Abstract
New zirconia compositions with optimized esthetic properties have emerged due to the fast-growing technology in zirconia manufacturing. However, the large variety of commercial products and synthesis routes, make impossible to include all of them under the general term of “monolithic zirconia ceramics”. Ultra- or high translucent monolithic formulations contain 3–8 mol% yttria, which results in materials with completely different structure, optical and mechanical properties. The purpose of this study was to provide an update to the current knowledge concerning monolithic zirconia and to review factors related to strength and aging resistance. Factors such as composition, coloring procedures, sintering method and temperature, may affect both strength and aging resistance to a more or less extend. A significant reduction of mechanical properties has been correlated to high translucent zirconia formualtions while regarding aging resistance, the findings are contradictory, necessitating more and thorough investigation. Despite the obvious advantages of contemporary monolithic zirconia ceramics, further scientific evidence is required that will eventually lead to the appropriate laboratory and clinical guidelines for their use. Until then, a safe suggestion should be to utilize high-strength partially-stabilized zirconia for posterior or long span restorations and fully-stabilized ultra-translucent zirconia for anterior single crowns and short span fixed partial dentures.
Keywords: Monolithic zirconia ceramics, Strength, Aging
1. Introduction
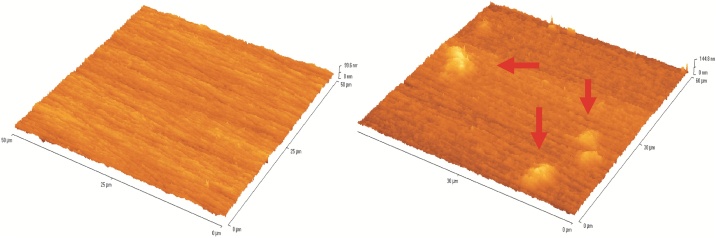
Zirconia was suggested as the first candidate for full contour monolithic restorations due to its significant advantages, such as excellent mechanical properties, superior to those of other ceramic systems, esthetic performance comparable to that of metal-ceramic restorations, radiopacity, low corrosion potential, good chemical properties, volumetric stability and elastic modulus values comparable to steel [[1], [2], [3], [4], [5], [6]]. According to in-vitro studies, zirconia restorations exhibit flexural or bending strength values of 900–1200 MPa and resistance to fracture of 9–10 MPa [7]. However, zirconia ceramics do suffer from low-temperature degradation (LTD), also known as aging [8]. In particular, the spontaneous and progressive transformation of the tetragonal phase to monoclinic degrades the mechanical properties of the Y-TZP and, in particular, its strength. Specific processing conditions, environmental humidity, stress and temperatures between 200–300 °C may accelerate it [5,[8], [9], [10]]. Many experimental studies have shown that water molecules can penetrate the zirconia structure when exposed to a hygroscopic environment. The triatomic character of yttrium contributes to the presence of several oxygen vacancies in the zirconia lattice, which facilitates the diffusion of water molecules into its mass [8]. The diffusion of water initially causes a lattice contraction that will result in tensile stresses’ concentration on the surface of the zirconia grains resulting in the transformation of the tetragonal phase to monoclinic phase. The increase in volume, that accompanies the transformation of a tetragonal grain to monoclinic, causes surface uplifts (Fig. 1) and grain pull out. This causes microcracks, which facilitate further the access of the water molecules within the internal grains and therefore the surface initial tetragonal to monoclinic transformation progresses deeper and deeper into the bulk of the material. As the microcracks grow and this process continues, the material fractures. Microstructural factors such as grain size, percentage of stabilizer, residual stresses and manufacturing imperfections may affect this phenomenon [[10], [11], [12]].
Fig. 1.
AFM images showing increased roughness and surface uplifts (red arrows on the right image) of transformed 3Y-TZP zirconia grains after aging in autoclave for 10 h.
Although a remarkable number of studies investigating the properties of zirconia ceramics currently exists, due to the fast growing of zirconia technology, new materials are released in the dental market, which have not been adequately evaluated. Consequently, the purpose of this paper was to provide an update to the current knowledge concerning strength and aging resistance of monolithic zirconia ceramics, aiming at highlighting the advantages and weaknesses of conventional and newly-released materials, through the data presented in recent literature.
2. Factors affecting strength and aging resistance of monolithic zirconia
2.1. Synthesis of zirconia nanowpowder for dental restorations
The first step towards the fabrication of monolithic zirconia restorations is the synthesis of the appropriate yttrium stabilized zirconia nanopowder. Nanopowder should be of high purity and with a narrow range of particle sizes, in order to yield densified structures of the desired crystallography. The properties of the starting powders are controled by the method of their production. In order to achieve higher densification, various methods have been developed for synthesizing nanoscale zirconia. These include co-precipitation, hydrothermal treatment, sol-gel, solution combustion synthesis, and mechanochemical processing. In the co-precipitation method, the desired cations are dissolved in an aqueous solution where a chemical precipitant agent is added to cause the precipitation of metal hydroxides. The precipitated powder is filtered, dried and calcined. By modifying the pH and temperature of the solution nucleation and growth mechanisms can be controlled. Although it is a low-cost method, broad particle size distribution and grain agglomeration are unavoidable [[13], [14], [15]]. Hydrothermal treatment involves an initial co-precipitation, followed by heat treatment at high temperatures to obtain an anhydrous crystalline powder. It is a low cost, soft and ecological method that allows good chemical homogeneity of the product. It can be combined with microwave (microwave-hydrothermal route) to supply further heat for the reactions. Its drawbacks are the long processing time and agglomeration, which leads to low sinterability [[16], [17], [18]]. The sol-gel method is based on hydrolysis and condensation reactions of inorganic salts and metal-organic compounds that form a sol which is converted into a gel. The gel is then dried and thermally treated to obtain a homogenous nano-powder. It is a low cost method, with relatively simple reaction conditions, that if properly monitored can tailor the microstructure and the chemical composition of the powder. Agglomeration is also a drawback of this method. A modified, nonaqueous sol-gel process has been recently proposed as a novel green method for the preparation of highly dispersive 3 mol% yttria-stabilized zirconia nanopowder with particle sizes of 15–25 nm [19]. In the solution combustion synthesis, different types of organic fuels (i.e. urea, glycine, sucrose, glucose) or their mixtures are typically dissolved in a solvent (i.e. water, hydrocarbons) with metal nitrate hydrates [20]. Two modes can be applied for the thermal treatment of the mixture. The first (volume combustion or thermal explosion) involves a sequential thermal treatment in various stages and the second (self-propagating combustion) the locally heating of a small portion of the reactive mixture to initiate an exothermic redox reaction between nitrate ions and the fuel, which self-propagates along with the rest of the volume in the form of a combustion wave. It is a fast method for preparing multicomponent, crystalline, homogeneous, with high purity and narrow particle size oxide nanopowders [[21], [22], [23]]. For mechanochemical processing, very pure oxide powders are mechanically mixed and milled before calcination. The advantage of mechanochemical synthesis is that it does not require any additional chemicals, such as organic solvents, however milling can result in contamination of the nanopowder, coarser inhomogeneous product and destabilization of the tetragonal zirconia through diffusion of yttrium towards the grain surface [24,25]. The synthesis by chemical routes, is usually more expensive than the mechanical methods, but offers a strict control of the powder characteristics, provided that a very carefull consideration of all the specific synthesis variables is involved.
2.2. CAD/CAM milling
Monolithic and core zirconia frameworks are fabricated through the CAD/CAM technology by milling commercially available blocks, which can be either pre-sintered or fully sintered. Pre-sintered blocks come from a fine grain or nanograin zirconia powder, synthesized as described in section 2.1., which is pressed to high-density compacts through cold isostatic pressing (CIP). Cold isostatic pressing is the most common method for compacting ceramic powders. During cold-isostatic pressing, pressure is applied at ambient temperature, gradually increasing from 50 to 400–1000 MPa and transmitted uniformly on zirconia powder until the green compacts reach 40–60% of their theoretical density prior to sintering [26,27]. Factors enhancing the densification and pore elimination during CIP are nano-sized powder particles, uniform particle size distribution, high specific surface area and low degree of agglomeration. CIP zirconia blocks require a relatively easier and faster milling procedure causing less wear of the machining tools but frameworks present a linear and non-uniform shrinkage of 20–25% during sintering [1,28] leading to non-uniform internal fit of Y-TZP copings [28]. Fully sintered blocks are prepared by presintering zirconia compacts at temperatures below 1500 °C to reach a density of at least 95% of the theoretical density. Following, hot isostatic pressing (HIP) is performed to increase densification by applying high pressure (50–200 MPa) and high temperature (400–2000 °C) via an inert isostatic gas pressure (e.g., argon or nitrogen). This process aims at eliminating sub-surface voids through a combination of plastic flow and diffusion. For densification of zirconia ceramics the temperature is elevated at temperatures ∼100–200 °C below its sintering temperature and for optimally sintering “green bodies” with no open porosity a remarkable increase in strength can be achieved by HIP [29] along with a small increase in densification [30]. Due to their high hardness and low machinability hard machining of HIP processes zirconia ceramics is more time consuming, requires tougher cutting tools and has been correlated to increased roughness, plastic deformation, surface damage, residual stresses’ development [31] and higher monoclinic phase transformation. The generated cracks, flaws and surface damage cannot be removed during the sintering process, and thus can cause early failure under mechanical loading.
2.3. Sintering
Different sintering methods have been proposed for the densification of CIP zirconia blocks. In general, they include conventional, microwave [32] and spark plasma sintering [33].
Conventional sintering of monolithic zirconia includes high temperatures and long heating times, thus being a time and energy consuming process. As it constitutes the most applied method of sintering, various studies have shown that differences in sintering parameters of zirconia can directly affect its microstructure and properties, such as translucency, grain size, and biaxial flexural strength [34,35]. A general trend is that as the sintering temperature increases, translucency and grain size also increase [[34], [35], [36]], but conflicting evidence exists regarding its effect on flexural strength. For core zirconia ceramics, an increase of sintering temperature above 1550 °C can cause a decrease in flexural strength [34], probably due to yttrium migration to the grain boundaries [37]. In the study of Ebeid et al. [36], who investigated various sintering times for monolithic zirconia, the authors concluded that even at 1600 °C the biaxial flexural strength was not affected. Similar were the results in a recent study by Sen et al. [38], who investigated various monolithic zirconia ceramics. They reported an increase in translucency by the increase in temperature through grain enlargement and reduction of grain boundaries that act as scattering centers, but no effect on biaxial flexural strength. Although translucency can be improved, larger grain size makes the material more susceptible to transformation [39] which may jeopardize its mechanical performance.
Microwave sintering is a low cost and time-consuming method. Its main advantage is that heating takes place through molecular interactions with the applied electromagnetic field and effective heating is achieved throughout the material [40] in significantly less time. In this way, the temperature gradients within the bulk of the material that are usually encountered during conventional sintering are avoided [41], which is important especially for large and geometrically complicated specimens, such as dental crowns. Almazdi et al. [42] compared density and flexural strength of specimens prepared from a commercial dental zirconia, and reported that the microwave-sintered specimens had a more uniform grain size distribution and were more closely packed than conventionally sintered specimens. No statistically significant difference was observed in the fracture toughness of various dental zirconia ceramics sintered in microwave or conventional ovens [43,44], suggesting that this method can be widely applied alternatively to conventional sintering. Recently Kim et al. [45] reported that microwave-sintered pre-colored monolithic zirconia ceramics exhibited similar color appearance and smoother surfaces compared to those conventionally sintered, but with reduced processing time and cost.
Spark plasma sintering, or plasma-activated sintering or field-assisted sintering technique (FAST), is a new promising method for very fast sintering leading to homogeneous and crack-free microstructures [46] with very limited porosity and high transparency. This technique provides direct contact between heating elements and samples, very rapid heating/cooling rates (several hundreds of °C min−1), and uniaxial mechanical pressure. Concerning yttrium stabilized zirconia, limited literature exists [[47], [48], [49]] but the results show that the material can reach very rapid densification with no cracks, shape distortions or density gradients in sintered samples with complex shapes and dimensions of centimeters [49]. However in-vitro studies are needed to evaluate the feasibility and effectiveness of this sintering method for monolithic zirconia ceramics.
2.4. Coloring of monolithic zirconia
For monolithic zirconia restorations, coloring can be achieved either by using pre-colored blocks or by immersing white zirconia restorations in coloring liquid or brushing their surfaces with it. Coloring liquids are solutions of metal oxides such as ferric chloride, manganese chloride, cerium acetate, cerium chloride, bismuth chloride, terbium (III) chloride, chromium (III) chloride, manganese (II) sulfate, etc. The effects of liquid-coloring on the properties of zirconia have been investigated in a few studies. In regards to LTD, liquid coloring has not been correlated with phase transformation but on the other hand, higher resistance to LTD compared to uncolored control specimens has been reported [50,51]. However, the mechanical properties of the liquid colored zirconia ceramics seem to be affected by the process. Although a few studies report no effect on flexural strength [[52], [53], [54]], there are a lot of studies emphasizing that immersion in coloring liquid can have detrimental effects on its flexural and fracture strength, hardness and densification [51,55]. Ban et al. [56] reported that in cases of liquids containing erbium (Er), and neodymium (Nd), both crystalline changes (presence of cubic phases) and decrease in mechanical properties can occur, attributed to the stabilization of the ions in the crystal lattice. Although significant t→m transformation is not recorded after aging, the increased grain size and open porosity attributed to some coloring oxides after sintering may negatively affect both the optical and mechanical properties [51].
Pre-coloring involves the synthesis of colored nanopowder by incorporating metal oxides such as Fe2O3 [57,58], Bi2O3 [57], CeO2 [59], Er2O3 [59,60], MnO2 [61,62] and Pr6O11 [60]. Doping oxides in pre-colored zirconia may have a negative effect on its mechanical properties [60]. This comes as a result of the changes in the crystal lattice that take place due to the replacement of a Zr ion with a metal ion. Depending on the valence and the ionic radius of the metal ion that enters zirconia crystal lattice, formation of oxygen vacancies and changes in lattice dimension (expansion or contraction) can occur [63], variously affecting both the mechanical/physical properties and color characteristics of zirconia [64,65]. By adding various amounts of Fe2O3 -which is the most common oxide for zirconia coloring- into a 3 mol% Y2O3 zirconia powder, Kao et al. [66] produced powders with varying combinations of red and yellow. Although the densification and sintering of the powders were improved, the size of zirconia grains as well as the monoclinic content was increased along with Fe content, making it necessary to reduce the total amount of the applied oxide [66].
3. Strength of monolithic zirconia
Although dental zirconia is the strongest dental material in terms of flexural strength and fracture resistance, during the last few years, the translucency of zirconia ceramics has increased at the expense of strength, and translucent full-contour, monolithic zirconia restorations have become increasingly popular as a result of advances in CAD/CAM technology. There are 2 types of monolithic zirconia materials; opaque and translucent zirconia. Opaque zirconia offers significantly greater flexural strength and is indicated for the posterior regions of the mouth, while translucent zirconia has the more natural esthetic appearance but lower mechanical properties. The presence of cubic zirconia in translucent compositions is responsible for the enhanced optical properties; however, a significant reduction of the mechanical properties is a consequent drawback. The mechanical strength of monolithic zirconia was evaluated in many studies, depicted in the following tables (Table 1, Table 2).
Table 1.
