Abstract
Background:
Revision surgery is a known complication after anterior cruciate ligament (ACL) reconstruction (ACLR), but the proportion of patients who seek a different surgeon for their revision procedure is unknown.
Purpose:
To determine the rate and risk factors for revision ACLR in New Zealand and to find the proportion of patients undergoing revision ACLR who see a different surgeon compared with their primary procedure as well as the factors that may influence this decision.
Study Design:
Case series; Level of evidence, 4.
Methods:
Data from New Zealand’s single government insurer, the Accident Compensation Corporation (ACC), were analyzed. All primary ACLR procedures performed between January 1, 2009, and December 31, 2014 were evaluated, and revision ACLR procedures performed between January 1, 2009, and December 31, 2016, were evaluated to allow for a minimum 2-year follow-up period. Cases undergoing subsequent revision were divided into those with the same or a different surgeon compared with the primary procedure. Risk factors for revision and change of surgeons were assessed, including age, sex, time from injury to surgery, time between primary and revision procedures, surgeon volume, and ethnicity.
Results:
A total of 15,212 primary ACLR procedures were recorded in 14,926 patients. The mean patient age was 29.2 years, and 61% were male patients. There were 676 subsequent revision procedures and 510 contralateral procedures during the study period, resulting in a 5-year survival rate of 95.5% for the ACL graft and 96.5% for the contralateral ACL. Risk factors for revision surgery included male sex, age <20 years, and <1 year from injury to surgery. Of the revision procedures, 44.5% (n = 301) were performed by a different surgeon compared with primary ACLR. For primary ACLR procedures performed by low-volume surgeons, 75.0% of patients requiring revision ACLR changed surgeons, compared with 21.5% for high-volume surgeons (≤10 vs >50 primary ACLR/y; hazard ratio, 10.70 [95% CI, 6.01-19.05]; P < .001). Other factors associated with change of surgeons included older age, longer time between primary and revision surgery, and Asian and Maori ethnicities.
Conclusion:
A significant proportion of patients change surgeons when requiring revision ACLR. In the absence of formal follow-up systems such as registries, surgeons, particularly those with a low volume of ACLRs, may underestimate their personal revision rate.
Keywords: ACL, revision ACL reconstruction, contralateral ACL reconstruction, knee, ligaments
Anterior cruciate ligament (ACL) reconstruction (ACLR) is a common orthopaedic procedure, with over 100,000 performed annually in the United States.5 Between 30% and 75% patients with functional instability after an ACL rupture seek ligament reconstruction.17,20 After ACLR, a repeat ACL injury occurs in up to 33% of young, active patients.18 Many of these patients undergo revision ACLR, estimated at around 7% of all ACLR procedures performed.26 Revision ACLR has poorer outcomes compared with primary procedures,1,9 with only 40% of patients returning to their previous level of sport.2
Reported risk factors for revision ACLR include male sex, younger age, and elevated body mass index15 as well as other factors including early return to sport and graft choice.3,15,18 Technical factors are also important, and it is unclear how many patients with reinjuries choose to see a different surgeon, as access to patient data often relies on patients returning to their original surgeon after a repeat injury. To our knowledge, this figure has never been reported. This has an effect on the surgeon’s perception of “success” after primary ACLR, as he or she may be unaware that subsequent revision surgery took place.
The Accident Compensation Corporation (ACC) is a government insurer and is the primary funder for the treatment of injuries in New Zealand. The ACC started in 1970 and has been the sole provider of accident insurance of all injuries since 2000. Their no-fault injury scheme allows every New Zealander to receive free compensation for accidental injuries, including coverage for private medical care and loss of income.7 The ACC funds almost all ACLR procedures performed in New Zealand, as an ACL injury typically has an accidental cause. If primary ACLR is funded by the ACC, any revision procedure will also receive funding and will be recorded in its database. Patients have some freedom in choosing which surgeon to see, requiring only a referral from any health care provider such as a physical therapist or general practitioner.
The aim of the study was to use ACC data to investigate the rate of revision and contralateral ACLR in New Zealand and the risk factors for patients requiring these procedures. We aimed to assess the frequency with which patients undergo a revision procedure with a different surgeon and the factors associated with this outcome.
Methods
Study Design, Data Collection, and Study Sample
A retrospective case series study was conducted using prospectively collected data from the ACC. Ethical approval was obtained before study commencement. After an injury is registered with the ACC, patient information is collected from registered health providers, where it is recorded in an electronic database including copies of all correspondence and operation notes. Standardized patient data include age, sex, ethnicity, date of injury, date of surgery, concurrent meniscal procedures, cause of injury, and a unique surgeon identification number. Patients can be identified in the database by a unique identification number assigned by the ACC and by their National Health Index (NHI) number, which is correlated to their patient information. Primary and revision ACLR procedures are entered separately in the database and can be identified by their operation codes (codes KNE80, KNE81, KNE82, KNE90, and KNE91 for primary surgery and KNE83, KNE84, and KNE93 for revision surgery) (Table 1).
