Abstract
Squamous cell carcinoma (SCC) is the second most common skin cancer worldwide, and exposure to ultraviolet (UV) light is a major cause of SCC. UV nail lamps can be used for drying and hardening acrylic or gel nail polish. We report a case of a 52-year-old Caucasian woman with an 18-year history of UV nail lamp use every 3 weeks and an 18-year history of weekly tanning bed use who presented with over 25 actinic keratoses and two SCC in situ on her dorsal hands. Of note, this patient has never had any previous biopsies, skin cancer or precancers, or skin cancer or precancer treatment at any time in the past and on skin examination had no precancers or cancers elsewhere on her body. We also review the existing research regarding nail lamp use, which overall suggests that the risk of carcinogenesis is low, and discuss ways dermatologists can educate patients regarding proper UV nail lamp use to minimize risks. This patient's extensive UV nail lamp use coupled with UVA exposure from tanning beds may have put her at particular risk and exacerbated the effects of the nail lamp alone.
Keywords: Squamous cell carcinoma, Actinic keratoses, Skin cancer risk factors, UV nail lamps
Introduction
Squamous cell carcinoma (SCC) is the second most common skin cancer worldwide [1]. Exposure to ultraviolet (UV) light is a major cause of SCC [1, 2, 3]. One source of UV light that has undergone increased investigation over the past decade is UV nail lamps. UV nail lamps are necessary for “curing,” or drying and hardening, acrylic or gel nail polish [4]. There are two forms of UV nail lamps. The original form uses fluorescent tubes as bulbs, and the newer form uses light-emitting diode (LED) bulbs [4]. Both bulbs emit UVA wavelengths that can cure artificial nails [4, 5], but LED style lamps require less time since they emit higher-intensity wavelengths [4]. The amount of time clients spend under UV light varies based on the number, type, and intensity of bulbs in the lamp, but on average the typical exposure time is 6–10 min under lamps with repeated treatments at most every 2 weeks [6].
Although limited, the research regarding UV nail lamp use suggests that the risk of carcinogenesis from UV nail lamps is low. However, the topic remains controversial, and a potential subject for both provider and patient education. We present a case of multiple actinic keratoses (AKs) and SCCs in situ on the dorsal hands of a patient with an extensive history of UV nail lamp use.
Case Presentation
A 52-year-old female was referred to dermatology for multiple scaly, erythematous papules that had been present on her hands for 1 year. Her primary care physician treated her lesions unsuccessfully with cryotherapy. No other treatment was attempted. She denied any personal or family history of skin cancer. Apart from the current lesions on her hands, she denied any previous biopsies, precancers or skin cancers, and any cryotherapy or precancer treatment at any time.
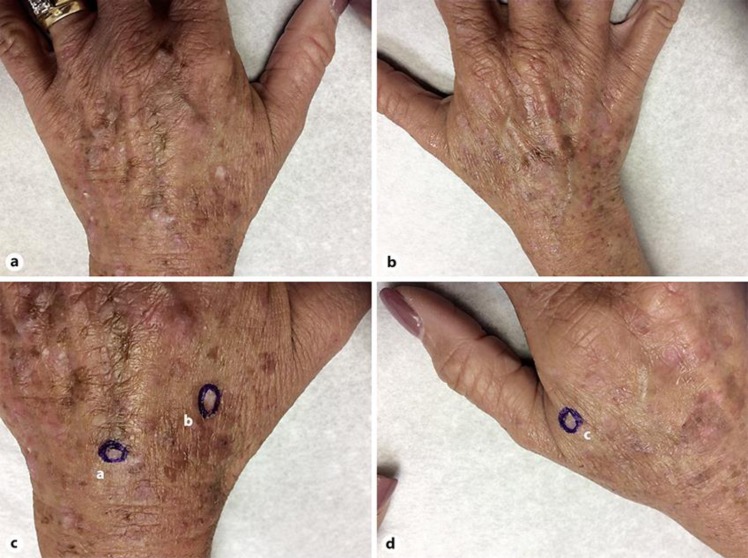
On examination, the patient was Fitzpatrick skin type II with tan skin. Examination of her dorsal hands revealed a bilateral distribution of multiple red-brown, irregular, hypertrophic erythematous papules and patches with hyperkeratotic scale consistent with AKs (Fig. 1, 2). Tangential shave biopsies were performed on three hyperkeratotic scaly papules involving her right radial dorsal hand and left ulnar and radial dorsal hands. Biopsy revealed SCC in situ of her left ulnar dorsal hand and right radial dorsal hand, and an AK of her left radial dorsal hand. In total, there were over 25 AKs on her dorsal hands treated with cryotherapy and no evidence of AKs or SCC on the rest of her total body skin examination.
