Abstract
Purpose
To assess radiation oncologists’ perceptions of training and research opportunities in the fields of genomics, bioinformatics, and immunology.
Materials and Methods
A 13-item electronic survey was sent to 101 radiation oncology department chairs and administrators. A separate 30-item electronic survey was sent to 132 members of the American Society for Radiation Oncology Science Council as well as to 565 members of the Association of Residents in Radiation Oncology. Survey responses were collected, and results were analyzed using descriptive statistics.
Results
Twenty-six department chairs and 91 general respondents submitted responses. Among general respondents, 69% were current trainees and 31% had completed training. The majority of respondents (92%) were affiliated with an academic/university main campus. Approximately half of respondents (43% to 53%) reported no prior formal training in bioinformatics, genomics, or immunology. More than half of department chairs (54% to 58%) and general respondents (57% to 63%) thought that current training opportunities in these areas were absolutely or moderately insufficient. A majority of respondents (53% to 65%) thought that additional training in these areas would provide opportunity for career advancement, and 80% could identify a current or future research project that additional training in these fields would allow them to pursue. More than half of respondents expressed interest in attending a formal training course, and the majority of department chairs (22 of 26 [85%]) reported that they would probably or definitely send trainees or faculty members to a formal training course.
Conclusion
Among radiation oncologists surveyed, there is a perceived lack of current training opportunities in bioinformatics, genomics, and immunology. A majority of respondents reported an interest in obtaining additional training in these areas and believed that training would provide opportunity for career advancement.
INTRODUCTION
The development and widespread application of novel genomic techniques and bioinformatics tools have resulted in an explosion of available tumor genomic information, transforming our understanding of tumor biology.1,2 The discovery and clinical implementation of therapies targeting the tumor immune response have reshaped the treatment landscape for several tumor types and have spurred additional basic and translational immunology research efforts.3,4
Radiation oncologists are poised to contribute to research efforts in genomics, bioinformatics, and immunology and to translate discoveries into clinical practice. However, given the pace at which these fields evolve, we hypothesize that there is an unmet need for formal training opportunities. Here, we report findings from a pair of surveys designed to elucidate academic radiation oncologist and trainee views of the training and research environment in the areas of cancer genomics, bioinformatics, and immunology.
MATERIALS AND METHODS
A 30-item electronic survey was sent to 132 members of the American Society for Radiation Oncology (ASTRO) Science Council on August 28, 2017, as well as to 565 members of the Association of Residents in Radiation Oncology on September 8, 2017. A single reminder e-mail was sent on October 30, 2017, and final results were collected on November 13, 2017.
A separate 13-item electronic survey was sent to 101 members of the Society of Chairs of Academic Radiation Oncology Programs on October 27, 2017. A link to the survey was subsequently included in the Association for Directors of Radiation Oncology Programs e-mail newsletter on November 3, 2017 (in lieu of a separate e-mail reminder). Results were collected on November 13, 2017.
One-sample t tests were used to compare the distribution of responses with a random distribution. All reported P values are two sided.
RESULTS
A total of 91 individuals submitted responses to the 30-item survey (91 of 697 individuals who were sent the survey [13% overall response rate]), and 26 department chairs submitted responses to the 13-item survey (26 of 101 individuals who were sent the survey [26% overall response rate]). Among the 91 general respondents to the 30-item survey, 63 (69%) were currently in residency or fellowship training, five (6%) had completed training within the past 7 years, and 23 (25%) were at least 8 years removed from training. Nearly all respondents to the 30-item survey (84 of 91 respondents [92%]) were affiliated with an academic/university center main campus, whereas the remaining respondents were affiliated with an academic/university satellite location, community practice, or private practice. Practice size varied among respondents, with 34 of 91 respondents (37%) reporting a practice size of four to 10 radiation oncologists, 34 (37%) reporting a practice size of 10 to 20 radiation oncologists, and 22 (24%) reporting a practice size of more than 20 radiation oncologists. Eighteen of the 91 respondents (20%) failed to complete the entire survey. There were no significant differences in training level, practice size/location, or previous training among respondents who completed the survey versus those who did not.
