Abstract
Background
The transmissible forms of Plasmodium parasites result from a process of sporogony that takes place inside their obligatory mosquito vector and culminates in the formation of mammalian-infective parasite forms. Ivermectin is a member of the avermectin family of endectocides, which has been proposed to inhibit malaria transmission due its insecticidal effect. However, it remains unclear whether ivermectin also exerts a direct action on the parasite’s blood and transmission stages.
Methods
We employed a rodent model of infection to assess the impact of ivermectin treatment on P. berghei asexual and sexual blood forms in vivo. We then made use of a newly established luminescence-based methodology to evaluate the activity of ivermectin and other avermectins against the sporogonic stages of P. berghei parasites in vitro independent of their role on mosquito physiology.
Results
Our results show that whereas ivermectin does not affect the parasite’s parasitemia, gametocytemia or exflagellation in the mammalian host, several members of the avermectin family of compounds exert a strong inhibitory effect on the generation and development of P. berghei oocysts.
Conclusions
Our results shed light on the action of avermectins against Plasmodium transmission stages and highlight the potential of these compounds to help prevent the spread of malaria.
Keywords: Plasmodium, Malaria transmission, Avermectins, Ivermectin
Background
Malaria is a parasitic disease caused by Plasmodium parasites that are transmitted to their mammalian hosts by the bites of infected female Anopheles mosquitoes. In 2017, an estimated 435,000 deaths were attributed to malaria, 80% of which occurred in the regions of Africa and India and 61% of which in children under the age of 5. Although the number of malaria cases decreased from 2010, progress appears to have stalled, and a small increase in the global number of cases was actually observed in recent years [1].
Plasmodium sporozoites are injected by infected Anopheles mosquitoes into a mammalian host, homing to the liver, where they replicate into thousands of blood-infective merozoites [2].While most merozoites cyclically invade red blood cells, leading to disease [3], some differentiate into female and male gametocytes, which can be uptaken by mosquitoes [4]. Inside the mosquito midgut, gametocytes differentiate into female and male gametes that fuse forming zygotes [5]. In rodent P. berghei parasites, zygotes transform into ookinetes within 18–24 h, penetrating the mosquito’s midgut wall, and developing into oocysts 48 h after the blood meal [6, 7]. Over 10–14 days, oocysts mature in the basal lamina of the midgut wall, forming sporozoites which are eventually released and migrate to the mosquito salivary glands, where they remain ready to initiate a new mammalian infection [4, 8, 9].
The complexity of the Plasmodium parasite’s life cycle constitutes one of the biggest hurdles in the fight against malaria. So far, the most successful strategies to reduce the number of cases of malaria result from a combination of vector control strategies, and artemisinin combination therapies (ACT) that target the symptomatic blood stage of infection [1]. However, the emergence of mosquito resistance to insecticides and of parasite resistance to antimalarial drugs severely threaten the efficacy of such measures [1, 10]. Therefore, the identification of new compounds that have a broad spectrum of action, long half-life and strong inhibitory activity remains a priority in the fight against malaria.
Avermectins are a class of macrocyclic lactones with insecticidal and antiparasitic properties. They are the most effective and well-developed class of endectocides, and are active against both endo- and ectoparasites [11]. Ivermectin, the best studied semi-synthetic derivate of avermectin, has been considered one of the most successful discoveries in the fight against infections caused by roundworm parasites [12]. Mass drug administration (MDA) of ivermectin in Africa and Latin America led to a reduction of onchocerciasis, as well as of lymphatic filariasis and scabies, which are also endemic in India and Southeast Asia [12–14]. The impact of ivermectin on insect vectors [12, 13], in particular its activity against Anopheles mosquitoes [15, 16] prompted the investigation of its action against Plasmodium parasites, towards harnessing its potential use as an integrated tool for malaria control [17, 18]. We have recently reported on ivermectin activity against Plasmodium liver stages in vivo [19]. However, discrepant results have emerged from several other studies aimed at assessing the impact of ivermectin on the blood and mosquito stages of the Plasmodium life-cycle [20–25]. Whereas results obtained by Nasveld et al. [20] indicated that ivermectin displays very low activity against P. falciparum blood stages in vitro, Panchal et al. [22] suggested that ivermectin inhibits the parasite’s blood stage development by blocking nucleo-cytoplasmic shuttling of P. falciparum signal recognition particle (SRP) components. This is in agreement with a recent study that demonstrated an impairment of sexual and asexual stages of P. falciparum development in vitro [25]. On the other hand, ivermectin was reported to reduce oocyst prevalence and intensity in different mosquito species infected with P. falciparum [21], contrary to reports by Kobylinski et al. [23] and Pinilla et al. [24], who did not observe a reduction on oocyst intensity, i.e. the number of oocysts per mosquito, but rather a decrease on oocyst prevalence (the proportion of mosquitoes harbouring oocysts), for P. vivax and P. falciparum.
The present study aimed to clarify the impact of ivermectin on P. berghei blood stages in vivo, as well as to assess the impact of ivermectin and other avermectins on the parasite’s mosquito stages in vitro.
