Abstract
Wearable accelerometers provide detailed, objective, and continuous measurements of physical activity (PA). Recent advances in technology and the decreasing cost of wearable devices led to an explosion in the popularity of wearable technology in health research. An ever-increasing number of studies collect high-throughput, sub-second level raw acceleration data. In this paper, we discuss problems related to the collection and analysis of raw accelerometry data and refer to published solutions. In particular, we describe the size and complexity of the data, the within- and between-subject variability, and the effects of sensor location on the body. We also discuss challenges related to sampling frequency, device calibration, data labeling and multiple PA monitors synchronization. We illustrate these points using the Developmental Epidemiological Cohort Study (DECOS), which collected raw accelerometry data on individuals both in a controlled and the free-living environment.
Keywords: Wearable computing, Accelerometry, Wearable accelerometers, Physical activity, Accelerometers
1. Introduction
Wearable physical activity (PA) monitors provide detailed, continuous, and objective measurements of individual PA in the free-living environment. They can complement or completely replace current subjective measurements collected via questionnaires. Recent advances in technology and the decreasing cost of wearable devices led to an explosion in the popularity of wearable technology in health research. Here we argue that, just like any new measurement used in health science, there is a need to understand, reproduce, and communicate the measurements produced by these new devices. This can lead to improved design of experiments, a higher quality of the acquired data, and more generalizable results.
Wearable PA monitors have a vast potential for health studies including an estimation of PA fragmentation into active and sedentary states, quantification of time spent at different PA intensity levels, and precise identification of activity types at the subsecond level. Data collected by PA devices provides information about the ability and will to initiate activity as well as quantify the activity choices (both in terms of intensity and type) for individuals in a wide range of health studies. Wearable PA monitors have already been successfully employed in a number of epidemiological studies. For example, accelerometry data collected in National Health and Nutrition Examination Survey (NHANES) 2003–2006 was used to describe the effects of age on PA (Varma et al, 2017) and estimated sleep characteristics (Urbanek et al, 2018a) over the whole lifespan of the US population. The accelerometry data in the Baltimore Longitudinal Study of Aging (BLSA) were used to describe the distribution of PA as a function of age. BMI and time of day Schrack et al (2014). Other applications include modeling of circadian rhythms of PA (Xiao et al, 2015), monitoring recovery after a major surgery (Cook et al, 2013), assessment of compliance in PA-interventions (Fitzsimons et al, 2013), comparing PA of different groups in clinical trials (Gresham et al, 2018), prediction of walking (Urbanek et al, 2018c) and estimation of gait parameters (Urbanek et al, 2018b).
At the core of all modern PA monitors there is a small accelerometer, a microelectromechanical system (MEMS) that measures accelerations relative to the Earth’s gravitational field. Hence, PA monitors are often referred to as wearable accelerometers. The output of these devices is a three-dimensional time series of accelerations expressed in gravitational units in the frame of reference of the device. More clearly, the device has its own frame of reference up-down, left-right, backward-forward. This frame is typically different from and can change with the frame of reference of the person who wears the device or who observes the experiment. These raw data produced by accelerometers are transformed using various algorithms into PA summaries, which have different labels (e.g. steps, calories, activity counts) and can be aggregated at different temporal resolutions (e.g. minutes, hours, or days).
Due to battery and memory limitations, PA monitors used to return only-aggregated minute-level data in the form of proprietary activity counts (AC) (Chen et al, 2012). The definition of AC varies between- and within-device manufacturers, across time, body location and between studies. Despite this issue, AC have been used effectively as a relative measure of PA within the same study, especially when the same devices and software were used and devices were calibrated (Matthews et al, 2008; Hcaly et al, 2011; Schrack et al, 2014; Xiao et al, 2015).
There are multiple ways to use minute-level PA data collected by wearable devices. A common approach is to determine the total PA performed during a 24-hour day in the form of a proxy measure of total activity counts (TAC) or total log-transformed activity counts (TLAC) (Varma et al, 2018). Another popular approach is to use summaries of the amount of time spent at different activity intensity levels (e.g. sedentary, light, moderate and vigorous). These levels are obtained by using published population level thresholds of activity intensity (Troiano et al, 2008). The daily summaries can be further refined by calculating them within pre-specified intervals during the day; for example, the TAC observed between 6 a.m. and 10 a.m. can be used to define morning activity whereas TAC observed between 10 p.m. and 6 a.m. can be used to define nighttime activity (Copeland and Esliger, 2009). Yet another way of summarizing PA activity data uses PA fragmentation measures, which quantify the switching patterns between activity intensity levels (e.g., sedentary and active bouts) (Di et al, 2017). A more recent line of research has focused on using activity counts data at the minute level collected over multiple days to model ultradian and circadian rhythms of PA. Multiple analytical approaches have been proposed to address this problem, including functional registration (Wrobel et al, 2018), principal component analysis (Shou et al, 2015), bivariate smoothing (Xiao et al, 2013), and the general linear mixed model (Trost et al, 2008). Although minute-level accelerometry data has a great potential in health research applications, there is always the question of what additional information can be extracted from the sub-second level data. Here we argue that having the sub-second level data allows for data harmonization across and within studies, detailed quantification of walking characteristics in the lab and free-living environment, and potential tracking of pathologies associated with movement alteration or impairment. As an example of the latter, one may consider quantifying gait changes in recovery after orthopedic surgery, quantifying tremors in Parkinson diseases (PD), and measuring lack of balance in elderly at risk of falls.
As battery and memory limitations have been mitigated, it has become possible to collect and store high-throughput, three-axial, sub-second level acceleration data, ranging between 10 and 200 observations per second. PA monitors have also become increasingly sophisticated and are now routinely equipped with a selection of supplementary sensors including gyroscopes, thermometers, inclinometers, pulsometers, light intensity and skin conductance sensors. Data collected by these supplementary sensors are beyond the scope of this paper.
The collection of raw accelerometry data opens a spectrum of new scientific and analytic problems. For example, researchers do not need to rely on proprietary aggregated measures and can use well-defined, open-source, reproducible summaries of the data. This allows to compare and combine studies that collect raw accelerometry data at the same location on the body and provides explicit measures of activity on a recognized measurement scale. For example, UKBiobank (Doherty et al, 2017) uses the magnitude of the 3-dimensional vector of acceleration summarized in 5-second intervals, whereas the Women’s Health Initiative (WHI) study has explored 1-second summaries based on standard deviations of accelerometry along each axis (Bai et al, 2016). Raw and summarized data have also been used for recognition of activity types. A common approach is to derive accelerometry data features in a particular time-window and use supervised classification algorithms to predict activity type (Pobor et al, 2006; Staudenmayer et al, 2009; Attal et al, 2015). Extensive reviews of classification techniques for activity recognition from accelerometry data are provided by Bao and Intille (2004) and Preece et al (2009). Dictionary learning based on raw accelerometry Bai et al (2012); He et al (2014); Xiao et al (2016) has also been proposed in the context of fine-resolution movement prediction.
The increased granularity of the sub-second level data may contain important additional information, but it also creates new challenges. Indeed, the volume and structure of the data are much more complex for the raw data, especially when it is recorded for weeks at a time in free-living settings. In this paper, we discuss problems related to the collection and analysis of sub-second level accelerometry data.
Some of existing challenges have been well documented in the literature. For example, Trost et al (2005) highlighted problems associated with device selection, placement of accelerometers, epoch length, and compliance enhancing strategies. Schrack et al (2016) discussed the limitations of using uncalibrated, population-level thresholds for aggregated accelerometry measures in older adults. Song et al (2018) commented that variability in device wear time between study participants may be associated with the underlying behavior of interest, and proposed a modeling approach to deal with bias induced by informative observation times. Staudenmayer et al (2012) and Troiano et al (2014) noted that the diversity of measurements and analytic methods for accelerometry data makes it difficult to compare results across different studies, and advocate for standardization of measurement and pre-processing pipelines across studies.
Currently, there is no universally accepted and standardized approach for measuring PA using wearable accelerometers in health research. However, some excellent guidelines and standardized protocols have been published. For example, Matthews et al (2012) compiled a list of best practices for making decisions about important choices, such as the number of monitors needed, device placement, device initialization, device tracking, and data collection. They also provide guidance on how to report the use of PA monitors in population-based studies. Freedson et al (2012) provided recommendations for the use of wearable monitors for assessing PA for researchers, end users, as well as developers of activity monitors. The authors also provide guidelines for sensor output calibration and validation and discuss necessary steps for maximizing the generalizability of the data analysis. Troiano et al (2008) describes the design of the NHANES accelerometry study, where participants were instructed to take off the hip-worn device during sleep. Most subjects complied, some did not, and the timing when the device was taken off varied substantially both within- and between-subjects. When the device was not worn it was simply recording a zero acceleration, exactly the same as during the non-movement periods. For this reason, it was very important to estimate periods of non-wear and distinguish them from periods of wear and non-movement. The most popular approach for dealing with missing data was proposed by Troiano (2007), modified by Choi et al (2012), and implemented by Van Domelen (2018). This approach is now commonly used in large observational studies. In addition, Catellier et al (2005) evaluated and discussed approaches to deal with missing measurements in accelerometry count data collected over multiple days, including discarding the days with insufficient accelerometer data and employing imputation techniques to predict counts on those days.
The another open question in objective measurements of PA is harmonization of data from different monitors. Unfortunately, harmonization of PA data between existing studies is often impossible due to the different formulation and interpretation of activity counts, body placement, and lack of universally accepted measurement. For example, step counts produced by Fitbit cannot be compared to activity counts produced by ActiGraph, as they are not on the same scale. In fact, is has been shown that step counts might differ substantially when measured by different devices (Storti et al, 2008; Fortune et al, 2014). Activity counts measured by the same device may also be different depending on the sensor location (Fairclough et al, 2016). For example, a device located on the hip or ankle is sensitive to ambulation, whereas a device located on the wrist will detect both ambulation and hand movements. Moreover, some activity counts may change substantially with the sampling frequency (Brønd and Arvidsson, 2016) even for the same device placed at a particular body location. These problems are not likely to be resolved as long as summary data obtained via proprietary manufacturer algorithms continue to be used. The best strategy is to go back to the raw data and construct open-source data pre-processing approaches that become increasingly accepted by the community. This, unfortunately, is not a panacea, as pre-processing pipelines need to take into account problems associated with device calibration, missing data, data size and complexity, and measurement translation and communication.
To provide a concrete illustration of these problems and some potential solutions, we use the Developmental Epidemiological Cohort Study (DECOS) data, which is described in Sections 2.1–2.2. Next, we introduce the notation and statistical methods used to pre-process and summarize the data in Section 2.3. In Section 3 we illustrate issues related to the analysis and interpretation of raw accelerometry data and review some published approaches designed to handle their complexity and heterogeneity. In Section 4 we summarize the ideas and discuss their implication for health studies using raw accelerometry data.