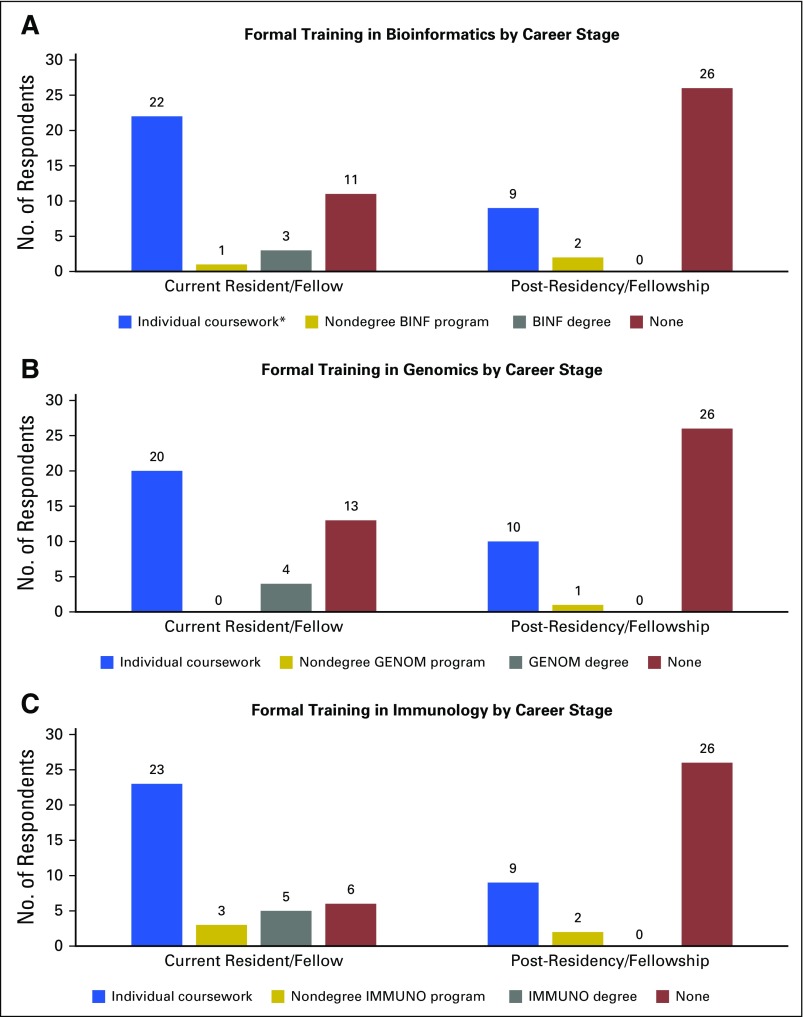
Previous training in bioinformatics, genomics, and immunology varied among respondents. A subset of respondents reported having completed individual courses in bioinformatics (31 of 74 respondents [42%]), genomics (30 of 74 [41%]), or immunology (32 of 74 [43%]). Approximately half of respondents (ranging from 32 of 74 respondents [43%] for immunology to 39 of 74 [53%] for genomics) reported no prior formal training in these disciplines (Appendix Fig A1). Completion of a formal degree in bioinformatics, genomics, or immunology was uncommon (ranging from three of 74 respondents [4%] for bioinformatics to five of 74 [7%] for immunology). Among respondents with prior training in these areas, undergraduate coursework was the most common mechanism, followed by institutional and departmental course offerings. Prior coursework was more common among current radiation oncology trainees (ranging from 20 of 37 respondents [54%] for genomics to 23 of 37 [62%] for immunology) than among respondents who had completed training (ranging from nine of 37 respondents [24%] for bioinformatics and immunology to 10 of 37 [27%] for genomics).
