Abstract
Tendinopathy is a critical medical condition that often hinders level of participation for professional and young athletes in many sports. The purpose of the study was to describe the incidence and severity of tendinopathy in a multi-sport club with professional and youth teams. We performed a retrospective epidemiological study. Incidence of tendinopathy in players (n = 3839; 8-38 years, professional and youth) was reviewed over 8 seasons (2008-2016) in 5 team sports: football, basketball, handball, roller hockey, and futsal. Team physicians diagnosed and classified tendinopathies according to anatomical location, sport types, playing category, sex, playing surface, lost training time, and severity (time to return to play). Injuries were coded using OSICS-10, and incidence of tendinopathies were calculated as the number of injuries per 100 players per season. The total relative frequency of tendinopathy (versus total injuries) was 22% (843/3839) over 8 seasons from 360 in youth and 483 in professional teams. The incidence of injury was the highest in professional basketball [69.9, 95%CI: (58.0-81.4)] followed by professional roller hockey [64.4, 95%CI: (47.3-85.6)], and professional futsal [36.2, 95%CI: (27.3-47.1)]. The most incidences commonly affected tendons were the patellar [11.7, 95%CI: (10.0-13.5)] and Achilles [10.3, 95%CI: (8.5-12.5)]. Tendinopathies represent a significant number of injuries in team sports and are more common in professional than youth teams, especially basketball and roller hockey. Additional studies are needed to understand associated time-loss and impact on performance, and to develop prevention strategies for high risk sports.
Key points.
The incidence of higher in indoor sports especially in professional basketball followed by professional roller hockey, and professional futsal.
The longest time to RTP were associated with tendinopathy of the adductor longus (probably related with groin pain pathology).
Most common tendinopathies, patellar and Achilles, demonstrated considerable variability in their RTP time according to sport.
Tendinopathies represent a significant number of injuries in team sports and are more common in professional than youth teams, especially basketball and roller hockey.
30% of all tendinopathies in professional players result in time loss.
Key words: Tendinopathy, injuries, injury prevention, epidemiology, team sports, sports medicine
Introduction
Tendinopathy, characterized by tendon degeneration association with severe pain, is common and significantly impairs various functions in human movements, especially athletes.
According to a study by Nourissat et al. (2015), tendon disorders account for approximately 30% of musculoskeletal consultations. Several studies indicated that athletes with tendinopathy often experience serious pain, which further lead to reduced level of performance, loss of playing time, and end of one’s career (Docking et al., 2018; Cook et al., 2000).
The most widely recognised risk factors of tendinopathy were increased load and high physical demand during training and matches (Docking et al., 2018). Specifically, an imbalance between tendon loads and adaptive potential were considered as main extrinsic factors leading to tendinopathy (Nourissat et al., 2015). Intrinsic risk factors such as age, sex, metabolic and hormonal variables were also reported as an intrinsic risk factor of tendinopathy injury in some individuals (Abate et al., 2013), which may explain a high proportion of individuals, up to 35%, to sustain tendinopathy even though they do not participate in sport (de Jonge et al., 2011).
In a field of sports medicine, it is important to understand magnitude of injuries, precisely, the incidence of injury in terms of the number of injuries per exposure hours. In Van Mechelen’s (1992) model of injury prevention, the first step is to understand the extent of the injury. After identifying the size of the injury, prevention efforts targeting the certain sports and/or demographic groups are considered as a next logical step. To identify incidence of tendinopathy injuries, several studies were performed. The cumulative lifetime incidence of Achilles tendinopathy was reported as 52% among elite runners compared to 6% in the general population (Kujala et al., 2005). Lian et al. (2005) surveyed the prevalence of patellar tendinopathy based on sport types and found that volleyball is the highest (44.6% ± 6.6%) followed by basketball (31.9% ± 6.8%) (Lian et al., 2005).
However, aside from this work, no studies have characterised the incidence of a range of common tendinopathies among elite athletes from various sports.
We need more studies, especially with a long-term and quality data. This was achieved by accessing a large, retrospectively collected (8 seasons) database from a multi-sport professional club. We report the relative frequency of tendinopathy (in relation to other injuries), as well as how tendinopathy is related to the sport played, training time-loss and demographic factors. Thus, the purpose of the study was to describe the incidence and severity of tendinopathy in a multi-sport club with professional and youth teams.
Methods
Study design and participants
A retrospective study was conducted of all cases of tendinopathy recorded in Football Club Barcelona (FCB) athletes in five sports disciplines (football, basketball, handball, roller hockey, and indoor football/futsal) over 8 seasons (2008-2009 season to 2015-2016 season). Players were informed of the purpose and nature of the study and were given the opportunity to decline inclusion of their data. Players were assigned an individual identifier code with the identity concealed, ensuring player anonymity was maintained. The local research ethics committee (Barça Innovation Hub, FCB) approved the study. The study participants were 3839 players who had 843 episodes that were included as the aim of this study (Figure 1). The mean ± SD age of total players was 26.4±4.4 years (n=3839), and according to team category the mean± SD age was 29.8±5.7 years for professional players (n=504) and 19.5±2.9 years for youth players (n=3335), respectively. Regarding sport, the mean ± SD age was 31.7 ± 4.8 for football (n=2105), 25.2±7.0 for basketball (n=639), 24.3±6.8 for handball (n=612), 29.5±6.7 for roller hockey (n=131), and 29.2±7.2 for futsal (n=352), respectively.
Figure 1.
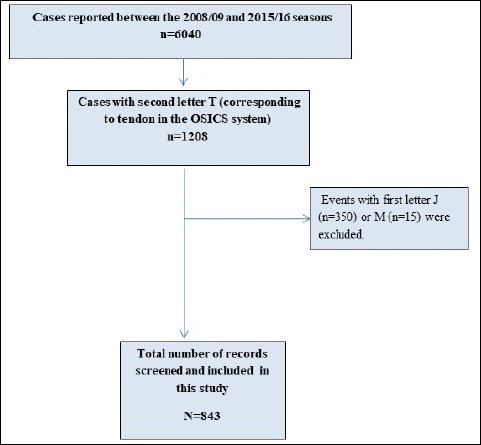
Flow chart tendinopathies record from the OSICS injury database.
Standardised injury registry at FCB
All injuries were securely stored in an injury registry containing standardised data for all injuries among all athletes at FCB. The medical department at FCB registered all injuries and illnesses of its athletes in an online database (Gestió Esportiva Mèdica, GEM). Each time an athlete required medical attention, the club’s team doctor registered the visit [diagnosis, physical assessment, complementary investigations (e.g. imaging, blood tests)], injury date, time of convalescence, treatment performed, progression of the symptom, and recurrences). In each case, return to play was managed by team physicians in accordance with the club’s clinical practice guidelines for tendinopathy injuries (FCB, 2010).