2. Methods
2.1. Study participants
Forty-nine community-dwelling older adults were recruited from the Pittsburgh, Pennsylvania area for the Developmental Epidemiologic Cohort Study (DECOS), part of the National Institute on Aging (NIA) Aging Research Evaluating Accelerometry (AREA) project (Lange-Maia et al, 2015). DECOS is a cross-sectional study designed to examine the impact of accelerometry wear location on PA and sedentary behavior assessment among healthy older adults. Individuals were excluded from DECOS if they suffered from any of the following conditions: hip fracture, stroke in the past 12 months, cerebral hemorrhage in the past 6 months, heart attack, angioplasty, heart surgery in the past 3 months, chest pain during walking in the past 30 days, current treatment for shortness of breath or a lung condition, usual aching, stiffness, or pain in their lower limbs and joints and bilateral difficulty bending or straightening the knees fully.
2.2. Data collection
Participants were equipped with three tri-axial wearable PA monitors (Acti-Graph GT3x+) that collected raw accelerometry data at a sampling frequency of 80Hz (80 observations per second for each axis). Monitors were located on the hip using an elastic belt and on both wrists using watch straps. During the “in-the-lab” phase of the experiment all participants were asked to perform a series of physical tasks including: lying still, standing still, washing dishes, sitting still, dough kneading, dressing, folding towels, vacuuming, shopping, writing, dealing cards, standing up from a chair, walking for 20 m, walking for 20 m with arms crossed on the chest, fast walking for 20 m, fast walking for 20 m with arms crossed on the chest, treadmill walking at 1.5 mph for 5 min, walking for 40 m and fast walking for 400 m. Before each task participants were given verbal instructions by a supervising trained professional recording the times of the beginning and end of each task with a stopwatch. During the free-living portion of the experiment, participants were equipped with accelerometers for seven consecutive days and were told to maintain their normal, unsupervised, free-living activities. They were instructed to take off the activity monitors only during sleep.
2.3. Open-source summaries of accelerometry data
The raw accelerometry data are collected along three orthogonal axes in the device-specific frame of reference. We denote the vector of raw acceleration data by x(t) = {x1(t), x2(t),x3(t)}, where xm(t) is the acceleration measurement along the m (= 1, 2, 3) axis at time t (for notational simplicity we drop the participant index). The acceleration time series, x(t), are sampled at a fixed frequency f. For example, in our application, the sampling frequency is 80 Hz, which means that for each second along each axis there are 80 acceleration recordings.
Here we describe four open-source methods that have been used in the literature to provide summaries of accelerometry data. All methods consider non-overlapping time windows of a given duration H and reduce the 3H measurements in the window to a single number.
Euclidean Norm Minus One (ENMO) was first introduced as a summary metric for accelerometry data in van Hees et al (2013). It is directly based on the Euclidean norm of x(t), defined as
| (1) |
The ENMO at time t is defined as r(t) – 1 when r(t) – 1 ≥ 0 and 0 otherwise, or notationally, max [r(t) – 1, 0]. Further, the ENMO in a window of size H is defined as the average ENMO across the time points in that window. Formally,
| (2) |
ENMO can be sensitive to calibration errors when the device-specific ENMO at rest is not close to zero. An additional calibration procedure was introduced to mitigate the effects of calibration (van Hees et al, 2014).
The Vector Magnitude Count (VMC) is an aggregation statistic that is also known as the Mean Amplitude Deviation (MAD) Vähä-Ypyä et al (2015). We use the notation VMC to avoid the confusion between the two MAD acronyms used in accelerometry literature, one for mean amplitude deviation (Vähä-Ypyä et al, 2015) and one for median amplitude deviation (Mariani et al, 2013). VMC computes the norm in each time window H. Denote the average Euclidean norm in the time window of length H starting at t as . Then VMC is defined as
| (3) |
The unnormalized Activity Index (AI0) (Bai et al (2014) is a measure based on the combination of the three within-axis standard deviations of the raw accelerometry signal. Because AI0 subtracts the local mean of the accelerometry signal, calibration is intrinsic and local, which allows it to adapt to cases when the device is not calibrated, when it gets decalibrated during studies, or when the device exhibits time-dependent decalibration. Let σm (t;H) be the standard deviation of the acceleration along axis m = 1, 2, 3 in the window of length H starting at t. The exact formula is
where . Then formally,
| (4) |
where is the systematic noise standard deviation calculated using the data collected during some non-moving period. The unnormalized Activity Index (AI0) is expressed in Earth gravitational units.
The normalized Activity Index (AI, Bai et al (2016)) is strongly related to the unnormalized Activity Index (AI0). The only difference is that the axis-specific variances are divided by the device-specific systematic noise. More specifically, AI is defined as follows
| (5) |
The downside of using AI versus AI0 is that its scale is no longer in Earth gravitational units. Instead, it is expressed in multiples of noise standard deviation. The advantage of AI could be when the devices are not calibrated in terms of their noise level at rest, which may induce batch effects. This, however, seems to be a smaller problem than the internal calibration obtained by subtracting the local mean in AI and AI0.
In the remainder of this paper, we use ENMO, VMC and AI0. We do not use normalized Activity Index (AI) so as to keep presentations of the statistics measurements on the same scale.
3. Statistical challenges and examples
3.1. Data volume and complexity
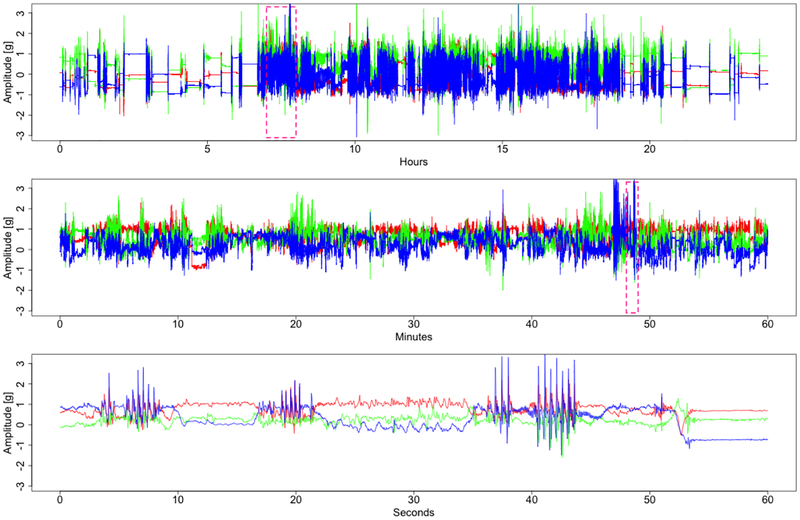
Figure 1 displays three-dimensional time series that represent the acceleration along each of the three orthogonal axes of an accelerometer located at the wrist. The top panel of Figure 1 presents 24 h of data, with each axis data shown in a different color. In this example, the first observation was taken at 12 a.m., while the last was taken 24 h later, also at 12 a.m. The middle panel in Figure 1 displays a particular 1 h interval from 8:40 a.m. to 9:40 a.m. (indicated in the top panel as a dashed-line rectangle). The bottom panel displays the one-minute interval marked as a dashed-line rectangle in the middle panel (from 8:51 a.m. to 8:52 a.m.). The signal was acquired at a sampling frequency of fs = 80Hz. Therefore, the number of observations per subject quickly explodes. For example, a week of accelerometry data collected at 80Hz results in 80 ∗ 60 ∗ 60 ∗ 24 ∗ 7 = 48,384,000 observations for each of the three axes. Thus, even for a small multi-subject observational study, researchers are faced with datasets consisting of billions of observations. This enormous volume of data creates challenges at every level of the scientific investigation. Storage and operational memory of modern computers are not unlimited and well-optimized solutions are needed for data management. Conducting exploratory data analysis, visualization, and modeling requires additional computational and methodological resources. Therefore, it is essential to implement carefully planned protocols for collection, management and analysis of the data. In recent years several protocols and experimental design guidelines have been proposed (Esliger et al, 2005; Cain, 2014; NHANES, 2011), though a universally accepted approach is still elusive. This could be due to the constant change of the technological and methodological landscape. For example, the US NHANES survey protocols have changed between survey cycles 2003–2004 (NHANES, 2006), 2005–2006 (NHANES, 2008), 2011–2012 and 2013–2014 (NHANES, 2011) both in terms of device type and body location. In the 2003–2004 and 2005–2006 cycles, participants wore an ActiGraph 7164 on a waist belt for 7 days during the non-sleeping time. In later cycles, the GT3X+ ActiGraph waterproof model was used on the non-dominant wrist for 7 days without taking it off. The protocol change was reported (Troiano et al, 2014) and was designed to improve participant compliance.
Figure 1.
Accelerometry data from three orthogonal axes of an accelerometer located on the left wrist. Each axis data is shown in a different color. The top panel displays 24 h of data collected between 12 a.m. and 12 a.m. The middle panel displays a 1-h interval from 8:40 a.m. to 9:40 a.m. (indicated in the top panel as a dashed-line rectangle). The bottom panel displays a 1-min interval from 8:51 a.m. to 8:52 a.m. marked as a dashed-line rectangle in the middle panel. The signal was acquired at a sampling frequency of fs = 80Hz.
The current approach to reduce the size and complexity of the raw accelerometer data is to create aggregated summaries in fixed time intervals, as described in Section 2.3. While these summaries reduce the volume of data, the potential loss of information can be substantial. To recover some of the information. a few methods have been proposed for recognition of activities using raw accelerometry data. Some approaches focus on the prediction of a group of movement types (Lyden et al, 2014). whereas others focus on the prediction of a specific movement type (e.g. walking) (Urbanek et al, 2015). Characterizing the kinematics of human walking both in the lab and in the free-living environments using accelerometry data could provide previously unavailable information on the physical condition of individuals (Studenski et al, 2011).
3.2. Data heterogeneity
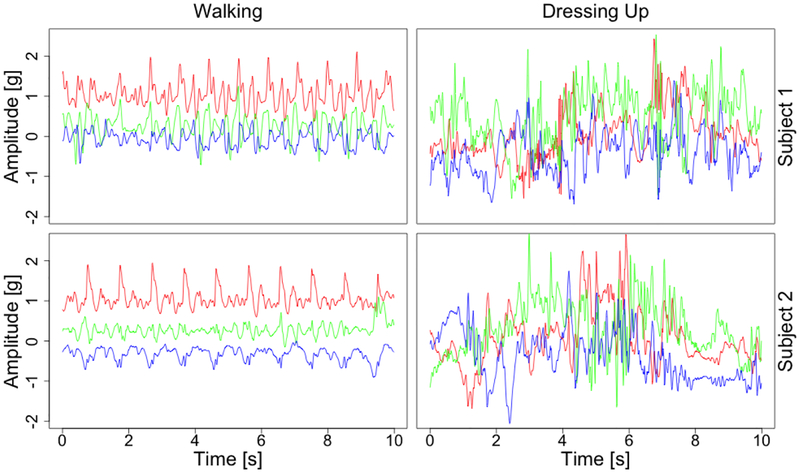
Interpretation of raw accelerometry data is an open and challenging problem due to the high heterogeneity of data, both within- and between-subjects. Within-subject variability is observed when one person performs the activity, but the characteristics of that activity change. For example, when walking, consecutive strides differ slightly in duration and shape due to natural stride-to-stride variability (IJmker and Lamoth, 2012; Urbanek et al, 2017). They can also differ substantially during the day, depending on the level fatigue of the individual, context of walking (e.g. hiking versus shopping), and local constraints (e.g. running to a meeting when late versus slow walking to the kitchen in the morning). Between-subject variability contains additional factors due to differences in body size, musculature, will, and ability to perform certain tasks. To further illustrate these points, the left column of Figure 2 displays acceleration data collected on the left wrist during walking for two individuals. The periodic character of time series is striking. However, both the duration and amplitude of accelerometry data can vary from cycle to cycle. A more extreme example is displayed in the right column of Figure 2, where the same two individuals perform the getting dressed activity. Indeed, the more random character of the observations and lack of synchronization between- and within individuals is remarkable.
