Abstract
Intraplacental choriocarcinoma is a rare type of gestational choriocarcinoma occurring in the placenta, of which only a small number of cases have been reported. Gestational choriocarcinoma rapidly metastasizes to organs such as the lung, brain, and liver; thus, early diagnosis and treatment are essential. In addition, intraplacental choriocarcinoma can affect fetal mortality. We present a case of a 33-year-old woman diagnosed with intraplacental choriocarcinoma based on placental biopsy performed after the pregnancy had reached term. The patient had pulmonary metastasis at the time of diagnosis, but after the combination chemotherapy with EMA-EP, complete remission is maintained.
Keywords: Gestational choriocarcinoma, Intraplacental, Metastasis, Term pregnancy, Live birth
Introduction
Gestational trophoblastic neoplasia (GTN) is a group of malignant tumors characterized by abnormal growth of trophoblastic tissue, which can occur after a molar or non-molar pregnancy. Gestational choriocarcinoma is a histologic subtype of GTN, and the one which presents the most aggressive evolution. After a non-molar pregnancy, the incidence of gestational choriocarcinoma is approximately 5–200 per 100,000 pregnancies in Southeast Asia and Japan. GTN is a highly malignant tumor, which shows rapid metastasis to organs like the lung, the vagina, the brain, or the liver. However, since this type of tumor shows a high cure rate, early diagnosis and subsequent treatment are important. Intraplacental choriocarcinoma is a rare type of tumor in which gestational choriocarcinoma is found in the placenta. As only a small number of cases have been reported to date, the effects of intraplacental choriocarcinoma on maternal mortality and perinatal progression are not well known. Here, we present a case of a 33-year-old woman with metastatic intraplacental choriocarcinoma, diagnosed one week after delivery via cesarean section and treated successfully.
Case Report
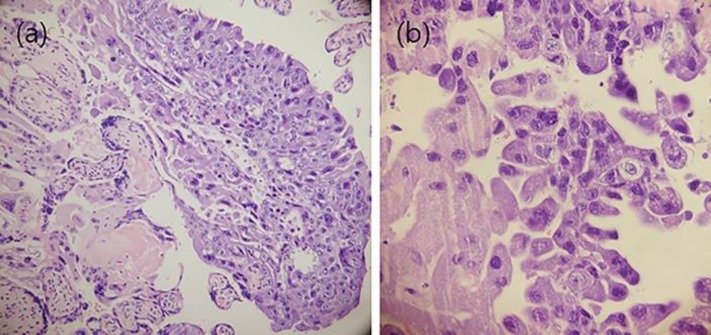
A 33-year-old primipara woman presented to the local clinic with a chief complaint of scanty bloody discharge in the 39th (38 + 6) weeks of gestation. The patient reported that fetal movements had decreased the day before. In the clinic, no abnormality in antenatal care had been reported up to two weeks before the visit. However, on the day, ultrasonography showed fetal ascites and hydrops with oligohydramnios. Fetal monitoring revealed late deceleration. Vaginal examination showed a closed cervix with spotting; leakage of amniotic fluid was not observed. The patient was transferred to the hospital and immediately delivered a male fetus weighing 3,210 g, via cesarean section. Apgar score was 1 and 5 at the 1st and 5th min after delivery, respectively. The newborn presented pallor and had a hemoglobin concentration of 3.5 g/dL. Upon further tests, he was diagnosed with fetomaternal transfusion. At the time of surgery, placental tissue was sent to the pathology department for histologic examination. The patient had no postoperative complications. Overall, the placenta weighted 370 g and measured 20.5 × 2.3 cm. The umbilical cord measured 18.0 cm. The cord color was grayish white and showed edema. The fetal side and maternal side of the placenta was unremarkable. Microscopic examination revealed gestational choriocarcinoma with decidual invasion in the mature placenta (Fig. 1). Other pathologic findings included the presence of chorioamnionitis and thrombosis.
Fig. 1.
(a) Intraplacental choriocarcinoma; (b) with arrangement of two populations of trophoblast.