TABLE 1.
Accident Compensation Corporation Operation Codesa
| Operation Code | Code Description |
|---|---|
| KNE80 | Knee ACL reconstruction - 1 |
| KNE81 | Knee ACL single-bundle reconstruction, arthroscopic/open |
| KNE82 | Knee ACL double-bundle reconstruction, primary/simple |
| KNE83 | Revision knee ACL single-bundle reconstruction, complex |
| KNE84 | Revision knee ACL double-bundle reconstruction, complex |
| KNE90 | Knee ACL reconstruction - 2 |
| KNE91 | KNE81 with meniscal repair and/or Outerbridge drilling |
| KNE93 | KNE83 with meniscal repair and/or Outerbridge drilling |
aACL, anterior cruciate ligament.
Our inclusion study dates started from 2009 because there was a coding modification within the ACC at that time. Primary ACLR procedures performed from January 2009 to December 2014 and revision or contralateral ACLR procedures performed from January 2009 to December 2016 were included, thus allowing for a minimum 2-year follow-up of the primary procedure. Patients’ ACC identification numbers were cross-checked with their NHI number, and patients who shared the same date of birth, sex, and ethnicity were identified to find and exclude duplicate entries. Revision procedures that did not match a primary procedure from 2009 to 2014 by patient identification number and side were excluded from the dataset. Where discrepancies were found in the dataset, deidentified patient notes were accessed to check and correct potential errors in coding. Patients with claims for more than 1 primary ACLR on the same side were studied. Operation notes were accessed to identify incorrectly coded revision ACLR or other procedures, which were sorted into the revision dataset or excluded accordingly. Patients with multiple revision ACLR procedures were identified, and only the first revision on each side was included. Surgeons in the dataset were analyzed and correlated to 1 surgeon identification number only. Patient data were deidentified before collection to protect patient privacy.
Outcomes of Interest
All primary ACLR procedures, including patients’ contralateral procedures, were followed up for revision ACLR. For those patients with bilateral primary ACLR, we also tracked the first primary ACLR until the subsequent contralateral primary ACLR to find the contralateral ACLR rate. Annual revision and contralateral ACLR rates were calculated for the years 2009 to 2014 to find the mean. Survival analyses were performed using Kaplan-Meier curves and Cox proportional hazards regression with revision ACLR and contralateral ACLR as the endpoints. Follow-up was taken from the date of the primary ACLR procedure to the revision or contralateral ACLR procedure. The cases that required revision surgery were studied, and we identified the surgeon for primary ACLR and any subsequent revision procedure. The percentage of revision ACLR procedures performed by a different surgeon from primary ACLR was determined.
Exposures of Interest
Patient factors at the time of primary ACLR, including age, sex, ethnicity, time from injury to primary ACLR, and cause of injury, were explored as possible risk factors for subsequent revision surgery. Age was divided a priori into <20 years and ≥20 years, as we aimed to ensure that “young age” covered school-aged patients in New Zealand. Time from injury to surgery was arbitrarily divided into <1 year and ≥1 year. Patients with a different surgeon for the primary and revision procedures were compared with those who had the same surgeon for both procedures. Surgeon volume was calculated for each surgeon and was expressed as the number of primary ACLR procedures performed per annum: low (≤10), medium low (11-30), medium high (31-50), and high (>50).
Statistical Analysis
Results were considered statistically significant at P < .05. Continuous variables were assessed for normality using Q-Q plots and histograms. Univariate analysis was performed using the chi-square test or Fisher exact test for categorical variables and the Student t test for continuous variables. The 5-year cumulative probability of ipsilateral revision and contralateral reconstruction after primary ACLR was calculated using Kaplan-Meier estimates. Variables that had a statistically significant association with the rate of ipsilateral revision or contralateral reconstruction on univariate analysis were entered into an adjusted Cox regression model to produce hazard ratios (HRs). The cumulative survival probability of revision and contralateral reconstruction for each sport type was analyzed using an adjusted Cox regression survival plot with statistically significant univariate factors entered into the model. Log(-log) plots were visualized to assess the assumption of proportional hazards.
To identify independent predictors associated with a change of surgeons in revision procedures, multivariable binary logistic regression was utilized to produce odds ratios.
STATA version 14 (StataCorp) was used to produce Kaplan-Meier survival curves with 95% CIs. All other statistical analyses were performed using SPSS version 25 (IBM).
