Abstract
Background
Galectins constitute a family of β-galactoside-binding proteins, which influence various hallmarks of pancreatic cancer, including cell proliferation, invasion and migration; immune escape; and angiogenesis. Although many studies have concentrated on the role of galectins in pancreatic cancer, the results remain controversial. Hence, we performed a comprehensive meta-analysis to clarify the precise diagnostic and prognostic value of galectins in pancreatic cancer.
Methods
PubMed/MEDLINE, EMBASE and Web of Science were used to search related published literature up to July 2019. Pooled hazard ratios (HRs), diagnostic accuracy variables and related 95% confidence intervals (CIs) were calculated using STATA 14.0 software.
Results
Eleven studies including 1227 participants met our inclusion criteria. High expression of galectin family was not correlated with overall survival (OS) in pancreatic cancer (HR, 1.19; 95% CI 0.67–2.11). According to subgroup analysis, high levels of galectin-1 were significantly correlated with worse OS in pancreatic cancer (HR, 4.77; 95% CI 2.47–9.21), while high levels of tandem-repeat galectins (galectin-4 or galectin-9) predicted both better OS (HR, 0.63; 95% CI 0.46–0.86) and disease-free survival (DFS) (HR, 0.63; 95% CI 0.48–0.83). The expression levels of galectin-3 did not directly correlate with prognosis (HR, 0.99; 95% CI 0.40–2.46). The pooled sensitivity, specificity, positive likelihood ratio, and negative likelihood ratios of galectin-3 were 0.64 (95% CI 0.41–0.82), 0.76 (95% CI 0.59–0.88), 2.70 (95% CI 1.21–6.1), and 0.47 (95% CI 0.23–0.98), respectively. The area under the curve (AUC) of galectin-3 was 0.77.
Conclusion
Taken together, our results suggest that high expression of galectin-1 and low levels of galectin-4 or galectin-9 are predictors of worse prognosis in pancreatic cancer patients. The expression of galectin-3 was not directly related to OS and other clinical characteristics. Although galectin-3 exhibited some diagnostic value in patients with pancreatic cancer in this meta-analysis, clinical application prospects remain to be validated. Further studies are warranted to confirm and strengthen these findings.
Keywords: Galectins, Pancreatic cancer, Prognosis, Diagnosis, Meta-analysis
Background
Pancreatic cancer is among the most aggressive malignancies due to limited early diagnosis and therapeutic strategies, ranking as the fourth leading cause of cancer-related deaths [1, 2]. Despite enormous advances in diagnostic and therapeutic strategies made in many other tumours over the past decades, the prognosis of pancreatic cancer remains unsatisfactory, with a 5-year survival rate of approximately 7% [3, 4]. Most patients with pancreatic cancer are diagnosed at advanced stages, and a lack of effective biomarkers for identifying patients with a high risk for recurrence contributes to poor prognosis.
Galectins constitute a family of multifunctional proteins that share similar β-galactoside-binding affinity and carbohydrate-recognition domains (CRDs) [5]. Galectins are divided into three subtypes (prototype, chimeric and tandem-repeat) based on their structural differences [6]. Prototype galectins (galectin-1, 2, 5, 7, 10, 11, 13, 14 and 15) contain one CRD that can homodimerize. Tandem repeat galectins (galectin-4, 6, 8, 9 and 12) consist of two CRDs that are connected by a linker up to 70 amino acids in length. Chimeric galectin (galectin-3) consists of a single CRD fused to unusual tandem repeats of proline- and glycine-rich short stretches (a total of approximately 120 amino acids) [7]. Eleven galectins have been identified in humans, among which, galectin-1, 3 and 9 have been the most widely studied across different fields [8]. Galectins can be localized both inside and outside of cells. Secreted galectins can crosslink with cell-surface glycoconjugates covered with galactose-containing oligosaccharides to induce intracellular signaling, including mitosis, apoptosis and cell-cycle progression. Intracellular galectins shuttle between the cytoplasm and nucleus to participate in processes such as pre-mRNA splicing [7]. In this review, we will discuss four different galectins. Galectin-1 (LGALS1, 22q13.1) belongs to the prototype galectins, and is usually released from stromal cells and endothelial cells [9]. Galectin-3 (LGALS3, 14q22.3) is the only galectin that belongs to the chimeric galectin, and was first described to be localized to the outer membrane of macrophages (Mac-2 antigen) [10]. It is also found in endothelial cells, immune cells and fibroblasts, and can be transported from the nucleus to the cytoplasm to interact with mitochondria and regulate apoptosis [11, 12]. Galectin-4 (LGALS4, 19q13.2) and galectin-9 (LGALS9, 17q11.2) belong to the tandem repeat type galectins and are involved in inflammatory and immune processes [13, 14]. Recent studies have elucidated the biological functions of galectins in tumors, including in the regulation of oncogenesis, cancer cell growth, apoptosis, cell adhesion, migration and immune escape [8].
Evidence has suggested that altered expression of galectins in pancreatic cancer tissues may have a role in tumour carcinogenesis, proliferation, progression, angiogenesis, metastasis and immune response [15–18]. Recent studies have also raised the possibility of using galectins in diagnostic, prognostic and other clinical characteristics, such as tumour node metastasis (TNM) stage pathological grade [17, 19–28]. Although many studies have concentrated on the correlation between galectins and pancreatic cancer, conclusions remain controversial. Therefore, we performed a comprehensive meta-analysis to clarify the diagnostic and prognostic role of galectins in pancreatic cancer.
Methods
Literature search
We undertook a comprehensive and systematic review by searching following databases, PubMed/MEDLINE, EMBASE and Web of Science. The species were limited to human, and the language was limited to English. The retrieval strategy was listed as follow: (Gal OR galectin OR S-type lectin OR galactose binding lectin OR D galactoside binding lectin OR galaptin OR beta galactoside binding lectin OR half curling element) AND (pancreatic OR pancreas) AND (cancer OR tumour OR tumor OR carcinoma Or adenocarcinoma OR neoplasia OR neoplasm) AND (prognosis OR prognostic OR prognoses OR prognos OR predict OR survival OR outcome OR biomarker OR diagnosis OR diagnostic). Reference lists of literature were manually retrieved for additional information. Studies included in this review are from peer reviewed journals. Two reviewers (Sun QQ and Zhang YY) independently scrutinized the initially identified articles for the assessment of eligibility. The last search time was in June 2019.
Selection criteria
The following inclusion criteria had to be fulfilled: (1) clinical studies of patients with pancreatic cancer; (2) a diagnosis of pancreatic cancer was confirmed by histopathology; (3) explicit methods for the detection of galectins in patients; (4) the cut-off value of galectin expression level was described; (5) studies described the correlation between galectin expression and survival outcome or diagnostic value, and for survival outcome, hazard ratio (HR) values and corresponding 95% confidence intervals (CIs) for overall survival (OS) or disease free survival (DFS) were either described in the studies or could be calculated by the published data; (6) the most recent or the most integrated report would be included when study populations overlapped. Exclusion criteria were as follows: (1) experiments not based in patients; (2) duplicated studies; (3) literature published as abstracts, letters, reviews, case reports, editorials and expert opinions; (4) no full text available or unable to extract the outcome indicators; (5) non-English publications. Any disagreement between the two reviewers was resolved by discussion or consultation with a third reviewer (Liu MQ).
Data extraction
The information extracted from each article were listed as follows: (1) baseline characteristics including first author’s name, publication year, region, sample size, gender and age of the patients, galectin type, TNM stage, treatment and the follow-up duration; (2) method to determine the expression level of galectins and cut-off value; (3) clinical outcomes including OS or DFS and HRs and its 95% CI. If an article only had Kaplan–Meier curves, we extracted survival data from the curves indirectly by Engauge Digitizer software before we put the data into a spreadsheet, called Tierney table to estimate its correlative HRs with 95% CI [29]; (4) diagnostic values including the number of true positives (TPs), false positives (FPs), true negatives (TNs); false negatives (FNs).
Quality assessment
Two reviewers (Sun QQ and Zhang YY) systematically assessed the methodological quality of each study independently using the Newcastle–Ottawa Quality Assessment Scale (NOS) [30], which is primarily used in non-randomized studies. A study with NOS > 5 was regarded as a high-quality study [31]. Additionally, the quality assessment approach reported by Hayden et al. was used to assess the quality of prognostic studies. This scale contains six aspects of measurement, including study participation, study attrition, prognostic factor measurement, outcome measurement, confounding measurement and account, and analysis [32]. Quality Assessment of Studies of Diagnostic Accuracy included in Systematic Reviews (QUADAS-2) was used to assess the methodological quality of diagnosis in this review [33]. Four key domains are included in this criteria: patient selection, index test, reference standard, and flow and timing. Divergence was resolved under discussion or consultation.