Studies investigating the strength of monolithic zirconia crowns. Studies are presented in ascending chronological order.
| Authors | Zirconia system | Test type/Methodology | Results | |
|---|---|---|---|---|
| Beuer et al. (2012) [67] | - Zirlunaa | Fracture strength, molar crowns, loading in chewing simulator, crosshead-speed 0.5 mm min−1. | Higher strength of monolithic compared to veneered zirconia | |
| Zhang et al. (2012) [68] | - Lava | Chipping test (Vickers) on zirconia and glass-infiltrated monolithic zirconia molar crowns | Chipping resistance: glass-infiltrated monolithic zirconia crowns comparable to monolithic zirconia and significantly higher compared to veneered zirconia crowns | |
| - In-Ceram Zirconia YZ | ||||
| Sun et al. (2014) [69] | - Lava Frame (MZC) | Axial load, molar crowns of varying occlusal thickness (0.6–1.5 mm), crosshead speed of 0.5 mm min−1. | MZC exhibited higher fracture loads than MLC, LZC and MCC. The fracture resistance of MZC (1.0 mm) was equal to MCC. Doubling the monolithic zirconia core from 0.6 mm to 1.5 mm increased the fracture resistance system threefold. | |
| - IPS e.max Press (MLC) | Cementation with resin cement | |||
| - Layered zirconia crowns (LZC) | ||||
| - Metal ceramic crowns (MCC) | ||||
| Nakamura et al. (2015) [70] | - Lava Plus | Fracture strength, molar crowns cemented to composite dies, crosshead-speed 0.5 mm min−1 | The occlusal thickness significantly affected the fracture load, but not the axial thickness. Higher strength compared to monolithic lithium disilicate crowns. | |
| Zhang et al. (2016) [71] | - Lava Plus | Fracture strength, molar crowns cemented to composite dies, crosshead-speed 0.1 mm min−1. | The stiffer and stronger zirconia and lithium disilicate crowns afforded superior stress shielding of the tooth interior and inhibited crack initiation | |
| Sorrentino et al. (2016) [72] | - Aadva | Fracture test, axially loaded molar crowns of various thicknesses (0.5, 1, 1.5 and 2 mm), crosshead speed 1 mm min−1 | The occlusal thickness did not influence the fracture resistance and the mode of failure of the restorations. | |
| Schriwer et al. (2017) [73] | Soft machined | - Bruxzir | Fracture strength, axially loaded premolar crowns from hard and soft machined zirconia ceramics, crosshead speed 0.5 mm min−1 | The hard-machined Y-TZP crowns had the best margin quality and the highest load at fracture. The BX and the PZ group had statistically significant weaker load at fracture than the other groups. Margin defects affected negatively the load at fracture. |
| - ICE Zirkon | ||||
| - DD Bio ZX2 | ||||
| − NobelProcera | ||||
| Hard machined: | - Denzir Y-TZP | |||
| - Denzir Mg-PSZ | ||||
| Rohr et al. (2018) [74] | - VITA YZ T | Fracture strength, implant supported monolithic crowns, crosshead speed 1 mm min−1 | For uncemented crowns the initial fracture initiated from the internal surface, for cemented crowns from the loading point. VITA YZ T presented the highest flexural strength and fracture strength. Increased compressive strength of the cement was correlated to high fracture toughness, but not for monolithic zirconia. | |
| - VITA In-Ceram AL VITABLOCS | Crowns cemented with temporary, adhesive dual-cured cements cement and self-adhesive dual-cured cement. | |||
| - Mark II VITA ENAMIC | ||||
| - IPS e.max CAD | ||||
| Tsuyuki Y et al. (2018) [75] | - Adamant, Tokyo, Japan | Fracture strength, crosshead speed 1 mm min−1. | The presence of an occlusal groove decreased fracture strength but to a smaller degree when resin cement was used. The use of glass ionomer cement was associated with lower fracture strength. | |
| Different types of abutments fabricated with different depths of occlusal groove or abscesnce of groove. Evaluation of the effects of abutment morphology, crown thickness and cement type. | ||||
| Moilanen et al. (2018) [76] | - PSZ Prettau | Fracture strength, 45° angle to the long axis, crosshead speed 1 mm/min. | Cementation of the crown on a titanium base was correlated to higher fracture strength compared to direct cementation on the implant’s surface. | |
| - FSZ Prettau Anterior | A titanium base on the implant surface was evaluated with regard to its effect on the monolithic crown’s fracture strength. | |||
The composition of the materials presented in this and all the tables in the manuscript are presented in Table 5.
Table 2.
Studies investigating mechanical properties of monolithic zirconia specimens. Studies are presented in ascending chronological order.
| Authors | Zirconia system | Test type/Methodology | Results | |
|---|---|---|---|---|
| Zhang et al. (2013) [106] | Experimental monolithic zirconia | Chipping (Vickers) and flexural strength (3- and 4- point bending, specimens cemented on composite), crosshead speed 1 mm min−1 | Monolithic restorations exhibited superior fracture resistance relative to their porcelain-veneered counterparts and higher resistance to failure than lithium disilicate glass–ceramics | |
| Basso et al. (2015) [108] | - IPS e.max ZirCAD | Flexural strength (3-point bending), monolithic and trilayer (zirconia core, fusion glass, veneer) specimens, crosshead-speed 0.5 mm min−1. | No significant differences between monolithic and trilayer structures | |
| Sulaiman et al. (2015) [100] | - Prettau (PSZ) | Biaxial strength test (piston-on-three balls), crosshead-speed 1 mm min−1. | Unstained PSZ had significantly higher strength than unstained FSZ. After staining both had similar strength. | |
| - Prettau, Anterior (FSZ) | ||||
| Schatz et al. (2016) [114] | - Ceramill Zolid (C) | Biaxial, 3-point, and 4-point flexural strength testing, crosshead speed 1 mm min−1 | No significant difference among the different ceramics. | |
| - Zenostar Zr (Z) | The 4-point flexural strength testing shows the lowest flexural strength data; biaxial test method the highest. | |||
| - DD Bio ZX2 | ||||
| Tong et al. (2016) [97] | - Zpex (High-Translucency) | Fracture toughness test (edge chipping), Vickers hardness test and flexural strength test (4-point bending) of specimens, crosshead-speed 0.1 mm min−1. | High-strength Y-TZP exhibited the best and high-translucency the worst mechanical properties. The opposite was for the translucency. | |
| - TZ-3YS-E (High-Strength) | ||||
| - TZ-3Y-E (High-Surface Area) | ||||
| Vichi et al. (2016) [104] | - IPS e.max Zir-CAD | Flexural strength (3-point bending test), crosshead-speed 1 mm min−1. | The new “augmented translucency” TZPs (VITA In-Ceram YZ HT and inCoris TZI) specimens showed higher translucency and similar flexural strength than “traditional” TZPs. | |
| - inCoris ZI | ||||
| - inCoris TZI | ||||
| - In-Ceram YZ | ||||
| - In-Ceram YZ HT | ||||
| Zhang et al. (2016) [102] | - TZ-3YE | Flexural strength (4-point bending), crosshead speed 1 mm min−1, hardness (Vickers indentation), toughness (Single-etchV-notch beam) | Increasing the yttria content decreased the fracture toughness and flexural strength but increased resistance to aging. The addition of La2O3 decreased the flexural strength but did not influence hardness and toughness. | |
| - Zpex | ||||
| - Zpex Smile | ||||
| - Experimental monolithic 1 | ||||
| - Experimental monolithic 2 | ||||
| Carrabba et al. (2017) [103] | - Aadva Standard Translucency [ST] | Flexural strength (3-point bending), crosshead-speed 1 mm min−1. | There was an inverse relationship between strength and translucency for the materials tested. Addition of Al2O3 and increased yttria content strongly downgraded the mechanical properties. | |
| - Aadva Enamel Intensive [EI] | ||||
| - Aadva Natural Translucency [NT] | ||||
| Chougule et al. (2017) [112] | Lava | Flexural strength (3-point bending test), crosshead-speed of 0.5 mm min−1. | Flexural strength was significantly higher after glazing but not after polishing. | |
| Church et al. (2017) [64] | BruXZir Shaded 16 | Flexural strength (3-point bending), crosshead-speed of 1 mm min−1. | The flexural strength of highly translucent zirconia materials was significantly higher than those of lithium disilicate. No statistically significant differences among the various monolithic ceramics were recorded. | |
| BruXZir HT | ||||
| Lava Plus | ||||
| inCoris TZI C | ||||
| Elsaka et al. (2017) [98] | - Ceramill Zolid FX | Flexural strength (3-point bending test), crosshead-speed 0.5 mm min−1, fracture toughness (3-point bending test), crosshead speed 0.5 mm min−1, Vickers hardness | ZT monolithic zirconia revealed higher flexural strength and fracture toughness compared with CZF and PA | |
| - Multilayer (CZF) | CZF revealed higher hardness compared with PA and ZT. | |||
| - Prettau Anterior (PA) | ||||
| - Zenostar T (ZT) | ||||
| Munoz et al. (2017) [99] | - Prettau Anterior | Biaxial flexural strength, crosshead-speed 1 mm min−1 | Pretatu Anterior presented the lowest strength which was significantly reduced by mechanical and thermomechanical cycling | |
| - Prettau | Hydrothermal degradation; mechanical cyclic load; mechanical cyclic plus hydrothermal degradation (H + M); non-treated specimens (control group). | |||
| - ICE Zirkon | ||||
| Ozer et al. (2017) [110] | - Pretau | Biaxial flexural strength (piston-on-three balls strength), crosshead-speed 0.5 mm min−1 | Statistically higher strength of the thicker specimens, but both had higher than the reported masticatory forces Airborne-particle abrasion increased the flexural strength of monolithic zirconia. Grinding did not affect flexural strength if subsequently polished | |
| Disc specimens of 0.8 and 1.3 mm : | ||||
| - untreated (control) | ||||
| - airborne-particle abrasion | ||||
| - grinding with a diamond rotary instrument followed by polishing. | ||||
| Sulaiman et al. (2017) [101] | - Prettau | Flexural strength (3-point bending), crosshead-speed 0.5 mm min−1. | The strength of FSZ was approximately half that of PSZ. Staining enhanced the strength of FSZ, with no effect on PSZ. Airborne-particle abrasion lowered the strength of FSZ, while enhanced that of PSZ. Artificial aging had no effect on the flexural strength of either. | |
| - Prettau, Anterior | ||||
| - ICE Zircon | ||||
| Kumchai et al. (2018) [111] | - inCoris TZI | Flexural strength (3-point bending test), crosshead-speed of 0.5 mm min−1. | Overglazing significantly decreased the flexural strength. | |
| - Prettau | - heat treated (glazed with no paste) | Heat treatment had no significant effect on the flexural strength. There was no significant difference in the flexural strengths of different brands | ||
| - Zirlux FC | - overglazed (use of glaze paste) | |||
| Two different glaze materials: | ||||
| - Zirkonzahn glaze paste + liquid | ||||
| - Zirlux FC glaze paste + liquid | ||||
| Sakai et al. (2019) [109] | - translucent TZP (Zpex, Tosoh) | Biaxial flexural strength, Monolithic zirconia materials of different tranclucencies were adhered and evaluated as a method for more accurate colour simulation. | Flexural strength was not affected negatively. | |
| - high- translucency PSZ (ZpexSmile, Tosoh) | ||||
| Reis et al. (2019) [80] | Vita In Ceram YZ | Nano-indentation (hardness evaluation), pulse-echo (elastic modulus), scratch test | Silica infiltration increased the hardness but reduced the fracture toughness. Adhesion of feldspathic porcelain to non-infiltrated zirconia proved to be stronger | |
| - monolithic zirconia | ||||
| - silica infiltrated monolithic zirconia(via the sol-gel method) | ||||
| - zirconia + feldspathic porcelain of two thicknesses | ||||
| - silica infiltrated zirconia + feldspathic porcelain of two thicknesses | ||||
| Juntavee et al. (2018) [96] | Y-TZP, VITA YZ HT color® | Flexural strength (3-point bending), crosshead speed 1 mm min−1 | Increasedsintering temperature and prolonged sintering holding time was correlated with higher flexural strength | |
| Sintering at different temperatures: | Sintered holding times: | |||
| - decreasing | - shortening | |||
| - regular | - regular | |||
| - increasing | - prolonged | |||
| Yan et al. (2018) [107] | dental zirconias (the Luxisse series) | Flexural strength (piston-on-three balls) ceosshead speed 1 mm min−1, specimens bonded to a dentin-like substrate | The load-bearing capacity of the lithium disilicate ceramic presented higher values than 5Y-TZP. | |
| - 5Y-PSZ | ||||
| - 4Y-PSZ | ||||
| - 3Y- TZP (control) | ||||
| IPS e.max CAD | ||||
| Candido et al. (2018) [105] | - Prettau Zircon | Flexural strength (four-point bending) crosshead speed 1 mm min−1 | Flexural strength did not present significant difference between monolithic and conventional zirconia. | |
| - ICE Zirkon Transluzent | ||||
| - BloomZir | ||||
| Nishioka et al. (2018) [81] | - Feldspathic ceramic (VITABLOCS Mark II) | Flexural strength (piston-on-three balls) under water (staircase approach :100,000 cycles at 10 Hz) | The highly translucent polycrystalline zirconia can withstand a higher cyclic load before failure | |
| - Polymer-infiltrated ceramic network (VITA Enamic) | ||||
| - Zirconia-reinforced lithium silicate glass-ceramic (VITA Suprinity) | ||||
| - Lithium disilicate glass-ceramic (IPS e.Max CAD) | ||||
| - High translucent yttrium partially stabilized tetragonal zirconia polycrystals (Zirconia YZ HT) | ||||
| Ozer et al. (2018) [86] | Prettau | Flexural strength (piston-on-three balls), crosshead speed 0.5 mm min−1 (disks of thickness 0.8 mm and 1.3 mm) | 1.3 mm specimens presented significantly higher flexural strength. Airborne-particle abrasion significantly increased the flexural strength. Grinding and polishing didn not affect the flexural strength | |
| - airborne-particle abrasion, 50-mmAl2O3 particles (pressure of 400 kPa, distance of 10 mm) | ||||
| - grinding with a diamond rotary instrument followed by polishing | ||||
| - control | ||||
| Ebeid et al. (2018) [95] | Bruxzir | Biaxial flexural strength (piston-on-three balls), crosshead speed 0.5 mm min−1 | Surface treatment at the pre-sintered was correlated with higher flexural strength | |
| - air-abrasion with Al2O3 50 mm particles | ||||
| - silica coating with 30 mm Rocatec soft particles | ||||
| - control (no surface treatment) | ||||
| - the surface treatments were performed either at the pre-sintered stage or the post-sintered stage | ||||
| Zucuni et al. (2017) [115] | Zenostar blank | Flexural strength (piston-on-three balls), fatigue tests included 20,000 cycles and a frequency of 6 Hz | -polishing after grinding is mandatory in order to avoid strength deterioration | |
| - control | - heat treatment is not a good alternative to polishing | |||
| - grinding | - polishing enhances fatigue | |||
| - polishing | ||||
| - glazing | ||||
| - heat treatment | ||||
| - polishing + heat treatment | ||||
| - polishing + glazing | ||||
Concerning fracture resistance of monolithic zirconia crowns, a clear superiority exists for full-contour monolithic crowns, even if they are glass-infiltrated [68], compared to veneered bilayer [67,77,78] and lithium disilicate crowns [[69], [70], [71],79]. Reis et al. [80], used the sol-gel method to infiltrate zirconia surfaces with silica in order to eliminate veneering ceramic delamination. This procedure only enhanced the structural homogeneity and hardness of monolithic zirconia, but it reduced its fracture toughness.