Results
There were 15,212 cases of primary ACLR performed in 14,926 patients between 2009 and 2014. The mean age of all patients at the time of the primary procedure was 29.2 ± 10.6 years, and the majority was male (n = 9337; 61%). There were 676 patients who underwent revision ACLR between 2009 and 2016, and of the 14,926 patients who underwent primary ACLR, 510 underwent subsequent contralateral ACLR between 2009 and 2016. The mean age of patients who required revision surgery was 23.2 ± 8.2 years compared with 29.5 ± 10.6 years for the patients who did not undergo revision (Table 2). The mean number of active ACLR surgeons was 151 each year, performing a mean of 36.0 ± 0.8 primary ACLR procedures per year (range, 0.5-105.0 primary ACLR/y).
TABLE 2.
Patient Characteristicsa
| Characteristic | Revision | Contralateral | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total Cases, n | Yes, n | No, n | % Revised | P | Total Patients, n | Yes, n | No, n | % Contralateral | P | |
| Primary ACLR | 15,212 | 676 | 14,536 | 4.4 | 14,926 | 510 | 14,416 | 3.4 | ||
| Age, y | ||||||||||
| Mean ± SD | 29.2 ± 10.6 | 23.2 ± 8.2 | 29.5 ± 10.6 | <.001b | 29.2 ± 10.6 | 24.0 ± 8.4 | 29.4 ± 10.7 | <.001c | ||
| <20 | 3135 | 275 | 2860 | 8.8 | <.001b | 3074 | 191 | 2883 | 6.2 | <.001c |
| ≥20 | 12,077 | 401 | 11,676 | 3.3 | 11,852 | 319 | 11,533 | 2.7 | ||
| Sex | ||||||||||
| Male | 9337 | 458 | 8879 | 4.9 | <.001b | 9168 | 311 | 8857 | 3.4 | .834 |
| Female | 5875 | 218 | 5657 | 3.7 | 5758 | 199 | 5559 | 3.5 | ||
| Time from injury to primary ACLR | ||||||||||
| Mean ± SD, d | 449.0 ± 1023.8 | 242.1 ± 508.0 | 458.7 ± 1040.6 | <.001b | 448.6 ± 1020.6 | 287.7 ± 569.8 | 454.3 ± 1032.5 | <.001c | ||
| <1 y | 11,954 | 604 | 11,350 | 5.1 | <.001b | 11,723 | 433 | 11,290 | 3.7 | <.001c |
| ≥1 y | 3258 | 72 | 3186 | 2.2 | 3203 | 77 | 3126 | 2.4 | ||
| Cause of injury | ||||||||||
| Sport | 11,337 | 538 | 10,799 | 4.7 | .002b | 11,121 | 411 | 10,710 | 3.7 | .001c |
| Other | 3875 | 138 | 3737 | 3.6 | 3805 | 99 | 3706 | 2.6 | ||
| Sport type | ||||||||||
| Netball | 2202 | 65 | 2137 | 3.0 | <.001b | 2154 | 83 | 2071 | 3.9 | <.001c |
| Rugby union | 2149 | 139 | 2010 | 6.5 | 2106 | 86 | 2020 | 4.1 | ||
| Soccer | 1937 | 103 | 1834 | 5.3 | 1896 | 82 | 1814 | 4.3 | ||
| Touch rugby | 904 | 42 | 862 | 4.6 | 876 | 41 | 835 | 4.7 | ||
| Rugby league | 475 | 35 | 440 | 7.4 | 467 | 15 | 452 | 3.2 | ||
| Basketball | 460 | 28 | 432 | 6.1 | 448 | 26 | 422 | 5.8 | ||
| Other | 2431 | 106 | 2325 | 4.4 | 2398 | 70 | 2328 | 2.9 | ||
| Skiing/snowboarding | 779 | 20 | 759 | 2.6 | 776 | 8 | 768 | 1.0 | ||
| Ethnicity | ||||||||||
| European | 9127 | 424 | 8703 | 4.7 | .235 | 8983 | 262 | 8721 | 2.9 | .001c |
| Maori | 2549 | 93 | 2456 | 3.7 | 2492 | 103 | 2389 | 4.1 | ||
| Pacific | 1646 | 74 | 1572 | 4.5 | 1600 | 74 | 1526 | 4.6 | ||
| Asian | 882 | 37 | 845 | 4.2 | 861 | 34 | 827 | 4.0 | ||
| Other | 703 | 36 | 667 | 5.1 | 689 | 27 | 662 | 3.9 | ||
| Unknown | 305 | 12 | 293 | 3.9 | 301 | 10 | 291 | 3.3 | ||
| Surgeon volume, primary ACLR/y | ||||||||||
| ≤10 | 2523 | 104 | 2419 | 4.1 | <.001b | 2492 | 65 | 2427 | 2.6 | .009c |
| 11-30 | 4438 | 157 | 4281 | 3.5 | 4351 | 140 | 4211 | 3.2 | ||
| 31-50 | 4576 | 215 | 4361 | 4.7 | 4485 | 155 | 4330 | 3.5 | ||
| >50 | 3675 | 200 | 3475 | 5.4 | 3598 | 150 | 3448 | 4.2 | ||
aACLR, anterior cruciate ligament reconstruction.