Methods
Experimental animals and P. berghei ANKA reference lines
Male BALB/cByJ mice (6–8 weeks-old) purchased from Charles River Laboratories Inc. (Lyon, France) were used. Two parasite lines were employed in the experimental work, a transgenic parasite line termed PbCSGFP-Luc (RMgm-152),which expresses the fusion gene gfp-luc under the control of the csp promotor (PBANKA_0403200) integrated into the silent 230p gene locus (PBANKA_0306000) [26], and the transgenic parasite line PbFluo-frmg (RMgm-164), which expresses GFP under control of the ‘male gametocyte-specific’ promoter of PB000791.03.0 (dynein heavy chain, putative) and RFP under the control of the ‘female gametocyte-specific’ promoter PB000504.02.0 (LCCL domain-containing protein CCP2). The rfp and gfp genes are integrated into the genome in the 230p locus (PBANKA_0306000) [27].
Ookinete production
Plasmodium berghei ANKA expressing green fluorescent protein (GFP) and luciferase under the control of the circumsporozoite protein (CSP) promoter (line 784cl1, RMgm-152, PbCSPGFP-Luc) was maintained in Anopheles stephensi mosquitoes and BALB/cByJ mice. To maintain gametocyte infectivity, only up to six passages of parasites from infected to naïve mice were performed. Ookinete in vitro production was performed as previously described [26]. Briefly, BALB/cByJ mice were treated with 0.1 ml phenylhydrazine (25 mg/ml) 3 days prior to infection with 107 P. berghei-infected red blood cells (iRBC) obtained from a donor mouse. On the third day after infection, gametocytemia was monitored by light microscopy for the presence of exflagellating gametocytes in ookinete medium (1:4 dilution). Blood collected by heart puncture was pooled from 2 mice and washed with RPMI at 37 °C, followed by centrifugation at 1100×g for 10 min at 37 °C. After washing, 5 μl of blood containing exflagellating gametocytes was mixed with medium supplemented for ookinete formation [RPMI1640 (Sigma-Aldrich, Saint Louis, USA), 25 mM HEPES, 0.4 mM hypoxanthine, 100 mM xanthurenic acid (85570, Fluka, Saint Gallen, Switzerland), 10% FBS (pH 7.6)] in a final volume of 200 μl, and cultured in 96-well plates for 24 h at 19 °C. Additionally, blood containing exflagellating gametocytes was mixed with the ookinete medium in 1:20 ratio and cultured in T75 flasks for 22–24 h at 19 °C. Following incubation, ookinete enrichment was performed as previously described [26], with some modifications. Briefly, cultured blood was collected, and erythrocytes were lysed for 15 min on ice with 30 volumes of ice-cold 0.17 M ammonium chloride. Lysed erythrocytes were removed by washing with RPMI, and ookinetes were purified by centrifugation on a 63% Nycodenz cushion at 650×g at 4 °C for 30 min. Following centrifugation, the ookinete-containing interface was collected, washed in ice-cold RPMI and resuspended in 0.5–1.0 ml of oocyst medium.
Oocyst cultures
Purified ookinetes were seeded with Drosophila melanogaster S2 cells (Drosophila Genomics Resource Center, Bloomington, USA) in a 1:10 ratio (104 ookinetes and 105 S2 cells) in Schneider’s medium (S0146, Sigma-Aldrich) supplemented with 15% FBS, penicillin/streptomycin (50 U/ml, 50 µg/ml) and gentamicin (50 µg/ml) to promote oocyst development. Oocysts were co-cultured with D. melanogaster S2 cells in flat bottom 96-well plates (Corning, New York, USA) for up to 15 days at 19 °C. One-quarter of the medium was changed 3 times per week (every 48 to 72 h), and 105 S2 cells were added once per week. In parallel, S2 cells were maintained at 27 °C in Schneider’s medium (S0146, Sigma-Aldrich) supplemented with 10% FBS and penicillin/streptomycin (50 U/ml, 50 µg/ml).
Bioluminescence assay
A bioluminescence assay was used to assess the development of the mosquito stages of PbCSGFP-Luc. In order to evaluate the effect of compounds on the development of the parasite’s mosquito stages, samples were collected at 3 different time points to determine the effect on ookinete and oocyst formation, and oocyst maturation, as previously described [26]. The bioluminescence assay was performed using the Firefly Luciferase Assay Kit (Biotium, Hayward, USA) according to the manufacturer’s instructions, with some modifications. Briefly, the whole well contents were collected and spun down, washed with PBS, frozen in 50 µl of lysis buffer (1:5 ratio) and stored at − 20 °C until further use. Collected samples were lysed and 30 µl of the resulting supernatant were transferred into white 96-well plates. Fifty µl of D-luciferin in Firefly luciferase assay buffer (1:50 ratio) were added to the samples and parasite load was determined by measuring luminescence intensity using a microplate reader (Tecan Infinite M200, Zurich, Switzerland).
Evaluation of the in vivo activity of ivermectin
In order to assess the in vivo activity of Iv, five BALB/cByJ (Charles River) mice per experimental group were infected by intraperitoneal injection of 107 P. berghei Fluo-frmg-infected red blood cells. Parasitaemia and gametocyteamia were measured the following days by flow cytometry analysis of 4 µl of tail blood. Blood was collected in 200 µl of PBS and 100 µl stored at 4 °C, while the remaining was transferred to 100 µl of PBS containing 1.25 mM of red fluorescent nucleic acid stain Syto®61 (Thermo Fisher Scientific, Waltham, USA) and incubated for 20 min at room temperature in the dark. The samples were analysed on a LSRFortessa X-20 flow cytometer (Becton, Dickinson and Co., New Jersey, USA). Female and male gametocytes were gated based on the analysis of GFP and Red Fluorescence Protein (RFP) fluorescence, and parasitemia was estimated based on the analysis of Syto®61 and forward scatter. The positive cell population was determined by comparison of infected blood samples with an uninfected blood sample. Results were then analysed with the FlowJoTM Software (Version 10, FlowJoTM Software, Ashland, USA). Exflagellation was also monitored every day, until parasitemia reached 3% by microscopy analysis. To this end, 2.5 µl of tail blood were collected and mounted on a glass slide, and 8 min later the number of exflagellation events present in 4 independent fields of vision at 40× were determined. When parasitemia reached up to 3%, either DMSO or ivermectin were administered by oral gavage, at a concentration of 5 mg/kg, to five mice of each experimental group. Parasitemia, gametocytemia and exflagellation were monitored for 3 days after treatment, following which the mice were euthanized, and the experiment was terminated.