Statistics analysis
Hazard ratios (HRs) were used to assess survival data, while odds ratios (ORs) were chosen for dichotomous data with corresponding 95% confidence intervals (CIs). Heterogeneity among studies was evaluated using Cochran’s Q test and Higgins I-squared statistics. The random-effects model was applied under obvious heterogeneity (I2 > 50% and/or P < 0.1); otherwise, the Mantel–Haenszel fixed-effects model was applied [34]. The pooled sensitivity, specificity, positive likelihood ratio (PLR), negative likelihood ratio (NLR), and diagnostic odds ratio (DOR) were calculated with corresponding 95% CIs. The summary receiver operating characteristic curve (SROC), were analysed according to the statistical methods described in a previous study [35]. We used area under the curve (AUC) to summarize diagnostic values. Potential publication bias of prognosis was assessed using Begg’s funnel plot and Egger’s test [36], and bias of diagnosis was evaluated using Deeks’ funnel plot [37]. The potential subgroup analysis was conducted considering the galectin subtype, region and sample size on OS and DFS. All analyses were conducted using STATA version 14.0 (Stata Corporation, College Station, TX, USA) and Review Manager (RevMan) version 5.3. (Cochrane Collaboration, Oxford, UK), and P < 0.05 was considered statistically significant.
Results
Characteristics of included studies
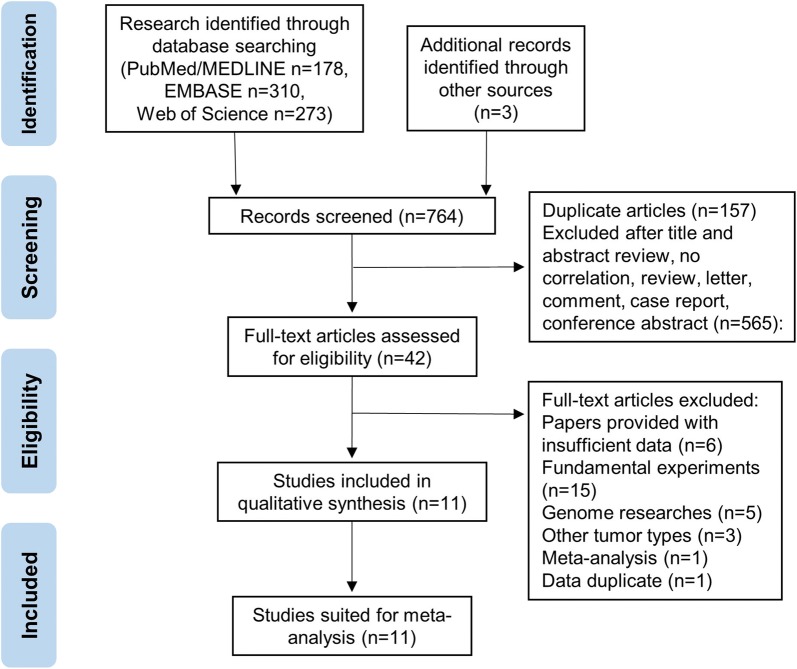
The flow diagram for article selection is illustrated in Fig. 1. We initially retrieved 761 publications from the four databases. 178 articles came from Pubmed/MEDLINE, 310 articles came from EMBASE, and 273 articles came from Web of Science. Then, we added 3 studies identified through other sources. After manually screening titles, abstracts, and keywords and removing duplicates, 42 studies remained for further full-text article assessment. Thirty-one publications were further excluded, among which six papers were excluded due to insufficient data, fifteen papers were fundamental experiments, five were genome research, three were found to be other tumor types, one were meta-analysis and one paper were discovered to be data duplicate. Ultimately, 11 studies comprising 1227 participants were eligible for the meta-analysis on the association between galectins and pancreatic cancer, and detailed information concerning these studies included in prognostic and diagnostic part is summarized in Tables 1 and 2 repectively. All studies were retrospective with publication years ranging from 2002 to 2019. Eight studies with 672 participants were enrolled for prognostic analysis, and all HRs and correlated 95% CIs were obtained using the methods mentioned above. Participants in this meta-analysis were from America, China, France, Germany, Japan, Italy, Netherlands, Sweden, and Taiwan. The cut-off values for galectins varied among the different studies. All pancreatic cancer patients’ diagnoses were confirmed by pathological examination.
Fig. 1.
Literature review process
Table 1.
Summary of the prognosis part of included studies
| Study | Region | Galectin types | Sample size | High expression (%) | Age (mean or median) | Sex (M/F) | Pathology | Stage or grade | Result | Survival analysis | HR (95% CI) | Cutoff value | Sample source | Detection method | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chen [19] | USA | Galactin-1 | 43 | 95 | NR | NR | PDAC | NR | OS | U | 4.90 (1.788–13.426) | Positive cells ≥ 5% | Tissue | IHC | 72 |
| Tang [17] | China | Galactin-1 | 66 | 71.21 | 55 (37–83) | 45/21 | PDAC | TNM I-IV | OS | M | 4.676 (1.963–11.134) | Positive cells > 30% | Tissue | IHC | 78 |
| Shimamura [20] | Japan | Galactin-3 | 104 | 50 | 62 (45–82) | 62/42 | PDAC | TNM I-IV | OS | M | 0.48 (0.28–0.81) | Positive cells ≥ 60% | Tissue | IHC | 104 |
| Gaida [21] | Germany | Galactin-3 | 130 | 80.80 | 66 (39–85) | 74/56 | PDAC | TNM I-IV | OS | KM | 0.85 (0.49–1.47) | Positive cells ≥ 1% | Tissue | IHC | 40 |
| Shimura [24] | Japan | Galactin-3 | 21 | 47.62 | 67.1 | 14/7 | PC | TNM I-III | OS | M | 4.559 (1.176–17.685) | 10.2 ng/ml | Serum | Immunoassay | 66 |
| Maftouh [26] | Italy | Galactin-4 | 20 | 55.00 | NR | 9/11 | PDAC | T3N0(1)Mx | OS | KM | 0.64 (0.25–1.68) | Staining score ≥ median | Tissue | IHC | 45 |
| DFS | KM | 0.87 (0.33–2.26) | |||||||||||||
| Hu [27] | Sweden | Galactin-4 | 140 | 79.30 | 69 (63–73) | 66/74 | PDAC | TNM I–IV | OS | M | 0.636 (0.380–1.063) | Positive cells ≥ 10% | Tissue | IHC | 60 |
| DFS | M | 0.638 (0.371–1.095) | |||||||||||||
| Sideras [28] | Netherlands | Galactin-9 | 148 | 53.30 | NR | NR | PC | Grade I-III | OS | M | 0.62 (0.40–0.97) | 0.4 (out of 3) | Tissue | IHC | 175 |
| DFS | U | 0.6 (0.43–0.85) |
DFS disease-free survival, HR hazard ratio, IHC immunohistochemistry, KM Kaplan–Meier analysis, M/F male/female, M multivariate analysis, NR not reported, OS overall survival, PC pancreatic cancer, PDAC pancreatic ductal adenocarcinoma, U univariate analysis
Table 2.
Characteristics of the diagnosis part of included studies
| Study | Region | Galectin type | Patient | Control | TP | FP | FN | TN | Cutoff value | Sample source | Detection method | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | Age (M) | Sex (M/F) | Pathology | Stage | Number | Age (M) | Sex (M/F) | ||||||||||
| Xie [22] | China | Galactin-3 | 49 | NR | NR | PDAC | TNM I–IV | 88 | NR | NR | 37 | 8 | 12 | 80 | 3.77 ng/ml | Serum | Immunoassay |
| Coppin [23] | France | Galactin-3 | 44 | 64 (41–82) | 22/22 | PDA | TNM I–IV | 58 | 60 (41–89) | 42/16 | 12 | 25 | 32 | 33 | 23.6 ng/ml (male), 27.2 ng/ml (female) | Serum | Immunoassay |
| Shimura [24] | Japan | Galactin-3 | 21 | 67 | 14/7 | PC | TNM I-III | 35 | 55 (25–84) | 20/15 | 18 | 14 | 3 | 21 | 6.2 ng/ml | Serum | Immunoassay |
| Liao [25] | Taiwan | Galactin-3 | 91 | 63 | 58/33 | PC | TNM I–IV | 91 | 59 | 70/21 | 61 | 16 | 30 | 75 | 6.5 ng/ml | Serum | Immunoassay |
Quality assessment
According to NOS, results for the assessment of methodological quality of prognosis are reported in Additional file 1: Table S1, with all studies achieving a score greater than 5. According to the QUADAS-2 analysis, results of the quality assessment of studies included in the diagnostic analysis are shown in Additional file 2: Fig. S1.
