Abstract
Remote photoplethysmography (rPPG) allows contactless monitoring of human cardiac activity through a video camera. In this study, we assessed the accuracy and precision for heart rate measurements of the only consumer product available on the market, namely the FacereaderTM rPPG by Noldus, with respect to a gold standard electrocardiograph. Twenty-four healthy participants were asked to sit in front of a computer screen and alternate two periods of rest with two stress tests (i.e. Go/No-Go task), while their heart rate was simultaneously acquired for 20 minutes using the ECG criterion measure and the FacereaderTM rPPG. Results show that the FacereaderTM rPPG tends to overestimate lower heart rates and underestimate higher heart rates compared to the ECG. The Facereader™ rPPG revealed a mean bias of 9.8 bpm, the 95% limits of agreement (LoA) ranged from almost -30 up to +50 bpm. These results suggest that whilst the rPPG FacereaderTM technology has potential for contactless heart rate monitoring, its predictions are inaccurate for higher heart rates, with unacceptable precision across the entire range, rendering its estimates unreliable for monitoring individuals.
Introduction
There is a growing interest in technologies related to the recording and monitoring of personal health parameters. In the current literature there is not yet a general agreement on the definition of personal health monitoring, which includes telecare, assistive technologies, environmental intelligence and wearable health sensors [1]. A review on the subject suggests that "monitoring of personal health" refers to any electronic device or system that monitors a health-related aspect of a person's life outside a traditional clinical or hospital setting. Examples include GPS tracking devices used with patients with mental disorders, blood pressure monitors and smart clothes capable of measuring physiological parameters [2, 3, 4, 5]. Personal health recording systems are more than just static patient data containers; they combine data, knowledge, tools and software, which help both patients with identified needs and generic consumers to become active participants in their health care [6]. Health monitoring technologies are currently being developed for a multitude of customers of all ages and health conditions aiming to integrate medical care environments with health monitoring outside traditional settings [1]. A primary driving factor is the rapid ageing of the population, which is expected to heavily impact on the performance of health systems in many countries, potentially exceeding the available medical resources [7]. Patients, policymakers, providers, tax-payers, employers, and other stakeholders have increasing interest in using personal health records to reduce healthcare costs, without affecting the quality and the efficiency of the healthcare delivery [8].
The monitoring of physiological information is very important for assessing health and access to physiological data is not only necessary in clinical setting but it is becoming increasingly so also in other environments and applications related, for example, to telemedicine [9–13], personal fitness [14–17], e-commerce [18], trading [19, 20] and mental stress caused by the interaction with technology [21–26]. Accurate and precise self-monitoring devices therefore provide potential benefits both to the individual user, by providing real-time feedback on specific physiological parameters, to the health care providers and also to those involved in retail intelligence and analytics [27, 28]. For example, typical physiological and neuroscience research techniques used to study cognitive and affective processes of individuals such as electroencephalography (EEG), functional magnetic resonance imaging (fMRI), eye tracking, biometrics of heart rate, galvanic skin response, and facial expression recognition, are becoming increasingly popular consumer neuroscience methods [29]. These techniques contribute to a deeper understanding of consumers behaviours by gathering quantitative information on their physical and mental state [30]. A growing interest has also raised in the context of emotion detection and recognition, where several devices are now available (e.g. Affectiva, Emotient—An Apple Company, Eyeris, Kairos Ar. Inc., Noldus, nViso, Realeyes) [31].
The conventional and well-established methods to capture physiological information, like electrocardiogram (ECG) or photoplethysmogram (PPG), require the application of electrodes or transducers on the skin (e.g. wet adhesive Ag/AgCl electrodes) during the monitoring period. These methods, although non-invasive, are bothersome, and perhaps irritating and distracting.
Recently, there has been an increasing interest in alternative and less obtrusive methods for monitoring physiological information such as, laser doppler velocimetry for measuring red blood cell velocity, electromagnetic approaches for heart and respiration monitoring, microwave systems or ultrasonic proximity sensor for respiration detection [32, 33].
The remote-photoplethysmography (rPPG) is a low-cost, non-contact and pervasive technique for measuring heart rate (HR) and to infer other psychophysiological data including heart rate variability, respiration rate, blood pressure and oxygenation [34, 35], quality of sleep, heart rhythm disturbances [36], and also mental stress [37] and drowsiness [38]. Its ease of use, low cost and convenience make it an attractive method for biomedical and clinical research as it allows remote heart rate measurements with a simple camera or a smartphone and it can also be integrated with augmented reality platforms [39]. The information acquired through the rPPG essentially refers to the cardiovascular functioning: the periodic blood flow and therefore the variations of blood volume in tissues that follow each cardiac cycle affects the optical properties of the tissues allowing those who are using this technology to measure HR remotely. For this reason, the reflection of the light that can be observed on the regions of the facial skin. This reflection of light is influenced not only by the various phenomena of interaction between light and skin, but also by the change in the volume of blood and the movement of the wall of blood vessels [40, 41]. Based on this principle, an accurate measurement of these changes generates a plethysmographic signal. Research has shown that, given suitable illumination, ambient light can be sufficient to obtain a plethysmographic signal [42] from changes in light reflected from facial skin and thus it is possible to measure and infer on the physiological phenomena of interest. The only hardware required to perform rPPG imaging is a standard camera. Although several techniques based on the use of infra-red (IR) or near infra-red (NIR) cameras exist [43, 44], the most developed and employed algorithms use a colour model method based on red, green and blue (RGB) imaging to acquire a signal from a distance of up to several meters [45, 46, 47]. In technical terms, the main difference between these two methods lies in the fact that both IR and NIR cameras allow a more accurate estimate of HR parameters and exploit the information provided by blood volume variation of vessels. In turn, RGB camera-based method (green light channel), does not provide such a profound and focused estimate of HR, and consider a wider and less focused range of processes which influence the optical properties of the tissues [48]. According to Wang and colleagues [49], the RGB camera-based method presents two main limitations: it is difficult to accurately estimate HR under low-light conditions and under significant ambient light fluctuations; these last two factors together with the head and body movements can drastically affect rPPG signal detection by generating strong artefacts. The general recommendation for proper measurement of HR is to keep the illumination constant and restrict individual movements.