bUnivariate analysis suggested a statistically significant difference in the rate of revision ACLRs between groups (P < .05).
cUnivariate analysis suggested a statistically significant difference in the rate of contralateral ACLRs between groups (P < .05).
Risk Factors for Revision and Contralateral ACLR
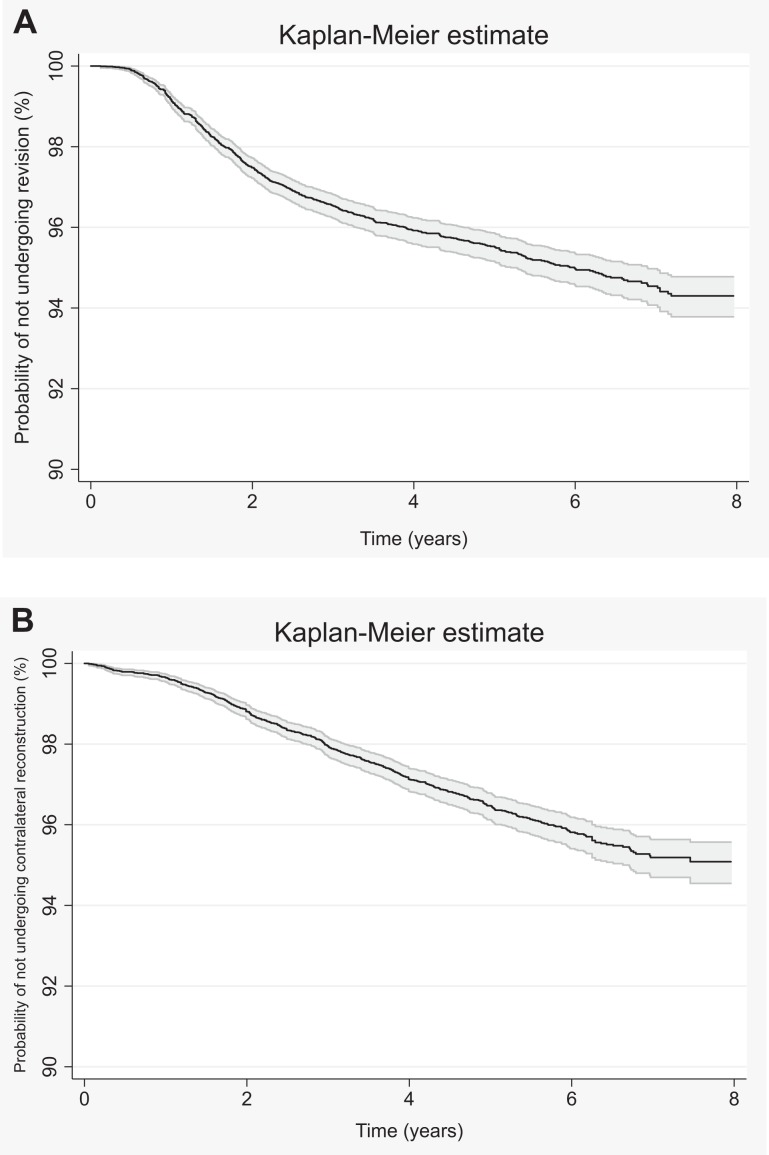
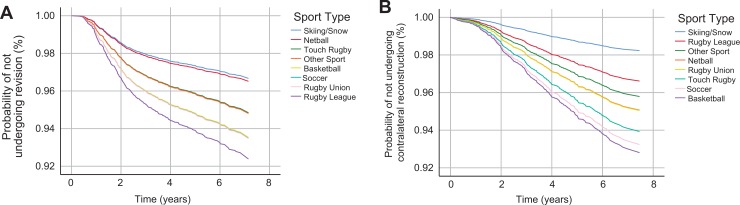
The 5-year ACL graft survival and contralateral knee survival were 95.5% (95% CI, 95.2-95.9) (Figure 1A) and 96.5% (95% CI, 96.1-96.8) (Figure 1B), respectively. On univariate analysis, factors associated with the risk of revision surgery included male sex, young age, and a shorter time from injury to primary surgery (Table 2). On multivariate analysis, associations included male sex (HR, 1.43 [95% CI, 1.22-1.68]; P < .001), age <20 years (<20 vs ≥20 years; HR, 2.68 [95% CI, 2.29-3.12]; P < .001), and shorter time between injury and primary ACLR (<1 vs ≥1 year; HR, 2.05 [95% CI, 1.61-2.63]; P < .001) (Table 3). When analyzing adjusted survival rates, the highest risk sport was rugby league for subsequent revision and basketball for contralateral ACLR (Figure 2).