Injury classification
Each diagnosis was classified according to the Orchard Sports Injury Classification System, version 10.1 (OSICS). (Rae and Orchard, 2007; Orchard et al., 2010) This system is free, widely used (e.g. football, Australian football, rugby union, cricket and tennis) and is designed to accurately identify the location of the affected body structure. OSICS was the coding system used by all FCB medical services, and all medical staff members were trained in standardised use of the system.
Tendon injury diagnosis
Tendinopathy diagnosis was made based on a detailed history (localised tendon pain that was provoked by loading of that tendon site, e.g. jumping for patellar tendon, running and jumping for Achilles tendon), physical examination (tenderness on tendon palpation, pain reproduced with tendon loading tests), and ultrasound/doppler of the affected tendon (a lack of fibrillar structure in the tendon thickening and hypoechoic lesion with or without vessels). Where necessary, a magnetic resonance imaging (MRI) was also performed. Once classified and evaluated, the pathology was generally followed up through clinical exploration and ultrasound.
Identifying tendon injury data from the OSICS classified database
To filter tendinopathies from all recorded episodes, all recorded events with second letter T were selected (corresponding to tendon in the OSICS system), resulting in 1208 episodes. Of these, those with first letter J (n = 350, apophysitis) or M (n = 15, medical illnesses) were discarded. The remaining 843 episodes were included in the study, of which 15 (1.8%) were tendon ruptures (Figure 1).
Data extraction
All data extracted (from July of 2008 to July of 2016) for each injury episode pertinent to this study were de-identified to maintain players’ confidential information. However, socio-demographic variables including athletes’ age, sex, type of competition (professional or not), and information related to the tendinopathy injury were extracted (Table 1).
Table 1.
Description of the study variables.
| Variable | Categories |
|---|---|
| Sport | Football, Basketball, Handball, Roller Hockey, and Futsal |
| Sex | Male, Female |
| Team Levels | Professional (athletes playing over 18 years old status team) / Youth (athletes playing in junior or lower categories, between 8 and 17 years) |
| Surface of Injury | Outdoor (Football) and Indoor (Basketball, Handball, Hockey and Futsal) |
| Anatomical Location | Knee, Ankle, Foot, Hip and Groin, Buttocks and Pelvis, Shoulder, Elbow, Hand and wrist, and other body locations*. |
| Specific Tendinopathies | Patellar Tendon, Achilles Tendon, Proximal Tendon, Thigh Adductor, Proximal Tendon of the Femoral Rectus, and Proximal Tendon of the Hamstrings. |
*Other tendinopathies include those less common than 3%, mainly those of the upper body.
Definitions
The metrics time loss (TL) and time to return to play (RTP) were obtained based on consensus definitions and data collection procedures suggested by the Union of European Football Associations (UEFA)(Ekstrand et al., 2011; Fuller et al., 2006; Hägglund et al., 2005). TL injuries included any injury that occurred during a training session or match and caused the player to be absent for at least the next training session or match.
The RTP was calculated as the recovery time (in days) from the day of the injury until the player safely returned to training or competition.
Reinjury was defined as any injury of the same type at the same anatomic location as a previous injury in the same individual within 2 months of RTP. (Ekstrand et al., 2011).
Statistical analysis
The relative frequency of tendinopathy versus other injuries was reported, and the incidence of tendinopathies among athletes was evaluated. Relative frequency was calculated as a percentage of tendinopathies in relation to the total number of injuries in each category of interest. We calculated the summary measures of tendinopathies incidences (i) according to the formula i=n/e, where n is the number of injuries during the study period and e is the respective number of exposed (participating) athletes ("Athlete-Exposures”, AE), with incidence proportions presented as injuries per 100 athletes per season. To calculate incidences, we used the 'pois.exact' function from the epitools library in R, (Aragon, no date) which estimates incidence and 95% confidence intervals under a Poisson distribution. All analyses were performed using SPSS v21 and R statistical package (The R Foundation for Statistical Computing, Vienna, Austria), version 3.3.3.
Results
Relative frequency of tendinopathy
A total of 843 tendinopathy episodes were recorded in FCB players at both youth and professional levels between the 2008/2009 and 2015/2016 seasons. The overall relative frequency of tendinopathy was 22% of the total number of injuries registered by the club during the study period of 8 seasons (2008-2016). Tendinopathy was the most common in basketball players (29.3%), male players (92.3%), professional teams (57.3%), and indoor surface (54.3%).
The most common types of tendinopathy were patellar (21.5%), followed by Achilles (13%), other ankle (9.8%), other knee anatomical regions such as distal biceps femoris, distal semitendinosus or quadricipital tendon (8.5%), adductor longus (7.4%), shoulder (6.5%), proximal rectus femoris (5.2%), and proximal hamstrings (3.1%); the remaining 24.9% were accounted for by other types. Among the 843 episodes of tendinopathy, there were 40 recurrences within the same season. A reinjury was defined as a reinjury of pain at the same site after a pain-free period of 2 months or longer. There were also 31 reinjuries in subsequent seasons.
Incidence of tendinopathy
Table 2 shows the overall incidence of tendinopathies stratified according to sport, demographic and injury severity factors. The incidence was the highest in professional basketball team [69.9, 95%CI: (58.0-81.4)] following professional [64.4, 95%CI: (47.3-85.6)] roller hockey team. Incidence was higher in professional teams [35.9, 95%CI: (32.8-39.3)] than youth teams [14.4, 95%CI: (13-16)], and was higher among male players [23.3, 95%CI: (21.7-25)] than female players [12.4, 95%CI: (9.4-15.9)].
Table 2.