Evaluation of the in vitro activity of avermectin compounds
The effect of eprinomectin, abamectin, ivermectin, moxidectin, doramectin and emamectin on the Plasmodium mosquito stages was evaluated as previously described [26]. The compounds were dissolved in dimethyl sulfoxide (DMSO) and the amount of DMSO equivalent to that present in the highest compound concentration was used as a control. The effect of 10 µM of each compound was assessed on ookinetes, and on oocyst development and maturation. Briefly, after 1 h of incubation, the compounds were added to 5 µl of infected blood cultures, and the bioluminescence intensity of the parasites on the ookinete cultures was assessed 24 h later. To assess the effect of the compounds on oocyst development and maturation, compounds were mixed with the mature ookinetes, and parasites collected after 3 days of culture or compounds were added to the oocyst culture after 3 days of culture, and parasites collected 15 days later.
Compound concentration resulting in 50% inhibition (IC50) for oocyst growth and maturation were estimated for eprinomectin, abamectin, ivermectin, moxidectin, doramectin and emamectin (assayed at 0.05, 0.5, 1, 5, 10, 25 and 50 µM) by nonlinear regression analysis.
Evaluation of avermectin compounds’ in vitro cytotoxicity
Compounds were screened for their in vitro cytotoxicity against D. melanogaster S2 cells, using the AlamarBlue® assay (Invitrogen, Carlsbad, USA). This assay allows to measure metabolic activity based on a fluoremetric/colorimetric indicator [28]. To assess the effect of the compounds on cell development, Drosophila melanogaster S2 cells were seeded in a 1:10 ratio (105 S2 cells) in Schneider’s medium (S0146, Sigma-Aldrich) supplemented with 15% FBS, penicillin/streptomycin (50 U/ml, 50 µg/ml) and gentamicin (50 µg/ml). All the above-mentioned compounds were added to the S2 cell cultures to a final concentration of 10 µM and the amount of DMSO equivalent to that present in the highest compound concentration was used as a control. Cultures were maintained for 7 days and one-quarter of the medium was changed 3 times per week every 48 to 72 h. Samples were collected every day by removing 120 µl of medium and adding 80 µl of AlamarBlue previously diluted in Schneider’s medium (1:10 dilution) to each well. The suspension was transferred to a 96 well flat bottom plate and incubated for one and a half hours at 37 °C. Fluorescence intensity was then measured using a microplate reader (Tecan Infinite M200) at 530 nm excitation wavelength/590 nm emission wavelength to determine cell viability.
Statistical analysis
Data on the assessment of the compounds’ effect in vitro were analysed using the Kruskal-Wallis test. Data on the compounds’ effect on parasitemia, gametocytemia and exflagellation in vivo were analysed employing non-linear regression analysis. Results were considered significant for P-values < 0.05. Nonlinear regression analysis was employed to fit the normalized results of the dose-response curves for IC50 determination. All statistical tests were performed by GraphPad Prism (version 6.00, GraphPad Software, La Jolla, USA).
Results
In vivo activity of ivermectin against P. berghei blood stages
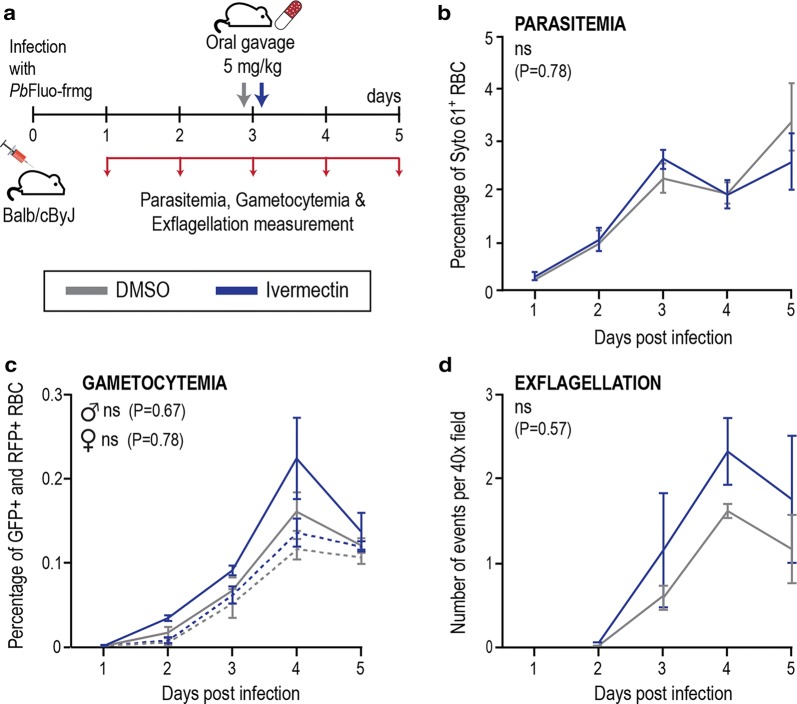
A mouse model of infection was employed to evaluate the effect of ivermectin on P. berghei sexual and asexual blood stage forms in vivo, as described (Fig. 1a). Our results show no statistically significant differences between untreated controls and ivermectin-treated mice regarding overall parasitemia (F(1, 26) = 0.074, P = 0.78), percentage of the parasite’s male and female gametocytemia (F(1, 26) = 0.18, P = 0.67 and F(1, 26) = 0.079, P = 0.78, respectively), and exflagellation events (F(1, 26) = 0.33, P = 0.57) up to 5 days after infection (Fig. 1b–d). These data suggest that, at the tested dosage, ivermectin does not appear to significantly inhibit Plasmodium asexual and sexual forms in the blood.