Meta-analysis results of prognostic significance
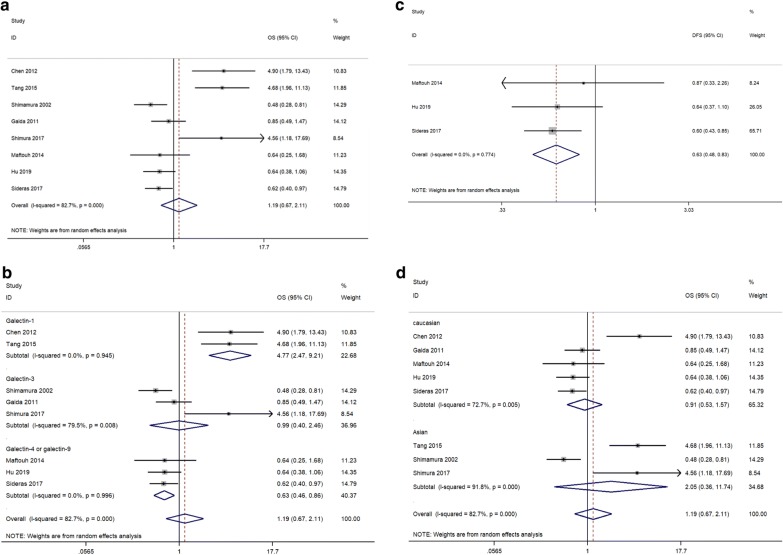
A total of 8 studies were included in the pooled survival analysis of OS. As described in Fig. 2a, results indicated that the galectin family is not correlated with OS in pancreatic cancer (HR, 1.19; 95% CI 0.67–2.11). Due to significant heterogeneity (I2 = 82.7%, p < 0.001), the random-effects model was applied to the analysis, and subgroup analysis were applied to seek for causes of heterogeneity. In the subgroup analysis by subtype of galectins, two studies were conducted in prototype galectins (two of galectin-1), three studies were in chimeric galectins (three of galectin-3), and three studies were in tandem-repeat galectins (two of galectin-4, one of galectin-9). In addition, survival analysis of DFS was conducted in the subgroup of tandem-repeat galectins. The heterogeneity (I2) decreased from 82.7% to 0%–79.5% after subgroup analysis of different galectin subtypes, which indicated that different galectin subtype is among the main cause of heterogeneity. High levels of galectin-1 were significantly correlated with poor OS in pancreatic cancer (HR, 4.77; 95% CI 2.47–9.21, Fig. 2b). Galectin-3 was not correlated with OS in pancreatic cancer (HR, 0.99; 95% CI 0.40–2.46, Fig. 2b). Conversely, high levels of tandem-repeat galectins (galectin-4 or galectin-9) predicted both better OS (HR, 0.63; 95% CI 0.46–0.86, Fig. 2b) and DFS (HR, 0.63; 95% CI 0.48–0.83, Fig. 2c) in pancreatic cancer. In addition, in the subgroup analysis by region, five studies were in Caucasian populations, and three studies were in Asian populations. The significant heterogeneity in different subgroups (Caucasian: HR, 0.91; 95% CI 0.53–1.57, I2 = 72.7%; Asian: HR, 2.05; 95% CI 0.36–11.74, I2 = 91.8%, Fig. 2d) indicated that different regions may not be among the main cause of heterogeneity.
Fig. 2.
Forest plots of OS or DFS in association with galectins in pancreatic cancer. a The overall group. b The subgroup analysis of galectin types on OS. c The subgroup analysis of galectin types on DFS. d The subgroup analysis of dominant ethnicity
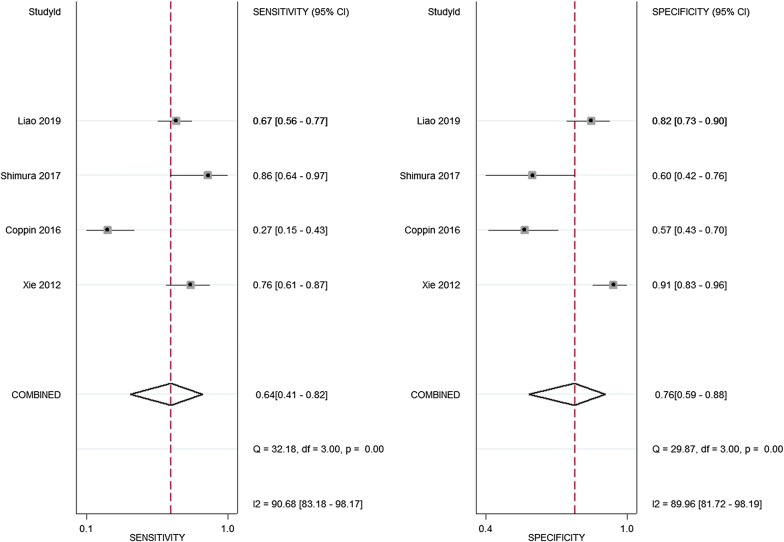
Meta-analysis results of diagnostic value
The characteristics of the studies included for diagnostic analysis are summarized in Table 2. The diagnostic accuracy of galectin-3 was evaluated. The pooled sensitivity of serum galectin-3 was 0.64 (95% CI 0.41–0.82), specificity was 0.76 (95% CI 0.59–0.88), PLR was 2.70 (95% CI 1.21–6.1), and NLR was 0.47 (95% CI 0.23–0.98) (Fig. 3). DOR combines the strengths of sensitivity and specificity, being a measure of the effectiveness of a diagnostic test. The pooled DOR of galectin-3 was 5.93 (95% CI 0.96–36.72, Additional file 2: Fig. S2a). The heterogeneity of these studies was assessed by I2 values of the diagnostic variables. The random-effects model was applied due to the substantial heterogeneity among the studies (I2 for sensitivity 90.68%, p < 0.01; I2 for specificity 89.06, p < 0.001; I2 for DOR 90.68%, p < 0.001). The SROC curve was applied to represent the accuracy of diagnostic testing by combining sensitivity and specificity, with an AUC approaching one reflecting a well-performed and precise diagnosis [38]. In this meta-analysis, the AUC of galectin-3 was 0.77 (95% CI 0.74–0.80, Additional file 2: Fig. S2b).
Fig. 3.
Forest plots of sensitivity and specificity of galectin-3 in pancreatic cancer
Meta-analysis results of for clinical characteristics
We then next undertook a meta-analysis concerning the cooperation between the expression of galectins and clinical characteristics of pancreatic cancer (Table 3). As shown in the table, neither high expression of galectins nor galectin-3 in pancreatic cancer were associated with clinical characteristics.
Table 3.
