Abstract
A model to explain the orientation selectivity of the neurophysiologic effects of electric‐field transients applied to cerebral cortex is proposed and supported with neuroimaging evidence. Although it is well known that transcranial magnetic stimulation (TMS) excites cerebral cortex in an orientation‐selective manner, a neurophysiologically compelling explanation of this phenomenon has been lacking. It is generally presumed that TMS‐induced excitation is mediated by horizontal fibers in the cortical surfaces nearest to the stimulating coil, i.e., at the gyral crowns. No evidence exists, however, that horizontal fibers are orientation selective either anatomically or physiologically. We used positron emission tomography to demonstrate that TMS‐induced cortical activation is selectively sulcal. This observation allows the well‐established columnar organization of cerebral cortex to be invoked to explain the observed orientation selectivity. In addition, Rushton's cosine principle can used to model stimulation efficacy for an electrical field applied at any cortical site at any intensity and in any orientation. Hum. Brain Mapp. 22:1–16, 2004. © 2004 Wiley‐Liss, Inc.
Keywords: cerebral cortex, transcranial magnetic stimulation, TMS, positron emission tomography, PET
INTRODUCTION
Transcranial magnetic stimulation (TMS) excites neurons in cerebral cortex via electrical currents induced in the cortex by the rapidly changing applied magnetic field. For electrical stimulation, it has been well established that neurons are excited at lower thresholds when applied voltages induce currents oriented longitudinally (along the axon) rather than transversely (across the axon) [Day, 1989; Phillips and Porter, 1962; Ranck, 1975; Rushton, 1927]. In cerebral cortex, the threshold for TMS excitation is also sensitive to orientation [Brasil‐Neto et al., 1992; Mills et al., 1992], with certain orientations being reliably more effective than others. The orientation selectivity of cortical responsivity to TMS is most parsimoniously presumed to derive from the well‐documented orientation selectivity of the response of cortical neurons (isolated and in vivo) to applied currents. Greater and lesser degrees of excitation indicate that induced electrical currents are aligned more longitudinally (greater excitation) or more transversely (less excitation) relative to the neural elements being affected. Which neural components of the cerebral cortex are excited by TMS, however, has not been explained adequately. Our purpose was to infer the orientation (horizontal or vertical) of TMS‐excited neural elements in cerebral cortex using functional and anatomic imaging to observe the location and orientation of the cortical surfaces showing TMS‐induced activation.
The clearest demonstrations of the orientation selectivity of cerebral cortex to magnetic stimulation are those Mills et al. [1992] and Brasil‐Neto et al. [1992]. The methodological similarity employed in these concurrent reports is striking. TMS was applied to the hand representation of primary motor cortex (M1‐hand), cortical response magnitude was quantified by electromyographic (EMG) response in the first dorsal interosseous muscle (FDI), and TMS was delivered with a B‐shaped coil placed flat against the scalp and tested at 45‐degree increments through a full circle. A B‐shaped coil was used because induced currents are effectively linear, being strongest at the short, straight segment where the two loops of the “B” meet. The induced current parallels the current in the coils, being tangential to the scalp at the stimulated site. A clear orientation preference was observed, namely, the optimal response was observed when the induced current was oriented ∼45 degrees medial to the anteroposterior plane. Although neither study employed anatomic imaging to confirm the underlying surface anatomy, both groups interpreted this orientation as indicating that optimal stimulation of primary motor cortex was achieved when the induced current was perpendicular to the central sulcus. Surprisingly, neither group interpreted this orientation selectivity as being due to alignment of the applied current with the orientation of the columns (surface normal) of the motor cortex lying in the central sulcus. Both instead based their interpretation on a prior study by Day et al. [1989].
Day et al. [1989] accepted the principle that “a voltage gradient parallel to the long axis of the neuron is the most favorable” for neuronal excitation by electrical or magnetic stimulation. Nevertheless, in the context of a comparison between magnetic and electrical transcranial stimulation of primary motor cortex, Day et al. argued that “all forms of stimulation are most likely to activate those neurons nearest the stimulating electrode…” [Day et al., 1989]. In the case of magnetic stimulation of primary motor cortex (also studied here), they postulated that a magnetic field would penetrate only far enough to excite neurons “on the convexity of the precentral gyrus,” rather than on the sulcal bank, the location of the great preponderance of pyramidal neurons. Because TMS coils are flat and placed tangential to the scalp, the induced current is also tangential to the scalp and at the crown of the gyrus would be in a plane horizontal to the radial alignment of the cortical columns. Accordingly, Day et al. [1989] hypothesized that TMS stimulation must be exciting the tangentially oriented neural elements at the gyral crown, such as horizontal interneurons or horizontal collaterals of pyramidal track axons. This inference is based entirely on the assumption that TMS‐induced excitation occurs at the cortical surface closest to the stimulation coil. They hypothesized that proximity to the coil (strength of the induced electrical current) will outweigh all other factors [Day et al., 1989].
Although the postulate of TMS being selective for gyral crowns [Day et al., 1989] was not inherently unreasonable, it is difficult to maintain this assumption in the face of the orientation selectivity observed by Mills et al. [1992] and Brasil‐Neto et al. [1992]. Horizontal fibers are isotropic, extending uniformly in all directions within a plane parallel to the cortical surface. The isotropism of the horizontal fibers should translate into a lack of a preferred orientation for TMS, as the induced current should excite an equivalent fraction of the total horizontal‐fiber population in any orientation. Both of the above research groups recognized that isotropically distributed horizontal fibers cannot explain the observed orientation effect. Both, however, accepted Day et al.'s [1989] hypothesis of selective activation of the nearest cortical surface (gyral crowns). They were obligated, therefore, to posit some mechanism for the orientation selectivity they had observed. Mills et al. [1992] speculated that horizontal fibers might have an anatomic orientation preference, tending to lie at right angles to the central sulcus. Brasil‐Neto et al. [1992], on the other hand, postulated a functional preference, “horizontal interneurons which are aligned perpendicular to the central sulcus are preferentially activated by magnetic stimuli.” No empirical data were provided to support either postulate.
If the assumption of Day et al. [1989] that scalp‐applied magnetic fields lack the strength to excite sulcal neurons is wrong, and TMS‐induced currents are directly exciting sulcal cortex, the orientation selectivity observed by Mills et al. [1992] and Brasil‐Neto et al. [1992] is explained readily by invoking the well‐established columnar neuronal orientation and functional organization of cerebral cortex. In other words, the greatest excitation was achieved when the induced current was longitudinally aligned with respect to the cortical columns (normal to the sulcal surface) and declined as the angle relative to the columns became more transverse. A straightforward means to test this alternative hypothesis regarding the orientation selectivity reported by Mills et al. [1992] and Brasil‐Neto et al. [1992] is to use functional and anatomic neuroimaging in combination with TMS to observe the cortical location (sulcal versus gyral) of TMS‐induced activations, which is the purpose of the present study.
SUBJECTS AND METHODS
Subjects
Twelve, right‐handed, normal volunteers (6 men, 6 women; mean age, 35 years; age range, 22–43 years) participated in the study. All subjects were healthy (no medical, neurologic, or psychiatric illness) and taking no medications. For each subject, normal brain anatomy was confirmed by anatomic magnetic resonance imaging (MRI). Informed consent was obtained from all subjects in accordance with the declaration of Helsinki and under the auspices of the Institutional Review Board and Radiation Safety Committee of the University of Texas Health Science Center at San Antonio. The use of TMS at 3 Hz was approved by the US FDA (IDE K905059D held by Peter Fox). One subject was dropped from the study after data acquisition, due to excessive head‐motion artifacts.