The described methods capture the subject’s face on a video from which the plethysmographic signal is recovered using several image processing techniques and transformations. The rPPG technology, from its first presentation in 2007 [50], has been studied and developed to demonstrate its feasibility first in controlled environments and conditions, and then in increasingly realistic conditions and scenarios. Research has shown that reliable HR measurement can be achieved using low-cost, consumer-grade digital cameras and ambient light sources. Current literature on rPPG focuses on improvement over existing methodology by considering those imaging acquisition factors (environmental lighting, subject movement, and image sensor spectrum sensitivity) that, at this time, represent the main limitation to an optimal rPPG measurement and therefore to collect accurate physiological data (e.g. [51, 52]). All these methods are of interest for the easy, convenient and large-scale deployment of the non-contact HR monitoring technologies.
In this respect the goal of this study was to critically assess the accuracy of a consumer rPPG system by Noldus with respect to HR monitoring and compared its performance to a gold standard electrocardiograph. The FacereaderTM rPPG system by Noldus monitors HR activity through a patented rPPG technology [53]. Although on the market there are probably alternative and more advanced technologies such as the Vital Signs Camera by Philips, which is available for licensing to third part manufacturers, to the authors’ knowledge, the rPPG by Noldus is the only consumer product available on the market and up until today just one study involving this specific tool has been carried out [54]. Although recent evidence suggests that reliable HR measurement can be achieved using different rPPG algorithms [25, 49, 51, 55, 56], the need of further validations and cross comparisons is crucial. The objective of this study is to contribute to the improvement of this kind of technology, which has the potential to assess and monitoring the personal psychophysical status in a simple, convenient and non-invasive way with important applications (e.g. consumer analysis, e-commerce, personal fitness, driving conditions, telemedicine, customer neuroscience) and therefore to its diffusion. Our validation, in case of significant results, could assume a strong relevance regarding the potential but realistic application of remote heart rate monitoring in workplace environments.
Materials and methods
The accuracy and precision of the Facereader rPPG by Noldus (Noldus Information Technology bv, Wageningen—The Netherlands) for measuring HR was assessed with respect to an ECG criterion measure. The ProComp Infiniti T7500M (Thought Technology LTD, Toronto, Canada), is a professional 8 channel multi-modality encoder for real-time, computerized biofeedback and data acquisition used in the clinical and experimental field and constitutes a gold-standard for the measurement of physiological signals. For ECG recorded, the electrode placement sites were prepared by standardized procedures of cleaning, shaving, and abrading the skin to improve signal acquisition and to minimize noise artefacts. Three silver/silver-chloride self-adhesive electrodes were placed in proximal position on the upper torso following the second standard deviation according to the Einthoven triangle [57]. On Einthoven's triangle, the theory of unipolar electrocardiographic leads, and the interpretation of the precordial electrocardiogram). ECG data were recorder and processed using BioGraph Infinity (Thought Technology LTD, Toronto, Canada). HR data was converted to beats per minute (bpm) automatically by the data acquisition software program prior to analysis. For rPPG, the facial landmark estimation is achieved using the Active Appearance Modelling (AAM) technique [54, 58] that has been improved and integrated in the Facereader framework [59]. The AAM is a method of matching statistical models of appearance to images that consists in an efficient iterative matching algorithm by learning the relationship between perturbations in the model parameters and the induced image errors [54, 58]. Using the selected facial regions, skin colour changes are tracked for observing the periodic components caused by the blood volume changes at each heartbeat [60].
The rPPG system requires the use of a video acquisition source for recording the face of the participants. To this end a Logitech HD Pro Webcam C920–1080 HD was employed. The resolution of the videos was 1280 x 720 pixel, and the frame-rate acquisition was 30 fps for a duration of 20 minutes. In order to ensure a high quality of rPPG signal acquired from the skin surface, the whole experiment was carried out under constant lighting conditions. Both the ambient (illumination) and the screen (luminance) were controlled during the entire experiment. These parameters were assessed by an Extech 403125 digital light meter (Extech Instruments, Nashua, NH) pointed towards the screen and placed 5cm above participants’ head and laterally centred with respect to their head. Overall, the total amount of light impacting on participants’ face coming from both the ambient lighting and the screen was kept constant during the entire experiment and did not vary because of the stimuli presentation triggered by the Go/No-Go task. The distance between participants and the 24” LCD stimulus screen (Dell P2414H; www.dell.com) was approximately 60 cm (see Fig 1).