Correlation of galectins with clinical characteristics
| Clinical characteristics | Galectins | Galectin-3 | ||||||
|---|---|---|---|---|---|---|---|---|
| No. of studies | OR | 95% CI | I2 (P) | No. of studies | OR | 95% CI | I2 (P) | |
| TNM stages III + IV vs. I + II | 5 | 0.529 | 0.252–1.109 | 13.1% (0.327) | 3 | 0.364 | 0.106–1.244 | 21.1% (0.281) |
| Invasion depth T3 + T4 vs. T2 + T1 | 6 | 1.476 | 0.366–5.947 | 75.6% (0.003) | 3 | 0.870 | 0.091–8.301 | 65.3% (0.056) |
| Perineural invasion positive vs. negative | 4 | 1.302 | 0.735–2.304 | 0.0% (0.415) | 1 | 1.226 | 0.350–4.299 | – |
| Vascular invasion positive vs. negative | 2 | 2.135 | 0.514–8.857 | 50.0% (0.157) | 1 | 1.295 | 0.573–2.929 | – |
| Lymphatic invasion positive vs. negative | 6 | 0.902 | 0.501–1.626 | 29.4% (0.215) | 4 | 0.722 | 0.380–1.373 | 0.0% (0.594) |
| Distant metastasis positive vs. negative | 3 | 0.837 | 0.397–1.768 | 0.0% (0.611) | 3 | 0.837 | 0.397–1.768 | 0.0% (0.611) |
| Differentiation grade poor + vs. well + moderate | 5 | 0.791 | 0.256–2.442 | 75.2% (0.003) | 2 | 1.066 | 0.506–2.243 | 0.0% (0.859) |
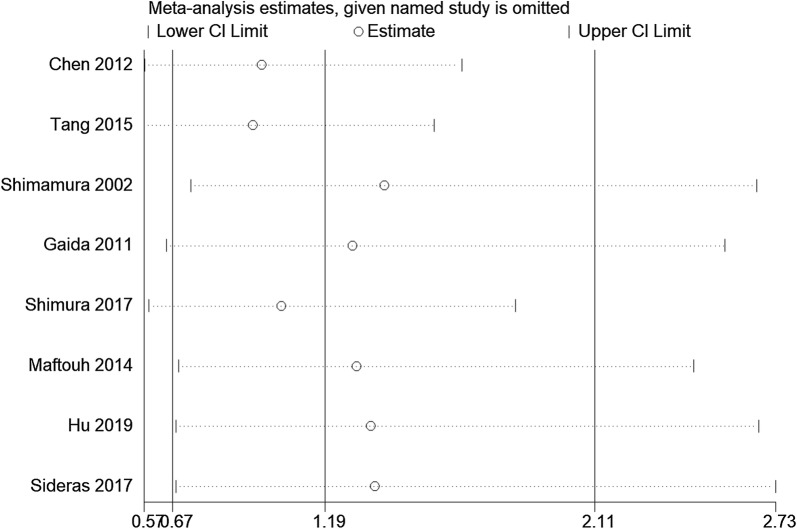
Sensitivity analysis and publication bias
Sensitivity analysis was applied to detect the stability of the pooled HR and its 95% CI, and results indicated that no significant heterogeneity was present among the included studies (Fig. 4). Begg’s funnel plot and Egger’s test were applied to evaluate the publication bias for OS. Begg’s tests showed that publication bias was not significant for the enrolled studies (p = 0.108, Additional file 2: Fig. S3a). However, Egger’s test revealed that publication bias did exist among the studies (p = 0.022). Additionally, Deeks’ tests suggested that there was no significant publication bias for the diagnostic analysis (p = 0.77, Additional file 2: Fig. S3b).
Fig. 4.
Sensitivity analysis of prognosis from the included study
Discussion
Due to the lack of early diagnosis and the poor survival rate after surgery, efforts have been made to identify novel diagnostic and prognostic biomarkers in patients with pancreatic cancer. Carbohydrate antigen 19-9 (CA19-9) is the most widely used serum biomarker for detecting pancreatic cancer. The correlation between CA19-9 and surgical outcomes has been described in many studies and indicates that CA19-9 could assist in identifying resectable or nonresectable pancreatic cancer. However, the thresholds identified in each study were varied [39]. Our team previously conducted a series of relevant studies in this field [40–42]. We found that the serum signature of CEA+/CA125+/CA19-9 > 1000 U/ml was a preoperative indicator for worse surgical outcome in pancreatic cancer, even though the R0-resection was successfully conducted. However, no consensus has been reached on how CA19-9 serum levels change and their predictive value in managing pancreatic cancer patients. A pooled analysis of 6 prospective trials indicated that baseline CA19-9 is prognostic in patients with advanced pancreatic cancer who underwent treatment with gemcitabine-containing regimens. However, reduced CA19-9 after the second cycle of chemotherapy is no longer predictive [43]. Therefore, multiple studies have been conducted to search for novel biomarkers that provide earlier or more accurate prediction for pancreatic cancer.
As part of the lectin superfamily, galectins are soluble proteins widely expressed in a variety of cells, exerting their primary biological functions both intracellularly and extracellularly [44]. In general, galectins are involved in diverse biological process, including regulation of cell signalling, progression of the cell cycle, apoptosis, pre-mRNA splicing and cell motility and adhesion [45, 46]. Consistent with these various biological functions, altered expression levels or dysfunction of galectins have been correlated with the development of diseases, such as cancer. Evidence has suggested the influence of galectins on different hallmarks of pancreatic cancer, including cell proliferation, invasion and migration, immune escape and angiogenesis [17, 47–49]. As a result, therapeutic strategies have been developed that target galectins in pancreatic cancer. Yao et al. suggested that HH1-1, a novel galectin-3 inhibitor, inhibited the progression of pancreatic cancer both in vitro and in vivo [49]. Shih et al. found that combination treatment of paclitaxel and LLS2, a novel galectin-1 inhibitor, enhanced toxicity in human pancreatic cancer cell lines [50]. However, for clinical applications, most clinical trials on galectin inhibitors combined with chemotherapy for the treatment of different tumors were neither withdrawn nor terminated, and only one trial has completed although no results are currently available (NCT00054977). Thus, the use of galectin inhibitors for the treatment of cancer has received renewed interest. Recently, a novel biomarker on the galectin-9 binding partner, T cell immunoglobulin mucin-3 (TIM-3), was found to be upregulated in response to anti-PD-1 therapy and has been targeted as a novel immune checkpoint in tumor immunotherapy [51]. Although these studies are still in their early stages, anti-TIM-3 agents (e.g., TSR-022, LY3321367) combining anti-PD-1/PD-L1 have been applied in several ongoing clinical trials (NCT02817633; NCT03099109), highlighting their promising role for the treatment of advanced solid tumors.
Many studies have also explored the prognostic role of galectins in cancer. Galectins are thought to be associated with patient outcome. Increasing evidence has suggested that galectin-1 is elevated in cancer tissues and a high expression level of galectin-1 is associated with poor OS and DFS in different cancer types, particularly in digestive cancers [19, 52]. Galectin-1 has also been proved to play oncogenic role by some researches in pancreatic cancer. Galectin-1 could regulate acinar-to-ductal metaplasia by promoting Hedgehog pathway signaling in PDAC cells and tumor-stroma crosstalk [16]. Galectin-1 also reportedly enhances the production of stromal cell-derived factor-1via NF-κB signalling, resulting in increased metastasis in pancreatic cancer both in vitro and in vivo [53]. In addition, a novel galectin-1 inhibitor LLS2 was found to potentiate the antitumor effects of paclitaxel in several human cancer cell lines including pancreatic cancer cells in vitro [50]. Consistent with the oncogenic role in pancreatic carcinogenesis, our results indicated that in patients with pancreatic cancer, high levels of galectin-1 were significantly correlated with poor OS, as complements to some previous meta-analysis in solid tumors, demonstrating that higher expression of galectin-1 was associated with worse prognosis in cancers [52], though more excellently-designed large-sized prospective researches are needed in the future.
However, another subtype of galectins, tandem-repeat galectins, seemed to exhibit the opposite picture in prognostic value. Although only limited tumor types were evaluated, higher galectin-9 expression was reported in a meta-analysis to be related to better prognosis in solid tumors especially in digestive cancers [54]. Due to the limited number of studies about galectin-4 and galectin-9, their biological behaviours and underlying mechanisms in malignancies still remain controversy. Galectin-9 was found to suppress the proliferation of pancreatic cancer cell lines, and metastatic liver cancer cell lines [55, 56]. Conversely, higher serum galectin-9 was observed in PDAC patients [57]. Inhibition of galectin-9 leads to significant tumour regression in a mouse model. Mechanistically, dectin-1 binds to galectin-9, resulting in immunogenic or tolerogenic phenotypes of CD4 + and CD8 + T cells that promote tumour progression in pancreatic cancer [58]. Though only a small number of studies have been performed, low expression of galactin-4 has been described to be significantly correlated with early recurrence and poor survival of pancreatic cancer [27]. Reduced expression of galectin-4 was also described in colorectal cancer, skin cancer and prostate cancer [59–62]. Our meta-analysis supported the various function of different galectin subtypes in cancer prognosis, that converse to galectin-1, high levels of galectin-4 or galectin-9 predicted better OS and DFS in pancreatic cancer.