TMS Procedures
TMS was delivered with a water‐cooled, B‐shaped coil (Cadwell Inc., Kennewick, WA). A water‐cooled coil was required to prevent overheating and failure‐to‐fire at the rate (3 Hz) and intensities required during imaging. The coil was powered by a Cadwell HSMS unit, which delivers a triphasic electric pulse with a total duration of 240 μsec and a peak E field of 435 V/m at 100% of machine output at the coil surface. Before imaging, while finding the location and threshold of the M1 hand region, the TMS coil was handheld. During imaging, the TMS coil was held in position with a robotic TMS delivery system (Fig. 1), based on a NeuroMate neurosurgical robot (ISS, Sacramento, CA).
Figure 1.
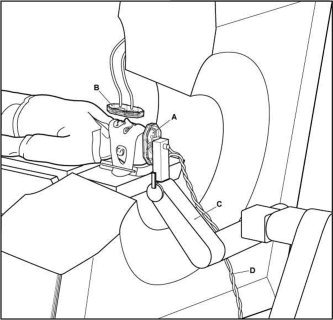
Experimental preparation. The subject is immobilized in the PET scanner with a thermoplastic mask. The stimulating coil (A) is held by a NeuroMate robot (C) customized in‐house for this purpose. A second coil (B) was used to deliver sham stimulation, an auditory control. The rate of stimulation used (3 Hz) required a water‐cooled coil with waterlines (D).
The optimal location and orientation of the TMS coil for stimulation of the primary motor cortex representation of the intrinsic muscles of the right hand (M1‐hand) was identified before imaging and recorded. Location was established first, with the coil oriented to aim the induced current 45 degrees medial to the anteroposterior plane, in the manner prescribed by Mills et al. [1992] and Brasil‐Neto et al. [1992]. In this orientation, the location eliciting palpable contractions of the first dorsal interosseous muscle (FDI) at the lowest threshold was determined. Orientation was then optimized. At the optimal orientation, location was re‐optimized. At this optimal location‐orientation combination, the motor threshold was determined, being defined as the intensity that elicited barely palpable contractions of the FDI on half the trials, when stimulating at ≤0.3 Hz. The optimal location‐orientation combination was marked in ink on a tightly fitted elastic cap, worn by the subject throughout the study. The cap marking was used to guide robotic positioning once the subject was immobilized within the positron emission tomography (PET) camera. (For motor threshold values for all 11 subjects, see Table IV.)
Table IV.
TMS stimulation intensity
| Group | % Output | E at scalp (V/m) | M1 depth (mm) | E at M1 (V/m)* |
|---|---|---|---|---|
| PET Responders | ||||
| 1246 | 80 | 348 | 38 | 87 |
| 1265 | 66 | 284 | 26 | 96 |
| 1280 | 75 | 325 | 37 | 73 |
| 1281 | 72 | 312 | 27 | 125 |
| 1286 | 55 | 235 | 31 | 66 |
| 1316 | 72 | 312 | 22 | 137 |
| 1355 | 62 | 267* | 29 | 73 |
| Mean | 68.9 | 297.8 | 29.9 | 94.1 |
| Non‐responders | ||||
| 1266 | 62 | 270 | 29 | 87 |
| 1285 | 75 | 326 | 21 | 120 |
| 1328 | 72 | 269 | 32 | 91 |
| 1329 | 70 | 304 | 44 | 87 |
| Mean | 67.3 | 292.5 | 27.3 | 96.1 |
There was no difference in intensity of the applied E field between subjects in whom a cortical response to TMS was observed with PET (n = 7) and those in whom a cortical response to transcranial magnetic stimulation (TMS) was not observed with PET (n = 4). % Output, percentage of maximum output of the coil. E, E fields; M1 depth, depth of M1 response to voluntary finger movement from the scalp surface.
E at M1 is the absolute E field at the depth of M1.
TMS was delivered at a rate of 3 Hz and at an intensity of 125% of the motor threshold of left M1‐hand. This rate was used because pilot studies demonstrated that rates of 0.5 Hz and 1 Hz were unreliable in giving M1 excitation detected by PET. This intensity was used to give a readily detectable contraction of the FDI on all trials, to ensure a robust cortical response would be detected by PET and to make the TMS state comparable to the voluntary movement state in rate and finger excursion. As the control state for voxel‐wise image contrasts, sham TMS (illustrated in Fig. 1) was delivered. True TMS was delivered with a TMS coil mounted to the tool‐holding apparatus of the NeuroMate. Sham TMS was delivered with a coil mounted to the final limb of the NeuroMate, parallel to and approximately 12 inches behind the treatment coil. For sham TMS, the percent output of the Cadwell HSVS was adjusted until the sound level measured at the external auditory meatus was the same in each ear and the same as that during the TMS condition. Other stimulation conditions were acquired in each session and will be reported separately.
Imaging Conditions
Each subject underwent two trials of TMS at 125% of the motor threshold value, two trials of sham TMS, and two trials of finger movement. For the true TMS conditions, TMS was applied at the location determined previously to be the left hemisphere M1 FDI representation. Finger movement consisted of self‐paced tapping of the thumb and index finger of the right hand. Subjects were instructed to approximate the rate of TMS stimulation (3 Hz). Sham TMS was delivered during finger movement, as an auditory control. TMS was started 120 sec before tracer injection and continued through the first 40 sec of a 90‐sec image acquisition. The 2‐min stimulation before tracer injection was intended to take advantage of the progressive augmentation of the cortical response reported by Fox et al. [1997].
Image Acquisition
Subjects were scanned using a GE‐4096WB camera (pixel spacing 2 mm, spatial resolution 6.5 mm full width at half maximum [FWHM] in the axial plane, inter‐plane center to center distance 6.5 mm, scan planes 15, z axis field of view [FOV] 10.5 cm). Contrary to the recommendations of Thompson et al. [1998], mu metal shielding was not employed, as this has been shown to be unnecessary [Fox et al., 1997; Lee et al., 2003; Speer et al., 2003]. Transmission scans using a Ge‐68/Ga‐68 source were used for calculating regional attenuation correction coefficients. Brain blood flow was measured using [15O] water, administered as an intravenous bolus of 8–10 ml saline containing 50–70 mCi per injection, tailored to obtain satisfactory coincidence detection rates. A 40‐sec scan was triggered as the tracer bolus entered the brain; TMS, sham TMS, or hand movement accompanied this scan segment. A 50‐sec scan immediately followed the 40‐sec scan, during which TMS, sham TMS or hand movement were not carried out. The averaged data from the 40‐sec and the 50‐sec scans were used for all further analysis. Interscan intervals of at least 10 min were used to permit isotope decay (five physical half‐lives) and to reestablish baseline levels of blood flow in the brain. Throughout the PET session, subjects' heads were immobilized with an individually fitted, thermoplastic facial mask. To minimize auditory activation induced by the TMS, foam earplugs were worn throughout the imaging study.
Anatomic MRI was acquired in each subject and used to optimize spatial normalization. MR imaging was carried out on the 1.9‐Tesla, Elscint Prestige using a high‐resolution, 3‐D GRASS sequence (TR = 33 msec; TE= 12 msec; flip angle = 60 degrees; voxel size = 1 mm3; matrix size = 256 × 192 × 192).
Electromyographic Acquisition and Processing
Electromyographic (EMG) recordings were obtained from the FDI and flexor digitorum communis of the upper limb contralateral to TMS stimulation. EMG was recorded with a Synamp 1.0 ERP recording system and processed with the Scan 4.0 software (Neuroscan, El Paso, TX). EMG was obtained throughout the period of TMS delivery. EMG data were analyzed only for the 40‐sec interval during imaging that TMS was applied. EMG was rectified and quantified as baseline‐to‐peak amplitude. Latency was obtained both for response onset and response peak.
