Abstract
Aims and objectives:
To clarify the meaning of sleep disturbance in people with diabetes and examine its antecedents, attributes and consequences through concept analysis.
Background:
Sleep is crucial for health, and people with diabetes are frequently beset with disturbances in their sleep. The concept of sleep disturbance in people with diabetes has not been clearly defined. The inconsistent use of sleep disturbance has created confusion and impeded our understanding of the sleep in people with diabetes. This analysis will provide a conceptual foundation of sleep disturbance in diabetes, thereby facilitating more effective means for assessment and treatment.
Design:
Concept analysis.
Methods:
A systematic search without time restriction on the publication year was carried out using PubMed, CINAHL, PsycINFO, Web of Science and ProQuest Dissertations and Theses. Rodgers’s method of evolutionary concept analysis guided the analysis. Inductive thematic analysis was conducted to identify the attributes, antecedents and consequences.
Results:
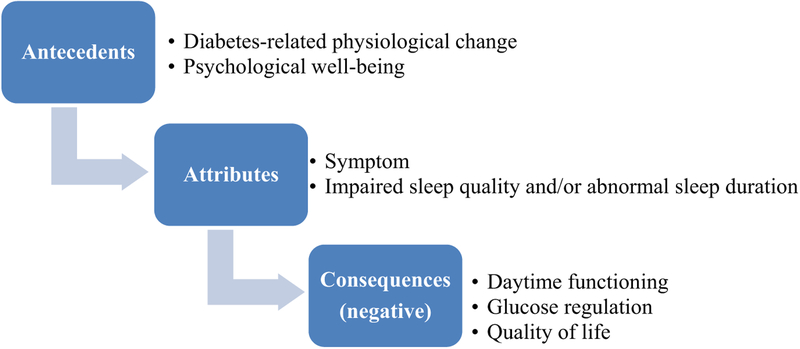
Based on the 26 eligible studies, two major attributes are that sleep disturbance is a symptom and is characterised by impaired sleep quality and/or abnormal sleep duration. Two antecedents are diabetes-related physiological change and psychological well-being. Sleep disturbance can result in impaired daytime functioning, glucose regulation and quality of life.
Conclusions:
Defining the concept of sleep disturbance in people with diabetes facilitates consistent use and effective communication in both practice and research. Sleep disturbance in people with diabetes is a complex symptom that includes impaired sleep quality and/or abnormal sleep duration. This paper contributes to the current knowledge of sleep in people with diabetes. Future research on antecedents and consequences of sleep disturbance is necessary for further clarifications.
Relevance to clinical practice:
Findings from this paper underscore the need for nursing education, clinical assessment and effective management of sleep disturbance in people with diabetes.
Keywords: concept analysis, diabetes, nursing, Rodgers, sleep disturbance, symptom
1 |. INTRODUCTION
Sleep is an important public health issue and one of the major topics covered in the Heathy People 2020 Project. The absence of sleep disturbance is a prerequisite for healthy sleep (Consensus Conference Panel et al. 2015). Sleep is a normal physiological process and one of the most fundamental human needs. Research is proliferating on the role sleep plays in individual well-being, especially in people with chronic illness, such as diabetes. In 2015, 12.2% of the US adults aged 18 or over had diabetes, and diabetes was the seventh leading cause of death (Centers for Disease Control and Prevention 2017). Increasing evidence indicates that individuals with sleep disturbance have a higher risk of developing diabetes (Anothaisintawee, Reutrakul, Van Cauter, & Thakkinstian, 2016); in turn, people who already have diabetes suffer from more sleep disturbance than those without diabetes (van Dijk et al., 2011; Keskin et al., 2015). Both diabetes and sleep disturbance are major health issues that affect a large proportion of people across the world. The combination of those two conditions likely poses a greater threat to an individual’s health.
Diabetes management includes attaining and maintaining good glycaemic control, as measured by A1C. A recent meta-analysis suggests that poor sleep quality has a negative impact on A1C levels, although the causality remains unclear (Lee, Ng, & Chin, 2017). The American Diabetes Association recommends that sleep assessments should be included in all medical evaluations of patients with diabetes (American Diabetes Association 2017). Healthcare professionals, particularly nurses, are essential in evaluating and identifying those with sleep disturbance. Equally imperative is the delivery of appropriate interventions to alleviate sleep disturbance in people with diabetes. This concept analysis proposes to develop a conceptual foundation that can be used to guide evaluation and interventions related to sleep disturbance in people with diabetes.
1.1 |. Background and aims
Sleep disturbance is complex and likely results from a variety of physiological, psychological and behavioural factors. Many of these factors, including chronic pain, may be similar between healthy populations and those with various health conditions, such as diabetes, cancer and musculo-skeletal disorders among others. However, the contextual basis for these factors across populations may vary in character, number and co-occurrence with other factors. Diabetes may impact sleep through specific, diabetes-related neuro-endocrine-metabolic dysregulation (Barone & Menna-Barreto, 2011). Yet, the term sleep disturbance in the context of diabetes has not been explicitly defined or formally analysed. Within the realm of sleep research, the term sleep disturbance is frequently seen in current literature, but the term sleep disorder is more common and has been widely used since 1920 (Schulz & Salzarulo, 2015). These two terms are different and should not be used interchangeably. Sleep disorder is diagnosed, using strict criteria, and may be classified into distinct categories, such as insomnia and sleep apnoea. Sleep disturbance does not require a diagnosis and might be universally experienced by anyone at some point in their lives (Rylance & Smith, 2016). When patients complain of sleep disturbance, any ambiguity of the concept limits our ability to evaluate or develop appropriate interventions for our patients. Clarification of the ambiguity and use of consistent terminology will provide a solid conceptual foundation for future studies and facilitate effective communications among the healthcare community. Thus, the purpose of this paper was to clarify the concept of sleep disturbance in diabetes through examining its use and identifying its attributes, antecedents and consequences.
Rodgers’s (2000) method of evolutionary concept analysis was used to analyse the concept of sleep disturbance in diabetes. According to Rodgers (2000), concept analysis consists of six iterative steps: identifying the concept of interest; choosing the setting and sample; collecting and managing the data; analysing the data; identifying exemplars; and interpreting the results and proving implications.
2 |. METHODS
2.1 |. Identifying the concept of interest
Identification of the concept of interest and exploration of surrogate terms is the first step of concept analysis. Surrogate terms share similar characteristics with the concept of interest and are frequently used interchangeably (Rodgers, 2000). Explicating surrogate terms ensures a more thorough review of the literature. Potential surrogate terms for sleep disturbance include sleep problem and sleep impairment, which are common in the sleep literature and frequently used interchangeably. We included the use of both terms in our search so that important studies were not missed.