The prognostic role of galectin-3 has been widely studied, but appears to be unclear and disparate between different cancer types. For example, although galectin-3 has been proven to be related to poor survival and play an oncogenic role in many types of cancer, such as ovarian, colorectal, and non-small cell lung cancer [63], high expression of galectin-3 appears to better predict survival in patients with gastric cancer [64]. Alterations in galectin-3 expression have also been reported in previous studies wherein it is implicated in cell proliferation, apoptosis, adhesion, and angiogenesis [65]. Therefore, substantial studies have explored its role in pancreatic cancer, and most studies proved evidence to support its oncogenic role. Overexpressed galectin-3 in pancreatic cancer cells induced cell proliferation and invasion by activating Ras signaling [15]. Silencing of galectin-3 decreased pancreatic cancer cell proliferation and cyclin-D1 levels [66]. Zhao et al. found that inhibition of galectin-3 resulted in smaller tumour size and fewer metastases in a co-implanted murine model of pancreatic cancer cells and pancreatic stellate cells (PSCs). Galectin-3 activates the integrin subunit beta 1 on PSCs, resulting in activated NF-κB through integrin-linked kinase, which influences the transcription of interleukin-8 [67]. The controversial role of galectin-3 in prognosis has been addressed in numerous studies, our present study indicated that galectin-3 showed limited prognostic value, with no direct correlation to OS and clinical characteristics in pancreatic cancer.
One reason for the conflict between the oncogenic mechanism and clinical features may be due to the function of galectins likely being dynamic during tumour progression, which is one part of the balance in the tumour microenvironment. Another reason could be that galectins might only play an important role in a certain group of patients, while a large population covering the small group could potentially lead to negative results. Differences in methodologies among these studies may have caused these controversial results; thus, standardization of the evaluation methods used for galectin expression and proper cut-off points are urgently needed. A consensus needs to be reached on research design and analysis of results in future studies, especially for other types of galectins that are less well studied. These findings provide hints for reconsidering the efficacy of galectin-targeting strategies, and identification of a specific population sensitive to galectins should be performed.
Although novel markers are being evaluated for more accurate prediction, a systematic review on serum tumor markers for the detection of recurrent pancreatic cancer reported that although the biomarker CA 19-9 has certain limitations, it remains the most widely used serum biomarker for postoperative surveillance of pancreatic cancer with a sensitivity and specificity 0.73 and 0.83, respectively [68]. Though galectins alone may not be an effective independent prognostic biomarker for pancreatic cancer compared to the performance of traditional clinical biomarkers such as CA19-9 and carcinoembryonic antigen (CEA) [69], the strategy to combine galectins with other biomarkers is worth consideration. A recent study has shown that the overexpression of galectin-3 and ezrin had stronger predictive value than either alone in cervical cancer [70]. In addition, another study in non-small cell lung cancer observed higher expression of cyclin D1 in galectin-3 free tumor tissues [71]. Similarly, to avoid the limitations of a single predictor, galectin-9 was included in a compelling immune biomarker panel to predict cancer-specific survival in pancreatic cancer, which might also benefit future prospective immunotherapy trials [28]. These results suggest that the potential role of galectins in predicting survival outcomes in cancer patients should not be underestimated and that the combination of biomarkers might be a more powerful prognostic tool.
The search for effective diagnostic serum markers of pancreatic cancer remains intense due to its relatively simple and noninvasive features. Various serum markers with potential diagnostic value have been widely investigated, particularly CA19-9, CA125 and CEA [41, 72]. CA 19-9 is still the most widely used diagnostic marker for pancreatic cancer due to its relatively high diagnostic accuracy, with an AUC reaching nearly 87% [73–75]. However, CA 19-9 is also elevated in some other conditions including other types of cancers as well as nonmalignant pathologies such as pancreatitis and cirrhosis. This has limited the sensitivity and specificity of CA19-9 for early detection. Furthermore, approximately 5–10% patients do not express CA19-9 [39]. Therefore, many studies have focused on the development of novel diagnostic panels to improve diagnostic accuracy based on this marker. Increased levels of circulating galectins have been reported in pancreatic cancer and some other cancer types, which has generated interest in galectins as potential diagnostic markers [76]. Galectin-1 and galectin-3 are intriguing markers for oral squamous cell carcinoma for the screening of higher risk populations [77]. The serum level of galectin-3 could assist as a diagnostic marker in bladder cancer patients [78]. With respect to diagnostic value in pancreatic cancer, our meta-analysis suggested that the pooled DOR of galectin-3 was 5.93, but the 95% CI was 0.96–36.72, indicating an unsatisfactory diagnostic accuracy and substantial heterogeneity. The most probable reason for the heterogeneous diagnostic performance of galectin-3 may be inconsistency in the control groups (healthy volunteer or pancreatitis patients). Some studies have proposed elevated circulating expression of galectin-3 as a potential biomarker for pancreatic cancer, and combined determination of galectin-3, CA19-9, and CA125 provided complementary diagnostic value for pancreatic cancer with a diagnostic sensitivity of 97.5% [22, 79]. However, those studies included a control group of healthy people and ignored patients with pancreatic or liver fibrosis despite the role of galectins in inflammation and collagen production [65]. Another study focused on the diagnostic value of galectin-3 in inflammatory pancreatic disease and indicated that galectin-3 is not an interesting biomarker for the detection of pancreatic adenocarcinoma [23]. Similarly, no significant difference in galectin-3 was observed between cirrhotic and hepatocellular carcinoma patients [80]. Therefore, although elevated galectin-3 has been observed in pancreatic cancer patients, galectin-3 alone might not be a viable diagnostic marker of pancreatic cancer due to its role in inflammatory diseases. Notably recent studies have suggested that the ligands of galectin-3 demonstrated relatively good performance for the diagnosis of cancer [81, 82]. Thus, adding galectin-binding glycoproteins in a galectin-based diagnostic panel might provide a strategy to improve the diagnostic performance of galectins. Hence, these results indicate the potential clinical diagnostic value of galectin-3, although more well-designed studies are needed to reach a definitive conclusion. Combination strategies are worthy of further exploration to improve the diagnostic capability of galectin-3.
Several limitations should be addressed for this meta-analysis. First, this meta-analysis includes a relatively small amount of studies with limited patients, which may have led to insufficient statistical power for analysing the diagnostic and prognostic role of galectins in pancreatic cancer. Second, given the lack of a standard cut-off value for galectins, different cut-off points were applied in the different included studies. Third, some of the HRs with 95% CIs were estimated by data extraction from the survival curves, which might convey certain statistical deviations. Fourth, we found that the different galectins, sample sizes, patient characteristics and cut-off values of the included studies might be potential sources of heterogeneity through subgroup analysis. Fifth, a potential publication bias and flawed methodologic design exists in the smaller studies included in the prognostic analysis. Finally, considering the limitations of the present study, additional well-designed studies with larger sample sizes need to be conducted.
Conclusion
Our current research describes the first meta-analysis to comprehensively and systematically address the prognostic and diagnostic role of galectins in patients with pancreatic cancer. Our meta-analysis found that high expression galectin-1 and a low level of galectin-4 or galectin-9 were associated with worse prognosis, while galectin-3 expression did not show a correlation with prognosis and other clinical characteristics in pancreatic cancer patients. Although galectin-3 exhibited some diagnostic value in patients with pancreatic cancer in this meta-analysis, clinical application prospects remain to be validated.
Supplementary information
Additional file 1: Table S1. Quality assessment of eligible studies with Newcastle–Ottawa Scale.
Additional file 2: Fig. S1. a Risk of bias and applicability concerns; b Risk of bias and applicability concerns. Fig. S2. a Diagnostic odds ratio of galectin-3 for diagnosis of pancreatic cancer; b Summary receiver operating characteristic (SROC) curve for the diagnostic accuracy of galectin-3 for the diagnosis of pancreatic cancer. Fig. S3. Funnel plot for publication bias. a Begg’s funnel plot; b Deeks’ funnel plot.
Acknowledgements
Not applicable.
Abbreviations
- AUC
area under the curve
- CA125
carbohydrate antigen 125
- CA15-3
carbohydrate antigen 15-3
- CA19-9
carbohydrate antigen 19-9
- CEA
carcinoembryonic antigen
- CI
confidence interval
- CRDs
carbohydrate-recognition domains
- DFS
disease free survival
- DOR
diagnostic odds ratio
- FNs
false negatives
- FPs
false positives
- HR
hazard ratio
- NLR
negative likelihood ratio
- OR
odds ratio
- OS
overall survival
- PLR
positive likelihood ratio
- PSCs
pancreatic stellate cells
- SROC
summary receiver operating characteristic curve
- TNM
tumor node metastasis
- TNs
true negatives
- TPs
true positives
Authors’ contributions
YQ, XWX: protocol/project development; QQS, YYZ, MQL: data collection or management; ZY, XJY, QQS: data analysis; QQS, YYZ: manuscript writing/editing. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation (81871950) and the National Science Fund for Distinguished Young Scholars (81625016).
Availability of data and materials
The datasets used in this study are available from the corresponding author upon reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have declared that no competing interest exists.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Qiqing Sun and Yiyin Zhang contributed equally to this article
Contributor Information
Qiqing Sun, Email: sunqiqing@fudanpci.org.