Image Preprocessing
Images were reconstructed into 60 slices, each of a 2‐mm thickness and with an image matrix size of 60 × 128 × 128, using a 5‐mm Hann filter resulting in images with a spatial resolution of approximately 7 mm (FWHM). PET images were value normalized to a whole‐brain mean of 1,000. PET and MRI data were co‐registered using the Convex Hull algorithm [Lancaster et al., 1999]. MRI data were spatially normalized using Spatial Normalization (SN) [Lancaster et al., 1995] and OSN algorithms [Kochunov et al., 1999] in series. The SN algorithm carried out “global” (9‐parameter) spatial normalization, which registered each subject to the target shape provided by the Talairach and Tournoux [1988] atlas. In this atlas space, locations are expressed as millimeter coordinates referenced to the anterior commissure as origin, with right, superior and anterior directions being positive. The OSN algorithm carried out “local” spatial normalization, in which each subject's brain was anatomically deformed to match the median of the group in a high‐resolution (1 mm3), fully 3D (each image voxel provides three deformation vectors) manner. Octree SN (OSN) processing was used to optimize registration of anatomical features (and thereby functional areas) across subjects. OSN‐derived deformation fields were applied to the PET data before computation of statistical parametric images (SPIs).
Statistical Parametric Images
Image analysis was based on statistical parametric images (SPI). All SPI were voxel‐wise computations of Z‐score (SPI[z]), contrasting task state with control state (sham TMS). The primary objective of the analysis was to determine the locations of the left hemisphere M1‐hand response induced by TMS and that induced by finger movement both relative to sulcal anatomy and relative to standardized coordinates. A group SPI(z) (n = 11) was created for the finger‐movement condition (vs. control), which showed a very robust response in the M1‐hand region for finger movement. The group‐mean location of the finger‐movement response was −45, −20, +45 (x, y, z). Having made this initial determination of the group‐mean location, a per‐subject analysis was then carried out specifically targeting the M1‐hand region.
Per‐subject SPI(z) were created for each of the 11 subjects for both conditions (vs. control). Responses were detected by an automated, local‐maximum search algorithm and reported as x‐y‐z coordinates of the centers‐of‐mass in standardized space. Searches were limited to a cubical volume 40 mm in diameter centered on the group‐mean location for finger movement. In all 11 subjects, robust responses to finger movement were observed. Of these 11 subjects, TMS‐induced responses were detected (z > 1.96) in the search volume for seven subjects; not for the remaining four subjects. For these seven subjects, the per‐subject response locations to TMS and to finger movement are reported, illustrated, and analyzed. Response locations were obtained both in standardized stereotatic coordinates and as perpendicular distances from the scalp (Fig. 2). Distances from the scalp to the observed responses were measured using software developed in‐house for image‐based TMS delivery (TMS Planning Tool). For TMS‐induced responses, the E field at the response site was computed using a 3D model of the field.
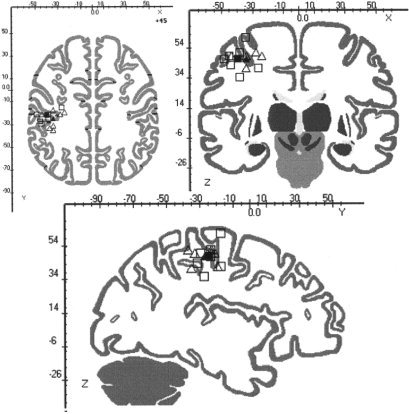
Figure 2.
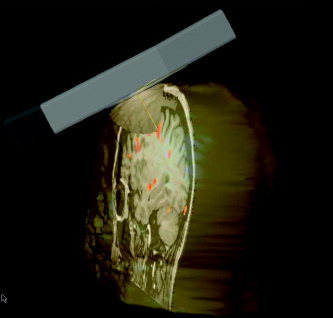
Measurement of the distance from the stimulation point at the scalp to the detected response is illustrated for Subject 1246. The T1‐weighted MRI is shown in grey‐scale. The TMS‐induced PET activation response is shown in color overlay; note that it lies on the sulcal surface, and does not include the gyral crown. The scalp surface model was constructed from the tissue‐air interface of the MRI. The TMS coil is to scale. The shaded half‐dome is a calibrated 3D model of the E field created by the TMS coil. The distance to the center‐of‐mass of the TMS‐induced activation was measured with the depth probe function (yellow line) of the TMS Planning Tool software (RIC, UTHSCSA).
Group SPI(z) were created separately for the seven subjects showing a TMS‐induced M1 response and for the four subjects not showing an M1 response to TMS. These group SPIs were created for two reasons. For the PET responders (n = 7), the purpose was to obtain the most robust group‐wise determination of response location for finger‐movement and TMS stimulation. For the PET non‐responders (n = 4), the purpose was to determine if any M1 cortical response could be detected when signal‐to‐noise ratio was enhanced through averaging.
RESULTS
Finger movement‐induced responses in primary motor cortex (M1) were detected with PET imaging in all 11 subjects. TMS‐induced M1 responses were detected with PET in 7 of 11 subjects. The bulk of the analyses presented here address these seven subjects (cortical responders). The lack of a PET‐detected response, however, in the face of clear EMG evidence of corticospinal excitation is an important phenomenon in its own right and is also addressed (cortical non‐responders).
Cortical Responders
For voluntary finger movement, PET‐detected M1 activations were centered on the banks of the central sulcus on the lateral convexity in all seven subjects (Fig. 3). For TMS‐induced M1 activation, responses were also located in the central sulcus (Fig. 3), being very similar in location and shape to the activations induced by voluntary movement. In all subjects, all M1 responses were sulcal rather than gyral for both hand movement and TMS stimulation. In addition, no evidence of gyral activation was observed in M1 in any subject for either task. This is entirely in keeping with the known location of M1 cortex (Brodmann's area [BA] 4). At the hand representation, BA4 extends upward from the pit of the central sulcus an amount that varies across individuals but rarely extends to the gyral crown [Garey et al., 1994: Geyer et al., 1996; Grafton et al., 1991; Kawashima et al., 1995].
Figure 3.
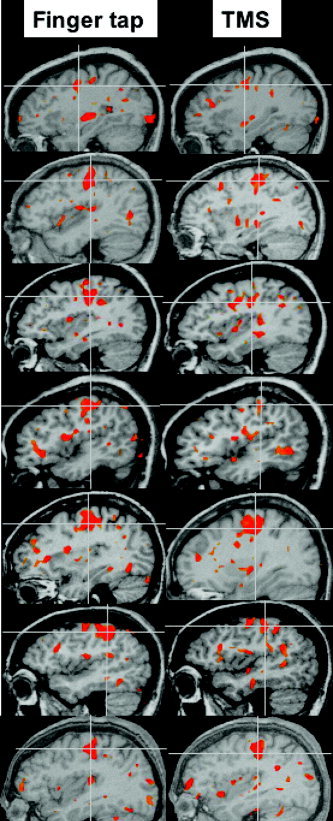
M1 responses to voluntary finger tapping (left column) and to TMS (right column) are shown for each of the seven subjects in whom an M1 blood‐flow response was observed in per‐subject PET images. In each instance the response is visualized in the parasagittal plane at the center‐of‐mass of the M1 response (cross‐hair). In every subject and for both stimuli, responses were on the sulcal surface of the central sulcus (BA4). There was no evidence of a response being present on the gyral crown during TMS stimulation or finger movement. This supports a column‐based model of E field interaction with cortex. Overlays were created using the TMS Planning Tool.
The depth of the M1 responses to TMS and to finger movement were measured as the shortest distance to a plane perpendicular to the scalp in each subject (Fig. 2) and are reported in Table I. The average depth of activation during TMS was 31.2 mm (range, 22–40 mm) and during voluntary finger movement was 29.9 (range, 22–38). This difference is not significant (paired t‐test; P = 0.3). TMS‐induced activations of M1 were not more superficial than voluntary movement‐induced activations, contradicting the prediction of Day et al. [1989]; instead, responses to both conditions were equally deep within the central sulcus. Moreover, response depth was significantly correlated across the two conditions (r = 0.93; P < 0.002), as is illustrated in Figure 4. That depth of activation was so highly correlated across conditions argues strongly that this measurement is a good index of the per‐subject variability of the distance that BA4 extends up the anterior bank of the central sulcus. It also argues strongly that M1 activations induced by TMS and voluntary finger movement are in the same functional and cytoarchitectural subregion of M1 [Geyer et al., 1996; Kawashima et al., 1995].