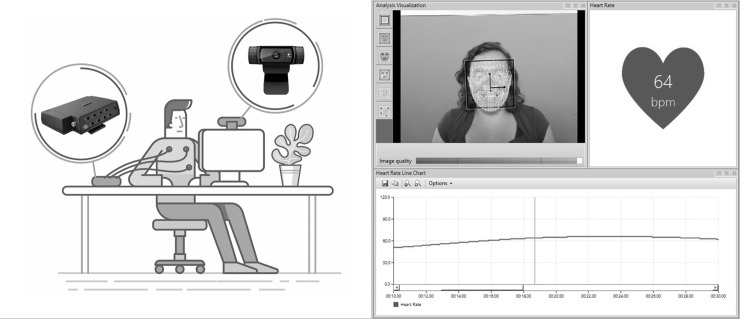
Fig 1. Experimental setup and software.
On the left, a schematic representation of the experimental setup and the devices: ProComp Infiniti T7500M (ECG recording) and Logitech HD Pro Webcam (video acquisition). On the right, a screenshot of the Facereader rPPG software by Noldus.
Twenty-Four healthy participants (11 females) of Western European descent took part in the experiment. The selection of such a specific population was mainly due to the fact that we wanted to reduce the possible effects of skin tone, which constitutes one of the main detection issues for rPPG. All participants gave written informed consent before participation. We excluded participants with cardiovascular diseases (CVD) and with neurological or cognitive disorders. The study was performed in a controlled experiment room at TSW XP Lab, Treviso—Italy (www.tsw.it) complying with the Declaration of Helsinki. The TSW XP Lab Ethics Committee approved the study. Participants were asked to sit in front of the computer screen and alternate two periods of rest with two stress tests (Go/No-Go task), as follows:
Rest [5 min]
Stress test (Go/No-Go task) [5 min]
Rest [5 min]
Stress test (Go/No-Go task) [5 min]
The Go/No-Go task required participants to press the spacebar when they saw a green rectangle appeared (Go) but refrain from pressing the spacebar when they saw a blue rectangle (No-Go). The blue and green rectangles could be either vertically or horizontally aligned. The vertical rectangle had a higher probability of being green (Go trial) and the horizontal rectangle had a higher probability of being blue (No-Go trial). Participants got information about the orientation of the rectangle (cue) shortly before the colour of the rectangle was revealed [61].
The goal of the experiment was to collect enough HR data spanning a range of BPMs as wide as possible. HR was simultaneously acquired for 20 minutes using the ECG criterion measure and the Facereader rPPG by Noldus. With the aim of improving the overall data quality, the rPPG analysis was carried out offline. Given that Facereader allows collecting data at 8 Hz and that BioGraph Infinity allows pre-processing at 8 Hz, we decided to use this frequency for processing cardiac data. Moreover, since movements from the participant may cause artefacts in the HR monitoring, we have manually removed any motion-induced artefacts. Agreement between the Facereader rPPG and the ECG gold standard was estimated using the Bland-Altman method, adapted to consider repeated measures from the same person when the true value varies over time [62, 63]. Bland-Altman plots are widely used to evaluate the agreement among two different instruments or two measurements techniques. This provided an estimate of agreement between the rPPG and ECG in the instantaneous value of the changing heart rate. We also estimated the intraclass correlation coefficient (ICC), which indicates how strongly units in the same group resemble each other, as a complementary measure of agreement. All statistical analyses were performed using StataCorp Stata 15.1.
Results
Table 1 shows means, standard deviations (SD) and ranges for age, weight, height, and Body Mass Index (BMI) of the participants.
Table 1. Means, standard deviations and ranges for Age, Weight, Height, and BMI.
| Male | Female | |||
|---|---|---|---|---|
| Variables | Mean ± SD | Range | Mean ± SD | Range |
| Age (Years) | 31 ± 5 | 23–38 | 27 ±3 | 23–31 |
| Weight (kg) | 76 ± 10 | 62–92 | 59 ± 8 | 45–71 |
| Height (cm) | 178 ± 5 | 168–189 | 166 ± 3 | 160–174 |
| BMI (kg/m2) | 24 ± 2 | 20–27 | 21 ± 3 | 16–25 |
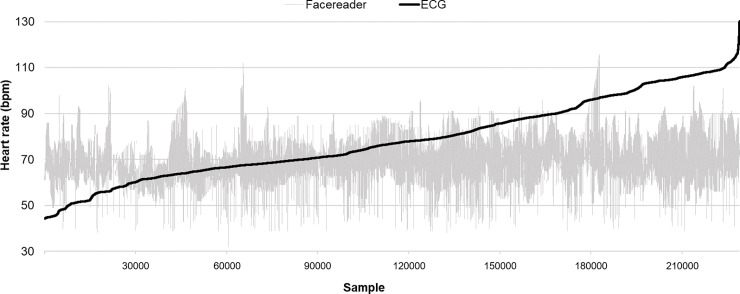
The dataset consisted of 230400 samples of data (1200 seconds x 24 participants x 8 Hz). However, since both the ECG and the Facereader rPPG produced several disruptions to continuous HR detection, the dataset was reduced by around 23%. The final dataset was then made of 177629 samples. Fig 2 shows all time-synced ECG and Facereader rPPG ordered by ECG data in aggregate, with the rPPG estimate demonstrating wide variability and lack of responsiveness to changing heart rate recorded by ECG.
Fig 2. Ordered HR data (Facereader rPPG vs. ECG).
Data have been ordered according to the frequencies collected by the criterion measure (ECG). (n = 230400).
