Abstract
Persistent pulmonary hypertension of the newborn (PPHN) is an essential cause for hypoxic respiratory failure with significant morbidity and mortality in term and near-term neonates. Hydrocortisone has been shown to decrease oxygen dependency and pulmonary hypertension in neonates with meconium aspiration syndrome and animal studies, respectively. We hypothesize that hydrocortisone will improve oxygenation in term and near-term infants with pulmonary hypertension. We performed a retrospective chart review of all infant with PPHN who received intravenous hydrocortisone therapy as a rescue for severe PPHN. Clinical response was objectively measured using, oxygenation index (OI), PaO2/FiO2 ratio, and inotrope score before, during, and after the hydrocortisone course. We found that hydrocortisone administration resulted in significant improvement of systolic blood pressure, OI, and PaO2/FiO2. In conclusion, hydrocortisone increased systolic blood pressure and improved oxygenation in term and near-term infants with persistent pulmonary hypertension. Prospective randomized trials are required to evaluate these findings further.
Keywords: hydrocortisone, steroids, PPHN, oxygenation index, systolic blood pressure, neonates, infants, NICU
Background
Persistent pulmonary hypertension of the newborn (PPHN) is an essential cause for hypoxic respiratory failure with significant morbidity and mortality in term and near-term neonates.1,2 It is a complex syndrome characterized by high pulmonary vascular resistance (PVR) to suprasystemic levels resulting in the extrapulmonary right-to-left shunting of blood leading to severe hypoxemia.3-5 Current standard therapy of PPHN includes supplemental oxygen, ventilation of the lung, hemodynamic support to maintain systemic vascular resistance, and inhaled nitric oxide (iNO) to reduce PVR.6,7 However, some infants do not respond to these measures necessitating the use of extracorporeal membrane oxygenation (ECMO), with the hope to allow enough time for lung vasculature to recover.8,9 Experimental studies both in animals and humans have shown that hydrocortisone (HC) can reduce the inflammatory process, stabilize systemic blood pressure, improve the cardiovascular stability in neonates with hypotension and low perfusion.10-12 Postnatal systemic steroids have been shown to decrease the duration of hospital length of stay and oxygen dependence in meconium aspiration syndrome (MAS).13 In the fetal lamb model of PPHN, HC treatment postnatally has been shown to improve oxygenation, increase cGMP levels, and reduce reactive oxygen species (ROS) levels.14 In spite of these effects, the role of HC in the management of PPHN, due to causes other than MAS in neonates is not clear. We conducted a retrospective chart review to evaluate the impact of intravenous (IV) HC in infants with severe PPHN on oxygenation and systolic blood pressure (SBP). We hypothesized that HC would increase SBP, decrease the right-to-left shunting, and improve oxygenation.
Methods
We conducted a retrospective chart review of all infants admitted to a level 4, neonatal intensive care unit (NICU) from January 2010 to June 2017. Term or near-term infants ⩾35 weeks of gestational age with the diagnosis of PPHN were included in the study. The diagnosis of PPHN was confirmed by echocardiography demonstrating elevated pulmonary arterial pressure (right-to-left shunting of blood at patent foramen ovale or ductus arteriosus, tricuspid regurgitation, and dilated right side of the heart with or without decrease right ventricular function).15 Only infants with PPHN and who received HC rescue for management of PPHN were reviewed and analyzed. Infants with congenital malformations or those who died within the first 24 hours after life were excluded from the study. Severity of the hypoxemic respiratory failure (HRF) was determined by two measures: oxygenation index (OI) = Fraction of inspired oxygen concentration (FiO2) × mean airway pressure (MAP) × 100/partial pressure of oxygen in the arterial blood in mmHg (PaO2) and PaO2/FiO2 ratio (P/F ratio). A higher OI and a lower P/F ratio would indicate the severity of HRF. Inhaled nitric oxide was started per unit protocol at 20 parts per million with echocardiographic evidence of PPHN and an OI of >15 by at least 2 arterial blood gases 4 hours apart after optimizing mechanical ventilation (partial pressure of carbon dioxide [pCO2] of 40-50 mm Hg and 8 ribs or more lung inflation on chest radiograph). Systemic hypotension was defined as a mean arterial blood pressure of less than the gestational age at the timepoint of measurement. Infants with hypotension were treated with inotropic agents per the discretion of the attending physician. Infants who failed to respond to the measures as mentioned above were started on IV HC (initial dose of 4 mg/kg/dose followed by 1 mg/kg/dose given every 6 hours for 48 hours). The response to HC on oxygenation and hemodynamics was trended by calculating the OI at several timepoints: before administration of HC; 6 hours into HC therapy; 24 hours into therapy, and 24 hours after completion of the therapy. Systolic blood pressures were collected, the inotrope scores (cumulative mean of dopamine dose (mcg/kg/min) + dobutamine dose (mcg/kg/min) + 100 × epinephrine dose (mcg/kg/min)) were calculated,16 and PaO2/FiO2 ratios were noted at the same timepoints. The demographic and clinical characteristics of the infants with PPHN who received HC treatment were recorded.