Table I.
Per‐subject M1 depths
| Subject | M1 depth (mm)* | Threshold (E, V/m)** | 125% MT (E, V/m)** | |
|---|---|---|---|---|
| Voluntary | TMS | |||
| 1246 | 38 | 37 | 70 | 87 |
| 1265 | 26 | 28 | 77 | 96 |
| 1280 | 37 | 40 | 59 | 73 |
| 1281 | 27 | 24 | 100 | 125 |
| 1286 | 31 | 33 | 54 | 66 |
| 1316 | 22 | 22 | 109 | 137 |
| 1355 | 29 | 34 | 59 | 73 |
| Mean | 29.9 | 31.2 | 79.2 | 94.1 |
Depth (in mm) from scalp surface to center‐of‐mass of M1 activation induced by movement of the right index finger (voluntary) and by transcranial magnetic stimulation (TMS) eliciting movement of the right first dossal interosseous muscle (FDI). The two distances did not differ significantly but did covary significantly (r = 0.93; Fig. 4).
Absolute E field values at the response site for stimulation at motor threshold and at 125% of motor threshold (MT) were computed in volts per meter (V/m) using a 3D computer model of the E field created by the Cadwell coil scaled by the machine setting (% output) and the distance from the scalp.
Figure 4.
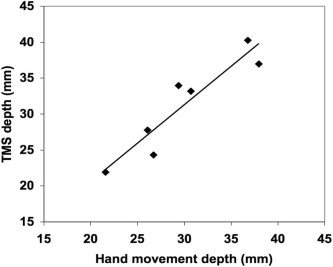
A scatter plot of the depths from the scalp surface for the M1 response to voluntary index finger movement (x‐axis) and TMS‐induced FDI activation (y‐axis) is shown. The depths of the responses were highly correlated (r = 0.93; P < 0.002). This indicates that the depth of the TMS‐induced activation was a function of the actual depth of the M1 cortex, as BA4 is known to extend a varying distance upward from the BA 3 border in the depths of the sulcal pit.
The locations of the M1 responses to TMS and to finger movement were also expressed as coordinates within a standardized space (Table II, Fig. 5). For both conditions, the coordinates are in good agreement with previous reports of response locations for the hand representation within M1 [e.g., Fox et al., 1985, 1987]. If TMS‐induced activation were on the gyral crowns and voluntary movement‐induced activation were sulcal, it would be expected that response locations would differ between conditions with TMS effects being more lateral (more negative x), more superior (greater z) and more posterior (more negative y). The response would be more posterior because the central sulcus is angled in the anterior–posterior axis, with the sulcal pit being more anterior than the gyral crown. None of these effects were observed, as the two conditions did not differ significantly in response location in any axis. In the y‐ and z‐axes, response locations covaried (in y, r = 0.71; in z, r = 0.60), although not as strongly as was seen for depth values (above). In the x‐axis, the location covariance between conditions was weak (0.38) and there was a trend (P < 0.06) for TMS‐induced responses to be more medial than finger movement‐induced responses. All of these effects are contrary to the prediction from selective gyral activation theory of Day et al. [1989] and others.
Table II.
Per subject coordinates
| Subject | Voluntary movement | TMS‐induced movement | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| x | y | z | Volume | Z‐score | x | y | z | Volume | Z‐score | |
| 1246 | −26 | −16 | 40 | 1,152 | 3.3 | −34 | −18 | 40 | 1,304 | 3.7 |
| 1265 | −44 | −30 | 42 | 3,504 | 4.6 | −34 | −36 | 50 | 2,208 | 4.2 |
| 1280 | −38 | −26 | 34 | 2,656 | 3.9 | −37 | −34 | 39 | 408 | 3.2 |
| 1281 | −45 | −28 | 48 | 856 | 4.0 | −28 | −22 | 50 | 336 | 3.3 |
| 1286 | −34 | −16 | 60 | 5,592 | 4.9 | −24 | −20 | 48 | 6,104 | 6.2 |
| 1316 | −48 | −22 | 46 | 1,960 | 4.19 | −44 | −22 | 48 | 1,128 | 3.5 |
| 1355 | −38 | 22 | 50 | 2,520 | 4.3 | −34 | −32 | 48 | 12,640 | 5.6 |
| Mean | −39 | −23 | 48 | 2,605 | 4.17 | −34 | −26 | 46 | 3,447 | 4.26 |
The standardized location coordinates of the M1 responses to voluntary movement (right index finger) and to transcranial magnetic stimulation (TMS)‐induced movement (right FDI) are shown for 7 subjects in whom an M1 TMS response could be detected.
Locations are expressed in millimeters relative to the anterior commissure, with x being medial‐lateral (right hemisphere = positive), y being anterior‐posterior (anterior = positive) and z being superior‐inferior (super = positive.) No significant differences between response locations were observed in any axis: x, P = 0.06; y, P = 0.07; z, P = 0.2). Response locations did covary between conditions in all axes: x, r = 0.38; y, r = 0.71; z, r = 0.60). Volume of activation and Z‐score did not differ between the two conditions. Z‐scores were significantly correlated across conditions (r = 0.64), but activation volumes were not.
Figure 5.
The locations of M1 responses to voluntary finger movement (squares) and to TMS‐induced finger movement (triangles) in standardized coordinates for each of seven subjects are illustrated. Per‐subject locations are open symbols; average locations are solid symbols. Location of activation did not differ significantly in any axis between the two types of M1 activation. Responses are plotted using the BrainMap Search and View software (online at http://www.brainmapdbj.org).
Group‐mean SPIs were created for both conditions (contrasted to a sham‐stimulation control state) for the seven subjects having TMS‐induced M1 activation (Fig. 6). For both conditions, the activations patterns are quite similar in location (Table III), shape, and extent (Fig. 6). The trend for TMS responses to be more medial than those of finger movement is again seen, although the significance of this location difference cannot be tested in group‐mean images.
Figure 6.
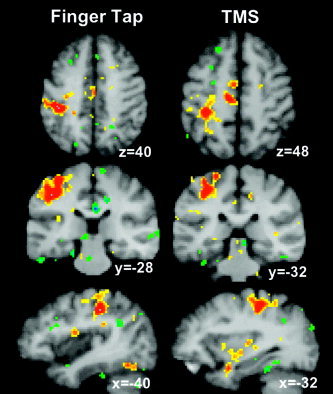
PET Responders. The M1 response to voluntary finger tapping (left group) and the M1 response to TMS (right group) are shown in group‐mean SPIs formed from the seven subjects in whom a significant M1 response to TMS was observed with per‐subject PET image analysis. For both conditions, Z‐score rose with averaging: to 5.7 (from 4.2) for voluntary movement, and to 5.0 (from 4.3) for TMS. The center‐of‐mass of the responses in the two images are very similar (Table III). In both SPIs, the response lies deep in the central sulcus, not on the gyral crown, supporting a column‐based model of E field effects on cortex.
Table III.
Group‐image coordinates
| Voluntary | TMS | |||||
|---|---|---|---|---|---|---|
| x | y | z | x | y | z | |
| Group SPI | −40 | −28 | 40 | −32 | −32 | 48 |
| Individual | −39 | −23 | 48 | −34 | −26 | 46 |
The standardized location coordinates taken from group‐mean statistical parametric images (SPIs) averaging 7 subjects with significant M1 response to transcranial magnetic stimulation (TMS) compared to those obtained by averaging per‐subject response locations (Table II). In group‐mean images, center‐of‐mass of the response to voluntary movement and the response to TMS are similar.
