Abstract
Follicular hyperkeratotic spicules is a rare skin disorder that is usually associated with multiple myeloma. The condition typically presents with tiny hyperkeratotic spicules in follicular distribution and predominantly on the face. To our knowledge, there has been one reported case of this condition without underlying disease. We herein report the second case of idiopathic follicular hyperkeratotic spicules in a 54-year-old Thai woman presenting with multiple follicular horn-like spicules on her face and neck.
Keywords: Follicular hyperkeratosis, Myeloma, Spiky, Spinulosis, Spiny
Introduction
Follicular hyperkeratotic spicules is a rare cutaneous disorder characterized by spiky, skin-colored to yellowish, follicular digitate hyperkeratosis. This condition was firstly introduced by Heidenstorm and Tottie in 1944 [1]. Since then, several subsequent case reports had been published, sharing similar locations on the face, particularly the nose, chin, and forehead. Although its etiology is still unknown, it is often reported in association with multiple myeloma. It is also associated with other conditions such as Crohn's disease and drug-induced reactions [2, 3, 4]. We herein report a case of follicular hyperkeratotic spicules without associated condition.
Case Report
A 54-year-old Thai female presented with a group of multiple spiky spicules along her face, jawline, and neck for 1 month. No pain or pruritus accompanied the lesions. The spicules were easily removed by scratching or rubbing without bleeding, then reappeared within a few weeks. She denied previous illness before the development of the skin lesion. She had no underlying disease and was not taking any supplement or medication.
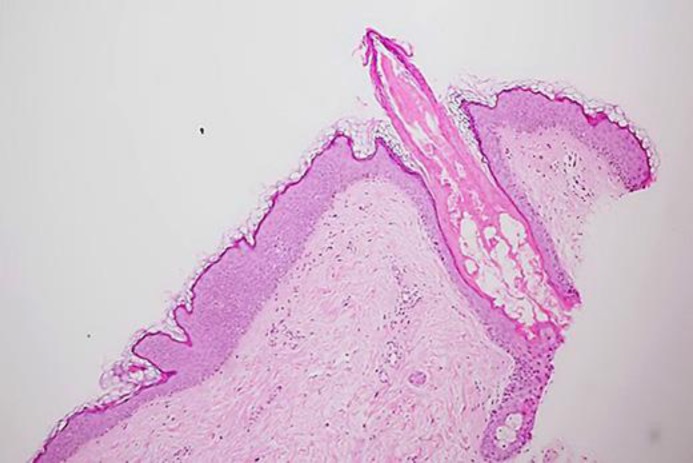
Physical examination revealed multiple discrete tiny filiform hyperkeratotic papules on the face and neck (Fig. 1). The histopathological study demonstrated dilated follicles with digitate follicular hyperkeratosis and parakeratosis. Neither trichostasis nor koilocyte was observed (Fig. 2). Laboratory investigations, including complete blood count, blood chemistry, serum protein electrophoresis, and urinalysis were within normal limit. Based on the history, physical examination, histopathological study, and laboratory findings, the diagnosis of idiopathic follicular hyperkeratotic spicules was performed. The patient received topical 0.1% adapalene gel to be applied once daily. Two months later, the condition showed mild improvement.
Fig. 1.
Multiple discrete tiny filiform hyperkeratotic papules on the face and neck.
Fig. 2.
Microscopic examination showing dilated follicle with digitate follicular hyperkeratosis and parakeratosis together with sparse superficial perivascular cells infiltration of lymphocytes (hematoxylin-eosin, original magnification ×20).
Discussion
Follicular hyperkeratotic spicules is a rare skin disorder presenting with tiny, skin-colored to yellowish, hyperkeratotic spikes that are commonly located on the face, specifically on the nose, and occasionally on the trunk and extremities. However, the lesion can appear anywhere on the body. Most of the affected patients were middle-aged and elderly [4]. Histopathological examination reveals focal spike-like orthokeratotic or parakeratotic column filling the infundibulum with eosinophilic inclusions and protruding above the epidermis. Lymphocytic infiltrations in the papillary dermis are usually sparse [5, 6, 7].