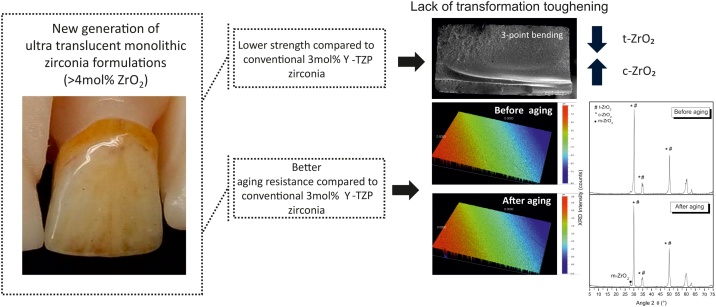
After cyclic loading, high translucency tetragonal zirconia demonstrated the higher fatigue strength among a feldspathic ceramic, a polymer-infiltrated ceramic network, a lithium disilicate glass-ceramic and a zirconia-reinforced lithium silicate glass-ceramic [81]. According to Pereira et al. [82], third generation ultra-translucent monolithic zirconia materials present no transformation toughening when aged as well as significantly inferior mechanical properties. All fractures started from surface defects on the tensile surface. High-translucency monolithic zirconia has a reduced bi-axial flexural strength compared to conventional zirconia, but it is appropriate for clinical us [83]. According to Camposilva et al. [84], translucent zirconia presents significantly lower toughness and strength compared to conventional zirconia ceramics and it should be considered carefully for clinical application.
The occlusal thickness of the crown has shown to be correlated to fracture [69,70], as well as the presence of an occlusal groove [75]. Monolithic zirconia crowns cemented on abutments with an occlusal groove presented lower fracture resistance compared to crowns cemented on abutments with flat occlusal surfaces [75]. Sun et al. [69], reported a threefold increase from 0.6 to 1.5 mm, but on the contrary, Sorrentino et al. [72] did not find any significant correlation. It has recently been reported by Weigl et al. [85], that monolithic zirconia crowns with a thickness of 0.5 mm ensure acceptable strength regardless of the type of cementation, following in-vitro cyclic loading to simulate the clinical function of the restoration. However, thickness of 0.2 mm was too low to establish predictability, regardless of cement type. Ozer et al. [86] suggest that thickness between 0.7 and 1.3 mm are ideal for the fabrication of monolithic zirconia restorations and air-borne particle abrasion enhances the materials flexural strength, whereas grinding and polishing did not influence the material’s strength. Schriwer et al. [73] investigated the strength of hard machined versus soft machined premolar crowns and resulted that the hard-machined Y-TZP crowns had the best margin quality and the highest load at fracture, pointing out the significance of good marginal fit for higher performance. Sarikaya et al. [87] reported that Bruxzir and Incoris TZI monolithic zirconia systems present acceptable resistance to fracture for the fabrication of monolithic crowns when tested at physiologic mastication forces. Overall, several studies have concluded that high translucency cubic zirconia presents significantly lower mechanical properties due to the absence of transformation toughening mechanism and this can compromise their use in clinical cases where high loads are applied [84,88]. An increase of yttrium oxide percentage in zirconia ceramics can lead to a reduction of the mechanical strength, but only following artificial aging [88]. However, even the high-translucency materials demonstrate fracture strength acceptable for clinical application exceeding 3000 N [88]. According to Yin et al. [89], the fracture strength of monolithic zirconia crowns increased after treatment with polishing burs and polishing can reduce the monoclinic phase.
Several studies have evaluated the fracture resistance of monolithic zirconia crowns retained by implants. According to Moilanen et al. [76], the fabrication technique of monolithic zirconia implant-retained crowns using a prefabricated titanium base led to crowns with superior strength to static mechanical testing compared to crowns fabricated directly on the implant surface. According to Rohr et al. [74], the use of resin cements with high compressive strength was found to be correlated linearly to fracture resistance and flexural strength of implant-supported monolithic zirconia crowns. Elshiyab et al. [90] proved that after 5 years equivalent chewing simulation, implant retained monolithic zirconia crowns survived, although their resistance to fracture had decreased.
The effect of grinding and polishing on monolithic zirconia restorations has been evaluated by a few studies. In the study of Khayat et al. [91], grinding was found to increase the surface roughness of monolithic zirconia and decrease the flexural strength. However, polishing after grinding leads to the preservation of the flexural strength. The authors suggest that monolithic zirconia’s mechanical strength can be compromised when zirconia surfaces are left rough leading to higher susceptibility to aging. The monolithic zirconia ceramic evaluated was not compromised by grinding and low-temperature degradation and both thicknesses tested maintained acceptable mechanical strength [92]. Polishing after grinding was determined mandatory in order to prevent crack propagation and to enhance the material’s fatigue [93]. A 2nd generation zirconia ceramic was submitted to grinding and artificial aging to assess its fatigue strength and survival rates and it was found that its properties were not compromised [94].
In order to evaluate sintering parameters for monolithic zirconia, specimens were submitted to air-borne particle abrasion and silica coating in the pre-sintered stage and this led to higher biaxial flexural strength. Thus, surface pre-treatment in the pre-sintered stage of monolithic zirconia might be beneficial to the final restoration’s strength [95]. Juntavee et al. [96] studied the effect of sintering temperature and duration alterations and proved that high sintering temperature combined with long sintering time attribute higher flexural strength and hence translucent monolithic zirconia restorations with higher strength.
Based on the majority of the studies included in Table 2, it can be concluded that high translucent specimens of zirconia ceramics with yttrium content >3 mol% present significantly lower strength compared to the partial stabilized 3 mol% Y-TZP ones (Fig. 2) [[97], [98], [99], [100], [101], [102], [103]]. However, translucent zirconia ceramics with 3 mol% Y-TZP presented similar strength compared to conventional 3 mol% Y-TZP ceramics [64,104]. In addition, Candido et al. [105] reported that the monolithic zirconia tested showed similar flexural strength to a conventional zirconia ceramic. All monolithic zirconia specimens presented higher strength compared to lithium disilicate ones [64,106], although this is not in agreement with a recent study by Yan et al. [107] who reported that when bonded on a dentin-like substrate, lithium disilicate presented higher load-bearing capacity compared to an ultra-translucent 5Y-PSZ ceramic. Compared to veneered specimens one study reported higher strength for bilayer [106] and another similar strength for trilayer specimens [108]. Sakai et al. [109] reported that layering zirconia of various translucencies with resin cement between the layers is a method that improves the optical properties of the restoration while maintaining the flexural strength of the monolithic zirconia ceramic. Sulaiman et al. [100,101] investigated the effect of staining on partially and fully stabilized zirconia specimens and reported a significant increase of strength for fully stabilized monolithic zirconia ceramics. Air-borne particle abrasion had a positive effect on the strength of partially stabilized but a detrimental effect to fully stabilized zirconia specimens [100,110], while glazing had either no effect [111] or positive effect [112] on partially stabilized zirconia specimens. According to Nam et al. [113], glazing of translucent monolithic zirconia plates led to a significant reduction in flexural strength, whereas low-temperature degradation did not present any significant effects.
Fig. 2.
Graphical summary with the major findings of this review regarding strength and aging resistance of high translucency zirconia ceramics.
3.1. Aging resistance
Aging resistance of monolithic zirconia restorations is a fundamental property as the whole surface is exposed to aggressive oral conditions. The aging behavior of zirconia is generally investigated through an accelerating aging test in an autoclave [116]. According to theoretical calculations, 1 h at 134 °C corresponds to 3–4 years in-vivo. By this, 10 h of in-vitro aging, have theoretically the same effect as a restoration in the oral cavity for 30–40 years, which is a more than sufficient lifespan for a fixed partial denture (FPD). Despite the criticism that this test does not correspond to actual clinical conditions and that it may underestimate the actual degradation of zirconia ceramics in the oral environment [117], it still remains an efficient method to estimate the long-term performance of these materials. Other tests include boiling in hot water or artificial saliva, mechanical cyclic loading, thermocycling, and combinations of mechanical and thermal fatigue.
Autoclave aging has been correlated to no significant change in strength [84,118,119], as well as to significant decrease and increase depending on time of treatment, brand and composition [120,121] of the zirconia system investigated (Table 3, Table 4). Comparing 3 mol% Y-TZP ceramics with translucent monolithic ceramics of higher yttrium amount [101,121,122], significantly higher resistance to aging degradation was recorded for the new generation translucent ceramics, but only after prolonged aging [84,121]. This is not in agreement with Almansour et al. [83], whose study found significant differences in several monolithic zirconia systems following shorter periods of aging. In a recent study [121], the monoclinic phase fraction increased remarkably between 5 and 50 h of aging, especially for Prettau and BruxZir, and less for Katana ML and Katana HT13. The aged specimens had a detectable layer of transformed material which reached ˜60 μm in Prettau and BruxZir and less than 5 μm in Katana ML and HT13. Although significant differences were recorded, these exceedingly long periods of accelerating autoclave treatment (usually after 10 h) are beyond the clinical lifespan of a restoration. In the other three studies [99,101,122] investigating the ultra-translucent Pretau Anterior zirconia, no significant differences in strength were recorded after 8 h of steam autoclave treatment in two of the studies [101,122] and significant reduction in one studies [99]. Similarly, no significant change in strength was recorded in another study [84], neither for 3 mol% nor for 5.5 and >6 mol% translucent zirconia ceramics, even after the significant amount of m-ZrO2 present on their surface (Table 5).
Table 3.
Studies investigating mechanical properties of monolithic zirconia specimens/crowns after hydrothermal aging (steam autoclave and boiled water/artificial saliva). Studies are presented in ascending chronological order.
| Authors | Zirconia system | Test type /Aging test | Flexural strength change | m-ZrO2 content | ||
|---|---|---|---|---|---|---|
| Specimens | ||||||
| Alghazzawi et al. (2012) [118] | − 5.3 mol% Y2O3 | Flexural strength (piston-on-three balls), crosshead-speed 1 mm min−1 | No significant change | Control = 2.4 ± 0.6% | ||
| Boiled: 100 °C, 7 days, artificial saliva | Aged = 21.0 ± 2.0% | |||||
| Dehestani and Adolfsson (2013) [125] | - 3Y-TZP | Flexural strength (4-Point Bending) | No significant change. 3Y-TZP containing materials showed the highest strength | Values cannot be extrapolated. 12Ce-TZP: almost no change in m-ZrO2, 10Ce-TZP: m-ZrO2 up to 90% and 3Y-TZP: m-ZrO2 ˜ 50% after 32 days. | ||
| - 3Y-TZP/Al2O3 | Aging in water at 90 °C for 2, 4, and 6 months | |||||
| - 12Ce-TZP/Al2O3 | ||||||
| - 10Ce-TZP /Al2O3 | ||||||
| All composites had 70/30 vol zirconia/alumina | ||||||
| Adabo et al. (2015) [122] | - ICE Zirkon | Flexural strength (piston-on-three balls), crosshead-speed 1 mm min−1 | No significant change | No values are reported, however all specimens presented increase | ||
| - Prettau | Steam autoclave: 120 °C, 2 kg/cm2, 8 h | |||||
| - Prettau Anterior | ||||||
| Alghazzawi et al. (2015) [120] | - Lava Plus (Lav) | Flexural strength (3-point bending), crosshead speed 0.5 mm min−1 | Coupons: | N/A | ||
| - Argen HT (Arg) | Steam autoclave: 134 °C, 0.2 MPa, 50 hours | - increase for Arg, Zir and Zen | ||||
| - Zirlux (zir) | - no significant change for Lav, Brux and DDB | |||||
| - BruxZir (Bru) | ||||||
| - Zenostar (Zen) | ||||||
| - DDBioZX2 (DDB) | ||||||
| Pereira et al. (2016) [124] | - Zirlux FC | Flexural strength (piston-on-three balls), grinded specimens (diamond burs, water cooling), crosshead speed 1 mm min−1 | Significant increase of characteristic strength for control, no significant change for the rest | Before aging | After aging | |
| Steam autoclave: 134 °C, 2 bars, 20 h | Control | 0% | 67.97% | |||
| Fine grinded | 9.49% | 38.74% | ||||
| Coarse grinded | 9.66% | 42.76% | ||||
| Stawarczyk et al. (2016) [119] | - Zenostar | Flexural strength (4-Point Bending), crosshead-speed 1 mm min−1 | No significant change. All monolithic showed lower flexural strength values compared to the conventional zirconia. | N/A | ||
| - DD Bio ZX2 | Steam autoclave: 134 °C, 2.3 bars, 5 h | |||||
| - Ceramill Zolid | ||||||
| - InCoris TZI | ||||||
| - Ceramill ZI | ||||||
| Flinn et al. (2017) [121] | - Prettau | Flexural strength (4-point bending), crosshead speed 0.5 mm min−1 | Significant reduction only for Prettau and BruxZir | Before aging (%) | After aging for 200h (%) | |
| - BruxZir | Steam autoclave: 134 °C, 0.2 Mpa, 5, 50, 100, 150, and 200 h | Prettau | 2.90 ± 0.34% | 76.1 ± 0.64% | ||
| - Katana HT13 | BruxZir | 2.69 ± 0.18% | 76.0 ± 0.26% | |||
| - Katana ML | Katana HT | 4.6 ± 0.19% | 35.8 ± 0.80% | |||
| Katana ML | 3.57 ± 0.35% | 33.2 ± 1.1% | ||||
| Guilardi et al. (2017) [123] | - InCeram YZ | Flexural strength (piston-on-three balls), fine and coarse grinded specimens (diamond burs under water cooling), crosshead speed 1 mm min−1 | No significant change. Grinding affected positively the material’s aging sensitivity. | Before aging (%) | After aging (%) | |