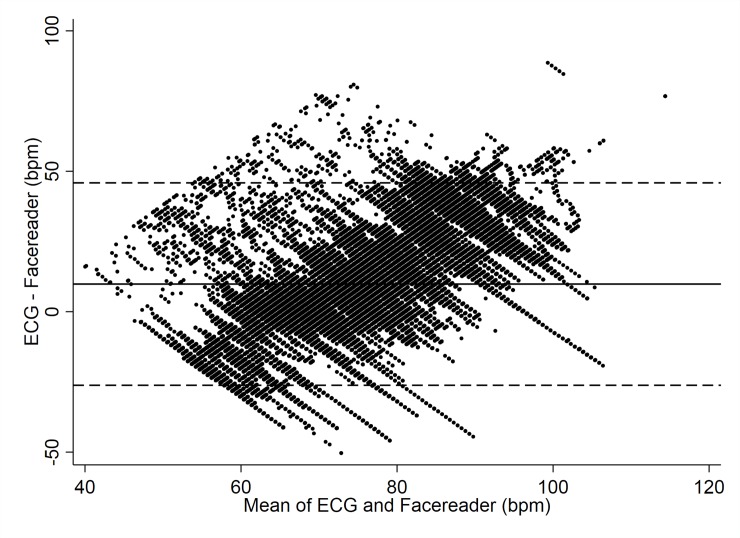
The Facereader rPPG revealed a mean bias of 9.8 bpm (95% CI—Confidence Interval: 9.7 to 9.9 bpm). As to the limits of agreement (LoA) between the Facereader rPPG and criterion measure the upper LoA was 46 bpm, whereas the lower LoA was -26 bpm (Fig 3). The ICC between Facereader rPPG and gold standard ECG was 0.75 (95% CI: 0.64 to 0.86).
Fig 3. HR data (Facereader vs. ECG).
Bland-Altman Plot indicating mean difference in HR detection between the Facereader rPPG and ECG criterion measure.
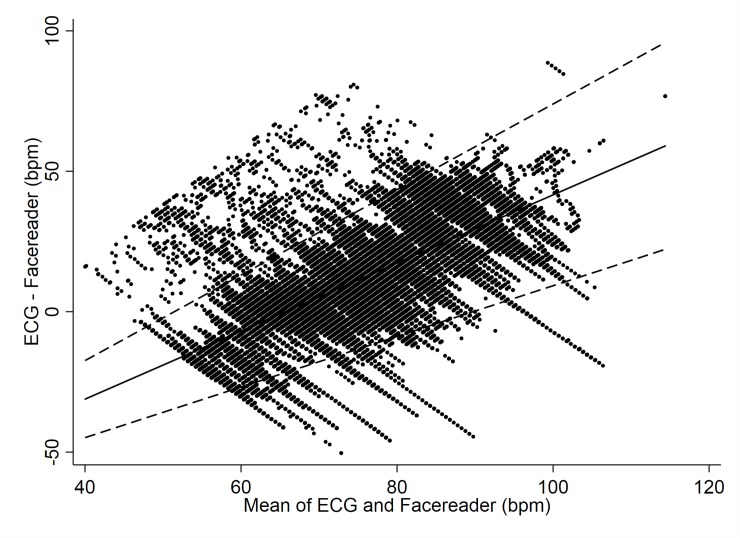
Furthermore, the extent of agreement varied substantially across the range of heart rates (see Fig 4). The Facereader rPPG tends to overestimate lower heart rates (< 80 bpm) compared to the ECG and underestimates higher heart rates (> 80 bpm) compared to the ECG. Since the previous Bland-Altman Plot (see Fig 3) and relative statistics related to the mean bias ignore the general trend, we also provide the Bland-Altman plot with the trend incorporated (Fig 4). At 70 bpm the rPPG under-estimated by just 5 bpm compared to the mean, but with very wide limits of agreement from -18 to 28 bpm. At 80 bpm the rPPG under-estimated by 17 bpm, again with wide limits of agreement from -9 to 43 bpm.
Fig 4. HR data with trend (Facereader vs. ECG).
Bland-Altman Plot modelling a trend over continuous heart rate indicating mean difference in HR detection between the Facereader rPPG and ECG criterion measure.
Discussion
The aim of the present study was to assess in a controlled experimental setting the accuracy of the Facereader rPPG for remote HR monitoring with respect to a gold standard electrocardiograph. Although, recent evidence suggests that reliable HR measurement can be achieved using different rPPG algorithms [25, 49, 51, 55, 56], the need of further validations and cross comparisons is crucial.
To the authors’ knowledge the rPPG by Noldus is the only consumer product available on the market and up until today just one study involving this specific tool has been carried out [54]. Our results show that the agreement between the Facereader rPPG and the ECG is poor. The Facereader tends to over-estimate lower heart rates, and under-estimates higher heart rates compared to the ECG and the error ranges from almost -30 up to +50 bpm (see Fig 2). A first and single validation of the Facereader rPPG has been carried out by the inventors of this patented technology [53, 60]. In their study, the estimated rPPG signal was compared to a ground truth contact PPG sensor and the results of the objective performance tests show strong correlation between the estimated remote and the reference HR [60]. However, the validation was carried out using an unspecified PPG sensor, which cannot be considered a gold standard, no information was provided on the exact value of the correlation and no ICC was calculated. These issues limit our ability to compare our results with theirs. When comparing our results with those of two other related studies, it is possible to observe that in Gonzalez Viejo et al. [54] no correlation was found between the HR results of the oscillometric monitor and those obtained by analysing the video with the Facereader; and that Tasli HE et al. [60], which proposed a novel signal processing approach to extract the periodic component of the raw colour signal for the heart rate and variation estimation, found that the higher HR values (> 100 bpm) are underestimated by Facereader (Fig 3, points outside the confidence limit).