The disease is often reported as being a paraneoplastic cutaneous sign of multiple myeloma or cryoglobulinemia [3]. Additionally, it has also been reported in associations with other conditions such as Crohn's disease, HIV infection, and drug-induced reactions from cyclosporine, sorafenib, and acitretin [8, 9, 10, 11]. There has been one reported case without the associated disease [5]. To our knowledge, our patient is the second reported case of idiopathic follicular hyperkeratotic spicules. Previously reported cases of this disorder are demonstrated in Table 1 and Table 2 [1, 2, 3, 5, 6, 7, 8, 9, 10, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23].
Table 1.
Reported cases of follicular hyperkeratotic spicules
| Author | Year | Sex | Age | Distribution | Associations | Treatment response |
| Heidenstorm and Tottie [1] | 1944 | M | 39 | Face, chest | Multiple myeloma | NA |
| Bravermana | 1970 | M | NA | Face | Multiple myeloma | NA |
| Lukitsch et al. [12] | 1985 | M | 42 | Face, arms | Multiple myeloma, cryoglobulinemia | Disappearance |
| Kuokkanen et al. [13] | 1987 | M | 54 | Face, legs | Multiple myeloma | Disappearance |
| Castanet et al.a | 1987 | M | 59 | Face, scalp, chest, extremities | Multiple myeloma | Disappearance |
| Brunner et al.a | 1987 | M | 66 | Face, scalp | Multiple myeloma | Disappearance |
| Bork et al. [14] | 1990 | M | 62 | Face | Multiple myeloma, cryoglobulinemia | No response |
| Requena et al. [3] | 1995 | M | 79 | Face, scalp, back | Multiple myeloma, cryoglobulinemia | Disappearance |
| Paul et al. [15] | 1995 | M | 61 | Face, scalp, lumbar area | Multiple myeloma | Partial response |
| Pestarino et al.a | 2000 | M | 79 | Face | Multiple myeloma | Partial response |
| Braun et al. [7] | 2002 | M | 58 | Face | Multiple myeloma | Increase with worsening of multiple myeloma |
| Satta et al. [6] | 2003 | F | 68 | Face | Multiple myeloma, cryoglobulinemia | Disappearance, recurrence with worsening multiple myeloma |
| Satta et al. [6] | 2003 | M | 79 | Face, trunk, arms | Multiple myeloma | NA |
| Miller et al. [16] | 2006 | F | 70 | Face | Multiple myeloma | Partial response |
| Tay et al. [17] | 2010 | F | 55 | Face | Multiple myeloma | Disappearance |
| Dalal et al. [18] | 2010 | F | 67 | Face | Multiple myeloma | Increase with worsening of multiple myeloma |
| van Boheemen et al. [19] | 2015 | M | 70s | Face, chest, arms | Multiple myeloma | Disappearance (cidofovir gel 1% added) |
| Aloi et al. [2] | 1989 | F | 38 | Trunk, neck, upper extremities | Crohn's disease | No response |
NA, not available.
Reference cited in Satta et al. [6].
Table 2.
Reported cases of follicular hyperkeratotic spicules (continued)
| Author | Year | Sex | Age | Distribution | Associations | Treatment response |
| Farina et al. [20] | 1998 | F | 78 | Face | Polycythemia vera (suspected of demodicidosis) | No response |
| Franck et al. [8] | 2010 | M | 61 | Face, scalp, trunk, arms | Sorafenib-induced reaction | Disappearance after stop medication |
| Franck et al. [8] | 2010 | M | 72 | Face, scalp, trunk, arms | Sorafenib-induced reaction | Disappearance after stop medication |
| Franck et al. [8] | 2010 | M | 78 | Face, scalp, trunk, arms | Sorafenib-induced reaction | Disappearance after stop medication |
| Franck et al. [8] | 2010 | M | 59 | Face, scalp, trunk, arms | Sorafenib-induced reaction | Disappearance after stop medication |
| Franck et al. [8] | 2010 | M | 49 | Face, scalp, trunk, arms | Sorafenib-induced reaction | Disappearance after stop medication |
| Franck et al. [8] | 2010 | F | 79 | Face, scalp, trunk, arms | Sorafenib-induced reaction | Disappearance after stop medication |
| Franck et al. [8] | 2010 | M | 65 | Face, scalp, trunk, arms | Sorafenib-induced reaction | Disappearance after stop medication |
| Franck et al. [8] | 2010 | M | 60 | Face, scalp, trunk, arms | Sorafenib-induced reaction | Disappearance after stop medication |
| Franck et al. [8] | 2010 | M | 60 | Face, scalp, trunk, arms | Sorafenib-induced reaction | Disappearance after stop medication |
| Chia et al. [21] | 2010 | M | 22 | Neck | SuspectedPropionibacterium acnes | Response to oral erythromycin |
| Nemeth et al. [22] | 2016 | M | NA | Scalp | Lung transplantation | Response to systemic valganciclovir |
| Yanik et al. [9] | 2016 | F | 51 | Face, neck | Acitretin-induced reaction | Disappearance after stop medication |
| Ruiz-Rivero et al. [23] | 2017 | F | 16 | Face | Plaque morphea (suspected demodicosis) | Response to ivermectin |
| Maddy et al. [10] | 2018 | M | 52 | Face | HIV infection | Increased with worsening HIV infection |
| Kim et al. [5] | 1997 | F | 52 | Face | Idiopathic | No response |
| Current case | 2019 | F | 54 | Face | Idiopathic | Partial response |
NA, not available.