Fig. 1.
Ivermectin activity against P. berghei asexual and sexual blood stages in the mammalian host. a Schematics of assessment of in vivo compound activity on parasitemia, gametocytemia and exflagellation of mice treated with ivermectin. b In vivo activity of ivermectin on parasitemia of mice treated by a single oral dosage of ivermectin. Results are a representation of Syto 61 positive events on flow cytometry analysis and are expressed as the mean of parasitemia values (percentage of infected red blood cells) ± standard deviation (SD). c In vivo activity of ivermectin on female and male gametocytemia of mice treated by a single oral dosage of ivermectin. Female gametocytemia is represented by a dashed line and male gametocytemia by a solid line. Female and male gametocytes were identified by flow cytometry analysis of RFP+ or GFP+ events, respectively. Results are expressed as the mean of gametocytemia values (percentage of gametocytes) ± SD. d In vivo activity of ivermectin on the number of exflagellation events per 40× microscopic field of mice treated by a single oral dosage of selected drug. Results are expressed as the mean of observed exflagellation events ± SD. Abbreviations: ns, non-significant
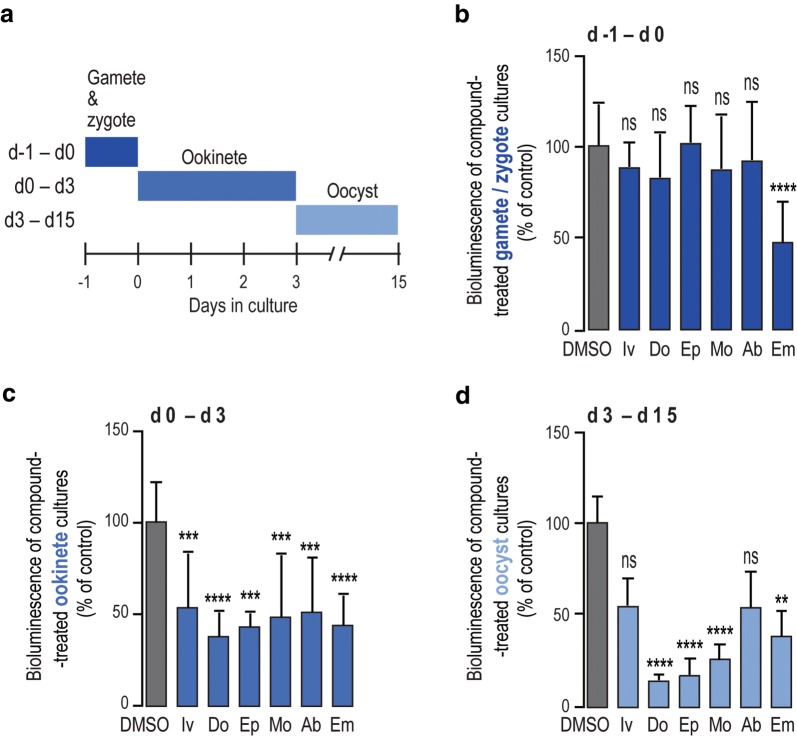
In vitro activity of avermectins against P. berghei sporogonic development
We then sought to clarify whether the proposed transmission-reducing activity of ivermectin would include a direct action of the drug on the parasite’s transmission stages in the mosquito or if it would result solely from its effect on the mosquito. Given the marked structural similarities between avermectins, the effect an additional 5 compounds of this family, doramectin, moxidectin, abamectin, emamectin, and eprinomectin on the parasite’s sporogonic stages was also evaluated, as described (Fig. 2a).
Fig. 2.
Activity of avermectins against Plasmodium mosquito stages in vitro. a Schematics of the progress of the parasite culturing process, highlighting the different schedules of compound treatment employed. b Assessment of compound effects on ookinete formation, expressed as the percentage of inhibition of P. berghei ookinete formation. c In vitro activity of selected compounds against oocyst formation. d In vitro activity of selected compounds on oocyst development. A total of 6 compounds were screened at a concentration of 10 μM: Iv; Do, Ep, Mo, Ab and Em. Bars correspond to RLU measurements represented as the percentage of RLU of the DMSO control. Results are expressed as the mean + SD. ****P < 0.0001, ***P < 0.001, **P < 0.01. Abbreviations: Iv, ivermectin; Do, doramectin; Ep, eprinomectin; Mo, moxidectin; Ab, abamectin; Em, emamectin
Our assessment of the compounds’ effect on the transformation of gametes/zygote into ookinetes, showed that whereas emamectin inhibited parasite differentiation by approximately 47%, ivermectin and the remaining avermectins had a very small and non-significant impact on the formation of ookinetes (Fig. 2b). The effect of avermectins on oocyst formation and growth was subsequently assessed. At 10 µM, both these processes are inhibited by at least 50% by all compounds (Fig. 2c, d). Half-maximal inhibitory concentrations (IC50) for oocyst formation by the compounds under evaluation were then determined and found to range from ~ 5.7 µM to ~ 11.6 µM, with eprinomectin, doramectin and emamectin displaying the greatest potency against this early stage of parasite sporogony (Table 1, Additional file 1: Figure S1a). Their IC50 values for oocyst growth varied between ~ 4.3 µM and ~ 9.3 µM (Table 1, Additional file 1: Figure S1b), with eprinomectin, doramectin and moxidectin standing out as the three compounds that most potently inhibited oocyst development (Table 1). Since oocysts are co-cultured in the presence of Drosophila S2 cells, we evaluated the latter’s viability for up to 7 days in the presence of each of the compounds under study (Additional file 1: Figure S2). Of note, these results indicate that emamectin displays some cytotoxicity against S2 cells, which might suggest a moderate overestimation of this compound’s activity against developing oocysts.