The lack of accurate and precise estimates from the rPPG monitor are in line with our expectations; the technology employed by the Facereader is still in its infancy and other improvements are needed to increase the precision and accuracy of this tool. The Facereader technology and the underlying technique do not overcome the limits of PPG methods in terms of accuracy of HR measurements [17].
With respect to validation studies involving other rPPG methods and ECG criterion measures, the literature is very dense, and the general idea is that rPPG seems to perform quite well. Our results are in contrast with these recent studies in which HR was reliably estimated in various scenarios through rPPG when compared to an ECG reference signal. For example, van Gastel et al. [64] found that, when rPPG was employed for estimate the cardiac activity of infants, the pulse rate can be detected with an average error which ranges from 1.5 to 2.1 bpm and overall the correct HR is detected for 87% of the time; also Fukunishi et al. [65] performed an experiment to measure participants at rest and under cognitive stress in which the remote measurement of HR (rPPG) showed an high correlation with the ECG (around 99% accuracy). In contrast with previous investigations [50, 63, 64], our study has a large sample size (24 participants) and dataset (230400 samples): these elements together are important factors of study validity.
In general, technical features of the camera, body and head movements and ambient lighting are the main causes for the inaccuracy of any rPPG acquisition. Compatibly with the guidelines suggested by the FaceReader Reference Manual about lighting (light diffuse, no strong shadows on the face, preferably from a frontal direction), the camera and its setting (which should be able to capture a frontal view of the subject's face throughout the session with a recommended video resolution: 1280 x 720; frame rate: at least 15 fps, preferred 30 fps; distance between camera and subject: 0.5–1 m) and the skin tones of the participants, our experimental design was specifically built to control all these factors which if not respected would constitute limits to the accuracy of an optimal rPPG measurement. The fact the ICC, which indicates how strongly units in the same group resemble each other, is good (0.75), depends on the way the experimental procedure was conceived: all the participants performed the same task in the same order, under the same experimental conditions, which included stable and constant environmental lighting, temperature and minimization of head and body movements.
In case other commercial rPPG will be developed, future work will be devoted to a more naturalistic assessment and validation of these devices. Our suggestion for future research is to deepen the study of consumer products that can be used without the need for special expertise or sophisticated software and hardware. In fact, our study did not aim to assess the effectiveness and the accuracy of under development rPPG algorithms and methodologies. We aimed to evaluate the precision and accuracy of a consumer product, easily accessible by final users and industrial partners interested in monitoring HR. In this respect, our further studies will explore remote psychophysiological monitoring technologies and, considering its main imaging acquisition issues will include assessment of environmental lighting conditions, correlation with head and body movements, as well as widen the sample and testing conditions. This will allow to evaluate potential variability of the instrument performances with respect to different users’ characteristics (e.g. skin type, ages) and different application scenarios (e.g. clinical settings, fitness environments, driving conditions, working environments).
Conclusion
The FacereaderTM rPPG allows for remote HR measurement through a video camera. Although the Facereader™ rPPG’s algorithm does not represent the state-of-the-art, our assessment revealed that the agreement between the Facereader rPPG and the ECG is poor, with a mean bias of 9.8 bpm compared to the ECG gold standard. The mean bias is highly influenced by the fact that the Facereader tends to over-estimate lower heart rates, and under-estimates higher heart rates compared to the ECG. The error ranges from almost -30 up to +50 bpm. The infancy of this peculiar technology may potentially explain these results. Future investigations will further allow improvement and diffusion of this kind of technology, which has the potential to assess and monitor the personal psychophysical status in a simple, convenient and non-invasive way with important applications beyond clinical patients’ monitoring [66], such as consumer analysis, e-commerce, personal fitness, driving conditions, telemedicine, and customer neuroscience.