Incidence of tendinopathy.
| Num. of Injuries | Athlete-exposure (AE) | Incidence (95% CI) | |||
|---|---|---|---|---|---|
| Sport | Basketball | Professional | 140 | 203 | 69.9 (58.0-81.4) |
| Youth | 107 | 422 | 25.4 (20.8-30.6) | ||
| Football | Professional | 136 | 411 | 33.1 (27.8-39.1) | |
| Youth | 113 | 1052 | 10.7 (8.9-12.9) | ||
| Women Football | Professional | 39 | 257 | 15.2 (10.8-20.7) | |
| Youth | 21 | 228 | 9.2 (5.7-14.1) | ||
| Futsal | Professional | 55 | 152 | 36.2 (27.3-47.1) | |
| Youth | 21 | 177 | 11.9 (7.3-18.1) | ||
| Handball | Professional | 66 | 248 | 26.6 (20.6-33.9) | |
| Youth | 71 | 478 | 14.9 (11.6-18.7) | ||
| Roll Hockey | Professional | 47 | 73 | 64.4 (47.3-85.6) | |
| Youth | 27 | 138 | 19.6 (12.9-28.5) | ||
| Gender | Female | 60 | 485 | 12.4 (9.4-15.9) | |
| Male | 783 | 3354 | 23.3 (21.7-25) | ||
| Category | Youth | 360 | 2495 | 14.4 (13-16) | |
| Professional | 483 | 1344 | 35.9 (32.8-39.3) | ||
| Surface | Outdoor | 385 | 2277 | 16.9 (15.3-18.7) | |
| Indoor | 458 | 1562 | 29.3 (26.7-32.1) | ||
| Time-Loss | No | 546 | 2887 | 18.9 (17.4-20.6) | |
| Yes | 297 | 2771 | 10.7 (9.5-12) | ||
| Severity | No time loss | 546 | 2887 | 18.9 (17.4-20.6) | |
| 1-3 days | 76 | 1062 | 7.2 (5.6-9) | ||
| 4-7 days | 82 | 1221 | 6.7 (5.3-8.3) | ||
| 8-28 days | 98 | 1333 | 7.4 (6-9) | ||
| >28 days | 41 | 674 | 6.1 (4.4-8.3) | ||
Tables 3 and 4 show the incidence of common tendinopathy sites stratified according to sport, demographics (sex, team category, playing surface, and TL), and injury severity factors. The incidence of patellar tendinopathy was the highest in basketball players [professional 22.7, 95%CI: (16.6-30.2); youth 11.4, 95%CI: (8.4-15.1)], representing more than double that observed in professional football players (7.1, 95%CI: (4.7-10.1)). The incidence of Achilles tendinopathy was also higher in professional basketball [19.7, 95%CI: (14.1-26.8)], less so in youth basketball, followed by professional indoor football [7.9, 95%CI: (4.1-13.8)]. The incidence of hamstring tendinopathy was higher in professional roller hockey players [6.8, 95%CI: (2.2-16.0)], followed by professional football players [1.5, 95%CI: (0.5-3.2)]. The incidence of adductor tendinopathy was also highest in professional roller hockey [11.0, 95%CI: (4.7-21.6)], followed by professional and indoor football. The incidence of rectus femoris tendinopathy was highest in indoor professional football [2.0, 95%CI: (0.4-5.8)], followed by youth football [1.8, 95%CI: (1.1-2.8)]. Finally shoulder tendinopathy was the highest in handball [5.2, 95%CI: (2.8-9.0)] followed by roller hockey [4.1, 95%CI: (0.8-12.0)] and basketball [3.0, 95%CI: (1.1-6.4)] - (Table 3). The incidences of other tendinopathies (Other Knee, Other Ankle and Others) are shown in the Supplementary Table 4.
Table 3.
Incidence of tendinopathies (Patellar, Achilles, Hamstring, Adductor, Rectus Femoris and Shoulder)
| Patellar | Achilles | Hamstrings | Abductor | Rectus | Shoulder | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AE | n | Incidence (95% CI) | n | Incidence (95% CI) | n | Incidence (95% CI) | n | Incidence (95% CI) | n | Incidence (95% CI) | n | Incidence (95% CI) | |||
| Sport | Basketball | Professional | 203 | 46 | 22.7 (16.6-30.2) | 40 | 19.7 (14.1-26.8) | 1 | 0.5 (0.0-2.7) | 1 | 0.5 (0.0-2.7) | 1 | 0.5 (0.0-2.7) | 6 | 3.0 (1.1-6.4) |
| Youth | 422 | 48 | 11.4 (8.4-15.1) | 8 | 1.9 (0.8-3.7) | 2 | 0.5 (0.1-1.7) | 1 | 0.2 (0.0-1.3) | 2 | 0.5 (0.1-1.7) | 4 | 0.9 (0.3-2.4) | ||
| Football | Professional | 411 | 29 | 7.1 (4.7-10.1) | 20 | 4.9 (3.0-7.5) | 6 | 1.5 (0.5-3.2) | 21 | 5.1 (3.2-7.8) | 4 | 1.0 (0.3-2.5) | 5 | 1.2 (0.4-2.8) | |
| Youth | 1052 | 10 | 1.0 (0.5-1.7) | 2 | 0.2 (0.0-0.7) | 4 | 0.4 (0.1-1.0) | 10 | 1.0 (0.5-1.7) | 19 | 1.8 (1.1-2.8) | 3 | 0.3 (0.1-0.8) | ||
| Women's Football | Professional | 257 | 4 | 1.6 (0.4-4.0) | 6 | 2.3 (0.9-5.1) | 3 | 1.2 (0.2-3.4) | 2 | 0.8 (0.1-2.8) | 4 | 1.6 (0.4-4.0) | 2 | 0.8 (0.1-2.8) | |
| Youth | 228 | 4 | 1.8 (0.5-4.5) | 1 | 0.4 (0.0-2.4) | 0 | 0.0 (0.0-1.6) | 0 | 0.0 (0.0-1.6) | 3 | 1.3 (0.3-3.8) | 1 | 0.4 (0.0-2.4) | ||
| Futsal | Professional | 152 | 8 | 5.3 (2.3-10.4) | 12 | 7.9 (4.1-13.8) | 2 | 1.3 (0.2-4.8) | 5 | 3.3 (1.1-7.7) | 3 | 2.0 (0.4-5.8) | 1 | 0.7 (0.0-3.7) | |
| Youth | 177 | 5 | 2.8 (0.9-6.6) | 1 | 0.6 (0.0-3.1) | 0 | 0.0 (0.0-2.1) | 10 | 5.6 (2.7-10.4) | 0 | 0.0 (0.0-2.1) | 1 | 0.6 (0.0-3.1) | ||
