Abstract
Contrast-enhanced ultrasound (CEUS) is an emerging technology with no known nephrotoxicity. CEUS has been utilized in cardiac and abdominal imaging for decades in Asia and Europe and has recently received greater attention in the United States with its approval for characterization of indeterminate liver lesions. Emerging data suggest that CEUS has potential as a diagnostic imaging tool among individuals who have contraindications to CT and MRI. Few nephrologists are aware of CEUS and even fewer are aware of its potential applications among individuals with kidney disease. This review introduces CEUS to the nephrology community and provides a basic overview of CEUS technology. Knowledge of the applications, advantages, and disadvantages of CEUS provides the framework for nephrologists to make informed decisions regarding this emerging imaging test in appropriate circumstances. This review focuses on the use of CEUS for the characterization of indeterminate kidney lesions and summarizes the most recent data, some of which specifically includes patients with chronic kidney disease (CKD). The results demonstrate that CEUS has high sensitivity and moderate specificity for detecting malignancy in indeterminate kidney lesions among individuals with and without CKD. In conclusion, CEUS is an emerging imaging technique that may have clinically useful applications for detecting malignant kidney lesions, specifically in patients with CKD. However, most of the current data come from small, single-center studies, and larger, multicenter studies are needed.
Keywords: Chronic kidney disease, Contrast media, Ultrasound
Introduction
New imaging technologies capable of characterizing kidney anatomy and physiology have recently garnered increased attention as potential innovative diagnostic tools for nephrologists. Advances in ultrasound, an imaging technique known for its safety profile, low cost, patient tolerability, and bedside accessibility, are particularly promising. One such advance is contrast enhanced ultrasound (CEUS). Evaluation of the malignant potential of kidney lesions is currently the most common kidney-related clinical application of CEUS. As CEUS becomes more widely available, it is important that nephrologists understand its capabilities, advantages, and disadvantages. This review provides the practicing nephrologist with a basic understanding of CEUS and its potential clinical applications, particularly for the evaluation of kidney lesions.
Case
A 78-year old man with chronic kidney disease (CKD) stage 4 and estimated glomerular filtration rate (eGFR) of 20 mL/min/1.73 m2 presented to the nephrology clinic for routine CKD follow-up. Due to a recent increase in serum creatinine (2.3–3.0 mg/dL over 6 months), a kidney ultrasound was performed to evaluate for urinary obstruction. No obstruction was found, but a kidney lesion with internal vascularity by Doppler ultrasound was detected (Fig. 1). Further imaging with MRI was recommended. However, due to low eGFR, the MRI was performed without the gadolinium-based contrast agent. The non-contrast MRI showed a potential renal cell carcinoma (RCC), but results were inconclusive. The treating nephrologist and patient had to make tough decisions. The patient had to do one of the following: (1) pursue a definitive diagnosis via surgery, (2) pursue an accepted surrogate imaging diagnosis via contrast-enhanced CT, or (3) undergo non-contrasted imaging surveillance. All 3 choices carried potential risks.
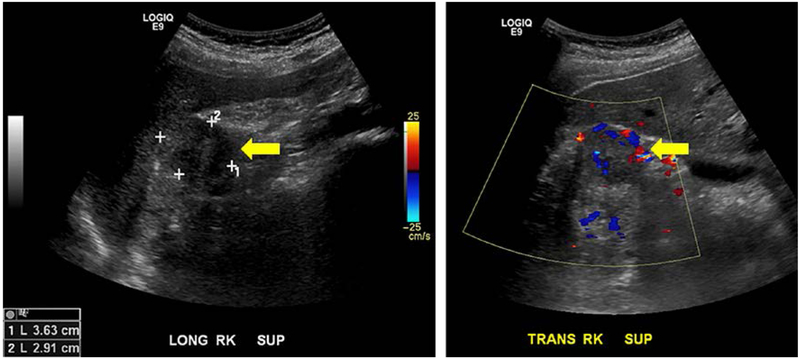
Fig. 1.
Ultrasound of lesion of interest. Left panel is the B-mode image in longitudinal plane. Right panel is the Doppler image in transverse plane. An arrow indicates the lesion of interest on each image.
The Problem
Scenarios similar to this case are increasingly common in clinical practice due to increased rates of detection of kidney lesions on imaging tests. A couple of overt factors contribute to this phenomenon. First, the prevalence of acquired cystic kidney disease and cystic RCC is greater in patients with CKD than in those without. This is evidence by a more than twofold increase in the incidence of RCC in patients with GFR <30 mL/min/1.73 m2 compared to those with GFR of 60–89 mL/min/1.73 m2 [1]. Nephrologists often utilize kidney ultrasound to rule out obstruction as the cause of acute kidney injury [2] and for guidance during kidney biopsy [3], leading to detection of incidental findings. Second, an increasing number of transplant programs use yearly native and transplant kidney ultrasounds to screen for new lesions [4, 5]. Contrasted imaging is often the next step in the work-up of an incidentally detected indeterminate or complex kidney lesion, but many patients with transplants with or without CKD have contraindications to contrast agents.
The risk of contrast-induced nephropathy from iodinated contrast agent exposure has been documented for decades. While recent data suggest that the risk of contrast-induced nephropathy is not as great as initially suspected in patients with mild CKD [6–8], most clinicians avoid iodinated contrast in patients with later stages of CKD (GFR <30 mL/min) and those on dialysis with residual kidney function. Until 2006, MRI with gadolinium-based contrast agent was used in individuals with CKD who could not receive iodinated contrast agents. However, the identification of Nephrogenic Sclerosing Fibrosis, a devastating condition related to the use of gadolinium-based contrast agents in patients with impaired kidney function [9, 10], led to a reduction of gadolinium exposure in patients with lower GFR essentially eliminating Nephrogenic Sclerosing Fibrosis [11, 12]. More recently, a new entity has emerged, called gadolinium deposition disease [13–15]. Patients with impaired kidney function are postulated to have greater accumulation of gadolinium in the brain than the general population [16], but the clinical significance of this finding is unclear.