Fig. 1.
a Left dorsal hand at the initial visit with diffuse AKs and solar damage. b Right dorsal hand at the initial visit with diffuse AKs and solar damage. c Left dorsal hand biopsy sites. Site “a” was a SCC in situ, and “b” was an AK. d Right dorsal hand biopsy sites. Site “c” was a SCC in situ.
Fig. 2.
Bilateral dorsal hands 7 days after cryotherapy treatment for over 25 AKs. Blistering and crusted lesions indicate the AK locations.
The patient had an indoor occupation and denied a history of outdoor gardening or outdoor recreational activities, exposure to chemicals or irritants to her hands, radiation treatment, or immunosuppression. The patient admitted to an 18-year history of once-a-week indoor tanning with cessation 2 years ago. Further questioning revealed the patient had an 18-year history of UV nail lamp use every 3 weeks at a nail salon. Fifteen of these years was with fluorescent bulbs, and 3 years was with LED bulbs.
Discussion
Given the anecdotal nature of this case and significant tanning bed history, we cannot claim the skin findings were the direct result of UV nail lamps. However, her unique presentation of such a significant number of AKs and multiple SCCs in situ restricted to her dorsal hands and none on the rest of her body does raise concern that her extensive UV nail lamp history may have been a contributing factor in the development of the solar damage to her hands, its effects possibly exacerbated by her previous tanning history given the known carcinogenic effects of tanning beds [7]. This presentation is also more unique given that the dorsa of the hands are considered the most UV-resistant location of the body due to photoadaptations [8]. This case prompts a discussion of the existing research regarding UV nail lamp use and ways to minimize any existing cancer risk.
Initial concern regarding UV exposure from UV nail lamps stemmed from a 2009 case report describing the development of SCC in situ on the dorsal hands of a woman with a 15-year history and SCCs on the dorsal hands of a woman with a 1-year history of UV nail lamp use [9]. Although this case received criticism due to flawed claims in its comparison of tanning bed UV emittance to that of nail lamps [6], a series of research studies were conducted to assess the safety of UV nail lamps.
The first study by Schoon et al. [6] compared the UV output from nail lamps to that of natural sunlight and concluded the UV output from the lamps is equal to an additional 1.5–2.7 min outside each day between bimonthly salon visits. A mathematical model based on age and UV exposure created by Diffey [10] indicated tens to hundreds of thousands of women would have to routinely use the lamps before a SCC developed directly from UV nail lamp usage. Both studies concluded the carcinogenesis risk is low.
Markova and Weinstock [11] compared UV nail lamps to narrowband UVB, a standard type of phototherapy that is accepted as low risk for cancer. They found that over 250 years of weekly UV nail lamp use is required to match the carcinogenic equivalence from a single narrowband UVB course. Dowdy and Sayre [12] conducted an evaluation of six types of nail lamps and concluded that for UV nail lamps, a daily occupational exposure limit of 30–130 min is acceptable, which is several times longer than salon use.
In contrast, Curtis et al. [13] found that a single 10-min session of UV nail lamp use exposes clients to an energy dose that matches the exposure limit for outdoor workers in a single day [13]. This study faced controversy from other authors who claimed it used inappropriate measurement techniques [14]. Lastly, Shipp et al. [15] studied the energy density from 17 UV nail lamps and found that to reach the UVA light threshold that causes DNA damage in keratinocytes and potential carcinogenesis, a median number of 11.8 visits with UV nail lamp, or 35.3 months with a frequency of one visit per 3 months, is needed.
