Abstract
Background
Subacute thyroiditis is generally believed to be induced by viral infection, and little attention has been paid to anti-thyroid antibodies.
Objectives
Our study aimed to assess the prevalence of anti-thyroid antibodies in patients with subacute thyroiditis.
Methods
Anti-thyroglobulin (TgAb) and anti-thyroid peroxidase antibodies (TPOAb) were measured with 4 different immunoassay kits currently used in 40 patients in the early phase of subacute thyroiditis.
Results
The proportion of samples positive for TgAb was 52.5 ± 13.7% (mean of 4 kits), which was significantly (p < 0.05) higher than that positive for TPOAb (15.6 ± 6.5%). The prevalence of positive TgAb alone (negative TPOAb) was also significantly higher than that of TPOAb alone (negative TgAb). TgAb titers decreased or disappeared within 4 months to 6 years in 6 patients.
Conclusions
Patient samples were moderately positive for TgAb initially, but the titer decreased or disappeared afterwards in subacute thyroiditis.
Keywords: Anti-thyroglobulin antibodies, Subacute thyroiditis, Autoimmune thyroiditis, Anti-TPO antibodies
Introduction
Subacute thyroiditis, also referred to as granulomatous or De Quervain's thyroiditis, is a spontaneously remitting, inflammatory disorder of the thyroid gland [1, 2, 3]. Patients usually present with tenderness and enlargement of the thyroid gland, and initially show destruction-induced thyrotoxicosis, which is often followed by transient hypothyroidism [1, 2, 3]. The disease is self-limiting and often does not require treatment. In some cases, short-term steroid therapy is effective [4]. Subacute thyroiditis is thought to be caused by a viral infection or a postviral inflammatory process [5], and a minimal role of autoimmunity has been suggested [6, 7]. Therefore, data on anti-thyroid antibodies in subacute thyroiditis are limited. In some reviews or textbooks, circulating thyroid antibodies have been described to be absent or have low titers [2, 3].
For the detection of antibodies, the tanned red cell hemagglutination method was initially applied in the 1980s, and positivity for thyroglobulin (Tg) hemagglutination antibodies and microsomal antibodies was tested [8]. However, the method was not sensitive enough to detect low levels of anti-thyroid antibodies. Therefore, earlier negative reports using Tg and/or microsomal hemagglutination antibodies cannot deny the possible presence of low titers of circulating anti-thyroid antibodies in subacute thyroiditis. More recently, further sensitive automated immunoassays have been introduced for the detection of both antibodies [9]. Because subacute thyroiditis is encountered less frequently than Hashimoto's thyroiditis or Graves' disease, the number of patients reported with this condition is too small to clarify the frequency of circulating anti-thyroid antibodies [10, 11, 12]. Painful Hashimoto's thyroiditis shows clinical features similar to those of subacute thyroiditis in the presence of anti-thyroid antibodies, and their differential diagnosis is critical [13]. Therefore, in this study, we applied 4 sensitive immunoassays currently used to clarify the frequency of circulating anti-thyroid antibodies in 40 patients with subacute thyroiditis.
Subjects and Methods
Subjects
We examined 40 untreated patients with subacute thyroiditis (mean age ± SD, 47.9 ± 12.9 years; 33 females and 7 males) and 100 healthy subjects (41.5 ± 11.9 years; 69 females and 31 males). With regard to “patient controls,” 70 untreated patients with Hashimoto's thyroiditis (a hypothyroid or euthyroid status) (45.4 ± 18.3 years; 65 females and 5 males) were also examined. These patients were consecutive outpatients at the Kuma Hospital between September 2011 and March 2012. As reported previously [1], the disease was diagnosed according to the diagnostic guidelines of the Japan Thyroid Association [14]. Early-phase subacute thyroiditis was diagnosed based on clinical findings of a painful swelling and tenderness in the thyroid gland, laboratory findings of elevated C-reactive protein and serum free thyroxine (FT4) and decreased levels of serum thyroid-stimulating hormone (TSH), and a hypoechoic lesion at the painful site of the thyroid gland confirmed by ultrasonography. Painful Hashimoto's thyroiditis was excluded following the previously reported criteria [15, 16]. Diagnosis of Hashimoto's thyroiditis was made as previously reported [9]. Healthy control subjects were euthyroid without goiter and over the age of 20 years with no previous personal history of a thyroid disease.