These contraindications to contrast-enhanced CT and MRI are reflected in the 2014 American College of Radiology Appropriateness Criteria, which rank ultrasound with duplex Doppler as the first test for “indeterminate renal mass” among individuals with kidney insufficiency. MRI and CT with contrast are described as “usually not appropriate” [17].
GFR is not the only consideration when choosing an appropriate imaging study. MRI is contraindicated in patients with metal implants and can be challenging in children, obese patients, and patients with claustrophobia. CT involves radiation exposure, and allergies to iodinated contrast agents are relatively common [18]. Despite these drawbacks, both MRI and CT provide cross-sectional imaging, making it possible for detecting metastases and imaging of multiple organs. Ultrasound, on the other hand, is generally well tolerated, has no associated radiation exposure, and is substantially lower in cost than CT or MRI but only allows for imaging of a single organ at a time. Additionally, ultrasound is also highly operator dependent, requiring experienced sonographers. Considering these imaging advantages and disadvantages, ultrasound is often the initial kidney imaging modality used by nephrologists.
Contrast-Enhanced Ultrasound: A Potential Solution
Contrast Agent
Lack of information about enhancement characteristics is another critical drawback of standard B-mode ultrasound. Duplex Doppler ultrasound imaging, when added to standard B-mode ultrasound, allows for the detection of blood flow but is not sensitive to slower flow in small vessels. However, in the 1980s, the introduction of ultrasound contrast agents, which consist of microbubbles, addressed this deficiency and paved the way for modern CEUS imaging.
Microbubbles consist of a high molecular weight gas core surrounded by a lipid or albumin shell and have evolved over the years to be more persistent in the circulation, allowing for longer imaging times. The distinct advantage of microbubble contrast agents over CT and MRI contrast agents is their safety profile, particularly for patients with kidney disease. Microbubbles have no known kidney adverse effects. The drug is well tolerated with the majority of adverse effects being transient, while it is still in circulation, and not requiring medical treatment [19]. The most serious risk is a true allergic reaction to the gas in the microbubbles, which has been reported in a small number of patients (0.006–0.009%) [19, 20].
The Evolution of Safety Issues Related to Microbubbles and CEUS
While the overall safety of microbubble contrast agents is now more generally accepted, this has not always been the case. The earliest data on microbubble safety come from the field of cardiology, the specialists with the most experience with CEUS. The controversial contraindications to ultrasound contrast agents are primarily among individuals with cardiopulmonary disease states. One study of individuals with cardiopulmonary disease reported 4 deaths that were temporally related but not clearly attributable to contrast agent injection [21], leading to the institution of an FDA black box warning in 2007. The black box warning listed cardiopulmonary disease states as contraindications to the use of CEUS and instituted a 30-min monitoring period after the administration of injection for all individuals [21].
CEUS usage dropped significantly following the issue of this black box warning, prompting the publication of numerous subsequent reports and studies demonstrating CEUS safety and efficacy [22, 23]. In response, FDA revised product labels in late 2008 and changed the contraindications to warnings and removed the mandatory 30-min monitoring period for all patients except those with pulmonary hypertension and unstable cardiopulmonary conditions. Further investigations into safety were conducted, including one retrospective review of over 15,000 propensity matched critically ill patients [24]. In 2011, FDA removed the 30-min monitoring period among patients with pulmonary hypertension and unstable cardiopulmonary conditions and modified the black box warning to state that severe reactions occur uncommonly.
Since that time, safety studies have focused on microbubble use in specific disease populations, including individuals with pulmonary hypertension [25] and right-to-left intracardiac shunts [26] and in specific imaging modalities (resting and stress echocardiograms) [27]. The low rate of serious adverse events has remained consistent in these subsequent studies. Currently, the only contraindication listed on the package inserts for the contrast agents – Lumason, Definity, and Optison – is known hypersensitivity to any of the contrast agent contents. The FDA removed the cardiac shunt contraindication for all 3 US-marketed agents by early 2017. All agents maintain a black box warning of the uncommon occurrence of serious cardiopulmonary reactions necessitating the availability of resuscitation equipment and trained personnel on site.
Specific safety issues related to kidney CEUS have also been examined in animal studies. Preclinical studies in rat and pig kidneys suggest potential risks of injury from CEUS based on histologic findings of glomerular capillary hemorrhage, surface bruising, and microhematuria [28–30]. However, contrast dose, mechanical index (MI) settings, frequency of ultrasound pulse, and total exposure used in these studies were much higher than those used in clinical applications (Table 1). For this reason, limits on maximal MI and total contrast dose are placed on clinical CEUS imaging. The potential for clinically significant bioeffects should be periodically reevaluated as experience with CEUS increases.
Table 1.