While a conclusion regarding the safety of UV nail lamps cannot be drawn from this case alone, the association between the sun damage on the patient's dorsal hands and the UV nail lamps does raise considerations for patient education regarding UV nail lamp use. First, while some of the research regarding UV nail lamps is controversial, most authors agree the risk for skin cancer from the lamps is low and can be minimized by using fingerless manicure gloves as well as use of sunscreen 30 min prior to manicures [5, 6, 10, 15].
It is unknown how many nail salons have sunscreen or manicure gloves available or how many dermatologists are aware such gloves exist for patients. A 2018 survey found that only 3% of the respondents use sunscreen prior to manicures and only 2 respondents were told at nail salons to use sunscreen [16]. Dermatologists and nail salons need to be aware of the potential use of gloves and sunscreen and should advise patients or clients of such measures to ensure the safety of UV nail lamp use. This aspect of patient education is especially important in individuals with increased risk for skin cancer, such as fair skinned individuals, immunosuppressed patients, or those with a family history of skin cancer. Secondly, these preventative measures and patient education regarding nail lamps are also important for patients with photosensitivity disorders, since not all patients may know the lamps have UV light output.
Lastly, UV nail lamps are not limited to nail salons but can also be purchased for use at home. In their analysis of the safety of UV nail lamps, Dowdy et al. [12] claimed the most dangerous aspect of the lamps is the risk for accidental use of more potent UVB bulbs in the lamps, which would increase the risk of injury from the devices [17]. In addition, there is a lack of regulation regarding nail lamps, and a multitude of models with various lamp strengths, number of bulbs, and required exposure times exist [18]. This, coupled with findings from the Shipp et al. study [15] that the number of visits needed to reach the DNA damage threshold varied based on the type of lamp ranging from 8 to 208 visits, is www.concerning.In order to prevent improper use of UV nail lamps, this should be a topic of education between dermatologists and patients who use them.
In conclusion, while existing research suggests a low risk of carcinogenesis resulting from UV nail lamp use, ways to minimize any risks should be kept in mind. Although this case is anecdotal in nature, it does raise the question if significant UV nail lamp use can contribute to skin cancer development. In the case of this patient, the additive effect of a UV nail lamp for hardening, along with her prior UVA exposure from tanning bed use, may have put her at particular risk and exacerbated the effects of the nail lamp alone. Regardless, dermatologists should be aware of the effect of such risk factors and advise patients who regularly use nail lamps regarding the use of sunscreen and manicure gloves, especially in patients with a tanning bed history as well. Moreover, patients should be warned that improper use of home UV nail lamps could result in increased risks.
Statement of Ethics
Informed consent was obtained from this patient to publish this case (including the images). The research for this case report was conducted ethically and complied with the World Medical Association Declaration of Helsinki.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
This article received no funding.
Author Contributions
All authors made significant contributions towards writing and revising the manuscript and all are authors have approved the final version of the submitted manuscript.
References
- 1.Skin Cancer Foundation [Internet] Squamous Cell Carcinoma. Skin Cancer Foundation Skin Cancer Information. 2019 [cited 2019 July 10]. Available from: https://www.skincancer.org/skin-cancer-information/squamous-cell-carcinoma. [Google Scholar]