Figure 2.
Data recorded by an accelerometer located on the left wrist while walking (left column) and getting dressed (right column), for two individuals (top and bottom row). Each axis is shown in a different color.
These data indicate that it is important to better define the types of physical activity. Indeed, the bottom panels of Figure 2 show that data can be very different even for what is defined as the same type of activity (e.g. getting dressed). In retrospect, this should not be surprising as “getting dressed” is a complex task that is only vaguely defined, may involve different types of clothes, body sizes and shapes, movements that individuals use to getting dressed, and order of various tasks. It should be apparent that if we want to make any progress in this area, we need to identify well-defined sub-movements that then translate them into research language. Clearly, in this case, the activity “getting dressed” does not have a sharp definition, especially from the point of view of an accelerometer. Things may be different if we had a video camera instead of an accelerometer, but this raises other problems that exceed the scope of the current paper.
Classifying activity types while accounting for between- and within-subject variability is under intense methodological development. The approach discussed in Bai et al (2012) and He et al (2014) uses short segments of training accelerometry data, called “movelets”, to construct dictionaries used as a reference to predict activity types on new data. Dictionaries are activity- and subject-specific to account for the individual variations in movement patterns across subjects. Xiao et al (2016) proposed a related movelet-based method to use labeled activity data from some subjects to predict the activity labels of other subjects.
3.3. Sensor location
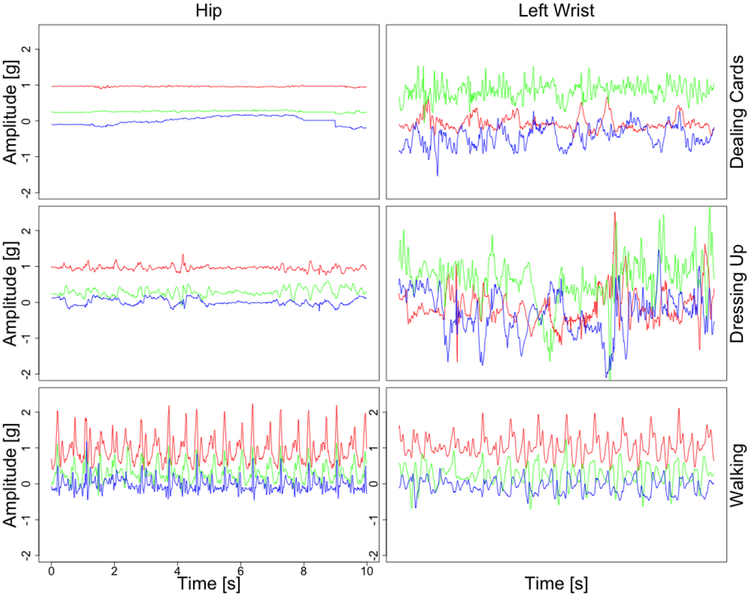
The location of the accelerometer sensor on the body can also have substantial effects on predicting activity types, PA volume, and PA distribution as a function of time of the day. Indeed, the sensor collects only its own acceleration, which is a proxy of the acceleration of the particular body location where the sensor is attached. Therefore, a wrist sensor will produce different signals from a hip or thigh sensor. To illustrate this point, Figure 3 displays the raw accelerometry data collected simultaneously by sensors located on the hip (left column) and left wrist (right column) while dealing cards (top panel), getting dressed (middle panel) and walking (bottom panel). For dealing cards, an activity that requires mostly hand-movements, the signal amplitude for the wrist sensor is much higher than for the hip sensor. For more complex, whole-body activities, such as getting dressed, the signals corresponding to both locations have higher amplitudes than for dealing cards. However, the amplitude of the signal at the wrist is higher and there are no clear correlations between the hip and wrist signals. In the case of walking, the amplitudes of the data collected on the wrist and the hip look periodic and highly correlated. This is likely due to the fact that both hands and legs are involved in walking, with roughly the same frequency of movement. The slightly lower amplitudes observed at the wrist are probably due to the more intense PA in the lower body during walking. In our experience, an accelerometer placed at the ankle would display even higher amplitudes of the acceleration signal.
Figure 3.
Accelerometry data from three orthogonal axes of an accelerometer located on the hip (left column) and left wrist (right column), while dealing cards (top row), getting dressed (middle row) and walking (bottom row). Each axis data are shown in a different color.
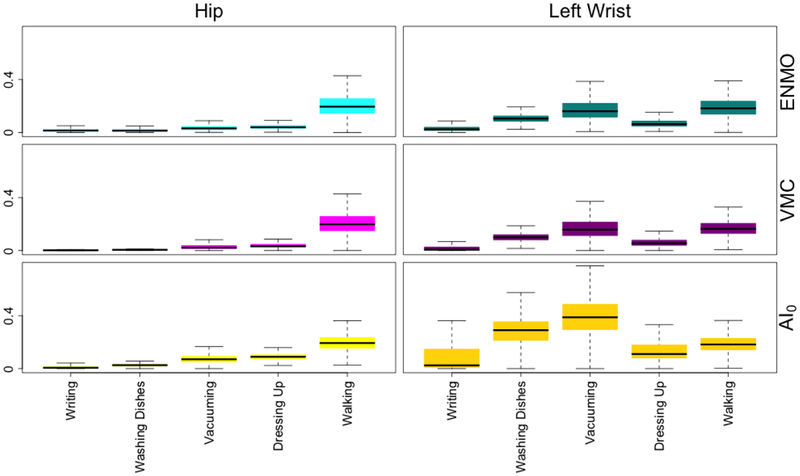
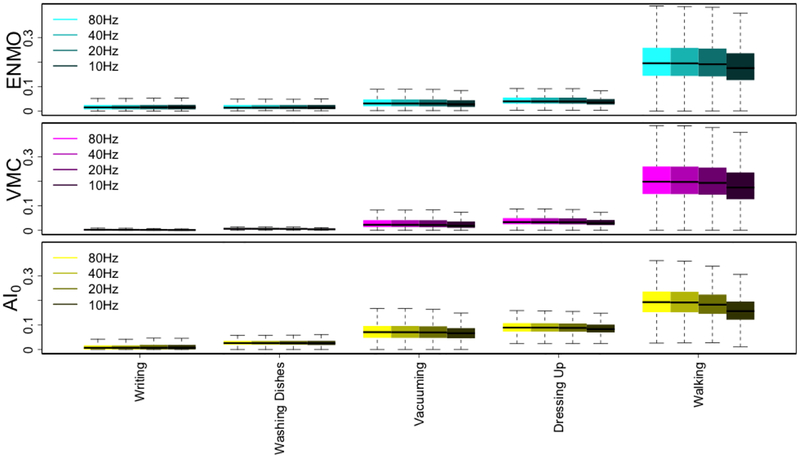
Figure 4 provides the summary-metrics introduced in Section 2.3 using data collected during various activities performed in the controlled lab environment. The boxplots for ENMO, VMC and AI0 are displayed in the top, middle and bottom panels, respectively, while the data for the hip and left wrist are displayed in the left and right columns, respectively. All summary statistics are calculated for a window size of 5 s during writing, washing dishes, vacuuming, getting dressed and walking for each of 5-s intervals and all 49 individuals. The difference between the wrist and hip data can be observed for all summaries and activities requiring dynamic upper body movements (washing dishes, vacuuming). These differences are much lower for low-intensity hand movements (writing), though AI0 seems to better capture these differences. Also, substantial differences can be observed for moderate-intensity whole-body activities (getting dressed), where, again, AI0 seems to be more sensitive. For walking, the difference in the distribution of all summaries between the wrist and the hip is relatively small. When comparing AI0 versus ENMO versus VMC at the wrist there is a more clear differentiation between activities. This is likely due to the fact that AI0 automatically corrects for possible device miss-calibration, whereas the other methods do not. It is an open problem whether the methods perform more similarly after the device and/or signal calibration.
Figure 4.
Boxplots of ENMO, (top panels) VMC (middle panels) and AI0 (bottom panels) statistics derived for τ = 5-s length intervals of data collected from the hip (left column) and left wrist (right column) during writing, washing dishes, vacuuming, getting dressed and walking (x-axis), for all 49 individuals.
Summaries have been used extensively in the literature. For example. Koster et al (2016) showed that different cut-points of the vector magnitude can be used for the classification of sedentary time in older adults using both hip-worn and wrist-worn ActiGraph accelerometers. It has also been shown that activity recognition algorithms perform differently across body locations. For example, Rosenberger et al (2013) reported greater sensitivity and specificity of both sedentary and moderate- to vigorous-intensity PA when using accelerometry data collected at the hip compared to the wrist. Trost et al (2014) reported higher accuracy for hip-derived than for wrist-derived data in the classification of specific, whole-body engaging activities. Higher accuracy of classifying sitting was obtained with data collected from the wrist compared to data collected from the hip. Del Din et al (2016) showed that estimated gait characteristics, such as step time and length, can depend on body location and suggested that the chest location is more appropriate than the wrist. We conclude that the body location may lead to different results, that body location will favor movements that directly engage that particular location, and that translating various summaries into well-defined activity categories (e.g. walking, sedentary) requires location-specific calibration of the accelerometry summaries.