Cortical Non‐Responders
In four subjects, no M1 responses to TMS were observed with PET. EMG responses were present in all subjects andwere not different in magnitude or latency between the two subgroups. In each of the four subjects, moreover, a robust response to finger movement was observed with PET. One possible explanation of the lack of PET‐detected responses in non‐responders is that responses were present, but fell below the statistical threshold (z = 1.96). To test this possibility, two additional tests were carried out. In view of the correlation (r = 0.64) observed in M1 between the response intensities (peak Z‐score) induced by voluntary movement and those induced by TMS, we compared finger movement response intensity between the two subgroups. Despite the small sample size, the average response intensities for finger movement were significantly different between subgroups (P = 0.015; t = 2.54; df = 9) with the non‐responders having a weaker response (Z‐score = 3.4) than responders (Z‐score = 4.1). In view of the similar average response intensities, however, for TMS (Z‐score = 4.26) and voluntary movement (Z‐score = 4.17) in the responders subgroup, the magnitude of the voluntary movement response in the non‐responders would predict a readily detected TMS response even in this subgroup.
Reasoning that if a cortical response were present but weak it should be detected by averaging, group‐average SPIs were created for both TMS stimulation and finger movement in the non‐responders subgroup. In the four‐subject finger movement SPI, there were strong responses in M1 and other components of the motor system, including supplementary motor area, cerebellum and lateral premotor cortex (Fig. 7). In the four‐subject TMS SPI, however, there was no detectable M1 response and no significant responses in other motor structures connected to M1. Cortical responses were present in anterior insula and posterior superior insula (S2), both of which are plausibly interpreted as proprioceptive responses to the TMS‐induced displacements of the finger. Consequently, we interpret the absence of a cortical response to TMS in this subgroup as a real effect, not an artifact of statistical thresholding. Furthermore, we interpret this as indicating that in the non‐responders subgroup TMS acted directly on the axons of the pyramidal neurons projecting into the corticospinal tract, rather than by exciting M1 cortex proper. The absence of a PET response in white matter (in the non‐responders) does not contradict this inference, because focal blood flow increases detected by PET (and functional MRI) are restricted to grey matter.
Figure 7.
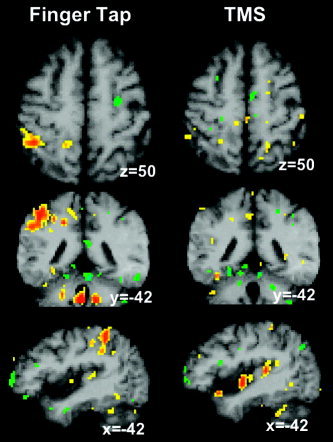
PET Non‐responders. The M1 response to voluntary finger tapping (left) and the absence of an M1 response to TMS (right) are shown in group‐mean SPIs formed from four subjects in whom a significant M1was not observed with per‐subject PET image analysis. Although the response to hand movement rose with averaging to a Z‐score of 4.0 (average of per‐subject Z‐scores = 3.4), no response to TMS was observed even with averaging. As TMS did produce corticospinal track excitation (as evidenced by TMS‐induced muscle contractions), we infer that the EMG was induced via direct axonal depolarization rather than via cortical excitation.
In an attempt to identify other factors that might explain the absence of a cortical response to TMS in the presence of an EMG response, TMS stimulation, and response parameters were compared between cortical responders and non‐responders. The EMG‐defined motor threshold was not different between responders and non‐responders (Table IV). The average magnitude of the E field applied at the scalp or at the M1 index finger representation (i.e., scalp intensity scaled for depth) was not different between the two groups (Table IV). The x‐y‐z locations and depth of the M1 responses to hand movement did not differ between groups (Table IV).
DISCUSSION
PET imaging of the TMS‐induced responses in the finger representation of primary motor cortex in seven subjects showed excitation of the sulcal cortical surface, not of the gyral crown, as hypothesized by Day et al. [1989] and others [Brasil‐Neto et al., 1992; Mills et al., 1992; Wasserman et al., 1996]. The location of TMS‐induced activations was not statistically different from the location of finger movement‐induced activations, either when expressed as absolute depths or when expressed in standardized coordinates. Rather, response depths and location coordinates covaried strongly across conditions, indicating that both conditions were eliciting activation in the same cortical region. These findings suggest that orientation of a TMS‐induced E field relative to the columnar functional organization of cortex is critical for successful cortical excitation. They argue against Day et al.'s [1989] assumption that proximity to the stimulation coil (i.e., the strength of the applied E field) is the primary determinant of cortical excitation. Taken together with the established orientation selectivity of primary motor cortex, the results provide support for a column‐based model of the effects of transient electrical fields on cerebral cortex.
Functional Imaging
Previously published PET/TMS experiments also demonstrate that TMS preferentially excites buried cortex (sulcal banks) rather than gyral crowns, although these studies have not done per‐subject mapping of response location as was done here. For example, Paus et al. [1997] used PET to image the functional response to TMS stimulation of the frontal eye fields (FEF). In a group‐mean SPI, the resulting activation was distinctly sulcal, lying approximately 3 cm deep to the gyral crown [Paus et al., 1997, Fig. 3]. Similarly, Fox et al. [1997] used PET to image the response to TMS stimulation of primary motor cortex. Also in a group‐mean SPI the resulting activation was clearly sulcal, lying 2 cm deep to the gyral crown [Fox et al., 1997, Fig. 1]. This study did not include voluntary finger movement, however, so the similarity of response location for voluntary and TMS‐induced finger movements was not determined.
Wasserman et al. [1996] used functional and anatomic imaging to infer the location of TMS‐induced excitation of motor cortex. TMS was applied by hand so as to elicit a contraction of the FDI. The stimulated location was marked with a fiducial and projected onto each subject's MRI. In accordance with the hypothesis of Day et al. [1989], the site of action was projected no deeper than the gyral crown. At this depth, the location projection was “just anterior to the central sulcus.” The central sulcus, however, is angled forward, such that the pit of the sulcus lies anterior to the crown. If the activated site were projected more deeply than the crown, it would have intersected the anterior bank of the central sulcus. The location of motor cortex (determined by PET subtraction images) was on the anterior bank of the central sulcus, up to 2.2 cm deep to the gyral crown and immediately beneath the projected TMS activation site. We suggest that if Wasserman et al. [1996] had accepted the possibility that the TMS activation site could have been the anterior bank of the central sulcus (rather than accepting Day et al.'s [1989] unproven hypothesis), he would have found that voluntary FDI contraction and TMS‐induced FDI contraction give similarly localized responses, as was observed here. Consequently, we interpret the existing functional imaging data as corroborating our present findings as well as our hypothesis of selective TMS excitation of sulci (below).
Electrophysiology
A large body of electrophysiologic observations supports the hypothesis that alignment of the TMS‐induced current with orientation of the cortical column (normal to the cortical surface) is optimal for cortical excitation.
Longitudinal current membrane sensitivity
“From the time of Galvani [1790] onwards, it has been recognized that a nerve is nearly or quite inexcitable to currents perpendicular to the axis” [Rushton, 1927]. This was convincingly demonstrated in isolated axons by Rushton [1927], who found that when the voltage gradient was entirely transverse to the axon, the axon could not be stimulated. Rushton concluded that the depolarization threshold is inversely proportional to the cosine of the angle between the current and the nerve. Rudin and Eisenman [1954] found that four or five times more current was required to depolarize an axon when applied transversely than when applied longitudinally. Rushton [1927], Rudin and Eisenman [1954], and others [see Ranck, 1975] have found consistently that orthodromic current is more effective than antidromic current, which, in turn, is more effective than transverse current. This principle implies that TMS is most effectively applied by orienting the E field longitudinal and orthodromic to the greatest possible number of neurons at the site of interest.