Differential diagnosis of follicular hyperkeratotic spicules includes lichen spinulosus, multiple minute digitate hyperkeratosis, trichodysplasia spinulosa, and spiky follicular mycosis fungoides [4, 24, 25, 26, 27]. Details of these diseases regarding clinical manifestations, histopathological findings, and their associated conditions are summarized in Table 3.
Table 3.
Differential diagnosis of follicular hyperkeratotic spicules
| Diseases | Clinical findings | Histopathology | Associations |
| Lichen spinulosus | Patches of follicular papules topped by keratotic spines, predilection for trunk and extremities | Dilated infundibulum filled with columnar orthokeratotic keratin plug, occasionally dense lymphocytic perifollicular infiltrates | Ichthyosis, Atopic dermatitis, HIV infection |
| Multiple minute digitate hyperkeratosis | Multiple minute digitate hyperkeratosis, predominantly affect trunk and extremities | Nonfollicular, focal columns of orthokeratotic hyperkeratosis arising from a tented epidermis, with prominent stratum granulosum | Familial, sporadic, post-inflammation, paraneoplastic |
| Trichodysplasia spinulosa | Multiple keratotic spicules on follicular erythematous papules, mostly on face | Dilated and dystrophic hair follicles with proliferation of the inner root sheath cells containing large trichohyaline granules | Immunocompromised host, associated with papovavirus |
| Spiky follicular mycosis fungoides | Slightly erythematous, hyperkeratotic spiky or coneshaped follicular papules | Hyperkeratotic columns protruding from follicular plugs with infiltration of atypical lymphocytes around follicular epithelium | Mycosis fungoides, Sezary syndrome |
The etiology of follicular hyperkeratotic spicules is still inconclusive. There have been various hypotheses regarding the pathogenesis of the disease. Bork et al. [14]demonstrated that myeloma dysprotein and cryoglobulins precipitated in the follicular infundibulum, resulting in follicular plugs and spiky presentation. A subsequent report of cryoglobulins accumulation in follicular content obtained from a patient with multiple myeloma supports this finding [3]. Besides, there has been speculation that Merkel cell polyomavirus, Propionibacterium acne, and Demodex folliculorum are the causes of the disease [15, 19, 20, 21, 22, 23]. However, there is a lack of evidence to support that these microorganisms play a role in the disease pathogenesis.
Several topical agents, including 12% lactic acid cream, adapalene gel, tretinoin cream, fluocinolone acetonide oil, and antibiotics have been tried to treat follicular hyperkeratotic spicules [5, 16]. None of them showed effectiveness. However, improvement of the lesions in patients with multiple myeloma after receiving systemic chemotherapy has been reported [6, 12, 13, 16].
In conclusion, we present a rare case of idiopathic follicular hyperkeratotic spicules. Due to multiple reports of associated conditions, we recommend that complete physical examination and laboratory evaluation are important to find the associated disease. Moreover, long-term monitoring and re-assessment are suggestive in all cases of idiopathic follicular hyperkeratotic spicules.
Statement of Ethics
The patient provided written informed consent to perform all necessary investigations, to take clinical photographs, and use them for research purposes and publication. This case report was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
None.