3.4. Device rotation
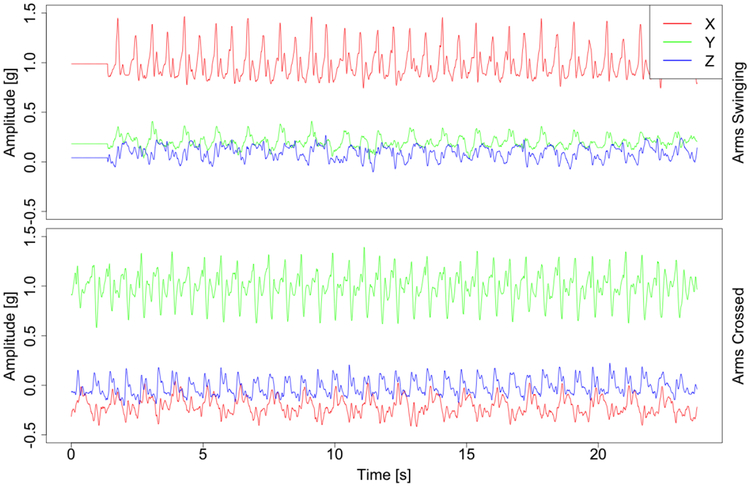
Because wearable PA monitors collect acceleration data relative to earth gravity, they are sensitive not only to movement but also to their own orientation with respect to Earth’s gravity. To better understand this, the top panels in Figure 5 display accelerometry data collected by a wrist-worn device during two walking tasks performed by the same individual. The upper panel corresponds to walking with both hands moving naturally, whereas the bottom panel corresponds to walking with arms crossed on the chest. The change in the device orientation is manifested in the change of mean values, most clearly seen in the signals shown in green. In the free-living environment changes in device rotation are quite common and can be due to multiple sources. For example, when walking individuals could sway their hands normally, hold them in their pockets or perform an activity (e.g. holding a smartphone), walking with hands hanging loose or with hands in the pockets. Additionally, the device can rotate around the wrist or move higher or lower on the hand, resulting in an altered distribution of the observed signal.
Figure 5.
Accelerometry data from three orthogonal axes of an accelerometer located on the left wrist, collected during two walking tasks performed by the same individual. Each axis data is shown in a different color. The upper panel corresponds to walking with both hands moving naturally, whereas the bottom panel corresponds to walking with arms crossed on the chest.
To prevent a device from rotating, it can be directly attached to the skin with adhesive pads or affixed indirectly with a waistband clip or elastic belt (Matthews et al, 2012). Indeed, it has been recommended that devices should be fitted as tightly to the body as possible (Boerema et al, 2014). However, even with these precautions, belts can loosen up, resulting in device orientation changes (O’Neill et al, 2017). Devices that adhere to the skin might be attached upside-down or placed in a slightly different position when detached and reattached. Moreover, for devices that have it, the orientation chart can be obscured, which can result in improper device orientation (Edwardson et al, 2016). We consider that all these precautions should be carefully implemented and adapted to the specific problem that one tries to address. In addition, it is important to understand the extent of the problem in specific applications and, when possible, attempt to correct it. Several methods were proposed to address this problem by rotating the observed three-dimensional vector to the common, reference, orientation (Xiao et al, 2016; Yurtman and Barshan, 2017). When one uses summary metrics that are robust to device orientation, this problem is less important. For example, ENMO, VMC and AI are all rotation invariant.
3.5. Sampling frequency
Sampling frequency fs (expressed in Hz) is the parameter describing how often accelerometry data are collected by the device. In modern wearable accelerometers sampling frequency usually ranges between 10 to 200 Hz, though it could be set as high as 1000 Hz for specialized applications, such as precise human movement tracking during sports activities (Dominguez-Vega et al, 2015). One of the hidden problems is that the summaries produced by various devices can depend on the sampling frequency of the device. This could have substantial implications if, for example, in a study the sampling frequency is varied between- and within-individuals and/or devices. For example, according to ActiGraph, LLC, the manufacturer of ActiGraph PA monitors, the observed activity counts depend on the sampling frequency (ActiGraph, 2016).
Figure 6 illustrates the boxplots of ENMO (top panel), VMC (middle panel) and AI0 (bottom panel) calculated for all 49 participants during writing, washing dishes, vacuuming, getting dressed and walking in 5-s time intervals. Data were collected by the device located on the left wrist with the original sampling frequency fs = 80 Hz. Additionally, to simulate lower sampling frequencies, data has been filtered with low-pass FFT filter and decimated to obtain sampling frequencies of 40, 20 and 10 Hz. The cut-off of the FFT filter was set up to corresponding Nyquist frequencies of 20, 10, and 5 Hz respectively. The median summary values are reported in Table 1. Interestingly, all open source summaries are relatively stable as a function of frequency, with stronger decreases at 10 Hz. For the AI0 statistic, the change is most pronounced for walking, where the median AI0 decreases by 19.0% from 80 to 10 Hz. For the other activities the reduction is much smaller in the 1 to 7% range. These smaller differences in open source measures are encouraging. Indeed, Brønd and Arvidsson (2016) investigated the effects of sampling frequency on ActiGraph activity counts. They compared results obtained during walking and running with the default 30 Hz sampling frequency with 40 and 100 Hz sampling frequencies. For fast run activity, they reported approx. 6,800 counts per minute (cpm) mean for default 30 Hz frequency and an increase of mean cpm as high as 24% for 40 Hz and 18% for 100 Hz frequency.
Figure 6.
Boxplots of ENMO, (top panels) VMC (middle panels) and AI0 (bottom panels) for 5 second time windows. Data is shown for all 49 individuals in the study and were collected from the left wrist during writing, washing dishes, vacuuming, getting dressed and walking (x-axis). Data were collected with the original sampling frequency fs = 80 Hz and then decimated to simulate sampling frequencies of 40, 20 and 10 Hz.
Table 1.
Median values of ENMO, VMC and AI0 statistics derived for τ = 5-s length intervals of data collected from the left wrist during writing, washing dishes, vacuuming, getting dressed and walking, for all 49 individuals. Results are obtained for original sampling frequency fs = 80Hz (3rd column) and simulated sampling frequencies fs = 40, 20, 10 Hz (4–6th columns).
| Statistic | Activity | 80 Hz | 40Hz | 20Hz | 10Hz |
|---|---|---|---|---|---|
| ENMO | Writing | 0.015 | 0.015 | 0.016 | 0.016 |
| ENMO | Washing Dishes | 0.014 | 0.014 | 0.014 | 0.014 |
| ENMO | Vacuuming | 0.031 | 0.031 | 0.031 | 0.028 |
| ENMO | Getting Dressed | 0.040 | 0.040 | 0.040 | 0.036 |
| ENMO | Walking | 0.195 | 0.195 | 0.191 | 0.176 |
| VMC | Writing | 0.003 | 0.002 | 0.002 | 0.002 |
| VMC | Washing Dishes | 0.007 | 0.006 | 0.006 | 0.004 |
| VMC | Vacuuming | 0.023 | 0.022 | 0.022 | 0.019 |
| VMC | Getting Dressed | 0.034 | 0.033 | 0.033 | 0.029 |
| VMC | Walking | 0.198 | 0.197 | 0.193 | 0.175 |
| AI0 | Writing | 0.007 | 0.007 | 0.007 | 0.007 |
| AI0 | Washing Dishes | 0.026 | 0.027 | 0.027 | 0.026 |
| AI0 | Vacuuming | 0.071 | 0.071 | 0.070 | 0.066 |
| AI0 | Getting Dressed | 0.089 | 0.089 | 0.088 | 0.083 |
| AI0 | Walking | 0.193 | 0.192 | 0.183 | 0.156 |
The Table 3 in Appendix A) provides the medians, 25-th, and 75-th percentile for the same five activities, but broken down by subject for 5 different subjects. Results are only shown for the hip accelerometer, though similar results are available for wrist accelerometers. The ranking of activity intensities by medians across subjects is the same, but the medians for individual subjects are quite variable even for the same activity and summary metric. For reference, at the hip, AI0 is roughly around 0 mg for writing, between 1 and 2 mg for washing dishes, 3 and 14 mg for vacuuming, 5 and 10 mg for getting dressed, and 20 to 100 mg for walking. Here we used only the minimum of the first and maximum of the third quartiles across the five subjects to create these ranges. These measures are averages per second during the 5-second intervals and not totals. If one would like to transform these numbers into totals per minute then the values need to be multiplied by 60; similar for other intervals.
3.6. Measurement bias and calibration effects
Measurement bias is the difference between the measured accelerations and their true values. Estimation of both bias and measurement error of accelerometry data requires a dedicated experimental setup utilizing calibrated vibration exciters. The device is exposed to a known acceleration and the measured acceleration time series is compared to this known acceleration, as described in Bassett et al (2012). Authors noted that newer devices, such ActiGraph GT1M, undergo initial unit calibration during production and are supposed to be calibrated for as long as they are used. However, the calibration standards of the different manufacturers may be different. Therefore, we recommend doing some basic calibration checks before utilizing the device in a study.
Even when dynamic calibration is conducted, bias in static measurements can still exist. Ideally, an accelerometer resting on a flat surface, with one measurement axis oriented perpendicularly to the ground, should measure a constant acceleration of 1g for that axis and 0g for the other two orthogonal axes. In practice, measurements may deviate slightly due to their imprecision or to the quality of assembly, which may, for example, misalign the accelerometer axes with the monitors’ casing. In theory, the vector magnitude (Eq. (1)) for resting state (no movement) is equal to 1g, as the earth’s gravity is the only force acting on the accelerometer. In practice, however, the vector magnitude at rest can be slightly different from 1g. To quantify this calibration bias, we calculated a vector magnitude r(t) averages from 5-s time windows, denoted , for the acceleration signal collected from the hip during sitting still activity, for all 49 subjects. We report the percentiles of this distribution in Table 2. Ideally, if no bias was present in the data, values should all be equal to 1. The median is 1.007 indicating very close agreement with what we expect. However, the 5 and 95 percentiles were 0.964 and 1.047, indicating that 10% of the devices have a deviation of 5% or more from 1g at rest.
Table 2.
Percentiles of , vector magnitude r(t) averages from 5-s time windows, for the acceleration signal collected from the hip during sitting still activity, for all 49 subjects.
| Percentile | 5 | 25 | 50 | 75 | 95 |
| 0.964 | 0.991 | 1.007 | 1.016 | 1.047 |
The Activity Index (Bai et al, 2016) was designed to be robust to bias by subtracting the local mean around each axis and to measurement error by constructing the mean relative to the variability- at rest. An additional calibration procedure was also introduced for ENMO to mitigate the effects of calibration bias (van Hees et al (2014)). This procedure performs a linear transformation on the raw data before computing the Euclidean norm, resulting in a calibrated version of ENMO.
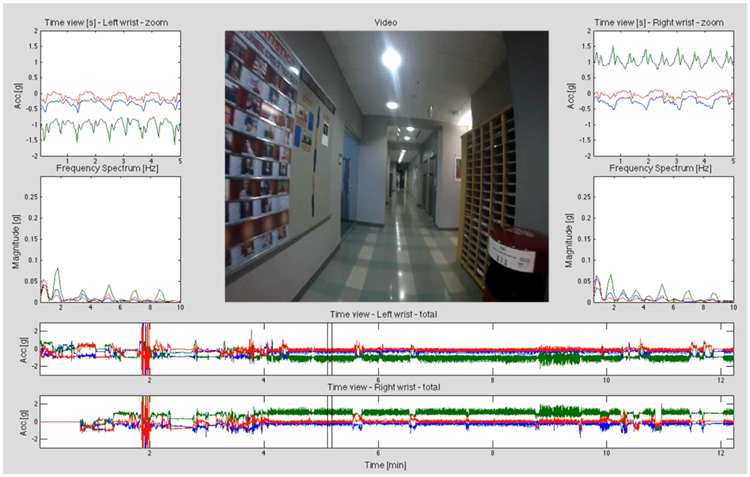
3.7. Data labeling
Classification of physical activity types requires a training set that contains the “gold standard” activity labels. Usually, labeling of accelerometry data is performed by a human observer who marks the times of the beginning and end of each activity. This procedure can be conducted either by direct observation of participants’ activity or during a post-experiment inspection of video recording. An example of a proprietary software created using Matlab (Mathworks, 2016) and used for manual labeling of accelerometry data based on video recordings is shown in Figure 7. The process of obtaining “gold standard” labels is labor-intensive and typically limited to “in-the-lab” experiments or to a small number of participants of “in-the-wild” experiments.