| Handball | Professional | 248 | 16 | 6.5 (3.7-10.5) | 11 | 4.4 (2.2-7.9) | 1 | 0.4 (0.0-2.2) | 1 | 0.4 (0.0-2.2) | 1 | 0.4 (0.0-2.2) | 13 | 5.2 (2.8-9.0) | |
| Youth | 478 | 10 | 2.1 (1.0-3.8) | 7 | 1.5 (0.6-3.0) | 1 | 0.2 (0.0-1.2) | 5 | 1.0 (0.3-2.4) | 7 | 1.5 (0.6-3.0) | 13 | 2.7 (1.4-4.7) | ||
| Roller Hockey | Professional | 73 | 0 | 0.0 (0.0-5.1) | 1 | 1.4 (0.0-7.6) | 5 | 6.8 (2.2-16.0) | 8 | 11.0 (4.7-21.6) | 0 | 0.0 (0.0-5.1) | 3 | 4.1 (0.8-12.0) | |
| Youth | 138 | 1 | 0.7 (0.0-4.0) | 1 | 0.7 (0.0-4.0) | 1 | 0.7 (0.0-4.0) | 5 | 3.6 (1.2-8.5) | 0 | 0.0 (0.0-2.7) | 3 | 2.2 (0.4-6.4) | ||
| Gender | Female | 485 | 8 | 1.6 (0.7-3.3) | 7 | 1.4 (0.6-3.0) | 3 | 0.6 (0.1-1.8) | 2 | 0.4 (0.0-1.5) | 7 | 1.4 (0.6-3.0) | 3 | 0.6 (0.1-1.8) | |
| Male | 3354 | 173 | 5.2 (4.4-6.0) | 103 | 3.1 (2.5-3.7) | 23 | 0.7 (0.4-1.0) | 60 | 1.8 (1.4-2.3) | 37 | 1.1 (0.8-1.5) | 52 | 1.6 (1.2-2.0) | ||
| Category | Young | 2495 | 78 | 3.1 (2.5-3.9) | 20 | 0.8 (0.5-1.2) | 8 | 0.3 (0.1-0.6) | 24 | 1.0 (0.6-1.4) | 31 | 1.2 (0.8-1.8) | 25 | 1.0 (0.6-1.5) | |
| Senior | 1344 | 103 | 7.7 (6.3-9.3) | 90 | 6.7 (5.4-8.2) | 18 | 1.3 (0.8-2.1) | 38 | 2.8 (2.0-3.9) | 13 | 1.0 (0.5-1.7) | 30 | 2.2 (1.5-3.2) | ||
| Surface | Outdoor | 2277 | 60 | 2.6 (2.0-3.4) | 42 | 1.8 (1.3-2.5) | 15 | 0.7 (0.4-1.1) | 41 | 1.8 (1.3-2.4) | 33 | 1.4 (1.0-2.0) | 13 | 0.6 (0.3-1.0) | |
| Indoor | 1562 | 121 | 7.7 (6.4-9.3) | 68 | 4.4 (3.4-5.5) | 11 | 0.7 (0.4-1.3) | 21 | 1.3 (0.8-2.1) | 11 | 0.7 (0.4-1.3) | 42 | 2.7 (1.9-3.6) | ||
| Time-Loss | No | 2887 | 138 | 4.8 (4.0-5.6) | 81 | 2.8 (2.2-3.5) | 16 | 0.6 (0.3-0.9) | 25 | 0.9 (0.6-1.3) | 12 | 0.4 (0.2-0.7) | 35 | 1.2 (0.8-1.7) | |
| Yes | 2771 | 43 | 1.6 (1.1-2.1) | 29 | 1.1 (0.7-1.5) | 10 | 0.4 (0.2-0.7) | 37 | 1.3 (0.9-1.8) | 32 | 1.2 (0.8-1.6) | 20 | 0.7 (0.4-1.1) | ||
| Severity | No Time-loss | 2887 | 138 | 4.8 (4.0-5.6) | 81 | 2.8 (2.2-3.5) | 16 | 0.6 (0.3-0.9) | 25 | 0.9 (0.6-1.3) | 12 | 0.4 (0.2-0.7) | 35 | 1.2 (0.8-1.7) | |
| 1-3 days | 1062 | 12 | 1.1 (0.6-2.0) | 15 | 1.4 (0.8-2.3) | 2 | 0.2 (0.0-0.7) | 7 | 0.7 (0.3-1.4) | 3 | 0.3 (0.1-0.8) | 9 | 0.8 (0.4-1.6) | ||
| 4-7 days | 1221 | 11 | 0.9 (0.4-1.6) | 4 | 0.3 (0.1-0.8) | 3 | 0.2 (0.1-0.7) | 9 | 0.7 (0.3-1.4) | 12 | 1.0 (0.5-1.7) | 6 | 0.5 (0.2-1.1) | ||
| 8-28 days | 1333 | 13 | 1.0 (0.5-1.7) | 8 | 0.6 (0.3-1.2) | 3 | 0.2 (0.0-0.7) | 19 | 1.4 (0.9-2.2) | 11 | 0.8 (0.4-1.5) | 4 | 0.3 (0.1-0.8) | ||
| >28 days | 674 | 7 | 1.0 (0.4-2.1) | 2 | 0.3 (0.0-1.1) | 2 | 0.3 (0.0-1.1) | 2 | 0.3 (0.0-1.1) | 6 | 0.9 (0.3-2.0) | 1 | 0.2 (0.0-0.8) | ||
Table 4.
Other knee and ankle tendinophaty incidence.
| Other Knee | Other Ankle | Others | |||||||
|---|---|---|---|---|---|---|---|---|---|
| AE | n | Incidence (95% CI) | n | Incidence (95% CI) | n | Incidence (95% CI) | |||
| Sport | Basketball | Professional | 203 | 4 | 2.0 (0.5-5.0) | 17 | 8.4 (4.9-13.4) | 6 | 3.0 (1.1-6.4) |
| Youth | 422 | 8 | 1.9 (0.8-3.7) | 8 | 1.9 (0.8-3.7) | 26 | 6.2 (4.0-9.0) | ||
| Football | Professional | 411 | 8 | 1.9 (0.8-3.8) | 16 | 3.9 (2.2-6.3) | 5 | 1.2 (0.4-2.8) | |
| Youth | 1052 | 11 | 1.0 (0.5-1.9) | 14 | 1.3 (0.7-2.2) | 40 | 3.8 (2.7-5.2) | ||
| Women's Football | Professional | 257 | 9 | 3.5 (1.6-6.6) | 1 | 0.4 (0.0-2.2) | 2 | 0.8 (0.1-2.8) | |
| Youth | 228 | 4 | 1.8 (0.5-4.5) | 2 | 0.9 (0.1-3.2) | 6 | 2.6 (1.0-5.7) | ||
| Futsal | Professional | 152 | 5 | 3.3 (1.1-7.7) | 8 | 5.3 (2.3-10.4) | 1 | 0.7 (0.0-3.7) | |
| Youth | 177 | 1 | 0.6 (0.0-3.1) | 7 | 4.0 (1.6-8.1) | 3 | 1.7 (0.3-5.0) | ||
| Handball | Professional | 248 | 9 | 3.6 (1.7-6.9) | 4 | 1.6 (0.4-4.1) | 13 | 5.2 (2.8-9.0) | |
| Youth | 478 | 5 | 1.0 (0.3-2.4) | 4 | 0.8 (0.2-2.1) | 19 | 4.0 (2.4-6.2) | ||
| Roll Hockey | Professional | 73 | 6 | 8.2 (3.0-17.9) | 0 | 0.0 (0.0-5.1) | 3 | 4.1 (0.8-12.0) | |
| Youth | 138 | 2 | 1.4 (0.2-5.2) | 2 | 1.4 (0.2-5.2) | 12 | 8.7 (4.5-15.2) | ||
| Category | Youth | 2495 | 31 | 1.2 (0.8-1.8) | 37 | 1.5 (1.0-2.0) | 106 | 4.2 (3.5-5.1) | |
| Professional | 1344 | 41 | 3.1 (2.2-4.1) | 46 | 3.4 (2.5-4.6) | 104 | 7.7 (6.3-9.4) | ||
| Gender | Female | 485 | 13 | 2.7 (1.4-4.6) | 3 | 0.6 (0.1-1.8) | 14 | 2.9 (1.6-4.8) | |
| Male | 3354 | 59 | 1.8 (1.3-2.3) | 80 | 2.4 (1.9-3.0) | 196 | 5.8 (5.1-6.7) | ||
| Surface | Outdoor | 2277 | 38 | 1.7 (1.2-2.3) | 48 | 2.1 (1.6-2.8) | 95 | 4.2 (3.4-5.1) | |
| Indoor | 1562 | 34 | 2.2 (1.5-3.0) | 35 | 2.2 (1.6-3.1) | 115 | 7.4 (6.1-8.8) | ||
| Time-loss | No | 2887 | 41 | 1.4 (1.0-1.9) | 51 | 1.7 (1.3-2.3) | 147 | 5.1 (4.3-6.0) | |