2.2 |. Setting, sample and data sources
This step focuses on the determination of settings, including time period and discipline or type of literature to be searched. A sample needs to be rigorously selected to obtain a representative literature and minimise researcher bias. The ultimate goal of this step is to answer the research question through rigorous design (Rodgers, 2000).
We conducted electronic searches of PubMed, CINAHL, Psyc-INFO and ProQuest Dissertations and Theses using combinations of “diabetes” and “sleep disturbance*,” “sleep problem*” or “sleep impairment” in the abstract/title. Additionally, a search of Web of Science was conducted using the above combinations as the “topic.” The search was carried out without time restriction to capture as many relevant studies as possible. This choice would also enable an overview of the use of the concept over time. The search was limited to the English language. Sleep disturbance in humans also carries social–behavioural characteristics. Therefore, studies conducted in animals were excluded. Published abstracts and comments were excluded as the detailed information was not available. Studies conducted in other populations (including healthy people) rather than those with diabetes were excluded.
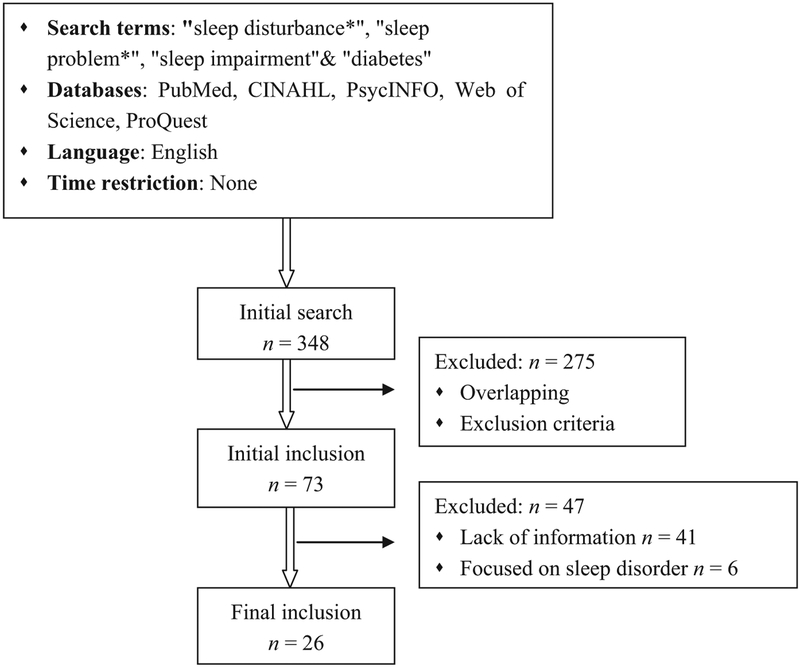
The initial search resulted in 348 articles after removing duplicates (Figure 1). Further screening based on the exclusion criteria was conducted by reviewing title and abstract of the article, which resulted in an initial sample size of 73. There is no consensus on how to evaluate the quality of the primary sources included in a concept analysis. In this analysis, only papers that described sleep disturbance were included. Thus, 41 of the 73 studies were further excluded because no information could be found about characteristics of sleep disturbance, which makes the identification of attributes impossible. Sleep disturbance was mentioned in six studies; but sleep disorder (e.g., obstructive sleep apnoea, insomnia and restless legs syndrome) was the primarily measured construct, so these six studies were also excluded. Ancestry searching of the bibliography of the 26 articles resulted in no further studies that met our criteria. Consequently, the final analysis included 26 articles. Rodgers (2000) proposed a minimum sample size of 30 from a variety of disciplinary strata to identify contextual variation. This was not feasible in the current analysis. Therefore, the 26 studies were pooled and analysed together.
FIGURE 1.
Literature search and selection process
2.3 |. Collecting and managing the data
During data collection and management (Rodgers, 2000), primary sources were reviewed to further identify the actual use of surrogate terms and related concepts. The primary accomplishment of a concept analysis is the identification of attributes. It is not uncommon that authors do not explicitly present the definition of a concept. However, statements that highlight characteristics of the concept should be identified and used as the attributes. Additionally, contextual basis (i.e., antecedents and consequences of the concept) also needs to be identified. Thus, a table matrix was used for efficient and reliable abstraction of pertinent information (Garrard, 2011). The matrix was developed by two reviewers (BZ and CV). Primary sources were reviewed by one review (BZ) and randomly checked by another (CF). Study characteristics, sentences that described the concept attributes, antecedents and consequences, were extracted and tabulated into the matrix.
2.4 |. Analysing the data
Based on Rodgers’s (2000), the standard procedure of thematic analysis was performed until a cohesive and comprehensive consensus was reached. One reviewer (BZ) coded the data and identified the recurring themes. Major themes for attributes, antecedents and consequences of the concept were examined separately. The final pool of themes was identified by two reviewers (BZ and CF). Appropriate “labels” were developed to describe each theme. A conceptual definition of sleep disturbance in diabetes was developed by the review team.
3 |. RESULTS
3.1 |. Study characteristics
The studies were published between 1994 and 2016. Three of the 26 studies were review papers, and cross-sectional design was used in a majority of the studies. Both types of diabetes were included in the analysis. Sample size ranged from 15 to 1,322. Participant characteristics are shown in Table 1.
TABLE 1.