Current clinically available ultrasound contrast agents
| Sonovue®/lumason® | Definity®/luminity® | Optison® | Sonazoid® | |
|---|---|---|---|---|
| Manufacturer | Bracco imaging | Lantheus medical imaging | GE healthcare | GE healthcare/daiichi sankyo |
| Approval indication(s) | LVO/EBD, breasta, livera, vasculara, urinary tract | LVO/EBD, livera, kidneya, vasculara | LVO/EBD | Myocardial perfusiona, livera, breasta |
| Countries available | North America, New Zealand, Europe, Brazil, Asia | North America, Europe, Australia, Asia | North America, Europe | Japan, South Korea, Norway |
| Shell/gas | Phospholipid/sulfur hexafluoride | Phospholipid/perflutren | Albumin/perflutren | Phospholipid/perfluorobutane |
| Contraindications | Hypersensitivity to sulfur hexafluoride or any inactive ingredient in lumason | Hypersensitivity to perflutren | Hypersensitivity to perflutren, blood, blood products or albumin | Egg allergy |
| Vial supplied | 10 mL vial containing 25 mg powder 5 mL saline |
2 mL vials | 3 mL vials | 16 μL vial 2 mL solvent |
| Storage | Room temperature | 2°−8°C | 2°−8°C | Unable to identify |
| Typical doses | 2 mL of reconstituted agent | Weight based bolus (10 μL/kg) or infusion rate of 4.0 mL/min of 1.3 + 50 mL saline | 0.5 mL | Weight based 15 μL/kg or 0.12 μL MB/kg |
| Administration recommendation | Bolus Bolus dose can be repeated once Doses varies depending on age and indication |
Bolus or infusion Dose varies based on organ being imaged |
Rate not to exceed 1 mL/s Max dose in 10 min: 5.0 mL Max dose for one study: 8.7 mL |
Bolus or infusion |
| MI | MI ≤0.8 | MI ≤0.8 | Safety of MI >0.8 has not been tested | Unable to identify |
| Advantages | Approved for use in pediatric populations Reconstitution by hand mixing |
Bolus or infusion | Resuspension by hand mixing | Bolus or infusion |
| Disadvantages | Bolus and infusion dosing are used, although package insert only describes bolus dosing | Requires 45-s activation on VialMix®. Hand agitation thereafter if being used >5 min after activation | Typically only bolus dosing | Usually only single dose administration |
LVO, left ventricular opacification; EBD, endocardial border definition; R-L, right-to-left; MB, microbubble; MI, mechanical index.
Only in certain countries.
Implementation of CEUS
Determination of the best imaging protocol (contrast agent, method of administration, and type of imaging) varies based on individual radiologist and institutional practices, the clinical scenario and the imaging indication. Contrast agents currently approved for clinical use are summarized in Table 1 [31, 32]. CEUS contrast agents are activated either by shaking or reconstituting a powder in solvent. Intravenous injection is typically performed through a forearm 20-gauge or larger catheter in order to avoid microbubble disruption.
Injection can be either by bolus or by infusion. Bolus dosing uses low MI settings of <0.2 in order to prevent microbubble destruction. Video clips of contrast agent entry into the plane of imaging (wash-in) and exit of contrast agent form the plane of imaging (wash-out) are captured. Depending on the agent, repeat bolus dosings may be administered. Total imaging time typically ranges from 5 to15 min (3–5 min per dose with 5 min between doses). In contrast, infusion dosing requires dilution of the contrast agent before it is injected at a constant rate. This method provides longer actual imaging time (10–15 min), but does not capture wash-out. Because of the longer imaging time, several planes can be imaged using the flash-replenishment technique in which a higher MI (0.8–1.1) brief pulse or flash (≤1 s) destroys the microbubbles in the field, and reperfusion of microbubbles in the imaged plane is captured. This technique raises the possibility of bioeffects when using infusion imaging as described in animal studies [28, 29]. However, the MI levels used in clinical imaging remain well below the levels used in these animal studies.
During both bolus and infusion administration, a dual mode display (B-mode and contrast mode) allows the sonographer to localize the lesion by B-mode and maintain the probe in the correct location during enhancement. Because a low MI setting is used to avoid microbubble destruction, B-mode images in dual mode are of poor quality and used only for localization.
Advantages and disadvantages exist for both the bolus and infusion approaches to contrast administration. Due to the complex nature of contrast agents and indications for imaging, close consultation with the radiologist is an essential step to selecting the best imaging protocol and ultimately obtaining the most optimal diagnostic studies.
Comparison to Other Modalities
CEUS has several other potential advantages over CT and MRI. In contrast to iodinated or gadolinium-based contrast agents, which extravasate out of the vasculature, CEUS microbubbles remain intravascular and therefore reflect tissue perfusion. CEUS is thus more sensitive to enhancement than contrast-enhanced CT or MRI.
Another unique attribute of CEUS is the ability to obtain real-time imaging. The entry and exit of microbubbles into and out of the imaging plane (with bolus dosing) facilitate enhancement of the plane in its entirety, as opposed to contrast-enhanced CT or MRI, which provides images at single snapshots in time. Thus, if a certain phase of enhancement is missed by CT or MR, the diagnosis may be missed. Image enhancement in real time provides a detailed understanding of enhancement characteristics. In the case of indeterminate liver imaging, such real-time imaging helps distinguish between benign liver lesions and hepatocellular carcinoma [33–35].
CEUS does have limitations. Like standard ultrasound, CEUS takes single plane images. With infusion dosing, several different planes can be imaged with a single vial. Currently, CEUS-based three-dimensional rendering of whole organs is not available but may become possible in the future with transducer and image-processing advancements. For this reason, CEUS cannot be used to identify metastases or for whole body cross-sectional imaging as can CT or MRI. In addition, consistent CEUS images can be difficult to obtain in patients with large body habitus or who cannot hold their breath. Because of these challenging features, CEUS sonography requires more training and specialized skills than technicians administering MRI or CT.
Approved Indications for CEUS
The World Federation of Ultrasound in Medicine and Biology and European Federation for the Society of Ultrasound in Medicine and Biology Guidelines from 2012 provide recommendations for liver applications of CEUS [36]. The 2011 European Federation for the Society of Ultrasound in Medicine and Biology Guidelines for non-hepatic applications [19] provide recommendations for use of CEUS for non-liver imaging, including the pancreas, gastrointestinal tract, and genitourinary tract. The specific kidney indications include kidney infarct and cortical necrosis, abscesses, characterization of indeterminate lesions when conventional ultrasound is equivocal, determination of surgical strategy for complex cystic masses, follow-up imaging of non-surgical complex masses, and tumor ablation under ultrasound guidance.