| Yes | 2771 | 31 | 1.1 (0.8-1.6) | 32 | 1.2 (0.8-1.7) | 63 | 2.3 (1.7-2.9) | ||
| Severity | No Time Loss | 2887 | 41 | 1.4 (1.0-1.9) | 51 | 1.8 (1.3-2.3) | 147 | 5.1 (4.3-6.0) | |
| 1-3 Days | 1062 | 3 | 0.3 (0.1-0.8) | 13 | 1.2 (0.7-2.1) | 12 | 1.1 (0.6-2.0) | ||
| 4-7 Days | 1221 | 11 | 0.9 (0.4-1.6) | 7 | 0.6 (0.2-1.2) | 19 | 1.6 (0.9-2.4) | ||
| 8-28 Days | 1333 | 10 | 0.8 (0.4-1.4) | 5 | 0.4 (0.1-0.9) | 25 | 1.9 (1.2-2.8) | ||
| >28 Days | 674 | 7 | 1.1 (0.4-2.2) | 7 | 1.0 (0.4-2.1) | 7 | 1.1 (0.4-2.2) | ||
Return to play
Most tendinopathies did not cause the player to miss training or matches (64.4%), and only 5% had a severe effect on play (>28 days lost). Among tendinopathies that resulted in TL but did not involve rupture (n = 158), the median time to RTP was 7 days (interquartile range [IQR]:3-14). RTP time was the longest in cases of adductor longus tendinopathy and was most variable in cases involving the most commonly affected tendons, the patellar (IQR:3-14 days) and Achilles (IQR:1.7-12.5 days) tendons (Figure 2).
Figure 2.
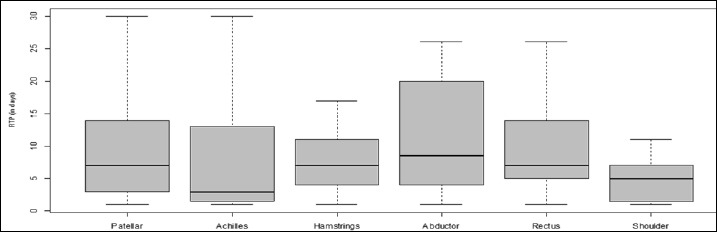
A box plot of time to return to play, according to type of tendinopathy
Discussion
The main finding of this study was that the relative frequency of tendinopathy is 22% of the total number of players registered at the club during the study period of 8 seasons (2008-2016). The incidence of injury was the highest in professional basketball [69.9, 95%CI: (58.0-81.4), Table 2] followed by professional roller hockey [64.4, 95%CI: (47.3-85.6), Table 2], and professional futsal [36.2, 95%CI: (27.3-47.1), Table 2]. With regards to the most commonly affected tendons, patellar tendon [11.7, 95%CI: (10.0-13.5), Table 3] and Achilles tendon [10.3, 95%CI: (8.5-12.5), Table 3]. The longest times to RTP were associated with tendinopathy of the hip adductor, and the most common tendinopathies, patellar and Achilles, demonstrated considerable variability the RTP times.
In our data, the highest incidence of tendinopathy was observed in professional basketball and roller hockey players, which is consistent with the past evidence given that it has found the highest incidence in basketball (Zwerver et al., 2011), handball (Janssen et al., 2015) and football players (Hägglund et al., 2011). It should be taken into account that these sports have, in matches and in training sessions, repetitive plyometric movements such as high-speed jumping, which is demanding for the tendons, especially Achilles and patellar tendon (Malliaras et al., 2013). Knowing which sports a higher incidence of tendinopathy and the most commonly affected tendons are likely useful to develop appropriate injury prevention strategies.
While Achilles and patellar tendons are commonly affected by tendinopathy in professional athletes, the prevalence of symptoms and morphological changes from adolescents to adults is unclear (Cassel et al., 2015; Visnes et al., 2015). A past investigation showed that patellar tendinopathy was more common than Achilles tendinopathy in adolescent athletes, (Lian et al., 2005) and our study results support the finding. Incidence of patellar tendinopathy [3.1, 95%CI: (2.5-3.9)] was higher than Achilles tendinopathy incidence [0.8, 95%CI: (0.5-1.2), Table 3]. However, once the level changed from young to professional status (older than 18 years old), the incidence between patellar and Achilles tendinopathy became comparable, indicating patellar tendinopathy of [7.7, 95%CI: (6.3-9.3)] and Achilles tendon of [6.7, 95%CI: (5.4-8.2), Table 3]. Furthermore, this is not unexpected since studies in the past indicated that tendinopathy prevalence increases with age.(Simpson et al., 2016; Cassel et al., 2015). Among adolescent athletes, patellar tendinopathy was more common than Achilles tendinopathy (Lian et al., 2005).
Furthermore, incidence was also higher among male athletes than among female athletes (ratio 9:1), which is consistent with a study that reported higher incidence of tendon related pathologies in men than in women (Morrison et al., 2015). This may be explained by many sex differences including hormone differences (i.e. estrogen may be protective in females until menopause) or sex differences in load-profile (e.g. high peak load and tendon stress in men (ref-include maximal jump ref being higher in men) and tendon mechanical property profiles for the Achilles (Kubo et al., 2003) and patellar tendon (Onambélé et al., 2007).