Yiyin Zhang, Email: zhangyiyin@fudanpci.org.
Mengqi Liu, Email: liumengqi@fudanpci.org.
Zeng Ye, Email: yezeng@fudanpci.org.
Xianjun Yu, Email: yuxianjun@fudanpci.org.
Xiaowu Xu, Email: xuxiaowu@fudanpci.org.
Yi Qin, Email: qinyi@fudanpci.org.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12935-019-1025-5.
References
- 1.Hidalgo M. Pancreatic cancer. N Engl J Med. 2010;362:1605–1617. doi: 10.1056/NEJMra0901557. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 3.Petrushnko W, Gundara JS, De Reuver PR, O’Grady G, Samra JS, Mittal A. Systematic review of peri-operative prognostic biomarkers in pancreatic ductal adenocarcinoma. HPB. 2016;18:652–663. doi: 10.1016/j.hpb.2016.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yabar CS, Winter JM. Pancreatic cancer: a review. Gastroenterol Clin North Am. 2016;45:429–445. doi: 10.1016/j.gtc.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Barondes SH, Castronovo V, Cooper DN, Cummings RD, Drickamer K, Feizi T, Gitt MA, Hirabayashi J, Hughes C, Kasai K, et al. Galectins: a family of animal beta-galactoside-binding lectins. Cell. 1994;76:597–598. doi: 10.1016/0092-8674(94)90498-7. [DOI] [PubMed] [Google Scholar]
- 6.Demetter P, Nagy N, Martin B, Mathieu A, Dumont P, Decaestecker C, Salmon I. The galectin family and digestive disease. J Pathol. 2008;215:1–12. doi: 10.1002/path.2334. [DOI] [PubMed] [Google Scholar]
- 7.Liu F-T, Rabinovich GA. Galectins as modulators of tumour progression. Nat Rev Cancer. 2005;5:29–41. doi: 10.1038/nrc1527. [DOI] [PubMed] [Google Scholar]
- 8.Chou FC, Chen HY, Kuo CC, Sytwu HK. Role of galectins in tumors and in clinical immunotherapy. Int J Mol Sci. 2018;19:430. doi: 10.3390/ijms19020430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cousin JM, Cloninger MJ. The role of galectin-1 in cancer progression, and synthetic multivalent systems for the study of galectin-1. Int J Mol Sci. 2016;17:1566. doi: 10.3390/ijms17091566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ho MK, Springer TA. Mac-2, a novel 32,000 Mr mouse macrophage subpopulation-specific antigen defined by monoclonal antibodies. J Immunol. 1982;128:1221–1228. [PubMed] [Google Scholar]
- 11.Takenaka Y, Fukumori T, Yoshii T, Oka N, Inohara H, Kim HR, Bresalier RS, Raz A. Nuclear export of phosphorylated galectin-3 regulates its antiapoptotic activity in response to chemotherapeutic drugs. Mol Cell Biol. 2004;24:4395–4406. doi: 10.1128/MCB.24.10.4395-4406.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brinchmann MF, Patel DM, Iversen MH. The role of galectins as modulators of metabolism and inflammation. Mediators Inflamm. 2018;2018:9186940. doi: 10.1155/2018/9186940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huflejt ME, Leffler H. Galectin-4 in normal tissues and cancer. Glycoconj J. 2003;20:247–255. doi: 10.1023/B:GLYC.0000025819.54723.a0. [DOI] [PubMed] [Google Scholar]
- 14.Heusschen R, Griffioen AW, Thijssen VL. Galectin-9 in tumor biology: a jack of multiple trades. Biochim Et Biophys Acta Rev Cancer. 2013;1836:177–185. doi: 10.1016/j.bbcan.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 15.Song S, Ji B, Ramachandran V, Wang H, Hafley M, Logsdon C, Bresalier RS. Overexpressed galectin-3 in pancreatic cancer induces cell proliferation and invasion by binding Ras and activating Ras signaling. PLoS ONE. 2012;7:e42699. doi: 10.1371/journal.pone.0042699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martinez-Bosch N, Fernandez-Barrena MG, Moreno M, Ortiz-Zapater E, Munne-Collado J, Iglesias M, Andre S, Gabius HJ, Hwang RF, Poirier F, et al. Galectin-1 drives pancreatic carcinogenesis through stroma remodeling and Hedgehog signaling activation. Cancer Res. 2014;74:3512–3524. doi: 10.1158/0008-5472.CAN-13-3013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tang D, Gao J, Wang S, Yuan Z, Ye N, Chong Y, Xu C, Jiang X, Li B, Yin W, et al. Apoptosis and anergy of T cell induced by pancreatic stellate cells-derived galectin-1 in pancreatic cancer. Tumour Biol. 2015;36:5617–5626. doi: 10.1007/s13277-015-3233-5. [DOI] [PubMed] [Google Scholar]
- 18.Orozco CA, Martinez-Bosch N, Guerrero PE, Vinaixa J, Dalotto-Moreno T, Iglesias M, Moreno M, Djurec M, Poirier F, Gabius HJ, et al. Targeting galectin-1 inhibits pancreatic cancer progression by modulating tumor-stroma crosstalk. Proc Natl Acad Sci USA. 2018;115:E3769–E3778. doi: 10.1073/pnas.1722434115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen R, Pan S, Ottenhof NA, de Wilde RF, Wolfgang CL, Lane Z, Post J, Bronner MP, Willmann JK, Maitra A, Brentnall TA. Stromal galectin-1 expression is associated with long-term survival in resectable pancreatic ductal adenocarcinoma. Cancer Biol Ther. 2012;13:899–907. doi: 10.4161/cbt.20842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shimamura T, Sakamoto M, Ino Y, Shimada K, Kosuge T, Sato Y, Tanaka K, Sekihara H, Hirohashi S. Clinicopathological significance of galectin-3 expression in ductal adenocarcinoma of the pancreas. Clin Cancer Res. 2002;8:2570–2575. [PubMed] [Google Scholar]
- 21.Gaida MM, Bach ST, Gunther F, Baseras B, Tschaharganeh DF, Welsch T, Felix K, Bergmann F, Hansch GM, Wente MN. Expression of galectin-3 in pancreatic ductal adenocarcinoma. Pathol Oncol Res. 2012;18:299–307. doi: 10.1007/s12253-011-9444-1. [DOI] [PubMed] [Google Scholar]
- 22.Xie L, Ni WK, Chen XD, Xiao MB, Chen BY, He S, Lu CH, Li XY, Jiang F, Ni RZ. The expressions and clinical significances of tissue and serum galectin-3 in pancreatic carcinoma. J Cancer Res Clin Oncol. 2012;138:1035–1043. doi: 10.1007/s00432-012-1178-2. [DOI] [PubMed] [Google Scholar]
- 23.Coppin L, Benomar K, Corfiotti F, Cattan S, Renaud F, Lapere C, Leteurtre E, Vantyghem MC, Truant S, Pigny P. CA-125, but not galectin-3, complements CA 19-9 for discriminating ductal adenocarcinoma versus non-malignant pancreatic diseases. Pancreatology. 2016;16:115–120. doi: 10.1016/j.pan.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 24.Shimura T, Shibata M, Gonda K, Kofunato Y, Okada R, Ishigame T, Kimura T, Kenjo A, Kono K, Marubashi S. Significance of circulating galectin-3 in patients with pancreatobiliary cancer. Anticancer Res. 2017;37:4979–4986. doi: 10.21873/anticanres.11909. [DOI] [PubMed] [Google Scholar]
- 25.Liao WC, Huang BS, Yu YH, Yang HH, Chen PR, Huang CC, Huang HY, Wu MS, Chow LP. Galectin-3 and S100A9: novel diabetogenic factors mediating pancreatic cancer-associated diabetes. Diabetes Care. 2019;42:1752–1759. doi: 10.2337/dc19-0217. [DOI] [PubMed] [Google Scholar]
- 26.Maftouh M, Belo AI, Avan A, Funel N, Peters GJ, Giovannetti E, Van Die I. Galectin-4 expression is associated with reduced lymph node metastasis and modulation of Wnt/beta-catenin signalling in pancreatic adenocarcinoma. Oncotarget. 2014;5:5335–5349. doi: 10.18632/oncotarget.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hu D, Ansari D, Zhou Q, Sasor A, Said Hilmersson K, Andersson R. Galectin 4 is a biomarker for early recurrence and death after surgical resection for pancreatic ductal adenocarcinoma. Scand J Gastroenterol. 2019;54:95–100. doi: 10.1080/00365521.2018.1561937. [DOI] [PubMed] [Google Scholar]
