Abstract
Background
Erectile dysfunction (ED) is a common disorder, which affects at least 50% of males aged 50-70 years. According to EAU Guidelines on male sexual dysfunction, implantation of an inflatable penile prosthesis (IPP) is a valid, third-line therapeutic option for treatment of ED.
Objective
We conducted a retrospective single centre study to analyze mechanical reliability, complication rate, patient satisfaction and quality of life after penile prosthesis implantation.
Materials and Methods
A total of 126 electronic patient files after primary implantation of an IPP during a 5-year period were investigated. A structured telephone interview concerning patient and partner satisfaction was conducted at least 1 year after implant surgery.
Results
We found that 15 patients (11.9%) had revision surgery for various reasons. Mechanical failure occurred in 7.14% of the patients and was the main reason for revision surgery. Other major complications and complaints were loss of penile length (18.53%), postoperative pain (11.9%) and altered sensation (8.73%). No patients required explantation for infection, and 1 patient (0.79%) underwent revision surgery for an imminent erosion. One year or more after surgery, the patient and partner satisfaction rates, were 83.2 and 85.4%, respectively. We observed very high patient and partner satisfaction rates for the implantation of an IPP, with improvement of the general quality of life. These rates are negatively influenced by the occurrence of postoperative complications and complaints such as postoperative penile length shortening, pain and floppy glans syndrome. Most patients regain sexual function 6 weeks after surgery with no or minimal effect on the orgasm.
Conclusion
The implantation of a 3-piece IPP has proven an effective, third-line treatment for patients with ED.
Keywords: Inflatable penile prosthesis, Erectile dysfunction, Patient satisfaction
Introduction
Erectile dysfunction (ED) is a common disorder, which affects more than 50% of males aged 50-70 years [1]. ED is defined as the inability to achieve and maintain an erection sufficient for satisfactory sexual performance [2]. For many years prosthetic devices have been used to improve, replace or restore penile function [3]. According to EAU Guidelines on male sexual dysfunction, implantation of a penile prosthesis is a valid, third-line therapeutic option for treatment of ED, when medication and vacuum devices prove to be ineffective, unsatisfactory or contraindicated by comorbidities [2]. The first inflatable device was initially introduced by Scott in 1973, after which the long-term mechanical reliability and reduction in infection rate have been gradually improved [4]. Boston Scientific and Coloplast produce the most widely used inflatable penile prosthesis (IPP). Our primary study goal was to investigate patient satisfaction and quality of life (QoL) after implantation of a penile prosthesis and secondary goals were mechanical reliability and complication rate.
Materials and Methods
This retrospective study included 126 consecutive patients who underwent first-time implantation of an IPP by a single surgeon between September 2011 and August 2016. Coloplast and Boston Scientific prostheses were used. After obtaining approval of the local ethics committee (Jessa Hospital), patient data were collected from the electronic health records and 2 medical students performed a structured telephone interview. We were able to contact and interview 95 of the 126 patients who underwent surgery during this period. Four patients refused to participate, 3 patients were deceased and 24 patients could not be reached or could not be interviewed due to a medical condition. The inclusion criteria were a first-time implantation of an IPP and approval for a telephonic interview. Exclusion criteria were loss of follow-up within 1 year after implantation, major comorbidities and a combined implantation of an artificial sphincter prosthesis and refusal or inability for a telephone interview. We classified the patients in 5 etiological groups: vasculogenic, post-prostatectomy, Peyronie's disease, diabetes mellitus and others.
A retrospective analysis of the electronic health records was performed regarding complications and mechanical failure (loss of penile length, prolonged postoperative pain, altered sensation, autoinflation of the prosthesis, pronounced postoperative hematoma, floppy glans syndrome, penile deformity, infection and erosion of the prosthesis).
A structured telephone interview was conducted at least 1 year after implantation of the prosthesis to evaluate the patient and partner satisfaction rates. The questions asked included patient satisfaction, partner satisfaction, recommendation to a friend and overall QoL on a scale from 0 to 5, both pre- and post-operatively. The sexual encounter profile (SEP) questions 2 (“Were you able to insert your penis into your partner's vagina?”) and 3 (“Did your erection last long enough for you to complete intercourse with an orgasm?”) were asked pre- and 1 year post-operatively as well. Information regarding time to first sexual intercourse and first orgasm after activation was collected retrospectively during the telephone interview.