Data expressed as mean ± standard deviation, with n being the number of infants studied. We performed student t-test and analysis of variance with Fisher’s Post hoc testing when appropriate (SAS Systems, Cary, NC, USA) for data analysis. P-value < .05 was considered significant.
Ethical approval and informed consent
This study was approved by the ethics committee of University at Buffalo (Approval No. 030-753144). Informed consent requirement was waived as we analyzed the data with no identifiable private information.
Results
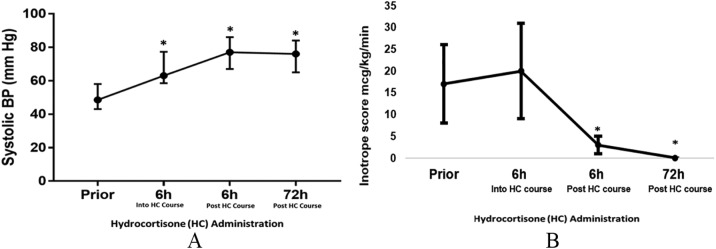
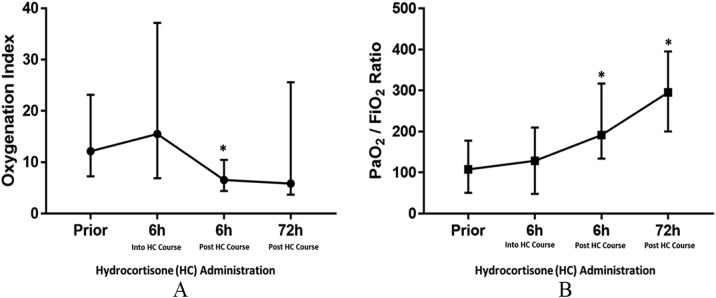
We identified 15 infants with PPHN who receive intravenous HC during the study period. All infants received iNO before HC treatment (Table 1). All infants were treated with dopamine as inotrope before HC administration. Milrinone was started on 7 infants (7/15, 46%) before HC administration. Two infants with severe PPHN did not respond to medical management and required ECMO support. In total, 7 infants (7/15, 47%) had asphyxia as the primary cause for PPHN, out of which 5 underwent whole body hypothermia. None of the infants included had intestinal perforation or necrotizing enterocolitis. Systolic blood pressure increased significantly with HC and remained elevated even after discontinuation of HC. In addition; there was a significant decrease in inotropic support as measured by inotropic score following initiation of HC (Figure 1). Significant reduction in OI, and an increase in PaO2/FiO2 ratio (Figure 2) were also observed in these infants. In attempt to identify a correlation between the SBP and P/F ration, we demonstrated a linear relationship between the two parameters (PaO2/FiO2 ratio and systolic blood pressure) (Figure 3), which could explain the significant improvement overtime noted after HC administration.
Table 1.