Figure 1.
(A) Kaplan-Meier probability of not undergoing revision anterior cruciate ligament reconstruction (ACLR) after primary ACLR. (B) Kaplan-Meier probability of not undergoing contralateral ACLR after primary ACLR. Factors entered into model: age, time to surgery, ethnicity, surgeon volume, and sport type.
TABLE 3.
Cox Regression Analysis of Risk Factors for Revision and Contralateral ACLR in Patients Who Underwent Primary ACLRa
| Risk Factor | Revision | Contralateral | ||
|---|---|---|---|---|
| Adjusted HR (95% CI) | P | Adjusted HR (95% CI) | P | |
| Age, y | ||||
| <20 | 2.68 (2.29-3.12) | <.001b | 2.23 (1.85-2.68) | <.001c |
| ≥20 | Reference | Reference | ||
| Sex | ||||
| Male | 1.43 (1.22-1.68) | <.001b | ||
| Female | Reference | |||
| Time to surgery, y | ||||
| <1 | 2.05 (1.61-2.63) | <.001b | 1.35 (1.06-1.73) | .016c |
| ≥1 | Reference | Reference | ||
| Cause of injury | ||||
| Sport | 1.18 (0.98-1.43) | .081 | 1.30 (1.04-1.62) | .021c |
| Not sport | Reference | Reference | ||
| Ethnicity | ||||
| European | Reference | |||
| Maori | 1.35 (1.07-1.69) | .011c | ||
| Pacific | 1.40 (1.08-1.82) | .011c | ||
| Asian | 1.42 (1.00-2.03) | .054 | ||
| Other | 1.36 (0.92-2.02) | .128 | ||
| Surgeon volume, primary ACLR/y | ||||
| ≤10 | Reference | Reference | ||
| 11-30 | 0.81 (0.63-1.03) | .09 | 1.22 (0.91-1.65) | .186 |
| 31-50 | 1.05 (0.83-1.32) | .712 | 1.25 (0.93-1.68) | .141 |
| >50 | 1.20 (0.94-1.52) | .139 | 1.56 (1.16-2.10) | .003c |
aACLR, anterior cruciate ligament reconstruction; HR, hazard ratio.
bStatistically significant risk factor for revision ACLR (P < .05).
cStatistically significant risk factor for contralateral ACLR (P < .05).
Figure 2.
(A) Adjusted Cox regression probability of not undergoing revision anterior cruciate ligament reconstruction (ACLR) after primary ACLR by sport. (B) Adjusted Cox regression probability of not undergoing contralateral ACLR after primary ACLR by sport. Factors entered into model: age, time to surgery, ethnicity, surgeon volume, and sport type.
On multivariate analysis, subsequent contralateral ACLR was associated with age <20 years (<20 vs ≥20 years; HR, 2.23 [95% CI, 1.85-2.68]; P < .001), shorter time from injury to primary surgery (<1 vs ≥ 1 year; HR, 1.35 [95% CI, 1.06-1.73]; P = .016), injuries caused by sport (sport vs not sport; HR, 1.30 [95% CI, 1.04-1.62]; P = .021), Maori and Pacific ethnicities (Maori vs European; HR, 1.35 [95% CI, 1.07-1.69], P = .011) (Pacific vs European; HR, 1.40 [95% CI, 1.08-1.82], P = .011), and higher surgeon volume (>50 vs ≤10 primary ACLR/y; HR, 1.56 [95% CI, 1.16-2.10]; P = .003) (Table 3).