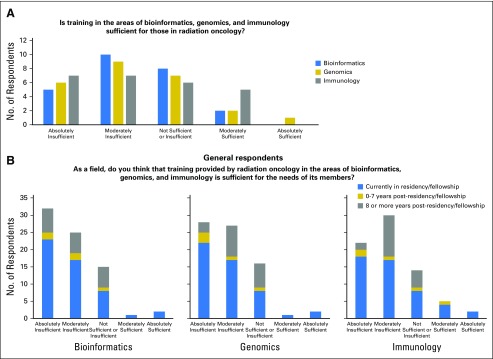
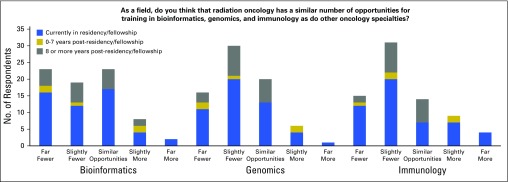
Overall, there was a perceived insufficiency in the current training opportunities in bioinformatics, genomics, and immunology. Among 26 department chairs, more than half (ranging from 14 of 26 department chairs [54%] for immunology to 15 of 26 [58%] for bioinformatics and genomics) believed that training in these three areas was either absolutely insufficient or moderately insufficient. A minority of respondents (ranging from two of 26 department chairs [8%] for bioinformatics and genomics to five of 26 [19%] for immunology) thought that training in any of these areas was moderately sufficient or absolutely sufficient (P < .001; Fig 1A). Similarly, among general respondents, a majority (ranging from 52 of 73 respondents [57%] for immunology to 57 of 75 [63%] for genomics) believed that training in these areas was either absolutely insufficient or moderately insufficient. On the other hand, few respondents (ranging from three of 75 respondents [4%] for bioinformatics and genomics to seven of 73 [10%] for immunology) reported that training in these areas was either moderately sufficient or absolutely sufficient (P < .001 for each discipline; Fig 1B). The percentage of respondents who believed that current training opportunities were insufficient did not vary significantly on the basis of extent of prior training (Appendix Fig A2). Approximately half of general respondents (ranging from 42 of 75 respondents [56%] for bioinformatics to 46 of 73 [63%] for genomics and immunology) thought that fewer training opportunities in these areas were available within radiation oncology than within other oncology specialties (Appendix Fig A3).
Fig 1.
Perceived sufficiency of current training environment for bioinformatics, genomics, and immunology. (A) Department chairs (n = 25 responses). (B) General respondents (n = 73 responses).
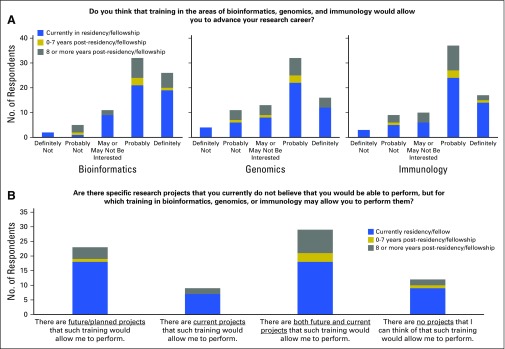
Despite a lack of perceived sufficiency of the current training environment, respondents thought that training in the areas of bioinformatics, genomics, and immunology could provide career advancement opportunities. A majority of respondents (ranging from 48 of 76 respondents [63%] for genomics to 58 of 76 [76%] for bioinformatics) reported that additional training would either definitely or probably allow advancement of their research career (P < .001 for each discipline; Fig 2A). These rates were similar among current trainees (ranging from 34 of 52 current trainees [65%] for genomics to 40 of 52 [77%] for bioinformatics) and those respondents who are 8 or more years removed from training (ranging from 11 of 18 [61%] for genomics to 14 of 19 [74%] for bioinformatics). Furthermore, a majority of respondents (61 of 73 respondents [84%]) could identify a research project relevant to their work that they could not currently perform, but for which training in bioinformatics, genomics, or immunology would allow them to perform it (Fig 2B).
Fig 2.
Perceived potential for career advancement and research opportunities with additional training. (A) Career advancement (n = 74 responses). (B) Specific research projects (n = 73 responses).