Membrane length effect
For any neuron, increasing the total length of neuronal membrane exposed to an applied current lowers the depolarization threshold [Rushton, 1927]. For TMS stimulation, current aligned with a cortical column (along the long axis of the preponderance of neurons) would expose the maximum membrane length of the maximum number of neurons to the exciting stimulus. The membrane‐length effect also predicts optimum responsivity (lowest thresholds) when the TMS‐induced current is aligned with the cortical column.
Principal axis sensitivity
For intact neurons, the most effective orientation for a stimulating current is along the long‐axis of the neuron and orthodromic. Although some neurons (e.g., stellate cells) have no clear geometrical axis, most neurons (>90%) have a well‐defined principal axis. This axis is particularly well defined by the soma and axon, with the dendritic tree having a larger component of horizontal fibers and less rigid conformation to the longitudinal orientation. A long series of studies applying anodal stimulation to the intact motor cortex [Fritsch and Hitzig, 1870; Landau et al., 1965; Purpura and McMurty, 1965; Ranck, 1975] have demonstrated exclusive or nearly exclusive excitation of neural elements oriented along the path of current flow, with little or no excitation of elements exposed to transverse currents. Although suggestive of a neuron‐specific orientation effect (in addition to the membrane orientation effect), these studies are not conclusive. The clearest evidence for a distinct principal axis effect comes from modeling isolated neurons in an electrical field [Trachina and Nicholson, 1986]. Trachina and Nicholson [1986] confirm that the most effective depolarizing current is orthodromically oriented with the long axis of the neuron. This effect can be considered an additional effect, beyond membrane orientation and length effects, in that despite containing most of the total membrane, the dendritic tree contributes little to triggering axonal depolarization when the cortex is exposed to an externally applied E field. For TMS aiming, the implication is to emphasize further that the applied field should be oriented with the long axis of most neurons, i.e., along the cortical column.
Somal sensitivity
The importance of depolarization of the soma to neuronal discharge has long been recognized. Applying an optimally oriented current to intact cortex, the site of action‐potential initiation is the soma [Chan and Nicholson, 1986; Gorman, 1966; Hern et al., 1962; Landau et al., 1965; Purpura and McMurty, 1965; Ranck, 1975; Rosenthal et al., 1967]. Modeling the effects of uniform E fields, Trachina and Nicholson [1986] confirmed that the somal region is the most likely site for action potential initiation by an applied field. This effect is due in part to the fact that the membrane potential in a uniform field decays exponentially with distance from the soma. Another conclusion from their modeling was that axonal polarization, particularly that of the initial segment, containing the axon hillock, has the strongest influence on somal depolarization. Another important factor contributing to the low threshold of the somal region to applied currents is the high density of Na+ channels in the axon hillock, the axon segment abutting the soma. At the hillock, the depolarization threshold is only 10 mV, whereas in dendrites it exceeds 30 mV [Kandel and Schwartz, 1991]. An electrical field oriented along the principal axis of a neuron and passing through the soma (rather than being limited to the axon or dendrites) will thus elicit depolarization at the lowest possible threshold. In reference to TMS, the implication is that cortex (if longitudinally stimulated) will be preferentially activated by virtue of its containing somata, which are absent in subcortical white matter.
Vertical Cortical Anatomic Organization
The principle of the vertical anatomic organization in the cerebral and cerebellar cortex was established by Ramon Y Cajal, for which he was awarded the Nobel prize in 1910. Most neurons have a well‐defined long axis that is almost always aligned at right angles to the cortical surface (i.e., vertically). Horizontally oriented, intracortical fibers form a minority and chiefly serve to connect adjacent neurons over distances of <1 mm. The principle of vertical anatomic organization implies that a vertically applied E field will follow the long axis of most neurons, thereby providing maximal excitation.
Vertical Cortical Functional (Columnar) Organization
The principle of vertical functional organization of the cortex was established by Hubel and Wiesel [1979], for which they were awarded the Nobel prize in 1981. Jones and Wise [1978] demonstrated a similar phenomenon in somatomotor cortex. The column is now accepted as the fundamental organizational unit of the cortex. The cells within a cortical column form a functional ensemble, firing in concert and influencing one another in the process. For TMS, the implication is that an E field oriented along the cortical columns will benefit from this functional synergy in addition to the anatomic synergy of the vertical orientation predominance.
In discussions of the various factors that might contribute to the proposed vertical orientation preference of cortex, it has been noted that electrical stimulation is most effective when the applied current has the same orientation and sense as the normal flow of current during depolarization: from dendrites, through soma, to axon. The event‐related potentials (ERP) literature has repeatedly addressed the direction and sense of normal cortical excitation, for the purpose of modeling the origin of scalp‐recorded electrical currents. The overwhelming consensus is that virtually all measurable current flows normal to the surface [Lopez da Silva, 1991]. This implies that cortex will be most sensitive to applied electric field that induce similarly oriented currents.
Horizontal Isotropism
The columnar functional organization of cortex has no horizontal counterpart. Although it is well known that horizontal fibers are more common in superficial layers than in deep ones, within a layer, horizontal fibers run in all directions, i.e., horizontal fibers exhibit in‐plane isotropism, having no preferred orientation within a layer. Otherwise stated, cortex has vertical “columns” (and horizontal layers) but no “rows” within the layers. For TMS, the implications are twofold. First, at any given cortical location, a horizontally oriented E field will be aligned so as to excite only a small fraction of the total population of horizontal fibers, whereas a vertically oriented E field of the same magnitude will be aligned so as to excite a large fraction total population of the vertical neurons/fibers. This inefficiency is in addition to the preceding factors enhancing vertical responsivity and diminishing horizontal sensitivity. Second, horizontal fiber stimulation by an E field intersecting the crown of a gyrus would have no preferred orientation. A TMS coil rotated about its z‐axis would be equally effective in every orientation. Much evidence to the contrary exists, arguing that horizontal‐fiber excitation plays little or no role in TMS. The absence of gyral crown excitation in the present study and in previous PET/TMS studies is further evidence against the horizontal fiber model of TMS excitation.
The Cortical Column Cosine Model of TMS Efficacy
Based on the above evidence and arguments, we propose that a general model for predicting the effects of TMS on cortex can be derived from Rushton's cosine principle [Rushton, 1927] as applied to the cortical column. We hypothesize that for TMS stimulation of intact cerebral cortex, the cortical column as a whole is the affected neural element. The effective stimulating E field (Eeff) is the column‐aligned E field. When the applied E field is off‐axis, Eeff is computed as the cosine of the angle between the applied field and the cortical column (Fig. 8). As the cortical columns are aligned normal to the cortical surface, Eeff can be computed for any point on the cortex, if the orientation and intensity of the absolute E field and the orientation of the cortical surface are known. With this information and PET‐observed responses over a range of stimulation intensities, it should be possible to measure thresholds for excitation (as determined by a blood‐flow response) for any cortical location.
Figure 8.
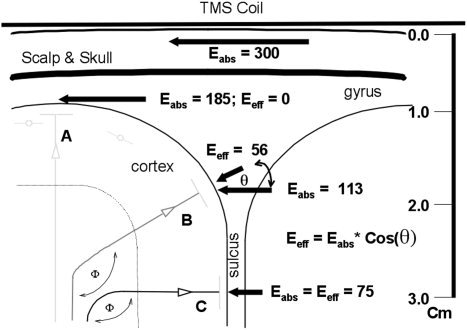
The cortical column cosine (C3) model. The linear, scalp‐parallel E field (bold arrows) induced by a B‐shaped coil is illustrated. In this study, the average value of the E field applied at the scalp was 300 V/m. The average depth of M1 excitation by TMS was 31 mm. (A centimeter ruler is shown at right). The E field diminishes exponentially with distance from the scalp. The C3 model posits that activation is induced only by the column‐aligned component of E. The absolute E field vector (Eabs) is decomposed into two components: a column‐aligned component that is effective (Eeff) and column‐normal component that is ineffective. Otherwise stated, Eeff is the product of Eabs and the cosine of the angle between the column and the E vector (θ). Whereas the Eabs is greatest at the gyrus, the Eeff is least and activation fails to occur (A). In the sulcal depth (C), Eabs is least, but Eeff is greatest and cortical excitation threshold is achieved. On the shoulder of the gyrus (B), Eabs can be greater than in the sulcus (C), but Eeff may still fall below threshold. The bending angle (Φ) of the pyramidal cell axon as it exits cortex and enters the corticospinal tract is illustrated.