| Steam autoclave: 134 °C, 2bars, 20 h | Control | 0 ± 0.0 | 76.1 ± 0.64 | |||
| Fine grinding | 9.70 ± 0.89 | 24.42 ± 3.45 | ||||
| Coarse grinding | 13.07 ± 1.5 | 40.94 ± 1.61 | ||||
| Khayat et al. (2017) [91] | Tizian Blank Translucent | Flexural strength (piston-on-three balls), crosshead-speed 0.5 mm min−1 | Grinding significantly increased roughness and decreased strength. Grinding and polishing had no significant effect on flexural strength. Rough zirconia was more prone to aging. | N/A | ||
| Steam autoclave: 134 °C, 200 kPa, 3 h | ||||||
| Specimens were: | ||||||
| - grinded | ||||||
| - grinded and polished (polishing kit 1) | ||||||
| - grinded and polished (polishing kit 2) | ||||||
| - glazed | ||||||
| Munoz et al. (2017) [99] | - Prettau Anterior | Flexural strength (piston-on-three balls), crosshead-speed 1 mm min−1 | Significant difference for Pretau Anterior, but not for the others | Prettau Anterior | Pretau | ICE Zirkon |
| - Prettau | Steam autoclave: 134 °C, 0.2 MPa, 8 h | 0% | 39.71% | 24.89% | ||
| - ICE Zirkon | ||||||
| Sulaiman et al. (2017) [101] | - Prettau (PSZ) | Flexural strength (3-point bending test), crosshead speed 0,5 mm min−1. | No significant effect of either FSZ or PSZ | N/A | ||
| - Prettau Anterior (FSZ) | Steam autoclave: 125 °C, 200 kPa, 8 h | |||||
| - ICE Zircon (PSZ) | ||||||
| Camposilvan et al. (2018) [84] | - Aadva ST | Flexural strength (piston-on-three balls) | No significant change | Arithmetic values cannot be extrapolated from the graph. NT and ML showed no transformation at all, while ST and EI presented high amounts of m-ZrO2 (˜45%) | ||
| - Aadva EI | Steam autoclave: 134 °C, 2 bar, 0, 2, 6, 18, 54 h | |||||
| - Aadva NT | ||||||
| - Katana UT | ||||||
| Crowns | |||||
| Alghazzawi et al. (2015) [120] | - Lava Plus (Lav) | Fracture toughness, axially oriented molar crowns, crosshead speed 0.5 mm min−1 | - no significant effect | N/A | |
| -Argen HT (Arg) | Steam autoclave: 134 °C, 0.2 MPa, 50 hours | ||||
| - Zirlux (zir) | |||||
| - BruxZir (Bru) | |||||
| - Zenostar (Zen) | |||||
| - DDBioZX2 (DDB) | |||||
| Nakamura et al. (2015) [126] | Lava Plus | Fracture toughness, axially oriented molar crowns, crosshead speed 0.5 mm min−1 | Significant decrease up to 50 h of aging and no change thereafter. | 70% after 50 h of aging and no increase thereafter | |
| Combination of cycling loading (50, 300 N, 240,000 cycles, water) and autoclave treatment for 100 h | Cycling loading had no effect on strength. | ||||
| Steam autoclave: 134 °C, 0.2 Mpa, 0, 10, 50, 100 h | |||||
| Bergamo et al. (2016) [128] | - Ceramill Zolid | Fracture test, molar crowns: axial load, crosshead-speed 1 mm min−1 | No significant change | Control: 4% | |
| Steam autoclave: 122 °C, 2 bars, 1 h | Steam autoclave: up to 4.5% | ||||
| Leone et al. (2016) [127] | - GC Initial Zr: | Flexural strength (piston-on-three balls), crosshead-speed 1 mm min−1 | Significant change for ST. The presence of glaze had a protective effect. The mechanical properties of cubic crowns (UHT) were lower than for tetragonal ones. | No values are reported, complete absence of hydrothermal degradation for UHT. | |
| Ultra high translucency (UHT) | steam autoclave 134 °C, 2 bars, for 2, 6, 18 and 54 h | ||||
| High translucency (HT) | |||||
| Standard translucency (ST) | |||||
| Prado et al. (2017) [92] | Zirlux FC | Flexural strength, crosshead speed 1 mm min−1 | Low temperature degradation led to an increase in flexural strength | control group: 58.17% | |
| Aging: Grinding with extra-fine diamond burs (grit size 30 μm) under constant water-cooling, autoclave storage at 134 °C / 2 bar / 20h | ground samples: 9.25% | ||||
| ground + low temperature degradation: 16.13 | |||||
| Pereira et al. (2018) [82] | Katana YSZ ceramics used: | Flexural strength (piston-on-three balls), crosshead-speed 1 mm min−1, step stress fatigue approach, autoclave aging at 134 °C / 2 bars pressure/20 h | No significant change for STML and UTML. | - Increase for ML | |
| – ML/HT | Significant increase for ML. | - No impact on STML and UTML | |||
| - STML | |||||
| - UTML | |||||
| Almansour et al. (2018) [83] | - Lava Plus HT | Flexural strength (piston-on-three balls), crosshead-speed 0.5 mm min−1, fatigue (chewing simulator with 250,000 cycles / frequency of 1.6 Hz / load of 200 N), accelerated artificial aging at 3500 cycles (two water baths, 5 °C and 55 °C. 60 sec per cycle in 5 °C bath, 10 sec to transfer samples to 55 °C bath, 20 seconds in 55 °C bath and 10 seconds to transfer back to 5 °C bath | before: Ceramill ZI (935.3 ± 47.1 MPa)>Copran Zr-i Monolithic HT (847.8 ± 20.7 MPa)>Lava Plus (732.4 ± 25.5 MPa)>Ceramill Zolid White (685.7 ± 32.6 MPa) | Not evaluated | |
| - Ceramill Zolid White HT | after: Copran Zr-i Monolithic HT (777.5 ± 21.2 MPa)>Ceramill ZI (668.0 ± 20.1 MPa)>Lava Plus (666.4 ± 21.1 MPa)>Ceramill Zolid White (575.0 ± 36.3 MPa) | ||||
| - Copran Zr-i Monolith HT | |||||
| - Ceramill ZI-LT | |||||
| Dapieve et al. (2018) [94] | - Zirlux FC2 | Flexural strength, step-stress fatigue, 20 Hz and minimum stress of 10 MPa, 5000 cycles under 200 MPa + incremental steps of 25 MPa for 10,000 cycles from 400 MPa to complete failure | Fatigue strength change: aging increased the fatigue strength for ground groups, it did not affected the as-sintered groups | Before aging: Control Autoclaved samples: 56.75%, Ground + Autoclaved: 30.63% | |
| - Ardent | Aging protocol: Grinding with coarse diamond burs (#3101 G – grit size 181 μm) in a slow-speed motor under constant water-cooling (≈30 mL/min). Dry storage in sealed vessel for 2 years (mean temperature of 27 °C and mean humidity of 80% + autoclave LTD / 134 °C / 2 bar / 20 h | After: Control Autoclaved: 75.27%. Ground + Autoclaved: 40.14% | |||
Table 4.
Studies investigating mechanical properties of monolithic zirconia specimens/crowns after cycling loading, mechanical loading and various combinations of thermomechanical loading. Studies are presented in chronological order.
| Authors | Zirconia system | Test type /Aging test | Flexural strength change | m-ZrO2 content |
|---|---|---|---|---|
| Specimens | ||||
| Salihoglu-Yener et al. (2015) [129] | -ZirkonZahn | Flexural strength (piston-on-three balls), crosshead-speed 1 mm min−1 | Significant decrease only of unglazed zirconia. ZirkonZahn presented the highest strength with or without thermal cycling. | N/A |
| - Cercon | Thermal cycling (0-control, 1000, 3000, 5000 cycles, 5-55 °C, water). | |||
| – Ceramill | ||||
| Stawarczyk et al. (2016) [119] | - Zenostar | Flexural strength (4-Point Bending), crosshead-speed 1 mm min−1 | No significant change. All monolithic showed lower flexural strength values compared to the conventional zirconia. | N/A |
| - DD Bio ZX2 | Chewing simulator (100 N for 1.2 million times at 1.64 Hz) | |||
| - Ceramill Zolid | ||||
| - InCoris TZI | ||||
| - Ceramill ZI | ||||
| Munoz et al. (2017) [99] | - Prettau Anterior | Flexural strength (piston-on-three balls), crosshead-speed 1 mm min−1 | Significant reduction after M and H + M for Pretau Anterior. Significant reduction after M for the rest. Anterior zirconia had the lowest flexural strength | |
| - Prettau | - mechanical cyclic load (M) | |||
| - ICE Zirkon | - mechanical cyclic + hydrothermal (H + M) | |||
| -non-treated specimens (C). | ||||
| Crowns | ||||
| Johansson et al. (2014) [78] | - Z-CAD HTL | Flexural strength after thermocycling (5000 cycles, 5–55°, water), molar crowns, crosshead-speed 0,025 mm min−1. | The fracture strength of high translucent Y-TZP crowns is considerably higher than that of porcelain-veneered Y-TZP crown cores, porcelain-veneered high translucent Y-TZP crown cores and monolithic lithium disilicate crowns. | N/A |
| - NexxZr HT | ||||
| - Z-CAD HTL-veneered | ||||
| - NexxZr HT- veneered | ||||
| - NexxZr_ HS-veneered | ||||
| Lameira et al. (2015) [77] | - Lava Plus for monolithic crowns | Fracture strength, crowns (on bovine incisors) after thermocycling (2,500, 000 cycles, 80 N, 37 °C, artificial saliva) and loading in chewing simulator, crosshead-speed 0.5 mm min−1. | Monolithic crowns (polished and glazed) presented higher fracture strength than bilayer veneered crowns. No difference between polished and glazed monolithic crowns. | N/A |
| - Lava Frame for bi-layer crowns | ||||
| Nordahl et al. (2015) [131] | - Lava | Fracture toughness, 10° angulated molar crowns of varying thicknesses: 0.3, 0.5, 0.7, 1.0, and 1.5 mm, crosshead-speed 0,025 mm min−1 | Absence of non-aged specimens. There was no difference in strength between crowns of high- or low-translucency. The load at fracture decreased from thicker to thinner | N/A |
| - Lava Plus | Thermocycling of crowns (5000 cycles, 6-55 °C, water) | |||
| Bergamo et al. (2016) [128] | - Ceramill Zolid | Fracture test, molar crowns,crosshead-speed 1 mm min−1 | No significant change | Control: 4% |
| - Thermal fatigue (T): 104 cycles, 5–55 °C | Thermal fatigue:up to 4.5% | |||
| - Mechanical fatigue (M): 106 cycles, 70 N, 1.4-Hz, water, 37 °C | Mechanical fatigue: up to 8,9% | |||
| - Combination of M + T fatigue | Combination of mechanical and thermal fatigue: up to 8.3% | |||
| Mitov et al. (2016) [130] | Zeno Zr | Fracture toughness,molar crowns with various preparation designs (shoulderless, 0.4 mm and 0.8 mm chamfer), crosshead speed 0.5 mm min−1 | Autoclave + chewing simulation caused a significant decrease of the fracture load for all groups, but thermocycling did not. Circumferential shoulderless preparation had a significantly higher fracture | N/A |
| Steam autoclave 134 °C, 2 bar, 3 h + chewing simulation | ||||
| Thermocycling 5–55 °C, 5000 cycles, + chewing simulation | ||||
| Bankoglu et al. (2017) [132] | Incoris TZI | Fracture toughness, molar crowns, crosshead-speed 0.5 mm min−1. | Absence of non-aged specimens. The highest resistance was observed for zirconia crowns. All specimens survived the mastication simulation. | N/A |
| Thermal and mechanical cycling 5000 cycles, 5°-55 °C, water | ||||
| Mechanical loading 100 N, 12 × 105 cycles. | ||||
| Sarıkaya et al. (2018) [87] | - Bruxzir | Fracture strength, crosshead speed 1 mm min−1 (crowns: force applied on buccal and lingual cusps, FPDs: force applied on occlusal connector area). | - No fractures during chewing simulation | N/A |
| - Incoris TZI | Aging: thermocycling (10,000 cycles /5–55 °C / dwell time = 60 s / transfer time = 10 s, | - Bruxzir crowns and FPDs presented significantly higher fracture strength compared to Incoris TZI | ||
| Dual axis chewing simulator with a total of 1,200,000 cycles. | - No significant difference in fracture strength of crowns and FPDs fabricated from Bruxzir | |||
| Weigl et al. (2018) [85] | Zirkon BioStar HT | Fracture strength, crosshead speed 1 mm min−1 | - All 0.5 mm crowns exceeded 900 N. | N/A |
| Aging: chewing simulation (1,200,000 cycles, 50 N, f = 1.6 Hz)) | − 0.2 mm adhesively cemented control crowns exceeded 900 N. | |||
| Thermal cycling (2 × 3000 between 5 °C and 55 °C, 2 minutes for each cycle) | ||||
| Elshiyab et al. (2018) [90] | -Zenostar Zr | Fracture strength, crosshead speed 1 mm min−1 | - Monolithic lithium disilicate crowns presented lower fracture strength compared to monolithic zirconia | N/A |
| - IPS e.max- CAD | Aging: fatigue by chewing simulation with 1.2 million cycles + thermal cycling at 5–55 °C in distilled water (5118 thermal cycles with 60 s dwell time for each cycle, 15 s pause time). | - All crowns presented a reduction in fracture strength following fatigue aging. | ||
| Yin et al. [89](2019) | A3 12 T, Liaoning Upcera, Benxi, China | Fracture strength, crosshead speed 1 mm min−1 | After polishing the crown presented higher fracture strengths than after adjustment of occlusal contact | Not calculated but observed in the diffraction patterns depending on the polishing method |
| Different polishing protocols were evaluated. Cementation using resin cement. | ||||
| Chewing simulation with cyclic loads between 2 and 300 N, frequency 1 Hz (100,000 cycles) | ||||
| Elsayed et al. (2019) [88] | - DD Bio ZX2 (3Y-TZP) | Fracture strength, lower molar crowns with minimum thickness 0.8 mm (buccal) and 1.0 mm (occlusal, lingual, and approximal), crosshead speed 0.5 mm min−1. | Significantly higher fracture strength was noted for 3Y-TZP compared to 5Y-TZP. | N/A |
| - DD cubeX2 HS (4Y-TZP) | chewing simulator for 1,200,000 cycles + simultaneous thermocycling between 5 °C and 55 °C. Vertical load of 49 N applied 2 mm buccal to the central fissure with a lateral movement of 0.3 mm towards the center | (3Y-TZP > 4Y-TZP > 5Y-TZP) | ||
| - DD cubeX2 (5Y-TZP) | ||||
| Fixed partial dentures | ||||
| Preis et al. (2012) [133] | - Cercon ht | Fracture strength, 3-unit FDPs after thermal cycling, crosshead-speed 1 mm min−1 | Similar strength of monolithic compared to veneered zirconia | |
| Alshahrani et al. (2017) [134] | - ICE Zirkon Translucent | Fracture strength, cantilevered frameworks after thermal cycling, crosshead-speed 1 mm min−1 | Increased occlusocervical thickness and decreased cantilever length allowed the cantilever to withstand higher loads. | N/A |
| Villefort et al. (2017) [135] | In-Ceram YZ | Fatigue limit after cycling loading (100,000cycles, 5 Hz frequency), 3-unit posterior FDPs | The glass/silica infiltration techniques in the monolithic zirconia bridges significantly increased the fatigue limits compared with the glazed control group | N/A |
| Control group (CTL) | ||||
| Silica sol-gel group (SSG) | ||||
| Glass-zirconia-glass group (GZG) | ||||
| Lopez-Suarez et al. (2017) [136] | Veneered FDPS: | Fracture strength, 3-unit FPDs after loading in chewing simulator, crosshead-speed 1 mm min−1. | Comparable fracture resistance of monolithic and veneered zirconia FDPs. | N/A |
| - Lava | ||||
| Monolithic FDPs: | ||||
| - Lava Plus | ||||
Table 5.