Autoantibodies
TgAb and TPOAb were measured with 4 different kits using automated instruments as follows: kit A, ECLusys (Roche Diagnostics, Mannheim, Germany); kit B, Architect I 2000 SR (Abbott Diagnostics, IL, USA); kit C, AIA (Tosoh Bioscience, Tokyo, Japan); and kit D, Lumipulse Presto II (Fujirebio Inc, Tokyo, Japan). Assay characteristics provided by the manufacturer have been reported precisely [9]. All assays were performed using reagents provided by the manufacturers according to the instruction in the package insert, and each cutoff is shown in Table 1. All TgAb assays have been calibrated against the WHO First International Reference Preparation 66/387. All TPOAb assays have been calibrated against the WHO First International Reference Preparation 65/93. Native Tg and recombinant human TPO were used in all assay systems for the detection of TgAb and TPOAb, respectively.
Table 1.
Prevalence of thyroglobulin antibodies (TgAb) and thyroid peroxidase antibodies (TPOAb) in patients with subacute thyroiditis and healthy controls measured using 4 different kits
| Kit A |
Kit B |
Kit C |
Kit D |
|||||
|---|---|---|---|---|---|---|---|---|
| TgAb [28] | TPOAb [16] | TgAb [4.1] | TPOAb [5.6] | TgAb [13.6] | TPOAb [3.2] | TgAb [12.2] | TPOAb [5.1] | |
| Subacute thyroiditis | 37.5 | 25.0 | 60.0a | 12.5 | 45.0a | 10.0 | 67.5a | 15.0 |
| (n=40) | (25.0) | (12.5) | (50.0a) | (2.5) | (40.0a) | (5.0) | (55.0a) | (2.5) |
| Controls | 7.0 | 4.0 | 7.0b | 1.0 | 6.0 | 1.0 | 11.0b | 2.0 |
| (n=100) | (7.0) | (4.0) | (7.0b) | (1.0) | (6.0) | (1.0) | (10.0b) | (1.0) |
Data indicate percent positive reaction. The prevalence of TgAb was significantly different from that of TPOAb at
p < 0.001 and
p < 0.05. The cutoff value for each assay kit is presented in brackets [IU/mL]. The prevalence of a positive reaction for TgAb or TPOAb alone is presented in parentheses.
Statistical Analysis
Comparisons of TgAb and TPOAb prevalence were performed by the χ2 test in different assay kits. Differences in antibody titers between subacute thyroiditis and Hashimoto's thyroiditis were evaluated by Mann-Whitney U test. Differences were considered to be significant at p < 0.05.
Results
We concurrently evaluated the frequency of TgAb and TPOAb in 40 untreated patients with subacute thyroiditis using 4 different kits. As shown in Table 1, TgAb positivity ranged from 37.5 to 67.5%, and kit D detected TgAb positivity more frequently. The frequency of positive titers for TgAb was significantly higher than that of positive titers for TPOAb in kits B, C, and D, and a high tendency was also shown in kit A. As a whole, the prevalence of TgAb was 52.5 ± 13.7% (mean ± SD of 4 kits), and it was significantly (p < 0.05) higher than that of TPOAb (15.6 ± 6.5%) at the onset of subacute thyroiditis. The prevalence of TgAb alone (negative TPOAb) was significantly higher than that of TPOAb alone (negative TgAb) in kits B, C, and D (Table 1).