Study characteristics and attributes reflected in each study
| Attributes | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author (year) | Country | Design | Sample | Age (years) | Female | Symptom | Impaired sleep quality | Abnormal sleep duration |
| Sridhar and Madhu (1994) | India | Cross-sectional | 184 diabetes | 46.0 | 33 (17.9%) | √ | √ | |
| Han et al. (2002) | Korea | Cross-sectional | 82 diabetes | 58.7 (27–78) | 32 (39.0%) | √ | √ | |
| Happe et al. (2005) | Germany | Cross-sectional | 46 T1DM | 12.0 (3–18) | 25 (54.4%) | √ | ||
| Sridhar and Putcha (2006) | India | Cross-sectional | 4624 T2DM | NA | NA | √ | ||
| Martins et al. (2008) | Review | √ | ||||||
| Wrobel et al. (2008) | Poland | RCT | 61 diabetes | 54.5 | 36 (59.0%) | √ | ||
| Chasens et al. (2009) | USA | Cross-sectional | 244 diabetes | 68.0 | 121 (49.8%) | √ | √ | |
| Bener and Al-Hamaq (2010) | Qatar | Cross-sectional | 847 T2DM | >20 | 450 (53.1%) | √ | √ | √ |
| Reddy et al. (2010) | Australia | Cross-sectional | 561 diabetes | 67 | 252 (44.9%) | √ | √ | |
| Knutson et al. (2011) | USA | Cross-sectional | 40 T2DM | 45.6 (38–51) | 28 (70.0%) | √ | √ | √ |
| Olsson et al. (2011) | Sweden | Cross-sectional | 1322 T2DM | ≥35 | NA | √ | ||
| van Dijk et al. (2011) | USA | Cross-sectional | 99 T1DM | 43.9 | 44 (44.4%) | √ | √ | |
| Voinescu et al. (2011) | Ireland | Cross-sectional | 97T2DM | 55.9 | 48 (49.5%) | √ | √ | √ |
| Reutrakul, Zaidi (2013) | USA | Cross-sectional | 15 gestational diabetes | 29.2 | 15 (100%) | √ | √ | |
| Reutrakul, Hood (2013) | USA | Cross-sectional | 194 T2DM | 58.4 (18–85) | 135 (69.6%) | √ | √ | |
| Caruso et al. (2014) | Australia | Cross-sectional | 49 T1DM | 12.0 | 25 (51.0%) | √ | √ | |
| Cho et al. (2014) | Korea | Cross-sectional | 614 T2DM | 59.7 | 233 (37.9%) | √ | √ | |
| Izci-Balserak and Pien (2014) | Review | √ | √ | |||||
| Reutrakul and Van Cauter (2014) | Review | √ | √ | √ | ||||
| Barnard et al. (2015) | UK | Mixed method | 192 T1DM | 19–89 | 145 (75.5%) | √ | ||
| Eshkoor et al. (2015) | Malaysia | Cross-sectional | 502 diabetes | ≥60 | NA | √ | ||
| Fritschi and Redeker (2015) | USA | Cross-sectional | 54 diabetes | 62.9 | 15 (27.8%) | √ | √ | √ |
| Hazen et al. (2015) | USA | Cross-sectional | 72 T1DM | 14.2 (10–18) | 44 (61.1%) | √ | √ | |
| Keskin et al. (2015) | Turkey | Cross-sectional | 585 T2DM | 57.0 (50–64) | 392 (67.0%) | √ | ||
| Nefs et al. (2015) | The Netherlands | Cross-sectional | 267 T1DM; 361 T2DM |
T1DM: 47.0; T2DM: 62.0 |
T1DM: 157 (59.0%); T2DM: 166 (46.0%) |
√ | ||
| Chontong et al. (2016) | Thailand | Cross-sectional | 41 T1DM | 41.5 | 25 (61.0%) | √ | √ | |
T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus; NA, not available; RCT, randomised controlled trial.
3.1.1 |. Definition of sleep disturbance from dictionaries
Sleep is defined as “a complex reversible neurobiological state characterized by closed eyes, behavioral quiescence, and perceptual disengagement from one’s surroundings” (Hall, 2013, p. 1795). According to Merriam-Webster’s Learners Dictionary (Merriam-Webster 2016), disturbance is defined as “an unhealthy physical or mental condition in which something is not normal.” Although the term sleep disturbance appeared as early as the first decade of the 1800s (Schulz & Salzarulo, 2015), it was only used as an alternate term for sleep disorder.
Cormier (1990) described the term sleep disturbance in 1990. He used it to refer to sleep disorder and defined it as “encompassing disorders of initiating and maintaining sleep, disorders of excessive somnolence, disorders of sleep-wake schedule, and dysfunction associated with sleep, sleep stage, or partial arousal” (p. 398). The term “sleep disturbance” in the context of diabetes was first mentioned in 1992 (Bendtson, Gade, Thomsen, Rosenfalck, & Wildschiodtz, 1992). However, no specific description was provided. In the two studies conducted in 1994 and 2002, sleep disturbance was mainly used to represent insomnia symptoms (Han et al., 2002; Sridhar & Madhu, 1994). As is shown in Table 1, over the next decade between 2005 and 2016, the use of sleep disturbance increased and its description was enriched.
3.1.2 |. Attributes
Attributes are characteristics lending the concept unique meanings; they constitute the real definition of a concept (Rodgers, 2000). Two attributes of sleep disturbance in people with diabetes emerged based on the description of sleep disturbance in the primary sources:(i) sleep disturbance is a symptom and (ii) sleep disturbance involves impaired sleep quality and/or abnormal sleep duration. Studies supporting each attribute are shown in Table 1.
Symptom
The first attribute of sleep disturbance is that it is a symptom. Specifically, sleep disturbance was referred to as a symptom that can be present or absent (Sridhar & Madhu, 1994). Han et al. (2002) also indicated that sleep disturbance is characterised by insomnia symptoms. Bener & Al-Hamaq (2010) concluded that “symptoms of sleep are not to be ignored but discussed” (p. 339). In Vionescu et al.’s study (Voinescu, Vesa, & Coogan, 2011), sleep disturbance consisted of both insomnia that met the diagnostic criteria by the International Classification of Sleep Disorders (ICSD) and insomnia symptoms.
Impaired sleep quality and/or abnormal sleep duration
Based on the current evidence, sleep disturbance in people with diabetes was most commonly described as impaired sleep quality that is characterised by difficulty in initiating or maintaining sleep (Chasens, Sereika, & Burke, 2009; Happe, Treptau, Ziegler, & Harms, 2005; Izci-Balserak & Pien, 2014; Knutson, Van Cauter, Zee, Liu, & Lauderdale, 2011; Olsson et al., 2011; Reddy, Philpot, Ford, & Dunbar, 2010; Reutrakul & Van Cauter, 2014; Sridhar & Madhu, 1994; Sridhar & Putcha, 2006). For instance, Knutson et al. (2011) defined sleep disturbance as “self-reported difficulty falling asleep or waking up in the night three or more times per week plus average sleep efficiency of <80% based on actigraphy” (p. 1172). Frequent nocturnal awakening was also identified in several studies (Barnard et al., 2015; Caruso et al., 2014; Chasens et al., 2009; Fritschi & Redeker, 2015; Han et al., 2002; Izci-Balserak & Pien, 2014; Knutson et al., 2011; Reutrakul & Van Cauter, 2014). Different terms were used to express the same meaning of nocturnal awakening, such as arousal, sleep fragmentation or fragmented sleep. Izci-Balserak & Pien (2014) described sleep disturbance as including sleep dysfunction related to partial arousals (transition from deep sleep stages to lighter stages). Chasens et al. (2009) referred this aspect of sleep disturbance as “waking frequently during the night” (p. 456). Although the frequency and number of awakenings during night varied across studies, they are the hallmark of impaired sleep quality. Several studies used the generic term overall poor sleep quality as a characteristic of sleep disturbance (Bener & Al-Hamaq, 2010; Cho, Lee, Ryu, Choi, & Kim, 2014; Chontong, Saetung, & Reutrakul, 2016; van Dijk et al., 2011; Fritschi & Redeker, 2015; Reutrakul, Hood et al., 2013; Reutrakul, Zaidi et al., 2013; Voinescu et al., 2011; Wrobel et al., 2008).