- 28.Sideras K, Biermann K, Yap K, Mancham S, Boor PPC, Hansen BE, Stoop HJA, Peppelenbosch MP, van Eijck CH, Sleijfer S, et al. Tumor cell expression of immune inhibitory molecules and tumor-infiltrating lymphocyte count predict cancer-specific survival in pancreatic and ampullary cancer. Int J Cancer. 2017;141:572–582. doi: 10.1002/ijc.30760. [DOI] [PubMed] [Google Scholar]
- 29.Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. doi: 10.1186/1745-6215-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 31.Wong WC, Cheung CS, Hart GJ. Development of a quality assessment tool for systematic reviews of observational studies (QATSO) of HIV prevalence in men having sex with men and associated risk behaviours. Emerg Themes Epidemiol. 2008;5:23. doi: 10.1186/1742-7622-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hayden JA, Cote P, Bombardier C. Evaluation of the quality of prognosis studies in systematic reviews. Ann Intern Med. 2006;144:427–437. doi: 10.7326/0003-4819-144-6-200603210-00010. [DOI] [PubMed] [Google Scholar]
- 33.Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 34.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Walter SD. Properties of the summary receiver operating characteristic (SROC) curve for diagnostic test data. Stat Med. 2002;21:1237–1256. doi: 10.1002/sim.1099. [DOI] [PubMed] [Google Scholar]
- 36.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 2005;58:882–893. doi: 10.1016/j.jclinepi.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 38.Rosman AS, Korsten MA. Application of summary receiver operating characteristics (sROC) analysis to diagnostic clinical testing. Adv Med Sci. 2007;52:76–82. [PubMed] [Google Scholar]
- 39.Goggins M. Molecular markers of early pancreatic cancer. J Clin Oncol. 2005;23:4524–4531. doi: 10.1200/JCO.2005.19.711. [DOI] [PubMed] [Google Scholar]
- 40.Luo G, Xiao Z, Long J, Liu Z, Liu L, Liu C, Xu J, Ni Q, Yu X. CA125 is superior to CA19-9 in predicting the resectability of pancreatic cancer. J Gastrointest Surg. 2013;17:2092–2098. doi: 10.1007/s11605-013-2389-9. [DOI] [PubMed] [Google Scholar]
- 41.Liu L, Xu H, Wang W, Wu C, Chen Y, Yang J, Cen P, Xu J, Liu C, Long J, et al. A preoperative serum signature of CEA+/CA125+/CA19-9≥ 1000 U/ml indicates poor outcome to pancreatectomy for pancreatic cancer. Int J Cancer. 2015;136:2216–2227. doi: 10.1002/ijc.29242. [DOI] [PubMed] [Google Scholar]
- 42.Chen T, Zhang MG, Xu HX, Wang WQ, Liu L, Yu XJ. Preoperative serum CA125 levels predict the prognosis in hyperbilirubinemia patients with resectable pancreatic ductal adenocarcinoma. Medicine. 2015;94:e751. doi: 10.1097/MD.0000000000000751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bauer TM, El-Rayes BF, Li X, Hammad N, Philip PA, Shields AF, Zalupski MM, Bekaii-Saab T. Carbohydrate antigen 19-9 is a prognostic and predictive biomarker in patients with advanced pancreatic cancer who receive gemcitabine-containing chemotherapy: a pooled analysis of 6 prospective trials. Cancer. 2013;119:285–292. doi: 10.1002/cncr.27734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Compagno D, Jaworski FM, Gentilini L, Contrufo G, Gonzalez Perez I, Elola MT, Pregi N, Rabinovich GA, Laderach DJ. Galectins: major signaling modulators inside and outside the cell. Curr Mol Med. 2014;14:630–651. doi: 10.2174/1566524014666140603101953. [DOI] [PubMed] [Google Scholar]
- 45.Liu FT, Patterson RJ, Wang JL. Intracellular functions of galectins. Biochim Biophys Acta. 2002;1572:263–273. doi: 10.1016/S0304-4165(02)00313-6. [DOI] [PubMed] [Google Scholar]
- 46.Elola MT, Wolfenstein-Todel C, Troncoso MF, Vasta GR, Rabinovich GA. Galectins: matricellular glycan-binding proteins linking cell adhesion, migration, and survival. Cell Mol Life Sci. 2007;64:1679–1700. doi: 10.1007/s00018-007-7044-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Song S, Ji B, Ramachandran V, Mazurek N, Wang H, Logsdon CD, Bresalier RS. Galectin-3 induces cell proliferation and invasion by binding K-RAS and activating RAS signaling in pancreatic cancer cells. Gastroenterology. 2010;138:S448. doi: 10.1371/journal.pone.0042699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Berberat PO, Friess H, Wang L, Zhu Z, Bley T, Frigeri L, Zimmermann A, Buchler MW. Comparative analysis of galectins in primary tumors and tumor metastasis in human pancreatic cancer. J Histochem Cytochem. 2001;49:539–549. doi: 10.1177/002215540104900414. [DOI] [PubMed] [Google Scholar]
- 49.Yao Y, Zhou L, Liao W, Chen H, Du Z, Shao C, Wang P, Ding K. HH1-1, a novel galectin-3 inhibitor, exerts anti-pancreatic cancer activity by blocking galectin-3/EGFR/AKT/FOXO3 signaling pathway. Carbohydr Polym. 2019;204:111–123. doi: 10.1016/j.carbpol.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 50.Shih TC, Liu R, Fung G, Bhardwaj G, Ghosh PM, Lam KS. A novel galectin-1 inhibitor discovered through one-bead two-compound library potentiates the antitumor effects of paclitaxel in vivo. Mol Cancer Ther. 2017;16:1212–1223. doi: 10.1158/1535-7163.MCT-16-0690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Koyama S, Akbay EA, Li YY, Herter-Sprie GS, Buczkowski KA, Richards WG, Gandhi L, Redig AJ, Rodig SJ, Asahina H, et al. Adaptive resistance to therapeutic PD-1 blockade is associated with upregulation of alternative immune checkpoints. Nat Commun. 2016;7:10501. doi: 10.1038/ncomms10501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wu R, Wu T, Wang K, Luo S, Chen Z, Fan M, Xue D, Lu H, Zhuang Q, Xu X. Prognostic significance of galectin-1 expression in patients with cancer: a meta-analysis. Cancer Cell Int. 2018;18:108. doi: 10.1186/s12935-018-0607-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Qian D, Lu Z, Xu Q, Wu P, Tian L, Zhao L, Cai B, Yin J, Wu Y, Staveley-O’Carroll KF, et al. Galectin-1-driven upregulation of SDF-1 in pancreatic stellate cells promotes pancreatic cancer metastasis. Cancer Lett. 2017;397:43–51. doi: 10.1016/j.canlet.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 54.Wang K, Chen Z, Wu R, Yin J, Fan M, Xu X. Prognostic role of high gal-9 expression in solid tumours: a meta-analysis. Cell Physiol Biochem. 2018;45:993–1002. doi: 10.1159/000487294. [DOI] [PubMed] [Google Scholar]
- 55.Tadokoro T, Fujihara S, Chiyo T, Oura K, Samukawa E, Yamana Y, Fujita K, Mimura S, Sakamoto T, Nomura T, et al. Induction of apoptosis by galectin-9 in liver metastatic cancer cells: in vitro study. Int J Oncol. 2017;51:607–614. doi: 10.3892/ijo.2017.4053. [DOI] [PubMed] [Google Scholar]
- 56.Okura R, Fujihara S, Iwama H, Morishita A, Chiyo T, Watanabe M, Hirose K, Kobayashi K, Fujimori T, Kato K, et al. MicroRNA profiles during galectin-9-induced apoptosis of pancreatic cancer cells. Oncol Lett. 2018;15:407–414. doi: 10.3892/ol.2017.7316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tavares LB, Silva-Filho AF, Martins MR, Vilar KM, Pitta MGR, Rego M. Patients with pancreatic ductal adenocarcinoma have high serum galectin-9 levels: a sweet molecule to keep an eye on. Pancreas. 2018;47:e59–e60. doi: 10.1097/MPA.0000000000001126. [DOI] [PubMed] [Google Scholar]