Commercial products listed in the studies included in the review, manufacturers and compositions.
| Brand | Manufacturer | Composition (wt%) | Source |
|---|---|---|---|
| Aadva Standard Translucency [ST] | GC Tech, Leuven, Belgium | 3 mol% Y-TZP: 94.8% ZrO2, 3%Y2O3, 0.2%Al2O3 | Reference [103] |
| Aadva Enamel Intensive [EI] | GC Tech, Leuven, Belgium | 3 mol% Y-TZP: 95%ZrO2, 5%Y2O3, trace of Al2O3 | Reference [103] |
| Aadva Natural Translucency [NT] | GC Tech, Leuven, Belgium | 5.5 mol% Y-TZP: 91%ZrO2, 9%Y2O3, trace of Al2O3 | Reference [103] |
| Argen HT | Argen Corp, USA | ˜5 mol% Y-TZP: ZrO2 >99%, Y2O3 6.1 – 8.2%, HfO2 <5%, Al2O3 <0.2% | https://www.argen.com/store/products/9164 |
| BruXZir HT | Glidewell laboratories, USA | 3 mol% Y-TZP (No other details can be found) | Reference [64] |
| BruxZir Prismatik | Glidewell laboratories, USA | 3 mol% Y-TZP (No other details can be found) | Reference [73] |
| BruXZir Shaded 16 | Glidewell laboratories, USA | 3 mol% Y-TZP (No other details can be found) | Reference [64] |
| Ceramill | Amann Girrbach AG, Austria | 3 mol% Y-TZP: ZrO2 w% main component, Y2O3 4-6 w%, Al2O3 0-1 w%, HfO2 1-5 w% | Reference [129] |
| Ceramill ZI | Amann Girrbach AG, Austria | 3 mol% Y-TZP: ZrO2 + HfO2 + Y2O3: > 99,0%, Y2O3: 4,5 – 5,6%, HfO2: ≤ 5%, Al2O3: ≤ 0,5%, Other oxides: ≤ 1% | https://www.amanngirrbach.com/en/products/cadcam-material/ceramic/zolid-zirconia/zi/ |
| Ceramill Zolid | Amann Girrbach AG, Austria | 3 mol% Y-TZP: ZrO2 + HfO2 + Y2O3 > 99%, Y2O3: 4.5–5.6%, HfO2 < 5%,Al2O3 < 0.5% | Reference [114] |
| Ceramill Zolid FX –Multilayer | Amann Girrbach AG, Austria | ˜5 mol% Y-TZP: ZrO2 + HfO2 + Y2O3≥99%, Y2O3 8.5-9.5%, HfO2<5%, Al2O3<0.5%, other oxides<1% | Reference [98] |
| Cercon | DeguDent GmbH, Germany | 3 mol% Y-TZP: ZrO2 (+HfO2) % main component, Y2O3 5 w%, Al2O3 + SiO2 1 %, HfO2 2 % | Reference [129] |
| Cercon ht | DeguDent GmbH, Germany | 3 mol% Y-TZP: ZrO2, Y2O3 5 %, HfO2< 3 %, Al2O3, SiO2 < 1 % | http://www.degudent.com/Communication_and_Service/Download/Cercon/Download_Cercon.php |
| DD Bio ZX2 | Dental Direkt GmbH, Germany | 3 mol% Y-TZP: ZrO2 + HfO2 + Y2O3 > 99; Al2O3 < 0.5; other oxides ≤ 1 | Reference [114] |
| Denzir Y-TZP | Denzir AB, Sweden | 3 mol% Y-TZP: ZrO2 + Y2O3 + HfO2 + Al2O3>99,95 wt% | Reference [73] |
| Denzir Mg-PSZ | Denzir AB, Sweden | ZrO2 + MgO˜99,95 wt% | Reference [73] |
| Diazir | Ivoclar Vivadent, Lichtenstein | 3 mol% Y-TZP (No other details can be found) | Reference [137] |
| D max Natura Z-B2018 | DMAX Co., Daegu, Korea | 3 mol% Y-TZP (No other details could be found) | http://www.dmax.biz/eng/zirconia-block/block_properties.html |
| DDcubex2 | Dental Direct Materials, Germany | ZrO2%+HfO2 > 90%,Y2O3 < 10%Al2O3 < 0.1%,other oxide<0.005% | Reference [138] |
| GC Initial Zr | GC Corp., Japan | 3 mol% Y-TZP (No other details can be found) | Reference [127] |
| ICE Zirkon | Zirkonzahn, Italy | 3 mol% Y-TZP: ZrO2, Y2O3 4–6%, Al2O3 < 1% SiO2 < 0.02%, Fe2O3 < 0.01% Na2O < 0.04% | Reference [139,140] |
| ICE Zirkon Translucent | Zirkonzahn, Italy | 3 mol% Y-TZP: 4%-6% Y2O3, <1% Al2O3, < 0.02% SiO2,< 0.01% Fe2O3, < 0.04% Na2O | Reference [139] |
| In-Ceram Zirconia YZ | Vita Zahnfabrik, Bad Sackingen, Germany | 3 mol% Y-TZP: ZrO2 90.9 – 94.5%, Y2O3 4 – 6%, HfO2 1.5 – 2.5%, Al2O3 0 – 0.3% Er2O3 0%, Fe2O3 0 – 0.3% | Reference [141] |
| In-Ceram zirconia YZ HT | Vita Zahnfabrik, Bad Sackingen, Germany | 3 mol% Y-TZP: ZrO2 90.4 – 94.5%, Y2O3 4 – 6%, HfO2 11.5 – 2.5%, Al2O3 0 – 0.3%, Er2O3 0 0 – 0.5%, Fe2O3 0 – 0.3% | Reference 2016 [141] |
| Incoris TZI | Dentsply Sirona, USA | 3 mol% Y-TZP: ZrO2+HfO2+Y2O3 ≥ 99.0%, Y2O3 > 4.5 - ≤ 6.0%, HfO2 ≤ 5%, Al2O3 ≤ 0.04%, Other oxides ≤ 1.1% | Reference [104] |
| inCoris TZI C | Dentsply Sirona, USA | 3 mol% Y-TZP: ZrO2+HfO2+Y2O3≥ 99.0%, Y2O3> 4.5 - ≤ 6.0%, HfO2≤ 5%, Al2O3≤0.04%, Other oxides≤ 1.1% | http://manuals.sirona.com/en/digital-dentistry/cad-cam-materials/incoris-tzi-c.html |
| inCoris ZI | Dentsply Sirona, USA | 3 mol% Y-TZP: ZrO2+HfO2+Y2O3 ≥ 99.0%, Y2O3 > 4.5 - ≤ 6.0%, HfO2 ≤ 5%, Al2O3 ≤ 0.5%, Fe2O3 ≤ 0.3% | Reference [104] |
| IPS e.max ZirCAD | Ivoclar Vivadent AG, Schaan, Liechtenstein | 3 mol% Y-TZP: ZrO2 =87.0– 95.0%, Y2O3 =4.0 – 6.0, HfO2 =1.0 – 5.0%, Al2O3 =0.0 – 1.0% | Reference [104] |
| Katana HT13 | KURARAY CO, LTD, Japan | ˜5.5 mol% Y-TZP: Al2O3 = 0.13 (0.10), Y2O3 = 10.91 (0.73), ZrO2 = 86.50 (0.85), HfO2 = 2.46 (0.26) | Calculated by the authors in Reference [121] |
| Katana ML | KURARAY CO, LTD, Japan | ˜5.5 mol% Y-TZP: Al2O3 = 0.16 (0.10), Y2O3 = 10.95 (0.29), ZrO2 = 86.21 (0.59), HfO2 = 2.41 (0.27) | Calculated by the authors in Reference [121] |
| Katana ST | KURARAY CO, LTD, Japan | 88–93% ZrO2, 7–10% Y2O3, Other<2% | Reference [142] |
| Katana UT | KURARAY CO, LTD, Japan | 5.4 mol% Y-TZP: Al2O3 = 0.1 (0.1), Y2O3 = 10.1(0.7), ZrO2 = 87.8 (0.7), HfO2 = 2 (0.1) | Reference [143] Calculated by the authors in Reference [144] |
| Katana UTML | KURARAY CO, LTD, Japan | 87–92% ZrO2 + HfO2, 8–11% Y2O3, other oxides 0-2% | https://www.bego.com/fileadmin/user_downloads/Mediathek/Medical/en_Keramik/KATANA_Zirconia/me_800369_0000_pp_en.pdf |
| Everest ZS | KaVo Dental GmbH, Germany | 3 mol% Y-TZP (No other details can be found) | Reference [145] |
| KZ-3YF type AC | KCM, Nagoya, Japan | 3% mol% Y-TZP: ZrO2 as main component, Y2O3 5.4%, Al2O3 0.25% | http://www.kyoritsu-kcm.co.jp/english/new_material/new_material_01.html |
| Lava, Lava Frame | 3M ESPE, USA | 3 mol% Y-TZP (No other details could be found) | http://www.lava-elite.com/lava-classic-crowns-bridges.shtml |
| Lava Plus al | 3M ESPE, USA | 3 mol% Y-TZP (No other details could be found) | http://www.lava-elite.com/lava-classic-crowns-bridges.shtml |
| Lava TM Esthetic | 3M ESPE, USA | 5 mol% Y-TZP (No other details could be found) | https://www.3m.com/3M/en_US/company-us/all-3m-products/˜/3M-Lava-Esthetic-Fluorescent-Full-Contour-Zirconia-Disc/?N=5002385+3291669973rt=rud |
| Nissin Dental Zirconia Blank | Nissin-Metec China Co., Ltd., China | 3% mol% Y-TZP: ZrO2 ≥99.0% Inorganic Pigment (Fe2O3, Er2O3)≤ 1 | https://www.accessdata.fda.gov/cdrh_docs/pdf16/K160367.pdf |
| NexxZr_ HS | Sagemax Bioceramics, Inc., Federal Way, WA | 3% mol% Y-TZP: ZrO2+HfO2+Y2O3 = 99.1%, Al2O3 <0.3% | http://sagemax.com/portfolio-item/nexxzr-s/ |
| NexxZr HT | Sagemax Bioceramics, Inc., Federal Way, WA | 3 mol% Y-TZP: ZrO2+HfO2+Y2O3 = 99.1%, Al2O3 <0.1% | http://sagemax.com/portfolio-item/nexxzr-t/ |
| Nobel Procera | Nobel Biocare Services AG, Switzerland | 3 mol% Y-TZP: ZrO2 + Y2O3 + HfO2 ≥ 99.0%, Y2O3 > 4.5 to ≤6.0, HfO2 ≤ 5%, Al2O3 ≤ 0.5%. Other oxides ≤0.5% | Reference [73] |
| Prettau | Zirkonzahn, Italy | 3 mol% Y-TZP: ZrO2= main component, Y2O3 = 4 – 6 %, Al2O3< 1 %, SiO2< 0.02 %, Fe2O3< 0.01 %, Na2O< 0.04 % | Reference [100] |
| Prettau, Anterior | Zirkonzahn, Italy | ˜8 mol% Y-TZP: ZrO2= Main component, Y2O3< 12 %, Al2O3< 1 %, SiO2<0.02 %, Fe2O3 < 0.02 % | Reference [100] |
| Tizian Blank Translucent | Schutz Dental GmbH, Germany | 3 mol% Y-TZP: ZrO2< 96%, yttrium oxide > 4%, HfO2> 1%, Al2O3 < 1%, SiO2< 0.02% | Reference [146] |
| TZ-3Y-E | Tosoh Corporation, Tokyo, Japan | 3 mol% Y-TZP: 5.2% Y2O3, 0.25% Al2O3, 5.2 ± 0.5 Y2O3, < 5.0HfO2, 0.1 ˜ 0.4%, Al2O3, ≤ 0.02% SiO2, ≤ 0.01% Fe2O3, ≤0.04% Na2O | Reference [102] https://www.tosoh.com/our-products/advanced-materials/zirconia-powders |
| TZ-3YS-E | Tosoh Corporation, Tokyo, Japan | 3 mol% Y-TZP: 5.2% Y2O3, 0.25% Al2O3, 5.2 ± 0.5 Y2O3, < 5.0 HfO2, 0.1 ˜ 0.4% Al2O3, ≤ 0.02% SiO2, ≤ 0.01% Fe2O3, ≤0.06% Na2O | https://www.tosoh.com/our-products/advanced-materials/zirconia-powders |
| VITA YZ-HT | Vita Zahnfabrik, Bad Säckingen, Germany | 3 mol% Y-TZP: ZrO2 90.4-94.5, + HfO2 + Y2O3 4 -6, HfO2 1.5-2.5, Al2O3 0-0.3, Er2O5 0-0.5, Fe2O3 0-0.3 | VITA_10160_10160E_YZ_TWD_EN_V02_screen_en.pdf (www.vita-zahnfabrik.com/en/) |
| VITA YZ-T | Vita Zahnfabrik, Bad Säckingen, Germany | 3 mol% Y-TZP: ZrO2 90.4-94.5, + HfO2 + Y2O3 4 -6, HfO2 1.5-2.5, Al2O3 0-0.3, Fe2O3 0-0.3 | VITA_10160_10160E_YZ_TWD_EN_V02_screen_en.pdf (www.vita-zahnfabrik.com/en/) |
| Zenostar Zr | Wieland Dental + Technik GmbH & Co. KG, Germany | 3 mol% Y-TZP: ZrO2 + HfO2 + Y2O3 > 99; 4,5 < Y2O3 ≤6; HfO2 ≤ 5; Al2O3 + other oxides ≤1 | Reference [114] |
| Zeno Zr | Wieland Dental + Technik GmbH & Co. KG, Germany | 3 mol% Y-TZP: (ZrO2+ HfO2) 94%, (Y2O3) 5%, (Al2O3) <1%, other oxides <1%) | Reference [130] |
| ZirkonZahn | Steger, Ahrntal, Italy | 3 mol% Y-TZP: ZrO2 (+HfO2) w% main component, Y2O3 4.95˜5.26 w%, Al2O3 0.15˜0.35 w%, SiO2 0.02 w%, Fe2O3 0.01 w%, Na2O 0.04 w% | Reference [129] |
| ZirLuna | ACF, Amberg, Germany | 3 mol% Y-TZP (No other details can be found) | Reference [67] |
| Zirlux | Ardent Inc., Pentron Ceramics, USA | 3 mol% Y-TZP: ZrO2+HfO2>94%, Y2O3 <6 %, HfO2< 3 %, Al2O3< 0.5 % | https://www.custom-milling.com/images/pdfs/materials/Zirlux_Full_Contour_Zirconia_Discs_MSDS.pdf |
| Zirlux FC | Ardent Inc., Pentron Ceramics, USA | 3 mol% Y-TZP: ZrO2+HfO2:>94%, Y2O3: 5.35% ± 0.20, AL2O3: <0.1%, HfO2: Typically <3.0% | https://www.zirlux.com/fc2/ |
| ZirPremium | ACUCERA, Korea | 3 mol% Y-TZP (No other details could be found) | http://www.buykorea.org/product-details/zirpremium-dental-cad-cam-blocks--3039039.html |
| Zmatch | Dentaim, Seoul, Korea | 3 mol% Y-TZP : 94– 95% ZrO2 and HfO2, 5 ± 0.2% Y2O3 and 0.25% Al2O3 | Reference [147] |
| Zpex | Tosoh Corporation, Tokyo, Japan | 3 mol% Y-TZP: 5.2% Y2O3, 0.05% Al2O3 | Reference [102] |
| Zpex Smile | Tosoh Corporation, Tokyo, Japan | ˜5 mol% Y-TZP: 9.35% Y2O3, 0.05% Al2O3 | Reference [102] |
| Z-CAD_ HTL | Metoxit AG, Thayngen, Switzerland | 3 mol% Y-TZP: ZrO2+HfO2+Y2O3> 99.5%, Y2O3 = 5.2%, Al2O3 = 0.05%, other oxides≤0.5% | http://www.metoxit.com/ |
Guilardi et al. [123] examined the effects of grinding and low temperature aging on flexural strength, roughness, and phase transformation of Y-TZP ceramics. Grinding increased significantly the characteristic strength and affected positively the material’s sensitivity to the tetragonal to monoclinic phase transformation during aging, a transformation which was less for the fine ground specimens. Exactly the same results came from the study of Pereira et al. [124]. On the other side, Khayat et al. [91] reported that grinding alone can significantly increase roughness and make the material more prone to aging, however they did not investigate the effect of aging on the strength of rough grinded specimens. Polishing after grinding, however, significantly reduced roughness. Although boiling in artificial saliva for 7 days increased monoclinic fraction from 2.4% to 21%, the increase was superficial and there was no reduction in strength, but in some ceramics, an increase was recorded instead [118]. The flexural strength was not affected by the amount of monoclinic fraction on the surface. Dehestani and Adolfsson [125] found no significant change in strength after immersion in boiling water up to 6 months, although a significant amount of monoclinic fraction was recorded after 32 days (50% for 3 Y-TZP monolithic ceramics). On the recent study of Pereira et al. [82], three different translucencies of monolithic zirconia ceramics were evaluated following autoclave aging at 134 °C under pressure of 2 bars pressure for 20 h and it was reported that the high translucency system presented a significant increase in flexural strength as well as increased monoclinic phase percentage, compared to the super- and ultra-translucency systems. Another recent study’s findings, in which monolithic zirconia specimens were submitted to fatigue strength test, have shown that ground specimens presented higher fatigue strength, whereas ground specimens which were submitted to autoclave aging presented lower percentages of monoclinic phase [94]. This is in agreement with previous findings from Prado et al. [92].