Sleep disturbance can also be labelled as abnormal sleep duration, which includes both insufficient and long sleep duration. Insufficient sleep, sleep loss or sleep deprivation (whether voluntary or forced) was frequently referred to as a major characteristic of sleep disturbance (Bener & Al-Hamaq, 2010; Cho et al., 2014; Chontong et al., 2016; van Dijk et al., 2011; Fritschi & Redeker, 2015; Hazen et al., 2015; Knutson et al., 2011; Martins, Andersen, & Tufik, 2008; Reutrakul & Van Cauter, 2014; Reutrakul, Hood et al., 2013; Voinescu et al., 2011). Traditionally, insufficient sleep was considered a sleep disturbance. However, an increasing number of studies (Caruso et al., 2014; Hazen et al., 2015; Martins et al., 2008; Reddy et al., 2010) also describe long sleep duration as a characteristic of sleep disturbance. For instance, Reddy et al. (2010) defined sleep disturbance as “trouble falling or staying asleep, or sleeping too much” (p. 241).
3.1.3 |. Use of surrogate terms and related concepts
Several surrogate terms have been used interchangeably with sleep disturbance. Although sleep disorder is a distinctly different term from sleep disturbance, it has been used to mean sleep disturbance in several studies (Bener & Al-Hamaq, 2010; van Dijk et al., 2011; Keskin et al., 2015; Martins et al., 2008; Sridhar & Madhu, 1994; Voinescu et al., 2011). Other interchangeably used terms are sleep problem (Caruso et al., 2014; Cho et al., 2014; Olsson et al., 2011), sleep disruption (Barnard et al., 2015; Eshkoor, Hamid, Nudin, & Mun, 2015; Voinescu et al., 2011), disrupted sleep (Olsson et al., 2011; Sridhar & Putcha, 2006), abnormal sleep (Sridhar & Putcha, 2006), sleep complaint (Cho et al., 2014), sleep impairment (Martins et al., 2008) and impaired sleep (Chasens et al., 2009). Surprisingly, even in the same paper, different terms were used. For instance, Olsson et al. (2011) used sleep disturbance, sleep problem and disrupted sleep in their article, while Cho et al. (2014) used sleep complaint and sleep problem. This inconsistent use of different terms to express the same meaning has brought confusion to the field.
There are two main related concepts: sleep disorder and insomnia. A disorder (Roth, 2007) “is a condition associated with negative consequences, and importantly, these consequences are not a normal result of the condition but rather a result of some sort of pathological response” (p. s7). Sleep disorder is defined as disorders related to sleep; it is an umbrella term that consists of several classifications, including insomnia (Sateia, 2014). As the most commonly seen sleep disorder, insomnia has been treated as both a symptom and disorder that requires standard diagnosis (Sateia, 2014). The diagnostic criteria for insomnia include difficulty falling asleep, staying asleep or nonrestorative sleep despite circumstance allows; it is associated with daytime impairment or distress; it occurs at least three times per week for at least 1 month (Roth, 2007). Both insomnia and sleep disorder are used as diagnostic terms; however, people may have sleep disturbance that does not meet the diagnostic criterion. Examination of the included studies revealed that insomnia was frequently referenced in the definition of sleep disturbance. However, insomnia was not used as a disorder as defined by the ICSD-3, but rather a symptom. Thus, it is reasonable to differentiate sleep disturbance and insomnia.
3.1.4 |. Antecedents
Antecedents are events or situations preceding the concept of interest (Rodgers, 2000). Two major antecedents of sleep disturbance in people with diabetes were identified: diabetes-related physiological change and reduced psychological well-being. Studies supporting each antecedent are shown in Table 2.
TABLE 2.
Literature support for antecedents and consequences of sleep disturbance in people with diabetes
Diabetes-related physiological change
Diabetes-related physiological change is the most commonly seen antecedent of sleep disturbance. Diabetes itself can influence sleep disturbance (Fritschi & Redeker, 2015; Reutrakul, Zaidi et al., 2013). Sleep disturbance was suggested resulting from neuropathic symptoms, including pain and “burning soles,” which is a sensation of tingling or hot feet (Cho et al., 2014; van Dijk et al., 2011; Sridhar & Madhu, 1994; Sridhar & Putcha, 2006; Voinescu et al., 2011; Wrobel et al., 2008). People with diabetes frequently complain about waking up during the night to use the bathroom (Eshkoor et al., 2015; Sridhar & Putcha, 2006; Voinescu et al., 2011). Voinescu et al. (2011) also described that “diabetes itself is also associated with complications and symptoms, such as neuropathic pain, nocturia, and depression, that may contribute to sleep disorder” (p. 70). The underlying mechanisms for sleep disturbance in diabetes are unclear. Barone and Menna-Barreto (Barone & Menna-Barreto, 2011) indicated that diabetes and sleep disturbance together create a vicious circle through the regulation of sympathetic system, hypothalamic-pituitary-adrenal axis, appetite hormones and inflammatory processes. Particularly, glycaemic excursions or poor glycaemic control in people with diabetes could lead to sleep disturbance. In this review, several studies supported that glucose control could potentially contribute to sleep disturbance (Barnard et al., 2015; Caruso et al., 2014; Cho et al., 2014; van Dijk et al., 2011; Happe et al., 2005; Sridhar & Madhu, 1994). This perspective can be traced back to 1994 when Sridhar and Madhu (Sridhar & Madhu, 1994) indicated “sleep disturbances may be due to … fluctuations in metabolic control and perhaps also hyperinsulinemia” (p. 183). Caruso et al. (2014) suggested that “both nocturnal hypoglycemia and hyperglycemia will result in sleep disruption” (p. 1492).