A descriptive analysis of the patient characteristics and the operative details was performed. A z-score was performed to investigate significant difference between the continuous data. The null hypothesis states that there is no difference between the 2 population proportions; or, more formally, that the difference is zero.
Results
A total of 126 patients underwent virgin implantation of an IPP during a 5-year period. The mean age at the time of surgery was 58.32 ± 8.68 years and mean postoperative follow-up was 39.39 ± 2.27 months. The etiology of ED was subdivided into 5 categories: vasculogenic (70.6%), Peyronie's disease (25.4%), post-prostatectomy (23%), diabetic (10.3%) and others (14.3%) such as neurogenic, traumatic, post-priapism etc. The mean duration of ED was 5.65 ± 5.68 years and 119 (94.4%) patients received previous treatment which were PDE5 inhibitors (89.6%), intracavernosal injections (34.9%), vacuum erection devices (9.5%) and other treatment options (8.7%). The mean testosterone level was within normal reference limits (5.02 ± 2.60 ng/ml) (Table 1).
Table 1.
Characteristics of the patient population (n = 126)
| Characteristic | n (%) |
|---|---|
| Mean age, year | 58.32± 8.68 |
| Mean follow-up period, month | 39.39± 2.27 |
| Etiologies of ED | |
| Vasculogenic, n (%) | 89 (70.6%) |
| Peyronie's disease, n (%) | 32 (25.4%) |
| Post-prostatectomy, n (%) | 29 (23.0%) |
| Diabetic, n (%) | 13 (10.3%) |
| Other, n (%) | 18 (14.3%) |
| Mean duration of ED, year | 5.65± 5.68 |
| Mean number of preoperative consultations | 3.49± 2.72 |
| Number of patients receiving previous treatment, n (%) | 119 (94.4%) |
| PDE5 inhibitor | 113 (89.6%) |
| Intracavernosal injections | 44 (34.9%) |
| Vacuum erection device | 12 (9.5%) |
| Other | 11 (8.7%) |
| Mean testosteron level, ng/ml | 5.02± 2.60 |
The surgical approach was infrapubic in 52 patients (41.3%) and penoscrotal in 74 patients (58.7%). The overall mean surgical duration was 49.71 ± 13.91 minutes. The mean duration for the infrapubic and penoscrotal approach was 52.80 ± 15.69 versus 47.01 ± 10.83 minutes, respectively (p < 0.05).
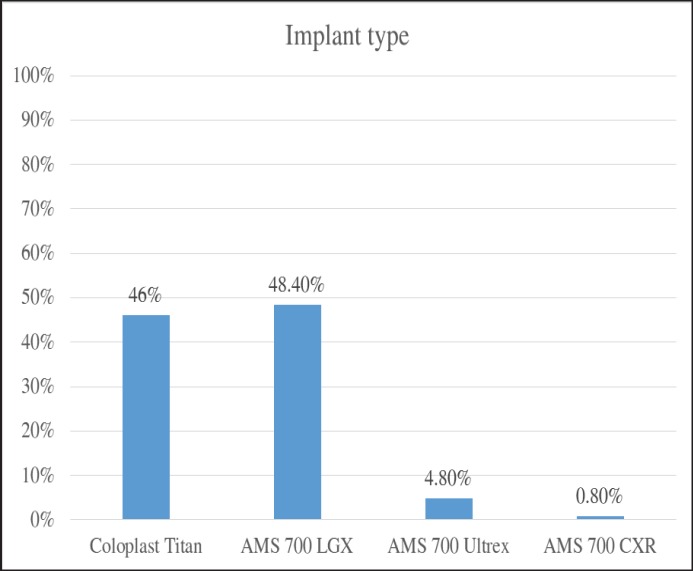
Out of 126 patients, 58 (46%) received a Coloplast Titan® implant, 61 (48.4%) with AMS 700™ LGX implant, 6 (4.8%) patients with Ultrex™ implant and 1 (0.8%) patient with AMS 700™ CXR implant. The length of the cylinders varied from 12 to 22 cm with rear tip extenders varying from 1 to 5 cm (Fig. 1). Only 1 patient (0.8%) received a wound drain system peroperatively.