Baseline and clinical characteristics of infants with PPHN who received hydrocortisone.
| Gestational age in weeks | 38.2 ± 1.6 |
| Birth weight (g) | 2991 ± 650 |
| Sex (male) n (%) | 12 (80) |
| Normal vaginal delivery n (%) | 9 (60) |
| Cord pH | 7.05 ± 0.28 |
| APGAR at 5 minutes (range) | 6 (1-9) |
| Etiology of PPHN | |
| Asphyxia n (%) | 7 (47) |
| MAS n (%) | 2 (13) |
| Pneumonia or sepsis n (%) | 6 (40) |
| Surfactant n (%) | 11 (73) |
| Dopamine n (%) | 15 (100) |
| Inhaled NO n (%) | 15 (100) |
| Milrinone n (%) | 7 (46) |
| ECMO n (%) | 2 (13) |
Abbreviations: APGAR, Appearance, Pulse, Grimace, Activity, and Respiration, PPHN, persistent pulmonary hypertension, ECMO, extracorporeal membrane oxygenation; MAS, meconium aspiration syndrome; NO, nitric oxide.
Figure 1.
(A) Systolic blood pressure changes over time before and after the hydrocortisone (HC) administration. (B) Inotrope score overtime before and after hydrocortisone administration. *P value <.001 compared with before HC administration.
Figure 2.
(A) Oxygenation index changes overtime before and after the hydrocortisone (HC) administration. (B) PaO2/ FiO2 ratio changes overtime before and after hydrocortisone administration. *P < .001 compared with before HC administration.
Figure 3.
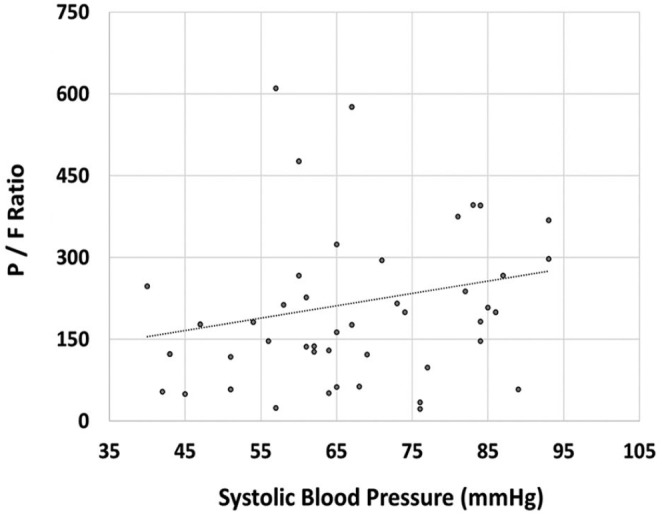
Correlation between PaO2/FiO2 ratio and systolic blood pressure. Significant linear correlation was demonstrated between systolic blood pressures and P/F ratio (r2 = 0.504; P < .001). P/F indicates PaO2/FiO2.
Discussion
To our knowledge, this is the first clinical study to evaluate the effects of intravenous HC in infants with severe PPHN due to all medical causes (Congenital anomalies were excluded). A course of HC in infants not responding to iNO and inotropes resulted in a significant improvement in SBP and oxygenation in our study. The findings suggest a potential role of HC in infants with PPHN and hypoxic respiratory failure and hypotension refractory to the conventional treatment.
Hydrocortisone is a commonly used medication in neonates for its anti-inflammatory properties. Common indications for HC in the NICU include bronchopulmonary dysplasia (or severe lung disease with the goal of extubation), systemic hypotension, and adrenal insufficiency.17-20 Majority of studies evaluating HC in the NICU have been conducted in preterm infants. A randomized trial to study HC in term infants was closed early due to low recruitment.21 Methylprednisolone decreased the length of stay with a rapid reduction in oxygen dependence and clearance of X-ray abnormalities in infants with MAS. The dose of methylprednisolone administered (0.5 mg/kg/day divided q 12 hours) was equivalent to HC used in our study.13 Interestingly, these patients with MAS enrolled in this study has a high incidence of sepsis (1/3 had a positive blood culture), but the frequency was not higher in the steroid group. In contrast, these results are not consistent with Yeh et al. showing no improvement in oxygenation with HC (10 mg/kg q 12 hours × 4 doses) in MAS.22 In spite of such a high dose of HC, there was no difference in oxygenation or radiological clearance. Infants with MAS who received HC took a more extended period to wean to room air and had prolonged respiratory distress compared with the placebo group. However, it is not clear if infants in either of these studies had evidence of PPHN by echocardiography.