Another interesting finding of this study is effect of playing surface. A higher incidence of tendinopathies was observed in indoor compared to outdoor sports. The potential underlying mechanism may be because indoor sports involve more jumping actions (volleyball, basketball and handball). Additionally, there may also be more abrupt stopping and changes of directions because the playing space is smaller than playing space of outdoor sports. Indoor playing surfaces (usually parquet or cement) are also known as harder than outdoor surfaces (usually clay or grass). This may be a crucial extrinsic risk factor for tendinopathy due to excessive loading to the tendons in repetitive stress in nature that can lead to an overuse and, and may be resulted in tendon pathology (FCB, 2010; Paavola et al., 2005; Ferretti, 1986).
Consistent with most previous studies (Zwerver et al., 2011; Hägglund et al., 2011; Orchard et al., 2013; De Vries et al., 2017), the most common tendinopathy in our cohort was patellar tendinopathy, followed by Achilles tendinopathy. This finding is expected, since the patellar and Achilles are the largest locomotor tendons in the lower limb and have a key role in storing and releasing energy during stretch shorten cycle activities (Docking et al., 2016; 2018; Cook et al., 2016; Rio et al., 2014; Malliaras et al., 2013). Their histological, structural, biomechanical and functional characteristics make them more susceptible to injury, regardless of the workload (de Jonge et al., 2011; Lian et al., 2005; Magnusson et al., 2010).
In professional football there was a high incidence of adductor tendinopathy (5.1 and 1.0 in professional and youth players, respectively). Previous investigations suggested that groin pain accounts for up to 13% of football injuries (Ekstrand and Gillquist, 1983; Emery and Meeuwisse, 2001; Seward et al., 1993) and a key risk factor was considered as repetitive high-intensity change of direction such as cutting actions (Malliaras et al., 2009; Thorborg et al., 2018; Malliaras and O’Neill, 2017). In young footballers, proximal enthesopathy of the rectus femoris was also common. Since these players are still in the growing phase, tendon pathology at this site can be directly linked to traction epiphysitis at the antero-inferior iliac spine (Simpson et al., 2016; Cassel et al., 2015; Mersmann et al., 2017).
Moreover, regarding incidence in relation to the sport practiced, the highest incidence of Achilles and patellar tendinopathy was in basketball, likely because of the repetitive jumping, change of direction and sprinting demands of basketball. The ankle is another commonly affected region in basketball players, particularly the peroneal tendons and the posterior tibialis tendon. These findings are consistent with previous studies among basketball players (Drakos et al., 2010) that found that lateral ankle sprains were the most frequent orthopaedic injuries (13.2% of all injuries).
It is interesting to note that handball was the sport with the highest incidence of upper limb tendinopathies, particularly at the shoulder, probably because of the high velocity repetitive throwing motions that occurs in upper extremities. According to one study, shoulder flexion angular velocity in handball throwing motion may occur as fast as 150-550 degrees/second, (Wagner et al., 2014) and previous studies have also reported a high prevalence/incidence of shoulder tendinopathy in handball (Giroto et al., 2017).
One of the clinically challenging issue of assessing the tendinopathies in competitive club sports is the fact athletes still participate in their sports with pain, which did not require TL from their practices and competitions. The athletes themselves often tolerate the discomfort induced by tendinopathies, and they seek a consult from medical service only when the discomfort intensifies and becomes too pain to play (Rio et al., 2015). In our study the incidence of tendinopathy that did not result in lost playing or training time was 18.9 cases per 100 players per season (95%CI: 17.4-20.6), which was almost double the incidence of injuries that resulted in lost time playing (10.7, 95%CI: 9.5-12.00). However, recent evidence from elite Australian rules football indicates that even if players continue to compete, their performance is adversely affected (Docking et al., 2018)Another study also reported that patellar tendon abnormality was found by ultrasound examination; however, competitive athletes rated themselves “asymptomatic.” Those evidence indicates that performance level relative to tendinopathy symptoms should be assessed more carefully in order to examine the full impact of injuries (Rio et al., 2015; Clarsen et al., 2013).
Regarding time to RTP, the longest median RTP was found with adductor tendinopathies, with a significant proportion of severe cases with long RTP (Figure 2). Most cases of adductor tendinopathy are associated with adductor- or pubic-related groin pain, so this longer time in RTP may be related to pubic or groin involvement, especially in football players. Another interesting finding in the analysis of RTP, the greatest variability in RTP was observed in cases of patellar and Achilles tendinopathy (Rudavsky and Cook, 2014). Collectively, those findings suggest that each tendinopathy case is unique and requires individualized treatment plans.
Limitations and strengths
A possible limitation of this study was that we only studied athletes from one club, so our results might not be generalizable to other sports environments with different training or monitoring methods. Furthermore, athletes included in this dataset consisted of professional players and young athletes who were scouted by the study institution. Thus, the current results may be only applicable to elite athletes.
On the other hand, the aforementioned limitations of this study can be considered as strengths. Because the current study was performed by one institution, data collection method was consistent during the study period. Additionally, training and competition schedules were well tracked, and playing surface was the same across all sports and both levels. Moreover, the current study consisted of an 8-year of longitudinal data.
Perspectives
We analysed 843 episodes of tendinopathy among youth and adult athletes from five sports at FCB. Approximately one in every five injuries over an 8-year period was diagnosed as a tendinopathy, signifying that this injury category is a significant issue in elite sport. The highest incidence of tendinopathy was in basketball and roller hockey, and the most common sites of injury were the patellar and Achilles tendons. However, only about one in every three injuries resulted in significant time-loss, and the time loss was infrequently, and the TL ranged from 1 to 2 weeks. Findings of this study suggested that athletes are, for the most part, able to continue to play with tendinopathies. Future work should investigate the impact of tendinopathies on player and team performance to elucidate the full impact of these injuries.
Conclusion
Our study found that tendinopathies was commonly diagnosed injury/condition in FCB professional and youth level athletes. They were more common among professional players than youth players, and also more prevalent among indoor sports players than outdoor sports players. Approximately, 30% of all tendinopathies in professional players result in time loss. These data make an important contribution to understanding the magnitude of the problem and designing specific preventive and directed strategies according to sport, age, and playing surface.
Acknowledgements
The experiments comply with the current laws of the country in which they were performed. The authors have no conflicts of interests to declare.