Table 1.
IC50 of avermectins against oocyst formation and maturation in vitro
| Compound | Day0–Day3 (µM) | Day3–Day15 (µM) | ||
|---|---|---|---|---|
| IC50 | SD | IC50 | SD | |
| Eprinomectin | 5.70 | 2.31 | 4.59 | 2.26 |
| Doramectin | 7.08 | 1.91 | 4.32 | 1.76 |
| Emamectin | 7.31 | 2.45 | 7.36 | 1.50 |
| Abamectin | 8.77 | 4.38 | 7.93 | 4.14 |
| Moxidectin | 10.85 | 8.56 | 5.49 | 1.00 |
| Ivermectin | 11.58 | 0.44 | 9.32 | 1.64 |
Notes: Compound concentration resulting in 50% inhibition (IC50) for oocyst growth and maturation were calculated for Ep, Do, Em, Ab, Mo, and Iv (assayed at 0.05, 0.5, 1, 5, 10, 25 and 50 µM). Results are expressed as the mean ± SD
Abbreviations: Ep, eprinomectin; Do, doramectin; Em, emamectin; Ab, abamectin; Mo, moxidectin; Iv, ivermectin
Discussion
In the present study, we aimed to assess the impact of ivermectin on the blood stages of P. berghei in vivo, as well as the effect of several avermectins on the parasite’s mosquito stages in vitro. Our results show that ivermectin is not active against Plasmodium asexual and sexual blood forms in a mouse model. However, both ivermectin and other members of the avermectin family strongly inhibited parasite sporogony, at IC50 values consistent with those reported for the antibiotic thiostrepton and the antimalarial pyronaridine, whose impact on sporogony has been demonstrated [29].
In light of their versatility as antiparasitic and insecticidal compounds, avermectins and, particularly ivermectin, have been considered as potential aids in the fight against malaria [16, 18, 19, 21–23]. Of note, the use of ivermectin in MDA to treat other neglected tropical diseases in malaria-endemic regions has led to the investigation of its potential to block malaria transmission [18, 30, 31]. A recent study showed that a 3 weekly MDA of ivermectin in African villages reduced the incidence of uncomplicated malaria episodes among children, which the authors attributed to the drug’s mosquitocidal effect [18]. However, it should be noted that the results of this study have recently been questioned on the basis of the statistical methods employed [32].
Nevertheless, the issue of whether the impact of ivermectin stems solely from its impact on mosquitoes or, additionally, results from a combination of its insecticidal activity and of its ability to inhibit the parasite’s blood and mosquito stages remains unresolved. In fact, while the inhibitory effect of ivermectin against the liver stages of Plasmodium parasites has been demonstrated [19], the evaluation of its impact against the blood [20, 22, 25] and sporogonic [15, 23, 24] stages of the parasite’s life-cycle has yielded contradictory results [15, 20, 22–25].
In invertebrates, ivermectin interacts with the glutamate-gated chloride channels in neuronal and neuromuscular tissues [33–35] and may also act on the γ-aminobutyric acid-gated chloride channels [36–38]. However, neither of these molecular targets is present in P. falciparum, which might explain the lack of ivermectin in vitro effect against P. falciparum blood stages [20]. Contradictorily, ivermectin was reported to lead to the arrest the development of P. falciparum blood stages by inhibiting the nuclear import of SRP polypeptides, thus arresting parasite growth [22]. The sporontocidal activity of ivermectin against P. vivax in An. darlingi led to a reduction of oocyst prevalence, but not of their intensity [24], similarly to what has been observed for P. falciparum in An. gambiae [16]. This contradicts previous studies suggesting that ivermectin reduces oocyst prevalence and intensity in An. dirus and An. minimus [21]. Although the mechanism of action of ivermectin against the sporogonic stages of Plasmodium parasites remains to be elucidated, these observations suggest that the compound may act on the mosquito midgut physiology, preventing parasite establishment [23]. As such, the different results obtained experimentally in previous studies might result from differences in insect biology.
Our study sheds a new light on these controversial issues and helps clarify whether ivermectin exerts an impact on the blood and/or on the mosquito stages of Plasmodium parasites. Our in vivo investigation revealed that treatment of infected mice with 5 mg/kg of ivermectin had no impact on parasitemia, indicating an absence of activity of this compound against the parasite’s asexual forms in the blood, in accordance with Nasveld et al. [20] for P. falciparum.