Supporting information
(XLSX)
Acknowledgments
We would like to thank Federica Bomben for her precious help with figures editing, as well as the anonymous reviewers for their constructive and useful comments.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This work was supported by TSW XP Lab, which only provided financial support in the form of authors’ salaries [SB, CC, NB] and/or research materials. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Mittelstadt B, Fairweather B, Shaw M, Mcbride N. The Ethical Implications of Personal Health Monitoring. International Journal of Technoethics. 2014;5: 37–60. 10.4018/ijt.2014070104 [DOI] [Google Scholar]
- 2.Lauriks S, Reinersmann A, Roest HGVD, Meiland F, Davies R, Moelaert F, et al. Review of ICT-Based Services for Identified Unmet Needs in People with Dementia. Advanced Information and Knowledge Processing Supporting People with Dementia Using Pervasive Health Technologies. 2010; 37–61. 10.1007/978-1-84882-551-2_4 [DOI] [Google Scholar]
- 3.Pantelopoulos A, Bourbakis NG. A survey on wearable sensor-based systems for health monitoring and prognosis. IEEE Transactions on Systems, Man, and Cybernetics, Part C (Applications and Reviews). 2010; 40(1): 1–12. 10.1109/TSMCC.2009.2032660 [DOI] [Google Scholar]
- 4.Majumder S, Mondal T, Deen M. Wearable Sensors for Remote Health Monitoring. Sensors. 2017;17: 130 10.3390/s17010130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nedungadi P, Jayakumar A, Raman R. Personalized Health Monitoring System for Managing Well-Being in Rural Areas. Journal of Medical Systems. 2017;42 10.1007/s10916-017-0854-9 [DOI] [PubMed] [Google Scholar]
- 6.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal Health Records: Definitions, Benefits, and Strategies for Overcoming Barriers to Adoption. Journal of the American Medical Informatics Association. 2006;13: 121–126. 10.1197/jamia.M2025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agree EM, Freedman VA, Cornman JC, Wolf DA, Marcotte JE. Reconsidering Substitution in Long-Term Care: When Does Assistive Technology Take the Place of Personal Care? The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2005;60 10.1093/geronb/60.5.s272 [DOI] [PubMed] [Google Scholar]
- 8.Kaelber DC, Jha AK, Johnston D, Middleton B, Bates DW. A research agenda for personal health records (PHRs). Journal of the American Medical Informatics Association. 2008; 15(6): 729–736. 10.1197/jamia.M2547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perednia DA. Telemedicine Technology and Clinical Applications. JAMA: The Journal of the American Medical Association. 1995;273: 483 10.1001/jama.1995.03520300057037 [DOI] [PubMed] [Google Scholar]
- 10.Hu PJ, Chau PY, Sheng ORL, Tam KY. Examining the Technology Acceptance Model Using Physician Acceptance of Telemedicine Technology. Journal of Management Information Systems. 1999;16: 91–112. 10.1080/07421222.1999.11518247 [DOI] [Google Scholar]
- 11.Norris AC. Essentials of Telemedicine and Telecare. 2001; 10.1002/0470846348 [DOI] [Google Scholar]
- 12.Martinez AW, Phillips ST, Carrilho E, Thomas SW, Sindi H, Whitesides GM. Simple Telemedicine for Developing Regions: Camera Phones and Paper-Based Microfluidic Devices for Real-Time, Off-Site Diagnosis. Analytical Chemistry. 2008;80: 3699–3707. 10.1021/ac800112r [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao F, Li M, Qian Y, Tsien JZ. Remote Measurements of Heart and Respiration Rates for Telemedicine. PLoS ONE. 2013;8 10.1371/journal.pone.0071384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang Z. Heart rate monitoring from wrist-type photoplethysmographic (PPG) signals during intensive physical exercise. 2014 IEEE Global Conference on Signal and Information Processing (GlobalSIP). 2014; 10.1109/globalsip.2014.7032208 [DOI]
- 15.Wallen MP, Gomersall SR, Keating SE, Wisløff U, Coombes JS. Accuracy of Heart Rate Watches: Implications for Weight Management. Plos One. 2016;11 10.1371/journal.pone.0154420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shcherbina A, Mattsson C, Waggott D, Salisbury H, Christle J, Hastie T, et al. Accuracy in Wrist-Worn, Sensor-Based Measurements of Heart Rate and Energy Expenditure in a Diverse Cohort. Journal of Personalized Medicine. 2017;7: 3 10.3390/jpm7020003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benedetto S, Caldato C, Bazzan E, Greenwood DC, Pensabene V, Actis P. Assessment of the Fitbit Charge 2 for monitoring heart rate. Plos One. 2018;13 10.1371/journal.pone.0192691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adam MT, Krämer J, Müller MB. Auction Fever! How Time Pressure and Social Competition Affect Bidders’ Arousal and Bids in Retail Auctions. Journal of Retailing. 2015;91: 468–485. 10.1016/j.jretai.2015.01.003 [DOI] [Google Scholar]
- 19.Astor PJ, Adam MTP, Jerčić P, Schaaff K, Weinhardt C. Integrating Biosignals into Information Systems: A NeuroIS Tool for Improving Emotion Regulation. Journal of Management Information Systems. 2013;30: 247–278. 10.2753/mis0742-1222300309 [DOI] [Google Scholar]
- 20.Teubner T, Adam M, Riordan R. The Impact of Computerized Agents on Immediate Emotions, Overall Arousal and Bidding Behavior in Electronic Auctions. Journal of the Association for Information Systems. 2015;16: 838–879. 10.17705/1jais.00412 [DOI] [Google Scholar]
- 21.Arnetz BB. Techno-Stress. Journal of Occupational & Environmental Medicine. 1996;38: 53–65. 10.1097/00043764-199601000-00017 [DOI] [PubMed] [Google Scholar]
- 22.Riedl R. On the biology of technostress. ACM SIGMIS Database. 2012;44: 18 10.1145/2436239.2436242 [DOI] [Google Scholar]
- 23.Riedl R, Kindermann H, Auinger A, Javor A. Technostress from a Neurobiological Perspective. Business & Information Systems Engineering. 2012;4: 61–69. 10.1007/s12599-012-0207-7 [DOI] [Google Scholar]
- 24.Fischer T, Halmerbauer G, Meyr E, Riedl R. Blood Pressure Measurement: A Classic of Stress Measurement and Its Role in Technostress Research. Information Systems and Neuroscience Lecture Notes in Information Systems and Organisation. 2017;: 25–35. 10.1007/978-3-319-67431-5_4 [DOI] [Google Scholar]