Fig. 1.
Bar chart of the different types of IPP used in our patient cohort.
Penile shortening was reported in 23 patients (18.25%) and was the most frequent complaint after surgery, followed by postoperative pain in 15 patients (11.9%). No chronic pain (more than 6 weeks) complaints were reported.
Mechanical failure occurred in 9 patients (7.1%); 4 patients with pump-dysfunction, 4 patients with leakage of the tubing and/or reservoir and 1 patient with malfunction of the cylinders 5 months after implantation. Two out of 4 patients (50%) with pump-dysfunction needed revision. Of all mechanical failures, 77.8% occurred with an AMS-prosthesis. Minor auto-inflation was reported by 8 patients (6.3%) without significant inconvenience for the patient. Postoperative hematoma formation occurred in 7 patients (5.6%) and resolved spontaneously after a few weeks, causing only a delay in activation of the prosthesis. Floppy glans syndrome was present in 6 patients (4.8%) and 5 patients (3.97%) complained of postoperative penile deformity.
Three patients (2.4%) received prolonged antibiotic treatment due to possible signs of an infection but no explantation of the prosthesis or salvage procedure was required.
A total of 15 patients (11.9%) had revision surgery for various reasons such as impending erosion, mechanical failure, herniation of implant components, floppy glans syndrome etc. One patient (0.8%) had an imminent erosion and needed revision of the prosthesis (Table 2). We found no significant difference in overall complication rate between the infrapubic and penoscrotal surgical approach. There was however, a significant difference in the occurrence of a floppy glans syndrome between both groups (p < 0.05, Table 3). Floppy glans syndrome occurred in 5/52 patients (9.61%) who underwent implantation with the infrapubic approach and in 1/74 patients (1.35%) with the penoscrotal approach.
Table 2.
Overall complaints and complications (n = 126)
| Complaint/complication | n (%) |
|---|---|
| Loss of penile length | 23 (18.25%) |
| Postoperative pain | 15 (11.9%) |
| Altered sensation | 11 (8.73%) |
| Mechanical failure | 9 (7.14%) |
| Auto inflation | 8 (6.35%) |
| Hematoma | 7 (5.56%) |
| Floppy glans syndrome | 6 (4.76%) |
| Penile deformity | 5 (3.97%) |
| Possible signs of infection | 3 (2.38%) |
| Infection | 0 (0%) |
| Imminent erosion | 1 (0.79%) |
| Other | 17 (13.49%) |
Table 3.
Complaints and complications for infrapubic and penoscrotal approach
| Complaint/complication | Infrapubic approach, n (%) | Penoscrotal approach, n (%) |
|---|---|---|
| Loss of penile length | 11 (21%) | 12 (16%) |
| Pain | 5 (9.16%) | 10 (13.51%) |
| Altered sensation | 2 (3.84%) | 9 (12.16%) |
| Mechanical failure | 6 (11.54%) | 3 (4.05%) |
| Auto inflation | 3 (5.77%) | 5 (6.75%) |
| Hematoma | 1 (1.92%) | 6 (8.11%) |
| Floppy glans syndrome | 5 (9.61%) | 1 (1.35%) |
| Penile deformity | 3 (5.77%) | 2 (2.70%) |
| Possible sings of infection | 1 (1.92%) | 2 (2.70%) |
| Imminent erosion | 0 (0%) | 1 (1.35%) |
| Other | 10 (19.23%) | 7 (9.16%) |
Of all patients, 95 could be reached by telephone, of which 79 (83.2%) were satisfied with the penile implant 1 year or longer after surgery and 80 of them (84.2%) would recommend a penile implant to a friend. In the successfully contacted patients, 93 had a regular partner, of which 76 (85.4%) were satisfied, 1 year or longer after penile implant surgery.