Figure 7.
View of a software used for labeling of raw accelerometry data synchronized with video recordings from a body-worn camera.
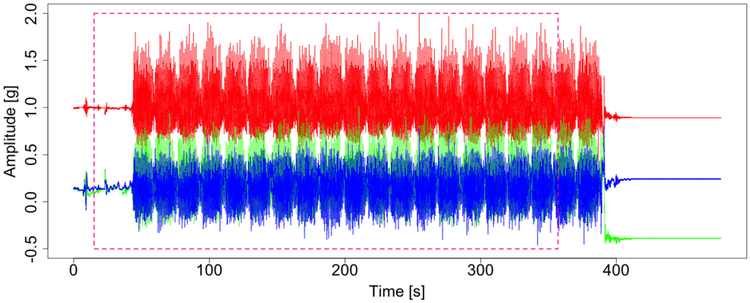
Even “gold standard” labels are of different quality, depending on the accuracy and resolution at which the activity type is predicted. For example, when one is interested in predicting standing up from a chair, the duration of the activity is in the 1 to 4 second range. This makes accurate labeling even for a human observer extremely difficult. If one is interested in predicting whether the person walked or not in a particular 1 minute interval, the labels will be less accurate and will simply indicate whether the person has walked in a particular interval and approximately around what time stamp and for how long. However, even these labels can be substantially misaligned. This can be due to multiple factors including imperfect synchronization of clocks, time elapsed between the beginning and recording of the task, basic observer or data entry error. As an example, Figure 8 displays a portion of the acceleration data recorded at the hip for one subject. The dashed-line box is the portion of 400-meter-walk period labeled by the human observer. There is a clear 45 second shift in the label relative to the actual activity. In such cases using the original label without inspection would lead to inferior prediction algorithms and a waste of resources during the modeling phase. We chose to manually inspect all “in-the-lab” data for each subject and re-label walking as periods that closely correspond to the sustained harmonic walking (SHW). The overlap between the labels provided by the human observer and the labels improved by human inspection of the data was below 80% in 18 out of 49 subjects.
Figure 8.
Accelerometry data from three orthogonal axes at the hip collected around the time when a participant performed a 400-meter-walk activity. The dashed-line red box indicates the portion of the 400-meter-walk period identified by a human observer.
The most effective approach to proper labeling is synchronization of accelerometry data with video-recordings of the experiment (Bussmann et al, 1998). This method has been successfully used in many “in-the-lab” experiments (Godfrey et al, 2015; Del Din et al, 2016). However, using video-recordings for labeling free-living data is harder and subject to privacy considerations. Indeed, it is possible to equip participants with body-worn cameras, but video data de-identification can be quite challenging as it might contain family members, car plates, and addresses. In spite of these limitations, body-worn cameras have been used to label PA collected in the free-living environment. For example, Ellis et al (2016) used video data to train a PA classifier and Hickey et al (2017) used video data to train a walking prediction algorithm. In Hickey’s experiment, body-worn cameras were facing down to record only the feet movement.
Another, less labor-intensive, approach for precise labeling of raw accelerometry data is to use landmarks introduced by the individual wearing the device. For example, in the case of wrist-worn devices, participants can clap their hands before and after each task. Claps result in high-amplitude, short-time spikes in the observed data that can be used to estimate timestamps for each task. For other body locations, participants can vigorously tap the device to generate proper landmarks in the data. This approach was successfully used in Straczkiewicz et al (2016). Another approach is to use the device-specific own event-markers to place labeling landmarks. Some modern PA monitors have built-in event marker buttons (e.g. Actiwatch Spectrum Plus and Pro). These event-markers generate binary indicators at the same granularity as that of the observed accelerations. When pressed, they return a value of 1 until pressed again. Initially, they were intended to mark major everyday activities (e.g. sleep) and critical events (e.g. falls), but they can be used for labeling data, as well. Unfortunately, the utility of event markers is limited by the compliance of participants (Chen et al, 2014; Boudebesse et al, 2015).
3.8. Synchronization of multiple PA monitors
Many studies collect data using multiple PA sensors. Synchronizing data across different monitors allows combining information about specific human movements at multiple locations on the body (Bao and Intille, 2004; Cleland et al, 2013; He et al, 2014; Altini et al, 2015). Most devices can be set up to initialize their measurement collection at a given time (e.g. at midnight) and/or can be initialized manually. In practice, even if such approaches are used, measurements might still be desynchronized between devices. We identify two main reasons for device desynchronization.
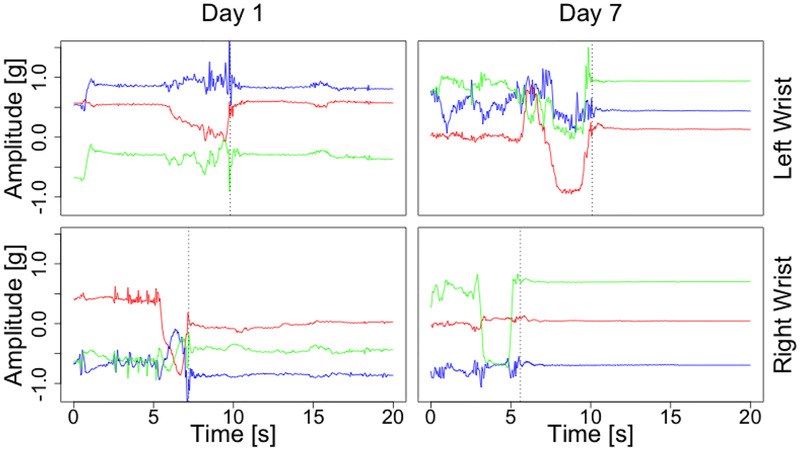
First, most operating systems used in personal computers are not real-time operational systems. Therefore, time of execution of any command can not be precisely determined (see details in Stallings (2008)). That may result in subsecond level differences in measurements start times on multiple PA monitors. Second, the internal drift of device clocks can lead to inaccurate stamping of the time interval (Bennett et al, 2015). Such drifts are usually small (a few seconds per day) and can typically be ignored. However, when combining sub-second level data from multiple sensors in the free-living environment, the effects of the drift can have substantial side effects. To illustrate these problems, Figure 9 displays 20 seconds of data collected in the free-living environment by two monitors located on the left (top panels) and the right wrist (bottom panels). The two sensors were synchronized at the beginning of the experiment. The left and right column provide data collected on the first and seventh day of observation, respectively. The dotted vertical lines mark the end of a high-amplitude activity for each device. Although visually, data from the two devices appear to be correlated during both days, a shift in the two recordings is apparent on both days. On day 1 the time-shift is around 2.5 s, which is probably due to the imperfect timing of device initialization. On day 7 the time shift is about 4 s, with the additional 1.5 s probably due to drift in device clocks. This drift need not be in the same direction or of the same magnitude for all devices. Such de-synchronization would have minor implications for PA summaries at the minute level collected over a 7 to 14 days period, but they can lead to substantial differences when one is interested in analyzing sub-second level data.
Figure 9.
Accelerometry data representing 20 s of data collected in the free-living environment using two monitors located on the left wrist (top panels) and the right wrist (bottom panels). The two sensors were synchronized at the beginning of the experiment. The left and right column provide data collected on the first and seventh day of observation, respectively.
The time shift introduced during device synchronization and initialization can be addressed using video recordings or landmarks. Lab experiments rarely last more than a few hours, and the effects of time drift can often be ignored. However, for data collected ‘in the free-living environment, the effects of time drift are cumulative, which can raise substantial challenges for data analysis. A possible solution could be to use devices designed specifically for parallel measurements. For example, GaitUp (GaitUp, 2017) is a system for synchronous measurement of feet movement. Alternatively, one can perform landmark-based synchronization for every time-interval in the data (e.g. everyday).
4. Discussion
We have presented challenges related to the collection and analysis of raw, sub-second level accelerometry data. The increased granularity of observations when moving from minute to sub-second resolution leads to a large increase both in the volume and complexity of the data. This makes raw data more difficult to use than summarized data, but also holds promise of unlocking additional information glossed over by taking minute-, hour-, or day-level summaries. For example, describing gait parameters during the course of the day in the free-living environment and characterizing their potential association with health outcomes cannot be done without using sub-second level data (Urbanek et al, 2018b). Additionally, prediction of activities of daily living (Bai et al, 2012; He et al, 2014) or detection of posture changes (Curone et al, 2010) would be impossible with minute-level summaries.
Raw accelerometry data requires specialized visualization and analytic methods. This is fertile ground both for scientific researchers, as additional information is likely embedded in the raw signals, and for data scientists, as new methods and insights are becoming increasingly necessary. To start addressing this complexity we make a few points that are worth remembering: 1) activity counts are summaries of the raw data, which can depend on the device manufacturer, software version, and body location; 2) open source summary statistics are increasingly available, though more research is needed to understand their relative performance; 3) raw and summarized PA data can vary substantially with the device location, between- and within-individuals; 4) proper location choice might yield data signatures tailored to a particular study purpose; 5) device orientation can change over the course of an experiment and needs to be standardized both within- and between-individuals and devices; 6) sampling frequency can affect both raw accelerometry and summarized measurements; 7) device calibration, bias removal, and measurement error quantification can lead to higher quality data; 8) proper labeling of data is very important for training activity classifiers at the sub-second level, especially for short activities; and 9) synchronizing multiple devices must be done carefully and needs to be accounted for during the design of the experiment phase. The relevance of each challenge depends intrinsically on the scientific problem. For example, if one is interested in the total volume of activity then it is not very important when walking took place during the day. In this case, the sensor location and proper calibration are particularly important factors in calculating PA activity summaries (e.g., ENMO, VMC, AI). However, if one is interested in characterizing the timing, type, and context of movement then a deeper look at the signals is necessary. Body-location, the orientation of the device, sampling frequency, and labeling are crucially important in these situations. Synchronization of multiple devices is probably the least prevalent problem in health research, as most studies employ one wearable device per participant. However, integrating information from multiple accelerometers increases the accuracy of activity type prediction (He et al. 2014) and provides information about the type of activity (e.g.. primarily upper or lower body activity). In addition, it has become increasingly useful to deploy accelerometers with other wearable and implantable devices, such as ambulatory ECG monitors (e.g. Zio XT Patch; Irhythm Technologies Inc, 650 Townsend Street, Suite 500, San Francisco, CA 94103) or implantable blood-glucose monitors (e.g. Eversense CGM System; Senseonics Inc, 20451 Seneca Meadows Pkwy, Germantown, MD 20876). Synchronizing these measurements, especially when they collect data sampled at different time scales, will thus become increasingly important.