- 25.Rouast PV, Adam MTP, Chiong R, Cornforth D, Lux E. Remote heart rate measurement using low-cost RGB face video: a technical literature review. Frontiers of Computer Science. 2018;12: 858–872. 10.1007/s11704-016-6243-6 [DOI] [Google Scholar]
- 26.Rouast PV, Adam MTP, Cornforth DJ, Lux E, Weinhardt C. Using Contactless Heart Rate Measurements for Real-Time Assessment of Affective States. Information Systems and Neuroscience Lecture Notes in Information Systems and Organisation. 2016;: 157–163. 10.1007/978-3-319-41402-7_20 [DOI] [Google Scholar]
- 27.Wang YJ, Minor MS. Validity, reliability, and applicability of psychophysiological techniques in marketing research. Psychology and Marketing. 2008;25: 197–232. 10.1002/mar.20206 [DOI] [Google Scholar]
- 28.Souiden N, Ladhari R, Chiadmi N-E. New trends in retailing and services. Journal of Retailing and Consumer Services. 2018; 10.1016/j.jretconser.2018.07.023 [DOI] [Google Scholar]
- 29.Karmarkar U. R., & Plassmann H. (2019). Consumer neuroscience: Past, present, and future. Organizational Research Methods, 22(1), 174–195. [Google Scholar]
- 30.Shaw SD, Bagozzi RP. The neuropsychology of consumer behavior and marketing. Consumer Psychology Review. 2017;1: 22–40. 10.1002/arcp.1006 [DOI] [Google Scholar]
- 31.Rouast P. V., Adam M., & Chiong R. (2019). Deep learning for human affect recognition: insights and new developments. IEEE Transactions on Affective Computing. 10.1109/TAFFC.2017.2678472 [DOI] [Google Scholar]
- 32.Castellini P, Martarelli M, Tomasini E. Laser Doppler Vibrometry: Development of advanced solutions answering to technologys needs. Mechanical Systems and Signal Processing. 2006;20: 1265–1285. 10.1016/j.ymssp.2005.11.015 [DOI] [Google Scholar]
- 33.Melis MD, Morbiducci U, Scalise L, Tomasini E, Delbeke D, Baets R, et al. A preliminary study for the evaluation of large artery stiffness: a non contact approach. Artery Research. 2008;2: 100–101. 10.1016/j.artres.2008.08.343 [DOI] [PubMed] [Google Scholar]
- 34.Nam Y, Kong Y, Reyes B, Reljin N, Chon KH. Monitoring of Heart and Breathing Rates Using Dual Cameras on a Smartphone. Plos One. 2016;11 10.1371/journal.pone.0151013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wieringa FP, Mastik F, Van Der Steen A. F. W. Contactless Multiple Wavelength Photoplethysmographic Imaging: A First Step Toward “SpO2 Camera” Technology. Annals of Biomedical Engineering. 2005;33: 1034–1041. 10.1007/s10439-005-5763-2 [DOI] [PubMed] [Google Scholar]
- 36.Shaffer F, Ginsberg JP. An Overview of Heart Rate Variability Metrics and Norms. Frontiers in Public Health. 2017;5 10.3389/fpubh.2017.00258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zangróniz R, Martínez-Rodrigo A, López M, Pastor J, Fernández-Caballero A. Estimation of Mental Distress from Photoplethysmography. Applied Sciences. 2018;8: 69 10.3390/app8010069 [DOI] [Google Scholar]
- 38.Li G, Chung W-Y. Detection of Driver Drowsiness Using Wavelet Analysis of Heart Rate Variability and a Support Vector Machine Classifier. Sensors. 2013;13: 16494–16511. 10.3390/s131216494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mcduff D, Hurter C, Gonzalez-Franco M. Pulse and vital sign measurement in mixed reality using a HoloLens. Proceedings of the 23rd ACM Symposium on Virtual Reality Software and Technology—VRST 17. 2017; 10.1145/3139131.3139134 [DOI]
- 40.Allen J. Photoplethysmography and its application in clinical physiological measurement. Physiological Measurement. 2007;28 10.1088/0967-3334/28/3/r01 [DOI] [PubMed] [Google Scholar]
- 41.Lindberg L-G. Optical properties of blood in motion. Optical Engineering. 1993;32: 253 10.1117/12.60688 [DOI] [Google Scholar]
- 42.Verkruysse W, Svaasand LO, Nelson JS. Remote plethysmographic imaging using ambient light. Optics Express. 2008;16: 21434 10.1364/oe.16.021434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gastel MV, Stuijk S, Haan GD. Motion Robust Remote-PPG in Infrared. IEEE Transactions on Biomedical Engineering. 2015;62: 1425–1433. 10.1109/TBME.2015.2390261 [DOI] [PubMed] [Google Scholar]
- 44.Mitsuhashi R, Okada G, Kurita K, Kagawa K, Kawahito S, Koopipat C, et al. Noncontact pulse wave detection by two-band infrared video-based measurement on face without visible lighting. Artificial Life and Robotics. 2018;23: 345–352. 10.1007/s10015-018-0430-5 [DOI] [Google Scholar]
- 45.Poh M-Z, Mcduff DJ, Picard RW. Non-contact, automated cardiac pulse measurements using video imaging and blind source separation. Optics Express. 2010;18: 10762 10.1364/OE.18.010762 [DOI] [PubMed] [Google Scholar]
- 46.Lewandowska M, Nowak J. Measuring Pulse Rate with a Webcam. Journal of Medical Imaging and Health Informatics. 2012;2: 87–92. 10.1166/jmihi.2012.1064 [DOI] [Google Scholar]
- 47.Li X, Chen J, Zhao G, Pietikainen M. Remote Heart Rate Measurement from Face Videos under Realistic Situations. 2014 IEEE Conference on Computer Vision and Pattern Recognition. 2014; 10.1109/cvpr.2014.543 [DOI]
- 48.Sviridova N, Zhao T, Aihara K, Nakamura K, Nakano A. Photoplethysmogram at green light: Where does chaos arise from? Chaos, Solitons & Fractals. 2018;116: 157–165. 10.1016/j.chaos.2018.09.016 [DOI] [Google Scholar]
- 49.Wang W, Stuijk S, Haan GD. Exploiting Spatial Redundancy of Image Sensor for Motion Robust rPPG. IEEE Transactions on Biomedical Engineering. 2015;62: 415–425. 10.1109/TBME.2014.2356291 [DOI] [PubMed] [Google Scholar]
- 50.Takano C, Ohta Y. Heart rate measurement based on a time-lapse image. Medical Engineering & Physics. 2007;29: 853–857. 10.1016/j.medengphy.2006.09.006 [DOI] [PubMed] [Google Scholar]
- 51.Tang C, Lu J, Liu J. Non-contact heart rate monitoring by combining convolutional neural network skin detection and remote photoplethysmography via a low-cost camera. IEEE Conference on Computer Vision and Pattern Recognition Workshops. 2018. 1309–1315.