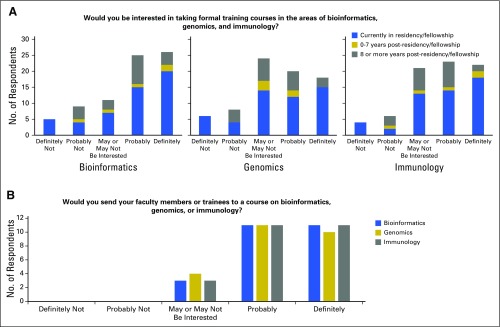
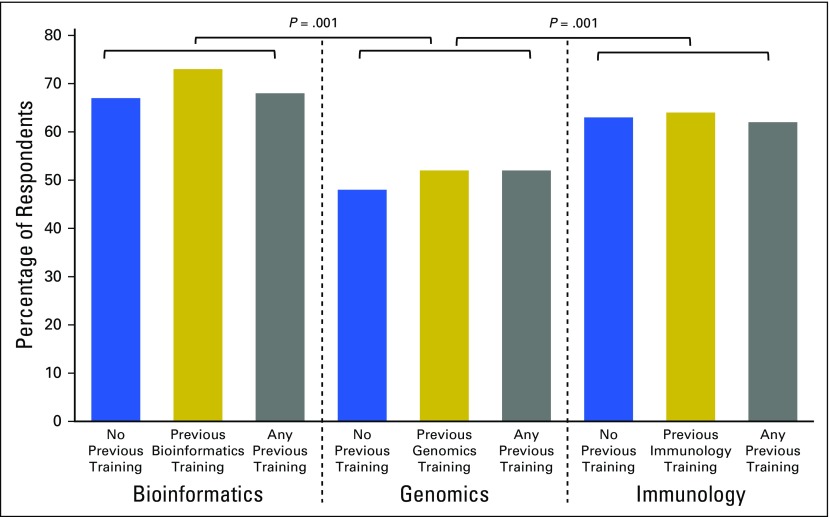
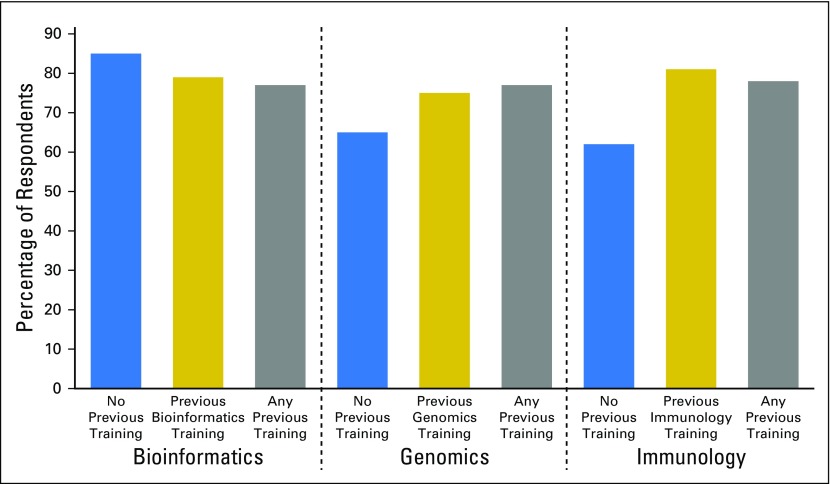
Respondents were asked to report their interest in attending a formal training course in bioinformatics, genomics, and immunology. At least half of respondents (ranging from 38 of 76 respondents [50%] for genomics to 51 of 76 [67%] for bioinformatics) reported being probably or definitely interested in participating in a formal training course (P < .009 for each discipline; Fig 3A). Interest in additional training was similar among respondents with versus without previous training in these areas and was significantly higher for bioinformatics and immunology than for genomics (P = .001; Fig 4). Among department chairs, a majority (ranging from 21 of 25 department chairs [84%] for genomics to 22 of 25 [88%] for bioinformatics and immunology) reported that they would probably or definitely send faculty members or trainees to attend a formal training course (P < .001; Fig 3B).
Fig 3.
Assessing interest in a formal training course in bioinformatics, genomics, and immunology. (A) General respondents (n = 76 responses). (B) Department chairs (n = 25 responses).