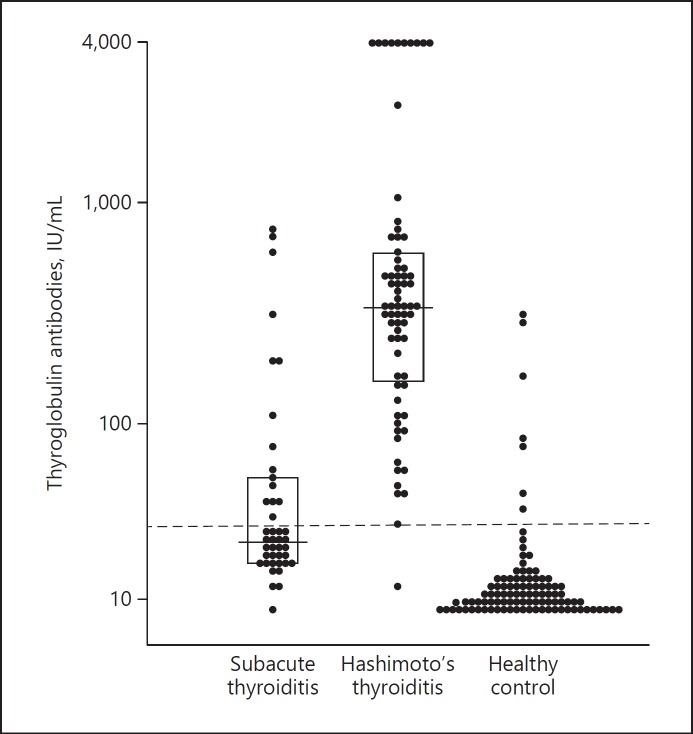
The distribution of individual values of TgAb in kit A is shown in Figure 1. Overall, the titers are significantly lower in subacute thyroiditis than in Hashimoto's thyroiditis (median and interquartile range, 22.3 and 16.7–51.5 vs. 353.2 and 163.1–618.5 IU/mL, respectively; p < 0.001). Even on comparing positive values of TgAb in both disease groups, the difference remained significant (75.4 and 42.1–306.0 vs. 356.8 and 195.3–669.3 IU/mL, respectively; p = 0.002). In 6 patients, follow-up data concerning TgAb-positive titers using kit A were available from 4 months to 6 years after their initial examination. In all 6 patients, TgAb titers decreased or disappeared (Table 2).
Fig. 1.
Individual values of thyroglobulin antibodies measured using kit A in patients with subacute thyroiditis and Hashimoto's thyroiditis and in healthy controls. Dotted line indicates the cutoff value.
Table 2.
Changes in TgAb titers from onset to follow-up in 6 patients with subacute thyroiditis
| Patient | TgAb titer, IU/mL |
Interval period, months | |
|---|---|---|---|
| onset | follow-up | ||
| 1 | 690.3 | 282.3 | 15 |
| 2 | 681.5 | 298.9 | 8 |
| 3 | 216.4 | <28.0 | 4 |
| 4 | 127.0 | <28.0 | 10 |
| 5 | 82.7 | 43.0 | 5 |
| 6 | 45.5 | <28.0 | 72 |
Discussion
Circulating thyroid antibodies have been described to be absent in subacute thyroiditis, or the titer has been reported to be low in some reviews or textbooks [2, 3]. In this study, however, we clarified that TgAb was present rather moderately in the early phase of the disease, although titers were significantly lower than those observed in Hashimoto's thyroiditis. The prevalence of TgAb ranged from 37.5 to 67.5%, and the difference depended on the kits used.
Table 3 summarizes the frequency of anti-thyroid antibodies in subacute thyroiditis from reports published after 1980 [10, 11, 12, 17, 18, 19, 20, 21, 22, 23, 24]. In earlier studies using the hemagglutination method, Tg hemagglutination antibody levels were negative or low, possibly because of the insensitiveness of the assay method. Even while using sensitive assays, positive TgAb results were observed in 0–67% cases. In this study, 52.5% (mean of 4 different kits) of the 40 patients with subacute thyroiditis were positive for TgAb, and the prevalence was higher than that of TPOAb. The higher prevalence of TgAb was also common in Hashimoto's thyroiditis and healthy controls using the same immunoassays [9]. However, the epitopes that TgAb recognizes against several thyroglobulin regions are reported to have different patterns between subacute thyroiditis and Hashimoto's thyroiditis [25], suggesting that TgAb produced in acute thyroid destruction is not similar to that produced in a chronic autoimmune reaction, but represents a nonspecific response to the release of thyroid antigens.
Table 3.
