syndrome. Nat Genet. 2006;38:331–6. doi: 10.1038/ng1748. [DOI] [PubMed] [Google Scholar]
- 52.Siroy AE, Boland GM, Milton DR, Roszik J, Frankian S, Malke J, et al. Beyond BRAF(V600): clinical mutation panel testing by next-generation sequencing in advanced melanoma. J Investig Dermatol. 2015;135:508–15. doi: 10.1038/jid.2014.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.