Change of Surgeons for Revision Procedure
Of all cases undergoing revision surgery (n = 676), 44.5% (n = 301) were performed by a different surgeon from primary ACLR (Table 4). On multivariate analysis, change of surgeons was strongly associated with surgeon volume (Table 5). For primary ACLR performed by low-volume surgeons, 75.0% of patients changed surgeons for their revision surgery (≤10 vs >50 primary ACLR/y; HR, 10.70 [95% CI, 6.01-19.05]; P < .001) compared with 59.2% for medium-low–volume surgeons (11-30 vs >50 primary ACLR/y; HR, 5.46 [95% CI, 3.36-8.86]; P < .001), 40.5% for medium-high–volume surgeons (31-50 vs >50 primary ACLR/y; HR, 2.31 [95% CI, 1.47-3.63]; P < .001), and 21.5% for high-volume surgeons (>50 primary ACLR/y). Change of surgeons was also associated with older age (≥20 vs <20 years; HR, 1.47 [95% CI, 1.03-2.09]; P = .033), a longer time between primary and revision surgery (>2 vs ≤2 years; HR, 2.37 [95% CI, 1.67-3.35]; P < .001), Asian ethnicity (Asian vs European; HR, 2.21 [95% CI, 1.04-4.69]; P = .04), and Maori ethnicity (Maori vs European; HR, 2.00 [95% CI, 1.21-3.31]; P = .007) (Table 5).
TABLE 4.
Change of Surgeons Between Primary and Revision ACLRa
| Variable | Total, n | Different Surgeon, n | Same Surgeon, n | % Different Surgeon | P |
|---|---|---|---|---|---|
| Revision ACLR | 676 | 301 | 375 | 44.5 | |
| Sex | |||||
| Male | 458 | 204 | 254 | 44.5 | .991 |
| Female | 218 | 97 | 121 | 44.5 | |
| Age, y | |||||
| <20 | 275 | 107 | 168 | 38.9 | .015b |
| ≥20 | 401 | 194 | 207 | 48.4 | |
| Surgeon volume, primary ACLR/y | |||||
| ≤10 | 104 | 78 | 26 | 75.0 | <.001b |
| 11-30 | 157 | 93 | 64 | 59.2 | |
| 31-50 | 215 | 87 | 128 | 40.5 | |
| >50 | 200 | 43 | 157 | 21.5 | |
| Time between primary and revision ACLR, y | |||||
| ≤2 | 383 | 140 | 243 | 36.6 | <.001b |
| >2 | 293 | 161 | 132 | 55.0 | |
| Ethnicity | |||||
| Maori | 93 | 54 | 39 | 58.0 | .005b |
| European | 424 | 176 | 248 | 41.5 | |
| Pacific | 74 | 33 | 41 | 44.6 | |
| Asian | 37 | 22 | 15 | 59.5 | |
| Other | 36 | 11 | 25 | 30.6 | |
| Unknown | 12 | 5 | 7 | 41.7 |
aACLR, anterior cruciate ligament reconstruction.
bUnivariate analysis suggested a statistically significant difference in the proportion of patients who change surgeons for revision procedures between groups (P < .05).
TABLE 5.
Binary Logistic Regression of Risk Factors for Change of Surgeons in Patients Who Underwent Revision ACLRa
| Risk Factor | Adjusted HR (95% CI) | P |
|---|---|---|
| Age, y | ||
| <20 | Reference | |
| ≥20 | 1.47 (1.03-2.09) | .033b |
| Surgeon volume, primary ACLR/y | ||
| ≤10 | 10.70 (6.01-19.05) | <.001b |
| 11-30 | 5.46 (3.36-8.86) | <.001b |
| 31-50 | 2.31 (1.47-3.63) | <.001b |
| >50 | Reference | |
| Time between primary and revision ACLR, y | ||
| ≤2 | Reference | |
| >2 | 2.37 (1.67-3.35) | <.001b |
| Ethnicity | ||
| European | Reference | |
| Maori | 2.00 (1.21-3.31) | .007b |
| Pacific | 1.23 (0.71-2.13) | .458 |
| Asian | 2.21 (1.04-4.69) | .04b |
| Other | 0.58 (0.26-1.30) | .183 |
aACLR, anterior cruciate ligament reconstruction; HR, hazard ratio.
bMultivariate analysis suggested a statistically significant difference in the proportion of patients who change surgeons for revision procedures between groups (P < .05).
Discussion
This study found that in a large cohort of 15,212 primary ACLR procedures, the 5-year survivorship of the index ACL graft and contralateral ACL were 95.5% and 96.5%, respectively. Male sex, young age, and a shorter period between injury and primary surgery were associated with a higher risk of revision ACLR, whereas young age, a shorter period between injury and primary surgery, sporting activities, and Maori and Pacific ethnicities were risk factors for requiring contralateral ACLR.