In animal models of PPHN, we have shown that HC treatment improves oxygenation and decreases hyperoxia-induced changes in PDE5 activity and increasing cGMP levels in lambs with PPHN.14 A decrease in pulmonary phosphodiesterase 5 activity (an enzyme that converts cGMP to inactive 5′GMP), with increasing levels of cGMP results in smooth muscle relaxation.14 Hydrocortisone also reduces ROS levels in part by increasing superoxide dismutase activity in PPHN lambs ventilated with 100% O2.14
Glucocorticoids improve oxygenation and attenuate pulmonary hypertensive response in animal models of meconium aspiration.23 Improvement in oxygenation with HC can also be explained by its effect on the systemic blood pressure, as shown in our study.24 This effect persisted even after the discontinuation of HC treatment. The increase in SBP was associated with an improvement in oxygenation as measured by the P/F ratio and the OI. An increase in SBP can result in decreasing the right-to-left shunting at both the ductal and atrial levels. Increased systemic pressure can also improve the coronary arterial perfusion, which plays a critical role to support the function of the right ventricle to pump unoxygenated blood to the lungs. Finally, dopamine is a nonselective vasoconstrictor agent and can increase pulmonary arterial blood pressure. Weaning of dopamine following HC therapy may have played a role in increased pulmonary blood flow and oxygenation.
This study has several significant limitations, including its small sample size and is a retrospective study. Both of these limitations can result in the possibility of confounding variables that could affect outcomes. Echocardiogram was not performed at regular intervals to assess the effects of HC on pulmonary arterial pressures and right-to-left shunting in our cohort. We relied on indirect measures of severity of lung disease and PPHN by measuring P/F ratio and OI during and after HC. However, all infants had an echocardiogram before HC to confirm the diagnosis of PPHN. Follow up echocardiograms were obtained until the resolution of the PPHN. Cortisol levels were not obtained before HC initiation. In spite of these limitations, we observed that HC increased SBP and improved OIs.
In conclusion, HC increases SBP and improves oxygenation as measured by OI and P/F ratio. Increase in SBP with a reduction in right-to-left shunt may contribute partly to improvement in oxygenation in PPHN. Prospective randomized trials are required to evaluate the role of HC therapy in infants with PPHN.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: MA: conceptualized and designed the study, collected, analyzed and interpreted the data; drafted the initial manuscript and reviewed and revised the manuscript.
SL, VHSK: conceptualized the study design, contributed to analyses and interpretation of data, and revising the manuscript for critically important intellectual content.
AM: Collected, analyzed and interpreted the data, and reviewed the manuscript.
ORCID iD: Mahdi Alsaleem  https://orcid.org/0000-0002-2285-2963
https://orcid.org/0000-0002-2285-2963
References
- 1. Levin DL, Heymann MA, Kitterman JA, Gregory GA, Phibbs RH, Rudolph AM. Persistent pulmonary hypertension of the newborn infant. J Pediatr. 1976; 89:626-630. [DOI] [PubMed] [Google Scholar]
- 2. Mathew B, Lakshminrusimha S. Persistent pulmonary hypertension in the newborn. Children (Basel). 2017;4:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lakshminrusimha S, Keszler M. Persistent pulmonary hypertension of the newborn. NeoReviews. 2015;16:e680-e692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Steinhorn RH. Neonatal pulmonary hypertension. Pediatr Crit Care Med. 2010;11:S79-S84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Teixeira-Mendonca C, Henriques-Coelho T. Pathophysiology of pulmonary hypertension in newborns: therapeutic indications. Rev Port Cardiol. 2013;32: 1005-1012. [DOI] [PubMed] [Google Scholar]