Fig 4.
Interest in additional training on the basis of extent of prior training. The percentage of respondents who were definitely or probably interested in taking formal training courses in bioinformatics, genomics, or immunology are shown. Responses are grouped by the type of previous training: no previous training, previous training in the specific area, or previous training in any of the areas (bioinformatics, genomics, or immunology).
DISCUSSION
Advances in genomics, bioinformatics, and immunology are transforming oncology practice. Access to evidence-based instruction for oncology trainees and practitioners in these rapidly evolving fields presents a significant challenge. Here, we report results from surveys conducted to understand radiation oncologists’ perceptions of training and research opportunities in these areas.
The nature and extent of previous training in bioinformatics, genomics, and immunology varied among respondents. However, most respondents reported either no formal training in these areas or completion of individual courses, which were often at the undergraduate level. This heterogeneity in experience may reflect a lack of established formal training opportunities in these dynamic scientific fields.
The majority of respondents believe that current training opportunities for radiation oncologists in these three areas are insufficient. This view is shared by department chairs, practicing radiation oncologists, and trainees. Interestingly, there was not a significant difference in this perception on the basis of extent of prior training. For example, although slightly more respondents with no previous bioinformatics training thought that the current bioinformatics training opportunities were insufficient, respondents with previous training in genomics or immunology were actually more likely to report that the current genomics and immunology training opportunities were insufficient.
Importantly, a majority of respondents believed that additional training in these areas would provide opportunity for career advancement. Most respondents could identify specific research projects that additional training would allow them to pursue. Together, these results suggest an unmet need in training opportunities for radiation oncologists in bioinformatics, genomics, and immunology, and that providing training opportunities in these areas could expand the radiation oncology research portfolio.
The results from these surveys have important limitations. The overall response rates were relatively low, and most respondents are affiliated with an academic/university main campus. Therefore, the results may not reflect the experiences or interests of all radiation oncologists, particularly those practicing outside of a university-based setting. In addition, the fields of bioinformatics, genomics, and immunology are immense, and the survey results do not provide detailed insights into respondents’ preferred educational content or medium.
The clinical application of novel bioinformatics tools and genomic assays is reshaping management of many common tumor types and is ushering in a new era of precision radiation oncology.5 In addition, immune-directed therapies are being investigated in combination with radiation in a variety of disease contexts and will probably become integrated into primary management. Therefore, basic fluency in the disciplines of bioinformatics, genomics, and immunology will be required for radiation oncologists to efficiently integrate new treatment paradigms into clinical practice. Formal instruction in these areas could be integrated into residency program didactic curriculums and outlined in the ASTRO Radiobiology and Radiation Physics Curriculum. Beyond the integration of formal instruction into the clinical training curriculum, access to advanced training and research opportunities in these fields will be required to attract talented physician-scientists into the field and to expand representation of radiation oncologists in leadership roles at the national and international levels. These initiatives will require collaboration with experts across scientific and medical disciplines to create cutting-edge training opportunities in more established fields such as bioinformatics and immunology, as well as in newer fields such as machine learning and artificial intelligence.
ASTRO is working to enhance educational opportunities for radiation oncology professionals in the areas of bioinformatics, genomics, and immunology. Recent ASTRO Research Workshops have included topics such as Big Data (2015), Precision Medicine (2016), and Immunotherapy (2017).5-7 In addition, ASTRO has established an Informatics track at the Annual Meeting that includes several scientific panel and education sessions each year, and immunotherapy has been a prominent topic at several recent Annual Meetings as well as at specialty meetings. Finally, ASTRO is planning two relevant Think Tank meetings in 2018, one focused on Nanotechnology and Biomarkers in Radiation Oncology and a second on Genomic Profiling in Radiation Oncology. More broadly, initiatives by the National Science Foundation and the National Institutes of Health (NIH) have been designed to fund data science and informatics training curriculums (NIH R25 RFA-HG-16-016) and scientific meetings (NIH U13 RFA-CA-16-020), which may provide additional opportunities for instruction and career advancement for radiation oncologists.