Our findings are comparable with those of Maletis et al,15 who found revision and contralateral ACLR rates of 95.1% and 95.8%, respectively, at a mean follow-up period of 2.4 years in 17,436 primary ACLR procedures from the Kaiser Permanente ACLR Registry. Similar to our study, they found a higher risk of revision in male and younger patients.15 Other studies have reported crude rates of approximately 4% for revision ACLR and 5% for contralateral ACLR at 5 years1,12,22 and 3% for both procedures at 2-year follow-up.13,24 The higher risk of revision and contralateral ACLR in male and young patients is a consistent finding in many studies8,9,15,21,22,25 and may represent patients with an increased tendency to return to riskier sports (ie, rugby). Return to sport is associated with an increased risk of graft failure and contralateral ACLR, especially in high-level or high-risk pivoting and cutting sports.1,3,6,8,10,14,19,21,25 Male patients are known to be more likely to attempt to return to sport after ACLR,4 and a study from the United States found that 92% of patients younger than 18 years returned to high-risk sports after ACLR compared with 68% in those older than 25 years.22
Almost half (44.5%) of the revision procedures in this study were performed by a different surgeon from primary ACLR. Change of surgeons was associated with surgeon volume, with patients more likely to change surgeons if their primary ACLR was performed by a lower volume surgeon. While lower volume surgeons may be more likely to make a tertiary referral if revision is required, patients themselves may prefer to seek subspecialist care if a graft fails. If surgeons are unaware that a failure has occurred, they may underestimate their true revision rate, and these data help quantify that potential. While government funded, the ACC functions similar to a private insurance model in which patients are free to see any specialist, requiring only a referral from a health care provider such as a physical therapist. Changing surgeons was also associated with a longer time between primary and revision surgery, which is to be expected, as loss of contact between the patient and original surgeon is more likely over time. Patients may also have moved regions, in which case their choice of health care provider is likely to be driven by accessibility/proximity to a health care facility.23
While some studies have reported that higher volume surgeons have improved outcomes such as lower infection rates, transfusion rates, procedure times, and shorter length of patient hospital stay,11,12,16 we did not find an association between surgeon volume and revision rates. However, we did find that high-volume surgeons had significantly higher rates of contralateral ACLR. This may reflect their having higher-demand patients such as elite athletes, who are potentially at a greater risk of further ACL injuries. While we have no specific data on return-to-play criteria, it is possible that higher volume surgeons may be more aggressive with return to sport, thus increasing the risk to the contralateral ACL, particularly if patients are not properly rehabilitated.
We found that patients with a shorter time from their initial injury to primary ACLR had an increased risk of revision ACLR. This supports the findings of Yabroudi et al,25 who found no association between delay to surgery and the risk of ACL graft ruptures. Rather, it seems likely that patients who are more motivated to return to sport or participate in organized sports (ie, professional, collegiate, or high school sports) seek primary ACLR sooner and on their return are more exposed to further injuries. The relatively long time from injury to ACLR in New Zealand (mean, 449 days) is comparable with rates in Sweden, where the average delay to surgery is between 8 and 24 months, as patients commonly undergo a supervised rehabilitation period before deciding whether to undergo ACLR.1,9
Our study has a number of limitations. First, the ACC does not collect intraoperative surgical and rehabilitation data on important variables that may affect the risk of revision, including graft choice. New Zealand recently instituted a national ACL registry, and future studies will be able to incorporate such variables. Second, we were only able to evaluate the revision risk after ACLR, lacking information on other important outcomes such as functional scores, return to sport, and graft laxity. This likely underestimates the number of clinical failures after ACLR; in particular, we did not capture patients with graft failure who chose not to proceed with revision surgery. Third, we have no way of knowing if patients changed surgeons as a result of a referral from their original surgeon, who may not be comfortable performing revision procedures. This is more likely for lower volume ACLR surgeons and may contribute to the higher percentage of their patients changing surgeons for revision procedures. However, up to 40% of patients changed surgeons even when their primary procedure was performed by a high-volume ACLR surgeon, so surgeons are still likely to underestimate their true revision rate to some degree. Finally, there is no internationally accepted definition for high- or low-volume surgeons, and our definition of high volume as >50 per year was arbitrary.11 Strengths of the study include its large population-based cohort, which makes our findings generalizable to the greater population of patients undergoing ACLR. Data integrity was aided, as in New Zealand it is linked to a patient’s unique NHI number. We were also able to access deidentified clinical data such as operation notes in the case of discrepancies to check for and correct errors in coding or data entry.
Conclusion
In this study of 15,212 primary ACLR procedures, we found revision ACLR to be associated with male sex, age <20 years, and a shorter time from injury to primary ACLR. A high proportion (44.5%) of patients changed surgeons when undergoing a revision procedure. Tertiary referrals between surgeons may account for many instances of change of surgeons; however, in the absence of formal follow-up systems such as registries, surgeons are at risk of underestimating their personal revision rate.
Footnotes
One or more of the authors declared the following potential conflict of interest or source of funding: K.S. received educational support in the form of a scholarship from the University of Auckland to complete this research. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Accident Compensation Corporation Research Ethics Committee.