Reduced psychological well-being
Psychological well-being is crucial to an individual’s overall health; it is another antecedent of sleep disturbance. Sleep disturbance in people with diabetes could be caused by psychological discomfort (Bener & Al-Hamaq, 2010). Psychological factors, including depression and mood, were also suggested contributing to sleep disturbance (Han et al., 2002; Hazen et al., 2015; Sridhar & Madhu, 1994; Voinescu et al., 2011). Han and colleagues even recommended routine assessment of depression to predict sleep disturbance status.
3.1.5 |. Consequences
Consequences are events or phenomenon that results from the concept (Rodgers, 2000). Three consequences usually follow after the occurrence of sleep disturbance: impaired daytime functioning, glucose regulation and quality of life. Studies supporting each consequence are shown in Table 2.
Impaired daytime functioning
Sleep disturbance can impair daytime functioning, including daytime sleepiness. Inadequate or disrupted sleep can result in complaints about daytime sleepiness (Chasens et al., 2009; Happe et al., 2005; Izci-Balserak & Pien, 2014; Nefs et al., 2015). Sleep disturbance made coping with diabetes difficult (Nefs et al., 2015; Sridhar & Madhu, 1994). In several studies (Barnard et al., 2015; Chasens et al., 2009; Hazen et al., 2015; Nefs et al., 2015), sleep disturbance was considered as having detrimental effects on diabetes-related self-care and decision-making, such as exercising regularly and eating healthily. Sleep disturbance might also explain the neurocognitive and behavioural deficits that are crucial for normal daytime functioning (Caruso et al., 2014).
Impaired glucose regulation
Sleep disturbance might impair glucose regulation in people with diabetes. “Decreased sleep duration and/or impaired sleep quality negatively influence glucoregulation” (van Dijk et al., 2011) (p. 1967). Reutrakul and Van Cauter concluded that there is “a causal relationship between sleep disturbances and alterations in multiple physiological pathways resulting in abnormal glucose metabolism, increased diabetes risk, and possibly contributing to poor glycemic control in people who are prediabetic or diabetic” (p. 163). Studies on the underlying pathways linking sleep disturbance to impaired glucose regulation are emerging. Such pathways include a decrease in brain glucose use, increase in sympathetic system activity and inflammation, as well as alteration in appetite-regulating hormones (Martins et al., 2008; Reutrakul & Van Cauter, 2014).
Impaired quality of life
Another consequence of sleep disturbance is the impaired quality of life. Sleep disturbance can have an enormous impact on health-related quality of life (Eshkoor et al., 2015; Sridhar & Madhu, 1994). “Awareness and identifying sleep complaints in such (diabetes) patients are necessary to improve their quality of daily life” (Cho et al., 2014) (p. 243) and “reduction of such (sleep) problems plays a critical role in improving the quality of life in the older people with diabetes” (Eshkoor et al., 2015) (p. S271).
3.1.6 |. Conceptual definition
Based on the attributes, antecedents and consequences identified above, we propose this definition of sleep disturbance in people with diabetes: sleep disturbance in people with diabetes is a symptom characterised by impaired sleep quality (e.g., difficulty in initiating or maintaining sleep or frequent nocturnal awakenings) and/or abnormal sleep duration. Sleep disturbance can result from diabetes-related or other physical/physiological impairment. Sleep disturbance can exert detrimental effects on daytime functioning, glucose regulation and quality of life. A description of this definition is provided in Figure 2.
FIGURE 2.
Conceptual model of the concept of sleep disturbance in people with diabetes
3.2 |. Providing exemplars
According to Rodgers (2000), an exemplar is not a model case, but it shows the empirical application of the concept within a context. It is not uncommon that no ideal exemplar can be identified. However, an exemplar should be identified (not constructed). Here, we provide two practical exemplars to demonstrate the current use of the concept of sleep disturbance in people with diabetes.
Both exemplars were case studies. The first exemplar came from Perfect and Elkins’s study with a 14-year-old Caucasian girl with type 1 diabetes (Perfect & Elkins, 2010). The second came from a case study of a 52-year-old female (Yoosefinejad, Shadmehr, Olyaei, Talebian, & Bagheri, 2014). Case characteristics, attributes, antecedents and consequences of the concept reflected in the case are shown in Table 3.
TABLE 3.
Exemplars demonstrating the empirical use of sleep disturbance in people with diabetes
| Exemplar | Participant characteristics | Attributes reflected | Antecedents reflected | Consequences reflected |
|---|---|---|---|---|
| Case 1 | 14-year-old girl with type 1 diabetes (Perfect & Elkins, 2010) Diabetes duration: 9 years Diabetes treatment regimen: insulin pump A1C: 8.9% Sleep: (i) complained about symptoms of trouble falling and staying asleep due to stress; (ii) experienced frequent awakenings due to concerns about hypoglycaemia; (iii) had an average of 6.8 hr of sleep, less than the recommended 8–10 hr for teenagers Sleep intervention effect: after the sleep intervention using cognitive-behavioural therapy and hypnotic relaxation, patient glucose regulation improved. The authors suggested that “the improvement may have been attributable, at least in part, a reduction in her stress and improvement in sleep.” (p. 9) |
Sleep disturbance as a symptom Sleep disturbance as impaired sleep quality (difficulty in initiating and maintaining sleep/frequent nocturnal awakenings) and abnormal sleep duration | Reduced psychological wellbeing (excessive stress) | Impaired glucose regulation as a consequence (supported by improvement in glycaemic control after treatment) |
| Case 2 | 52-year-old female with type 2 diabetes (Yoosefinejad et al., 2014) Diabetes duration: 10 years Diabetes complication: neuropathy characterised by a sensation of tingling and numbness in feet for 1 year Sleep: frequently awakened during the night by this abnormal sensation accompanied by pain scored 6 of 10 |
Sleep disturbance not explicitly described as a symptom Sleep disturbance as impaired sleep quality characterised by frequent nocturnal awakenings |
Diabetes-related physiological changes (i.e., neuropathic pain) |
4 |. DISCUSSION
4.1 |. Variations in the use of sleep disturbance
Likely, some data may not fit cleanly or solely within the themes identified above. Variations in the antecedents, attributes and consequences of sleep disturbance were observed. In this analysis, frequent snoring (Cho et al., 2014; Knutson et al., 2011; Reutrakul, Zaidi et al., 2013), obstructive sleep apnoea (Chontong et al., 2016; Martins et al., 2008; Reddy et al., 2010; Reutrakul & Van Cauter, 2014) or sleep-disordered breathing (Caruso et al., 2014; Reutrakul, Zaidi et al., 2013) were frequently described as sleep disturbance. However, snoring is a major sign of obstructive sleep apnoea. Obstructive sleep apnoea or sleep-disordered breathing may be potentially connected to sleep disturbance; they represent a common type of sleep disorder (Knutson et al., 2011). Additionally, impaired sleep quality and inadequate sleep were also described as consequences of sleep disturbance in two studies (Chasens et al., 2009; Izci-Balserak & Pien, 2014). Similarly, daytime sleepiness has been considered both an attribute (Sridhar & Madhu, 1994) and an antecedent (Eshkoor et al., 2015) rather than a consequence. These variations in the conceptual use of sleep disturbance suggest more studies are needed to further clarify the attributes of sleep disturbance in people with diabetes. Future inquiries on the relationship between sleep disturbance, obstructive sleep apnoea and daytime sleepiness would be useful. Regardless, the concept consensus reached in this analysis has important theoretical and clinical implications.