In spite of these challenges, the number of publications focused on raw accelerometry is continuously increasing, especially in the area of activity type classification. This is due in part to the increased popularity of these devices, their convenient design, and reduced cost. The application of raw accelerometry data in epidemiological studies is still in its infancy, though some important steps forward have been made. We anticipate that, as the interest changes to understanding the details of human movement kinematics in the free-living environment, the focus on raw data will become stronger. The number of studies that both collect and disseminate raw activity data will probably provide a huge boost to raw accelerometry data research. For example, the UK Bio-bank PA dataset is currently the largest of its kind. It was collected using the open-hardware AX3 acceleration sensor (Doherty et al, 2017).
In closing, we offer a few practical suggestions for the scientists who would like to conduct their own activity studies: 1) discuss your plans with a team that has expertise in activity research; 2) avoid the pitfalls of accelerometry by choosing high-quality, research-grade devices; 3) if possible, use established protocols for data collection and pre-processing; 4) record and store the raw accelerometry data in addition to summaries, such as activity counts; 5) conduct a lab study and record the activity summaries for a well-defined group of activities in 10 to 100 individuals who are representative of the population to be studied.
5. Acknowledgements
The authors would like to acknowledge Annemarie Koster, PhD and Paolo Caserotti, PhD for designing the DECOS experiments.
6. Funding
This research was supported by Pittsburgh Claude D. Pepper Older Americans Independence Center, Research Registry, and Developmental Pilot Grant (PI: Glynn) NIH P30 AG024826 and NIH P30 AG024827. National Institute on Aging Professional Services Contract HHSN271201100605P. NIA Aging Training Grant (PI: AB Newman) T32-AG-000181. The project was supported, in part, by the Intramural Research Program of the National Institute on Aging.
A. Appendix
Table 3.
Summary of the four statistics: ENMO, VMC, AI0 and AI for five selected subjects and all subjects: median, 25-th percentile and 75-th percentile (percentiles are reported in brackets), obtained from accelerometry data collected at the hip during five activities: writing, washing dishes, vacuuming, getting dressed and walking.
| id | Writing | Washing Dishes | Vacuuming | Getting Dressed | Walking |
|---|---|---|---|---|---|
| ENMO | |||||
| Sub. 1 | 0.021 (0.019,0.023) |
0.033 (0.032,0.033) |
0.037 (0.035,0.039) |
0.035 (0.032,0.038) |
0.189 (0.161,0.204) |
| Sub. 2 | 0.084 (0.083,0.085) |
0.029 (0.028,0.030) |
0.031 (0.027,0.047) |
0.055 (0.052,0.058) |
0.147 (0.122,0.158) |
| Sub. 3 | 0.024 (0.022,0.024) |
0.037 (0.037,0.038) |
0.039 (0.037,0.043) |
0.064 (0.059,0.071) |
0.175 (0.157,0.198) |
| Sub. 4 | 0.005 (0.003,0.006) |
0.008 (0.006,0.009) |
0.043 (0.028,0.089) |
0.041 (0.024,0.051) |
0.181 (0.154,0.192) |
| Sub. 5 | 0.017 (0.014,0.023) |
0.019 (0.018,0.019) |
0.038 (0.030,0.066) |
0.035 (0.031,0.044) |
0.297 (0.263,0.318) |
|
All Sub. |
0.015 (0.007,0.025) |
0.014 (0.009,0.025) |
0.031 (0.020,0.047) |
0.040 (0.031,0.055) |
0.195 (0.143,0.257) |
| VMC | |||||
| Sub. 1 | 0.004 (0.002,0.005) |
0.006 (0.006,0.007) |
0.020 (0.015,0.023) |
0.021 (0.017,0.025) |
0.194 (0.166,0.206) |
| Sub. 2 | 0.003 (0.003,0.003) |
0.005 (0.004,0.005) |
0.018 (0.014,0.034) |
0.022 (0.021,0.025) |
0.154 (0.13,0.166) |
| Sub. 3 | 0.002 (0.000,0.003) |
0.006 (0.005,0.007) |
0.015 (0.012,0.026) |
0.058 (0.049,0.068) |
0.182 (0.164,0.205) |
| Sub. 4 | 0.003 (0.000,0.003) |
0.008 (0.006,0.008) |
0.043 (0.028,0.092) |
0.041 (0.024,0.051) |
0.186 (0.158,0.196) |
| Sub. 5 | 0.002 (0.000,0.003) |
0.009 (0.008,0.010) |
0.030 (0.024,0.065) |
0.032 (0.027,0.037) |
0.303 (0.271,0.323) |
|
All Sub. |
0.003 (0.000,0.004) |
0.007 (0.005,0.009) |
0.022 (0.014,0.041) |
0.034 (0.025,0.050) |
0.198 (0.147,0.258) |
| AI0 | |||||
| Sub. 1 | 0.000 (0.000,0.002) |
0.001 (0.001,0.002) |
0.005 (0.003,0.007) |
0.006 (0.005,0.007) |
0.042 (0.033,0.047) |
| Sub. 2 | 0.000 (0.000,0.000) |
0.000 (0.000,0.001) |
0.005 (0.003,0.009) |
0.017 (0.013,0.019) |
0.024 (0.021,0.027) |
| Sub. 3 | 0.000 (0.000,0.001) |
0.001 (0.001,0.002) |
0.003 (0.002,0.006) |
0.009 (0.008,0.009) |
0.034 (0.028,0.040) |
| Sub. 4 | 0.000 (0.000,0.000) |
0.001 (0.001,0.003) |
0.018 (0.007,0.024) |
0.014 (0.010,0.017) |
0.037 (0.033,0.041) |
| Sub. 5 | 0.000 (0.000,0.000) |
0.001 (0.001,0.002) |
0.009 (0.005,0.014) |
0.006 (0.005,0.010) |
0.093 (0.081,0.103) |
|
All Sub. |
0.000 (0.000,0.000) |
0.001 (0.000,0.002) |
0.006 (0.003,0.010) |
0.009 (0.006,0.013) |
0.040 (0.024,0.062) |
| AI | |||||
| Sub. 1 | 5.745 (2.504,7.369) |
14.505 (12.166,16.730) |
37.066 (33.375,41.246) |
28.311 (24.978,37.332) |
128.847 (113.873,135.39) |
| Sub. 2 | 1.124 (0.536,2.210) |
8.421 (7.398,9.537) |
44.291 (39.960,49.576) |
24.230 (21.487,39.287) |
97.084 (88.253,103.289) |
| Sub. 3 | 0.000 (0.000,2.442) |
10.437 (7.720,15.131) |
55.963 (51.028,59.763) |
27.359 (21.271,33.922) |
111.914 (102.208,121.594) |
| Sub. 4 | 0.000 (0.000,2.598) |
11.002 (9.077,13.150) |
51.713 (40.562,61.589) |
59.428 (34.030,83.187) |
117.736 (109.104,122.844) |
| Sub. 5 | 0.000 (0.000,0.544) |
12.948 (11.625,15.230) |
39.288 (34.278,45.534) |
41.695 (30.223,61.612) |
177.989 (161.927,184.464) |
|
All Sub. |
0.000 (0.000,2.294) |
11.396 (7.407,15.713) |
44.566 (35.171,56.015) |
32.03 (20.833,46.736) |
122.077 (95.299,149.542) |
Contributor Information
Marta Karas, Department of Biostatistics, Bloomberg School of Public Health, Johns Hopkins University, Tel.: +1-317-665-4551, mkaras2@jhu.edu.
Jiawei Bai, Department of Biostatistics, Bloomberg School of Public Health, Johns Hopkins University.
Marcin Strączkiewicz, Department of Epidemiology and Biostatistics, School of Public Health, Indiana University Bloomington.
Jaroslaw Harezlak, Department of Epidemiology and Biostatistics, School of Public Health, Indiana University Bloomington.
Nancy W. Glynn, Center for Aging and Population Health, Department of Epidemiology, Graduate School of Public Health, University of Pittsburgh
Tamara Harris, Laboratory of Epidemiology Demography, and Biometry, National Institute on Aging.
Vadim Zipunnikov, Department of Biostatistics, Bloomberg School of Public Health, Johns Hopkins University.
Ciprian Crainiceanu, Department of Biostatistics, Bloomberg School of Public Health, Johns Hopkins University.