Author Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for the manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
References
- 1.Heidenstrom N, Tottie M. Haut und gelenkvanderungen bei Multiplem myelom. Acta Derm Venereol. 1944;24:192–9. [Google Scholar]
- 2.Aloi FG, Molinero A, Pippione M. Parakeratotic horns in a patient with Crohn's disease. Clin Exp Dermatol. 1989 Jan;14((1)):79–81. doi: 10.1111/j.1365-2230.1989.tb00892.x. [DOI] [PubMed] [Google Scholar]
- 3.Requena L, Sarasa JL, Ortiz Masllorens F, Martín L, Piqué E, Olivares M, et al. Follicular spicules of the nose: a peculiar cutaneous manifestation of multiple myeloma with cryoglobulinemia. J Am Acad Dermatol. 1995 May;32((5 Pt 2)):834–9. doi: 10.1016/0190-9622(95)91542-7. [DOI] [PubMed] [Google Scholar]
- 4.Caccetta TP, Dessauvagie B, McCallum D, Kumarasinghe SP. Multiple minute digitate hyperkeratosis: a proposed algorithm for the digitate keratoses. J Am Acad Dermatol. 2012 Jul;67((1)):e49–55. doi: 10.1016/j.jaad.2010.07.023. [DOI] [PubMed] [Google Scholar]
- 5.Kim TY, Park YM, Jang IG, Yi JY, Kim CW, Song KY. Idiopathic follicular hyperkeratotic spicules. J Am Acad Dermatol. 1997 Mar;36((3 Pt 1)):476–7. doi: 10.1016/s0190-9622(97)80231-9. [DOI] [PubMed] [Google Scholar]
- 6.Satta R, Casu G, Dore F, Longinotti M, Cottoni F. Follicular spicules and multiple ulcers: cutaneous manifestations of multiple myeloma. J Am Acad Dermatol. 2003 Oct;49((4)):736–40. doi: 10.1067/s0190-9622(03)00122-1. [DOI] [PubMed] [Google Scholar]
- 7.Braun RP, Skaria AM, Saurat JH, Borradori L. Multiple hyperkeratotic spicules and myeloma. Dermatology. 2002;205((2)):210–2. doi: 10.1159/000063918. [DOI] [PubMed] [Google Scholar]
- 8.Franck N, Barete S, Moguelet P, Blanchet B, Carlotti A, Ropert S, et al. Spiny follicular hyperkeratosis eruption: a new cutaneous adverse effect of sorafenib. J Clin Oncol. 2010 Nov;28((31)):e640–2. doi: 10.1200/JCO.2010.31.3783. [DOI] [PubMed] [Google Scholar]
- 9.Yanik ME, Erfan G, Albayrak H, Tasolar K, Albayrak S, Gelincik I, et al. Acitretin-induced spiny follicular hyperkeratosis. Cutan Ocul Toxicol. 2016;35((2)):165–7. doi: 10.3109/15569527.2015.1072545. [DOI] [PubMed] [Google Scholar]
- 10.Maddy AJ, Lee EE, Maderal AD, Wang RC, Tosti A, Cho-Vega JH. A case of disseminated follicular spicules in HIV-associated follicular syndrome in the absence of the seven known human polyomaviruses, suggesting that this disorder is distinct from trichodysplasia spinulosa. Br J Dermatol. 2018 Sep;179((3)):774–5. doi: 10.1111/bjd.16562. [DOI] [PubMed] [Google Scholar]
- 11.Izakovic J, Büchner SA, Düggelin M, Guggenheim R, Itin PH. [Hair-like hyperkeratoses in patients with kidney transplants. A new cyclosporin side-effect] Hautarzt. 1995 Dec;46((12)):841–6. doi: 10.1007/s001050050350. [DOI] [PubMed] [Google Scholar]
- 12.Lukitsch O, Gebhardt KP, Kövary PM. Follicular hyperkeratosis and cryocrystalglobulinemia syndrome. Occurrence in a patient with multiple myeloma. Arch Dermatol. 1985 Jun;121((6)):795–8. [PubMed] [Google Scholar]
- 13.Kuokkanen K, Niemi KM, Reunala T. Parakeratotic horns in a patient with myeloma. J Cutan Pathol. 1987 Feb;14((1)):54–8. doi: 10.1111/j.1600-0560.1987.tb00127.x. [DOI] [PubMed] [Google Scholar]