To further clarify whether a direct drug effect on Plasmodium mosquito stages contributes to transmission blocking, ivermectin and other avermectins were employed in a mosquito-free in vitro assay. Our results indicate that while these compounds exert little or no activity against ookinete formation, they efficiently inhibit the parasite’s sporogonic stages after fertilization, most effectively targeting late stage oocysts. Further investigation on the mechanism of action of avermectins is required in order to fully clarify the exact targets of their activity against Plasmodium sporogony.
Conclusions
Our results suggest that the impact of ivermectin on Plasmodium transmission does not result from an inhibition of Plasmodium spp. transmissible forms in the mammalian host, and stems solely from its effect during the mosquito stage of infection. Our data show that the transition from gamete/zygote to ookinete is highly resistant to avermectins, and that the oocyst is the most vulnerable stage of the parasite’s sporogonic cycle to treatment with avermectins. Collectively, these observations support the notion that, besides their mosquitocidal effect, avermectins may also directly target the parasite’s sporogonic stages, which likely contributes to transmission-blocking activity. Our results lend further support to the use of avermectins for MDA as a tool for malaria control in endemic regions, and suggest that the inclusion of members of this family of avermectin compounds besides ivermectin in these interventions should be considered.
Supplementary information
Additional file 1: Figure S1. Dose-response of avermectins against Plasmodium sporogonic stages. a Representative curves of avermectins effect resulting in 50% inhibition (IC50) of oocyst formation. Curves are presented for Ep, Do, Em, Ab, Mo and Iv (assayed at 0.05, 0.5, 1, 5, 10, 25 and 50 µM). Results are expressed as the mean ± standard deviation (SD). b Representative curves of avermectinʼs effect resulting in 50% inhibition (IC50) of oocyst maturation. Curves are presented for Ep, Do, Em, Ab, Mo and Iv (assayed at 0.05, 0.5, 1, 5, 10, 25 and 50 µM). Results are expressed as the mean ± SD. Figure S2. Evaluation of avermectinʼs cytotoxicity on S2 cells. Determination of cell viability in a time course of 7 days by the AlamarBlue® assay. Results are normalized to the DMSO control and expressed as the mean ± SD. Abbreviations: DMSO, dimethyl sulfoxide; Ep, eprinomectin; Do, doramectin; Em, emamectin; Ab, abamectin; Mo, moxidectin; Iv, ivermectin.
Acknowledgements
We are grateful to Andreia Santos and Bárbara Oliveira for technical assistance and Gunnar Mair for sharing the parasite line PbFluo-frmg. We are also very grateful to Margarida Sanches-Vaz for useful discussions and for critically reviewing the manuscript.
Abbreviations
- CSP
circumsporozoite protein
- DMSO
dimethyl sulfoxide
- FBS
foetal bovine serum
- GFP
green fluorescent protein
- IC50
concentration that inhibits parasite load by 50%
- iRBC
infected red blood cells
- Luc
luciferase
- MDA
mass drug administration
- RFP
red fluorescent protein
- RPMI
Roswell Park Memorial Institute
Authors’ contributions
RA performed the experimental work, AMM and MP designed and supervised the study, RA and MP wrote the manuscript. All authors read and approved the final manuscript.
Funding
This work was carried out with the support of grants PTDC-BBB-BMD-2695-2014 and 02/SAICT/2017/29550 from Fundação para a Ciência e Tecnologia, Portugal (FCT) to AMM and MP, respectively, and by FCT grant UID/BIM/50005/2019 (Ministério da Ciência, Tecnologia e Ensino Superior (MCTES) through Fundos do Orçamento de Estado). RA was supported by FCT’s fellowship BD/131334/2017, AMM was supported by FCT’s fellowship SFRH/BPD/80693/2011, and MP was supported by FCT’s Investigador FCT 2013 and CEEC 2018 fellowships.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its additional file.
Ethics approval and consent to participate
All work with laboratory animals was performed according to national and European regulations (Directive 2010/63/EU). All protocols were approved by the Animal Experimentation Ethics Committee (AWB_2015_09_MP_Malaria) of the Instituto de Medicina Molecular-João Lobo Antunes and are in accordance with the Federation of European Laboratory Animal Science Associations (FELASA) guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Raquel Azevedo, Email: raquel.azevedo@medicina.ulisboa.pt.
António M. Mendes, Email: antoniomendes@medicina.ulisboa.pt
Miguel Prudêncio, Email: mprudencio@medicina.ulisboa.pt.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13071-019-3805-0.
References
- 1.WHO. World malaria report 2018. Geneva: World Health Organization; 2018. https://apps.who.int/iris/bitstream/handle/10665/275867/9789241565653-eng.pdf?ua=. Accessed 29 Feb 2019.