Jacek K. Urbanek, Center on Aging and Health, Division of Geriatric Medicine and Gerontology, Department of Medicine, School of Medicine, Johns Hopkins University, jurbane2@jhu.edu
References
- ActiGraph (2016) What are counts? URL https://actigraph.desk.com/customer/en/portal/articles/2515580-what-are-counts-, accessed: 2017-11-23
- Altini M, Penders J, Vullers R, Amft O (2015) Estimating energy expenditure using body-worn accelerometers: A comparison of methods, sensors number and positioning. IEEE Journal of Biomedical and Health Informatics 19(1):219–226, DOI 10.1109/JBHI.2014.2313039 [DOI] [PubMed] [Google Scholar]
- Attal F, Mohammed S, Dedabrishvili M, Chamroukhi F, Oukhellou L, Amirat Y (2015) Physical Human Activity Recognition Using Wearable Sensors. Sensors (Basel) 15(12):31, 314–38, DOI 10.3390/sl51229858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai J, Goldsmith J, Caffo B, Glass TA, Crainiceanu CM (2012) Movelets: A dictionary of movement. Electronic Journal of Statistics 6:559–578, DOI 10.1214/12-EJS684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai J, He B, Shou H, Zipunnikov V, Glass TA, Crainiceanu CM (2014) Normalization and extraction of interpretable metrics from raw accelerometry data. Biostatistics 15(1): 102–116, DOI 10.1093/biostatistics/kxt029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai J, Di C, Xiao L, Evenson KR, LaCroix AZ, Crainiceanu CM, Buchner DM (2016) An activity index for raw accelerometry data and its comparison with other activity metrics. PLoS ONE 11(8), DOI 10.1371/journal.pone.0160644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao L, Intille SS (2004) Activity Recognition from User-Annotated Acceleration Data Pervasive Computing. Pervasive Computing 3001:1–17, DOI 10.1007/978-3-540-24646-6_1 [DOI] [Google Scholar]
- Bassett DR, Rowlands A, Trost SG (2012) Calibration and validation of wearable monitors. Medicine and Science in Sports and Exercise 44(SUPPL.1), DOI 10.1249/MSS.0b013e3182399cf7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett TR, Gans N, Jafari R (2015) Multi-sensor data-driven: Synchronization using wearable sensors In: Proceedings of the 2015 ACM International Symposium on Wearable Computers, ACM, New York, NY, USA, ISWC ‘15, pp 113–116, DOI 10.1145/2802083.2808393, URL http://doi.acm.org/10.1145/2802083.2808393 [DOI] [Google Scholar]
- Boerema S, van Velsen L, Schaake L, Tönis T, Hermens H (2014) Optimal Sensor Placement for Measuring Physical Activity with a 3D Accelerometer. Sensors 14(2):3188–3206, DOI 10.3390/sl40203188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boudebesse C, Geoffroy PA, Henry C, Germain A, Scott J, Lajnef M, Leboyer M, Bellivier F, Etain B (2015) Links between sleep and body mass index in bipolar disorders: An exploratory study. European Psychiatry 30(l):89–93, DOI 10.1016/j.eurpsy.2014.04.006 [DOI] [PubMed] [Google Scholar]
- Brønd JC, Arvidsson D (2016) Sampling frequency affects the processing of Actigraph raw acceleration data to activity counts. Journal of Applied Physiology 120(3):362–369, DOI 10.1152/japplphysiol.00628.2015 [DOI] [PubMed] [Google Scholar]
- Bussmann J, Tulen J, van Herel E, Stam H (1998) Quantification of physical activities by means of ambulatory accelerometry: A validation study. Psychophysiology 35(5):488–96, DOI 10.1017/S0048577298971153 [DOI] [PubMed] [Google Scholar]
- Cain KL (2014) Accelerometer scoring protocol for the ipen-adult study. URL http://www.ipenproject.org/documents/methods_docs/IPEN_Protocol.pdf, accessed: 2017-11-19 [Google Scholar]
- Catellier DJ, Hannan PJ, Murray DM, Addy CL, Conway TL, Yang S, Rice JC (2005) Imputation of Missing Data When Measuring Physical Activity by Accelerometry. Medicine & Science in Sports & Exercise DOI 10.1249/01.mss.0000185651.59486.4e, NIHMS150003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen JH, Waite L, Kurina LM, Thisted Ra, McClintock M, Lauderdale DS (2014) Insomnia Symptoms and Actigraph-Estimated Sleep Characteristics in a Nationally Representative Sample of Older Adults. The journals of gerontology Series A, Biological sciences and medical sciences (8): 1–8, DOI 10.1093/gerona/glul44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen KY, Janz KF, Zhu W, Brychta RJ (2012) Redefining the roles of sensors in objective physical activity monitoring. Medicine and Science in Sports and Exercise 44(SUPPL. 1), DOI 10.1249/MSS.0b013e3182399bc8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi L, Ward SC, Schnelle JF, Buchowski MS (2012) Assessment of wear/nonwear time classification algorithms for triaxial accelerometer. Med Sci Sports Exerc 44 (10): 2009–2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleland I, Kikhia B, Nugent C, Boytsov A, Hallberg J, Synnes K, McClean S, Finlay D (2013) Optimal placement of accelerometers for the detection of everyday activities. Sensors (Basel, Switzerland) 13(7):9183–9200, DOI 10.3390/sl30709183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook DJ, Thompson JE, Prinsen SK, Dearani JA, Deschamps C (2013) Functional recovery in the elderly after major surgery: Assessment of mobility recovery using wireless technology. Annals of Thoracic Surgery DOI 10.1016/j.athoracsur.2013.05.092 [DOI] [PubMed] [Google Scholar]
- Copeland JL, Esliger DW (2009) Accelerometer assessment of physical activity in active, healthy older adults. Journal of Aging and Physical Activity DOI 10.1123/japa.l7.1.17 [DOI] [PubMed] [Google Scholar]
- Curone D, Bertolotti GM, Cristiani A, Secco EL, Magenes G (2010) A real-time and self-calibrating algorithm based on triaxial accelerometer signals for the detection of human posture and activity. IEEE Transactions on Information Technology in Biomedicine DOI 10.1109/TITB.2010.2050696 [DOI] [PubMed] [Google Scholar]
- Del Din S, Hickey A, Hurwitz N, Mathers JC, Rochester L, Godfrey A (2016) Measuring gait with an accelerometer-based wearable: influence of device location, testing protocol and age. Physiological measurement 37(10):1785–1797, DOI 10.1088/0967-3334/37/10/1785 [DOI] [PubMed] [Google Scholar]
- Di J, Leroux A, Urbanek J, Varadhan R, Spira A, Schrack J, Zipunnikov V (2017) Patterns of sedentary and active time accumulation are associated with mortality in us adults: The nhanes study. bioRxiv DOI 10.1101/182337, URL https://www.biorxiv.org/content/early/2017/08/31/182337, https://www.biorxiv.org/content/early/2017/08/31/182337.full.pdf [DOI] [Google Scholar]
- Doherty A, Jackson D, Hammerla N, Plötz T, Olivier P, Granat MH, White T, Van Hees VT, Trenell MI, Owen CG, Preece SJ, Gillions R, Sheard S, Peakman T, Brage S, Wareham NJ (2017) Large scale population assessment of physical activity using wrist worn accelerometers: The UK biobank study. PLoS ONE 12(2), DOI 10.1371/journal.pone.0169649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominguez-Vega ZT, Martinez-Mendez R, Lorias-Espinoza D (2015) High sampling rate datalogger for the characterization of acceleration signals on the human body running In: 25th International Conference on Electronics, Communications and Computers, CONIELECOMP 2015, pp 173–177, DOI 10.1109/CONIELECOMP.2015.7086947 [DOI] [Google Scholar]
- Edwardson CL, Winkler EA, Bodicoat DH, Yates T, Davies MJ, Dunstan DW, Healy GN (2016) Considerations when using the activPAL monitor in field based research with adult populations. Journal of Sport and Health Science (May): 13–24, DOI 10.1016/j.jshs.2016.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis K, Kerr J, Godbole S, Staudenmayer J, Lanckriet G (2016) Hip and wrist accelerometer algorithms for free-living behavior classification. Medicine and Science in Sports and Exercise 48(5):933–940, DOI 10.1249/MSS.0000000000000840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esliger DW, Copeland JL, Barnes JD, Tremblay MS (2005) Standardizing and optimizing the use of accelerometer data for free-living physical activity monitoring. Journal of Physical Activity and Health 2(3):366–383, DOI http://dx.doi.Org/10.1123/jpah.2.3.366 [Google Scholar]
- Fairclough SJ, Noonan R, Rowlands AV, van Hees V, Knowles Z, Boddy LM (2016) Wear compliance and activity in children wearing wrist- and hip-mounted accelerometers. Medicine and Science in Sports and Exercise 48(2):245–253, DOI 10.1249/MSS.0000000000000771 [DOI] [PubMed] [Google Scholar]
- Fitzsimons CF, Kirk A, Baker G, Michie F, Kane C, Mutrie N (2013) Using an individualised consultation and activPALc feedback to reduce sedentary time in older Scottish adults: Results of a feasibility and pilot study. Preventive Medicine DOI 10.1016/j.ypmed.2013.07.017 [DOI] [PubMed] [Google Scholar]
- Fortune E, Lugade V, Morrow M, Kaufman K (2014) Validity of using triaxial accelerometers to measure human movement - Part II: Step counts at a wide range of gait velocities. Medical Engineering and Physics 36(6):659–669, DOI 10.1016/j.medengphy.2014.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedson P, Bowles HR, Troiano R, Haskell W (2012) Assessment of physical activity using wearable monitors: Recommendations for monitor calibration and use in the field. Medicine and Science in Sports and Exercise 44(SUPPL. 1):S1–S4, DOI 10.1249/MSS.0b013e3182399b7e [DOI] [PMC free article] [PubMed] [Google Scholar]
- GaitUp (2017) Products. URL https://www.gaitup.com/products/, accessed: 2017-11-25
- Godfrey A, Del Din S, Barry G, Mathers JC, Rochester L (2015) Instrumenting gait with an accelerometer: A system and algorithm examination. Medical Engineering and Physics 37(4):400–407, DOI 10.1016/j.medengphy.2015.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gresham G, Schrack J, Gresham LM, Shinde AM, Hendifar AE, Tuli R, Rimel BJ, Figlin R, Meinert CL, Piantadosi S (2018) Wearable activity monitors in oncology trials: Current use of an emerging technology. DOI 10.1016/j.cct.2017.11.002 [DOI] [PubMed]
- He B, Bai J, Zipunnikov VV, Koster A, Caserotti P, Lange-Maia B, Glynn NW, Harris TB, Crainiceanu CM (2014) Predicting human movement with multiple accelerometers using movelets. Medicine and Science in Sports and Exercise 46(9):1859–1866, DOI 10.1249/MSS.0000000000000285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy GN, Matthews CE, Dunstan DW, Winkler EAH, Owen N (2011) Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 200306. European Heart Journal 32(5):590–597, DOI 10.1093/eurheartj/ehq451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hees VT, Gorzelniak L, Dean León EC, Eder M, Pias M, Taherian S, Ekelund U, Renström F, Franks PW, Horsch A, Brage S (2013) Separating Movement and Gravity Components in an Acceleration Signal and Implications for the Assessment of Human Daily Physical Activity. PLoS ONE 8(4), DOI 10.1371/journal.pone.0061691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hees VT, Fang Z, Langford J, Assah F, Mohammad A, da Silva ICM, Trenell MI, White T, Wareham NJ, Brage S (2014) Autocalibration of accelerometer data for free-living physical activity assessment using local gravity and temperature: an evaluation on four continents. Journal of Applied Physiology 117(7):738–744, DOI 10.1152/japplphysiol.00421.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickey A, Del Din S, Rochester L, Godfrey A (2017) Detecting free-living steps and walking bouts: Validating an algorithm for macro gait analysis. Physiological Measurement 38(1):N1–N15, DOI 10.1088/1361-6579/38/1/N1 [DOI] [PubMed] [Google Scholar]
- IJmker T, Lamoth CJ (2012) Gait and cognition: The relationship between gait stability and variability with executive function in persons with and without dementia. Gait and Posture 35(1):126–130, DOI 10.1016/j.gaitpost.2011.08.022 [DOI] [PubMed] [Google Scholar]