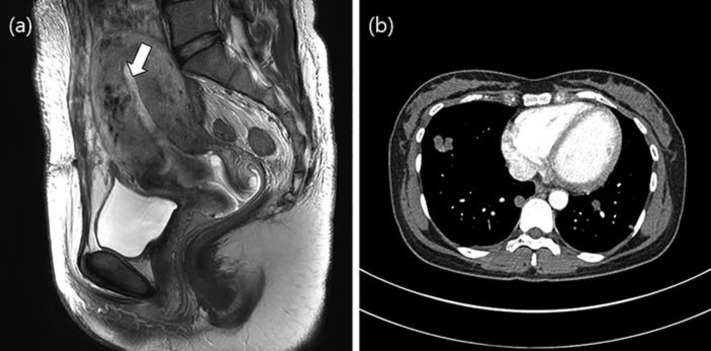
After intraplacental choriocarcinoma was diagnosed, serum beta-human chorionic gonadotropin (bHCG) level was measured as part of the initial diagnosis. bHCG levels on day 9 postpartum were 77,417 mIU/mL and increased to 200,821 mIU/mL on day 18. Abdomen computed tomography (CT) showed an abnormal, low-density endometrial expansile mass, with invasion to the anterior myometrium and engorged vascular structures in the anterior wall, suggesting invasive choriocarcinoma. Chest CT showed multiple round nodules and masses of variable sizes in both lungs, with scanty amounts of right pleural effusion, compatible with lung metastasis (Fig. 2). The patient was finally diagnosed with International Federation of Gynecology and Obstetrics (FIGO) stage III gestational intraplacental choriocarcinoma, with a World Health Organization (WHO) risk score of 7.
Fig. 2.
(a) Contrast enhanced T2-weighted sagittal image shows endometrial expansile mass with invasion to the anterior myometrium and engorged vascular structures in the anterior wall, suggesting invasive choriocarcinoma; (b) lung metastasis.
On day 19 postpartum, the patient began chemotherapy with the EMA-EP regimen (etoposide, methotrexate, and actinomycin D, alternating with etoposide and cisplatin). bHCG levels gradually decreased with each cycle of chemotherapy. However, during the sixth cycle of chemotherapy, treatment was discontinued as an elevation of serum liver enzyme was observed. At that point, bHCG levels had decreased to 1.7 mIU/mL and the size of the pulmonary metastases had decreased. The patient is presently closely observed on an outpatient basis, without receiving further treatment. Moreover, complete remission has been maintained for one year.
Discussion/Conclusion
Intraplacental choriocarcinoma is generally diagnosed during the postpartum examination of the placenta, or during evaluation based on disease-related symptoms. As examination of the placenta is not performed routinely, a lack of symptoms can make it difficult to detect intraplacental choriocarcinoma [1, 2]. Previous reports suggest that intraplacental choriocarcinoma cases amount to approximately 2% of gestational choriocarcinomas [2, 3].
More than 60% of intraplacental choriocarcinoma cases are diagnosed postpartum. Approximately 50% of reported intraplacental choriocarcinoma cases are asymptomatic. In this case, 61% of placental examinations were performed because of fetal status indicators, such as fetomaternal hemorrhage, IUFD, IUGR, and fetal distress [4]. Moreover, 16% of these were performed because of maternal health indicators, such as gestational hypertension and markedly elevated AFP levels in the maternal serum. In 6% of cases, further examinations were conducted owing to abnormalities observed during macroscopic placental examinations [5]. In the case described here, the patient was incidentally diagnosed based on placental examination owing to fetal distress and fetomaternal transfusion.
Metastatic intraplacental choriocarcinoma has been reported in approximately 52% of patients, and metastatic tumors can be found in organs such as the lung, the uterus, the brain, and the vagina. Symptoms of metastases in other organs may be observed depending on the site of the tumor. Pulmonary metastases can cause cough, hemoptysis, or chest pain. In brain metastases, headaches, paresthesia, or seizures may occur [6]. In the present case, the patient had multiple pulmonary metastases but presented no symptoms.
In some cases, infantile metastasis has been reported in relation to mothers with intraplacental choriocarcinoma. Infantile metastasis has also been observed in the liver, lung, brain, and skin [3, 5]. According to a systematic review by Blohm et al., live birth was reported in 38 out of 58 cases (66%), and 20 cases (53%) presented uncomplicated births [6]. In the present case, the baby was born at term but is being treated for fetal hydrops and fetomaternal transfusion.
The systematic review by Blohm et al. also described that, of the 62 cases in which intraplacental choriocarcinoma was diagnosed during histopathological placental examination, 18 cases (29%) were macroscopically normal, 34 (55%) presented a single lesion, and 6 cases (10%) presented multiple lesions. In these cases, placentas presented infarcts or thrombi with a median diameter of 2 cm (ranging 1–6 cm) [5, 6, 7, 8].