The cortical column cosine (C3) model is based on cortical orientation relative to the E field (Fig. 8), not whether the cortical surface is sulcal or gyral. On the lateral convexity of the hemisphere, gyral crowns generally are parallel to the scalp and to the applied E field, making them unable to be stimulated by TMS. On the medial surface of the hemisphere, the gyral crowns are perpendicular to the scalp. The C3 model would, therefore, predict ready excitation of the medial surface, so long as the E field were aimed at a right‐angle to the inter‐hemispheric fissure. We have confirmed this by successfully imaging with PET activation of supplementary motor area (SMA) induced by an E field oriented perpendicular to the midsagittal plane [Tandon et al., 2001]. When the E field was aligned with the midline, the medial hemispheric surface did not activate but sulcal surfaces perpendicular to the midline did (unpublished data; manuscript in preparation). The C3 model would also predict that an E field perpendicular to the scalp would activate gyral crowns on the lateral convexity. This prediction has not been tested, as a coil shaped to deliver a scalp‐normal E field has not been constructed. In addition, it is unclear whether an E field applied perpendicular to the scalp would be effective in penetrating to cortex, or whether charge build‐up on opposite sides of each tissue interface would cancel the field.
The C3 model predicts that the E field orientation effect observed by Brasil‐Neto et al. [1992] and Mills et al. [1992] is a fundamental component of TMS' interaction with cortex. If applicable in M1, it should be applicable everywhere, as all cerebral cortex has the same basic columnar structure. If true, this means that image‐guided TMS, precisely orienting the E field to be normal to the cortical surface at the targeted site, will be useful, at least, and may possibly be critical for applications of TMS anywhere in cortex. The current practice in many laboratories, particularly for clinical trials, is to apply TMS hand‐held (rather than in a rigid holding system), to use the 10–20 electrode placement system as a location guide (rather than guided by functional imaging), and to angle the E field medially at 45 degrees emulating optimal orientation found for M1 (rather than guided by anatomic imaging to be perpendicular to the cortical surface stimulated). These violations of the requirements of the C3 model may well explain why the efficacy of TMS under such conditions has proven so highly variable across studies and across individuals.
Direct Axonal Excitation
The previous discussion has been directed solely to cortical effects of scalp‐applied E field transients. Cortical excitation, however, may not be the only mechanism by which TMS excites the brain. That a TMS‐generated electric‐field transient can directly excite axons is demonstrated readily by application of the coil to a peripheral nerve. In many subjects, peripheral nerve excitation can be observed with the face of the stimulating coil at distances of 2 cm or more from the skin overlying the nerve. This raises the possibility that TMS applied to the scalp may directly excite axons in white matter. Some have argued that direct axonal excitation is the principal neurophysiologic mechanism of TMS [Amassian et al., 1998; Ruohonen and Ilmoniemi, 1999]. In this context, we raise the possibility that the four subjects in whom no cortical M1 response was observed with PET but in whom excitation of corticospinal neurons was evidenced by FDI contraction are examples of direct axonal excitation.
An experimentally induced action potential will propagate orthodromically across multiple synapses. In the present instance, corticospinal excitation propagates across the synapse at the anterior horn cell in the spinal cord and at the myoneural junction to generate the observed FDI contraction. The same action potential, however, will not propagate transynaptically in the antidromic direction. Consequently, if the pyramidal cell axons were excited in subcortical white matter, the induced action potentials would propagate antidromically only within the pyramidal cell, not spreading to other M1 neurons and not propagating to other cortical regions within the motor system. This is consistent with our observations in the four PET non‐responders. In these subjects, cortical activation was not seen in M1, SMA, or cerebellum, all of which were highly activated in the seven PET responders. The regions that were activated most strongly (anterior insula and posterior, superior insula [S2]) may well have been driven by the proprioceptive input of the induced movement and not by cortico‐cortical connections. Taking the PET and EMG data together, direct axonal excitation seems to be the most parsimonious explanation.
If cortical excitation occurs in some subjects whereas subcortical excitation occurs in others, it is physiologically and practically important to understand what parameters determine the predominant effect. Considering the finger movement‐induced PET activations, cortical non‐responders do not seem to differ from responders in the depth, location (x‐y‐z), or extent (mm3) M1 responses. Considering the TMS‐induced EMG activations, cortical non‐responders did not seem to differ from responders in motor threshold either when expressed as E field intensity at the scalp or when expressed as E field intensity at M1 (i.e., corrected for depth from scalp). One possibility is that the relative excitabilities of cortex and white matter are similar but vary among individuals, with the four non‐responders having a lower axonal threshold than cortical threshold. The observation that PET responses to voluntary finger movement were less robust in the TMS cortical non‐responders than in the responders may also indicate a lower level of M1 excitability in general, which may equate to a higher cortical excitation threshold. Another possibility is that variations in gyral geometry offer an explanation.
Axons are stimulated most effectively by steep gradients in an E field, relative to the axon's direction of travel [Amassian et al., 1992, 1998; Ruohonen and Ilmoniemi, 1999]. In a uniform field, an axonal membrane will experience an E field gradient when its direction of travel changes sharply. An axon is depolarized most readily when one segment of the axon (e.g., pre‐bend) is aligned with the E field and the bend turns the membrane at a right angle to the field. In cortex, the preponderance of neurons will be aligned with the E field when it is column‐aligned (cortical surface normal), so the C3 model should apply to direct axonal excitation as well as to cortical excitation. The cortical non‐responders (inferred to be axonal responders) may be the subjects in whom the descending corticospinal axon makes the most abrupt turn to exit the gyrus (Fig. 8, angle Φ), making the axonal excitation threshold lower than the cortical threshold. As with the C3 model, the direct axonal excitation model will require highly precise, image‐guided aiming to be tested and, if proven correct, equally precise aiming to be applied.
Acknowledgements
We thank B. Heyl and S. Leal for assistance with PET data acquisition, J. Li and J.H. Gao for assistance with MRI data acquisition, C. Franklin, M. Martinez, and F. Zamarippa for expert processing of image data. We also thank D. Wenzel for implementing the Planning Tool and Delivery Tool software and for assistance with robot operations.