- 14.Bork K, Böckers M, Pfeifle J. Pathogenesis of paraneoplastic follicular hyperkeratotic spicules in multiple myeloma. Follicular and epidermal accumulation of IgG dysprotein and cryoglobulin. Arch Dermatol. 1990 Apr;126((4)):509–13. [PubMed] [Google Scholar]
- 15.Paul C, Fermand JP, Flageul B, Caux F, Duterque M, Dubertret L, et al. Hyperkeratotic spicules and monoclonal gammopathy. J Am Acad Dermatol. 1995 Aug;33((2 Pt 2)):346–51. doi: 10.1016/0190-9622(95)91431-5. [DOI] [PubMed] [Google Scholar]
- 16.Miller JJ, Anderson BE, Ioffreda MD, Bongiovanni MB, Fogelberg AC. Hair casts and cutaneous spicules in multiple myeloma. Arch Dermatol. 2006 Dec;142((12)):1665–6. doi: 10.1001/archderm.142.12.1665. [DOI] [PubMed] [Google Scholar]
- 17.Tay LK, Lim FL, Ng HJ, Lee HY, Pang SM, Thirumoorthy T. Cutaneous follicular hyperkeratotic spicules—the first clinical sign of multiple myeloma progression or relapse. Int J Dermatol. 2010 Aug;49((8)):934–6. doi: 10.1111/j.1365-4632.2009.04369.x. [DOI] [PubMed] [Google Scholar]
- 18.Dalal A, David M, Feinmesser M, Trattner A. Multiple myeloma unveiled by multiple hyperkeratotic spicules. Isr Med Assoc J. 2010 Nov;12((11)):709–10. [PubMed] [Google Scholar]
- 19.van Boheemen S, Jones T, Muhlemann B, Feltkamp MC, Fouchier RA, Hajdarbegovic E. Cidofovir gel as treatment of follicular spicules in multiple myeloma. JAMA Dermatol. 2015 Jan;151((1)):82–4. doi: 10.1001/jamadermatol.2014.1616. [DOI] [PubMed] [Google Scholar]
- 20.Fariña MC, Requena L, Sarasa JL, Martín L, Escalonilla P, Soriano ML, et al. Spinulosis of the face as a manifestation of demodicidosis. Br J Dermatol. 1998 May;138((5)):901–3. doi: 10.1046/j.1365-2133.1998.02234.x. [DOI] [PubMed] [Google Scholar]
- 21.Chia HY, Tey HL, Lee JS. Follicular spicules associated with Propionibacterium acnes in response to erythromycin. J Dermatol. 2011 Apr;38((4)):409–11. doi: 10.1111/j.1346-8138.2010.00979.x. [DOI] [PubMed] [Google Scholar]
- 22.Nemeth K, Gorog A, Mezey E, Pinter D, Kuroli E, Harsing J, et al. Image Correspondence: Cover Image: Detection of hair follicleassociated Merkel cell polyomavirus in an immunocompromised host with follicular spicules and alopecia. Br J Dermatol. 2016 Dec;175((6)):1409. doi: 10.1111/bjd.15039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ruiz-Rivero J, Campos Domíngez M, Parra Blanco V, Suárez-Fernández R. Filiform follicular hyperkeratosis on the face. Actas Dermosifiliogr. 2017 Oct;108((8)):773–4. doi: 10.1016/j.ad.2016.02.025. [DOI] [PubMed] [Google Scholar]
- 24.Friedman SJ. Lichen spinulosus. Clinicopathologic review of thirty-five cases. J Am Acad Dermatol. 1990 Feb;22((2 Pt 1)):261–4. [PubMed] [Google Scholar]
- 25.Kazem S, van der Meijden E, Feltkamp MC. The trichodysplasia spinulosa-associated polyomavirus: virological background and clinical implications. APMIS. 2013 Aug;121((8)):770–82. doi: 10.1111/apm.12092. [DOI] [PubMed] [Google Scholar]
- 26.Al-Niaimi F, Cox NH, Taylor WD. Follicular hyperkeratosis as a manifestation of Sézary syndrome. Br J Dermatol. 2010 Mar;162((3)):695–6. doi: 10.1111/j.1365-2133.2009.09599.x. [DOI] [PubMed] [Google Scholar]
- 27.Tomasini C, Kempf W, Novelli M, Fava P, Annessi G, Rongioletti F, et al. Spiky follicular mycosis fungoides: a clinicopathologic study of 8 cases. J Cutan Pathol. 2015 Mar;42((3)):164–72. doi: 10.1111/cup.12399. [DOI] [PubMed] [Google Scholar]