- Koster A, Shiroma EJ, Caserotti P, Matthews CE, Chen KY, Glynn NW, Harris TB (2016) Comparison of Sedentary Estimates between activPAL and Hip- and Wrist-Worn ActiGraph. Medicine and Science in Sports and Exercise 48(8):1514–1522, DOI 10.1249/MSS.0000000000000924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange-Maia BS, Newman AB, Strotmeyer ES, Harris TB, Caserotti P, Glynn NW (2015) Performance on fast- and usual-paced 400-m walk tests in older adults: are they comparable? Aging Clinical and Experimental Research 27(3):309–314, DOI 10.1007/s40520-014-0287-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyden K, Keadle SK, Staudenmayer J, Freedson PS (2014) A method to estimate free-living active and sedentary behavior from an accelerometer. Medicine and Science in Sports and Exercise 46(2):386–397, DOI 10.1249/MSS.0b013e3182a42a2d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariani B, Rouhani H, Crevoisier X, Aminian K (2013) Quantitative estimation of foot-flat and stance phase of gait using foot-worn inertial sensors. Gait and Posture 37(2):229–234, DOI 10.1016/j.gaitpost.2012.07.012 [DOI] [PubMed] [Google Scholar]
- Mathworks (2016) MATLAB - Mathworks - MATLAB & Simulink. DOI 2016-11-26
- Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, Troiano RP (2008) Amount of time spent in sedentary behaviors in the United States, 2003–2004. American Journal of Epidemiology 167(7):875–881, DOI 10.1093/aje/kwm390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews CE, Hagströmer M, Pober DM, Bowles HR (2012) Best practices for using physical activity monitors in population-based research. Medicine and Science in Sports and Exercise 44(SUPPL. 1):68–76, DOI 10.1249/MSS.0b013e3182399e5b [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHANES (2006) National Health and Nutrition Examination Survey. 2003–2004 Data Documentation, Codebook, and Frequencies. Physical Activity Monitor Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS), Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, URL https://wwwn.cdc.gov/Nchs/Nhanes/2003-2004/PAXRAW_C.htm, accessed: 2017-11-19. [Google Scholar]
- NHANES (2008) National Health and Nutrition Examination Survey. 2005–2006 Data Documentation, Codebook, and Frequencies. Physical Activity Monitor Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS), Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, URL https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/PAXRAW_D.htm, accessed: 2017-11-19. [Google Scholar]
- NHANES (2011) National Health and Nutrition Examination Survey. 2011–2012 Physical Activity Monitor (PAM) Procedures Manual Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS), Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, URL https://wwwn.cdc.gov/nchs/data/nhanes/2011-2012/manuals/Physical_Activity_Monitor_Manual.pdf, accessed: 2017-11-19. [Google Scholar]
- O’Neill B, McDonough SM, Wilson JJ, Bradbury I, Hayes K, Kirk A, Kent L, Cosgrove D, Bradley JM, Tully MA (2017) Comparing accelerometer, pedometer and a questionnaire for measuring physical activity in bronchiectasis: a validity and feasibility study. Respiratory Research 18(1):16, DOI 10.1186/sl2931-016-0497-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pober DM, Staudenmayer J, Raphael C, Freedson PS (2006) Development of Novel Techniques to Classify Physical Activity Mode Using Accelerometers. Medicine and Science in Sports and Exercise 38(9):1626–1634, DOI 10.1249/01.mss.0000227542.43669.45 [DOI] [PubMed] [Google Scholar]
- Preece SJ, Goulermas JY, Kenney LPJ, Howard D, Meijer K, Crompton R (2009) Activity Identification using Body-Mounted Sensors - A Review of Classification Techniques. Physiological Measurement 30(4):R1–R33, DOI 10.1088/0967-3334/30/4/R01 [DOI] [PubMed] [Google Scholar]
- Rosenberger ME, Haskell WL, Albinali F, Mota S, Nawyn J, Intille S (2013) Estimating activity and sedentary behavior from an accelerometer on the hip or wrist. DOI 10.1249/MSS.0b013e31827f0d9c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrack JA, Zipunnikov V, Goldsmith J, Bai J, Simonsick EM, Crainiceanu C, Ferrucci L (2014) Assessing the physical cliff: Detailed quantification of age-related differences in daily patterns of physical activity. Journals of Gerontology - Series A Biological Sciences and Medical Sciences 69(8):973–979, DOI 10.1093/gerona/gltl99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrack JA, Cooper R, Koster A, Shiroma EJ, Murabito JM, Rejeski WJ, Ferrucci L, Harris TB (2016) Assessing Daily Physical Activity in Older Adults: Unraveling the Complexity of Monitors, Measures, and Methods. DOI 10.1093/gerona/glw026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shou H, Zipunnikov V, Crainiceanu CM, Greven S (2015) Structured functional principal component analysis. Biometrics DOI 10.1111/biom.12236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song J, Swartz MD, Gabriel KP, Basen-Engquist K (2018) A semiparametric model for wearable sensor-based physical activity monitoring data with informative device wear. Biostatistics DOI 10.1093/biostatistics/kxx073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stallings W (2008) Operating Systems: Internals and Design Principles, 6th edn. Prentice Hall Press, Upper Saddle River, NJ, USA [Google Scholar]
- Staudenmayer J, Pober D, Crouter S, Bassett D, Freedson P (2009) An artificial neural network to estimate physical activity energy expenditure and identify physical activity type from an accelerometer. Journal of Applied Physiology (Bethesda, Md: 1985) 107(4): 1300–7, DOI 10.1152/japplphysiol.00465.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staudenmayer J, Zhu W, Catellier DJ (2012) Statistical considerations in the analysis of accelerometry-based activity monitor data. Medicine and Science in Sports and Exercise 44(SUPPL. 1), DOI 10.1249/MSS.0b013e3182399e0f [DOI] [PubMed] [Google Scholar]
- Storti KL, Pettee KK, Brach JS, Talkowski JB, Richardson CR, Kriska AM (2008) Gait speed and step-count monitor accuracy in community-dwelling older adults. Medicine and Science in Sports and Exercise 40(l):59–64, DOI 10.1249/mss.0b013e318158b504 [DOI] [PubMed] [Google Scholar]
- Straczkiewicz M, Urbanek JK, Fadel WF, Crainiceanu CM, Harezlak J (2016) Automatic car driving detection using raw accelerometry data. Physiological Measurement 37(10):1757–1769, DOI 10.1088/0967-3334/37/10/1757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, Brach J, Chandler J, Cawthon P, Connor EB, Nevitt M, Visser M, Kritchevsky S, Badinelli S, Harris T, Newman AB, Cauley J, Ferrucci L, Guralnik J (2011) Gait speed and survival in older adults. JAMA: the Journal of the American Medical Association 305(l):50–58, DOI 10.1001/jama.2010.1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano RP (2007) Large-scale applications of accelerometers: New frontiers and new questions. DOI 10.1097/mss.0b013e318150d42e [DOI] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, Mcdowell M (2008) Physical activity in the United States measured by accelerometer. Medicine and Science in Sports and Exercise 40(1): 181–188, DOI 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- Troiano RP, McClain JJ, Brychta RJ, Chen KY (2014) Evolution of accelerometer methods for physical activity research. British Journal of Sports Medicine 48(13):1019–1023, DOI 10.1136/bjsports-2014-093546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trost SG, Mciver KL, Pate RR (2005) Conducting Accelerometer - Based Activity Assessments in Field - Based Research. Medicine and Science in Sports and Exercise 37(ll):531–543, DOI 10.1249/01.mss.0000185657.86065.98 [DOI] [PubMed] [Google Scholar]
- Trost SG, Rosenkranz RR, Dzewaltowski D (2008) Physical activity levels among children attending after-school programs. Medicine and Science in Sports and Exercise DOI 10.1249/MSS.0b013e318161eaa5 [DOI] [PubMed] [Google Scholar]
- Trost SG, Zheng Y, Wong WK (2014) Machine learning for activity recognition: hip versus wrist data. Physiological Measurement 35(11):2183–2189, DOI 10.1088/0967-3334/35/11/2183 [DOI] [PubMed] [Google Scholar]
- Urbanek JK, Vadim Zipunnikov TH, Fadel W, Glynn N, Koster A, Caserotti P, Crainiceanu C, Harezlak J (2015) Prediction of sustained harmonic walking in the free-living environment using raw accelerometry data. URL https://arxiv.org/abs/1505.04066, accessed: 2017-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbanek JK, Harezlak J, Glynn NW, Harris T, Crainiceanu C, Zipunnikov V (2017) Stride variability measures derived from wrist- and hip-worn accelerometers. Gait and Posture 52:217–223, DOI 10.1016/j.gaitpost.2016.11.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbanek JK, Spira AP, Di J, Leroux A, Crainiceanu C, Zipunnikov V (2018a) Epidemiology of objectively measured bedtime and chronotype in US adolescents and adults: NHANES 20032006. Chronobiology International DOI 10.1080/07420528.2017.1411359, 1706.05416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbanek JK, Zipunnikov V, Harris T, Crainiceanu C, Harezlak J, Glynn NW (2018b) Validation of Gait Characteristics Extracted from Raw Accelerometry during Walking Against Measures of Physical Function, Mobility, Fatigability, and Fitness. Journals of Gerontology - Series A Biological Sciences and Medical Sciences DOI 10.1093/gerona/glxl74, 1612.06313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbanek JK, Zipunnikov V, Harris T, Fadel W, Glynn N, Koster A, Caserotti P, Crainiceanu C, Harezlak J (2018c) Prediction of sustained harmonic walking in the free-living environment using raw accelerometry data. Physiological Measurement DOI 10.1088/1361-6579/aaa74d, 1505.04066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vähä-Ypyä H, Vasankari T, Husu P, Suni J, Sievänen H (2015) A universal, accurate intensity-based classification of different physical activities using raw data of accelerometer. Clinical Physiology and Functional Imaging 35(1):64–70, DOI 10.1111/cpf.12127 [DOI] [PubMed] [Google Scholar]
- Van Domelen DR (2018) accelerometry: Functions for Processing Accelerometer Data. URL https://CRAN.R-project.org/package=accelerometry, r package version 3.1.2
- Varma VR, Dey D, Leroux A, Di J, Urbanek J, Xiao L, Zipunnikov V (2017) Re-evaluating the effect of age on physical activity over the lifespan. Preventive Medicine DOI 10.1016/j.ypmed.2017.05.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varma VR, Dey D, Leroux A, Di J, Urbanek J, Xiao L, Zipunnikov V (2018) Total volume of physical activity: TAC, TLAC or TAC(λ). DOI 10.1016/j.ypmed.2017.10.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wrobel J, Zipunnikov V, Schrack J, Goldsmith J (2018) Registration for exponential family functional data. Biometrics 0(ja), DOI 10.1111/biom.12963, URL https://onlinelibrary.wiley.com/doi/abs/10.1111/biom.12963, https://onlinelibrary.wiley.com/doi/pdf/10.1111/biom.12963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao L, Li Y, Ruppert D (2013) Fast bivariate P-splines: the sandwich smoother. Journal of the Royal Statistical Society: Series B (Statistical Methodology) DOI 10.1111/rssb.12007, arXiv:1011.4916v2 [DOI] [Google Scholar]
- Xiao L, Huang L, Schrack JA, Ferrucci L, Zipunnikov V, Crainiceanu CM (2015) Quantifying the lifetime circadian rhythm of physical activity: A covariate-dependent functional approach. Biostatistics 16(2):352–367, DOI 10.1093/biostatistics/kxu045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao L, He B, Koster A, Caserotti P, Lange-Maia B, Glynn NW, Harris TB, Crainiceanu CM (2016) Movement prediction using accelerometers in a human population. Biometrics 72(2):513–524, DOI 10.1111/biom.12382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yurtman A, Barshan B (2017) Activity recognition invariant to sensor orientation with wearable motion sensors. Sensors (Switzerland) 17(8), DOI 10.3390/s17081838 [DOI] [PMC free article] [PubMed] [Google Scholar]