In the United States, the use of CEUS is growing. Three ultrasound contrast agents are currently FDA approved for intravenous use (Table 1): Lumason (Bracco, Milan, Italy), Definity (Lantheus, North Billerica, MA, USA) and Optison (GE Healthcare, Oslo, Norway). All 3 agents are FDA-approved for cardiac imaging for the delineation of the endocardial border in suboptimal echocardiograms. One other agent, Sonazoid (GE Healthcare/Daiichi Sankyo, Oslo, Norway/Tokyo, Japan) is available outside the United States (Table 1). The FDA approval of Lumason for imaging of indeterminate liver lesions in April 2016 is likely to lead to a surge of interest in CEUS liver-based programs [37]. In June 2016, The American College of Radiology incorporated CEUS into the Liver Imaging Reporting and Data System, a standardized system for interpreting, reporting, and collecting data for radiologic exams in patients with an indeterminate liver lesion at risk for developing hepatocellular carcinoma [35].
In the United States, Lumason is also FDA-approved for voiding cystourethrogram, which requires intravesical injection of microbubbles. Utilization of this test by pediatric radiologists is on the rise, as it reduces radiation exposure for children [38]. While CEUS kidney lesion imaging is currently an off-label use, some centers have used CEUS for this indication for over a decade [37].
Evidence for the Use of CEUS for Lesion Characterization in the Kidney
In our prior published review of studies investigating the accuracy of CEUS for diagnosing kidney lesions, we reported that the overall sensitivity of CEUS for characterization of indeterminate kidney lesions is high and specificity is moderate [29]. These findings are comparable to the accuracy of both contrast-enhanced CT and MRI [39]. Since the publication of that review, additional CEUS studies, several including patients with CKD, have been published [40–45] and are summarized in Table 2. In summary, CEUS sensitivity for malignancy was consistently high, ranging from 90 to 100% [39, 42, 43, 45] and was either equal to, or better, than contrast-enhanced CT in studies directly comparing CEUS to contrast-enhanced CT, even among individuals with CKD [43, 44, 46–48]. CEUS specificity for malignancy ranges from 50 to 99%, with most studies in the 70–99% range, even among individuals with CKD [39, 42–44]. In one prospective study specifically including patients with CKD, sensitivity was shown to remain high at 90% in individuals with CKD [45].
Table 2.
Characteristics of studies since 2016 evaluating CEUS for characterization of kidney lesions (solid and cystic)
| Author | Country, year | Study type (n, lesion type) | Inclusion criteria | Inclusion of CKD? | Gold standard (n) | Modalities compared | Method of analysis | Results |
|---|---|---|---|---|---|---|---|---|
| Sanz et al. [44] | Spain (2016) | Prospective (67, all cystic) | Complex cystic kidney lesion | Not specified | Histology (24) Imaging follow-up (43) |
CECT | 1 reader (Bosniak) | CECT: sens 73%, spec 84%, PPV 67%, NPV 88% CEUS: sens 100%, spec 81%, PPV 70%, NPV 100% |
| Sawhney and Wilson [40] | Canada (2017) | Prospective (35 kidney cases, both solid and cystic) | Patients for which NECT ordered due to a contra-indication to CECT | Yes (Cr >1.5 mg/dL) | Histology or Imaging follow-up (numbers not specified) | NECT | 2 blinded readers (not specified) | Detecting pathology: NECT: sens 89% Conv US: sens 100% Characterizing pathology: NECT: sens 7% Conv US: sens 7% CEUS: sens 89% |
| Girometti et al. [41] | Italy (2017) | Observational (41 total: 21 solid and 20 cystic) | Patients with impaired kidney function and l esion on kidney CEUS | Yes (GFR <60 mL/min/1.73m2) | Histology (16) Imaging follow-up (25) |
N/A | 2 blinded readers (solid vs. cystic, Bosniak if cystic) | Descriptive statistics on a per lesion basis only |
| Zarzour et al. [42] | United States (2017) | Observational (41 with the reference standard, both solid and cystic) | Indeterminate CT, MRI or conv US studies | Yes (GFR <60 mL/min/1.73m2 or transplant) | Histology (16) Imaging follow-up (25) |
N/A | 1 blinded reader (adapted Barr) | CEUS: sens 100%, spec 86%, PPV 87%, NPV 100%, Acc 90% |
| Defortescu et al. [43] | France (2017) | Prospective (47, all cystic) | Bosniak 2F or 3 cyst on CECT | Not specified | Histology (19) Imaging follow-up (28) |
CECT CE-MRI |
1 blinded reader (enhancing) | CECT: sens 36%, spec 76%, PPV 38%, NPV 74%, Acc 64% CE-MRI: sens 71%, spec 91%, PPV 77%, NPV 88%, Acc 85% CEUS: sens 100%, spec 97%, PPV 93%, NPV 100%, Acc 98% |
| Chang et al. [45] | United States (2017) | Prospective (44, 26 cystic) | Suspicious lesion or CKD and indeterminate lesion on prior imaging | Yes (CKD stages II-VI or transplant) | Histology (23) Imaging follow-up (21) |
none | 2 blinded readers (Bosniak) | CEUS: sens 96%, spec 50% CEUS (CKD): sens 90%, spec 55% |
CKD, chronic kidney disease; conv, conventional; CECT, contrast-enhanced CT; NECT, non-enhanced CT; US, ultrasound; CEUS, contrast-enhanced ultrasound; CE-MRI, contrast-enhanced MRI; sens, sensitivity; spec, specificity; PPV, positive predictive value; NPV, negative predictive value; Acc, accuracy.
Findings from CEUS and CT are most often discordant in cases where CEUS suggests malignancy and CT does not [44]. One reason for this discrepancy is the difference in the ability of CEUS and CT to detect flow in septa and nodules of cystic lesions. Because microbubbles are purely intravascular, CEUS can detect enhancement where contrast-enhanced CT or MRI cannot [42, 46, 49]. This feature of CEUS may partially explain its moderate specificity. For this reason, several studies used a different classification scale [42, 48, 50] than the standard Bosniak criteria originally developed for contrast-enhanced CT. It is plausible that modified Bosniak criteria may improve CEUS specificity, but additional work in this regard is needed.