The prosthesis was activated after an average period of 6 weeks and 36 of the respondents (37.89%) had sexual intercourse within 2 weeks after activation. Fourteen patients (14.74%) had intercourse between 2 and 4 weeks after activation, 24 patients (25.26%) had intercourse between 1 and 2 months after activation and 18 patients (18.95%) had intercourse 2 months or longer after activation (Table 4). Three respondents (3.16%) did not yet have intercourse on the moment of the interview. The time to first orgasm after activation of the prosthesis is shown in Table 5. Eight patients (8.4%) did not reach an orgasm 1 year or longer after surgery. Of all 87 patients who did reach an orgasm, 63 patients (72.41%) had their first orgasm during their first sexual intercourse after activation of the prosthesis.
Table 4.
Time to first sexual intercourse after activation of the prosthesis (n = 95)
| Time to intercourse | n (%) |
|---|---|
| < 2 weeks | 36 (37.89%) |
| 2–4 weeks | 14 (14.74%) |
| 5–8 weeks | 24 (25.26%) |
| > 8 weeks | 18 (18.95%) |
| No intercourse | 3 (3.16%) |
Table 5.
Time to first orgasm after activation of the prosthesis (n = 95)
| Time to first orgasm | n (%) |
|---|---|
| < 2 weeks | 25 (26.32%) |
| 2–4 weeks | 12 (12.63%) |
| 5–8 weeks | 20 (21.05%) |
| > 8 weeks | 30 (31.58%) |
| No orgasm | 8 (8.42%) |
The average QoL before surgery was 2 ± 1.13 on a scale from 0 to 5 while the average QoL after surgery was 3.5 ± 1.26. Before surgery 18/126 patients (14.3%) and 3/126 patients (2.4%) responded positively on SEP questions 2 and 3, respectively. At least 1 year after surgery 92/95 respondents (96.8%) responded positively on SEP question 2 and 84/95 respondents (88.4%) on question 3 (Table 6).
Table 6.
Percentages before and after surgery who responded positively onto SEP questions 2 and 3
| Question | Before surgery, n (%) | After surgry, n (%) |
|---|---|---|
| SEP-2 | 18 (14.3%) | 92 (96.8%) |
| SEP-3 | 3 (2.4%) | 84 (88.4%) |
Discussion
Implantation of a penile prosthesis is a valid, third-line therapeutic option for patients with ED, refractory to classic treatment. Overall outcomes concerning mechanical failure, complications such as infection and erosion and patient satisfaction prove to be satisfactory in recent reports.
Mechanical Reliability
Mechanical failure is a major but sometimes inevitable complication in prosthetic surgery. The most common causes of mechanical failure include fluid leakage, pump-dysfunction, cylinder aneurysm and rupture, kinking of the tubing and auto-inflation [5,6]. Some of these complications require complete removal of the prostheses while others may be resolved by revision surgery. In a prospective multicentric study in 2,384 patients, Wilson et al. [7] noted a 5- and 10-year overall mechanical survival for primary implants of 88.9 and 79.4%, respectively. In our study, mechanical failure was not the main complication and occurred in only 9 out of 126 patients (7.1%) but was the main reason for revision surgery. Out of 9 patients with mechanical failure, 7 (77.7%) patients underwent a revision surgery.
Complications and Complaints
Infection of the prosthesis is an infrequent but severe complication, which occurs mostly immediately postoperative or in the first year after implantation. Still it can rarely present as a low-grade infection years after the implantation. In recent literature, the incidence varies from 0.6 to 8.9%, depending on the type of prosthesis used, the surgical indication, the follow-up period and patient population. Risk factors for infections are diabetes mellitus, spinal cord injury, use of immunosuppressive drugs and revision surgery. Infection is most commonly caused by skin-bacteria and Staphylococcus species are the most commonly isolated microorganisms [8,9,10]. Removal of the prosthesis is always required to eliminate the infection as antibiotic therapy is not effective. Reimplantation of the prosthetic device is usually delayed for 3 to 6 months in order to reduce the occurrence of re-infection and to allow proper wound healing. Alternatively, a novel prosthesis can be reimplanted right after prosthesis removal and abundant wound irrigation with antiseptic or antibiotic solutions [11]. We did not observe prosthetic infection in our population so far. Three patients (2.4%) did show signs (warmth, redness) of a possible infection short after the implantation. They received prolonged antibiotic treatment and no explantation of the prosthesis or salvage procedure was required.