4.2 |. Interpreting the results and identifying implications
Studies involving sleep disturbance in people with diabetes have increased over the past two decades, particularly during the last 5 years (Table 1). This trend demonstrates the significance attached to this concept. However, confusions and ambiguities about its use across time indicate that the concept is still underdeveloped. Concept analysis is an inductive process that aims at clarifying and enhancing the ongoing development of a concept. Consequently, interpretation of the results has two contributions: illustrate current status of the concept and generate implications for future research and practice (Rodgers, 2000).
4.2.1 |. Theoretical implications
Riegel & Weaver (2009) proposed a conceptual model illustrating the mechanisms linking poor sleep and impaired self-care. Although the model was proposed for people with heart failure and not as a generalisable theory, the relationships among the major concepts provide us with possible future research directions. In that model, poor sleep could affect daytime behaviours (e.g., self-care) through its influence on cognition. Similarly, depression is, directly and indirectly, related to poor sleep. The attributes of sleep disturbance in people with diabetes are not perfectly in line with the ones described in Riegel and Weaver’s model. However, their model supported the explanatory power of the antecedents and consequences of sleep disturbance identified in this concept analysis.
The concept of sleep disturbance in people with diabetes has not been clearly defined. Alternate terms are abundant, such as sleep impairment, sleep problem and sleep disruption. Sleep disturbance is different from sleep disorder; researchers are recommended to make clear which term they are using and use it consistently. Surprisingly, sleep disturbance was operationalised without providing a clear theoretical definition in most of the analysed studies. Our analysis will provide a conceptual foundation for the use of the term “sleep disturbance” in diabetes. Evidence suggests that sleep disorders, particularly sleep apnoea, can cause sleep disturbance (i.e., sleep fragmentation and sleep loss) (Hetzenecker et al., 2016; Tasali, Mokhlesi, & Van Cauter, 2008). However, sleep apnoea was considered a characteristic of sleep disturbance in several studies included in this analysis. Whether there is a causal relationship between sleep apnoea and sleep disturbance remains to be explored. The antecedents and consequences of sleep disturbance identified provide directions for future studies on the risk factors and effects of sleep disturbance in people with diabetes. It is worth mentioning that the relationship between sleep and psychological well-being has been suggested to be bidirectional (Kahn, Sheppes, & Sadeh, 2013). Although psychological well-being emerged as an antecedent of sleep disturbance in this concept analysis, its potential role as a consequence warrants further investigation.
4.2.2 |. Clinical implications
Identification of the attributes of sleep disturbance in people with diabetes has important clinical implications. Besides the difficulty in initiating sleep, difficulty in maintaining sleep (particularly frequent nocturnal awakenings) is also a common characteristic of impaired sleep quality. The findings demonstrate unique aspects of sleep disturbance in people with diabetes. Thus, in clinical practice, nocturnal awakenings should be emphasised when evaluating sleep quality. Meanwhile, not only inadequate sleep but also long sleep duration is suggested to indicate sleep disturbance. Long sleep duration might be compensation for poor sleep quality (Ferrie et al., 2015), and sleeping too much has been explicitly articulated as sleep disturbance (Grandner, Jackson, Pak, & Gehrman, 2012). Therefore, clinicians and nurses should be encouraged to pay equivalent attention to long sleep duration as they do for short sleep duration.
Analysis of the antecedents and consequences of sleep disturbance helps to identify potential risk factors and adverse effects of sleep disturbance in people with diabetes. Most of the antecedents are modifiable or treatable, which emphasises the need for clinicians and nurses to conduct a comprehensive assessment to help identify and appropriately address these antecedents. For instance, diabetes-related physiological changes, including nocturia, neuropathy and glucose levels, should be evaluated. Patients need to be informed that, by keeping diabetes under control, which could delay the occurrence of complications, they might have a lower chance of developing sleep disturbance. Similarly, patients with neuropathic pain should be encouraged to seek effective pharmacological treatment. Sleep disturbance could result in consequences impairing disease stability and well-being. It is important for clinicians and nurses to beware of these potential consequences. Sleep disturbance is a symptom rather than a diagnosis. Patients might not understand the severity of this problem. Therefore, nurses are encouraged to deliver sleep-related education and thereby increase patients’ awareness of the importance of sleep. Such education could include the high prevalence and adverse consequences of sleep disturbance in people with diabetes. In those who already have sleep disturbance, nurses can provide healthy sleep suggestions, such as follow a sleep schedule and optimise the wake-up routine.
4.3 |. Limitations
Although an exhaustive search was conducted, the sample size remained small (n = 26). This is partly because numerous studies were excluded due to lack of descriptions of sleep disturbance. It also indicates that the concept is at an early stage of development. Examining the areas of agreement and disagreement across disciplines of the concept constitutes an important step of a concept analysis (Rodgers, 2000). Nevertheless, the interdisciplinary variation in sleep disturbance could not be examined because of the small number of available studies within each discipline. More research about sleep disturbance in people with diabetes will enable examination of the disciplinary context. Data extraction and analysis were solely conducted by the first author, which might bring bias. However, random check by a second reviewer helped to mitigate the potential bias.
5 |. CONCLUSION
This concept analysis was undertaken to define the concept of sleep disturbance in people with diabetes. The analysis provides a conceptual foundation for the use of sleep disturbance in clinical practice and research. Future research is needed to shed more light on the attributes of sleep disturbance, particularly interdisciplinary variations. Additional studies designed to identify the risk factors and consequences of sleep disturbance are needed to facilitate the development of a theoretical framework.