Another advantage of CEUS is the lack of nephrotoxicity or adverse effects of microbubbles in patients with CKD. This has led to the prevailing belief that CEUS may be a reasonable alternative to contrast CT and MRI when contrast contraincdiations exist, but additional studies should be performed in such populations [40, 41].
Taken together, the complete body of work suggests that CEUS has potential as an alternative tool for the evaluation of indeterminate kidney lesions, particularly in patients with CKD or other populations with contraindications to contrast-enhanced CT or MRI. However, larger, multicenter studies need to be conducted to prove accuracy in these populations and determine the most appropriate diagnostic criteria.
Indeterminate Kidney Cyst Characterization with CEUS: Clinical Implementation
Use of kidney CEUS for lesion characterization is more widespread in Asia and Europe than in the United States. However, there is growing interest in establishing new CEUS programs at US institutions and elsewhere [37]. Institutions with extensive CEUS experience are offering training programs for radiologists and sonographers that will help radiologists and sonographers to gain up-to-date knowledge on techniques and interpretation. A successful CEUS program is further enhanced when ordering clinicians understand CEUS technology and its capabilities, advantages, and disadvantages, thus increasing the likelihood of its appropriate use.
Other institutional hurdles must be addressed before and during the development of a CEUS program. For example, contrast agents need to be added to the hospital formulary, and many institutions will require a safety review of existing data prior to approval. The pharmacy needs to determine the most appropriate storage plan since pharmacies and ultrasound suites are not always in close proximity. Appropriate billing charges need to be established for radiologist and sonographer compensation.
Potential Future Nephrology Applications
An exciting new frontier in CEUS research is the use of targeted microbubbles in which antibodies are attached to the outer shell of the microbubbles [51]. Targeted microbubbles are injected intravenously and if they encounter their molecular target during circulation, the bubble will adhere at the site and no longer circulate. Adherence, and thus the presence of the target, is measured by quantifying the persistence of enhancement [51].
The angiogenic signaling receptor, VEGFR-2, has been investigated as a molecular target in various cancers [52–54], particularly as a tool to monitor response to treatment [52, 54]. The endothelial cellular adhesion molecule, P-selectin, was investigated in mice undergoing ischemia reperfusion injury to the kidneys [55] and chemically induced colitis [56] and was shown to produce an increased signal in comparison to nontargeted microbubbles. Similarly, vascular cellular adhesion molecule 1 has been investigated in a rat atherosclerosis model [57] and in mice on a hypercholesterolemic diet [58]; it demonstrated increased signal intensity when compared to nontargeted microbubbles.
If microbubbles can detect disease by using molecular targets, this attribute can also be used to deliver therapy specifically to these locations, reducing systemic exposure. Examples of therapies include disruption of microbubbles at the disease site to produce cavitation, delivery of chemotherapy to a disease site to reduce systemic side effects, and delivery of gene therapy [51].
Case Conclusion
The patient with CKD stage 4 and an incidentaloma of undetermined clinical significance underwent CEUS to further characterize the kidney lesion. CEUS showed a cystic lesion with a clearly enhancing, large solid component (Fig. 2) consistent with an RCC. Due to the likelihood of progression to end-stage kidney disease with a partial nephrectomy, and the knowledge that RCC is typically slow-growing with no metastases identified on previous MRI, the patient opted for lesion surveillance with noncontrast MRI. The diagnosis was made without exposure to either iodinated contrast or gadolinium. The patient’s stated top priority was to remain off of dialysis as long as possible. Kidney function has remained stable at an eGFR of 20 mL/min/1.73 m2 one year after the initial diagnosis.
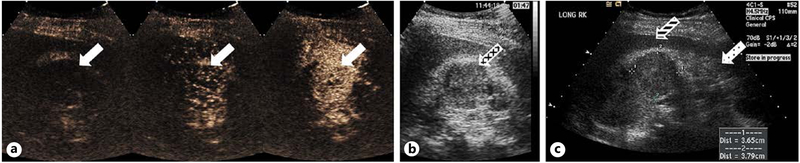
Fig. 2.
Contrast-enhanced ultrasound of the lesion of interest. The 3 images in (a) represent sequential images during wash-in enhancement of the lesion. A solid arrow denotes the lesion of interest. b Corresponding B-mode image taken in dual mode during contrast administration with a cross-hatched arrow denoting the lesion of interest. The dual mode B-mode image is of poor quality due to the low MI required to avoid bubble destruction. A true B-mode image taken prior to contrast administration is provided in (c). A dotted arrow denotes the kidney, and a striped arrow denotes the adjacent liver.
Conclusion
There is growing evidence supporting a role for CEUS in kidney lesion characterization. Existing CEUS data demonstrate high sensitivity and moderate specificity for the detection of malignant kidney lesions. Continued experience, training, and additional research are needed to improve the diagnostic accuracy of CEUS, ensure its safety, and determine the role of CEUS in kidney care. CEUS may be an option for patients in whom avoidance of MRI and CT contrast agents is desired, due to its adverse effect profile and tolerability. As use of CEUS continues to grow, it is important that nephrologists are aware of this technology and have an understanding of its capabilities and applications.