Biographies
Daniel FLORIT
Employment
Medical Department, Futbol Club Barcelona, Barça Innovation Hub, Spain
Degree
MD
Research interest
Sport and exercise medicine, injury prevention, Muscle injuries
E-mail: daniel.florit@fcbarcelona.cat
Carles PEDRET
Employment
Sports Medicine and Imaging Department, Clinica Creu Blanca, Barcelona, Spain. Ultrasonography Department, Clinica Diagonal, Esplugues de Llobregat, Spain
Degree
MD, PhD
Research interest
Sport and exercise medicine, injury prevention, Muscle injuries
E-mail: carles@carlespedret.com
Martí CASALS
Employment
Biostatistician of the University of Vic – Central University of Catalonia (UVic-UCC), and Medical Department, Futbol Club Barcelona, Barcelona, Spain
Degree
PhD Biostatistics, MS
Research interest
Injury prevention, Sports medicine and Sports biostatistics
E-mail: marticasals@gmail.com
Peter MALLIARAS
Employment
Department of Physiotherapy, School of Primary and Allied Health Care, Monash University, Australia.
Degree
MD, PhD
Research interest
Sport and exercise medicine, injury prevention, Muscle injuries
E-ail: peter@completesportscare.com.au
Dai SUGIMOTO
Employment
Micheli Center for Sports Injury Prevention, Division of Sports Medicine, Department of Orthopedics, Boston Children’s Hospital
Degree
PhD
Research interests
Sports injury prevention
E-mail: dai.sugimoto@childrens.harvard.edu
Gil RODAS
Employment
Medical Department, Futbol Club Barcelona, Barça Innovation Hub, Spain. Sports Medicine Department. Clinic hospital /Sant Joan de Deu Hospital, Barcelona, Spain
Degree
MD, PhD
Research interest
Sport and exercise medicine, injury prevention, Muscle injuries
E-mail: gil.rodas@fcbarcelona.cat
References
- Abate M., Schiavone C., Salini V., Andia I. (2013) Occurrence of tendon pathologies in metabolic disorders. Rheumatology 52, 599–608. [DOI] [PubMed] [Google Scholar]
- Aragon T. J. (n.d.) Epidemiology Tools [R package epitools version 0.5-10]. [Google Scholar]
- Cassel M., Baur H., Hirschmüller A., Carlsohn A., Fröhlich K., Mayer F. (2015a) Prevalence of Achilles and patellar tendinopathy and their association to intratendinous changes in adolescent athletes. Scandinavian Journal of Medicine & Science in Sports 25, e310–e318. [DOI] [PubMed] [Google Scholar]
- Cassel M., Carlsohn A., Fröhlich K., John M., Riegels N., Mayer F. (2015b) Tendon Adaptation to Sport-specific Loading in Adolescent Athletes. International Journal of Sports Medicine 37, 159–164. [DOI] [PubMed] [Google Scholar]
- Clarsen B., Myklebust G., Bahr R. (2013) Development and validation of a new method for the registration of overuse injuries in sports injury epidemiology: the Oslo Sports Trauma Research Centre (OSTRC) Overuse Injury Questionnaire. British Journal of Sports Medicine 47, 495–502. [DOI] [PubMed] [Google Scholar]
- Cook J. L., Khan K. M., Kiss Z. S., Griffiths L. (2000) Patellar tendinopathy in junior basketball players: a controlled clinical and ultrasonographic study of 268 patellar tendons in players aged 14-18 years. Scandinavian Journal of Medicine & Science in Sports 10, 216–220. [DOI] [PubMed] [Google Scholar]
- Cook J. L., Rio E., Purdam C. R., Docking S. I. (2016) Revisiting the continuum model of tendon pathology: what is its merit in clinical practice and research? British Journal of Sports Medicine 50, 1187–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jonge S., van den Berg C., de Vos R. J., van der Heide H. J. L., Weir A., Verhaar J. A. N., Bierma-Zeinstra S. M. A., Tol J. L. (2011) Incidence of midportion Achilles tendinopathy in the general population. British Journal of Sports Medicine 45, 1026–1028. [DOI] [PubMed] [Google Scholar]
- De Vries A. J., Koolhaas W., Zwerver J., Diercks R. L., Nieuwenhuis K., Van Der Worp H., Brouwer S., Van Den Akker-Scheek I. (2017) The impact of patellar tendinopathy on sports and work performance in active athletes. Research in Sports Medicine 25, 253–265. [DOI] [PubMed] [Google Scholar]
- Docking S. I., Rosengarten S. D., Cook J. (2016) Achilles tendon structure improves on UTC imaging over a 5-month pre-season in elite Australian football players. Scandinavian Journal of Medicine & Science in Sports 26, 557–563. [DOI] [PubMed] [Google Scholar]
- Docking S. I., Rio E., Cook J., Orchard J. W., Fortington L. V. (2018) The prevalence of Achilles and patellar tendon injuries in Australian football players beyond a time-loss definition. Scandinavian Journal of Medicine & Science in Sports 28, 2016–2022. [DOI] [PubMed] [Google Scholar]
- Drakos M. C., Domb B., Starkey C., Callahan L., Allen A. A. (2010) Injury in the national basketball association: a 17-year overview. Sports Health 2, 284–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekstrand J., Gillquist J. (1983) Soccer injuries and their mechanisms: a prospective study. Medicine and Science in Sports and Exercise 15, 267–270. [DOI] [PubMed] [Google Scholar]
- Ekstrand J., Hägglund M., Waldén M. (2011) Injury incidence and injury patterns in professional football: the UEFA injury study. British Journal of Sports Medicine 45, 553–558. [DOI] [PubMed] [Google Scholar]
- Emery C. A., Meeuwisse W. H. (2001) Risk factors for groin injuries in hockey. Medicine and Science in Sports and Exercise 33, 1423–1433. [DOI] [PubMed] [Google Scholar]
- FCB. (2010) Guía de práctica clínica de las tendinopatias. [Google Scholar]
- Ferretti A. (1986) Epidemiology of Jumper’s Knee. Sports Medicine 3, 289–295. [DOI] [PubMed] [Google Scholar]
- Fuller C. W., Ekstrand J., Junge A., Andersen T. E., Bahr R., Dvorak J., Hägglund M., McCrory P., Meeuwisse W. H. (2006) Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. British Journal of Sports Medicine 40, 193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giroto N., Hespanhol Junior L. C., Gomes M. R. C., Lopes A. D. (2017) Incidence and risk factors of injuries in Brazilian elite handball players: A prospective cohort study. Scandinavian Journal of Medicine & Science in Sports 27, 195–202. [DOI] [PubMed] [Google Scholar]