References
- 1. Ahldén M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40(10):2230–2235. [DOI] [PubMed] [Google Scholar]
- 2. Andriolo L, Filardo G, Kon E, et al. Revision anterior cruciate ligament reconstruction: clinical outcome and evidence for return to sport. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2825–2845. [DOI] [PubMed] [Google Scholar]
- 3. Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure. Am J Sports Med. 2009;37(12):2362–2367. [DOI] [PubMed] [Google Scholar]
- 4. Bourke HE, Salmon LJ, Waller A, Patterson V, Pinczewski LA. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40(9):1985–1992. [DOI] [PubMed] [Google Scholar]
- 5. Buller LT, Best MJ, Baraga MG, Kaplan LD. Trends in anterior cruciate ligament reconstruction in the United States. Orthop J Sports Med. 2015;3(1):2325967114563664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Joint Surg Am. 2017;99(11):897–904. [DOI] [PubMed] [Google Scholar]
- 7. Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport. 2009;12:622–627. [DOI] [PubMed] [Google Scholar]
- 8. Henle P, Bieri KS, Brand M, et al. Patient and surgical characteristics that affect revision risk in dynamic intraligamentary stabilization of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1182–1189. [DOI] [PubMed] [Google Scholar]
- 9. Kvist J, Kartus J, Karlsson J, Forssblad M. Results from the Swedish National Anterior Cruciate Ligament Register. Arthroscopy. 2014;30(7):803–810. [DOI] [PubMed] [Google Scholar]
- 10. Laboute E, Savalli L, Puig P, et al. Analysis of return to competition and repeat rupture for 298 anterior cruciate ligament reconstructions with patellar or hamstring tendon autograft in sportspeople. Ann Phys Rehabil Med. 2010;53(10):598–614. [DOI] [PubMed] [Google Scholar]
- 11. Lau RL, Perruccio AV, Gandhi R, Mahomed NN. The role of surgeon volume on patient outcome in total knee arthroplasty: a systematic review of the literature. BMC Musculoskelet Disord. 2012;13(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Leroux T, Wasserstein D, Dwyer T, et al. The epidemiology of revision anterior cruciate ligament reconstruction in Ontario, Canada. Am J Sports Med. 2014;42(11):2666–2672. [DOI] [PubMed] [Google Scholar]
- 13. Lind M, Menhert F, Pedersen AB. The first results from the Danish ACL reconstruction registry: epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc. 2009;17(2):117–124. [DOI] [PubMed] [Google Scholar]
- 14. Maletis GB, Chen J, Inacio MCS, Love RM, Funahashi TT. Increased risk of revision after anterior cruciate ligament reconstruction with bone–patellar tendon–bone allografts compared with autografts. Am J Sports Med. 2017;45(6):1333–1340. [DOI] [PubMed] [Google Scholar]
- 15. Maletis GB, Inacio MCS, Funahashi TT. Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR Registry. Am J Sports Med. 2015;43(3):641–647. [DOI] [PubMed] [Google Scholar]
- 16. Morche J, Mathes T, Pieper D. Relationship between surgeon volume and outcomes: a systematic review of systematic reviews. Syst Rev. 2016;5(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nordenvall R, Bahmanyar S, Adami J, Stenros C, Wredmark T, Felländer-Tsai L. A population-based nationwide study of cruciate ligament injury in Sweden, 2001-2009: incidence, treatment, and sex differences. Am J Sports Med. 2012;40(8):1808–1813. [DOI] [PubMed] [Google Scholar]
- 18. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948–957. [DOI] [PubMed] [Google Scholar]
- 20. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6):1502–1507. [DOI] [PubMed] [Google Scholar]
- 21. Schlumberger M, Schuster P, Schulz M, et al. Traumatic graft rupture after primary and revision anterior cruciate ligament reconstruction: retrospective analysis of incidence and risk factors in 2915 cases. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1535–1541. [DOI] [PubMed] [Google Scholar]
- 22. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246–251. [DOI] [PubMed] [Google Scholar]
- 23. Victoor A, Delnoij DM, Friele RD, Rademakers JJ. Determinants of patient choice of healthcare providers: a scoping review. BMC Health Serv Res. 2012;12(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wright R, Dunn W, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35(7):1131–1134. [DOI] [PubMed] [Google Scholar]
- 25. Yabroudi MA, Björnsson H, Lynch AD, et al. Predictors of revision surgery after primary anterior cruciate ligament reconstruction. Orthop J Sports Med. 2016;4(9):23259 67116666039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zbrojkiewicz D, Vertullo C, Grayson JE. Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000-2015. Med J Aust. 2018;208(8):354–358. [DOI] [PubMed] [Google Scholar]