REFERENCES
- Amassian VE, Eberle L, Maccabee PJ, Cracco RQ (1992): Modelling magnetic coil excitation of human cerebral cortex with a peripheral nerve submersed in a brain shaped volume conductor: the significance of fiber‐bending excitation. Electroencephalogr Clin Neurophysiol 77: 390–401. [DOI] [PubMed] [Google Scholar]
- Amassian VE, Cracco RQ, Maccabee PJ, Cracco JB, Rudell AP, Eberle L (1998): Transcranial magnetic stimulation in study of the visual pathway. J Clin Neurophysiol 15: 228–304. [DOI] [PubMed] [Google Scholar]
- Brasil‐Neto JP, McShane LM, Fuhr P, Hallett M, Cohen LG (1992): Topographic mapping of the human motor cortex with magnetic stimulation: factors affecting accuracy and reproducibility. Electroencephalogr Clin Neurophysiol 85: 9–16. [DOI] [PubMed] [Google Scholar]
- Chan CY, Nicholson C (1986): Modulation by applied electric fields of Purkinje and stellate cell activity in the isolated turtle cerebellum. J Physiol 371: 89–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da Silva L (1991): Neural mechanisms underlying brain waves: from neural membranes to networks. Electroencephalogr Clin Neurophysiol 79: 81–93. [DOI] [PubMed] [Google Scholar]
- Day BL, Dressler D, Maertens de Noordhout A, Marsden CD, Nakashima K, Rothwell JC, Thompson PD (1989): Electric and magnetic stimulation of human motor cortex: surface EMG and single motor unit responses. J Physiol 412: 449–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritsch G, Hitzig E (1870): On the electrical excitability of the cerebrum [Uber die elektrische Erregbarkeit des Frosshirns]. Translation by G. von Bonin. The Cerebral Cortex. Springfield, IL: Thomas; p 73–96. [Google Scholar]
- Fox PT, Burton H, Raichle ME (1987): Mapping human somatic sensory cortex with positron emission tomography. J Neurosurg 63: 34–43. [DOI] [PubMed] [Google Scholar]
- Fox PT, Fox JM, Raichle ME, Burde RM (1985): The role of cerebral cortex in the generation of saccadic eye movements: a positron emission tomographic study. J Neurophysiol 42: 348–368. [DOI] [PubMed] [Google Scholar]
- Fox PT, Ingham RJ, Mayberg H, George M, Martin C, Ingham J, Robey J, Jerabek P (1997): Imaging human cerebral connectivity by PET during TMS. Neuroreport 8: 2787–2791. [DOI] [PubMed] [Google Scholar]
- Garey LJ (1994): Brodmann's localization in the cerebral cortex. London: Smith Gordon. [Google Scholar]
- Geyer S, Ledberg A, Schleicher A, Kinomura S, Schormann T, Burgel U, Klingberg T, Larsson J, Zilles K, Roland PE (1996): Two different areas within the primary motor cortex of man. Nature 382: 805–807. [DOI] [PubMed] [Google Scholar]
- Gorman AL (1966): Differential patterns of activation of the pyramidal system elicited by surface anodal and cathodal cortical stimulation. J Neurophysiol 29: 547–564. [DOI] [PubMed] [Google Scholar]
- Grafton ST, Woods RP, Mazziotta JC, Phelps ME (1991): Somatotopic mapping of the primary motor cortex in humans: activation studies with cerebral blood flow and positron emission tomography. J Neurophysiol 66: 735–743. [DOI] [PubMed] [Google Scholar]
- Hern JE, Landgren S, Phillips CG, Porter R (1962): Selective excitation of corticofugal neurons by surface stimulation of the baboon's motor cortex. J Physiol 161: 73–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubel DH, Wiesel TN (1979): Brain mechanisms of vision. Sci Am 241: 150–162. [DOI] [PubMed] [Google Scholar]
- Jones EG, Wise SP (1978): Size, laminar and columnar distributions of efferent cells in the sensory‐motor cortex of monkeys. J Comp Neurol 175: 391–438. [DOI] [PubMed] [Google Scholar]
- Kandel E, Schwartz JH, Jessell TM (1991): Principles of neural science. New York: McGraw‐Hill; p 166–167. [Google Scholar]
- Kawashima R, Itoh H, Ono S, Satoh KI, Furumoto S, Gotoh R, Koyama M, Yoshioka S, Takahashi T, Yanagisawa T, et al. (1995): Activity in the human primary motor cortex related to arm and finger movements. Neuroreport 6: 238–240. [DOI] [PubMed] [Google Scholar]
- Kochunov PV, Lancaster JL, Fox PT (1999): Accurate high‐speed spatial normalization using an octree method. Neuroimage 10: 724–737. [DOI] [PubMed] [Google Scholar]
- Lancaster JL, Glass TG, Lankipalli BR, Downs JH, Mayberg H, Fox PT (1995): A modality‐independent approach to spatial normalization of tomographic images of the human brain. Hum Brain Mapp 3: 209–223. [Google Scholar]
- Lancaster JL, Fox PT, Downs H, Nickerson DS, Hander TA, El Mallah M, Kochunov PV, Zamarripa F (1999): Global spatial normalization of human brain using convex hulls. J Nucl Med 40: 942–55. [PubMed] [Google Scholar]
- Landau W, Bishop GH, Clare MH (1965): Site of excitation in stimulation of the motor cortex. J Neurophysiol 28: 1206–1222. [DOI] [PubMed] [Google Scholar]
- Lee JS, Narayana S, Lancaster J, Jerabek P, Lee DS, Fox P (2003): Positron emission tomography during transcranial magnetic stimulation does not require mu‐metal shielding. Neuroimage 19: 1812–1819. [DOI] [PubMed] [Google Scholar]
- Mills KR, Boniface SJ, Shubert M (1992): Magnetic brain stimulation with a double coil: the importance of coil orientation. Electroencephalogr Clin Neurophysiol 85: 17–21. [DOI] [PubMed] [Google Scholar]
- Paus T, Jech R, Thompson CJ, Comeau R, Peters T, Evans AC (1997): Transcranial magnetic stimulation during positron emission tomography: a new method for studying connectivity of the human cerebral cortex. J Neurosci 17: 3178–3184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips CG, Porter R (1962): Unifocal and bifocal stimulation of the motor cortex. J Physiol 162: 532–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purpura DP, McMurty JG (1965): Intracellular activities and evoked potential changes during polarization of motor cortex. J Neurophysiol 28: 166–185. [DOI] [PubMed] [Google Scholar]
- Ranck JB Jr (1975): Which elements are excited in electrical stimulations of mammalian central nervous system: a review. Brain Res 98: 417–440. [DOI] [PubMed] [Google Scholar]
- Rosenthal J, Waller HJ, Amassian VE (1967): An analysis of the activation of motor cortical neurons by surface stimulation. J Neurophysiol 30: 844–858. [DOI] [PubMed] [Google Scholar]
- Rudin DO, Eisenman G (1954): The action potential of spinal axon in vitro. J Gen Physiol 37: 505–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth BJ, Saypol JM, Hallet M, Cohen LG (1991): A theoretical calculation of the electric field induced in the cortex during magnetic stimulation. Electroencephalogr Clin Neurophysiol 18: 47–56. [DOI] [PubMed] [Google Scholar]
- Ruohonen J, Ilmoniemi RJ (1999): Modeling of the stimulating field generation in TMS. Electroencephalogr Clin Neurophysiol Suppl 51: 30–40. [PubMed] [Google Scholar]
- Rushton WA (1927): Effect upon the threshold for nervous excitation of the length of nerve exposed and the angle between current and nerve. J Physiol 63: 357–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speer AM, Willis MW, Herscovitch F, Daube‐Witherspoon M, Shelton JR, Benson BE, Post RM, Wasserman EM (2003): Intensity‐dependent regional cerebral blood flow during 1‐Hz repetitive transcranial magnetic stimulation in healthy volunteers studied with H2 15O positron emission tomography: I. Effects of primary motor cortex rTMS. Biol Psychiatry 54: 818–825. [DOI] [PubMed] [Google Scholar]
- Talairach J, Tournoux P (1988): Coplanar stereotactic atlas of the human brain: 3‐dimensional proportional system: an approach to cerebral imaging. Stuttgart: Verlag. [Google Scholar]
- Tandon N, Narayana N, Zamarripa F, Lancaster J, Fox P (2001): Connectivity of the human supplementary motor area revealed by concurrent TMS and PET. Neuroimage 13: 1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson CJ, Paus T, Clanc R 1998. Magnetic shielding requirements for PET detectors during transcranial magnetic stimulation. IEEE Trans Nucl Sci 45: 1303–1307. [Google Scholar]
- Trachina D, Nicholson C (1986): A model for the polarization of neurons by extrinsically applied electric fields. Biophys J 50: 1139–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassermann, EM , Wang B, Zeffiro T, Sadato N, Pascual‐Leone A, Toro C, Hallet M (1996): Locating the motor cortex on the MRI with transcranial magnetic stimulation and PET. Neuroimage 3: 1–9. [DOI] [PubMed] [Google Scholar]