Footnotes
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- 1.Lowrance WT, Ordoñez J, Udaltsova N, Russo P, Go AS: CKD and the risk of incident cancer. J Am Soc Nephrol 2014;25:2327–2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Faubel S, Patel NU, Lockhart ME, Cadnapaphornchai MA: Renal relevant radiology: use of ultrasonography in patients with AKI. Clin J Am Soc Nephrol 2014;9:382–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maya ID, Maddela P, Barker J, Allon M: Percutaneous renal biopsy: comparison of blind and real-time ultrasound-guided technique. Semin Dial 2007;20:355–358. [DOI] [PubMed] [Google Scholar]
- 4.Filocamo MT, Zanazzi M, Li Marzi V, Guidoni L, Villari D, Dattolo E, Nicita G: Renal cell carcinoma of native kidney after renal transplantation: clinical relevance of early detection. Transplant Proc 2009;41:4197–4201. [DOI] [PubMed] [Google Scholar]
- 5.Frascà GM, Sandrini S, Cosmai L, Porta C, Asch W, Santoni M, Salviani C, D’Errico A, Malvi D, Balestra E, Gallieni M: Renal cancer in kidney transplanted patients. J Nephrol 2015;28:659–668. [DOI] [PubMed] [Google Scholar]
- 6.McDonald JS, McDonald RJ, Carter RE, Katzberg RW, Kallmes DF, Williamson EE: Risk of intravenous contrast material-mediated acute kidney injury: a propensity score-matched study stratified by baseline-estimated glomerular filtration rate. Radiology 2014;271:65–73. [DOI] [PubMed] [Google Scholar]
- 7.Wilhelm-Leen E, Montez-Rath ME, Chertow G: Estimating the Risk of Radiocontrast-Associated Nephropathy. J Am Soc Nephrol 2017;28:653–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hinson JS, Ehmann MR, Fine DM, Fishman EK, Toerper MF, Rothman RE, Klein EY: Risk of acute kidney injury after intravenous contrast media administration. Ann Emerg Med 2017;69:577–586.e574. [DOI] [PubMed] [Google Scholar]
- 9.Grobner T: Gadolinium–a specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis? Nephrol Dial Transplant 2006;21:1104–1108. [DOI] [PubMed] [Google Scholar]
- 10.Marckmann P, Skov L, Rossen K, Dupont A, Damholt MB, Heaf JG, Thomsen HS: Nephrogenic systemic fibrosis: suspected causative role of gadodiamide used for contrast-enhanced magnetic resonance imaging. J Am Soc Nephrol 2006;17:2359–2362. [DOI] [PubMed] [Google Scholar]
- 11.Becker S, Walter S, Witzke O, Kreuter A, Kribben A, Mitchell A: Application of gadolinium-based contrast agents and prevalence of nephrogenic systemic fibrosis in a cohort of end-stage renal disease patients on hemodialysis. Nephron Clin Pract 2012;121:c91–c94. [DOI] [PubMed] [Google Scholar]
- 12.Soulez G, Bloomgarden DC, Rofsky NM, Smith MP, Abujudeh HH, Morgan DE, Lichtenstein RJ, Schiebler ML, Wippold FJ 2nd, Russo C, Kuhn MJ, Mennitt KW, Maki JH, Stolpen A, Liou J, Semelka RC, Kirchin MA, Shen N, Pirovano G, Spinazzi A: Prospective cohort study of nephrogenic systemic fibrosis in patients with stage 3–5 chronic kidney disease undergoing MRI with injected gadobenate dimeglumine or gadoteridol. AJR Am J Roentgenol 2015;205:469–478. [DOI] [PubMed] [Google Scholar]
- 13.Kanda T, Fukusato T, Matsuda M, Toyoda K, Oba H, Kotoku J, Haruyama T, Kitajima K, Furui S: Gadolinium-based contrast agent accumulates in the brain even in subjects without severe renal dysfunction: evaluation of autopsy brain specimens with inductively coupled plasma mass spectroscopy. Radiology 2015:276:228–232. [DOI] [PubMed] [Google Scholar]
- 14.McDonald RJ, McDonald JS, Kallmes DF, Jentoft ME, Murray DL, Thielen KR, Williamson EE, Eckel LJ: Intracranial Gadolinium Deposition after Contrast-enhanced MR Imaging. Radiology 2015:275:772–782. [DOI] [PubMed] [Google Scholar]
- 15.Olchowy C, Cebulski K, Łasecki M, Chaber R, Olchowy A, Kalwak K, Zaleska-Dorobisz U: The presence of the gadolinium-based contrast agent depositions in the brain and symptoms of gadolinium neurotoxicity – a systematic review. PLoS One 2017;12: e0171704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cao Y, Zhang Y, Shih G, Zhang Y, Bohmart A, Hecht EM, Prince MR: Effect of renal function on gadolinium-related signal increases on unenhanced T1-weighted brain magnetic resonance imaging. Invest Radiol 2016;51: 677–682. [DOI] [PubMed] [Google Scholar]
- 17.ACR, Appropriateness Criteria Indeterminate Renal Mass, 2014. [DOI] [PubMed] [Google Scholar]
- 18.Dillman JR, Ellis JH, Cohan RH, Strouse PJ, Jan SC: Frequency and severity of acute allergic-like reactions to gadolinium-containing i.v. contrast media in children and adults. AJR Am J Roentgenol 2007;189:1533–1538. [DOI] [PubMed] [Google Scholar]
- 19.Piscaglia F, Nolsøe C, Dietrich CF, Cosgrove DO, Gilja OH, Bachmann Nielsen M, Albrecht T, Barozzi L, Bertolotto M, Catalano O, Claudon M, Clevert DA, Correas JM, D’Onofrio M, Drudi FM, Eyding J, Giovannini M, Hocke M, Ignee A, Jung EM, Klauser AS, Lassau N, Leen E, Mathis G, Saftoiu A, Seidel G, Sidhu PS, ter Haar G, Timmerman D, Weskott HP: The EFSUMB guidelines and recommendations on the clinical practice of contrast enhanced ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med 2012;33:33–59. [DOI] [PubMed] [Google Scholar]