6 |. RELEVANCE TO CLINICAL PRACTICE
Findings from this study illustrate the characteristics of sleep disturbance in people with diabetes, which helps to raise awareness of the complexity and importance of sleep among healthcare communities. A collaborative clinical team approach, including multidisciplinary healthcare professionals and individuals with diabetes, would be beneficial to identify and manage sleep disturbance in people with diabetes effectively. In clinical practice, there is a need for routine assessment and intervention for sleep disturbance in people with diabetes. Regular health education regarding healthy sleep is recommended in both clinical and community settings.
What does this paper contribute to the wider global clinical community?
Findings from this study illustrate the characteristics of sleep disturbance in people with diabetes, which helps to raise awareness of the complexity of sleep and importance of addressing sleep disturbance.
Clarification of the theoretical definition provides a foundation for the operationalisation and measurement of sleep disturbance in people with diabetes, which would facilitate future research and clinical practice.
There is a need for routine sleep-related health education, assessment and intervention in people with diabetes in both clinical and community settings.
ACKNOWLEDGEMENTS
The authors thank Kevin Grandfield, Publication Manager, in the UIC Department of Biobehavioral Health Science, for editorial assistance.
Funding information
This project received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Footnotes
CONFLICTS OF INTEREST
No conflict of interest has been declared by the authors.
REFERENCES
- American Diabetes Association (2017). Standards of medical care in diabetes. Diabetes Care, 40, S25–S32. [DOI] [PubMed] [Google Scholar]
- Anothaisintawee T, Reutrakul S, Van Cauter E, & Thakkinstian A (2016). Sleep disturbances compared to traditional risk factors for diabetes development: Systematic review and meta-analysis. Sleep Medicine Reviews, 30, 11–24. [DOI] [PubMed] [Google Scholar]
- Barnard K, James J, Kerr D, Adolfsson P, Runion A, & Serbedzija G (2015). Impact of chronic sleep disturbance for people living with T1 diabetes. Journal of Diabetes Science and Technology, 10, 762–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barone MT, & Menna-Barreto L (2011). Diabetes and sleep: A complex cause-and-effect relationship. Diabetes Research and Clinical Practice, 91, 129–137. [DOI] [PubMed] [Google Scholar]
- Bendtson I, Gade J, Thomsen CE, Rosenfalck A, & Wildschiodtz G (1992). Sleep disturbance in IDDM patients with hypoglycemia. Sleep, 15, 74–81. [DOI] [PubMed] [Google Scholar]
- Bener A, & Al-Hamaq A (2010). Sleep quality and excessive daytime sleepiness in a Arab diabetic population. Biomedical Research-India, 21, 333–340. [Google Scholar]
- Caruso NC, Radovanovic B, Kennedy JD, Couper J, Kohler M, Kavanagh PS, … Lushington K (2014). Sleep, executive functioning and behaviour in children and adolescents with type 1 diabetes. Sleep Medicine, 15, 1490–1499. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2017). National diabetes statistics report, 2017. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services. [Google Scholar]
- Chasens ER, Sereika SM, & Burke LE (2009). Daytime sleepiness and functional outcomes in older adults with diabetes. The Diabetes Educator, 35, 455–464. [DOI] [PubMed] [Google Scholar]
- Cho EH, Lee H, Ryu OH, Choi MG, & Kim SW (2014). Sleep disturbances and glucoregulation in patients with type 2 diabetes. Journal of Korean Medical Science, 29, 243–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chontong S, Saetung S, & Reutrakul S (2016). Higher sleep variability is associated with poorer glycaemic control in patients with type 1 diabetes. Journal of Sleep Research, 25, 438–444. [DOI] [PubMed] [Google Scholar]
- Consensus Conference Panel, Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, … Grandner MA (2015). Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Journal of Clinical Sleep Medicine, 11, 843–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cormier RE (1990). Sleep disturbances In Walker HK, Hall WD, & Hurst JW (Eds.), Clinical methods: The history, physical, and laboratory examinations (pp. 398–403). Boston: Butterworths. [PubMed] [Google Scholar]
- van Dijk M, Donga E, van Dijk JG, Lammers GJ, van Kralingen KW, Dekkers OM, … Romijn JA (2011). Disturbed subjective sleep characteristics in adult patients with long-standing type 1 diabetes mellitus. Diabetologia, 54, 1967–1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eshkoor SA, Hamid TA, Nudin SSH, & Mun CY (2015). Can physical activity affect sleep disruption among the elderly with diabetes mellitus? International Journal of Diabetes in Developing Countries, 35, S271–S274. [Google Scholar]
- Ferrie JE, Kivimaki M, Akbaraly TN, Tabak A, Abell J, Davey Smith G, … Shipley MJ (2015). Change in sleep duration and type 2 diabetes: The Whitehall II Study. Diabetes Care, 38, 1467–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritschi C, & Redeker NS (2015). Contributions of comorbid diabetes to sleep characteristics, daytime symptoms, and physical function among patients with stable heart failure. Journal of Cardiovascular Nursing, 30, 411–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrard J (2011). Review matrix: How to abstract the research literature In Garrard J (Ed.), Health sciences literature review made easy: The matrix method, 3rd edn (pp. 105–126). Mississauga, ON: Jones & Bartlett Learning. [Google Scholar]
- Grandner MA, Jackson NJ, Pak VM, & Gehrman PR (2012). Sleep disturbance is associated with cardiovascular and metabolic disorders. Journal of Sleep Research, 21, 427–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall MH (2013). Sleep In Gellman MD, & Turner JR (Eds.), Encyclopedia of behavioral medicine (pp. 1795–1799). New York, NY: Springer. [Google Scholar]
- Han SY, Yoon JW, Jo SK, Shin JH, Shin C, Lee JB, … Suh SY (2002). Insomnia in diabetic hemodialysis patients: Prevalence and risk factors by a multicenter study. Nephron, 92, 127–132. [DOI] [PubMed] [Google Scholar]
- Happe S, Treptau N, Ziegler R, & Harms E (2005). Restless legs syndrome and sleep problems in children and adolescents with insulin-dependent diabetes mellitus type 1. Neuropediatrics, 36, 98–103. [DOI] [PubMed] [Google Scholar]
- Hazen RA, Fehr KK, Fidler A, Cousino MK, MacLeish SA, & Gubitosi-Klug R (2015). Sleep disruption in adolescents with type 1 diabetes mellitus: Relationships with adherence and diabetes control. Diabetes Management, 5, 257–265. [Google Scholar]
- Hetzenecker A, Escourrou P, Kuna ST, Series F, Lewis K, Birner C, … Arzt M (2016). Treatment of sleep apnea in chronic heart failure patients with auto-servo ventilation improves sleep fragmentation: A randomized controlled trial. Sleep Medicine, 17, 25–31. [DOI] [PubMed] [Google Scholar]
- Izci-Balserak B, & Pien GW (2014). The relationship and potential mechanistic pathways between sleep disturbances and maternal hyperglycemia. Current Diabetes Reports, 14, 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn M, Sheppes G, & Sadeh A (2013). Sleep and emotions: Bidirectional links and underlying mechanisms. International Journal of Psychophysiology, 89, 218–228. [DOI] [PubMed] [Google Scholar]
- Keskin A, Unalacak M, Bilge U, Yildiz P, Guler S, Selcuk EB, & Bilgin M (2015). Effects of sleep disorders on hemoglobin A1c levels in type 2 diabetic patients. Chinese Medical Journal-Peking, 128, 3292–3297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson KL, Van Cauter E, Zee P, Liu K, & Lauderdale DS (2011). Cross-sectional associations between measures of sleep and markers of glucose metabolism among subjects with and without diabetes: The Coronary Artery Risk Development in Young Adults (CARDIA) Sleep Study. Diabetes Care, 34, 1171–1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SW, Ng KY, & Chin WK (2017). The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: A systematic review and meta-analysis. Sleep Medicine Reviews, 31, 91–101. [DOI] [PubMed] [Google Scholar]
- Martins RC, Andersen ML, & Tufik S (2008). The reciprocal interaction between sleep and type 2 diabetes mellitus: Facts and perspectives. Brazil Journal of Medical and Biological Research, 41, 180–187. [DOI] [PubMed] [Google Scholar]
- Merriam-Webster (2016). Merriam-Webster’s Learners Dictionary. Retrieved from http://www.learnersdictionary.com/definition/disturbance (accessed May 13, 2016).