- 2.Mota MM, Pradel G, Vanderberg JP, Hafalla JC, Frevert U, Nussenzweig RS, et al. Migration of Plasmodium sporozoites through cells before infection. Science. 2001;291:141–144. doi: 10.1126/science.291.5501.141. [DOI] [PubMed] [Google Scholar]
- 3.Bannister L, Mitchell G. The ins, outs and roundabouts of malaria. Trends Parasitol. 2003;19:209–213. doi: 10.1016/S1471-4922(03)00086-2. [DOI] [PubMed] [Google Scholar]
- 4.Baton LA, Ranford-Cartwright LC. Spreading the seeds of million-murdering death: metamorphoses of malaria in the mosquito. Trends Parasitol. 2005;21:573–580. doi: 10.1016/j.pt.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 5.Sinden RE, Butcher GA, Billker O, Fleck SL. Regulation of infectivity of Plasmodium to the mosquito vector. Adv Parasitol. 1996;38:53–117. doi: 10.1016/S0065-308X(08)60033-0. [DOI] [PubMed] [Google Scholar]
- 6.Vinetz JM. Plasmodium ookinete invasion of the mosquito midgut. Curr Top Microbiol Immunol. 2005;295:357–382. doi: 10.1007/3-540-29088-5_14. [DOI] [PubMed] [Google Scholar]
- 7.Itsara LS, Zhou Y, Do J, Dungel S, Fishbaugher ME, Betz WW, et al. PfCap380 as a marker for Plasmodium falciparum oocyst development in vivo and in vitro. Malar J. 2018;17:135. doi: 10.1186/s12936-018-2277-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Staines HM, Sanjeev K. Treatment and prevention of malaria. 1. Basel: Springer; 2012. [Google Scholar]
- 9.Janse C. Life cycle of P. berghei. Leiden University Medical Center. https://www.lumc.nl/org/parasitologie/research/malaria/berghei-model/life-cycle-berghei/. Accessed 20 May 2019.
- 10.López Del Prado GR, Hernán García C, Moreno Cea L, Fernández Espinilla V, Muñoz Moreno MF, Delgado Márquez A, et al. Malaria in developing countries. J Infect Dev Ctries. 2014;8:1–4. doi: 10.3855/jidc.4610. [DOI] [PubMed] [Google Scholar]
- 11.Campbell WC. History of avermectin and ivermectin, with notes on the history of other macrocyclic lactone antiparasitic agents. Curr Pharm Biotechnol. 2012;13:853–865. doi: 10.2174/138920112800399095. [DOI] [PubMed] [Google Scholar]
- 12.Tambo E, Khater EIM, Chen J-H, Bergquist R, Zhou X-N. Nobel prize for the artemisinin and ivermectin discoveries: a great boost towards elimination of the global infectious diseases of poverty. Infect Dis Poverty. 2015;4:58. doi: 10.1186/s40249-015-0091-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campbell WC, editor. Ivermectin and abamectin. New York: Springer; 1989. [Google Scholar]
- 14.Cupp EW, Sauerbrey M, Richards F. Elimination of human onchocerciasis: history of progress and current feasibility using ivermectin (Mectizan(®)) monotherapy. Acta Trop. 2011;120(Suppl. 1):S100–S108. doi: 10.1016/j.actatropica.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 15.Kobylinski KC, Escobedo-Vargas KS, López-Sifuentes VM, Durand S, Smith ES, Baldeviano GC, et al. Ivermectin susceptibility, sporontocidal effect, and inhibition of time to re-feed in the amazonian malaria vector Anopheles darlingi. Malar J. 2017;16:474. doi: 10.1186/s12936-017-2125-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chaccour C, Lines J, Whitty CJM. Effect of ivermectin on Anopheles gambiae mosquitoes fed on humans: the potential of oral insecticides in malaria control. J Infect Dis. 2010;202:113–116. doi: 10.1086/653208. [DOI] [PubMed] [Google Scholar]
- 17.Foy BD, Kobylinski KC, da Silva IM, Rasgon JL, Sylla M. Endectocides for malaria control. Trends Parasitol. 2011;27:423–428. doi: 10.1016/j.pt.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Foy BD, Alout H, Seaman JA, Rao S, Magalhaes T, Wade M, et al. Efficacy and risk of harms of repeat ivermectin mass drug administrations for control of malaria (rimdamal): a cluster-randomised trial. Lancet. 2019;393:517–526. doi: 10.1016/S0140-6736(18)32321-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mendes AM, Albuquerque IS, Machado M, Pissarra J, Meireles P, Prudêncio M. Inhibition of Plasmodium liver infection by ivermectin. Antimicrob Agents Chemother. 2017;61:e02005–e02016. doi: 10.1128/AAC.02447-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nasveld P, Russell B, Kotecka B, Rieckmann K. Lack of in vitro effect of ivermectin on Plasmodium falciparum. Southeast Asian J Trop Med Public Health. 2003;34:552–553. [PubMed] [Google Scholar]
- 21.Kobylinski KC, Ubalee R, Ponlawat A, Nitatsukprasert C, Phasomkulsolsil S, Wattanakul T, et al. Ivermectin susceptibility and sporontocidal effect in Greater Mekong subregion Anopheles. Malar J. 2017;16:280. doi: 10.1186/s12936-017-1923-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Panchal M, Rawat K, Kumar G, Kibria KM, Singh S, Kalamuddin M, et al. Plasmodium falciparum signal recognition particle components and anti-parasitic effect of ivermectin in blocking nucleo-cytoplasmic shuttling of SRP. Cell Death Dis. 2014;5:e994. doi: 10.1038/cddis.2013.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kobylinski KC, Foy BD, Richardson JH. Ivermectin inhibits the sporogony of Plasmodium falciparum in Anopheles gambiae. Malar J. 2012;11:381. doi: 10.1186/1475-2875-11-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pinilla YT, Lopes SCP, Sampaio VS, Andrade FS, Melo GC, Orfanó AS, et al. Promising approach to reducing malaria transmission by ivermectin: sporontocidal effect against Plasmodium vivax in the South American vectors Anopheles aquasalis and Anopheles darlingi. PLoS Negl Trop Dis. 2018;12:e0006221. doi: 10.1371/journal.pntd.0006221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Carvalho LP, Sandri TL, de Melo EJT, Fendel R, Kremsner PG, Mordmüller B, et al. Ivermectin impairs the development of sexual and asexual stages of Plasmodium falciparum in vitro. Antimicrob Agents Chemother. 2019;63:00085-19. doi: 10.1128/AAC.00085-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Azevedo R, Markovic M, Machado M, Franke-Fayard B, Mendes AM, Prudêncio M. A bioluminescence method for in vitro screening of Plasmodium transmission-blocking compounds. Antimicrob Agents Chemother. 2017;61:02699-16. doi: 10.1128/AAC.02699-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ponzi M, Sidén-Kiamos I, Bertuccini L, Currà C, Kroeze H, Camarda G, et al. Egress of Plasmodium berghei gametes from their host erythrocyte is mediated by the MDV-1/PEG3 protein. Cell Microbiol. 2009;11:1272–1288. doi: 10.1111/j.1462-5822.2009.01331.x. [DOI] [PubMed] [Google Scholar]
- 28.AlamarBlue Cell Viability Reagent—Thermo Fisher Scientific. https://www.thermofisher.com/order/catalog/product/DAL1025. Accessed 10 May 2019.