Erosion of the device is another major complication after penile prosthesis implantation. Erosion usually occurs late and is always associated with infection. Erosion with a visible prosthesis should be treated by removal of the device, while impending erosion could be salvaged [6]. In our series, we noted 1 patient (1.35%) with an imminent erosion, who had successful revision surgery.
A common complaint after penile prosthesis implantation is loss of penile length, which has an important negative impact on overall patient satisfaction [12]. The subjective feeling of loss of penile length occurred in 18.53% of our patients and is therefore the most frequent complaint in our study group. It also had a significant impact on the satisfaction rates (p < 0.05). Only 10/17 patients (58.8%) with subjective loss of penile length were satisfied.
Pain is another important, subjective factor in determining success or failure of the implantation. Most studies report postoperative pain in up to 4-6 weeks after surgery. Postoperative pain in our series was the second most prevalent complaint (11.9%). Postoperative pain was correlated with lower satisfaction rates and a significant lower satisfaction rate (57.15%) was observed in this subgroup of patients (p < 0.05).
Another less-frequent complaint after surgery is hypermobility of the glans penis despite shaft erection (floppy glans syndrome). This can make penetration difficult and even painful. Only 6 patients (4.8%) complained about a floppy glans but these patients were significantly less satisfied (33.3%) (p < 0.05) [13].
Two types of surgical techniques, the infrapubic and penoscrotal approach, were used in our series. As surgical approach may influence complication rates, an analysis was performed. This demonstrated a significant lower occurrence of floppy glans syndrome in the penoscrotal approach group, probably due to better distal dilatation. Due to the abovementioned lower occurrence of floppy glans syndrome, better peroperative visualisation and a shorter operating time we prefer the penoscrotal approach to the infrapubic appraoch.
Patient and Partner Satisfaction
Patient satisfaction can be largely referred to as “an attitudinal response to the patient's clinical encounter” [10,12] and is clearly affected by many parameters like patient expectations, patient comorbidities, partner attitudes, surgical complications and premature device failures [12,14,15]. Multiple scoring systems exist to assess the satisfaction rate after IPP insertion. The Erectile Dysfunction Inventory of Treatment Satisfactions score and the International Index of Erectile Function score are larger questionnaires used in several studies. In our study, we defined patient and partner satisfaction by a single question and evaluated the subjective improvement in QoL on a scale from 1 to 5.
Previous studies already indicate high satisfaction rates for IPP, which is confirmed by our data. We noted an overall satisfaction rate of 83.2%, 1 year or longer after implantation and 84.2% of the patient population would recommend the same procedure to a friend. These high satisfaction rates support our opinion that implantation of an IPP should be offered (early) to a patient as a third-line treatment option or when a permanent solution for their ED is desirable.
A normal sex life is an important factor in men's overall QoL. Patients with ED tend to have lower QoL scores than patients without ED. We compared our patient's general QoL by scoring their QoL from 0/5 to 5/5 before and after surgery. A 30% increase in QoL from 2/5 pre-operatively to 3.5/5 (SD = 1.26) post-operatively was observed.
In previous literature, the 3-piece IPP seems to be the prosthesis with the highest satisfaction rates and no difference could be found between Boston Scientific and Coloplast penile prosthesis. In our study we only used the 3-piece IPP. Most of our patients received either the AMS-LGX or the Coloplast Titan prosthesis. The satisfaction rates were respectively 80.4 and 91.1%, but no significant difference was noted.