Concerning the effect of steam autoclave aging on molar crowns’ strength, significant reduction of strength up to 50 h of autoclave treatment has been reported [126] and no further reduction afterwards, while Leone et al. [127] reported significant reduction after 54 h of autoclave treatment only for the 3 mol% Y-TZP, and no change for the ultra high translucent zirconia, which however presented the lowest mechanical properties. On the other hand, in other studies [120,128], no significant difference among various brands of 3–5 mol% Y-TZP monolithic zirconia crowns was found, even after 50 h of aging [120,126]. Although limited evidence exists concerning ultra high translucent ceramics, they seem to present a high resistance to degradation, but lower mechanical strength [127].
Chewing simulator did not induce any significant alterations in the strength values of 3 mol% Y-TZ specimens, but all monolithic zirconia materials presented lower values compared to the conventional one [119]. In a recent study by Elsayed et al. [88], which evaluated the fracture strength of 3Y-TZP, 4Y-TZP and 5Y-TZP molar crowns following chewing simulation with simultaneous thermocycling, supports that crowns from zirconia with high Y2O3 content presented higher fracture strength. On the contrary, significantly higher decrease in strength after mechanical cyclic loading was recorded for 8 mol% monolithic zirconia specimens, especially after the combination of thermal and mechanical cycling [99]. In another study, unglazed monolithic crowns presented the lowest strength after thermal cycling in water [129]. In the opposite direction, other studies report that thermal cycling alone does not decrease significantly the fracture load of monolithic zirconia crowns as does the combination of mechanical and thermal aging, which according to Bergamo et al. [28], also increases the amount of monoclinic phase more than eightfold on the mesial palatal cusp of the crowns (8.3–8.9%). It was further reported that circumferential shoulderless preparation had a significantly higher fracture load than other groups [130]. No difference in strength between crowns made of high-translucent (HTZ) or low-translucent (LTZ) zirconia has been reported [131] while yttria stabilized zirconia presented higher resistance to fracture compared to lithium disilicate crowns [90,132]. According to Sarıkaya et al. [87], Bruxzir monolithic zirconia crowns and FPDs present higher fracture strength compared to Incoris TZI following simultaneous chewing simulation (1,200,000 cycles) and thermocycling (10,000 cycles). With regards to material thickness, according to Weigl et al. [85], monolithic zirconia crowns as thin as 0.2 mm present acceptable fracture strength test when they are cemented with adhesive luting agents. The fracture strength of 3 mol% Y-TZP monolithic 3-unit FDPs has been found similar to that of veneered bilayer FDPs [97,99], while glass infiltration of a sol-gel glass has been found to increase the fatigue limits of the restorations [100]. As expected, increased occluso-cervical thickness and decreased length of cantilevered frameworks were advantageous for higher loads. Sarıkaya et al. [87] reported that monolithic zirconia 3-unit FDPs fabricated with two different ceramic systems demonstrate acceptable fracture strength even after 5 years equivalent of chewing simulation.
4. Conclusions
Latest developments in CAD-CAM technology have rendered monolithic zirconia restorations a well-established restorative treatment in prosthodontic cases with advanced mechanical and esthetic needs. Various production synthesis and sintering parameters have been utilized, leading to promising results, however, further research is still needed for solid conclusions. Concerning tooth color reproduction, there are a lot of issues to be resolved, as multiple factors can affect the final color of a monolithic zirconia restoration. In regards to strength, ultra translucent fully stabilized monolithic zirconia ceramics present significantly lower strength compared to tetragonal partially stabilized ones, and thus should probably be applied only in areas with minimal biting forces, such as the anterior regions of the mouth or in patients without parufunctional habits and bruxism. The absence of aging sensitivity, however, may overwhelm their low strength, but only well designed clinical studies can verify or reject this hypothesis. However, it would be safe to suggest the utilization of the high-strength partially stabilized zirconia for posterior or long span restorations and fully stabilized ultra-translucent zirconia for anterior short span fixed partial dentures.
To summarize, despite the obvious advantages of contemporary monolithic zirconia ceramics, new scientific data emerges constantly about their properties, the limitations in their application and their resistance to low-temperature degradation that will eventually reach to laboratory and clinical guidelines for their use. However, monolithic zirconia ceramics include a group of materials with different properties and sound scientific knowledge should guide the selection of the appropriate material in each clinical situation.
Conflicts of interest
None.
References
- 1.Denry I., Kelly J.R. State of the art of zirconia for dental applications. Dent Mater. 2008;24:299–307. doi: 10.1016/j.dental.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 2.Denry I., Kelly J.R. Emerging ceramic-based materials for dentistry. J Dent Res. 2014;93:1235–1242. doi: 10.1177/0022034514553627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piconi C., Maccauro G. Zirconia as a ceramic biomaterial. Biomaterials. 1999;20:1–25. doi: 10.1016/s0142-9612(98)00010-6. [DOI] [PubMed] [Google Scholar]
- 4.Garvie R.C., Hannink R.H., Pascoe R.T. Ceramic steel? Nature. 1975;258:703–704. [Google Scholar]
- 5.Vagkopoulou T., Koutayas S.O., Koidis P., Strub J.R. Zirconia in dentistry: part 1. Discovering the nature of an upcoming bioceramic. Eur J Esthet Dent. 2009;4:130–151. [PubMed] [Google Scholar]
- 6.Koutayas S.O., Vagkopoulou T., Pelekanos S., Koidis P., Strub J.R. Zirconia in dentistry: part 2. Evidence-based clinical breakthrough. Eur J Esthet Dent. 2009;4:348–380. [PubMed] [Google Scholar]
- 7.Gupta T.K., Lange F.F., Bechtold J.H. Effect of stress-induced phase transformation on the properties of polycrystalline zirconia containing metastable tetragonal phase. J Mater Sci. 1978;13:1464–1470. [Google Scholar]
- 8.Chevalier J., Gremillard L., Deville S. Low-temperature degradation of zirconia and implications for biomedical implants. Annu Rev Mater Res. 2007;37:1–32. [Google Scholar]
- 9.Chevalier J., Cales B., Drouin J.M. Low-temperature aging of Y-TZP ceramics. J Am Ceram Soc. 2004;82:2150–2154. [Google Scholar]
- 10.Lawson S. Environmental degradation of zirconia ceramics. J Eur Ceram Soc. 1995;15:485–502. [Google Scholar]
- 11.Deville S., Chevalier J., Gremillard L. Influence of surface finish and residual stresses on the ageing sensitivity of biomedical grade zirconia. Biomaterials. 2006;27:2186–2192. doi: 10.1016/j.biomaterials.2005.11.021. [DOI] [PubMed] [Google Scholar]
- 12.Chevalier J., Gremillard L., Virkar A.V., Clarke D.R. The tetragonal-monoclinic transformation in zirconia: lessons learned and future trends. J Am Ceram Soc. 2009;92:1901–1920. [Google Scholar]
- 13.Hsu Y.W., Yang K.H., Chang K.M., Yeh S.W., Wang M.C. Synthesis and crystallization behavior of 3 mol% yttria stabilized tetragonal zirconia polycrystals (3Y-TZP) nanosized powders prepared using a simple co-precipitation process. J Alloys Compd. 2011;509:6864–6870. [Google Scholar]
- 14.Maridurai T., Balaji D., Sagadevan S. Synthesis and characterization of yttrium stabilized zirconia nanoparticles. Mater Res. 2016;19:812–816. [Google Scholar]
- 15.Geethalakshmi K., Prabhakaran T., Hemalatha J. Dielectric studies on nano zirconium dioxide synthesized through co-precipitation process. World Acad Sci Eng Technol. 2012;64:179–182. [Google Scholar]
- 16.Gonzalo-Juan I., Ferrari B., Colomer M.T. Influence of the urea content on the YSZ hydrothermal synthesis under dilute conditions and its role as dispersant agent in the post-reaction medium. J Eur Ceram Soc. 2009;29:3185–3195. [Google Scholar]
- 17.Lach R., Bu M.M., Haberko K., Marian R. Translucent zirconia polycrystals prepared from nanometric powders. Procesing Apl Dent Ceram. 2015:175–180. [Google Scholar]
- 18.Sato K., Horiguchi K., Nishikawa T., Yagishita S., Kuruma K., Murakami T. Hydrothermal synthesis of yttria-stabilized zirconia nanocrystals with controlled yttria content. Inorg Chem. 2015;54:7976–7984. doi: 10.1021/acs.inorgchem.5b01112. [DOI] [PubMed] [Google Scholar]
- 19.Feng G., Jiang W., Liu J., Zhang Q., Wu Q., Miao L. A novel green nonaqueous sol-gel process for preparation of partially stabilized zirconia nanopowder. Process Appl Ceram. 2017;11:220–224. [Google Scholar]
- 20.Varma A., Mukasyan, Rogachev A., Manukyan K. Solution combustion synthesis of nanoscale materials. Chem Rev. 2016;116:14493–14586. doi: 10.1021/acs.chemrev.6b00279. [DOI] [PubMed] [Google Scholar]
- 21.Silva D., A. C, Ribeiro N.F.P., Souza M.M.V.M. Effect of the fuel type on the synthesis of yttria stabilized zirconia by combustion method. Ceram Int. 2009;35:3441–3446. [Google Scholar]
- 22.Limaye A., Helble J. Morphological control of zirconia nanoparticles through combustion aerosol synthesis. J Am Ceram Soc. 2002;32:1127–1132. [Google Scholar]
- 23.Han A., Wu Z., Zou H. One-step alkali chloride-assisted solution combustion synthesis of 3YSZ nanopowders with ultrahigh specific surface area. Ceram Int. 2017;43:16043–16047. [Google Scholar]
- 24.Dodd A.C., Tsuzuki T., McCormick P.G. Nanocrystalline zirconia powders synthesised by mechanochemical processing. Mater Sci Eng A. 2001;301:54–58. [Google Scholar]
- 25.Macan J., Brcković L., Gajović A. Influence of preparation method and alumina content on crystallization and morphology of porous yttria stabilized zirconia. J Eur Ceram Soc. 2017;37:3137–3149. [Google Scholar]
- 26.Amat N.F., Muchtar A., Amril M.S., Ghazali M.J., Yahaya N. Preparation of presintered zirconia blocks for dental restorations through colloidal dispersion and cold isostatic pressing. Ceram Int. 2018;44:6409–6416. [Google Scholar]
- 27.Akimov G.Y. Cold isostatic pressing as a method for fabricating ceramic products with high physicomechanical properties. Refract Ind Ceram. 1998;39:283–287. [Google Scholar]
- 28.Edwards Rezende C.E., Sanches Borges A.F., Macedo R.M., Rubo J.H., Griggs J.A. Dimensional changes from the sintering process and fit of Y-TZP copings: micro-CT analysis. Dent Mater. 2017;33:e405–e413. doi: 10.1016/j.dental.2017.08.191. [DOI] [PubMed] [Google Scholar]
- 29.Druschitz A.P., Schroth J.G. Hot isostatic pressing of a presintered yttria-stabilized zirconia ceramic. J Am Ceram Soc. 1989;72:1591–1597. [Google Scholar]
- 30.Scherrer S.S., Cattani-Lorente M., Yoon S., Karvonen L., Pokrant S., Rothbrust F. Post-hot isostatic pressing: a healing treatment for process related defects and laboratory grinding damage of dental zirconia? Dent Mater. 2013;29:e180–190. doi: 10.1016/j.dental.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 31.Denkena B., Breidenstein B., Busemann S., Lehr C.M. Impact of hard machining on zirconia based ceramics for dental applications. Procedia Cirp. 2017;65:248–252. [Google Scholar]
- 32.Borrell A., Salvador M.D., Peñaranda-Foix F.L., Cátala-Civera J.M. Microwave sintering of Zirconia materials: mechanical and microstructural properties. Int J Appl Ceram Technol. 2013;10:313–320. [Google Scholar]
- 33.Ahsanzadeh-Vadeqani M., Razavi R.S. Spark plasma sintering of zirconia-doped yttria ceramic and evaluation of the microstructure and optical properties. Ceram Int. 2016;42:18931–18936. [Google Scholar]
- 34.Stawarczyk B., Özcan M., Hallmann L., Ender A., Mehl A., Hämmerlet C.H.F. The effect of zirconia sintering temperature on flexural strength, grain size, and contrast ratio. Clin Oral Invest. 2013;17:269–274. doi: 10.1007/s00784-012-0692-6. [DOI] [PubMed] [Google Scholar]
- 35.Kim M.-J., Ahn J.-S., Kim J.-H., Kim H.-Y., Kim W.-C. Effects of the sintering conditions of dental zirconia ceramics on the grain size and translucency. J Adv Prosthodont. 2013;5:161–166. doi: 10.4047/jap.2013.5.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ebeid K., Wille S., Hamdy A., Salah T., El-Etreby A., Kern M. Effect of changes in sintering parameters on monolithic translucent zirconia. Dent Mater. 2014;30 doi: 10.1016/j.dental.2014.09.003. e419–24. [DOI] [PubMed] [Google Scholar]
- 37.Jiang L., Liao Y., Wan Q., Li W. Effects of sintering temperature and particle size on the translucency of zirconium dioxide dental ceramic. J Mater Sci Mater Med. 2011;22:2429–2435. doi: 10.1007/s10856-011-4438-9. [DOI] [PubMed] [Google Scholar]
- 38.Sen N., Sermet I.B., Cinar S. Effect of coloring and sintering on the translucency and biaxial strength of monolithic zirconia. J Prosthet Dent. 2017;19(2) doi: 10.1016/j.prosdent.2017.08.013. 308.e1-308.e7. [DOI] [PubMed] [Google Scholar]
- 39.Lucas T.J., Lawson N.C., Janowski G.M., Burgess J.O. Effect of grain size on the monoclinic transformation, hardness, roughness, and modulus of aged partially stabilized zirconia. Dent Mater. 2015;31:1487–1492. doi: 10.1016/j.dental.2015.09.014. [DOI] [PubMed] [Google Scholar]