- 52.Chen, W., & McDuff, D. (2018). Deepphys: Video-based physiological measurement using convolutional attention networks. In Proceedings of the European Conference on Computer Vision (ECCV) (pp. 349–365)
- 53.Tasli HE, Gudi A, Ivan P, den Uyl M. European Patent Application No. 2960862A1. 2015
- 54.Gonzalez Viejo C., Fuentes S., Torrico D., & Dunshea F. (2018). Non-Contact Heart Rate and Blood Pressure Estimations from Video Analysis and Machine Learning Modelling Applied to Food Sensory Responses: A Case Study for Chocolate. Sensors, 18(6), 1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wu H, Wang T, Dai T, Lin Y, Wang Y. A Real-Time Vision-Based Heart Rate Measurement Framework for Home Nursing Assistance. Proceedings of the 3rd International Conference on Crowd Science and Engineering—ICCSE18. 2018; 10.1145/3265689.3265718 [DOI]
- 56.Wang W, Brinker ACD, Haan GD. Full video pulse extraction. Biomedical Optics Express. 2018;9: 3898 10.1364/BOE.9.003898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wilson F. N., Johnston F. D., Rosenbaum F. F., & Barker P. S. (1946). On Einthoven's triangle, the theory of unipolar electrocardiographic leads, and the interpretation of the precordial electrocardiogram [DOI] [PubMed] [Google Scholar]
- 58.Cootes TF, Edwards GJ, Taylor CJ. Active appearance models. IEEE Transactions on Pattern Analysis & Machine Intelligence. 2001; 6: 681–685. 10.1109/34.927467 [DOI] [Google Scholar]
- 59.Poh MZ, McDuff DJ, Picard RW. U.S. Patent Application. 2011: No. 13/048,965
- 60.Tasli HE, Gudi A, Uyl MD. Remote PPG based vital sign measurement using adaptive facial regions. 2014 IEEE International Conference on Image Processing (ICIP). 2014; 10.1109/icip.2014.7025282 [DOI]
- 61.Fillmore M. T., Rush C. R., & Hays L. (2006). Acute effects of cocaine in two models of inhibitory control: implications of non‐linear dose effects. Addiction, 101(9), 1323–1332 10.1111/j.1360-0443.2006.01522.x [DOI] [PubMed] [Google Scholar]
- 62.Bland JM, Altman DG. Measuring agreement in method comparison studies. Statistical Methods in Medical Research. 1999;8: 135–160. 10.1177/096228029900800204 [DOI] [PubMed] [Google Scholar]
- 63.Bland JM, Altman DG. Agreement Between Methods of Measurement with Multiple Observations Per Individual. Journal of Biopharmaceutical Statistics. 2007;17: 571–582. 10.1080/10543400701329422 [DOI] [PubMed] [Google Scholar]
- 64.van Gastel MV, Balmaekers B, Verkruysse W, Oetomo SB. Near-continuous non-contact cardiac pulse monitoring in a neonatal intensive care unit in near darkness. Optical Diagnostics and Sensing XVIII: Toward Point-of-Care Diagnostics. 2018; 10.1117/12.2293521 [DOI] [Google Scholar]
- 65.Fukunishi M, Kurita K, Yamamoto S, Tsumura N. Video Based Measurement of Heart Rate and Heart Rate Variability Spectrogram from Estimated Hemoglobin Information. 2018 IEEE/CVF Conference on Computer Vision and Pattern Recognition Workshops (CVPRW). 2018; 10.1109/cvprw.2018.00180 [DOI]
- 66.Green G, Chaichulee S, Villarroel M, Jorge J, Arteta C, Zisserman A et al. Localised photoplethysmography imaging for heart rate estimation of pre-term infants in the clinic. Optical Diagnostics and Sensing XVIII: Toward Point-of-Care Diagnostics. 2018; 10.1117/12.2289759 [DOI] [Google Scholar]