The results of this large national survey of radiation oncology physicians and trainees indicate a lack of perceived training opportunities in bioinformatics, genomics, and immunology. However, despite this perceived lack of current opportunities, a majority of respondents report interest in obtaining additional training in these areas and believe that such training could lead to career advancement. These findings represent both a challenge and an opportunity in the field of radiation oncology. Efforts are ongoing to develop and tailor training opportunities to keep pace with the rapidly evolving role of bioinformatics, genomics, and immunology in oncology research and practice.
Appendix
Fig A1.
Previous training in bioinformatics, genomics, and immunology (n = 74 responses). (A) Formal training in bioinformatics (BINF) by career stage. (B) Formal training in genomics (GENOM) by career stage. (C) Formal training in immunology (IMMUNO) by career stage.
Fig A2.
Percentage of respondents who believe that current training opportunities in bioinformatics, genomics, and immunology are absolutely or moderately insufficient.
Fig A3.
Respondents’ views on whether there are fewer training opportunities in bioinformatics, genomics, and immunology within radiation oncology than within other oncology specialties.
Footnotes
Supported by the National Cancer Institute (5K08CA219504), the Burroughs-Wellcome Fund, and the Bladder Cancer Advocacy Network (K.W.M.); and the National Cancer Institute-Sidney Kimmel Cancer Center (Support Grant 5P30CA056036-17) and the Prostate Cancer Foundation (Challenge Award) (A.P.D.).
AUTHOR CONTRIBUTIONS
Conception and design: Kent W. Mouw, Adam P. Dicker
Collection and assembly of data: All authors
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO’s conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/site/ifc.
Kent W. Mouw
Consulting or Advisory Role: Pfizer, EMD Serono
Tyler F. Beck
Other Relationship: National Cancer Institute (I)
Judith C. Keen
Stock and Other Ownership Interests: Johnson & Johnson
Adam P. Dicker
Leadership: Department of Defense-Prostate Cancer Research Program, NRG Oncology, American Society for Radiation Oncology
Consulting or Advisory Role: EMD Serono, Ferring, Janssen, RedHill Biopharma, Self Care Catalyst, Celldex, Johnson & Johnson
Research Funding: Prostate Cancer Foundation
Travel, Accommodations, Expenses: Merck KGaA, Ferring, Self Care Catalyst
REFERENCES
- 1.Garraway LA, Lander ES. Lessons from the cancer genome. Cell. 2013;153:17–37. doi: 10.1016/j.cell.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Berger MF, Van Allen EM. Delivering on the promise of precision cancer medicine. Genome Med. 2016;8:110. doi: 10.1186/s13073-016-0373-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.LaFleur MW, Muroyama Y, Drake CG, et al. Inhibitors of the PD-1 pathway in tumor therapy. J Immunol. 2018;200:375–383. doi: 10.4049/jimmunol.1701044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Antonia SJ, Villegas A, Daniel D, et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N Engl J Med. 2017;377:1919–1929. doi: 10.1056/NEJMoa1709937. [DOI] [PubMed] [Google Scholar]
- 5. Hall WA, Bergom C, Thompson RF, et al: Precision oncology and genomically guided radiation therapy: A report from the American Society for Radiation Oncology/American Association of Physicists in Medicine/National Cancer Institute Precision Medicine Conference. Int J Radiat Oncol Biol Phys 101:274-284, 2018. [DOI] [PubMed] [Google Scholar]
- 6.Benedict SH, El Naqa I, Klein EE. Introduction to big data in radiation oncology: Exploring opportunities for research, quality assessment, and clinical care. Int J Radiat Oncol Biol Phys. 2016;95:871–872. doi: 10.1016/j.ijrobp.2015.12.358. [DOI] [PubMed] [Google Scholar]
- 7.Marciscano AE, Walker JM, McGee HM, et al. Incorporating radiation oncology into immunotherapy: Proceedings from the ASTRO-SITC-NCI immunotherapy workshop. J Immunother Cancer. 2018;6:6. doi: 10.1186/s40425-018-0317-y. [DOI] [PMC free article] [PubMed] [Google Scholar]