- 40.Menezes R.R., Souto P.M., Kiminami R.H.G.A. Microwave sintering of ceramic materials. IOP Conf Ser Mater Sci Eng. 2016;161 [Google Scholar]
- 41.Karayannis V.G. Microwave sintering of ceramic materials. IOP Conf Ser Mater Sci Eng. 2016;161 [Google Scholar]
- 42.Almazdi A.A., Khajah H.M., Monaco E.A., Kim H. Applying microwave technology to sintering dental zirconia. J Prosthet Dent. 2012;108:304–309. doi: 10.1016/S0022-3913(12)60181-4. [DOI] [PubMed] [Google Scholar]
- 43.Marinis A., Aquilino S.A., Lund P.S., Gratton D.G., Stanford C.M., Diaz-Arnold A.M. Fracture toughness of yttria-stabilized zirconia sintered in conventional and microwave ovens. J Prosthet Dent. 2013;109:165–171. doi: 10.1016/S0022-3913(13)60037-2. [DOI] [PubMed] [Google Scholar]
- 44.Upadhyaya D.D., Ghosh A., Dey G.K., Prasad R., Suri A.K. Microwave sintering of zirconia ceramics. J Mater Sci. 2001;36:4707–4710. [Google Scholar]
- 45.Kim H.-K., Kim S.-H. Comparison of the optical properties of pre-colored dental monolithic zirconia ceramics sintered in a conventional furnace versus a microwave oven. J Adv Prosthodont. 2017;9:394–401. doi: 10.4047/jap.2017.9.5.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Anselmi-Tamburini U., Woolman J.N., Munir Z.A. Transparent nanometric cubic and tetragonal zirconia obtained by high-pressure pulsed electric current sintering. Adv Funct Mater. 2007;17:3267–3273. [Google Scholar]
- 47.Vasylkiv O., Borodianska H., Sakka Y., Demirskyi D. Flash spark plasma sintering of ultrafine yttria-stabilized zirconia ceramics. Scr Mater. 2016;121:32–36. [Google Scholar]
- 48.Lei L., Fu Z., Wang H., Lee S.W., Niihara K. Transparent yttria stabilized zirconia from glycine-nitrate process by spark plasma sintering. Ceram Int. 2012;38:23–28. [Google Scholar]
- 49.Salamon D., MacA K., Shen Z. Rapid sintering of crack-free zirconia ceramics by pressure-less spark plasma sintering. Scr Mater. 2012;66:899–902. [Google Scholar]
- 50.Kaplan M., Park J., Young Kim S., Ozturk A. Production and properties of tooth-colored yttria stabilized zirconia ceramics for dental applications. Ceram Int. 2018;44:2413–2418. [Google Scholar]
- 51.Shah K., Holloway J.A., Denry I.L. Effect of coloring with various metal oxides on the microstructure, color, and flexural strength of 3Y-TZP. J Biomed Mater Res - Part B Appl Biomater. 2008;87:329–337. doi: 10.1002/jbm.b.31107. [DOI] [PubMed] [Google Scholar]
- 52.Sedda M., Vichi A., Carrabba M., Capperucci A., Louca C., Ferrari M. Influence of coloring procedure on flexural resistance of zirconia blocks. J Prosthet Dent. 2015;114:98–102. doi: 10.1016/j.prosdent.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 53.Oh G.J., Lee K., Lee D.J., Lim H.P., Yun K.D., Ban J.S. Effect of metal chloride solutions on coloration and biaxial flexural strength of yttria-stabilized zirconia. Met Mater Int. 2012;18:805–812. [Google Scholar]
- 54.Pittayachawan P., McDonald A., Petrie A., Knowles J.C. The biaxial flexural strength and fatigue property of LavaTM Y-TZP dental ceramic. Dent Mater. 2007;23:1018–1029. doi: 10.1016/j.dental.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 55.Hjerppe J., Närhi T., Fröberg K., Vallittu P.K., Lassila L.V.J. Effect of shading the zirconia framework on biaxial strength and surface microhardness. Acta Odontol Scand. 2008;66:262–267. doi: 10.1080/00016350802247123. [DOI] [PubMed] [Google Scholar]
- 56.Ban S., Suzuki T., Yoshihara K., Sasaki K., Kawai T., Kono H. Effect of coloring on mechanical properties of dental zirconia. J Med Biol Eng. 2014;34:24–29. [Google Scholar]
- 57.Wen N., Yi Y., Zhang W., Deng B., Shao L., Dong L. The color of Fe2O3 and Bi2O3 pigmented dental zirconia ceramic. Key Eng Mater. 2010;435:582–585. [Google Scholar]
- 58.Kaya G. Production and characterization of self-colored dental zirconia blocks. Ceram Int. 2013;39:511–517. [Google Scholar]
- 59.Huang H., Zhang F.Q., Sun J., Gao L. Effect of three kinds of rare earth oxides on chromaticity and mechanical properties of zirconia ceramic. Zhonghua Kou Qiang Yi Xue Za Zhi. 2006;41:327–330. [PubMed] [Google Scholar]
- 60.Li J., Liu S.M., Lin Y.H. Synthesis of coloured dental zirconia ceramics and their mechanical behaviors. Key Eng Mater. 2014;602–603:594–597. [Google Scholar]
- 61.Liu S.M., Liu J., Deng X.L., Lin Y.H., Liu F. Color reproduction and shade stability of zirconia ceramics. Key Eng Mater. 2014;602–603:610–614. [Google Scholar]
- 62.Huang H., Zheng Y.L., Zhang F.Q., Sun J., Gao L. [Effect of five kinds of pigments on the chromaticity of dental zirconia ceramic] Shanghai Kou Qiang Yi Xue. 2007;16:413–417. [PubMed] [Google Scholar]
- 63.Rada S., Culea E., Rada M. Novel ZrO2based ceramics stabilized by Fe2O3, SiO2 and Y2O3. Chem Phys Lett. 2018;696:92–99. [Google Scholar]
- 64.Church T.D., Jessup J.P., Guillory V.L., Vandewalle K.S. Translucency and strength of high-translucency monolithic zirconium oxide materials. Gen Dent. 2017;65:48–52. [PubMed] [Google Scholar]
- 65.Casolco S.R., Xu J., Garay J.E. Transparent/translucent polycrystalline nanostructured yttria stabilized zirconia with varying colors. Scr Mater. 2008;58:516–519. [Google Scholar]
- 66.Kao C.T., Tuan W.H., Liu C.Y., Chen S.C. Effect of iron oxide coloring agent on the sintering behavior of dental yttria-stabilized zirconia. Ceram Int. 2017;44:4689–4693. [Google Scholar]
- 67.Beuer F., Stimmelmayr M., Gueth J.F., Edelhoff D., Naumann M. In vitro performance of full-contour zirconia single crowns. Dent Mater. 2012;28:449–456. doi: 10.1016/j.dental.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 68.Zhang Y., Chai H., Lee J.J.W., Lawn B.R. Chipping resistance of graded zirconia ceramics for dental crowns. J Dent Res. 2012;91:311–315. doi: 10.1177/0022034511434356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sun T., Zhou S., Lai R., Liu R., Ma S., Zhou Z. Load-bearing capacity and the recommended thickness of dental monolithic zirconia single crowns. J Mech Behav Biomed Mater. 2014;35:93–101. doi: 10.1016/j.jmbbm.2014.03.014. [DOI] [PubMed] [Google Scholar]
- 70.Nakamura K., Harada A., Inagaki R., Kanno T., Niwano Y., Milleding P. Fracture resistance of monolithic zirconia molar crowns with reduced thickness. Acta Odontol Scand. 2015;73:602–608. doi: 10.3109/00016357.2015.1007479. [DOI] [PubMed] [Google Scholar]
- 71.Zhang Y., Mai Z., Barani A., Bush M., Lawn B. Fracture-resistant monolithic dental crowns. Dent Mater. 2016;32:442–449. doi: 10.1016/j.dental.2015.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sorrentino R., Triulzio C., Tricarico M.G., Bonadeo G., Gherlone E.F., Ferrari M. In vitro analysis of the fracture resistance of CAD-CAM monolithic zirconia molar crowns with different occlusal thickness. J Mech Behav Biomed Mater. 2016;61:328–333. doi: 10.1016/j.jmbbm.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 73.Schriwer C., Skjold A., Gjerdet N.R., Øilo M. Monolithic zirconia dental crowns. Internal fit, margin quality, fracture mode and load at fracture. Dent Mater. 2017;33:1012–1020. doi: 10.1016/j.dental.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 74.Rohr N., Märtin S., Fischer J. Correlations between fracture load of zirconia implant supported single crowns and mechanical properties of restorative material and cement. Dent Mater J. 2018;37:222–228. doi: 10.4012/dmj.2017-111. [DOI] [PubMed] [Google Scholar]
- 75.Tsuyuki Y., Sato T., Nomoto S., Yotsuya M., Koshihara T. Effect of occlusal groove on abutment, crown thickness, and cement-type on fracture load of monolithic zirconia crowns. Dent Mater J. 2018;7:843–850. doi: 10.4012/dmj.2017-350. [DOI] [PubMed] [Google Scholar]
- 76.Moilanen P., Hjerppe J., Lassila L.V.J.N.T. Fracture strength and precision of fit of implant-retained monolithic zirconia crowns. J Oral Implant. 2018;44:330–334. doi: 10.1563/aaid-joi-D-17-00249. [DOI] [PubMed] [Google Scholar]
- 77.Lameira D.P., WABE Silva, Silva F.A.E., De Souza G.M. Fracture strength of aged monolithic and bilayer zirconia-based crowns. Biomed Res Int. 2015;15 doi: 10.1155/2015/418641. Article ID 418641, 7 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Johansson C., Kmet G., Rivera J., Larsson C., Vult Von Steyern P. Fracture strength of monolithic all-ceramic crowns made of high translucent yttrium oxide-stabilized zirconium dioxide compared to porcelain-veneered crowns and lithium disilicate crowns. Acta Odontol Scand. 2014;72:145–153. doi: 10.3109/00016357.2013.822098. [DOI] [PubMed] [Google Scholar]
- 79.Bankoğlu Güngör M., Karakoca Nemli S. Fracture resistance of CAD-CAM monolithic ceramic and veneered zirconia molar crowns after aging in a mastication simulator. J Prosthet Dent. 2018;119:473–480. doi: 10.1016/j.prosdent.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 80.AFNE Reis, Ramos G.F., Campos T.M.B., Prado P.H.C.O., Vasconcelos G., Borges ALS de M.R. The performance of sol-gel silica coated Y-TZP for veneered and monolithic dental restorations. J Mech Behav Biomed Mater. 2019;90:515–522. doi: 10.1016/j.jmbbm.2018.09.023. [DOI] [PubMed] [Google Scholar]
- 81.Nishioka G., Prochnow C., Firmino A., Amaral M., Bottino M.A., Valandro LF RM de M. Fatigue strength of several dental ceramics indicated for CAD-CAM monolithic restorations. Braz Oral Res. 2018;32:e53. doi: 10.1590/1807-3107bor-2018.vol32.0053. [DOI] [PubMed] [Google Scholar]
- 82.Pereira G.K.R., Guilardi L.F., Kiara S., Kleverlaan C.J., Rippe M.P., Valandro L.F. Mechanical reliability, fatigue strength and survival analysis of new polycrystalline translucent zirconia ceramics for monolithic restorations. J Mech Behav Biomed Mater. 2018;85:57–65. doi: 10.1016/j.jmbbm.2018.05.029. [DOI] [PubMed] [Google Scholar]
- 83.Almansour H.M., Alqahtani F. The effect of in vitro aging and fatigue on the flexural strength of monolithic the effect of in vitro aging and fatigue on the flexural strength of monolithic high-translucency zirconia restorations. J Contemp Dent Pr. 2018;19:867–873. [PubMed] [Google Scholar]
- 84.Camposilvan E., Leone R., Gremillard L., Sorrentino R., Zarone F., Ferrari M. Aging resistance, mechanical properties and translucency of different yttria-stabilized zirconia ceramics for monolithic dental crown applications. Dent Mater. 2018;34:879–890. doi: 10.1016/j.dental.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 85.Weigl P., Sander A., Wu Y., Felber R., Lauer H., Rosentritt M. In-vitro performance and fracture strength of thin monolithic zirconia crowns. J Adv Prosthodont. 2018;10:79–84. doi: 10.4047/jap.2018.10.2.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ozer F., Naden A., Turp V., Mante F. Effect of thickness and surface modifications on flexural strength of monolithic zirconia. J Prosthet Dent. 2018;119:987–993. doi: 10.1016/j.prosdent.2017.08.007. [DOI] [PubMed] [Google Scholar]
- 87.Sarıkaya I.H.Y. Effects of dynamic aging on the wear and fracture strength of monolithic zirconia restorations. BMC Oral Health. 2018;18(146):1–7. doi: 10.1186/s12903-018-0618-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Elsayed A., Meyer G., Wille S.K.M. Influence of the yttrium content on the fracture strength of monolithic zirconia crowns after artificial aging. Quintessence Int. 2019;50:344–349. doi: 10.3290/j.qi.a42097. [DOI] [PubMed] [Google Scholar]
- 89.Yin R., Lee M., Bae T., Song K. Effect of finishing condition on fracture strength of monolithic zirconia crowns. Dent Mater J. 2019;38:203–210. doi: 10.4012/dmj.2017-391. [DOI] [PubMed] [Google Scholar]
- 90.Elshiyab S.H., Nawafleh N., Öchsner A., George R. Fracture resistance of implant-supported monolithic crowns cemented to zirconia hybrid-abutments : zirconia-based crowns vs. Lithium disilicate crowns. J Adv Prosthodont. 2018;10:65–72. doi: 10.4047/jap.2018.10.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Khayat W., Chebib N., Finkelman M., Khayat S., Ali A. Effect of grinding and polishing on roughness and strength of zirconia. J Prosthet Dent. 2017;10:65–72. doi: 10.1016/j.prosdent.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 92.Prado R.D., Pereira G.K.R., Bottino M.A., Melo R.M.V.L. Effect of ceramic thickness, grinding, and aging on the mechanical behavior of a polycrystalline zirconia. Braz Oral Res. 2017;31 doi: 10.1590/1807-3107BOR-2017.vol31.0082. e82:1–9. [DOI] [PubMed] [Google Scholar]
- 93.Zucuni C.P., Guilardi L.F., Rippe M.P., Kalil G., Pereira R., Valandro L.F. Fatigue strength of yttria-stabilized zirconia polycrystals: effects of grinding, polishing, glazing, and heat treatment. J Mech Behav Biomed Mater. 2017;75:512–520. doi: 10.1016/j.jmbbm.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 94.Dapieve K.S., Guilardi L.F., Rippe M.P., Kalil G., Pereira R., Valandro L.F. Mechanical performance of Y-TZP monolithic ceramic after grinding and aging: survival estimates and fatigue strength. J Mech Behav Biomed Mater. 2018;87:288–295. doi: 10.1016/j.jmbbm.2018.07.041. [DOI] [PubMed] [Google Scholar]
- 95.Ebeid K., Wille S., Salah T., Wahsh M., Zohdy M., Kern M. Evaluation of surface treatments of monolithic zirconia in different sintering stages. J Prosthodont Res. 2018;62:210–217. doi: 10.1016/j.jpor.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 96.Juntavee N., Attashu S. Effect of different sintering process on flexural strength of translucency monolithic zirconia. J Clin Exp Dent. 2018;10:e821–e830. doi: 10.4317/jced.54749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tong H., Tanaka C.B., Kaizer M.R., Zhang Y. Characterization of three commercial Y-TZP ceramics produced for their high-translucency, high-strength and high-surface area. Ceram Int. 2016;42:1077–1085. doi: 10.1016/j.ceramint.2015.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Elsaka S.E. Optical and mechanical properties of newly developed monolithic multilayer zirconia. J Prosthodont. 2017;28:e279–e284. doi: 10.1111/jopr.12730. [DOI] [PubMed] [Google Scholar]