- 20.Piscaglia F, Bolondi L; Italian Society for Ultrasound in Medicine and Biology (SIUMB) Study Group on Ultrasound Contrast Agents: The safety of Sonovue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol 2006;32:1369–1375. [DOI] [PubMed] [Google Scholar]
- 21.Main ML, Goldman JH, Grayburn PA: Thinking outside the “box”-the ultrasound contrast controversy. J Am Coll Cardiol 2007;50: 2434–2437. [DOI] [PubMed] [Google Scholar]
- 22.Main ML, Ryan AC, Davis TE, Albano MP, Kusnetzky LL, Hibberd M: Acute mortality in hospitalized patients undergoing echocardiography with and without an ultrasound contrast agent (multicenter registry results in 4,300,966 consecutive patients). Am J Cardiol 2008;102:1742–1746. [DOI] [PubMed] [Google Scholar]
- 23.Wei K, Mulvagh SL, Carson L, Davidoff R, Gabriel R, Grimm RA, Wilson S, Fane L, Herzog CA, Zoghbi WA, Taylor R, Farrar M, Chaudhry FA, Porter TR, Irani W, Lang RM: The safety of deFinity and Optison for ultrasound image enhancement: a retrospective analysis of 78,383 administered contrast doses. J Am Soc Echocardiogr 2008;21:1202–1206. [DOI] [PubMed] [Google Scholar]
- 24.Main ML, Hibberd MG, Ryan A, Lowe TJ, Miller P, Bhat G: Acute mortality in critically ill patients undergoing echocardiography with or without an ultrasound contrast agent. JACC Cardiovasc Imaging 2014;7:40–48. [DOI] [PubMed] [Google Scholar]
- 25.Wever-Pinzon O, Suma V, Ahuja A, Romero J, Sareen N, Henry SA, De Benedetti Zunino M, Chaudhry FF, Suryadevara RS, Sherrid MV, Chaudhry FA: Safety of echocardiographic contrast in hospitalized patients with pulmonary hypertension: a multi-center study. Eur Heart J Cardiovasc Imaging 2012; 13:857–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kalra A, Shroff GR, Herzog CA: Safety of ultrasound contrast agents in patients with intracardiac shunts. J Am Soc Echocardiogr 2014;27:1359. [DOI] [PubMed] [Google Scholar]
- 27.Platts DG, Luis SA, Roper D, Burstow D, Call T, Forshaw A, Pascoe R: The safety profile of perflutren microsphere contrast echocardiography during rest and stress imaging: results from an Australian multicentre cohort. Heart Lung Circ 2013;22:996–1002. [DOI] [PubMed] [Google Scholar]
- 28.Miller DL, Dou C, Wiggins RC: Glomerular capillary hemorrhage induced in rats by diagnostic ultrasound with gas-body contrast agent produces intratubular obstruction. Ultrasound Med Biol 2009;35:869–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miller DL, Dou C, Wiggins RC: Contrast-enhanced diagnostic ultrasound causes renal tissue damage in a porcine model. J Ultrasound Med 2010;29:1391–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miller DL, Averkiou MA, Brayman AA, Everbach EC, Holland CK, Wible JH Jr, Wu J: Bioeffects considerations for diagnostic ultrasound contrast agents. J Ultrasound Med 2008;27:611–632; quiz 633–616. [DOI] [PubMed] [Google Scholar]
- 31.Paefgen V, Doleschel D, Kiessling F: Evolution of contrast agents for ultrasound imaging and ultrasound-mediated drug delivery. Front Pharmacol 2015;6:197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Appis AW, Tracy MJ, Feinstein SB: Update on the safety and efficacy of commercial ultrasound contrast agents in cardiac applications. Echo Res Pract 2015;2:R55–R62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.D’Onofrio M, Crosara S, De Robertis R, Canestrini S, Mucelli RP: Contrast-enhanced ultrasound of focal liver lesions. AJR Am J Roentgenol 2015;205:W56–W66. [DOI] [PubMed] [Google Scholar]
- 34.Bhayana D, Kim TK, Jang HJ, Burns PN, Wilson SR: Hypervascular liver masses on contrast-enhanced ultrasound: the importance of washout. AJR Am J Roentgenol 2010;194: 977–983. [DOI] [PubMed] [Google Scholar]
- 35.Kono Y, Lyshchik A, Cosgrove D, Dietrich CF, Jang HJ, Kim TK, Piscaglia F, Willmann JK, Wilson SR, Santillan C, Kambadakone A, Mitchell D, Vezeridis A, Sirlin CB: Contrast enhanced ultrasound (CEUS) liver imaging reporting and data system (LI-RADS ®): the official version by the American College of radiology (ACR). Ultraschall Med 2017;38:85–86. [DOI] [PubMed] [Google Scholar]
- 36.Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsoe CP, Piscaglia F, Wilson SR, Barr RG, Chammas MC, Chaubal NG, Chen MH, Clevert DA, Correas JM, Ding H, Forsberg F, Fowlkes JB, Gibson RN, Goldberg BB, Lassau N, Leen EL, Mattrey RF, Moriyasu F, Solbiati L, Weskott HP, Xu HX: Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver – update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med 2013;34:11–29. [DOI] [PubMed] [Google Scholar]
- 37.Barr RG: How to develop a contrast-enhanced ultrasound program. J Ultrasound Med 2017; 36:1225–1240. [DOI] [PubMed] [Google Scholar]
- 38.Giordano M, Marzolla R, Puteo F, Scianaro L, Caringella DA, Depalo T: Voiding urosonography as first step in the diagnosis of vesicoureteral reflux in children: a clinical experience. Pediatr Radiol 2007;37:674–677. [DOI] [PubMed] [Google Scholar]