- 29.Delves M, Plouffe D, Scheurer C, Meister S, Wittlin S, Winzeler EA, et al. The activities of current antimalarial drugs on the life cycle stages of Plasmodium: a comparative study with human and rodent parasites. PLoS Med. 2012;9:e1001169. doi: 10.1371/journal.pmed.1001169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chaccour CJ, Rabinovich NR, Slater H, Canavati SE, Bousema T, Lacerda M, et al. Establishment of the ivermectin research for malaria elimination network: updating the research agenda. Malar J. 2015;14:243. doi: 10.1186/s12936-015-0691-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kobylinski KC, Sylla M, Chapman PL, Sarr MD, Foy BD. Ivermectin mass drug administration to humans disrupts malaria parasite transmission in senegalese villages. Am J Trop Med Hyg. 2011;85:3–5. doi: 10.4269/ajtmh.2011.11-0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Foy BD, Rao S, Parikh S, Slater HC, Dabiré RK. Analysis of the rimdamal trial—authors’ reply. Lancet. 2019;394:1006–1007. doi: 10.1016/S0140-6736(19)32139-7. [DOI] [PubMed] [Google Scholar]
- 33.Cully DF, Vassilatis DK, Liu KK, Paress PS, Van der Ploeg LH, Schaeffer JM, et al. Cloning of an avermectin-sensitive glutamate-gated chloride channel from Caenorhabditis elegans. Nature. 1994;371:707–711. doi: 10.1038/371707a0. [DOI] [PubMed] [Google Scholar]
- 34.Kane NS, Hirschberg B, Qian S, Hunt D, Thomas B, Brochu R, et al. Drug-resistant Drosophila indicate glutamate-gated chloride channels are targets for the antiparasitics nodulisporic acid and ivermectin. Proc Natl Acad Sci USA. 2000;97:13949–13954. doi: 10.1073/pnas.240464697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cully DF, Paress PS, Liu KK, Schaeffer JM, Arena JP. Identification of a Drosophila melanogaster glutamate-gated chloride channel sensitive to the antiparasitic agent avermectin. J Biol Chem. 1996;271:20187–20191. doi: 10.1074/jbc.271.33.20187. [DOI] [PubMed] [Google Scholar]
- 36.Ludmerer SW, Warren VA, Williams BS, Zheng Y, Hunt DC, Ayer MB, et al. Ivermectin and nodulisporic acid receptors in Drosophila melanogaster contain both gamma-aminobutyric acid-gated Rdl and glutamate-gated GluCl alpha chloride channel subunits. Biochemistry. 2002;41:6548–6560. doi: 10.1021/bi015920o. [DOI] [PubMed] [Google Scholar]
- 37.Dent JA, Smith MM, Vassilatis DK, Avery L. The genetics of ivermectin resistance in Caenorhabditis elegans. Proc Natl Acad Sci USA. 2000;97:2674–2679. doi: 10.1073/pnas.97.6.2674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duce IR, Bhandal NS, Scott RH, Norris TM. Effects of ivermectin on γ-aminobutyric acid and glutamate-gated chloride conductance in arthropod skeletal muscle. In: Clark JM, editors. Molecular action of insecticides on ion channels. ACS Symposium Series, vol. 591. Washington: American Chemical Society; 1995. p. 251–63.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1. Dose-response of avermectins against Plasmodium sporogonic stages. a Representative curves of avermectins effect resulting in 50% inhibition (IC50) of oocyst formation. Curves are presented for Ep, Do, Em, Ab, Mo and Iv (assayed at 0.05, 0.5, 1, 5, 10, 25 and 50 µM). Results are expressed as the mean ± standard deviation (SD). b Representative curves of avermectinʼs effect resulting in 50% inhibition (IC50) of oocyst maturation. Curves are presented for Ep, Do, Em, Ab, Mo and Iv (assayed at 0.05, 0.5, 1, 5, 10, 25 and 50 µM). Results are expressed as the mean ± SD. Figure S2. Evaluation of avermectinʼs cytotoxicity on S2 cells. Determination of cell viability in a time course of 7 days by the AlamarBlue® assay. Results are normalized to the DMSO control and expressed as the mean ± SD. Abbreviations: DMSO, dimethyl sulfoxide; Ep, eprinomectin; Do, doramectin; Em, emamectin; Ab, abamectin; Mo, moxidectin; Iv, ivermectin.
Data Availability Statement
All data generated or analysed during this study are included in this published article and its additional file.