Reported frequency of TgAb and/or TPOAb in subacute thyroiditis in the individuals examined
| First author | Year | n | Positive,% |
Assay method | Antibody follow-up | Ref. | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| TgAb | TPOAb | TGHA | MCHA | |||||||
| Omori | 2008 | 27 | 67 | NT | NT | NT | RIA | decrease in5, increase in2 | 17 | |
| Benbassat | 2007 | 39 | 25a | NT | NT | EIA | not examined | 18 | ||
| Erdem | 2007 | 169 | 20 | 4 | NT | NT | CLIA | not examined | 19 | |
| Fatourechi | 2003 | 14 | NT | NT | NT | 21b | HA | not examined | 20 | |
| Hasanat | 2000 | 15 | 46.7 | 26.7 | NT | NT | ELISA | not examined | 10 | |
| Boechat | 1999 | 6 | 0 | NT | NT | NT | RIA | not examined | 11 | |
| Hwang | 1989 | 39 | NT | NT | 26c | HA | not examined | 21 | ||
| Benker | 1988 | 31 | NT | NT | 6.5 | 6.5 | HA | persistently positive in2 | 22 | |
| Weetman | 1987 | 9 | 11 | 11 | 0 | 0 | ELISA, HA | not examined | 12 | |
| Lio | 1984 | 62 | NT | NT | 24 | 64 | HA | negative in all but1 | 23 | |
| Tikkanen | 1982 | 32 | NT | NT | 16 | 9 | HA | persistently positive in2 | 24 | |
NT, not tested; EIA, enzyme immunoassay; RIA, radioimmunoassay; CLIA, chemiluminescent immunometric assay; HA, hemagglutination assay; ELISA, enzyme-linked immunosorbent assay.
Combined TgAb and/or TPOAb.
Three strong positives, 11 weak positives (probably negative).
Combined thyroglobulin (TGHA) and/or microsomal hemagglutination antibodies (MCHA).
Painful Hashimoto's thyroiditis shows overlapping clinical features such as destructive thyroiditis with inflammatory findings and presence of anti-thyroid antibodies. However, painful Hashimoto's thyroiditis frequently shows the preexistence of a clinical history of Hashimoto's thyroiditis, high titration of anti-thyroid antibodies, refractoriness to glucocorticoid treatment, increased thyroid blood flow in the hypoechoic lesions, and development of permanent hypothyroidism, which are unlikely to be seen in subacute thyroiditis [13, 15, 16, 26, 27]. In this study, no subjects with subacute thyroiditis presented with such findings typical of painful Hashimoto's thyroiditis. On the other hand, there was no available information on whether positive reactions for anti-thyroid antibodies were present before or after the development of subacute thyroiditis, because we excluded all patients with preexisting Hashimoto's thyroiditis from the analysis.
Very interestingly, titers of positive TgAb decreased or disappeared at 4 months to 6 years after the onset of the disease. This temporal elevation in TgAb is very different from painful Hashimoto's thyroiditis, which shows persistently high values of anti-thyroid antibodies [26]. Considering these data, subacute thyroiditis might be initially associated with the development of thyroid autoantibodies, especially TgAb, possibly induced by thyroid destruction, and then these antibodies probably escaped the immune surveillance system. As summarized in Table 3, only a few reports have showed consecutive changes in TgAb. In this study, a small number of patients were available on follow-up for the changes in TgAb titers, and their intervals of examination varied. To overcome this limitation and prove the significance of decreased or disappeared TgAb titers, periodical follow-up of TgAb titers is required in a larger patient cohort with subacute thyroiditis in the future.
In conclusion, TgAb was moderately positive initially but levels gradually decreased afterwards in subacute thyroiditis.
Statement of Ethics
These healthy control subjects were staff members of our hospital and signed an informed consent form to participate in the study. The protocol was approved by the Ethical Committee of the Kuma Hospital.
Disclosure Statement
None of the authors has any potential conflict of interest associated with this research.
Acknowledgment
We would like to thank Mr. Shinji Morita for his help in measuring TgAb and TPOAb.