Sexual satisfaction of the patient is largely influenced by their partner's satisfaction, which makes partner's satisfaction rates an important parameter [16]. Porena et al. [17] demonstrated in 46 patients a high partner satisfaction rate of 82% 1 year after surgery next to a high patients' satisfaction rate. A study by Vakalopoulos et al. [16] confirmed these results with a high mean female partners' Erectile Dysfunction Inventory of Treatment Satisfactions score and highlighting high satisfaction rates from their male partner's treatment. Regression analysis revealed a direct linear correlation between the degree of satisfaction for male patients and female partners. This correlation and high partner satisfaction rates were also demonstrated in our study. Seventy-six out of 93 (85.4%) partners were happy with the prosthesis. Only in 2 cases, we saw a satisfied patient without a satisfied partner. Conversely, 1 partner did mention to be satisfied without a satisfied patient.
Lower overall satisfactions rates could be prevented by preoperative counselling and creating realistic postoperative expectations, which might even be the most important factor in postoperative satisfaction. This requires shared decision making between surgeon and the patient [18]. Informed consent prior to surgery must include detailed discussions about risks that are unique to penile implant surgery [19].
Usage of the Prosthesis
The penile prosthesis can be activated at 4 weeks after surgery. An earlier activation is possible but is mostly discouraged because of pain or residual swelling [20]. The average activation time in our patient group is 6 weeks, after which patients can restart their sexual activities. More than 50% of the patients had their first sexual intercourse within 4 weeks after activation and 37.89% even had intercourse within 2 weeks after activation. Less than 20% had their first sexual intercourse more than 2 months after activation. Only 3 patients never used their prosthesis, even though it was functional. They were satisfied with the procedure but suffered from relationship problems or comorbidities. There is minimal or no effect on the patient's orgasm after implantation of a penile prosthesis, 72% of the patients already had an orgasm during their first sexual encounter.
The SEP questions 2 and 3 were asked pre- and 1 year post-operatively and an increase of 82.5% was observed for SEP questions 2 and 86 % for SEP questions 3, supporting previously described satisfaction rates.
There are some limitations to the present study. First, we performed a retrospective cohort study, this may be partly balanced by the, for this area, large sample size. Secondly, data concerning patient and partner satisfaction were collected using a telephone interview. A written questionnaire would have been more appropriate. Lastly, four different types of penile implants were used. Although there are no significant differences between these implants, there could be a difference in long-term use.
Conclusion
The implantation of a 3-piece IPP has proven an effective, third-line treatment for patients with ED. High patient and partner satisfaction rates were observed at least 1 year after implantation of the device. Extensive preoperative counselling is mandatory for obtaining good postoperative satisfaction rates. The infrapubic or penoscrotal approach are both reliable surgical techniques, with our personal preference for the penoscrotal approach because of the significant lower occurrence of floppy glans syndrome, shorter operating time and good visual exposure. Penile prosthesis is a safe procedure and should be offered to patients as a third-line treatment for ED or when a permanent solution for their ED is desirable.
References
- 1.Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151:54–61. doi: 10.1016/s0022-5347(17)34871-1. [DOI] [PubMed] [Google Scholar]
- 2.Hatzimouratidis K, Giuliano F, Moncada I, Muneer A, Salonia A, Verze P. Erectile dysfunction, premature ejaculation, penile curvature and priapism. EAU Guidelines. 2016 [Google Scholar]
- 3.Schultheiss D, Gabouev AI, Jonas U. Nikolaj A. Bogoraz (1874-1952): pioneer of phalloplasty and penile implant surgery. J Sex Med. 2005;2:139–146. doi: 10.1111/j.1743-6109.2005.20114.x. [DOI] [PubMed] [Google Scholar]