- 58.Daley D, Mani VR, Mohan N, Akkad N, Ochi A, Heindel DW, Lee KB, Zambirinis CP, Pandian GSB, Savadkar S, et al. Dectin 1 activation on macrophages by galectin 9 promotes pancreatic carcinoma and peritumoral immune tolerance. Nat Med. 2017;23:556–567. doi: 10.1038/nm.4314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Satelli A, Rao PS, Thirumala S, Rao US. Galectin-4 functions as a tumor suppressor of human colorectal cancer. Int J Cancer. 2011;129:799–809. doi: 10.1002/ijc.25750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cada Z, Smetana K, Jr, Lacina L, Plzakova Z, Stork J, Kaltner H, Russwurm R, Lensch M, Andre S, Gabius HJ. Immunohistochemical fingerprinting of the network of seven adhesion/growth-regulatory lectins in human skin and detection of distinct tumour-associated alterations. Folia Biol (Praha) 2009;55:145–152. [PubMed] [Google Scholar]
- 61.Laderach DJ, Gentilini LD, Giribaldi L, Delgado VC, Nugnes L, Croci DO, Al Nakouzi N, Sacca P, Casas G, Mazza O, et al. A unique galectin signature in human prostate cancer progression suggests galectin-1 as a key target for treatment of advanced disease. Cancer Res. 2013;73:86–96. doi: 10.1158/0008-5472.CAN-12-1260. [DOI] [PubMed] [Google Scholar]
- 62.Thijssen VL, Heusschen R, Caers J, Griffioen AW. Galectin expression in cancer diagnosis and prognosis: a systematic review. Biochim Biophys Acta. 2015;1855:235–247. doi: 10.1016/j.bbcan.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 63.Wang Y, Liu S, Tian Y, Wang Y, Zhang Q, Zhou X, Meng X, Song N. Prognostic role of galectin-3 expression in patients with solid tumors: a meta-analysis of 36 eligible studies. Cancer Cell Int. 2018;18:172. doi: 10.1186/s12935-018-0668-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Long B, Yu Z, Zhou H, Ma Z, Ren Y, Zhan H, Li L, Cao H, Jiao Z. Clinical characteristics and prognostic significance of galectins for patients with gastric cancer: a meta-analysis. Int J Surg. 2018;56:242–249. doi: 10.1016/j.ijsu.2018.06.033. [DOI] [PubMed] [Google Scholar]
- 65.Song L, Tang JW, Owusu L, Sun MZ, Wu J, Zhang J. Galectin-3 in cancer. Clin Chim Acta. 2014;431:185–191. doi: 10.1016/j.cca.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 66.Merlin J, Stechly L, de Beauce S, Monte D, Leteurtre E, van Seuningen I, Huet G, Pigny P. Galectin-3 regulates MUC1 and EGFR cellular distribution and EGFR downstream pathways in pancreatic cancer cells. Oncogene. 2011;30:2514–2525. doi: 10.1038/onc.2010.631. [DOI] [PubMed] [Google Scholar]
- 67.Zhao W, Ajani JA, Sushovan G, Ochi N, Hwang R, Hafley M, Johnson RL, Bresalier RS, Logsdon CD, Zhang Z, Song S. Galectin-3 mediates tumor cell-stroma interactions by activating pancreatic stellate cells to produce cytokines via integrin signaling. Gastroenterology. 2018;154(1524–1537):e1526. doi: 10.1053/j.gastro.2017.12.014. [DOI] [PubMed] [Google Scholar]
- 68.Daamen LA, Groot VP, Heerkens HD, Intven MPW, van Santvoort HC, Molenaar IQ. Systematic review on the role of serum tumor markers in the detection of recurrent pancreatic cancer. HPB. 2018;20:297–304. doi: 10.1016/j.hpb.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 69.Wu L, Huang P, Wang F, Li D, Xie E, Zhang Y, Pan S. Relationship between serum CA19-9 and CEA levels and prognosis of pancreatic cancer. Ann Transl Med. 2015;3:328. doi: 10.3978/j.issn.2305-5839.2015.11.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Li M, Feng YM, Fang SQ. Overexpression of ezrin and galectin-3 as predictors of poor prognosis of cervical cancer. Braz J Med Biol Res. 2017;50:e5356. doi: 10.1590/1414-431X20165356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kosacka M, Piesiak P, Kowal A, Golecki M, Jankowska R. Galectin-3 and cyclin D1 expression in non-small cell lung cancer. J Exp Clin Cancer Res. 2011;30:101. doi: 10.1186/1756-9966-30-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Benini L, Cavallini G, Zordan D, Rizzotti P, Rigo L, Brocco G, Perobelli L, Zanchetta M, Pederzoli P, Scuro LA. A clinical evaluation of monoclonal (CA19-9, CA50, CA12-5) and polyclonal (CEA, TPA) antibody-defined antigens for the diagnosis of pancreatic cancer. Pancreas. 1988;3:61–66. doi: 10.1097/00006676-198802000-00011. [DOI] [PubMed] [Google Scholar]
- 73.Yang Y, Yan S, Tian H, Bao Y. Macrophage inhibitory cytokine-1 versus carbohydrate antigen 19-9 as a biomarker for diagnosis of pancreatic cancer: a PRISMA-compliant meta-analysis of diagnostic accuracy studies. Medicine (Baltimore). 2018;97:e9994. doi: 10.1097/MD.0000000000009994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chan A, Prassas I, Dimitromanolakis A, Brand RE, Serra S, Diamandis EP, Blasutig IM. Validation of biomarkers that complement CA19.9 in detecting early pancreatic cancer. Clin Cancer Res. 2014;20:5787–5795. doi: 10.1158/1078-0432.CCR-14-0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Huang Z, Liu F. Diagnostic value of serum carbohydrate antigen 19-9 in pancreatic cancer: a meta-analysis. Tumour Biol. 2014;35:7459–7465. doi: 10.1007/s13277-014-1995-9. [DOI] [PubMed] [Google Scholar]
- 76.Gui JC, Yan WL, Liu XD. CA19-9 and CA242 as tumor markers for the diagnosis of pancreatic cancer: a meta-analysis. Clin Exp Med. 2014;14:225–233. doi: 10.1007/s10238-013-0234-9. [DOI] [PubMed] [Google Scholar]
- 77.Aggarwal S, Sharma SC, Das SN. Galectin-1 and galectin-3: plausible tumour markers for oral squamous cell carcinoma and suitable targets for screening high-risk population. Clin Chim Acta. 2015;442:13–21. doi: 10.1016/j.cca.2014.12.038. [DOI] [PubMed] [Google Scholar]
- 78.El Gendy H, Madkour B, Abdelaty S, Essawy F, Khattab D, Hammam O, El Kholy A, Nour HH. Galectin 3 for the diagnosis of bladder cancer. Arab J Urol. 2014;12:178–181. doi: 10.1016/j.aju.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Iurisci I, Tinari N, Natoli C, Angelucci D, Cianchetti E, Iacobelli S. Concentrations of galectin-3 in the sera of normal controls and cancer patients. Clin Cancer Res. 2000;6:1389–1393. [PubMed] [Google Scholar]
- 80.Eisa NH, Ebrahim MA, Ragab M, Eissa LA, El-Gayar AM. Galectin-3 and matrix metalloproteinase-9: perspective in management of hepatocellular carcinoma. J Oncol Pharm Pract. 2015;21:323–330. doi: 10.1177/1078155214532698. [DOI] [PubMed] [Google Scholar]
- 81.Paret C, Hildebrand D, Weitz J, Kopp-Schneider A, Kuhn A, Beer A, Hautmann R, Zoller M. C4.4A as a candidate marker in the diagnosis of colorectal cancer. Br J Cancer. 2007;97:1146–1156. doi: 10.1038/sj.bjc.6604012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Greco C, Vona R, Cosimelli M, Matarrese P, Straface E, Scordati P, Giannarelli D, Casale V, Assisi D, Mottolese M, et al. Cell surface overexpression of galectin-3 and the presence of its ligand 90k in the blood plasma as determinants in colon neoplastic lesions. Glycobiology. 2004;14:783–792. doi: 10.1093/glycob/cwh092. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Quality assessment of eligible studies with Newcastle–Ottawa Scale.
Additional file 2: Fig. S1. a Risk of bias and applicability concerns; b Risk of bias and applicability concerns. Fig. S2. a Diagnostic odds ratio of galectin-3 for diagnosis of pancreatic cancer; b Summary receiver operating characteristic (SROC) curve for the diagnostic accuracy of galectin-3 for the diagnosis of pancreatic cancer. Fig. S3. Funnel plot for publication bias. a Begg’s funnel plot; b Deeks’ funnel plot.
Data Availability Statement
The datasets used in this study are available from the corresponding author upon reasonable request.