References
- 1.Nishihara E, Ohye H, Amino N, Takata K, Arishima T, Kudo T, et al. Clinical characteristics of 852 patients with subacute thyroiditis before treatment. Intern Med. 2008;47((8)):725–9. doi: 10.2169/internalmedicine.47.0740. [DOI] [PubMed] [Google Scholar]
- 2.Shrestha RT, Hennessey J. Acute and Subacute, and Riedel's Thyroiditis. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, Dungan K, Grossman A, et al., editors. Endotext. South Dartmouth (MA): 2000. [Google Scholar]
- 3.Farwell A, Sporadic painless, painful subacute and acute infectious thyroiditis . Tenth edition ed: Philadelphia: Lippincott Williams & Wilkins (LWW); 2013. A Fundemental and Clinical Text Braverman LE, Utiger RD The Thyroid; pp. p. 414–429. [Google Scholar]
- 4.Kubota S, Nishihara E, Kudo T, Ito M, Amino N, Miyauchi A. Initial treatment with 15 mg of prednisolone daily is sufficient for most patients with subacute thyroiditis in Japan. Thyroid. 2013 Mar;23((3)):269–72. doi: 10.1089/thy.2012.0459. [DOI] [PubMed] [Google Scholar]
- 5.Desailloud R, Hober D. Viruses and thyroiditis: an update. Virol J. 2009 Jan;6((1)):5. doi: 10.1186/1743-422X-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Obuobie K, Al-Sabah A, Lazarus JH. Subacute thyroiditis in an immunosuppressed patient. J Endocrinol Invest. 2002 Feb;25((2)):169–71. doi: 10.1007/BF03343982. [DOI] [PubMed] [Google Scholar]
- 7.Ozdogu H, Boga C, Bolat F, Ertorer ME. Wegener's granulomatosis with a possible thyroidal involvement. J Natl Med Assoc. 2006 Jun;98((6)):956–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Amino N, Hagen SR, Yamada N, Refetoff S. Measurement of circulating thyroid microsomal antibodies by the tanned red cell haemagglutination technique: its usefulness in the diagnosis of autoimmune thyroid diseases. Clin Endocrinol (Oxf) 1976 Mar;5((2)):115–25. doi: 10.1111/j.1365-2265.1976.tb02822.x. [DOI] [PubMed] [Google Scholar]
- 9.Nishihara E, Amino N, Kudo T, Ito M, Fukata S, Nishikawa M, et al. Comparison of thyroglobulin and thyroid peroxidase antibodies measured by five different kits in autoimmune thyroid diseases. Endocr J. 2017 Oct;64((10)):955–61. doi: 10.1507/endocrj.EJ17-0164. [DOI] [PubMed] [Google Scholar]
- 10.Hasanat MA, Rumi MA, Alam MN, Hasan KN, Salimullah M, Salam MA, et al. Status of antithyroid antibodies in Bangladesh. Postgrad Med J. 2000 Jun;76((896)):345–9. doi: 10.1136/pmj.76.896.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boechat LH, Zollner RL. Reactivity of anti-thyroid antibodies to thyroglobulin tryptic fragments: comparison of autoimmune and non-autoimmune thyroid diseases. Braz J Med Biol Res. 1999 Apr;32((4)):449–55. doi: 10.1590/s0100-879x1999000400012. [DOI] [PubMed] [Google Scholar]
- 12.Weetman AP, Smallridge RC, Nutman TB, Burman KD. Persistent thyroid autoimmunity after subacute thyroiditis. J Clin Lab Immunol. 1987 May;23((1)):1–6. [PubMed] [Google Scholar]
- 13.Rotondi M, Capelli V, Locantore P, Pontecorvi A, Chiovato L. Painful Hashimoto's thyroiditis: myth or reality? J Endocrinol Invest. 2017 Aug;40((8)):815–8. doi: 10.1007/s40618-017-0655-5. [DOI] [PubMed] [Google Scholar]
- 14.JapanThyroidAssociation Guidelines for the diagnosis of thyroid disease. 2010 available at: wwwjapanthyroidjp/doctor/guideline/englishhtml. [Google Scholar]