- Hägglund M., Waldén M., Bahr R., Ekstrand J. (2005) Methods for epidemiological study of injuries to professional football players: developing the UEFA model. British Journal of Sports Medicine 39, 340–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hägglund M., Zwerver J., Ekstrand J. (2011) Epidemiology of Patellar Tendinopathy in Elite Male Soccer Players. The American Journal of Sports Medicine 39, 1906–1911. [DOI] [PubMed] [Google Scholar]
- Janssen I., Steele J. R., Munro B. J., Brown N. A. T. (2015) Previously identified patellar tendinopathy risk factors differ between elite and sub-elite volleyball players. Scandinavian Journal of Medicine & Science in Sports 25, 308–314. [DOI] [PubMed] [Google Scholar]
- Kubo K., Kanehisa H., Fukunaga T. (2003) Gender differences in the viscoelastic properties of tendon structures. European Journal of Applied Physiology 88, 520–526. [DOI] [PubMed] [Google Scholar]
- Kujala U. M., Sarna S., Kaprio J. (2005) Cumulative incidence of achilles tendon rupture and tendinopathy in male former elite athletes. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine 15, 133–135. [DOI] [PubMed] [Google Scholar]
- Lian Ø. B., Engebretsen L., Bahr R. (2005) Prevalence of Jumper’s Knee among Elite Athletes from Different Sports: A Cross-sectional Study. The American Journal of Sports Medicine 33, 561–567. [DOI] [PubMed] [Google Scholar]
- Magnusson S. P., Langberg H., Kjaer M. (2010) The pathogenesis of tendinopathy: balancing the response to loading. Nature Reviews Rheumatology 6, 262–268. [DOI] [PubMed] [Google Scholar]
- Malliaras P., Hogan A., Nawrocki A., Crossley K., Schache A. (2009) Hip flexibility and strength measures: reliability and association with athletic groin pain. British Journal of Sports Medicine 43, 739–744. [DOI] [PubMed] [Google Scholar]
- Malliaras P., Barton C. J., Reeves N. D., Langberg H. (2013) Achilles and Patellar Tendinopathy Loading Programmes. Sports Medicine 43, 267–286. [DOI] [PubMed] [Google Scholar]
- Malliaras P., O’Neill S. (2017) Potential risk factors leading to tendinopathy. Apunts. Medicina de l’Esport., 52, 71–77. [Google Scholar]
- Mersmann F., Bohm S., Schroll A., Boeth H., Duda G. N., Arampatzis A. (2017) Muscle and tendon adaptation in adolescent athletes: A longitudinal study. Scandinavian Journal of Medicine & Science in Sports 27, 75–82. [DOI] [PubMed] [Google Scholar]
- Morrison S. M., Dick T. J. M., Wakeling J. M. (2015) Structural and mechanical properties of the human Achilles tendon: Sex and strength effects. Journal of Biomechanics 48, 3530–3533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nourissat G., Berenbaum F., Duprez D. (2015) Tendon injury: from biology to tendon repair. Nature Reviews Rheumatology 11, 223. [DOI] [PubMed] [Google Scholar]
- Onambélé G. N. L., Burgess K., Pearson S. J. (2007) Gender-specific in vivo measurement of the structural and mechanical properties of the human patellar tendon. Journal of Orthopaedic Research 25, 1635–1642. [DOI] [PubMed] [Google Scholar]
- Orchard J., Rae K., Brooks J., Hägglund M., Til L., Wales D., Wood T. (2010) Revision, uptake and coding issues related to the open access Orchard Sports Injury Classification System (OSICS) versions 8, 9 and 10.1. Open Access Journal of Sports Medicine 1, 207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orchard J. W., Seward H., Orchard J. J. (2013) Results of 2 Decades of Injury Surveillance and Public Release of Data in the Australian Football League. The American Journal of Sports Medicine 41, 734–741. [DOI] [PubMed] [Google Scholar]
- Paavola M., Kannus P., Järvinen M. (2005) Epidemiology of Tendon Problems in Sport. In: Tendon Injuries. Springer-Verlag, London: 32–39. [Google Scholar]
- Rae K., Orchard J. (2007) The Orchard Sports Injury Classification System (OSICS) version 10. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine 17, 201–204. [DOI] [PubMed] [Google Scholar]
- Rio E., Moseley L., Purdam C., Samiric T., Kidgell D., Pearce A. J., Jaberzadeh S., Cook J. (2014) The Pain of Tendinopathy: Physiological or Pathophysiological? Sports Medicine 44, 9–23. [DOI] [PubMed] [Google Scholar]
- Rio E., Kidgell D., Purdam C., Gaida J., Moseley G. L., Pearce A. J., Cook J. (2015) Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. British Journal of Sports Medicine 49, 1277–1283. [DOI] [PubMed] [Google Scholar]
- Rudavsky A., Cook J. (2014) Physiotherapy management of patellar tendinopathy (jumper’s knee). Journal of Physiotherapy 60, 122–129. [DOI] [PubMed] [Google Scholar]
- Seward H., Orchard J., Hazard H., Collinson D. (1993) Football injuries in Australia at the élite level. Medical Journal of Australia 159, 298–301. [DOI] [PubMed] [Google Scholar]
- Simpson M., Rio E., Cook J. (2016) At What Age Do Children and Adolescents Develop Lower Limb Tendon Pathology or Tendinopathy? A Systematic Review and Meta-analysis. Sports Medicine 46, 545–557. [DOI] [PubMed] [Google Scholar]
- Thorborg K., Reiman M. P., Weir A., Kemp J. L., Serner A., Mosler A. B. (2018) Clinical Examination, Diagnostic Imaging, and Testing of Athletes With Groin Pain: An Evidence-Based Approach to Effective Management. Journal Orthopaedic Sports Physical Theraphy 48, 239–249. [DOI] [PubMed] [Google Scholar]
- van Mechelen W., Hlobil H., Kemper H. C. G. (1992) Incidence, Severity, Aetiology and Prevention of Sports Injuries. Sports Medicine 14, 82–99. [DOI] [PubMed] [Google Scholar]
- Visnes H., Tegnander A., Bahr R. (2015) Ultrasound characteristics of the patellar and quadriceps tendons among young elite athletes. Scandinavian Journal of Medicine & Science in Sports 25, 205–215. [DOI] [PubMed] [Google Scholar]
- Wagner H., Pfusterschmied J., Tilp M., Landlinger J., von Duvillard S. P., Müller E. (2014) Upper-body kinematics in team-handball throw, tennis serve, and volleyball spike. Scandinavian Journal of Medicine & Science in Sports 24, 345–354. [DOI] [PubMed] [Google Scholar]
- Zwerver J., Bredeweg S. W., van den Akker-Scheek I. (2011) Prevalence of Jumper’s knee among nonelite athletes from different sports: a cross-sectional survey. The American Journal of Sports Medicine 39, 1984–1988. [DOI] [PubMed] [Google Scholar]