- 4.Scott F, Bradley W, Timm G. Management of erectile impotence: use of implantable inflatable prosthesis. Urology. 1973;2:80–82. doi: 10.1016/0090-4295(73)90224-0. [DOI] [PubMed] [Google Scholar]
- 5.Bettocchi C, Palumbo F, Spilotros M, Palazzo S, Saracino G, Martino P, Battaglia M, Selvaggi FP, Ditonno P. Penile prostheses. Ther Adv Urol. 2010;2:35–40. doi: 10.1177/1756287209359174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chung E, Solomon M, DeYoung L, Brock GB. Clinical outcomes and patient satisfaction rates among elderly male aged ≥75 years with inflatable penile prosthesis implant for medically refractory erectile dysfunction. World J Urol. 2014;32:173–177. doi: 10.1007/s00345-013-1102-7. [DOI] [PubMed] [Google Scholar]
- 7.Wilson S, Delk J, Salem E, Cleves M. Longterm survival of inflatable penile prostheses: single surgical group experience with 2,384 first-time implants spanning two decades. J Sex Med. 2007;4:1074–1079. doi: 10.1111/j.1743-6109.2007.00540.x. [DOI] [PubMed] [Google Scholar]
- 8.Anastasiadis A, Wilson S, Burchardt M, Shabsigh R. Long-term outcomes of inflatable penile implants: reliability, patient satisfaction and complication management. Curr Opin Urol. 2001;11:619–623. doi: 10.1097/00042307-200111000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Trost L, McCaslin R, Linder B, Hellstrom W. Long-term outcomes of penile prosthesis for the treatment of erectile dysfunction. Expert Rev Med Devices. 2013;10:353–367. doi: 10.1586/erd.12.92. [DOI] [PubMed] [Google Scholar]
- 10.Mulcahy JJ, Kramer A, Brant WO, Parker JL, Perito PE, Myers JB, Bryson R, Dunne M. Current management of penile implant infections, device reliability, and optimizing cosmetic outcome. Curr Urol Rep. 2014;15:413. doi: 10.1007/s11934-014-0413-6. [DOI] [PubMed] [Google Scholar]
- 11.Mulcahy JJ. Current approach to the treatment of penile implant infections. Ther Adv Urol. 2010;2:69–75. doi: 10.1177/1756287210370330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee KC, Brock GB. Strategies for maintaining penile size following penile implant. Transl Androl Urol. 2012;2:67–73. doi: 10.3978/j.issn.2223-4683.2013.01.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bickell M, Manimala N, Parker J, Steixner B, Wiegand L, Carrion R. Floppy Glans Syndrome: pathogenesis and treatment. Sex Med Rev. 2016;4:149–156. doi: 10.1016/j.sxmr.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 14.Akakpo W, Pineda M, Burnett AL. Critical analysis of satisfaction assessment after penile prosthesis surgery. Sex Med Rev. 2017;5:244–251. doi: 10.1016/j.sxmr.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 15.Bernal RM, Henry GD. Contemporary patient satisfaction rates for three-piece inflatable penile prostheses. Adv Urol. 2012;2012:707321. doi: 10.1155/2012/707321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vakalopoulos I, Kampantais S, Ioannidis S, Laskaridis L, Dimopoulos P, Toutziaris C, Koptsis M, Henry GD, Katsikas V. High patient satisfaction after inflatable penile prostheses implantation correlates with female partner satisfaction. J Sex Med. 2013;10:2774–2781. doi: 10.1111/jsm.12311. [DOI] [PubMed] [Google Scholar]
- 17.Porena M, Mearini L, Mearini E, Marzi M, Zucchi A. Penile prosthesis implantation and couple's satisfaction. Urol Int. 1999;63:185–187. doi: 10.1159/000030444. [DOI] [PubMed] [Google Scholar]
- 18.Lyons MD, Carson CC, Coward RM. Special considerations for placement of an inflatable penile prosthesis for the patient with Peyronie's disease: techniques and patient preference. Med Devices (Auckl) 2015;8:331–340. doi: 10.2147/MDER.S57252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Narang GL, Figler BD, Coward RM. Preoperative counseling and expectation management for inflatable penile prosthesis implantation. Transl Androl Urol. 2017;6((suppl 5)):S869–S880. doi: 10.21037/tau.2017.07.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levine LA, Becher EF, Bella AJ, Brant WO, Kohler TS, Martinez-Salamanca JI, Trost L, Morey AF. Penile prosthesis surgery: current recommendations from the International Consultation on Sexual Medicine. J Sex Med. 2016;13:489–518. doi: 10.1016/j.jsxm.2016.01.017. [DOI] [PubMed] [Google Scholar]