- 15.Ohye H, Nishihara E, Sasaki I, Kubota S, Fukata S, Amino N, et al. Four cases of Graves' disease which developed after painful Hashimoto's thyroiditis. Intern Med. 2006;45((6)):385–9. doi: 10.2169/internalmedicine.45.1506. [DOI] [PubMed] [Google Scholar]
- 16.Kon YC, DeGroot LJ. Painful Hashimoto's thyroiditis as an indication for thyroidectomy: clinical characteristics and outcome in seven patients. J Clin Endocrinol Metab. 2003 Jun;88((6)):2667–72. doi: 10.1210/jc.2002-021498. [DOI] [PubMed] [Google Scholar]
- 17.Omori N, Omori K, Takano K. Association of the ultrasonographic findings of subacute thyroiditis with thyroid pain and laboratory findings. Endocr J. 2008 Jul;55((3)):583–8. doi: 10.1507/endocrj.k07e-163. [DOI] [PubMed] [Google Scholar]
- 18.Benbassat CA, Olchovsky D, Tsvetov G, Shimon I. Subacute thyroiditis: clinical characteristics and treatment outcome in fifty-six consecutive patients diagnosed between 1999 and 2005. J Endocrinol Invest. 2007 Sep;30((8)):631–5. doi: 10.1007/BF03347442. [DOI] [PubMed] [Google Scholar]
- 19.Erdem N, Erdogan M, Ozbek M, Karadeniz M, Cetinkalp S, Ozgen AG, et al. Demographic and clinical features of patients with subacute thyroiditis: results of 169 patients from a single university center in Turkey. J Endocrinol Invest. 2007 Jul-Aug;30((7)):546–50. doi: 10.1007/BF03346347. [DOI] [PubMed] [Google Scholar]
- 20.Fatourechi V, Aniszewski JP, Fatourechi GZ, Atkinson EJ, Jacobsen SJ. Clinical features and outcome of subacute thyroiditis in an incidence cohort: olmsted County, Minnesota, study. J Clin Endocrinol Metab. 2003 May;88((5)):2100–5. doi: 10.1210/jc.2002-021799. [DOI] [PubMed] [Google Scholar]
- 21.Hwang SC, Jap TS, Ho LT, Ching KN. Subacute thyroiditis—61 cases review. Zhonghua Yi Xue Za Zhi (Taipei) 1989 Feb;43((2)):113–8. [PubMed] [Google Scholar]
- 22.Benker G, Olbricht T, Windeck R, Wagner R, Albers H, Lederbogen S, et al. The sonographical and functional sequelae of de Quervain's subacute thyroiditis: long-term follow-up. Acta Endocrinol (Copenh) 1988 Apr;117((4)):435–41. doi: 10.1530/acta.0.1170435. [DOI] [PubMed] [Google Scholar]
- 23.Lio S, Pontecorvi A, Caruso M, Monaco F, D'Armiento M. Transitory subclinical and permanent hypothyroidism in the course of subacute thyroiditis (de Quervain) Acta Endocrinol (Copenh) 1984 May;106((1)):67–70. doi: 10.1530/acta.0.1060067. [DOI] [PubMed] [Google Scholar]
- 24.Tikkanen MJ, Lamberg BA. Hypothyroidism following subacute thyroiditis. Acta Endocrinol (Copenh) 1982 Nov;101((3)):348–53. doi: 10.1530/acta.0.1010348. [DOI] [PubMed] [Google Scholar]
- 25.Latrofa F, Ricci D, Montanelli L, Altea MA, Pucci A, Pinchera A, et al. Thyroglobulin autoantibodies of patients with subacute thyroiditis are restricted to a major B cell epitope. J Endocrinol Invest. 2012 Sep;35((8)):712–4. doi: 10.1007/BF03345804. [DOI] [PubMed] [Google Scholar]
- 26.Shigemasa C, Ueta Y, Mitani Y, Taniguchi S, Urabe K, Tanaka T, et al. Chronic thyroiditis with painful tender thyroid enlargement and transient thyrotoxicosis. J Clin Endocrinol Metab. 1990 Feb;70((2)):385–90. doi: 10.1210/jcem-70-2-385. [DOI] [PubMed] [Google Scholar]
- 27.Onoda N, Kato Y, Seki T, Kurimoto M, Takano K, Ito Y, et al. Increased thyroid blood flow in the hypoechoic lesions in patients with recurrent, painful Hashimoto's thyroiditis at the time of acute exacerbation. Endocr J. 2009;56((1)):65–72. doi: 10.1507/endocrj.k08e-194. [DOI] [PubMed] [Google Scholar]