As cases of intraplacental choriocarcinoma are rare, there is currently no established treatment. In cases with no metastasis, bHCG surveillance is generally sufficient and most tumors are spontaneously normalized [6]. In one case, natural progression with pulmonary metastasis was observed 9 months after diagnosis. However, the patient reached complete remission after chemotherapy with the multi-drug EMA-CO (etoposide, methotrexate, actinomycin D, cyclophosphamide, vincristine) regimen [9]. In metastatic cases, as in all cases of metastatic choriocarcinoma, chemotherapy with a multi-drug regimen such as EMA-CO shows 100% long-term remission [6, 10]. In our case, the patient was also treated with a multi-drug regimen due to pulmonary metastasis, and has been in complete remission for approximately 1 year.
Intraplacental choriocarcinoma, a rare condition, should be diagnosed with placental examination when accompanied by the mentioned clinical features and can be cured.
Statement of Ethics
The patient gave written informed consent to report this case including the images.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
None.
Author Contributions
Conceptualization: Hyunjin Cho.
Writing – original draft preparation: Eunhyun Lee.
Writing – review and editing: Hyunjin Cho.
Approval of final manuscript: all authors.
References
- 1.Caldas RF, Oliveira P, Rodrigues C, Reis I, Scigliano H, Nogueira R, et al. Intraplacental Choriocarcinoma: Rare or Underdiagnosed? Report of 2 Cases Diagnosed after an Incomplete Miscarriage and a Preterm Spontaneous Vaginal Delivery. Case Rep Med. 2017;2017:7892980. doi: 10.1155/2017/7892980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lele SM, Crowder SE, Grafe MR. Asymptomatic intraplacental choriocarcinoma diagnosed on routine placental examination. Journal of perinatology: official journal of the California Perinatal Association. 1999;19((3)):244–7. doi: 10.1038/sj.jp.7200140. [DOI] [PubMed] [Google Scholar]
- 3.Liu J, Guo L. Intraplacental choriocarcinoma in a term placenta with both maternal and infantile metastases: a case report and review of the literature. Gynecol Oncol. 2006 Dec;103((3)):1147–51. doi: 10.1016/j.ygyno.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 4.She Q, Cheng Z, El-Chaar D, Luo F, Guo X, Wen SW. Intraplacental choriocarcinoma coexisting with fetomaternal hemorrhage: case report, chemotherapy management, and literature review. Medicine (Baltimore) 2018 Apr;97((14)):e9977. doi: 10.1097/MD.0000000000009977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jiao L, Ghorani E, Sebire NJ, Seckl MJ. Intraplacental choriocarcinoma: systematic review and management guidance. Gynecol Oncol. 2016 Jun;141((3)):624–31. doi: 10.1016/j.ygyno.2016.03.026. [DOI] [PubMed] [Google Scholar]
- 6.Blohm ME, Göbel U. Unexplained anaemia and failure to thrive as initial symptoms of infantile choriocarcinoma: a review. Eur J Pediatr. 2004 Jan;163((1)):1–6. doi: 10.1007/s00431-003-1361-1. [DOI] [PubMed] [Google Scholar]
- 7.Lage JM, Roberts DJ. Choriocarcinoma in a term placenta: pathologic diagnosis of tumor in an asymptomatic patient with metastatic disease. International journal of gynecological pathology: official journal of the International Society of Gynecological Pathologists. 1993;12((1)):80–5. [PubMed] [Google Scholar]
- 8.Kanehira K, Starostik P, Kasznica J, Khoury T. Primary intraplacental gestational choriocarcinoma: histologic and genetic analyses. Int J Gynecol Pathol. 2013 Jan;32((1)):71–5. doi: 10.1097/PGP.0b013e3182566552. [DOI] [PubMed] [Google Scholar]
- 9.Landau D, Maor E, Maymon E, Rabinovich A, Piura B. Intraplacental choriocarcinoma metastasizing to the maternal lung. Eur J Gynaecol Oncol. 2006;27((1)):29–32. [PubMed] [Google Scholar]
- 10.Seckl MJ, Sebire NJ, Fisher RA, Golfier F, Massuger L, Sessa C, et al. Gestational trophoblastic disease: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Annals of Oncology. 2013;24((suppl_6)):vi39–vi50. doi: 10.1093/annonc/mdt345. [DOI] [PubMed] [Google Scholar]