- 6. Nair J, Lakshminrusimha S. Update on PPHN: mechanisms and treatment. Semin Perinatol. 2014;38:78-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dhillon R. The management of neonatal pulmonary hypertension. Arch Dis Child Fetal Neonatal Ed. 2012;97:F223-F228. [DOI] [PubMed] [Google Scholar]
- 8. Lazar DA, Cass DL, Olutoye OO, et al. The use of ECMO for persistent pulmonary hypertension of the newborn: a decade of experience. J Surg Res. 2012;177: 263-267. [DOI] [PubMed] [Google Scholar]
- 9. Van Berkel S, Binkhorst M, Van Heijst A, Liem D. Adapted ECMO entry criteria for newborns with persistent pulmonary hypertension (PPHN) following treatment with inhaled nitric oxide (INO) and/or high-frequency oscillatory ventilation (HFOV). Pediatr Res. 2011;70:744. [DOI] [PubMed] [Google Scholar]
- 10. Seri I. Hydrocortisone is effective in treatment of vasopressor-resistant hypotension in very low birth weight neonates. J Pediatr. 2006;149:422-423. [DOI] [PubMed] [Google Scholar]
- 11. Ibrahim H, Sinha IP, Subhedar NV. Corticosteroids for treating hypotension in preterm infants. Cochrane Database Syst Rev. 2011;12:CD003662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Abraham E, Evans T. Corticosteroids and septic shock. JAMA. 2002;288:886-887. [DOI] [PubMed] [Google Scholar]
- 13. Tripathi S, Saili A. The effect of steroids on the clinical course and outcome of neonates with meconium aspiration syndrome. J Trop Pediatr. 2006;53:8-12. [DOI] [PubMed] [Google Scholar]
- 14. Perez M, Lakshminrusimha S, Wedgwood S, et al. Hydrocortisone normalizes oxygenation and cGMP regulation in lambs with persistent pulmonary hypertension of the newborn. Am J Physiol Lung Cell Mol Physiol. 2012;302:L595-L603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jone P-N, Ivy DD. Echocardiography in pediatric pulmonary hypertension. Front Pediatr. 2014;2:124-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gaies MG, Jeffries HE, Niebler RA, et al. Vasoactive-inotropic score is associated with outcome after infant cardiac surgery: an analysis from the Pediatric Cardiac Critical Care Consortium and Virtual PICU System Registries. Pediatr Crit Care Med. 2014;15:529-537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pulmonary effects of neonatal hydrocortisone treatment in ventilator-dependent preterm infants. Int J Pediatr. 2011;2011:783893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Altit G, Vigny-Pau M, Barrington K, Dorval VG, Lapointe A. Corticosteroid therapy in neonatal septic shock-do we prevent death? Am J Perinatol. 2018;35: 146-151. [DOI] [PubMed] [Google Scholar]
- 19. Watterberg KL. Hydrocortisone dosing for hypotension in newborn infants: less is more. J Pediatr. 2016;174:23-26.e21. [DOI] [PubMed] [Google Scholar]
- 20. Watterberg KL, Gerdes JS, Gifford KL, Lin H-M. Prophylaxis against early adrenal insufficiency to prevent chronic lung disease in premature infants. Pediatrics. 1999;104:1258-1263. [DOI] [PubMed] [Google Scholar]
- 21. Watterberg KL, Fernandez E, Walsh MC, et al. Barriers to enrollment in a randomized controlled trial of hydrocortisone for cardiovascular insufficiency in term and late preterm newborn infants. J Perinatol. 2017;37:1220-1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yeh T, Srinivasan G, Harris V, Pildes R. Hydrocortisone therapy in meconium aspiration syndrome: a controlled study. J Pediatr. 1977;90:140-143. [DOI] [PubMed] [Google Scholar]
- 23. Soukka H, Halkola L, Aho H, Rautanen M, Kero P, Kaapa P. Methylprednisolone attenuates the pulmonary hypertensive response in porcine meconium aspiration. Pediatr Res. 1997;42:145. [DOI] [PubMed] [Google Scholar]
- 24. Sharma V, Berkelhamer S, Lakshminrusimha S. Persistent pulmonary hypertension of the newborn. Matern Health Neonatol Perinatol. 2015;1:14. [DOI] [PMC free article] [PubMed] [Google Scholar]