- 2.Cadet J, Douki T. Formation of UV-induced DNA damage contributing to skin cancer development. Photochem Photobiol Sci. 2018 Dec;17((12)):1816–41. doi: 10.1039/c7pp00395a. [DOI] [PubMed] [Google Scholar]
- 3.Rünger TM, Farahvash B, Hatvani Z, Rees A. Comparison of DNA damage responses following equimutagenic doses of UVA and UVB: a less effective cell cycle arrest with UVA may render UVA-induced pyrimidine dimers more mutagenic than UVB-induced ones. Photochem Photobiol Sci. 2012 Jan;11((1)):207–15. doi: 10.1039/c1pp05232b. [DOI] [PubMed] [Google Scholar]
- 4.Schoon Scientific Understanding UV Nail Lamps [Internet] Professional Beauty Association and Nail Manufacturers Council on Safety. 2012 [cited on 2019 July 10]. Available from: http://www.schoonscientific.com/resource/understanding-uv-nail-lamps/ [Google Scholar]
- 5.Skin Cancer Foundation [Internet] The Skin Cancer Foundation's Official Position on UV Light and Manicure Safety. 2015 Press Releases. 2015 [cited 2019 July 10]. Available from: https://www.skincancer.org/media-and-press/press-release-2015/nail-lamps. [Google Scholar]
- 6.Schoon D, Bryson P, McConnell J. Do UV nail lamps emit unsafe levels of ultraviolet light? [Internet] Schoon Scientific. 2010 [cited 2019 July 10]. Available from: http://www.schoonscientific.com/downloads/UV-Nail-Lamp-Facts.pdf. [Google Scholar]
- 7.International Agency for Research on Cancer Working Group on artificial ultraviolet (UV) light and skin cancer The association of use of sunbeds with cutaneous malignant melanoma and other skin cancers: A systematic review. Int J Cancer. 2007 Mar;120((5)):1116–22. doi: 10.1002/ijc.22453. [DOI] [PubMed] [Google Scholar]
- 8.Olson RL, Sayre RM, Everett MA. Effect of anatomic location and time on ultraviolet erythema. Arch Dermatol. 1966 Feb;93((2)):211–5. [PubMed] [Google Scholar]
- 9.MacFarlane DF, Alonso CA. Occurrence of nonmelanoma skin cancers on the hands after UV nail light exposure. Arch Dermatol. 2009 Apr;145((4)):447–9. doi: 10.1001/archdermatol.2008.622. [DOI] [PubMed] [Google Scholar]
- 10.Diffey BL. The risk of squamous cell carcinoma in women from exposure to UVA lamps used in cosmetic nail treatment. Br J Dermatol. 2012 Nov;167((5)):1175–8. doi: 10.1111/j.1365-2133.2012.11107.x. [DOI] [PubMed] [Google Scholar]
- 11.Markova A, Weinstock MA. Risk of skin cancer associated with the use of UV nail lamp. J Invest Dermatol. 2013 Apr;133((4)):1097–9. doi: 10.1038/jid.2012.440. [DOI] [PubMed] [Google Scholar]
- 12.Dowdy JC, Sayre RM. Photobiological safety evaluation of UV nail lamps. Photochem Photobiol. 2013 Jul-Aug;89((4)):961–7. doi: 10.1111/php.12075. [DOI] [PubMed] [Google Scholar]
- 13.Curtis J, Tanner P, Judd C, Childs B, Hull C, Leachman S. Acrylic nail curing UV lamps: high-intensity exposure warrants further research of skin cancer risk. J Am Acad Dermatol. 2013 Dec;69((6)):1069–70. doi: 10.1016/j.jaad.2013.08.032. [DOI] [PubMed] [Google Scholar]
- 14.Dowdy JC, Sayre RM. Nail curing UV lamps: trivial exposure not cause for public alarm. J Am Acad Dermatol. 2015 Nov;73((5)):e185–6. doi: 10.1016/j.jaad.2015.06.064. [DOI] [PubMed] [Google Scholar]
- 15.Shipp LR, Warner CA, Rueggeberg FA, Davis LS. Further investigation into the risk of skin cancer associated with the use of UV nail lamps. JAMA Dermatol. 2014 Jul;150((7)):775–6. doi: 10.1001/jamadermatol.2013.8740. [DOI] [PubMed] [Google Scholar]
- 16.Bollard SM, Beecher SM, Moriarty N, Kelly JL, Regan PJ, Potter SM. Skin cancer risk and the use of UV nail lamps. Australas J Dermatol. 2018 Nov;59((4)):348–9. doi: 10.1111/ajd.12806. [DOI] [PubMed] [Google Scholar]
- 17.de Gruijl FR. Photocarcinogenesis: UVA vs. UVB radiation. Skin Pharmacol Appl Skin Physiol. 2002 Sep-Oct;15((5)):316–20. doi: 10.1159/000064535. [DOI] [PubMed] [Google Scholar]
- 18.Wang JV, Korta DZ, Zachary CB. Gel manicures and ultraviolet A light: A call for patient education. Dermatol Online J. 2018 Mar;24((3)):13030/qt5hx4g5v4. [PubMed] [Google Scholar]