- 99.Muñoz E.M., Longhini D., Antonio S.G., Adabo G.L. The effects of mechanical and hydrothermal aging on microstructure and biaxial flexural strength of an anterior and a posterior monolithic zirconia. J Dent. 2017;63:94–102. doi: 10.1016/j.jdent.2017.05.021. [DOI] [PubMed] [Google Scholar]
- 100.Sulaiman T.A., Abdulmajeed A.A., Donovan T.A., Vallittu P.K., Narhi T.O., Lassila L.V. The effect of staining and vacuum sintering on optical and mechanical properties of partially and fully stabilized monolithic zirconia. Dent Mater J. 2015;34:605–610. doi: 10.4012/dmj.2015-054. [DOI] [PubMed] [Google Scholar]
- 101.Sulaiman T.A., Abdulmajeed A.A., Shahramian K., Lassila L. Effect of different treatments on the flexural strength of fully versus partially stabilized monolithic zirconia. J Prosthet Dent. 2017;118:216–220. doi: 10.1016/j.prosdent.2016.10.031. [DOI] [PubMed] [Google Scholar]
- 102.Zhang F., Inokoshi M., Batuk M., Hadermann J., Naert I., Van Meerbeek B. Strength, toughness and aging stability of highly-translucent Y-TZP ceramics for dental restorations. Dent Mater. 2016;32:e327–e337. doi: 10.1016/j.dental.2016.09.025. [DOI] [PubMed] [Google Scholar]
- 103.Carrabba M., Keeling A.J., Aziz A., Vichi A., Fabian Fonzar R., Wood D. Translucent zirconia in the ceramic scenario for monolithic restorations: a flexural strength and translucency comparison test. J Dent. 2017;60:70–76. doi: 10.1016/j.jdent.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 104.Vichi A., Sedda M., Fabian Fonzar R., Carrabba M., Ferrari M. Comparison of contrast ratio, translucency parameter, and flexural strength of traditional and “augmented translucency” zirconia for CEREC CAD/CAM system. J Esthet Restor Dent. 2016;28:S32–S39. doi: 10.1111/jerd.12172. [DOI] [PubMed] [Google Scholar]
- 105.Candido L.M., Miotto L.N., Fais L.M.G., Cesar P.F., Pinelli L.A.P. Mechanical and surface properties of monolithic zirconia. Oper Dent. 2018:119–128. doi: 10.2341/17-019-L. [DOI] [PubMed] [Google Scholar]
- 106.Zhang Y., Lee J.J., Srikanth R., Lawn B.R. Edge chipping and flexural resistance of monolithic ceramics. Dent Mater. 2013;29:1201–1208. doi: 10.1016/j.dental.2013.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Yan J., Kaizer M.R., Zhang Y. Load-bearing capacity of lithium disilicate and ultra-translucent zirconias. J Mech Behav Biomed Mater. 2018;88:170–175. doi: 10.1016/j.jmbbm.2018.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Basso G.R., Moraes R.R., Borba M., Griggs J.A., Della Bona A. Flexural strength and reliability of monolithic and trilayer ceramic structures obtained by the CAD-on technique. Dent Mater. 2015;31:1453–1459. doi: 10.1016/j.dental.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 109.Sakai T., Sato T., Hisanaga R., Shinya A., Takemoto S., Yoshinari M. Optical properties and flexural strength of translucent zirconia layered with high-translucent zirconia. Dent Mater J. 2019;38:368–377. doi: 10.4012/dmj.2018-157. [DOI] [PubMed] [Google Scholar]
- 110.Ozer F., Naden A., Turp V., Mante F., Sen D., Blatz M.B. Effect of thickness and surface modifications on flexural strength of monolithic zirconia. J Prosthet Dent. 2017;119:987–993. doi: 10.1016/j.prosdent.2017.08.007. [DOI] [PubMed] [Google Scholar]
- 111.Kumchai H., Juntavee P., Sun A.F., Nathanson D. Effect of glazing on flexural strength of full-contour zirconia. Int J Dent. 2018 doi: 10.1155/2018/8793481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chougule K.J., Wadkar A. An in vitro comparative evaluation of flexural strength of monolithic zirconia after surface alteration utilising two different techniques. J Clin Diagn Res. 2017;11:ZC20–ZC23. doi: 10.7860/JCDR/2017/25177.10361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Nam M., Park M. Changes in the flexural strength of translucent zirconia due to glazing and low-temperature degradation. J Prosthet Dent. 2018;120 doi: 10.1016/j.prosdent.2018.07.017. 969.e1-969.e6. [DOI] [PubMed] [Google Scholar]
- 114.Schatz C., Strickstrock M., Roos M., Edelhoff D., Eichberger M., Zylla I.M. Influence of specimen preparation and test methods on the flexural strength results of monolithic zirconia materials. Materials (Basel) 2016;9:E180. doi: 10.3390/ma9030180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zucuni C.P., Guilardi L.F.F., Rippe M.P.P., Pereira G.K.R., Valandro L.F.F. Fatigue strength of yttria-stabilized zirconia polycrystals: effects of grinding, polishing, glazing, and heat treatment. J Mech Behav Biomed Mater. 2017;75:512–520. doi: 10.1016/j.jmbbm.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 116.Chevalier J., Cales B., Drouin J.M. Low-temperature aging of Y-TZP ceramics. J Am Ceram Soc. 1999;82:2150–2154. [Google Scholar]
- 117.Lughi V., Sergo V. Low temperature degradation -aging- of zirconia: a critical review of the relevant aspects in dentistry. Dent Mater. 2010;26:807–820. doi: 10.1016/j.dental.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 118.Alghazzawi T.F., Lemons J., Liu P.R., Essig M.E., Bartolucci A.A., Janowski G.M. Influence of low-temperature environmental exposure on the mechanical properties and structural stability of dental zirconia. J Prosthodont. 2012;21:363–369. doi: 10.1111/j.1532-849X.2011.00838.x. [DOI] [PubMed] [Google Scholar]
- 119.Stawarczyk B., Frevert K., Ender A., Roos M., Sener B., Wimmer T. Comparison of four monolithic zirconia materials with conventional ones: contrast ratio, grain size, four-point flexural strength and two-body wear. J Mech Behav Biomed Mater. 2016;59:128–138. doi: 10.1016/j.jmbbm.2015.11.040. [DOI] [PubMed] [Google Scholar]
- 120.Alghazzawi T.F., Janowski G.M. Correlation of flexural strength of coupons versus strength of crowns fabricated with different zirconia materials with and without aging. J Am Dent Assoc. 2015;146:904–912. doi: 10.1016/j.adaj.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 121.Flinn B.D., Raigrodski A.J., Mancl L.A., Toivola R., Kuykendall T. Influence of aging on flexural strength of translucent zirconia for monolithic restorations. J Prosthet Dent. 2017;117:303–309. doi: 10.1016/j.prosdent.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 122.Adabo G.L., Mariscal E.M., Hatanaka G.R. Flexural strength and microstructure of anterior/monolithic zirconia after low-temperature aging. Dent Mater. 2015;31:e48–e49. [Google Scholar]
- 123.Guilardi L.F., Pereira G.K.R., Gündel A., Rippe M.P., Valandro L.F. Surface micro-morphology, phase transformation, and mechanical reliability of ground and aged monolithic zirconia ceramic. J Mech Behav Biomed Mater. 2017;65:849–856. doi: 10.1016/j.jmbbm.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 124.Pereira G.K.R., Silvestri T., Camargo R., Rippe M.P., Amaral M., Kleverlaan C.J. Mechanical behavior of a Y-TZP ceramic for monolithic restorations: effect of grinding and low-temperature aging. Mater Sci Eng C. 2016;63:70–77. doi: 10.1016/j.msec.2016.02.049. [DOI] [PubMed] [Google Scholar]
- 125.Dehestani M., Adolfsson E. Phase stability and mechanical properties of zirconia and zirconia composites. Int J Appl Ceram Technol. 2013;10:129–141. [Google Scholar]
- 126.Nakamura K., Harada A., Kanno T., Inagaki R., Niwano Y., Milleding P. The influence of low-temperature degradation and cyclic loading on the fracture resistance of monolithic zirconia molar crowns. J Mech Behav Biomed Mater. 2015;47:49–56. doi: 10.1016/j.jmbbm.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 127.Leone R., Sorrentino R., Camposilvan E., Chevalier J., Zarone F., Ferrari M. In vitro aging and mechanical properties of translucent monolithic zirconia. Dent Mater. 2016;32:e98. doi: 10.1016/j.dental.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 128.Bergamo E., da Silva W., Cesar P., Del Bel Cury A. Fracture load and phase transformation of monolithic zirconia crowns submitted to different aging protocols. Oper Dent. 2016;41:E118–E130. doi: 10.2341/15-154-L. [DOI] [PubMed] [Google Scholar]
- 129.Salihoglu Yener E., Ozcan M., Kazazoglu E. A comparative study of biaxial flexural strength and Vickers microhardness of different zirconia materials: effect of glazing and thermal cycling. Brazilian Dent Sci. 2015;18:19. [Google Scholar]
- 130.Mitov G., Anastassova-Yoshida Y., Nothdurft F.P., von See C., Pospiech P. Influence of the preparation design and artificial aging on the fracture resistance of monolithic zirconia crowns. J Adv Prosthodont. 2016;8:30–36. doi: 10.4047/jap.2016.8.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Nordahl N., Vult von Steyern P., Larsson C. Fracture strength of ceramic monolithic crown systems of different thickness. J Oral Sci. 2015;57:255–261. doi: 10.2334/josnusd.57.255. [DOI] [PubMed] [Google Scholar]
- 132.Bankoğlu Güngör M., Karakoca Nemli S. Fracture resistance of CAD-CAM monolithic ceramic and veneered zirconia molar crowns after aging in a mastication simulator. J Prosthet Dent. 2017;119:473–480. doi: 10.1016/j.prosdent.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 133.Preis V., Behr M., Hahnel S., Handel G., Rosentritt M. In vitro failure and fracture resistance of veneered and full-contour zirconia restorations. J Dent. 2012;40:921–928. doi: 10.1016/j.jdent.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 134.Alshahrani F.A., Yilmaz B., Seidt J.D., McGlumphy E.A., Brantley W.A. A load-to-fracture and strain analysis of monolithic zirconia cantilevered frameworks. J Prosthet Dent. 2017;118:752–758. doi: 10.1016/j.prosdent.2017.01.028. [DOI] [PubMed] [Google Scholar]
- 135.Villefort R.F., Amaral M., Pereira G.K.R., Campos T.M.B., Zhang Y., Bottino M.A. Effects of two grading techniques of zirconia material on the fatigue limit of full-contour 3-unit fixed dental prostheses. Dent Mater. 2017;33:e155–e164. doi: 10.1016/j.dental.2016.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lopez-Suarez C., Rodriguez V., Pelaez J., Agustin-Panadero R., Suarez M.j. Comparative fracture behavior of monolithic and veneered zirconia posterior fixed dental prostheses. Dent Mater J. 2017;36:816–821. doi: 10.4012/dmj.2016-391. [DOI] [PubMed] [Google Scholar]
- 137.Feitosa S., Patel D., Borges A., Alshehri E., Bottino M., Özcan M. Effect of cleansing methods on saliva-contaminated zirconia—an evaluation of resin bond durability. Oper Dent. 2015;40:163–171. doi: 10.2341/13-323-L. [DOI] [PubMed] [Google Scholar]
- 138.Sharafeddin F., Shoale S. Effects of universal and conventional MDP primers on the shear bond strength of zirconia ceramic and nanofilled composite resin. J Dent (Shiraz, Iran) 2018;19:48–56. [PMC free article] [PubMed] [Google Scholar]
- 139.Rosentritt M., Preis V., Behr M., Hahnel S., Handel G., Kolbeck C. Two-body wear of dental porcelain and substructure oxide ceramics. Clin Oral Invest. 2012;16:935–943. doi: 10.1007/s00784-011-0589-9. [DOI] [PubMed] [Google Scholar]
- 140.Sasse M., Kern M. Survival of anterior cantilevered all-ceramic resin-bonded fixed dental prostheses made from zirconia ceramic. J Dent. 2014;42:660–663. doi: 10.1016/j.jdent.2014.02.021. [DOI] [PubMed] [Google Scholar]
- 141.Stawarczyk B., Frevert K., Ender A., Roos M., Sener B., Wimmer T. Comparison of four monolithic zirconia materials with conventional ones : contrast ratio, grain size, four-point fl exural strength and two-body wear. J Mech Behav Biomed Mater. 2016;59:128–138. doi: 10.1016/j.jmbbm.2015.11.040. [DOI] [PubMed] [Google Scholar]
- 142.Aung S., Phyo M., Takagaki T., Kham S. Effects of alumina-blasting pressure on the bonding to super / ultra-translucent zirconia. Dent Mater. 2019;35:730–739. doi: 10.1016/j.dental.2019.02.025. [DOI] [PubMed] [Google Scholar]
- 143.Inokoshi M., Shimizu H., Nozaki K., Takagaki T., Yoshihara K., Nagaoka N. Crystallographic and morphological analysis of sandblasted highly translucent dental zirconia. Dent Mater. 2018;34:508–518. doi: 10.1016/j.dental.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 144.Putra A., Chung K.H., Flinn B.D., Kuykendall T., Zheng C., Harada K. Effect of hydrothermal treatment on light transmission of translucent zirconias. J Prosthet Dent. 2017;118:422–429. doi: 10.1016/j.prosdent.2016.10.024. [DOI] [PubMed] [Google Scholar]
- 145.Xie H., Cheng Y., Chen Y., Qian M., Xia Y., Chen C. Improvement in the bonding of Y-TZP by room-temperature ultrasonic HF etching. J Adhes Dent. 2017;19:425–433. doi: 10.3290/j.jad.a39278. [DOI] [PubMed] [Google Scholar]
- 146.Torabi Ardekani K., Ahangari A.H., Farahi L. Marginal and internal fit of CAD/CAM and slip-cast made zirconia copings. J Dent Res Dent Clin Dent Prospects. 2012;6:42–48. doi: 10.5681/joddd.2012.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Moon J.E., Kim S.H., Lee J.B., Han J.S., Yeo I.S., Ha S.R. Effects of airborne-particle abrasion protocol choice on the surface characteristics of monolithic zirconia materials and the shear bond strength of resin cement. Ceram Int. 2016;42:1552–1562. [Google Scholar]