- Nefs G, Donga E, van Someren E, Bot M, Speight J, & Pouwer F (2015). Subjective sleep impairment in adults with type 1 or type 2 diabetes: Results from Diabetes MILES – The Netherlands. Diabetes Research and Clinical Practice, 109, 466–475. [DOI] [PubMed] [Google Scholar]
- Olsson L, Pettersen E, Ahlbom A, Carlsson S, Midthjell K, & Grill V (2011). No effect by the common gene variant rs10830963 of the melatonin receptor 1B on the association between sleep disturbances and type 2 diabetes: Results from the Nord-Trondelag Health Study. Diabetologia, 54, 1375–1378. [DOI] [PubMed] [Google Scholar]
- Perfect MM, & Elkins GR (2010). Cognitive-behavioral therapy and hypnotic relaxation to treat sleep problems in an adolescent with diabetes. Journal of Clinical Psychology, 66, 1205–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy P, Philpot B, Ford D, & Dunbar JA (2010). Identification of depression in diabetes: The efficacy of PHQ-9 and HADS-D. British Journal of General Practice, 60, e239–e245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reutrakul S, Hood MM, Crowley SJ, Morgan MK, Teodori M, Knutson KL, & Van Cauter E (2013). Chronotype is independently associated with glycemic control in type 2 diabetes. Diabetes Care, 36, 2523–2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reutrakul S, & Van Cauter E (2014). Interactions between sleep, circadian function, and glucose metabolism: Implications for risk and severity of diabetes. Annals of the New York Academy of Science, 1311, 151–173. [DOI] [PubMed] [Google Scholar]
- Reutrakul S, Zaidi N, Wroblewski K, Kay HH, Ismail M, Ehrmann DA, & Van Cauter E (2013). Interactions between pregnancy, obstructive sleep apnea, and gestational diabetes mellitus. Journal of Clinical Endocrinology & Metabolism, 98, 4195–4202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riegel B, & Weaver TE (2009). Poor sleep and impaired self-care: Towards a comprehensive model linking sleep, cognition, and heart failure outcomes. European Journal of Cardiovascular Nursing, 8, 337–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers BL (2000). Concept analysis: An evolutionary view In Rodgers BL, & Knafl KA (Eds.), Concept development in nursing: Foundations, techniques, and applications, 2nd edn (pp. 77–102). Philadelphia, PA: Saunders. [Google Scholar]
- Roth T (2007). Insomnia: Definition, prevalence, etiology, and consequences. Journal of Clinical Sleep Medicine, 3, S7–S10. [PMC free article] [PubMed] [Google Scholar]
- Rylance R, & Smith GM (2016). Sleep disorders In Rylance R, & Smith GM (Eds.), Rapid mental health nursing (pp. 119–122). Oxford: Wiley-Blackwell. [Google Scholar]
- Sateia MJ (2014). International classification of sleep disorders: Highlights and modifications. Chest, 146, 1387–1394. [DOI] [PubMed] [Google Scholar]
- Schulz H, & Salzarulo P (2015). The evolution of sleep medicine in the nineteenth and the early twentieth In Chokroverty S, & Billiary M (Eds.), Sleep medicine: A comprehensive guide to its development, clinical milestones, and advances in treatment (pp. 75–89). New York, NY: Springer, Springer Science+Business Media. [Google Scholar]
- Sridhar GR, & Madhu K (1994). Prevalence of sleep disturbance in diabetes mellitus. Diabetes Research and Clinical Practice, 23, 183–186. [DOI] [PubMed] [Google Scholar]
- Sridhar GR, & Putcha V (2006). Sleep and body weight in diabetes mellitus: A large retrospective analysis from South India. Diabetes Research and Clinical Practice, 72, 209–211. [DOI] [PubMed] [Google Scholar]
- Tasali E, Mokhlesi B, & Van Cauter E (2008). Obstructive sleep apnea and type 2 diabetes: Interacting epidemics. Chest, 133, 496–506. [DOI] [PubMed] [Google Scholar]
- Voinescu B, Vesa S, & Coogan A (2011). Self-reported diurnal reference and sleep disturbance in type 2 diabetes mellitus. Acta Endocrinologica-Bucharest, 7, 69–81. [Google Scholar]
- Wrobel MP, Szymborska-Kajanek A, Wystrychowski G, Biniszkiewicz T, Sieron-Stoltny K, Sieron A, … Strojek K (2008). Impact of low frequency pulsed magnetic fields on pain intensity, quality of life and sleep disturbances in patients with painful diabetic polyneuropathy. Diabetes Metabolism, 34, 349–354. [DOI] [PubMed] [Google Scholar]
- Yoosefinejad AK, Shadmehr A, Olyaei G, Talebian S, & Bagheri H (2014). Effects of whole-body vibration on a diabetic type 2 patient with peripheral neuropathy. Health Science Journal, 6, 576–583. [Google Scholar]