- 39.Chang EH, Chong WK, Kasoji S, Dayton PA, Rathmell WK: Management of indeterminate cystic kidney lesions: review of contrasteEnhanced ultrasound as a diagnostic tool. Urology 2015;87:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sawhney S, Wilson SR: Can ultrasound with contrast enhancement replace nonenhanced computed tomography scans in patients with contraindication to computed tomography contrast agents? Ultrasound Q 2017;33:125–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Girometti R, Stocca T, Serena E, Granata A, Bertolotto M: Impact of contrast-enhanced ultrasound in patients with renal function impairment. World J Radiol 2017;9:10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zarzour JG, Lockhart ME, West J, Turner E, Jackson BE, Thomas JV, Robbin ML: Contrast-enhanced ultrasound classification of previously indeterminate renal lesions. J Ultrasound Med 2017;36:1819–1827. [DOI] [PubMed] [Google Scholar]
- 43.Defortescu G, Cornu JN, Bejar S, Giwerc A, Gobet F, Werquin C, Pfister C, Nouhaud FX: Diagnostic performance of contrast-enhanced ultrasonography and magnetic resonance imaging for the assessment of complex renal cysts: a prospective study. Int J Urol 2017;24:184–189. [DOI] [PubMed] [Google Scholar]
- 44.Sanz E, Hevia V, Gomez V, Alvarez S, Fabuel JJ, Martinez L, Rodriguez-Patron R, Gonzalez-Gordaliza C, Burgos FJ: Renal complex cystic masses: usefulness of contrast-enhanced ultrasound (CEUS) in their assessment and Its agreement with computed tomography. Curr Urol Rep 2016;17:89. [DOI] [PubMed] [Google Scholar]
- 45.Chang EH, Chong WK, Kasoji SK, Fielding JR, Altun E, Mullin LB, Kim JI, Fine JP, Dayton PA, Rathmell WK: Diagnostic accuracy of contrast-enhanced ultrasound for characterization of kidney lesions in patients with and without chronic kidney disease. BMC Nephrol 2017;18:266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ascenti G, Mazziotti S, Zimbaro G, Settineri N, Magno C, Melloni D, Caruso R, Scribano E: Complex cystic renal masses: characterization with contrast-enhanced US. Radiology 2007;243:158–165. [DOI] [PubMed] [Google Scholar]
- 47.Clevert DA, Minaifar N, Weckbach S, Jung EM, Stock K, Reiser M, Staehler M: Multislice computed tomography versus contrast-enhanced ultrasound in evaluation of complex cystic renal masses using the Bosniak classification system. Clini Hemorheol Microcirc 2008;39:171–178. [PubMed] [Google Scholar]
- 48.Quaia E, Bertolotto M, Cioffi V, Rossi A, Baratella E, Pizzolato R, Cov MA: Comparison of contrast-enhanced sonography with unenhanced sonography and contrast-enhanced CT in the diagnosis of malignancy in complex cystic renal masses. AJR Am J Roentgenol 2008;191:1239–1249. [DOI] [PubMed] [Google Scholar]
- 49.Park BK, Kim B, Kim SH, Ko K, Lee HM, Choi HY: Assessment of cystic renal masses based on Bosniak classification: comparison of CT and contrast-enhanced US. Eur J Radiol 2007; 61:310–314. [DOI] [PubMed] [Google Scholar]
- 50.Barr RG, Peterson C, Hindi A: Evaluation of indeterminate renal masses with contrast-enhanced US: a diagnostic performance study. Radiology 2014;271:133–142. [DOI] [PubMed] [Google Scholar]
- 51.Alzaraa A, Gravante G, Chung WY, Al-Leswas D, Bruno M, Dennison AR, Lloyd DM: Targeted microbubbles in the experimental and clinical setting. Am J Surg 2012; 204:355–366. [DOI] [PubMed] [Google Scholar]
- 52.Baron Toaldo M, Salvatore V, Marinelli S, Palama C, Milazzo M, Croci L, Venerandi L, Cipone M, Bolondi L, Piscaglia F: Use of VEGFR-2 targeted ultrasound contrast agent for the early evaluation of response to sorafenib in a mouse model of hepatocellular carcinoma. Mol Imaging Biol 2015;17:29–37. [DOI] [PubMed] [Google Scholar]
- 53.Gao Y, Hernandez C, Yuan HX, Lilly J, Kota P, Zhou H, Wu H, Exner AA: Ultrasound molecular imaging of ovarian cancer with CA-125 targeted nanobubble contrast agents. Nanomedicine 2017;13:2159–2168. [DOI] [PubMed] [Google Scholar]
- 54.Eschbach RS, Clevert DA, Hirner-Eppeneder H, Ingrisch M, Moser M, Schuster J, Tadros D, Schneider M, Kazmierczak PM, Reiser M, Cyran CC: Contrast-enhanced ultrasound with VEGFR2-targeted microbubbles for monitoring regorafenib therapy effects in experimental colorectal adenocarcinomas in rats with DCE-MRI and immunohistochemical validation. PLoS One 2017;12:e0169323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lindner JR, Song J, Christiansen J, Klibanov AL, Xu F, Ley K: Ultrasound assessment of inflammation and renal tissue injury with microbubbles targeted to P-selectin. Circulation 2001;104:2107–2112. [DOI] [PubMed] [Google Scholar]
- 56.Deshpande N, Lutz AM, Ren Y, Foygel K, Tian L, Schneider M, Pai R, Pasricha PJ, Willmann JK: Quantification and monitoring of inflammation in murine inflammatory bowel disease with targeted contrast-enhanced US. Radiology 2012;262:172–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yang H, Xiong X, Zhang L, Wu C, Liu Y: Adhesion of bio-functionalized ultrasound microbubbles to endothelial cells by targeting to vascular cell adhesion molecule-1 under shear flow. Int J Nanomedicine 2011;6:2043–2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kaufmann BA, Sanders JM, Davis C, Xie A, Aldred P, Sarembock IJ, Lindner JR: Molecular imaging of inflammation in atherosclerosis with targeted ultrasound detection of vascular cell adhesion molecule-1. Circulation 2007;116:276–284. [DOI] [PubMed] [Google Scholar]